Académique Documents
Professionnel Documents
Culture Documents
Hospice Care
Transféré par
JoAnne SabaCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Hospice Care
Transféré par
JoAnne SabaDroits d'auteur :
Formats disponibles
Running head: HOSPICE CARE
Hospice Care
JoAnne Saba
California State University, Stanislaus
HOSPICE CARE
2
Hospice Care
Hospice services provide care for clients who have an incurable terminal illness with a
prognosis of six months or less (Tsutsumi, Sekido, & Tanioka, 2014). The intent to provide the
patient with comfort until the end of life. Palliative care, however, aims to reduce the suffering
of a patient regardless of the patient's prognosis (Dobrina, Tenze, & Palese, 2014). Both forms
of care are modeled after the same theories and focus on the patient, the nurse, and the patientnurse relationship while providing care. It is imperative of the nurse in each model to assist the
patient in continuing to have a meaningful life and that the nurse, care environment, and
organization of care are all responsive to the needs of the patient (Sandsdalen, Hov, Hoye,
Rystedt,& Wilde-Larsson, 2015) . As end of life nears, patients tend to have a decline in
physical, psychological, social, and spiritual wellbeing. This paper will examine each in
accordance to Subject A, a specific client visited during the hospice rotation, as well as the the
role of the nurse in hospice care.
Physical Well-Being
As a person progresses toward the end of life, physical capabilities decrease and suffering
informs of pain increase (Tsutsumi, Sekido, & Tanioka, 2014). It is the goal of hospice care to
provide the patient with interventions to minimize the amount of suffering as much as possible.
Subject A was suffering from effects of chronic obstructive pulmonary disease and required
continuous oxygen therapy to reduce the amount of suffering that he or she endured due to
shortness of breath and other breathing difficulties. In addition, he or she required assistance
with mobility and was at high risk for falls due to reduced strength and limited activity tolerance.
He or she also required help with personal care and hygiene. Overall, Subject A has had a
decline in her physical capabilities.
HOSPICE CARE
3
Psychological Well-Being
Sandsdalen, Hov, Hoye, Rystedt, and Wilde-Larsson (2015) have found that
psychological well-being to patients have encompassed continuing to have a meaningful life
despite his or her prognosis. However, psychological well-being for the patient and family
include a strong therapeutic relationship between them and the nurse to ease the family in to the
idea of death (Dobrina, Tenze, & Palese, 2014) . Subject A had advanced stage of
Alzheimers/Dementia causing memory to be effected. This caused assessment of their
psychological well-being to be impaired. The patient presented to be content and was primarily
concerned with the whereabouts of his or her spouse.
Though not all family members were present during the time of the visit, it was apparent
that the psychological well-being was poor. Each member of the family had their own personal
way to cope with the impending death of Subject A. The spouse and one of the children of the
patient displayed nonchalance and annoyance due to the demanding care the patient required.
The other child showed distress toward the situation, however, was bitter over the attitudes of the
others. While the last child showed a positive regard toward the patient and his or her care.
Social Well-Being
Social contact and support is important for a patient even in end-of-life care (Sandsdalen,
Hov, Hoye, Rystedt,& Wilde-Larsson, 2015). An increased need for social support from a
patient's nurse or health care provider comes from a decreased amount of social support from a
patient's family. Adequate social well-being of a patient does not come solely with the length of
a conversation, but also, the quality of the interaction (Tsutsumi, Sekido, & Tanioka, 2014) .
Subject A had adequate social well-being due to the daughter having constant contact with the
HOSPICE CARE
patient and her consistent visits from the home health aide. These two spend time talking with
the patient while the other family members interacted with the patient out of obligation.
Spiritual Well-Being
There is conflicting data in regards to spiritual well-being. Some patients find comfort
and acceptance in their spirituality, while others, associate spiritual practices with death
(Sandsdalen, Hov, Hoye, Rystedt,& Wilde-Larsson, 2015) . There is no set norm and is
dependent on each patient's set of beliefs. Subject A had no apparent spiritual rituals that were
practiced.
Role of the Nurse
It is suggested that the role of the hospice nurse is to provide higher quality medical care
(Tsutsumi, Sekido, & Tanioka, 2014) that is complimentary to the patient's primary health care
provider (Dobrina, Tenze, & Palese, 2014) . Nurses are required to be present for not only their
patients' needs but also to build a therapeutic relationship for the patient and his or her family. It
is imperative that the nurse provide physical and mental relief so that the maximum amount of
comfort is provided and one can be at ease at the end of life.
End-of-life care is more holistic than previously conceived.
It was assumed that
palliative/hospice care focused only on the person nearing death. However, the patient in the
hospice model focuses on the ailing member and supportive family together. Though easing
physical pain and suffering is an essential aspect of end-of-life care, psychological well-being of
the patient and family are equally as important. Strong therapeutic communication skills are
necessary so that the patient/family have a person to express fears concerning death and feel
comfortable doing so.
HOSPICE CARE
5
References
Dobrina, R., Tenze, M., & Palese, A. (2014). An overview of hospice and palliative care nursing
models and theories. Inernational Journal of Palliative Nursing, 20(2), 75-81.
Sandsdalen, T., Hov, R., Hoye, S., Rystedt, I., & Wilde-Larsson, B. (2015). Patients preferences
in palliative care: A systematic mixed studies review. Palliative Medicine. doi:
10.1177/0269216314557882
Tsutsumi, K., Sekido, K. and Tanioka, T. (2014) Characteristics of Nursing Care for Terminally
Ill Patients in Hospice/Palliative Care Unit. Health, 6, 2121-2128.
Vous aimerez peut-être aussi
- Letter of Rec 2Document1 pageLetter of Rec 2JoAnne SabaPas encore d'évaluation
- Letter of Rec 1Document1 pageLetter of Rec 1JoAnne SabaPas encore d'évaluation
- Case Study VDocument2 pagesCase Study VJoAnne SabaPas encore d'évaluation
- Violence Aginst Nurses in The WorkplaceDocument12 pagesViolence Aginst Nurses in The WorkplaceJoAnne Saba100% (1)
- Herpes Simplex EncephalitisDocument11 pagesHerpes Simplex EncephalitisJoAnne SabaPas encore d'évaluation
- Case Study IDocument2 pagesCase Study IJoAnne Saba100% (2)
- Care PlanDocument24 pagesCare PlanJoAnne SabaPas encore d'évaluation
- Population AnalysisDocument31 pagesPopulation AnalysisJoAnne SabaPas encore d'évaluation
- Mexican Culture InterviewDocument17 pagesMexican Culture InterviewJoAnne Saba100% (1)
- HepatitisDocument8 pagesHepatitisJoAnne SabaPas encore d'évaluation
- Family Child AssessmentDocument12 pagesFamily Child AssessmentJoAnne SabaPas encore d'évaluation
- GHP FinalDocument24 pagesGHP FinalJoAnne SabaPas encore d'évaluation
- Ethical FrameworkDocument3 pagesEthical FrameworkJoAnne SabaPas encore d'évaluation
- Disruptive BehaviorsDocument16 pagesDisruptive BehaviorsJoAnne SabaPas encore d'évaluation
- Ethical FrameworkDocument3 pagesEthical FrameworkJoAnne SabaPas encore d'évaluation
- Joanne M. Saba: ObjectiveDocument2 pagesJoanne M. Saba: ObjectiveJoAnne SabaPas encore d'évaluation
- Delegation PaperDocument5 pagesDelegation PaperJoAnne SabaPas encore d'évaluation
- Violence Aginst Nurses in The WorkplaceDocument12 pagesViolence Aginst Nurses in The WorkplaceJoAnne Saba100% (1)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5784)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Nursing Student Guide: Associate in Applied Science (A.A.S.)Document42 pagesNursing Student Guide: Associate in Applied Science (A.A.S.)Kenny SharpensteenPas encore d'évaluation
- 1320-Doctors in Sweden Say There Is A Cure For ArthritisDocument5 pages1320-Doctors in Sweden Say There Is A Cure For Arthritisguapo210% (1)
- TFNDocument83 pagesTFNDarlene TrinidadPas encore d'évaluation
- Pengaruh Kombinasi Pursed-Lip Breathing Dan Guided Imagery Music TerhadapDocument7 pagesPengaruh Kombinasi Pursed-Lip Breathing Dan Guided Imagery Music TerhadapFaisal AmirPas encore d'évaluation
- Food - 5280 - Heath - EF - BC - 9AHeath - Annual - 2021 - UserUpload - NetDocument100 pagesFood - 5280 - Heath - EF - BC - 9AHeath - Annual - 2021 - UserUpload - NetEder OliveiraPas encore d'évaluation
- Vaginal Cleansing Before Unscheduled Cesarean DeliveryDocument14 pagesVaginal Cleansing Before Unscheduled Cesarean Deliveryida husenPas encore d'évaluation
- Olumide Adeola PidanDocument6 pagesOlumide Adeola Pidanpraveenkumar991Pas encore d'évaluation
- Hospital Design Data CollectionDocument59 pagesHospital Design Data CollectionSHERYL SHEKINAH E ARCH-2019 BATCH100% (1)
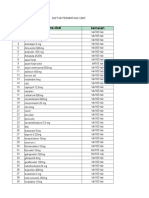
- Permintaan Obat Bulan April 2023Document8 pagesPermintaan Obat Bulan April 2023Putri Nurma SariPas encore d'évaluation
- Kierstens Resume and References-2Document2 pagesKierstens Resume and References-2api-394845409Pas encore d'évaluation
- Public Health Delivery The Role of Informatics and TechnologyDocument19 pagesPublic Health Delivery The Role of Informatics and Technologysbaracaldo2Pas encore d'évaluation
- James Griffiths Consultant em Barnsley Cem Foamed Network: @yorkshumberfoamDocument17 pagesJames Griffiths Consultant em Barnsley Cem Foamed Network: @yorkshumberfoamDede MaulanaPas encore d'évaluation
- Sterne 2020Document3 pagesSterne 2020GARINDA ALMA DUTAPas encore d'évaluation
- 2021 The Social Health Determinants of Health and Cancer FinalDocument17 pages2021 The Social Health Determinants of Health and Cancer FinalMilda InayahPas encore d'évaluation
- Lecture Component: MFR/BLS Draw Up Narcan TrainingDocument6 pagesLecture Component: MFR/BLS Draw Up Narcan TrainingKenneth SoloskyPas encore d'évaluation
- Fundamentals of Patient SafetyDocument2 pagesFundamentals of Patient SafetySarah AjodhaPas encore d'évaluation
- Telemedicine Seminar HMTI v1.5Document25 pagesTelemedicine Seminar HMTI v1.5PriaTongPas encore d'évaluation
- Doctors List - BhopalDocument4 pagesDoctors List - BhopalNaveen Gupta100% (4)
- Reporting in Ethical Principles Group 1 BSN 3ADocument89 pagesReporting in Ethical Principles Group 1 BSN 3AKristine NicolePas encore d'évaluation
- RhinosinusitisDocument8 pagesRhinosinusitisAyuPas encore d'évaluation
- Skenario English Blok 20Document17 pagesSkenario English Blok 20Rohma DwiPas encore d'évaluation
- FWD: UPCM AHEAD Patient Safety Hospital Coordinator Kit: 3 MessagesDocument3 pagesFWD: UPCM AHEAD Patient Safety Hospital Coordinator Kit: 3 MessagesNicoleAbdonPas encore d'évaluation
- Team Leader 2009 Job DescriptionDocument3 pagesTeam Leader 2009 Job DescriptionNCVOPas encore d'évaluation
- Examples of Triage ConditionsDocument9 pagesExamples of Triage ConditionsDevi Christina Damanik (Papua medical School)Pas encore d'évaluation
- JI ManifestoDocument32 pagesJI ManifestoHussain AfzalPas encore d'évaluation
- Biomedicalwastemanagement 180429140745Document39 pagesBiomedicalwastemanagement 180429140745SSR PRASAD KOVELAMUDIPas encore d'évaluation
- 11x17 2010-2011 UC MapDocument1 page11x17 2010-2011 UC MapSukmayati WiharjaPas encore d'évaluation
- Quality of Life in Pregnant Women With and Without ConstipationDocument8 pagesQuality of Life in Pregnant Women With and Without ConstipationMichimichi 78Pas encore d'évaluation
- Work ImmersionDocument3 pagesWork ImmersionV KimPas encore d'évaluation
- Periodontal Assessment and Managment in Fixed ProsthodonticsDocument56 pagesPeriodontal Assessment and Managment in Fixed ProsthodonticsCristina Ene100% (2)