Académique Documents
Professionnel Documents
Culture Documents
Pneumonia 1 2015
Transféré par
Min MawCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Pneumonia 1 2015
Transféré par
Min MawDroits d'auteur :
Formats disponibles
NICE Bites
January 2015: No 71
A summary of prescribing recommendations from NICE guidance
Pneumonia
NICE CG191; 2014
This guideline covers the diagnosis and management of
community- and hospital-acquired pneumonia in adults.
Definition of terms
CAP
CRP
LRTI
community-acquired pneumonia
C-reactive protein
lower respiratory tract infection
Assessment
Presentation in primary care
For people with symptoms of LRTI, consider a point of
care CRP test if after clinical assessment a diagnosis of
pneumonia has not been made and it is not clear whether
antibiotics should be prescribed.
Use the results of the CRP test to guide antibiotic
prescribing as follows:
Do NOT routinely offer antibiotic therapy if the CRP
concentration is <20mg/litre,
consider a delayed antibiotic prescription (a prescription
for use at a later date if symptoms worsen) if the CRP
concentration is between 20mg/litre and 100mg/litre,
offer antibiotic therapy if the CRP concentration is
>100mg/litre.
Community-acquired pneumonia
Severity assessment in primary care
When a clinical diagnosis of CAP is made, determine
whether patients are at low, intermediate or high risk of
death using the CRB65 score (see box 1).
Use clinical judgement in conjunction with the CRB65
score to inform decisions about whether patients need
hospital assessment as follows:
score of 0: consider home-based care,
all other patients, particularly if score 2: consider
hospital assessment.
Severity assessment in hospital
Ensure a process is in place to allow diagnosis (including
X-rays) and treatment of CAP within 4 hours of
presentation to hospital.
When a diagnosis of CAP is made at presentation to
hospital, determine whether patients are at low,
intermediate or high risk of death using the CURB65 score
(see box 1).
Use clinical judgement in conjunction with the CURB65
score to guide management, as follows:
score of 0 or 1: consider home-based care,
score 2: consider hospital-based care,
score 3: consider intensive care assessment.
Stratify patients presenting with CAP into those with low-,
moderate- or high-severity disease. The grade of severity
will usually correspond to the risk of death.
Consider measuring a baseline CRP concentration in
patients with CAP on admission to hospital, and repeat the
test if clinical progress is uncertain after 48 to 72 hours.
Microbiological tests
Do NOT routinely offer microbiological tests to patients
with low-severity CAP.
For patients with moderate- or high-severity CAP:
take blood and sputum cultures and consider
pneumococcal and legionella urinary antigen tests.
Pharmacological treatment
Antibiotic therapy
Offer antibiotic therapy as soon as possible after
diagnosis, and certainly within 4 hours to all patients with
CAP admitted to hospital.
Low-severity CAP
Offer a 5-day course of a single antibiotic.
Consider amoxicillin in preference to a macrolide or a
tetracycline except for patients allergic to penicillin.
Consider extending the course of antibiotic for >5 days as
a possible management strategy for patients whose
symptoms do not improve as expected after 3 days.
Explain to patients treated in the community, and when
appropriate their families or carers, they should seek
further medical advice if symptoms do not begin to improve
within 3 days of starting the antibiotic, or earlier if their
symptoms are worsening.
Do NOT routinely offer:
a fluoroquinolone, e.g. levofloxacin,
dual antibiotic therapy.
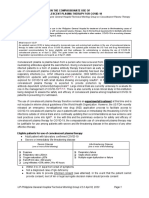
Box 1. Mortality risk assessment
CRB65 score in primary care
CRB65 score is calculated by giving 1 point for each of the following
prognostic features:
confusion (abbreviated Mental Test score 8, or new disorientation
in person, place or time),
raised respiratory rate (30 breaths per minute),
low blood pressure (diastolic 60 mmHg, or systolic <90 mmHg),
age 65 years.
Patients are stratified for risk of death as follows:
0: low risk (<1% mortality risk)
1 or 2: intermediate risk (1to 10% mortality risk)
3 or 4: high risk (>10% mortality risk).
CURB65 score in hospital
CURB65 score is calculated by giving 1 point for each of the following
prognostic features:
confusion (abbreviated Mental Test score 8, or new disorientation
in person, place or time),
raised blood urea nitrogen (>7 mmol/litre),
raised respiratory rate (30 breaths per minute),
low blood pressure (diastolic 60 mmHg, or systolic <90 mmHg),
age 65 years.
Patients are stratified for risk of death as follows:
0 or 1: low risk (<3% mortality risk)
2: intermediate risk (3 to15% mortality risk)
3 to 5: high risk (>15% mortality risk).
Produced for healthcare professionals by North West Medicines Information Service,
The Pharmacy Practice Unit, 70 Pembroke Place, Liverpool, L69 3GF.
Editor: Lindsay Banks. Telephone 0151 794 8117. E-mail: nwmedinfo@nhs.net
NICE Bites
No. 71
Pneumonia
NICE CG191; 2014
Moderate- and high-severity CAP
Consider a 7- to 10-day course of antibiotic therapy.
Moderate-severity CAP: consider dual antibiotic therapy
with amoxicillin and a macrolide e.g. erythromycin,
clarithromycin or azithromycin.
High-severity CAP: consider dual antibiotic therapy with a
macrolide and beta-lactamase stable beta-lactam e.g. coamoxiclav, cefotaxime, ceftaroline fosamil, ceftriaxone,
cefuroxime and piperacillin with tazobactam.
Glucocorticosteroid treatment
Do NOT routinely offer a glucocorticosteroid to patients
unless they have other conditions for which it is indicated.
Discharge from hospital
Do NOT routinely discharge patients with CAP if in the
past 24 hours they have had 2 of the following:
temperature >37.5C,
respiratory rate 24 breaths per minute,
heart rate >100 beats per minute,
systolic blood pressure 90 mmHg
oxygen saturation <90% on room air,
abnormal mental status,
inability to eat and drink without assistance.
Consider delaying discharge for patients if their
temperature is >37.5C.
Counselling
Explain to patients with CAP that after starting treatment
their symptoms should steadily improve, although the rate
of improvement will vary with the severity of the
pneumonia, and most people can expect that by:
1 week: fever should have resolved,
4 weeks: chest pain and sputum production should
have substantially reduced,
6 weeks: cough and breathlessness should have
substantially reduced,
3 months: most symptoms should have resolved but
fatigue may still be present,
6 months: most people will feel back to normal.
Advise patients to consult their healthcare professional if
their condition is deteriorating or not improving as
expected.
Hospital-acquired pneumonia
Offer antibiotic therapy as soon as possible after
diagnosis and certainly within 4 hours.
Choose antibiotic therapy in accordance with local hospital
policy (which should take into account knowledge of local
microbial pathogens) and clinical circumstances.
Consider a 5-to10-day course of antibiotic therapy.
Recommendations wording used such as offer and
consider denote the strength of the recommendation.
Drug recommendations the guideline assumes that
prescribers will use a drugs Summary of Product
Characteristics (SPC) to inform treatment decisions.
See NICE pathway: Pneumonia
The table below lists all NICE guidance included in NICE Bites in 2014
NICE Guidance
NICE Bites
Month/issue number
Atrial fibrillation
NICE CG180: 2014
August 2014/66
Bipolar disorder
NICE CG185: 2014
Nov/Dec 2014/70
Chronic kidney disease
NICE CG182: 2014
September 2014/67
Dyspepsia and gastro-oesophageal reflux
disease
NICE CG184: 2014
October 2014/68
Lipid modification
NICE CG181: 2014
July 2014/65
Long-acting reversible contraception (update)
NICE CG30: 2014
October 2014/69
NICE SC1: 2014
April/May 2014/63
MI: secondary prevention
NICECG172; 2013
January 2014/60
Pressure ulcers: prevention and management
NICE CG179; 2014
June 2014/64
Prostate cancer
NICECG175; 2014
February 2014/61
Psychosis and schizophrenia in adults
NICECG178; 2014
March 2014/62
Managing medicines in care homes
This bulletin summarises key prescribing points from NICE guidance. Please refer to the full guidance at www.nice.org.uk for further detail.
This is an NHS document not to be used for commercial purposes.
Vous aimerez peut-être aussi
- Community-Acquired Pneumonia (CAP) : Why FocusDocument4 pagesCommunity-Acquired Pneumonia (CAP) : Why FocusYoni KomalasariPas encore d'évaluation
- Pediatric Community Acquired Pneumonia Treatment GuidelinesDocument22 pagesPediatric Community Acquired Pneumonia Treatment GuidelinesJeanne Mae Lee AfallaPas encore d'évaluation
- Management of CAP: Recent Guideline in Daily PractisDocument38 pagesManagement of CAP: Recent Guideline in Daily PractisNila hermawatiPas encore d'évaluation
- Community Acquired Pneumonia: - Hafsah GhazaliDocument19 pagesCommunity Acquired Pneumonia: - Hafsah GhazaliCIk ChaPas encore d'évaluation
- Community Acquired Pneumonia: - Hafsah GhazaliDocument19 pagesCommunity Acquired Pneumonia: - Hafsah GhazaliloribyseaPas encore d'évaluation
- Discussion 112Document5 pagesDiscussion 112Frankline otienoPas encore d'évaluation
- ILOCOS TRAINING AND REGIONAL MEDICAL CENTER JUNIOR INTERNS’ EXIT EXAMINATIONDocument6 pagesILOCOS TRAINING AND REGIONAL MEDICAL CENTER JUNIOR INTERNS’ EXIT EXAMINATIONKai SibayanPas encore d'évaluation
- Neutropenic Fever Empiric TherapyDocument5 pagesNeutropenic Fever Empiric TherapyRominaPulvermüllerSalvatierraPas encore d'évaluation
- Protocols Sepsis Treatment Stony BrookDocument6 pagesProtocols Sepsis Treatment Stony BrookVicky Chrystine SianiparPas encore d'évaluation
- Assessment of Community-Acquired Pneumonia Assessment of Community-Acquired PneumoniaDocument10 pagesAssessment of Community-Acquired Pneumonia Assessment of Community-Acquired PneumoniaannisaPas encore d'évaluation
- PCAP ReportDocument28 pagesPCAP ReportAngeline Zamoras-ToledoPas encore d'évaluation
- Management of Adult Febrile Neutropenia: 15011500-10123 99 Street Edmonton, Alberta T5J 3H1Document4 pagesManagement of Adult Febrile Neutropenia: 15011500-10123 99 Street Edmonton, Alberta T5J 3H1Tio Prima SPas encore d'évaluation
- Case Studies of Lower Respiratory Tract InfectionsDocument25 pagesCase Studies of Lower Respiratory Tract InfectionsMarianPas encore d'évaluation
- C-Reactive ProteinDocument11 pagesC-Reactive Proteinshajibabitha67Pas encore d'évaluation
- BCCA Febrile Neutropenia GuidelinesDocument2 pagesBCCA Febrile Neutropenia GuidelinesdenokayuMRPas encore d'évaluation
- Cleveland Clinic Journal of Medicine 2013 BARON 354 9Document6 pagesCleveland Clinic Journal of Medicine 2013 BARON 354 9Stephanie PlascenciaPas encore d'évaluation
- Sepsis - 3Document36 pagesSepsis - 3Mohd Ekhwan DarusPas encore d'évaluation
- Screenshot 2020-03-20 at 08.25.44 PDFDocument10 pagesScreenshot 2020-03-20 at 08.25.44 PDFMiguel Angel Palacios FloresPas encore d'évaluation
- CAP.Document14 pagesCAP.sameh EidPas encore d'évaluation
- Guidelines For The Prevention and Management of Mycobacterium Tuberculosis Infection and Disease in Adult Patients With Chronic Kidney DiseaseDocument12 pagesGuidelines For The Prevention and Management of Mycobacterium Tuberculosis Infection and Disease in Adult Patients With Chronic Kidney DiseaseAnastasia Lilian SuryajayaPas encore d'évaluation
- Pneumonias UpToDateDocument52 pagesPneumonias UpToDateHEBA NAJJARPas encore d'évaluation
- Mark Anthony A. Tom, M.D. First Year Internal Medicine Resident Davao Doctors HospitalDocument55 pagesMark Anthony A. Tom, M.D. First Year Internal Medicine Resident Davao Doctors HospitalMark Anthony TomPas encore d'évaluation
- CAP CURB-65 GuidelinesDocument1 pageCAP CURB-65 GuidelinesAndy LoakPas encore d'évaluation
- Managing Pregnant COVID PatientsDocument17 pagesManaging Pregnant COVID Patientsfariska amanizataPas encore d'évaluation
- Acute Cough (Bronchitis) : 2011 UpdateDocument4 pagesAcute Cough (Bronchitis) : 2011 UpdatecorsaruPas encore d'évaluation
- Return To Work Post Covid CDCDocument5 pagesReturn To Work Post Covid CDCmikaelPas encore d'évaluation
- Cap CPGDocument40 pagesCap CPGMary Joy Oros-VallejeraPas encore d'évaluation
- Httpsentrada - Nusmedicine.nus - Edu.sgfile Event - Phpid 35997 2Document84 pagesHttpsentrada - Nusmedicine.nus - Edu.sgfile Event - Phpid 35997 2Tony NgPas encore d'évaluation
- Pediatric Sepsis Topic DiscussionDocument5 pagesPediatric Sepsis Topic Discussionapi-602288180Pas encore d'évaluation
- Newborn Sepsis GuidelineDocument2 pagesNewborn Sepsis GuidelineAmelia ArnisPas encore d'évaluation
- Pneumonia GuidelinesDocument4 pagesPneumonia GuidelinesFatkhul Ali ImronPas encore d'évaluation
- Clozapine Monitoring GuidelinesDocument3 pagesClozapine Monitoring GuidelinesAntoine JusticePas encore d'évaluation
- ULUAVNIV ProtocolDocument10 pagesULUAVNIV ProtocolsatishPas encore d'évaluation
- Multiple Myeloma Case Studies (Tandem 2017) (Final)Document52 pagesMultiple Myeloma Case Studies (Tandem 2017) (Final)Syed Ali Akbar100% (1)
- Pca PP Revised 6 4 14 v6Document12 pagesPca PP Revised 6 4 14 v6api-244230664Pas encore d'évaluation
- Intensified Antituberculosis Therapy in Adults With Tuberculous MeningitisDocument20 pagesIntensified Antituberculosis Therapy in Adults With Tuberculous MeningitisreginPas encore d'évaluation
- Penatalaksanaan CAPDocument31 pagesPenatalaksanaan CAPushagi-chanPas encore d'évaluation
- Philippine Guidelines on Diagnosis and Management of Community-acquired PneumoniaDocument42 pagesPhilippine Guidelines on Diagnosis and Management of Community-acquired PneumoniaMarion Andrea PoblacionPas encore d'évaluation
- TB CPG DR Jamalul AzizDocument71 pagesTB CPG DR Jamalul AzizSuhazeli AbdullahPas encore d'évaluation
- PACE TrialDocument32 pagesPACE TrialAppu EliasPas encore d'évaluation
- COVID-19 Management ProtocolDocument13 pagesCOVID-19 Management ProtocolajiPas encore d'évaluation
- ACTION TRIAL - Therapeutic Versus Prophylactic Anticoagulation For PatientsDocument22 pagesACTION TRIAL - Therapeutic Versus Prophylactic Anticoagulation For PatientsSheerazPas encore d'évaluation
- PCAP GuidelinesDocument20 pagesPCAP GuidelinesPatricia Anne Collantes90% (20)
- Manage patient conditions with this registry toolDocument24 pagesManage patient conditions with this registry toolPravin NamokarPas encore d'évaluation
- Current Recommendations For The Management of Severe Sepsis & Septic ShockDocument34 pagesCurrent Recommendations For The Management of Severe Sepsis & Septic ShockAmit KochetaPas encore d'évaluation
- Pulmonary Infection GuidelinesDocument16 pagesPulmonary Infection GuidelinesFawad AhmedPas encore d'évaluation
- Pca PP Revised 7 7 14 v7Document12 pagesPca PP Revised 7 7 14 v7api-244230664Pas encore d'évaluation
- Clinical Protocol for DVT ManagementDocument3 pagesClinical Protocol for DVT ManagementAnonymous cwRgUKv2MQ100% (1)
- Managing Cancer Therapy and Supportive CareDocument2 pagesManaging Cancer Therapy and Supportive CareOlive TheresePas encore d'évaluation
- Stroke Management Clinical Practice GuidelinesDocument26 pagesStroke Management Clinical Practice GuidelinesprinsepejessePas encore d'évaluation
- ProcalcitoninDocument1 pageProcalcitoningaelPas encore d'évaluation
- DR. ARIFIN - CAP (New PDPI Guideline)Document36 pagesDR. ARIFIN - CAP (New PDPI Guideline)Inggriht Senny BondangPas encore d'évaluation
- RNTCPDocument38 pagesRNTCPnewzoltPas encore d'évaluation
- Treatment of Pulmonary and Extra-Pulmonary Tuberculosis in AdultsDocument65 pagesTreatment of Pulmonary and Extra-Pulmonary Tuberculosis in AdultsLloyd Daniel BarrantesPas encore d'évaluation
- Pneumonia: Recent Evidence Based UpdatesDocument30 pagesPneumonia: Recent Evidence Based UpdatesAli AzamPas encore d'évaluation
- San Pedro Hospital Case Vignette on Pulmonary TBDocument7 pagesSan Pedro Hospital Case Vignette on Pulmonary TBShareen Joyce AgbayaniPas encore d'évaluation
- COVID-19 Antiviral and Pharmacotherapy Information: PreferentialDocument6 pagesCOVID-19 Antiviral and Pharmacotherapy Information: Preferentialmrosyidn0% (1)
- Deonne Thaddeus V Gauiran PhilippinesDocument25 pagesDeonne Thaddeus V Gauiran PhilippinesKathrine Ann FavoritoPas encore d'évaluation
- Complementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderD'EverandComplementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderPas encore d'évaluation
- USMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsD'EverandUSMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsÉvaluation : 5 sur 5 étoiles5/5 (9)
- Lectures in Paediatric SurgeryDocument86 pagesLectures in Paediatric SurgeryMin MawPas encore d'évaluation
- Final MBDocument17 pagesFinal MBMin MawPas encore d'évaluation
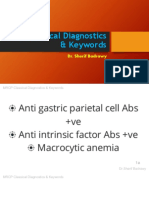
- MRCP Classical Diagnostics KeywordsDocument817 pagesMRCP Classical Diagnostics KeywordsMin MawPas encore d'évaluation
- Abdo Pain in ChildrenDocument31 pagesAbdo Pain in ChildrenMin MawPas encore d'évaluation
- Pneumonia 1 2015Document2 pagesPneumonia 1 2015Min MawPas encore d'évaluation
- High Yield Surgery Shelf ReviewDocument77 pagesHigh Yield Surgery Shelf ReviewDuke71% (7)
- Table of Contents - SurgDocument1 pageTable of Contents - SurgMin MawPas encore d'évaluation
- Common Surg Prob Fetus & NeonateDocument23 pagesCommon Surg Prob Fetus & NeonateMin MawPas encore d'évaluation
- Examining A LumpDocument3 pagesExamining A LumpMin MawPas encore d'évaluation
- ECG MeducationDocument15 pagesECG MeducationMin MawPas encore d'évaluation
- EYE Emergency Manual An Illustrated Guide: Second EditionDocument51 pagesEYE Emergency Manual An Illustrated Guide: Second EditionMin MawPas encore d'évaluation
- Peds OspeDocument85 pagesPeds OspeMin Maw60% (5)
- OSCE Preparation TipsDocument18 pagesOSCE Preparation TipsMin Maw100% (1)
- EYE Emergency Manual An Illustrated Guide: Second EditionDocument51 pagesEYE Emergency Manual An Illustrated Guide: Second EditionMin MawPas encore d'évaluation
- Limit Switch 1LX7001-J AZBILDocument8 pagesLimit Switch 1LX7001-J AZBILHoàng Sơn PhạmPas encore d'évaluation
- Lessons Learned - Risk Management Issues in Genetic Counseling (2007)Document151 pagesLessons Learned - Risk Management Issues in Genetic Counseling (2007)AditiPas encore d'évaluation
- PTW QuestionareDocument63 pagesPTW QuestionareIshtiaq Ahmad100% (2)
- Important instructions on judicial procedure from Narada SmritiDocument6 pagesImportant instructions on judicial procedure from Narada SmritirohitPas encore d'évaluation
- Vee 2003Document14 pagesVee 2003Syed faizan Ali zaidiPas encore d'évaluation
- Epidemiological Cutoff Values For Antifungal Susceptibility TestingDocument36 pagesEpidemiological Cutoff Values For Antifungal Susceptibility Testingdadrrui100% (1)
- Advantages of Computerizing and Networking ComputersDocument5 pagesAdvantages of Computerizing and Networking ComputersIn BioPas encore d'évaluation
- Beuys Begleitheft en ScreenDocument18 pagesBeuys Begleitheft en Screensofijawt0% (1)
- KOREADocument124 pagesKOREAchilla himmudPas encore d'évaluation
- Rostam's Seven LaboursDocument3 pagesRostam's Seven LaboursArifin SohagPas encore d'évaluation
- CFC KIDS FOR CHRIST 2020 FINAL EXAMDocument13 pagesCFC KIDS FOR CHRIST 2020 FINAL EXAMKaisser John Pura AcuñaPas encore d'évaluation
- The Ultimate Manifesting Money Blueprint by Sonia RicottiDocument34 pagesThe Ultimate Manifesting Money Blueprint by Sonia RicottiViolet VioletPas encore d'évaluation
- Format For Handout - Comparative Models of EducationDocument5 pagesFormat For Handout - Comparative Models of EducationAdrian AsiPas encore d'évaluation
- Augustine and The Devil Two BodiesDocument12 pagesAugustine and The Devil Two BodiesAlbert LancePas encore d'évaluation
- 2018 Cambridge Lower Second Progression Test Science Stage 8 QP Paper 2 - tcm143-430409Document16 pages2018 Cambridge Lower Second Progression Test Science Stage 8 QP Paper 2 - tcm143-430409AnisahPas encore d'évaluation
- Messier 88Document3 pagesMessier 88Matheus RochaPas encore d'évaluation
- MRP Format MbaDocument6 pagesMRP Format Mbasankshep panchalPas encore d'évaluation
- ATB Farmacología 2Document194 pagesATB Farmacología 2Ligia CappuzzelloPas encore d'évaluation
- Hope 03 21 22Document3 pagesHope 03 21 22Shaina AgravantePas encore d'évaluation
- (PDF) Teach Your Baby Math - Glenn DomanDocument200 pages(PDF) Teach Your Baby Math - Glenn Domansugapovex0% (1)
- Impacts of DecarbonizationDocument2 pagesImpacts of DecarbonizationCM SoongPas encore d'évaluation
- Macbeth Introduction0Document40 pagesMacbeth Introduction0MohammedelaminePas encore d'évaluation
- Solution Proposal For SGF - BomDocument2 pagesSolution Proposal For SGF - BomABHISHEK ADHIKARYPas encore d'évaluation
- Caribbean Studies - Lesson 8 - Concept and Indicator of Development PDFDocument37 pagesCaribbean Studies - Lesson 8 - Concept and Indicator of Development PDFDarrion BrucePas encore d'évaluation
- NVH PDFDocument3 pagesNVH PDFSubhendu BarisalPas encore d'évaluation
- Catalogue PDFDocument4 pagesCatalogue PDFShivam GuptaPas encore d'évaluation
- Description of Classroom Management PlanDocument10 pagesDescription of Classroom Management Planapi-575843180Pas encore d'évaluation
- Transactionreceipt Ethereum: Transaction IdentifierDocument1 pageTransactionreceipt Ethereum: Transaction IdentifierVALR INVESTMENTPas encore d'évaluation
- Thick Seam Mining Methods and Problems Associated With It: Submitted By: SAURABH SINGHDocument13 pagesThick Seam Mining Methods and Problems Associated With It: Submitted By: SAURABH SINGHPrabhu PrasadPas encore d'évaluation