Académique Documents
Professionnel Documents
Culture Documents
Blood & Hematology
Transféré par
Aymen OmerCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Blood & Hematology
Transféré par
Aymen OmerDroits d'auteur :
Formats disponibles
Blood & Hematology
Composition:
the human body is made up mostly of water (~65%)
most (almost 2/3rds) is in our body cells
about 30% in between cells (tissue spaces)
formed elements
45%
the liquid portion of blood
the bodys transport system plays key role in
balancing fluids in the bodys compartments
clear straw colored fluid
plasma consists of:
Marieb
liquid solvent (water) 93%
strictly speaking, blood is not a body fluid like tears,
mucous, or saliva or urine
solutes (7%)
! it is a living tissue consisting of cells within a
liquid matrix
1000s of different solutes
the total blood volume varies due to:
dehydration
hemorrhage
amount of body fat
etc.
most solutes are proteins (=plasma proteins)
also: salts, ions, gasses, hormones,
nutrients, wastes, enzymes
Average person (150lb) has ~5 L (1 gallon) of blood
! some of virtually every chemical found anywhere in the body
can be found in the blood
loss of 15-30% of blood ! pallor and weakness
the new science of epigenetics allows us to extract even
more information from a drop of blood:
loss of >30% ! severe shock, death
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
55% of volume
Plasma
only ~8% of that water is in the
circulatory system
! river of life
plasma
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
about 45% of whole blood
are you a smoker
did you have loving parents
abused as a child
do you live near a busy roadway
what is your socioeconomic status
have you been exposed to pesticides or toxins
erythrocytes (RBCs)
most, 45%, of formed elements
leukocytes (WBCs)
plasma proteins (most solutes are proteins)
thrombocytes (Platelets)
1. albumins (over half of plasma proteins)
of the formed elements only leukocytes are true
(complete) cells
! (with other proteins) contribute to viscosity, osmotic
pressure & blood volume
! helps buffer the blood
! transports many solutes by binding to them:
eg. drugs, penicillin, pigments, fatty acids, bile salts
!RBCs missing nucleus and some organelles
!platelets are small pieces of cells
all three are produced by blood stem cell
2. globulins (over a third of plasma proteins)
! some are antibodies, part of immune system
! some help transport solutes
! some involved in clotting
3. fibrinogen (~4% of plasma proteins)
! soluble precursor to fibrin = framework for clotting
serum = plasma with clotting factors removed
most blood proteins (except gamma globulins) are
synthesized by liver
gamma globulins produced by WBCs
Formed Elements
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
Erythrocytes (Red Blood Cells)
easily deforms to fit through narrow capillaries
Erythropoiesis
most abundant of the three types of formed elements
=formation of RBCs (vs hemopoiesis)
99% of formed elements (2.5 trillion RBCs in whole body)
RBCs are formed from stem cells in bone marrow
main job is to carry oxygen to cells
also deliver some carbon dioxide to lungs
critical nutrients required for hemopoiesis:
RBCs are packed full of hemoglobin molecules
iron, copper, B2(riboflavin) , B12, pyridoxine, & folic acid
in each RBC are 200-300 Million hemoglobin
molecules (transport proteins)
kidneys produce hormone = erythropoietin that
regulates erythropoiesis:
hemoglobin contains 4 Iron (Fe) atoms; 2/3rds of bodys iron is
contained in our bloods hemoglobin
blood doping = injection of erythropoietin
increases O2 carrying capacity of blood
but can cause blood to become too thick
!heart attack
each iron atom can combine with 1 O2 molecule
each hemoglobin molecule can combine with 4 O2s
= oxyhemoglobin
average RBC lives 100-120 days (4 months)
therefore, each RBC can carry ~1 Billion O2 molecules
as they age they become less flexible
RBCs are not true cells since they lack a nucleus
8 million blood cells die each second
RBCs have unique shape = biconcave disc
each day ~230 billion RBCs are replaced
thin center, thick edges
they are destroyed by fragmentation as they
squeeze through capillaries
! high surface/volume ratio
greater efficiency of gas exchange
dead cells removed from blood and destroyed by
macrophages in spleen, liver and marrow
! flexible
5
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
spleen = erythrocyte graveyard
normal:
males:
women:
!since RBCs have an especially hard time squeezing
through its small channels
14-20 g/100ml
12-16 g/100ml
anemia: hemoglobin <12 g/dL or
hemoglobin components are recycled after death and
transported to the liver
some causes of anemia:
hemorrhagic (bleeding)
hemolytic (disease, parasites, drug reactions, genetic)
aplastic (cancer)
Iron deficiency
Pernicious (no B12)
! biliverdin (green) & bilirubin (yellow/orange) ! bile
! iron stored in liver
Some Erythrocyte Disorders
2. Abnormal Hemoglobin
1. Anemias
anemia like symptoms
inability of blood to carry enough O2
! due to not enough RBCs or
! not enough hemoglobin in RBCs
eg. thalassemias
symptoms: pale
lack energy, physical weakness
shortness of breath
difficulty concentration
thin and delicate blood cells
eg. sickle cell
group of inherited diseases that afflicts several million
worldwide
due to low hematocrit:
normal:
men
women
include 80,000 african americans; 1 in 12 black babies in
US carries at least 1 ss gene
42 52%
37 48%
at worst: causes severe episodes of pain, stroke, damage
to internal organs and death
3. Polycythemia (too many RBCs)
anemia: hematocrit is <37%
8-11 million/mm3; hematocrit = 80%
or low hemoglobin
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
Leucocytes (White Blood Cells)
increased viscosity
causes:
overstimulation of stem cells
high altitude
prolonged physical activity
fluid loss
genetic factors
slightly larger than RBCs
are the only true cells of the formed elements
they retain their organelles, including nucleus
large, irregular, lobed nucleus
relatively few are found circulating in blood:
least abundant formed element in blood: 1% of blood volume
numbers are misleading since they do most of
their work outside the blood vessels
mainly function in protection of body as part of
immune system
!attack and destroy bacteria and pathogens
!remove dead cells and tissues
most WBCs are motile by amoeboid motion
(pseudopodia)
! they squeeze out of capillaries into tissue
spaces
5 different kinds of WBCs:
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
the two most common WBCs in a normal blood
sample are neutrophils & lymphocytes
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
10
some WBCs are formed from stem cells in
bone marrow
other WBCs are formed in lymphatic tissue
the others account for only a few % of all
WBCs
their production is also controlled by a hormone
the numbers of each type per unit of blood are
clinically important:
WBCs can live for hours or a lifetime, though most
have short lifespan
= differential WBC count
most WBCs live < 1 week
eg. neutrophils (normally ~65% of WBCs in blood)
dead neutrophils however are responsible for the
creamy color of puss
especially attack bacteria and some fungi
Some Leukocyte Disorders
increase may indicate acute bacterial infections &
appendicitis
1. Leukocytosis (high WBC count)
eg. eosinophils (normally ~3% of WBCs in blood)
total WBC count >10,000/!L
secrete chemicals that weaken or destroy parasitic
worms and dispose of inflammatory chemicals
and allergens
sometimes as high as 400,000/!L
indicate:
acute infections, eg appendicitis
vigorous exercise
excessive loss of body fluids
increase may indicate allergies, parasitic worm
infections
eg. monocytes (normally ~ 30% of WBCs in blood)
destroy dead or dying host and foreign cells and some
chemicals
increase during chronic inflammation (eg. TB) and viral
infections (eg mononucleosis)
eg. Leukemia
cancer characterized by uncontrolled production of
leucocytes
but large numbers are usually nonfunctional
Leucopoiesis
crowd out functioning WBCs
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
11
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
12
Thrombocytes (Platelets)
may become anemic as normal marrow is crowded out
2. Leukopenia (low WBC count)
not whole cells
total WBC count <5,000/mm3
!small, irregular shaped cell fragments
may be due to excessive destruction of WBCs
from bone marrow defects or irradiation
second most abundant formed elements
or may indicate viral infections
diverse functions in stopping the flow of blood
= Hemostasis
eg. influenza, measles, mumps, chickenpox
(NOT Homeostasis)
Hemostasis is a group of chemical cascades that
include:
1. vascular spasm
2. platelet plug
3. clotting cascade
1. vascular spasm
occurs instantly at site of injury
platelets release vasoconstrictors at injury site to
reduce blood loss
2. platelet plug
1-5 seconds after injury platelets become sticky
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
13
adhere to damaged area and to each other
forming a plug
14
fibrin is a protein forming fine threads that
tangle together forming a clot
5. once leak is sealed, platelets release growth
factors to stimulate repair of damaged area
if leak is sealed the process ends
if not hemostasis triggers clotting
6. when tissue repair is complete platelets release
chemicals to dissolve and remove the old clot
3. Blood Clotting
Thrombopoiesis
if injury is extensive clotting cascade is initiated
platelets are formed in red marrow, lungs and spleen
mechanism must be rapid to stop bleeding
formed by fragmentation of large cells
involve over 30 different chemicals
their production is also controlled by hormone
each is activated in a rapid sequence
platelets have a short life span: ~1-2 weeks
= cascade (positive feedback)
if not used they are destroyed by liver or spleen
1. trigger: damage to blood vessel
spleen also stores large numbers of platelets
2. clumps of platelets adhere to site (1-2sec)
! in time of stress (eg. hemorrhage or burns) can
release large numbers into the blood
3. platelets and damaged tissues release clotting
factors that trigger a series of enzymatic
reactions
Some Thrombocyte Disorders
1. Spontaneous Clotting (Thrombus)
4. at last step, thrombin converts circulating
fibrinogen to fibrin
typically clotting is triggered by some kind of
damage to blood vessels
(fibrinogen soluble protein)
(fibrin insoluble protein)
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
15
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
16
body has mechanism that help prevent
spontaneous clotting without vessel damage:
! when extremely low can cause potentially fatal
hemorrhages in intestines or brain
- endothelium is normally very smooth
2. Bleeding Disorders (=Hemophilias)
! platelets do not adhere
inability of blood to clot in normal amount of time
may be caused by
- blood also contains antithrombins
! inactivate thrombin
eg. decreased # of platelets
eg. heparin (a natural blood constituent)
abnormal thrombopoiesis
sometimes clots are triggered by internal factors
eg. liver disease
!rough spots on blood vessels
prothrombin and fibrinogen are produced in liver
require vitamin K (absorbed from intestine)
atherosclerosis may trigger clotting
absorption of vitamin K requires bile
!abnormally slow flow of blood
if bile ducts become obstructed results in
vitamin K deficiency
bedridden or imobilized patients
thrombus a fixed persistant clot
! liver cant produce prothrombin at
normal rate
embolism a traveling clot
eg. inability to form various clotting factors
2. Thrombocytopenia (low platelet count)
typically a genetic cause:
abnormally low number of platelets
eg. factor VIII
(<50,000 platelets /!L)
comprises 83% of cases
! increased risk of internal hemorrhage from
trauma or surgery
eg. factor X
a sex linked condition
! may produce hemorrhagic spots (petechiae) in skin and
sometimes spontaneous bleeding from mucous
membranes
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
17
18
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
Blood Types
leads to (eg.): heart attack
stroke
kidney failure
blood type refers to the kinds of antigens found on
the surface of blood cells (esp RBCs)
*most important consideration in transfusions:
related to immunity and how the body protects itself
from pathogens:
dont want recipient to be able to make
antibodies that would react with donors
antigens
our immune system recognizes and distinguishes
between self and nonself:
while there are 100s of potential antigens on blood
cells
self = all proteins and other chemicals that are part of our
bodies; that belong there
blood transfusions only involve 3 different
antigens in two systems:
nonself = any proteins or chemicals that dont belong
antigen = any foreign substance that enters our
body (generally large organic molecules)
ABO System
antibody = special proteins made by our immune
system to remove foreign substances
there are many potential antigens on surface of blood
cells creating many different blood types
only a few of these antigens are usually important
in transfusions:
involves two different blood antigens:
Blood
Type
A
B
AB
Antigens
antibodies
produced
anti-B
can receive
blood from
A, O
A, AB
anti-A
B, O
B, AB
A&B
neither
A, B, AB, O
AB
none
both
can donate
blood to
(universal recipient)
A, B, AB, O
(universal donor)
ABO system & Rh system
If these antigens are attacked by our antibodies it
causes agglutination (clumping) of blood cells
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
19
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
20
Rh System
Rh factors that get into her blood
Organ Transplants
involves a 3rd blood antigen:
Blood
Type
Rh+
Rh-
Antigens
Rh
antibodies
produced
none
can receive
blood from
Rh+, Rh-
Rh+
none
anti-Rh
Rh-
Rh+, Rh-
blood transfusions = tissue transplants
can donate
blood to
organ transplants are similar in that you dont want to
make antibodies against foreign antigens.
these 3 antigens produce 8 possible blood types
the problem is more complex since not only the 3
blood antigens must be matched
however there are dozens of other potential antigens
on blood cells
they usually dont cause a problem but sometimes
they do
of the 100 or so additional antigens the most
important, after the blood antigens, are 6 tissue
antigens also called HLA antigens
greater success in transplants with closely matched
donors
cross-matching confirms compatability
since many other antigens are present and some
may occasionally cause reactions
eg. Self to self ! autotransplants (autograph) ! completely
compatable
even type O donors must be cross matched
tissue or organ is moved from one place to another in the
same person
Rh incompatability:
eg. hair, bone, skin, bypass surgery
mother is Rh - & fetus is Rh +
eg. toe to thumb
no reaction if normal pregnancy
second such pregnancy antibodies cross placenta
eg. endocrine glands
RhoGAM blocks the mothers immune systems response and prevents
her sensitization to Rh+ blood of child.
if overactive: remove, cut up , freeze some
replace in arm,can more easily adjust
eg. Self, Identical Twins !complete compatability
RhoGAM is a serum containing anti-Rh agglutinins that agglutinate the
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
21
eg. Brother and sister ! 25% chance of match
eg. general public
The chance of a perfect, or six-antigen match, between two
unrelated people is about one in 100,000.
Immunosuppressive Drugs
cyclosporin a drug that selectively knocks out
cells of the immune system most likely to
cause organ rejection
does cause some impairment in bodys ability to
fight infections and cancers
must take it for life
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
23
Human Anatomy & Physiology: Blood & Hematology; Ziser Lecture Notes, 2014.4
22
Vous aimerez peut-être aussi
- Blood &hematologyDocument13 pagesBlood &hematologyAymen OmerPas encore d'évaluation
- BloodDocument7 pagesBloodNaanmatha PuspanathanPas encore d'évaluation
- Blood Anatomy and PhysiologyDocument4 pagesBlood Anatomy and PhysiologyRao Asad MubeenPas encore d'évaluation
- Blood Anatomy Physiology HandoutsDocument6 pagesBlood Anatomy Physiology HandoutsKids JangPas encore d'évaluation
- Blood and Clotting FactorsDocument34 pagesBlood and Clotting FactorsAnand KasiPas encore d'évaluation
- How Blood WorksDocument11 pagesHow Blood Worksalexandruleconiuc6199Pas encore d'évaluation
- Module 2 Blood and Bloostain Analysis Forensic 3Document29 pagesModule 2 Blood and Bloostain Analysis Forensic 3nikke requePas encore d'évaluation
- BloodDocument9 pagesBloodCailah Sofia SelausoPas encore d'évaluation
- Blood CirculatoryDocument5 pagesBlood CirculatoryRekesh SaeedPas encore d'évaluation
- Leukemia Case StudyDocument10 pagesLeukemia Case StudyQueennieMarelRamos100% (1)
- Biochemistry of Diseases Dr. Jishnunil Chakraborty: Analytical Clinical Biochemistry (Sec-A2)Document21 pagesBiochemistry of Diseases Dr. Jishnunil Chakraborty: Analytical Clinical Biochemistry (Sec-A2)Pedro SilvaPas encore d'évaluation
- Biochemistry of Diseases Dr. Jishnunil Chakraborty: Analytical Clinical Biochemistry (Sec-A2)Document28 pagesBiochemistry of Diseases Dr. Jishnunil Chakraborty: Analytical Clinical Biochemistry (Sec-A2)Pedro SilvaPas encore d'évaluation
- Biochemistry of Diseases Dr. Jishnunil Chakraborty: Analytical Clinical Biochemistry (Sec-A2)Document26 pagesBiochemistry of Diseases Dr. Jishnunil Chakraborty: Analytical Clinical Biochemistry (Sec-A2)Pedro SilvaPas encore d'évaluation
- The Blood: Overview of Blood CirculationDocument14 pagesThe Blood: Overview of Blood CirculationHarshil PatelPas encore d'évaluation
- Blood - Structure & FunctionsDocument8 pagesBlood - Structure & FunctionsYhan Brotamonte BoneoPas encore d'évaluation
- Blood Overview and IntroductionDocument8 pagesBlood Overview and IntroductionKathleen Joy Costales MagtanongPas encore d'évaluation
- Cardio Vascular SystemDocument18 pagesCardio Vascular SystemjeniferPas encore d'évaluation
- Tugas Anatomi IntegumenDocument26 pagesTugas Anatomi IntegumenLailia nur rachmaPas encore d'évaluation
- Biol 2301 - Unit 8 - Circulation StudentDocument82 pagesBiol 2301 - Unit 8 - Circulation Studentapi-664744800Pas encore d'évaluation
- Blood Overview and IntroductionDocument8 pagesBlood Overview and IntroductionWai KikiPas encore d'évaluation
- Blood Physiology 1Document78 pagesBlood Physiology 1Jude ChinecheremPas encore d'évaluation
- Blood@Wikipedia Org enDocument18 pagesBlood@Wikipedia Org enHelmiPas encore d'évaluation
- Anatomy and Physiology of BloodDocument9 pagesAnatomy and Physiology of BloodLharra Cagulada-PostranoPas encore d'évaluation
- Blood and CompDocument21 pagesBlood and Compdivyakai143Pas encore d'évaluation
- Blood DisordersDocument12 pagesBlood DisordersDebby Love GoodluckPas encore d'évaluation
- Lec-1 Hematopoiesis and RBCsDocument38 pagesLec-1 Hematopoiesis and RBCsMuna MPas encore d'évaluation
- Solution Manual For Human Biology 16th Edition Sylvia Mader Michael WindelspechtDocument7 pagesSolution Manual For Human Biology 16th Edition Sylvia Mader Michael WindelspechtRobertLynchwxey100% (41)
- IGCSE - BloodDocument7 pagesIGCSE - Bloodmubasherkatbar562Pas encore d'évaluation
- Case Study - LeukemiaDocument18 pagesCase Study - LeukemiaJerome Valdellon100% (1)
- BloodDocument38 pagesBloodchukwukerechimezirimPas encore d'évaluation
- BLOODDocument10 pagesBLOODChrisjohn Aster OsioPas encore d'évaluation
- Blood Is A Body Fluid in Human and Other Animals That Delivers Necessary Substances Such AsDocument24 pagesBlood Is A Body Fluid in Human and Other Animals That Delivers Necessary Substances Such AsPaulo DanielPas encore d'évaluation
- Anatomy and Physiology of LeukemiaDocument7 pagesAnatomy and Physiology of LeukemiaJamaica Aurelio75% (4)
- Aplastic AnemiaDocument7 pagesAplastic Anemianeil052288% (8)
- Module 12 The Composition and Function of BloodDocument11 pagesModule 12 The Composition and Function of BloodMisha WilliamsPas encore d'évaluation
- Blood Components and Their Function: BIS, Grade 8, BiologyDocument24 pagesBlood Components and Their Function: BIS, Grade 8, BiologyUsername18Pas encore d'évaluation
- Anatomi Fisiologi Manusia: HematologiDocument54 pagesAnatomi Fisiologi Manusia: HematologiARUMPas encore d'évaluation
- Lecture 1 Cardiovascular SystemDocument70 pagesLecture 1 Cardiovascular SystemJerilee SoCute WattsPas encore d'évaluation
- Bio Chap 8 Circulatory SystemDocument11 pagesBio Chap 8 Circulatory SystemJyoti AmbwaniPas encore d'évaluation
- A. Functions of Blood SystemDocument7 pagesA. Functions of Blood SystemPrant ChikyPas encore d'évaluation
- Chapter 20 - The Cardiovascular System - Blood Functions of BloodDocument7 pagesChapter 20 - The Cardiovascular System - Blood Functions of Bloodlovelyc95Pas encore d'évaluation
- Acute Myelogenous Leukemia - Patho, Anatomy, and Diagnostic TestDocument66 pagesAcute Myelogenous Leukemia - Patho, Anatomy, and Diagnostic TestCharles Kevin L. Bataga33% (3)
- Blood: What Is It and Why Is It Important?Document31 pagesBlood: What Is It and Why Is It Important?vallalPas encore d'évaluation
- Blood: From Wikipedia, The Free Encyclopedia Jump To:, For Other Uses, SeeDocument26 pagesBlood: From Wikipedia, The Free Encyclopedia Jump To:, For Other Uses, Seestev_brown89Pas encore d'évaluation
- HematologyDocument2 pagesHematologyMohammed Al-RahmaweePas encore d'évaluation
- Lab 25 BloodDocument23 pagesLab 25 Bloodrhycelayon304Pas encore d'évaluation
- Cardiovascular SystemDocument6 pagesCardiovascular Systemchristianoliver.aceroPas encore d'évaluation
- Physical Characteristics and VolumeDocument10 pagesPhysical Characteristics and Volumedeepika kushwahPas encore d'évaluation
- Erythrocytes: The erythrocyte is a biconcave disk between 5 and 7.5 μm inDocument7 pagesErythrocytes: The erythrocyte is a biconcave disk between 5 and 7.5 μm inJoselyn Vilcherrez CruzPas encore d'évaluation
- Bone Marrow Is The Soft, Flexible, Vascular Tissue Found in The Hollow InteriorDocument6 pagesBone Marrow Is The Soft, Flexible, Vascular Tissue Found in The Hollow InteriorIanne Sandra SorrosaPas encore d'évaluation
- Hematology: Shukur Wasman Smail PHD Student in ImmunologyDocument12 pagesHematology: Shukur Wasman Smail PHD Student in ImmunologyShukr Wesman BlbasPas encore d'évaluation
- Red Blood CellsDocument10 pagesRed Blood CellsReyl EspirituosoPas encore d'évaluation
- Nursing Anaphysio ITPDocument8 pagesNursing Anaphysio ITPEköw Santiago JavierPas encore d'évaluation
- Components of BloodDocument20 pagesComponents of BloodVishal SharmaPas encore d'évaluation
- ACTIVITY-7-Blood FINALDocument2 pagesACTIVITY-7-Blood FINALJARISSA DIZON GALLAZAPas encore d'évaluation
- Blood and Its ComponentsDocument22 pagesBlood and Its ComponentsSudhir Singh100% (1)
- Blood and Blood Vessels Module 3Document16 pagesBlood and Blood Vessels Module 3Jenevieve Tungcul SimanganPas encore d'évaluation
- Anatomy CVSDocument84 pagesAnatomy CVShamnafaisall8Pas encore d'évaluation
- Blood BasicsDocument24 pagesBlood BasicsMusallam M. AbukhalilPas encore d'évaluation
- Transplantation &: Tissue RejectionDocument15 pagesTransplantation &: Tissue RejectionAymen OmerPas encore d'évaluation
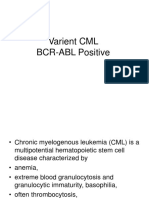
- Varient CML BCR-ABL PositiveDocument11 pagesVarient CML BCR-ABL PositiveAymen OmerPas encore d'évaluation
- Haploidentical Stem Cell Transplant: Zeina Al-Mansour, MDDocument22 pagesHaploidentical Stem Cell Transplant: Zeina Al-Mansour, MDAymen OmerPas encore d'évaluation
- Bacterial Contamination.: Prepared By: Raitha R Suleiman Alexandria University 2018Document13 pagesBacterial Contamination.: Prepared By: Raitha R Suleiman Alexandria University 2018Aymen OmerPas encore d'évaluation
- Chronic GVHD Symptoms: Sandra A. Mitchell, CRNP, M.SC.N., AOCN National Institutes of Health Bethesda, MDDocument5 pagesChronic GVHD Symptoms: Sandra A. Mitchell, CRNP, M.SC.N., AOCN National Institutes of Health Bethesda, MDAymen OmerPas encore d'évaluation
- A GVHDDocument40 pagesA GVHDAymen Omer100% (1)
- Testicular Feminization Syndrome TFM: Ruslan Bayramov .MD Medical Genetics Department Erciyes UniversityDocument25 pagesTesticular Feminization Syndrome TFM: Ruslan Bayramov .MD Medical Genetics Department Erciyes UniversityAymen OmerPas encore d'évaluation
- A Guideline For The Diagnosis and Management of Polycythaemia VeraDocument23 pagesA Guideline For The Diagnosis and Management of Polycythaemia VeraAymen OmerPas encore d'évaluation
- Hepatitis C Virus: Section: 3Document43 pagesHepatitis C Virus: Section: 3Aymen OmerPas encore d'évaluation
- Hypercalcaemia and Hypercalciuria: JamieDocument11 pagesHypercalcaemia and Hypercalciuria: JamieAymen OmerPas encore d'évaluation
- Basic Epidemiologic and Biostatistical Terminology ForDocument15 pagesBasic Epidemiologic and Biostatistical Terminology ForAymen OmerPas encore d'évaluation
- Target BG: Column No.2)Document2 pagesTarget BG: Column No.2)Aymen OmerPas encore d'évaluation
- Platelet CasesDocument13 pagesPlatelet CasesRaheel IftikharPas encore d'évaluation
- Plasma Cell DyscrasiaDocument45 pagesPlasma Cell DyscrasiaAymen OmerPas encore d'évaluation
- Hepatorenal SyndromeDocument4 pagesHepatorenal SyndromeAymen OmerPas encore d'évaluation
- Pharmacolgical Mangment of Diabetic Ketoacidosis: by Suliman OsmanDocument27 pagesPharmacolgical Mangment of Diabetic Ketoacidosis: by Suliman OsmanAymen OmerPas encore d'évaluation
- AMC Recall 1999 To 2008 (Magdi)Document243 pagesAMC Recall 1999 To 2008 (Magdi)zak67% (6)
- Use of Flow Cytometry Immunophenotyping For Diagnosis of Leukemia at Moi Teaching and Referral HospitalDocument24 pagesUse of Flow Cytometry Immunophenotyping For Diagnosis of Leukemia at Moi Teaching and Referral HospitalAymen OmerPas encore d'évaluation
- Dermatology Skin in Systemic DiseaseDocument47 pagesDermatology Skin in Systemic DiseaseNariska CooperPas encore d'évaluation
- Nadee 3Document1 pageNadee 3api-595436597Pas encore d'évaluation
- Lesson 3 - ReviewerDocument6 pagesLesson 3 - ReviewerAdrian MarananPas encore d'évaluation
- Micro Lab Midterm Study GuideDocument15 pagesMicro Lab Midterm Study GuideYvette Salomé NievesPas encore d'évaluation
- John L. Selzer - Merit and Degree in Webster's - The Duchess of MalfiDocument12 pagesJohn L. Selzer - Merit and Degree in Webster's - The Duchess of MalfiDivya AggarwalPas encore d'évaluation
- Rajiv Gandhi University of Health Sciences, Bengaluru, KarnatakaDocument9 pagesRajiv Gandhi University of Health Sciences, Bengaluru, KarnatakaNavin ChandarPas encore d'évaluation
- Sample Resume For Supply Chain Logistics PersonDocument2 pagesSample Resume For Supply Chain Logistics PersonAmmar AbbasPas encore d'évaluation
- BrochureDocument3 pagesBrochureapi-400730798Pas encore d'évaluation
- Where We Are in Place and Time "We Are Part of The Universe and Feel Compelled To Explore It."Document1 pageWhere We Are in Place and Time "We Are Part of The Universe and Feel Compelled To Explore It."Safia-umm Suhaim- FareedPas encore d'évaluation
- How To Configure PowerMACS 4000 As A PROFINET IO Slave With Siemens S7Document20 pagesHow To Configure PowerMACS 4000 As A PROFINET IO Slave With Siemens S7kukaPas encore d'évaluation
- Astm B19Document6 pagesAstm B19Davor IbarraPas encore d'évaluation
- Tool Charts PDFDocument3 pagesTool Charts PDFtebengz100% (2)
- Export Management EconomicsDocument30 pagesExport Management EconomicsYash SampatPas encore d'évaluation
- MCI Approved Medical College in Uzbekistan PDFDocument3 pagesMCI Approved Medical College in Uzbekistan PDFMBBS ABROADPas encore d'évaluation
- Applied Economics 2Document8 pagesApplied Economics 2Sayra HidalgoPas encore d'évaluation
- WAQF Podium Design Presentation 16 April 2018Document23 pagesWAQF Podium Design Presentation 16 April 2018hoodqy99Pas encore d'évaluation
- RFID Seminar AbstractDocument2 pagesRFID Seminar Abstractanushabhagawath80% (5)
- Sociology As A Form of Consciousness - 20231206 - 013840 - 0000Document4 pagesSociology As A Form of Consciousness - 20231206 - 013840 - 0000Gargi sharmaPas encore d'évaluation
- Miguel Augusto Ixpec-Chitay, A097 535 400 (BIA Sept. 16, 2013)Document22 pagesMiguel Augusto Ixpec-Chitay, A097 535 400 (BIA Sept. 16, 2013)Immigrant & Refugee Appellate Center, LLCPas encore d'évaluation
- Book 1518450482Document14 pagesBook 1518450482rajer13Pas encore d'évaluation
- Antena TelnetDocument4 pagesAntena TelnetMarco PiambaPas encore d'évaluation
- CHAPTER 1 SBL NotesDocument13 pagesCHAPTER 1 SBL NotesPrieiya WilliamPas encore d'évaluation
- Bom Details FormatDocument6 pagesBom Details FormatPrince MittalPas encore d'évaluation
- Rom 2 - 0-11 (En)Document132 pagesRom 2 - 0-11 (En)Mara HerreraPas encore d'évaluation
- Delonghi Esam Series Service Info ItalyDocument10 pagesDelonghi Esam Series Service Info ItalyBrko BrkoskiPas encore d'évaluation
- Promotion-Mix (: Tools For IMC)Document11 pagesPromotion-Mix (: Tools For IMC)Mehul RasadiyaPas encore d'évaluation
- Cyber Briefing Series - Paper 2 - FinalDocument24 pagesCyber Briefing Series - Paper 2 - FinalMapacheYorkPas encore d'évaluation
- CV Augusto Brasil Ocampo MedinaDocument4 pagesCV Augusto Brasil Ocampo MedinaAugusto Brasil Ocampo MedinaPas encore d'évaluation
- Sept Dec 2018 Darjeeling CoDocument6 pagesSept Dec 2018 Darjeeling Conajihah zakariaPas encore d'évaluation
- (1921) Manual of Work Garment Manufacture: How To Improve Quality and Reduce CostsDocument102 pages(1921) Manual of Work Garment Manufacture: How To Improve Quality and Reduce CostsHerbert Hillary Booker 2nd100% (1)