Académique Documents
Professionnel Documents
Culture Documents
UBF Chapter 9
Transféré par
Fait HeeCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
UBF Chapter 9
Transféré par
Fait HeeDroits d'auteur :
Formats disponibles
Urine Screening for Metabolic Disorder
Introduction
Many of the abnormal results are obtained in the routine
urinalysis are related to metabolic rather than renal disease
Urine as an end product of body metabolism may contain
additional abnormal substances not tested for by routine
urinalysis
Positive screening tests can then be followed up with more
sophisticated procedures performed in other sections of the
laboratory
Over Flow vs. Renal Disorders
The appearance of abnormal metabolic substances in the urine
can be caused by a variety of disorders that can be grouped
into 2 categories:
o Renal Type abnormal accumulations are caused by
malfunctions in the tubular reabsorption mechanism
o Overflow Type result from the disruption of a
normal metabolic pathway that causes increased
plasma concentrations of the non-metabolized
substance
Disorders Classified by Defects
Inherited Overflow
Phenylketonuria
Tyrosinemia
Maple Syrup Urine
Disease
Organic Acidemias
Cystinosis
Porphyria
Mucopolysaccharidoses
Galactosemia
Lesch-Nyhan Disease
Metabolic Overflow
Infantile
Tyrosinemia
Melanuria
5-Hydroxyindoleacetic acid
Pophyria
Renal Disorder
Hartnup Disease
Cystinuria
Newborn Screening
Performed primarily to detect and monitor newborns for
inborn error of metabolism
Current state-mandated screening for as many as 29 inborn
errors of metabolism
Urine test are primarily for follow-up
Heel stick blood tests are used for testing
o Performed before infant leaves hospital
o Metabolites appear first in the blood
o Gene testing is being worked on
Phenylalanine-Tyrosine Disorders
Most frequently requested special urinalysis proceudres are
associated with phenylalanine-tyrosine metabolic pathway
Major inherited disorders include:
o Phenylketonuria (PKU)
o Tyrosyluria
o Alkaptonuria
Phenylalanine-Tyrosine Disorders
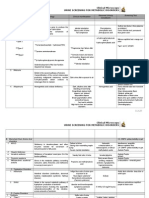
Disorder
Phenylketonuria
Etiology
Abnormal Urinary
Constituents
Clinical manifestation
Failure to inherit the gene to produce
phenylalanine hydroxylase that
converts phenylalanine to tyrosine
Mousy odor urine
Cause decrease production of tyrosine
Severe mental retardation,
and its pigmentation metabolite,
if uncured
Increased amount
melanin
Fair complexion
of keto acids
(phenylpyruvate)
Most well-known of the
aminoacidurias
1:10,000 20,000 births
Laboratory Test
Result
Ferric Chloride Tube Test
(urine)
Urine test for
phenylpyruvic acid
Based upon the ferric
chloride reaction
performed by the tube
test
Nonspecific may react with
other amino acids and
commonly ingested
medications
Permanent blue-green
color
Microbial Inhibition Assay
(blood)
Developed by Guthrie
Growth of Bacillus subtilis
around the paper disk
containing beta-2thienylalanine
Treatment
Eliminate
phenylalanine from
diet (milk)
Alternate pathways
as child matures
Avoid high in
phenylalanine foods
(aspartame)
Other Information
Phenylalanine can be
detected in blood as
early as 4 hours after
birth
Can b detected in urine
in 2 6 weeks
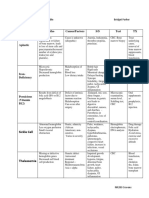
Tyrosyluria
Melanuria
Alkaptonuria
Mental retardation
Type I
Generalized renal
tubular disorder and
progressive liver failure
in infants soo after birth
Type II
Develop corneal erosion
and lesions on the
palms, fingers, soles of
the feet believed to be
caused by crystallization
of tyrosine in the cells
Type III
Result in mental
retardation if dietary
restrictions of
phenylalanine and
tyrosine are not
implemented
Accumulation of excess tyrosine in the
plasma (tyrosinemia) producing
urinary
Either inherited or metabolic defect
Urine may contain excess tyrosine or
its degradation products phydroxyphenylpyruvic acid or phydroxyphenyllactic acid
Increased urinary melanin production
by the second metabolic pathway for
tyrosine
Failure to inherit the gene that
produces the enzyme homogentisic
acid oxidase causing accumulation of
homogentisic acid in the blood, tissues
and urine
Darkened urine
after exposure to
air due increased
urinary melanin
Darkened urine
after after
standing at room
temperature
(alkali lover)
Malignant melanoma
Overproliferation of
melanocytes
Secrete 5,6dihydroxyindole which
oxidizes melanogen to
melanin = dark urine
Brown pigments in the
body (especially in the ear)
and cartilages (arthritis)
Cardiac and liver disorders
Blood from a heelstick is
absorbed into filter paper
circles
Blood-impregnated disks are
then placed on culture media
streaked with the bacterium
Bacillus subtilis
Nitroso-naphthol Test (urine)
Nonspecific
Place 5 drops of urine in
tube
+ 1 mL 2.63 N nitric acid
+ 1 drop 21.5% sodium
nitrite
+ 0.1 mL 1-nitroso-2naphthol
Mix
Wait 5 minutes
Observe color
Increased phenylalanine
levels counteracts the
action of beta-2thienylalanine (inhibitor)
Ferric Chloride Tube Test
(urine)
Green color that fades
rapidly
Ferric Chloride Tube Test
Gray or black precipitate
Red
Reverts back to greenblack color after addition
of glacial acetic acid
Acetone (purple)
Creatinine (amber)
Red
Red
Transient deep blue color
Yellow precipitate
Sodium Nitroprusside Test
Acetest
Ehrlich Reagent
Ferric Chloride Tube Test
Clinitest
Alkalization
Interference: Ascorbic acid
Addition of Silver Nitrate and
Ammonium Hydroxide
Spectrophotometry and
Chromatography
Orange-red color
Darkening of urine
Black urine
Quantitative result
Type I
Deficiency of
fumarylacetoacetate
hydrolase (FAH)
Type II
Lack of tyrosine
aminotransferase
Type III
Lack of phydroxyphenylpyruvi
c acid dioxygenase
Transitory Tryosinemia
Premature infants
Most frequently seen
Due to
underdevelopment
of the liver function
required to produce
enzymes (tyrosine
metabolism
Does not manifest in
early childhood
Observation of brownstained, black-stained
and reddish-stained
disposable diapers
Branched-chain Amino Acid Disorders
Having a methyl group that branches from the main aliphatic carbon chain
Two Major groups
o Accumulation of one or more of the early amino acid degradation products
o Result in accumulation of organic acids produced further down amino acid metabolic pathway
Branched-chain Amino Acid Disorders
Disorder
Maple Syrup Urine
Disorder (MSUD)
Etiology
Failure to inherit the gene for the
enzyme necessary to produce
oxidative carboxylation of the keto
acids from leucine, isoleucine and
valine
Caused by an IEM
Abnormal Urinary
Constituents
Maple syrup odor
due to
accumulation of
keto acids
Clinical manifestation
Failure to thrive after 1
week
Severe mental retardation
Laboratory Test
2,4-Dintirophenylhydrazine
Test
Used for homemonitoring of diagnosed
patients
Not specific for MSUD
Ferric Chloride Tube Test
Acetest
Organic Acidemias
Generalized symptoms:
o Vomiting accompanied by metabolic acidosis, hypoglycemia, ketonuria, and increased serum ammonia
Three most frequently encountered disorders are:
o Isolaveric acidemia
o Propionic acidemia
o Methylmalonic acidemia
Result
Yellow turbidity or
precipitate
Green-gray color
Purple
Treatment
If detected by the 11th
day, dietary regulation
and careful monitoring
of the urinary keto acid
concentrations can
control the disorder
Other Information
Vous aimerez peut-être aussi
- Group 4: Urine Screening for Metabolic DisordersDocument41 pagesGroup 4: Urine Screening for Metabolic DisordersBrent LagartoPas encore d'évaluation
- Metab DisordersDocument36 pagesMetab DisordersDaena TimtimanPas encore d'évaluation
- USMD, CSF, SEMEN - Professor'sDocument10 pagesUSMD, CSF, SEMEN - Professor'sMartin ClydePas encore d'évaluation
- Clinical Microscopy Urine Screening For Metabolic DisordersDocument5 pagesClinical Microscopy Urine Screening For Metabolic DisordersGlazel TulaganPas encore d'évaluation
- Vii. Urine Screening For Metabolic DisordersDocument4 pagesVii. Urine Screening For Metabolic DisordersDee GeePas encore d'évaluation
- Clin Path Trans 3.05 Urinalysis (2b)Document6 pagesClin Path Trans 3.05 Urinalysis (2b)Reymart FernandezPas encore d'évaluation
- Disorders of Cho MetabolismDocument4 pagesDisorders of Cho MetabolismJohn Christopher LucesPas encore d'évaluation
- UrinalysisDocument9 pagesUrinalysisSukma EffendyPas encore d'évaluation
- RBC Tests: MCV, MCH, MCHC, RDW, Polycythemia, AnemiaDocument11 pagesRBC Tests: MCV, MCH, MCHC, RDW, Polycythemia, AnemiaDingdongLopezPas encore d'évaluation
- Urinalysis GuideDocument32 pagesUrinalysis GuideMohamed SaadPas encore d'évaluation
- Examination of Urine Formation and CompositionDocument7 pagesExamination of Urine Formation and CompositionDaniel LamasonPas encore d'évaluation
- AnemiaDocument9 pagesAnemiaMila Canoza HerreraPas encore d'évaluation
- Midterm Chapter7Document43 pagesMidterm Chapter7Frances FranciscoPas encore d'évaluation
- Urinalysis Cases (Revised)Document3 pagesUrinalysis Cases (Revised)Gold NajmPas encore d'évaluation
- Disorders of Aromatic Amino AcidsDocument6 pagesDisorders of Aromatic Amino AcidsJohn Christopher LucesPas encore d'évaluation
- Lab Practical UrinalysisDocument7 pagesLab Practical UrinalysisHeatherIz AwwsomePas encore d'évaluation
- Introduction To UrinalysisDocument8 pagesIntroduction To UrinalysisKyle PicocPas encore d'évaluation
- Synovial Fluid and Fecal Analysis .Group 5Document39 pagesSynovial Fluid and Fecal Analysis .Group 5John Alfrey Dondiego PuebloPas encore d'évaluation
- Anemia Table283Document2 pagesAnemia Table283Bridget ParkerPas encore d'évaluation
- Kidney: Biochemical Tests For Assessing Renal FunctionsDocument56 pagesKidney: Biochemical Tests For Assessing Renal FunctionsPaulina Paskeviciute100% (1)
- Megaloblastic AnaemiaDocument11 pagesMegaloblastic AnaemiaJesmin_36Pas encore d'évaluation
- Complement SystemDocument4 pagesComplement SystemFait HeePas encore d'évaluation
- Analysis of Physical Properties of UrineDocument2 pagesAnalysis of Physical Properties of UrineameerabestPas encore d'évaluation
- Staphylococcus LectureDocument66 pagesStaphylococcus LectureFarhan Azmain FahimPas encore d'évaluation
- Gram Positive Cocci Reviewer 1Document6 pagesGram Positive Cocci Reviewer 1alianaPas encore d'évaluation
- Liver Function Tests Diagnostic GuideDocument2 pagesLiver Function Tests Diagnostic GuideostarburstoPas encore d'évaluation
- Anemia Flow ChartDocument1 pageAnemia Flow ChartCynthiaPas encore d'évaluation
- 'Aliah's Microbiology Notes1Document54 pages'Aliah's Microbiology Notes1Luqman Al-Bashir Fauzi100% (1)
- Sources of Parasitic InfectionDocument74 pagesSources of Parasitic InfectionCristy Jean100% (1)
- Renal SyndromeDocument13 pagesRenal SyndromeAndreas KristianPas encore d'évaluation
- Screening Test For Phagocytic Engulfment: DiapedesisDocument2 pagesScreening Test For Phagocytic Engulfment: DiapedesisBianca APas encore d'évaluation
- 06.2 Inborn Error of Metabolism - Iii B - Trans PDFDocument10 pages06.2 Inborn Error of Metabolism - Iii B - Trans PDFAshim AbhiPas encore d'évaluation
- Analytical EpidemiologyDocument7 pagesAnalytical EpidemiologySamridhi SrivastavaPas encore d'évaluation
- Biochem TestsDocument27 pagesBiochem TestsSteph VeePas encore d'évaluation
- Haematology-Summary My NotesDocument24 pagesHaematology-Summary My NotesToria053Pas encore d'évaluation
- Epilepsy: Causes of Seizures (Non-Epileptic)Document5 pagesEpilepsy: Causes of Seizures (Non-Epileptic)humdingerPas encore d'évaluation
- Red Blood Cell Anomalies: Elliptocytes & Oval MacrocyteDocument12 pagesRed Blood Cell Anomalies: Elliptocytes & Oval MacrocyteSHUPATUSSAI100% (1)
- Non Protein CompoundsDocument64 pagesNon Protein CompoundsAbigail Mayled LausPas encore d'évaluation
- Subcutaneous & Systemic MycosesDocument7 pagesSubcutaneous & Systemic MycosesDee GeePas encore d'évaluation
- Virlogy Made AwesomeDocument6 pagesVirlogy Made AwesomeUsman Ali AkbarPas encore d'évaluation
- Proteinuria in Adults and Diagnostic ApproachDocument9 pagesProteinuria in Adults and Diagnostic ApproachCindy JAPas encore d'évaluation
- Clinical Pathology ReviewDocument11 pagesClinical Pathology Reviewrob hPas encore d'évaluation
- Urine Case 2010-2Document9 pagesUrine Case 2010-2hendra_darmawan_4Pas encore d'évaluation
- CBCDocument12 pagesCBCDaNa Al-jomah100% (1)
- AnemiaDocument71 pagesAnemiaAnsu MaliyakalPas encore d'évaluation
- Haematopathology 3:: Leucocytosis/LeucopeniaDocument113 pagesHaematopathology 3:: Leucocytosis/LeucopeniaarwaPas encore d'évaluation
- Abnormal White Blood Cells Identification GuideDocument4 pagesAbnormal White Blood Cells Identification GuideBryan James LinPas encore d'évaluation
- Parasitic AmoebaDocument23 pagesParasitic AmoebaJethrö MallariPas encore d'évaluation
- NephroticDocument8 pagesNephroticsangheetaPas encore d'évaluation
- RBC DisordersDocument19 pagesRBC DisordersAbhiram KrishnaPas encore d'évaluation
- RBC DisordersDocument27 pagesRBC Disordersbpt2100% (1)
- Normal Lab Values (USMLE Step 1)Document12 pagesNormal Lab Values (USMLE Step 1)nmp274Pas encore d'évaluation
- Pre-Analytical Considerations in PhlebotomyDocument56 pagesPre-Analytical Considerations in PhlebotomyAngel joyce ValenciaPas encore d'évaluation
- Clinical Pathology 3-6 UrinalysisDocument3 pagesClinical Pathology 3-6 UrinalysisAndrew KalawPas encore d'évaluation
- TRACE ELEMENTS: BIOLOGICAL FUNCTIONS AND IRON DEFICIENCY ANEMIADocument7 pagesTRACE ELEMENTS: BIOLOGICAL FUNCTIONS AND IRON DEFICIENCY ANEMIAVinPas encore d'évaluation
- Systemic Lupus Erythematosus Lecture Salah Abdel BakyDocument8 pagesSystemic Lupus Erythematosus Lecture Salah Abdel Bakyahmed gabrPas encore d'évaluation
- 07 Pathological ClacificationDocument10 pages07 Pathological Clacificationraanja2Pas encore d'évaluation
- Metabolic Disorders GuideDocument80 pagesMetabolic Disorders GuideXeniyaFedoryakPas encore d'évaluation
- Problem-based Approach to Gastroenterology and HepatologyD'EverandProblem-based Approach to Gastroenterology and HepatologyJohn N. PlevrisPas encore d'évaluation
- Item IDocument123 pagesItem IFait HeePas encore d'évaluation
- EXECUTIVE ORDER NO. 200 June 18, 1987 (Links To An External Site.)Document5 pagesEXECUTIVE ORDER NO. 200 June 18, 1987 (Links To An External Site.)Fait HeePas encore d'évaluation
- ContinuationDocument2 pagesContinuationFait HeePas encore d'évaluation
- 31Document2 pages31Fait HeePas encore d'évaluation
- NationalityDocument85 pagesNationalityFait HeePas encore d'évaluation
- Digests TST StsDocument18 pagesDigests TST StsFait HeePas encore d'évaluation
- NationalityDocument85 pagesNationalityFait HeePas encore d'évaluation
- PALE Pre NoteDocument22 pagesPALE Pre NoteFait HeePas encore d'évaluation
- HLI Full TextDocument224 pagesHLI Full TextFait HeePas encore d'évaluation
- Lutz vs. Araneta, 98 Phil 148, G.R. No. L-7859, 22 December 1955Document7 pagesLutz vs. Araneta, 98 Phil 148, G.R. No. L-7859, 22 December 1955Fait HeePas encore d'évaluation
- 31Document2 pages31Fait HeePas encore d'évaluation
- LTD HomeworkDocument52 pagesLTD HomeworkFait HeePas encore d'évaluation
- Cir V. Ca G.R. No. 119322 FactsDocument2 pagesCir V. Ca G.R. No. 119322 FactsFait HeePas encore d'évaluation
- 2020 PALE OutlineDocument10 pages2020 PALE OutlineRyoPas encore d'évaluation
- Mactan Cebu Airport Authority Tax Exemption RepealDocument34 pagesMactan Cebu Airport Authority Tax Exemption RepealFait Hee100% (1)
- Complement SystemDocument4 pagesComplement SystemFait HeePas encore d'évaluation
- Transpo Digests 11 20Document11 pagesTranspo Digests 11 20Phoebe BalubarPas encore d'évaluation
- Cred CasesDocument22 pagesCred CasesFait HeePas encore d'évaluation
- Case Digest - Legal Ethics 020417Document16 pagesCase Digest - Legal Ethics 020417Fait HeePas encore d'évaluation
- Court Rules on Validity of Contracts of Sale and Homestead PatentsDocument3 pagesCourt Rules on Validity of Contracts of Sale and Homestead PatentsFait HeePas encore d'évaluation
- Adr ReportDocument2 pagesAdr ReportFait HeePas encore d'évaluation
- PFR Digests 2Document8 pagesPFR Digests 2Fait HeePas encore d'évaluation
- Registered Land Sale DeedDocument2 pagesRegistered Land Sale DeedFait Hee100% (1)
- Virology FinalsDocument8 pagesVirology FinalsFait HeePas encore d'évaluation
- Ra 7719 Blood Bank MT-B & C 8Document7 pagesRa 7719 Blood Bank MT-B & C 8Fait Hee100% (1)
- Cases - Consti 2 022417 Priority Cases 2Document75 pagesCases - Consti 2 022417 Priority Cases 2Fait HeePas encore d'évaluation
- Rule 126Document3 pagesRule 126Carlie MaePas encore d'évaluation
- Cred CasesDocument22 pagesCred CasesFait HeePas encore d'évaluation
- Case Digest - Consti 2 Ang Tibay - PurugananDocument67 pagesCase Digest - Consti 2 Ang Tibay - PurugananFait HeePas encore d'évaluation
- Case - Crim 2 People Vs Garcia 021517Document7 pagesCase - Crim 2 People Vs Garcia 021517Fait HeePas encore d'évaluation
- FortiEDR Product Overview TrainingDocument16 pagesFortiEDR Product Overview TrainingRafael Steven Soto del CampoPas encore d'évaluation
- Exery Analysis of Vapour Compression Refrigeration SystemDocument22 pagesExery Analysis of Vapour Compression Refrigeration Systemthprasads8356Pas encore d'évaluation
- LP Direct & Indirect SpeechDocument7 pagesLP Direct & Indirect SpeechJoana JoaquinPas encore d'évaluation
- 6710 NotesDocument45 pages6710 NotesAndrés SuquilloPas encore d'évaluation
- Precode Hollywood Movies and The Case of Busby BerkeleyDocument14 pagesPrecode Hollywood Movies and The Case of Busby Berkeleystessy92Pas encore d'évaluation
- GEY 102-Introduction To Geology 1-Lecture Slides - Prof. M.E. NtonDocument44 pagesGEY 102-Introduction To Geology 1-Lecture Slides - Prof. M.E. Ntonabuabdmuqseet2001Pas encore d'évaluation
- Evolution and Diversity of Coleochaete, Charales, and Green PlantsDocument4 pagesEvolution and Diversity of Coleochaete, Charales, and Green PlantsAndrei PusungPas encore d'évaluation
- Director VP Program Manager in Raleigh NC Resume Mary Paige ForresterDocument6 pagesDirector VP Program Manager in Raleigh NC Resume Mary Paige ForresterMaryPaigeForresterPas encore d'évaluation
- Personal Assistant With Telegram & ArduinoDocument8 pagesPersonal Assistant With Telegram & ArduinoAbhijit PattnaikPas encore d'évaluation
- 1 Prepositions With AnswersDocument6 pages1 Prepositions With AnswersManal El ShafiePas encore d'évaluation
- DualSPHysics v4.0 GUIDE PDFDocument140 pagesDualSPHysics v4.0 GUIDE PDFFelipe A Maldonado GPas encore d'évaluation
- Understanding Culture, Society, and Politics - IntroductionDocument55 pagesUnderstanding Culture, Society, and Politics - IntroductionTeacher DennisPas encore d'évaluation
- Adolescent HealthDocument19 pagesAdolescent Healthhou1212!67% (3)
- Solución: R T β T R (T) = 1000 Ω ΩDocument6 pagesSolución: R T β T R (T) = 1000 Ω ΩDuvan BayonaPas encore d'évaluation
- Conservation of Arabic ManuscriptsDocument46 pagesConservation of Arabic ManuscriptsDr. M. A. UmarPas encore d'évaluation
- Divorce Bill in The PhilippinesDocument19 pagesDivorce Bill in The PhilippinesNeiqui Aubrey Antaran CañetePas encore d'évaluation
- DragonDreaming International Ebook v02.03-2Document28 pagesDragonDreaming International Ebook v02.03-2Tim LueschenPas encore d'évaluation
- Africa S Top 15 Cities in 2030Document10 pagesAfrica S Top 15 Cities in 2030loca018Pas encore d'évaluation
- Word Meanings From ContextDocument4 pagesWord Meanings From ContextUsagi Yuki AnaPas encore d'évaluation
- Physics EducationDocument14 pagesPhysics Educationchrisuche100% (2)
- Aircrew Standards Manual FY2015 V1Document211 pagesAircrew Standards Manual FY2015 V1Anonymous Pb39klJ100% (1)
- 9 Oet Reading Summary 2.0-195-213Document19 pages9 Oet Reading Summary 2.0-195-213Vijayalakshmi Narayanaswami0% (1)
- PZO9401 Second Darkness Players Guide PDFDocument36 pagesPZO9401 Second Darkness Players Guide PDFAllan ChuaPas encore d'évaluation
- List of Private Schools in Batangas SY 2016-2017Document9 pagesList of Private Schools in Batangas SY 2016-2017Lucky MalihanPas encore d'évaluation
- Khulasa Al MadadDocument5 pagesKhulasa Al Madadmirwana100% (1)
- Balancing The Cybersecurity BattlefieldDocument4 pagesBalancing The Cybersecurity BattlefieldLilminowPas encore d'évaluation
- Past PaperDocument3 pagesPast PaperKyle CuschieriPas encore d'évaluation
- AripiprazoleDocument2 pagesAripiprazoleKrisianne Mae Lorenzo FranciscoPas encore d'évaluation
- Distinguish Opinion From TruthDocument12 pagesDistinguish Opinion From TruthMAR ANTERO R. CENIZA100% (2)
- GUINNESS F13 Full Year BriefingDocument27 pagesGUINNESS F13 Full Year BriefingImoUstino ImoPas encore d'évaluation