Académique Documents
Professionnel Documents
Culture Documents
0915RT Mini Cousins Wolfe Yonekawa
Transféré par
PrissilmaTaniaCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
0915RT Mini Cousins Wolfe Yonekawa
Transféré par
PrissilmaTaniaDroits d'auteur :
Formats disponibles
SPECIAL FOCUS DRUG DELIVERY
Intravitreal Implant
Options for Patients
With Diabetic Eye
Disease
The following articles discuss the use of the two intravitreal corticosteroids approved for
treatment of diabetic macular edema, as well as other indications.
Treatment of DME With
the 0.19-mg Fluocinolone
Acetonide Implant
Dexamethasone Intravitreal
Implant: Pharmacology and
Clinical Update
By Scott W. Cousins, MD
By Yoshihiro Yonekawa, MD; and Jeremy D. Wolfe, MD
s part of this review of sustained-release
steroid implants, I will discuss the 0.19-mg
fluocinolone acetonide intravitreal implant
(Iluvien, Alimera Sciences) in the setting
of managing patients with diabetes. But first, let us
acknowledge that the multiple comorbidities associated with diabetes often limit patients abilities to
receive the optimal course of anti-VEGF therapy that
adequately manages diabetic macular edema (DME).
LIMITED RESPONSE TO ANTI-VEGF TREATMENT
Unfortunately, some patients with DMEeven those
who adhere to the burdensome treatment regimen of
anti-VEGF injectionsdo not respond to anti-VEGF treatment. In fact, in the DRCR.net Protocol I study, approximately 50% of patients did not adequately respond to
anti-VEGF therapy.1 A post-hoc analysis of the DRCR.net
Protocol I study demonstrated that this disparity is not a
function of the number of injections a patient received,
as inconsistent responders and nonresponders averaged
more injections than responders.2 The recently published
DRCR.net Protocol T study data also illustrated that many
(Continued on page 58)
54RETINA TODAYSEPTEMBER 2015
he dexamethasone intravitreal implant
(Ozurdex, Allergan) is approved by the US
Food and Drug Administration (FDA) for the
treatment of diabetic macular edema (DME),1
macular edema associated with retinal vein occlusion
(RVO),2 and noninfectious posterior uveitis.3 It delivers
a potent corticosteroid via a biodegradable polymer
that gradually disintegrates into water and carbon
dioxide while the medication is released in a sustained
and safe dose over several months.4
Corticosteroids have a broad spectrum of biologic
action, including down-regulation of inflammatory
cytokines, endothelial adhesion molecules, and
growth factors such as VEGF, giving this class of drug
antiinflammatory, antivascular permeability, and
antiangiogenic effects, respectively.4 These molecular
mechanisms are dysregulated in many vitreoretinal
diseases to varying degrees, making corticosteroids
effective treatment options for a number of disease
states. However, not all corticosteroids are the same,
and their varying chemical structures result in different clinical properties.
(Continued on page 55)
SPECIAL FOCUS DRUG DELIVERY
In our practice, we most commonly
use the dexamethasone
intravitreal implant in patients
with DME and RVO who respond
poorly to anti-VEGF agents.
WATER SOLUBILITY
Triamcinolone is minimally water-soluble and becomes
a depot of crystals that release steroid, resulting in a long
half-life.5 Conversely, dexamethasone has two additional
hydroxyl groups in the acetonide functional group, making it significantly more hydrophilic compared with triamcinolone and fluocinolone.6 Water solubility has two
benefits: a shorter half-life, which makes it amenable as a
sustained-release medication by allowing controlled and
steady release6; and less aggregation onto ocular structures
such as the trabecular meshwork,7 which appears to result
in lower rates of intraocular pressure (IOP) elevation.
IOP CONSIDERATIONS
When using intravitreal corticosteroids in our practice, we
ensure that patients have a clear understanding of the risk
for cataract progression and possible ocular hypertension.
We find that patients are less concerned about cataract,
viewing cataract surgery as a matter of when rather than if.
Most patients are accepting of drops for ocular hypertension, but glaucoma surgery is always an undesirable course.
Among the various intravitreal steroid options, the dexamethasone intravitreal implant has a favorable IOP profile.
In the MEAD trial, incisional glaucoma surgery was
required in 0.6% of patients with DME treated with the
700-g dose of the dexamethasone intravitreal implant.1
By comparison, 33.8% of patients treated with the 0.59-mg
fluocinolone acetonide implant (Retisert, Bausch + Lomb),8
4.8% of patients treated with the 0.19-mg fluocinolone acetonide implant (Iluvien, Alimera Sciences),9 and 1.2% treated
with 4.0mg of intravitreal triamcinolone10,11 required incisional glaucoma surgery in the respective large clinical trials
evaluating these therapies in patients with DME.
As reflected in the MEAD study results, we find that
IOP elevation with the dexamethasone intravitreal
implant is mild and predictable. These elevations peak
at 6 to 8 weeks after injection and then return to close
to baseline by 3 or 4 months.1 In our practice, we have
not experienced the so-called staircase progressive IOP
elevation with repeated injections as is sometimes seen
with triamcinolone. IOP elevation with triamcinolone
also appears to be less predictable in terms of timing
(several days to many months)12 and severity (between
70-80mmHg).13-15 On the other hand, 89% of patients
who developed ocular hypertension at any point during
the MEAD trial did so within the first three injections,
and 99% of patients who developed ocular hypertension
did so within the first four injections.16 This means that
if a patient has not demonstrated an IOP spike by the
third or fourth injection, it is unlikely that he or she will
do so after future injections.
CLINICAL APPLICATION
Clinical application of the dexamethasone intravitreal
implant is broad, and many studies have reported on
usages beyond FDA-approved indications. Its efficacy has
been demonstrated in use for macular edema after cataract surgery,17-19 retinal detachment repair,19,20 epiretinal
membrane peeling,19,21 radiation maculopathy,22,23 retinitis pigmentosa,24,25 and in combination with anti-VEGF
agents for neovascular age-related macular degeneration.26
Pediatric uses have also been described.27,28
In our practice, we most commonly use the dexamethasone intravitreal implant in patients with DME and RVO
who respond poorly to anti-VEGF agents. The literature
supports the efficacy of the dexamethasone intravitreal
implant as rescue treatment for recalcitrant DME29-31 as
well as branch and central RVO.31,32 The controversial
question is when to switch to the dexamethasone intravitreal implantin other words, after how many ineffective
anti-VEGF injections do you consider a patient to be a poor
anti-VEGF responder?
SWITCHING THERAPY
It has been demonstrated that if central retinal thickness
does not decrease by at least 25% after the first anti-VEGF
injection in patients with RVO, the patient is likely to be a
poor responder regardless of the number of injections.33
Similar findings have been reported in DME patients (Shah
AR, et al, unpublished data). We are therefore comfortable
switching to the dexamethasone intravitreal implant relatively early, and these patients often respond well (Figure).
VITRECTOMIZED EYES
There is controversy over the faster clearance of
anti-VEGF agents34,35 and triamcinolone36 in eyes that
have undergone vitrectomy. The dexamethasone intravitreal implant, as well as other sustained-release products, have theoretical advantages in vitrectomized eyes
because cleared corticosteroid is immediately replaced
by more elution of medication.37 Studies have shown
the efficacy of the dexamethasone intravitreal implant
in vitrectomized eyes with uveitic cystoid macular
edema,38 DME,39 and RVO.40
SEPTEMBER 2015RETINA TODAY55
SPECIAL FOCUS DRUG DELIVERY
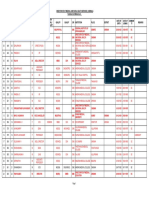
Figure. The efficacy of the dexamethasone intravitreal implant for DME with poor response to anti-VEGF agents is
illustrated. The patients eye had previously undergone vitrectomy for nonclearing vitreous hemorrhage (A). DME was
treated with ranibizumab 0.3 mg (Lucentis, Genentech; A). There was a subtle response seen 5 weeks after injection (B).
The patient returned after 11 weeks with worsening intraretinal fluid (C). Aflibercept (Eylea, Regeneron) was administered.
There was minimal response seen after 6 weeks, and another aflibercept injection was used (D). There was worsening of
edema 8 weeks subsequently, and the patient was switched to the dexamethasone intravitreal implant (E). The edema
acutely resolved for the first time, seen 7 weeks after injection of the dexamethasone intravitreal implant (F). There was
mild intraretinal fluid on follow-up examination 8 weeks later, and aflibercept was administered (G). The edema worsened
8 weeks later, and it was decided to resume treatment with the dexamethasone intravitreal implant (H). The edema
resolved 8 weeks subsequently (I). The patient remains on the dexamethasone intravitreal implant every 3 to 4 months
on an as-needed basis, demonstrating excellent control of edema for more than a year.
ADVANTAGE OF A DRAWBACK
The dexamethasone intravitreal implant and the two
fluocinolone acetonide implants are all sustained-release
devices, but they differ in their durations of action. The
fluocinolone implants were designed to last for 3 years.
Significantly fewer injections are required, but, once the
implant is placed, the eye is committed to potentially
3 years of steroid exposure and accompanying IOP
complications. On the other hand, the dexamethasone
intravitreal implant, while initially designed to last for
6 months, usually provides clinically meaningful effects
for 3 to 4 months based on our experience with refractory edema. The drawback of requiring more injections
becomes an advantage when managing IOP issues,
because the steroid effects subside sooner.
CONCLUSION
The dexamethasone intravitreal implant is an efficacious steroid delivery system that provides sustained
release of a safe and potent steroid in a controlled and
56RETINA TODAYSEPTEMBER 2015
predictable manner. It has played an important role in
our practices treatment paradigms for retinovascular
disorders and posterior uveitis. n
Yoshihiro Yonekawa, MD, is a second-year
vitreoretinal surgery fellow at Associated
Retinal Consultants/William Beaumont
Hospital in Royal Oak, Mich. He reports no
conflicts of interest. Dr. Yonekawa may be
reached at yoshihiro.yonekawa@beaumont.org.
Jeremy D. Wolfe, MD, is a partner at
Associated Retinal Consultants, Royal Oak,
Mich., and assistant professor of Ophthalmology
at Oakland University William Beaumont
School of Medicine. He is a consultant for
Allergan, Alimera, and Genentech. Dr. Wolfe
may be reached at jwolfe@arcpc.net.
1. Boyer DS, Yoon YH, Belfort R, et al. Three-year, randomized, sham-controlled trial of dexamethasone
intravitreal implant in patients with diabetic macular edema. Ophthalmology. 2014;121:1904-1914.
2. Haller JA, Bandello F, Belfort R, et al. Dexamethasone intravitreal implant in patients with macular edema related
SPECIAL FOCUS DRUG DELIVERY
to branch or central retinal vein occlusion twelve-month study results. Ophthalmology. 2011;118:2453-2460.
3. Lowder C, Belfort R, Lightman S, et al. Dexamethasone intravitreal implant for noninfectious intermediate or
posterior uveitis. Arch Ophthalmol. 2011;129:545-553.
4. Kuppermann BD, Zacharias LC, Kenney MC. Steroid differentiation: the safety profile of various steroids on
retinal cells in vitro and their implications for clinical use (an American Ophthalmological Society thesis). Trans Am
Ophthalmol Soc. 2014;112:116-141.
5. Sobrin L, DAmico DJ. Controversies in intravitreal triamcinolone acetonide use. Int Ophthalmol Clin.
2005;45:133-141.
6. Kurz PA, Suhler EB, Flaxel CJ, Rosenbaum JT. Injectable intraocular corticosteroids. In: Becker MD, Davis J, eds.
Surgical Management of Inflammatory Eye Disease. Philadelphia; 2008:5-16.
7. Thakur A, Kadam R, Kompella UB. Trabecular meshwork and lens partitioning of corticosteroids: implications for
elevated intraocular pressure and cataracts. Arch Ophthalmol. 2011;129:914-920.
8. Pearson PA, Comstock TL, Ip M, et al. Fluocinolone acetonide intravitreal implant for diabetic macular edema: a
3-year multicenter, randomized, controlled clinical trial. Ophthalmology. 2011;118:1580-1587.
9. Campochiaro PA, Brown DM, Pearson A, et al. Sustained delivery fluocinolone acetonide vitreous inserts provide
benefit for at least 3 years in patients with diabetic macular edema. Ophthalmology. 2012;119:2125-2132.
10. Diabetic Retinopathy Clinical Research Network. A randomized trial comparing intravitreal triamcinolone
acetonide and focal/grid photocoagulation for diabetic macular edema. Ophthalmology. 2008;115:1447-1449.
11. Diabetic Retinopathy Clinical Research Network (DRCR.net), Beck RW, Edwards AR, et al. Three-year follow-up
of a randomized trial comparing focal/grid photocoagulation and intravitreal triamcinolone for diabetic macular
edema. Arch Ophthalmol. 2009;127:245-251.
12. Lauer AK, Bressler NM, Edwards AR, Diabetic Retinopathy Clinical Research Network. Frequency of intraocular
pressure increase within days after intravitreal triamcinolone injections in the diabetic retinopathy clinical research
network. Arch Ophthalmol. 2011;129:1097-1099.
13. Quiram PA, Gonzales CR, Schwartz SD. Severe steroid-induced glaucoma following intravitreal injection of
triamcinolone acetonide. Am J Ophthalmol. 2006;141:580-582.
14. Ansari EA, Ali N. Intraocular pressure following intravitreal injection of triamcinolone acetonide. Open
Ophthalmol J. 2008;2:119-122.
15. Jain S, Thompson JR, Foot B, et al. Severe intraocular pressure rise following intravitreal triamcinolone: a
national survey to estimate incidence and describe case profiles. Eye (Lond). 2014;28:399-401.
16. Singer M, for the Ozurdex MEAD Study Group. Intraocular pressure in patients with diabetic macular edema
treated with dexamethasone intravitreal implant: MEAD study findings. Presented at: the American Society of
Retina Specialists Annual Meeting; August 9, 2014; San Diego, CA.
17. Dutra Medeiros M, Navarro R, Garcia-Arum J, et al. Dexamethasone intravitreal implant for treatment
of patients with recalcitrant macular edema resulting from Irvine-Gass syndrome. Invest Ophthalmol Vis Sci.
2013;54:3320-3324.
18. Khurana RN, Palmer JD, Porco TC, Wieland MR. Dexamethasone intravitreal implant for pseudophakic cystoid
macular edema in patients with diabetes. Ophthalmic Surg Lasers Imaging Retina. 2015;46:56-61.
19. Bellocq D, Korobelnik J-F, Burillon C, et al. Effectiveness and safety of dexamethasone implants for post-surgical
macular oedema including Irvine-Gass syndrome: the EPISODIC study. Br J Ophthalmol. 2015;99:979-983.
20. Bonfiglio V, Fallico MR, Russo A, et al. Intravitreal dexamethasone implant for cystoid macular edema and
inflammation after scleral buckling. Eur J Ophthalmol. 2015;25:0-0.
21. Taney LS, Baumal CR, Duker JS. Sustained-release dexamethasone intravitreal implant for persistent macular
(Continued from page 54)
patients did not adequately respond to anti-VEGF therapy.3
In Protocol T, approximately half of the patients had
persistent edema and required rescue laser at week 24 after
monthly anti-VEGF injections.3
FAME STUDY OVERVIEW AND RESULTS
The 0.19-mg fluocinolone acetonide intravitreal
implant was studied in two randomized, multicenter,
double-masked, parallel-group, 36-month clinical trials
(FAME A and FAME B) in patients with DME previously
treated with laser.4 Entry criteria required at least one
previous laser treatment and BCVA between 19 (20/50)
and 68 (20/400) letters in the study eye as measured
on the Early Treatment Diabetic Retinopathy Study
chart. Patients with a history of uncontrolled intraocular
pressure (IOP) elevation with steroid use that did not
respond to topical therapy were excluded from participation, as were patients with glaucoma, ocular hypertension, IOP greater than 21 mm Hg, or concurrent therapy
at screening with IOP-lowering agents in the study eye.
Study results of the phase 3 trials indicated that at
58RETINA TODAYSEPTEMBER 2015
edema after vitrectomy for epiretinal membrane. Ophthalmic Surg Lasers Imaging Retina. 2015;46:224-228.
22. Bui KM, Chow CC, Mieler WF. Treatment of recalcitrant radiation maculopathy using intravitreal dexamethasone (Ozurdex) implant. Retin Cases Brief Rep. 2014;8:167-170.
23. Caminal JM, Flores-Moreno I, Arias L, et al. Intravitreal dexamethasone implant for radiation maculopathy
secondary to plaque brachytherapy in choroidal melanoma [publishied online ahead of print May 27, 2015]. Retina.
24. Srour M, Querques G, Leveziel N, et al. Intravitreal dexamethasone implant (Ozurdex) for macular edema
secondary to retinitis pigmentosa. Graefes Arch Clin Exp Ophthalmol. 2013;251:1501-1506.
25. Ahn SJ, Kim KE, Woo SJ, Park KH. The effect of an intravitreal dexamethasone implant for cystoid macular
edema in retinitis pigmentosa: a case report and literature review. Ophthalmic Surg Lasers Imaging Retina.
2014;45:160-164.
26. Calvo P, Ferreras A, Adel Al F, et al. Dexamethasone intravitreal implant as adjunct therapy for patients with wet
age-related macular degeneration with incomplete response to ranibizumab. Br J Ophthalmol. 2015;99:723-726.
27. Bratton ML, He YG, Weakley DR. Dexamethasone intravitreal implant (Ozurdex) for the treatment of pediatric
uveitis. J AAPOS. 2014;18:110-113.
28. Lei S, Lam WC. Efficacy and safety of dexamethasone intravitreal implant for refractory macular edema in
children. Can J Ophthalmol. 2015;50:236-241.
29. Dutra Medeiros M, Postorino M, Navarro R, et al. Dexamethasone intravitreal implant for treatment of patients
with persistent diabetic macular edema. Ophthalmologica. 2014;231:141-146.
30. Zhioua I, Semoun O, Lalloum F, Souied EH. Intravitreal dexamethasone implant in patients with ranibizumab
persistent diabetic macular edema. Retina. 2015;35:1429-1435.
31. Alshahrani ST, Dolz-Marco R, Gallego-Pinazo R, et al. Intravitreal dexamethasone implant for the treatment of
refractory macular edema in retinal vascular diseases: Results of the KKESH International Collaborative Retina Study
Group [published online ahead of print June 15, 2015]. Retina.
32. Sharareh B, Gallemore R, Taban M, et al. Recalcitrant macular edema after intravitreal bevacizumab is responsive to an intravitreal dexamethasone implant in retinal vein occlusion. Retina. 2013;33:1227-1231.
33. Shah AR, Alfaran A, Abbey AM, Wolfe JD. Early identification of macular edema recalcitrant to intravitreal antivascular endothelial growth factor and efficacy of intravitreal dexamethasone implant treatment. Paper presented
at: The American Society of Retina Specialists Annual Meeting; August 9, 2014; San Diego, CA.
34. Christoforidis JB, Carlton MM, Wang J, et al. Anatomic and pharmakokinetic properties of intravitreal bevacizumab and ranibizumab after vitrectomy and lenstomy. Retina. 2013;33:946-952.
35. Ahn SJ, Ahn J, Park S, et al. Intraocular pharmacokinetics of ranibizumab in vitrectomized versus nonvitrectomized eyes. Invest Ophthalmol Vis Sci. 2014;55:567-573.
36. Chin HS, Park TS, Moon YS, OH JH. Difference in clearance of intravitreal triamcinolone acetonide between
vitretomized and nonvitrectomized eyes. Retina. 2005;25:556-560.
37. Chang-Lin JE, Burke JA, Peng Q, et al. Pharmacokinetics of a sustained-release dexamethasone intravitreal
implant in vitrectomized and nonvitrectomized eyes. Invest Ophthalmol Vis Sci. 2011;52:4605-4609.
38. Adn A, Pelegrn L, Rey A, et al. Dexamethasone intravitreal implant for treatment of uveitic persistent cystoid
macular edema in vitrectomized patients. Retina. 2013;33:1435-1440.
39. Boyer DS, Faber D, Gupta S, et al. Dexamethasone intravitreal implant for treatment of diabetic macular edema
in vitrectomized patients. Retina. 2011;31:915-923.
40. Shaikh AH, Petersen MR, Sisk RA, et al. Comparative effectiveness of the dexamethasone intravitreal implant
in vitrectomized and non-vitrectomized eyes with macular edema secondary to central retinal vein occlusion.
Ophthalmic Surg Lasers Imaging Retina. 2013;44:28-33.
month 24, 28% of patients treated with 0.19 mg fluocinolone acetonide achieved a 15-letter or greater improvement
in BCVA compared with 16% in the control group (P = .002).4
Center point retinal thickness measured on optical coherence tomography showed that patients in the fluocinolone
acetonide 0.19 mg group had a mean reduction of 167.7 m
at 1 week, and that this thickness reduction was sustained
through month 24.4
Safety
Safety was studied over 36 months in the FAME trials.
Adverse events (AEs) were consistent with other ocular
corticosteroids and were manageable in nature.4 The most
common AE was cataract, with 82% of patients in the
fluocinolone acetonide treatment group reporting cataract
compared with 50% in the control group. Cataract extraction was performed in 80% of these patients, compared with
27% of the control group. Increased IOP was reported in
20% of the fluocinolone acetonide patients compared with
4% in the control group; however, only 5% of patients experiencing increased IOP required incisional surgery. The study
SPECIAL FOCUS DRUG DELIVERY
data indicated that none of the patients with prior steroid
treatment required IOP-lowering eye surgery.
DISEASE MEDIATION
It is well established that DME is multifactorial and that
it may be mediated by multiple cytokinesnot strictly
VEGF. Differential responses to immediate versus delayed
therapy in the RISE and RIDE trials indicated that delayed
treatment, which perhaps allowed other disease-mediating
factors to contribute to disease progression, resulted in
poorer visual outcomes at multiple time points.5
A similar differential response to therapy was
observed in the FAME study. A subanalysis of FAME
data examined response based on duration of DME
diagnosis and compared patients with short-duration
DME (<1.73 years) with patients with long-duration
DME (> 1.73 years). In patients with short-duration
DME, the subanalysis showed that both control
patients treated with standard of care (laser, antiVEGF, and intravitreous triamcinolone acetonide)
and the 0.19 mg fluocinolone acetonidetreated
patients had similar outcomes: Approximately 25%
of patients in each group achieved a 3-line improvement in BCVA at month 36.6 However, in patients with
long-duration DME, the response in the standard of
care control group was diminished, with only 13.4% of
patients achieving 3 or more lines of BCVA improvement at month 36 compared with 34% of 0.19 mg
fluocinolone acetonidetreated patients gaining 3 or
more lines (P < .001).7
Patients treated with 0.19 mg fluocinolone acetonide
in FAME responded similarly regardless of disease duration; however, the standard of care offered in the sham
control group performed significantly worse in the
long-duration disease group.8
This clinical response reflects the differences in the
retinal microenvironment. When patients with DME do
not respond adequately to selective anti-VEGF therapy,
it may indicate that multiple cytokines, not strictly VEGF,
are the primary disease mediators. Duration of DME
appears to influence this increase in cytokine activity.
The differential treatment effect seen in long-duration
versus short-duration DME in FAME appears to be related to the continuous delivery of low-dose steroid.
THE IMPLANT IN A NUTSHELL
When patients do not respond adequately to anti-VEGF
therapy, it may be an indication that their disease has
evolved into a more inflammatory-based state, thus requiring a shift in treatment paradigm. New multifactorial steroids are proving to be promising therapeutic options. The
FAME study illustrated the potential value of continuous
60RETINA TODAYSEPTEMBER 2015
steroid therapy in long-term disease patient populations.6
The 0.19-mg fluocinolone acetonide intravitreal
implant received approval from the US Food and Drug
Administration (FDA) in September 2014. The drug is
indicated for patients who have been previously treated
with a course of corticosteroids and who did not have
a clinically significant rise in IOP. As a corticosteroid,
fluocinolone acetonide may address multiple cytokines.
The 0.19-mg fluocinolone acetonide intravitreal implant
is a nonbioerodible implant made of polyimide, the same
nonbioerodable material used in the haptics of many
intraocular lenses. The cylindrical implant measures 3.5 mm
0.37 mm and holds 190 g of fluocinolone acetonide. A
small 25-gauge needle places the device through the pars
plana into the vitreous, creating a self-sealing wound and
eliminating any need for tunneling. The implant delivers
a continuous, low dosage (0.2 g/day) over the course
of 36 months. Fluocinolone acetonide levels peak 1 week
after implantation and level off by the third month.
CONCLUSION
As physicians come to better understand the nature
of DME as the disease matures, they must calculate the
burden that their patients feel, as frequent injections
may present diminishing returns. Sustained-release steroid options have emerged as a viable and effective treatment option for patients with DME. In my practice, the
0.19-mg fluocinolone acetonide intravitreal implant has
shown positive outcomes since it received FDA approval,
and I will continue to recommend it to patients with
mature, multiple cytokinemediated DME. n
Scott W. Cousins, MD, is the Robert
Machemer, MD, Professor of Ophthalmology
and Immunology, vice chair for research, and
director of the Duke Center for Macular Diseases
at Duke Eye Center at Duke University, Durham,
N.C. Dr. Cousins may be reached at +1-919-684-3316.
1. Elman MJ, Bressler NM, Qin H, et al; Diabetic Retinopathy Clinical Research Network. Expanded 2-year follow-up
of ranibizumab plus prompt or deferred laser or triamcinolone plus prompt laser for diabetic macular edema.
Ophthalmology. 2011;118(4):609-614
2. Bressler SB, Qin H, Beck RW, et al; Diabetic Retinopathy Clinical Research Network. Factors associated with
changes in visual acuity and central subfield thickness at 1 year after treatment for diabetic macular edema with
ranibizumab. Arch Ophthalmol. 2012;130(9):1153-1161.
3. Wells JA, Glassman AR, Ayala AR, et al; Diabetic Retinopathy Clinical Research Network. Aflibercept, bevacizumab, or ranibizumab for diabetic macular edema. N Engl J Med. 2015;372(13):1193-1203.
4. Campochiaro PA, Brown DM, Pearson A, et al; FAME Study Group. Long-term benefit of sustained-delivery
fluocinolone acetonide vitreous inserts for diabetic macular edema. Ophthalmology. 2011;118(4):626-635.e2.
5. Brown DM, Nguyen QD, Marcus DM, et al; RISE and RIDE Research Group. Long-term outcomes of
ranibizumab therapy for diabetic macular edema: the 36-month results from two phase II trials. Ophthalmology.
2013;120(10):2013-2022.
6. Analysis of FAME data is on file at Alimera Sciences.
7. Canha-Vaz J, Ashton P, Iezzi R, et al; FAME Study Group. Sustained delivery fluocinolone acetonide vitreous implants:
long-term benefit in patients with chronic diabetic macular edema. Ophthalmology. 2014;121(10):1892-1903.
8. Campochiaro PA, Brown DM, Pearson A, et al; FAME Study Group. Sustained delivery fluocinolone acetonide
vitreous inserts provide benefit for at least 3 years in patients with diabetic macular edema. Ophthalmology.
2012;119(10):2125-2132.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The No B.S. Guide To Anterior Pelvic Tilt: In-Depth Assessment and 6-Week ProgramDocument39 pagesThe No B.S. Guide To Anterior Pelvic Tilt: In-Depth Assessment and 6-Week ProgramKosar83% (6)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Nurse - Resignation LetterDocument1 pageNurse - Resignation LetterphoenixdashPas encore d'évaluation
- Crisis Management and Human Behaviour Mca ApprovedDocument2 pagesCrisis Management and Human Behaviour Mca ApprovedVinil Gupta100% (1)
- Major Neurological Syndromes PDFDocument260 pagesMajor Neurological Syndromes PDFVirlan Vasile Catalin100% (1)
- Eyes in Marfan SyndromeDocument8 pagesEyes in Marfan SyndromePrissilmaTaniaPas encore d'évaluation
- Penetrating Traumatic Brain Injury A Review of Current Evaluation Andmanagement Concepts 2155 9562 1000336Document7 pagesPenetrating Traumatic Brain Injury A Review of Current Evaluation Andmanagement Concepts 2155 9562 1000336PrissilmaTaniaPas encore d'évaluation
- Marfans Occular ReviewDocument3 pagesMarfans Occular ReviewPrissilmaTaniaPas encore d'évaluation
- BR J Ophthalmol 2001 Falkner 1324 7Document5 pagesBR J Ophthalmol 2001 Falkner 1324 7PrissilmaTaniaPas encore d'évaluation
- Article Wrist Hand CTS MGT October2004 JOSPT MichlovitzDocument12 pagesArticle Wrist Hand CTS MGT October2004 JOSPT MichlovitzPrissilmaTaniaPas encore d'évaluation
- Article Wrist Hand CTS MGT October2004 JOSPT MichlovitzDocument12 pagesArticle Wrist Hand CTS MGT October2004 JOSPT MichlovitzPrissilmaTaniaPas encore d'évaluation
- Lecture 5 HMS Siklus MenstruasiDocument18 pagesLecture 5 HMS Siklus MenstruasiPrissilmaTaniaPas encore d'évaluation
- BR J Ophthalmol 2015 Danis Bjophthalmol 2015 306823Document7 pagesBR J Ophthalmol 2015 Danis Bjophthalmol 2015 306823PrissilmaTaniaPas encore d'évaluation
- Rheumatology 2013 Cramer Rheumatology Ket264Document6 pagesRheumatology 2013 Cramer Rheumatology Ket264PrissilmaTaniaPas encore d'évaluation
- UK National Guideline For The Management of Pelvic Inflammatory Disease 2011 PDFDocument18 pagesUK National Guideline For The Management of Pelvic Inflammatory Disease 2011 PDFPrissilmaTaniaPas encore d'évaluation
- 08 - GlaucomaDocument80 pages08 - GlaucomaabcdshPas encore d'évaluation
- Dr. H. I. Dr. H. I. Boediman Boediman,, Sp.A Sp.A (K) (K) : B Fdiii FR IlDocument49 pagesDr. H. I. Dr. H. I. Boediman Boediman,, Sp.A Sp.A (K) (K) : B Fdiii FR IlPrissilmaTaniaPas encore d'évaluation
- Appendix RismanDocument45 pagesAppendix RismanPrissilmaTaniaPas encore d'évaluation
- 084 Prissilma Tania JonardiDocument1 page084 Prissilma Tania JonardiPrissilmaTaniaPas encore d'évaluation
- Hostel Murah Di SingaporeDocument22 pagesHostel Murah Di SingaporePrissilmaTaniaPas encore d'évaluation
- Modul 7Document31 pagesModul 7PrissilmaTaniaPas encore d'évaluation
- RA7610Document3 pagesRA7610Andrew GallardoPas encore d'évaluation
- Kinds of Blood. Differences Between Men and WomenDocument11 pagesKinds of Blood. Differences Between Men and WomenTiagoSantosPas encore d'évaluation
- Lesson 4Document4 pagesLesson 4api-316910625Pas encore d'évaluation
- Neurophysiological Effects of Spinal ManipulationDocument15 pagesNeurophysiological Effects of Spinal ManipulationBojan AnticPas encore d'évaluation
- Glycerol MsdsDocument6 pagesGlycerol MsdsJX Lim0% (1)
- Bed Making LectureDocument13 pagesBed Making LectureYnaffit Alteza Untal67% (3)
- Urgensi Kepemimpinan Transformasional Dan Kecerdasan Emosional Pada Perusahaan Dalam Merespons Pandemi Covid-19Document11 pagesUrgensi Kepemimpinan Transformasional Dan Kecerdasan Emosional Pada Perusahaan Dalam Merespons Pandemi Covid-19Inspektorat KubarPas encore d'évaluation
- ASYNCHRONOUS-ACTIVITY-Module 1Document7 pagesASYNCHRONOUS-ACTIVITY-Module 1Grant Wynn ArnucoPas encore d'évaluation
- Engl7 Q4 W4 Determining-Accuracy Villanueva Bgo Reviewed-1Document18 pagesEngl7 Q4 W4 Determining-Accuracy Villanueva Bgo Reviewed-1johbaguilatPas encore d'évaluation
- Significance of HACCP and SSOP in Food Processing EstablishmentsDocument7 pagesSignificance of HACCP and SSOP in Food Processing EstablishmentselfiraPas encore d'évaluation
- 12 2012 TriclabendazoleDocument16 pages12 2012 Triclabendazolenia suwartiningsihPas encore d'évaluation
- A 58 Year Old Client Is Admitted With A Diagnosis of Lung CancerDocument9 pagesA 58 Year Old Client Is Admitted With A Diagnosis of Lung CancerNur SanaaniPas encore d'évaluation
- PDF 20221013 211252 0000Document1 pagePDF 20221013 211252 0000Meann جرابيللوPas encore d'évaluation
- HSMAI PHG - New Rules To Be Market ReadyDocument28 pagesHSMAI PHG - New Rules To Be Market ReadyAnna ShortPas encore d'évaluation
- DrFuhrmans Super Immunity FactsheetDocument2 pagesDrFuhrmans Super Immunity FactsheetPerrela Perrela100% (1)
- Effective Leadership Towards The Star Rating Evaluation of Malaysian Seni Gayung Fatani Malaysia Organization PSGFMDocument10 pagesEffective Leadership Towards The Star Rating Evaluation of Malaysian Seni Gayung Fatani Malaysia Organization PSGFMabishekj274Pas encore d'évaluation
- ACSM - 2007 SpringDocument7 pagesACSM - 2007 SpringTeo SuciuPas encore d'évaluation
- Book StickerDocument4 pagesBook Stickerilanabiela90Pas encore d'évaluation
- MBA Students Habit Toward ToothpasteDocument29 pagesMBA Students Habit Toward ToothpasteSunil Kumar MistriPas encore d'évaluation
- Attitude of EMPLOYEES in Terms of Compliance of Health and SafetyDocument6 pagesAttitude of EMPLOYEES in Terms of Compliance of Health and SafetyJanice KimPas encore d'évaluation
- Part-IDocument507 pagesPart-INaan SivananthamPas encore d'évaluation
- MfA Leadership ExperienceDocument49 pagesMfA Leadership ExperienceAlex MoralesPas encore d'évaluation
- DMF 40 199 PDFDocument14 pagesDMF 40 199 PDFsiraj_khan_13Pas encore d'évaluation
- 7th Edition NRP Brings Big Changes For NRP Instructors: Instructor UpdateDocument12 pages7th Edition NRP Brings Big Changes For NRP Instructors: Instructor UpdateJoev SaquinPas encore d'évaluation
- Identifikasi Dan Prevalensi Nematoda Saluran Pencernaan Kuda Lokal (Equus Caballus) Di Kecamatan Moyo Hilir SumbawaDocument7 pagesIdentifikasi Dan Prevalensi Nematoda Saluran Pencernaan Kuda Lokal (Equus Caballus) Di Kecamatan Moyo Hilir SumbawaBeebli PuchaPas encore d'évaluation
- Job Safety Analysis Worksheet: JSA JSA Participants PPE Required Tools And/or EquipmentDocument5 pagesJob Safety Analysis Worksheet: JSA JSA Participants PPE Required Tools And/or EquipmentVigiePas encore d'évaluation