Académique Documents
Professionnel Documents
Culture Documents
Retro-Molar Trigonal Reconstruction and Oncologic Outcomes After Resection of Large Malignant Ulcers in Elderly Patients
Transféré par
Peertechz Publications Inc.Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Retro-Molar Trigonal Reconstruction and Oncologic Outcomes After Resection of Large Malignant Ulcers in Elderly Patients
Transféré par
Peertechz Publications Inc.Droits d'auteur :
Formats disponibles
Archives of Otolaryngology and Rhinology
Sameh Roshdy1, Mohamed T Hafez1,
Islam A El Zahaby1, Osama Hussein1,
Fayez Shahatto1, Mosab Shetiwy1,
Shadi Awny1, Sherif Kotb1, Hend A ElHadaad1 and Adel Denewer2*
Department of Surgical Oncology, Oncology center,
Faculty of Medicine, Mansoura University, Egypt
2
Department of Clinical Oncology & Nuclear
Medicine, Faculty of Medicine, Mansoura
University, Egypt
1
Dates: Received: 09 September, 2015; Accepted:
07 December, 2015; Published: 09 December, 2015
Research Article
Retro-Molar Trigonal
Reconstruction and Oncologic
Outcomes after Resection of Large
Malignant Ulcers in Elderly Patients
*Corresponding author: Professor Adel Denewer,
Head of Department of Surgery, Faculty of Medicine,
Mansoura University, Egypt, Tel: +201223237791;
E-mail:
Abstract
www.peertechz.com
Aim: The research was designed to study suitability of submental island flap and radial forearm
free flap (RFFF) as one stage reconstructive procedure after resection of large retromolar-trigonal
cancers. And to assess locoregional recurrence and disease free survival after adjuvant treatment.
ISSN: 2455-1759
Keywords: Buccal mucosa cancer; Oral cancers;
Squamous cell cancer of oral mucosa; Submental
Background: Buccal mucosa carcinoma represents 3 to 5% of oral-cavity cancer. Retromolar
buccal trigon affected in one third of patients with buccal mucosal cancers. Squamous cell carcinoma
is the commonest pathological finding.
Methods and techniques: Fifty three patients with retromolar-trigonal cancer underwent
resection with safety margins, cervical block neck dissection and reconstruction with submental island
flap and radial forearm free flap (RFFF) in oncology center Mansoura University from August 2010
to May 2014.
Results: Seven patients underwent RFFF, 46 patients reconstructed with sub-mental flap.
Partial necrosis was encountered in 5 cases of sub-mental flaps but lost flaps were present in 2
cases of RFFF. 14 patients received neoadjuvant chemotherapy, 33 patients received postoperative
radiotherapy. Local recurrence was 13.2%, 2 year disease free survival (DFS) was 72.7%.
Introduction
Oral cavity cancer globally, wings between the sixth to the eighth
most common malignancy; it comprises more than 30% of all head
and neck cancers [1-3,4]. In Egypt about 4.500 people are diagnosed
with oral cancer every year [5]. Retromolar trigon (RMT) is the buccal
region near the lower third molar tooth that has affected in 15% of all
oral cancers [6-8]. Resection of RMT cancer with 1cm safety margins
all round results in large oral defect. Small defects can be left to heal
by secondary intention or are repaired by primary closure, buccal
advancement flap, palatal pedicled flap, split-thickness skin grafting
or tongue flap [9,10]. Reconstruction of larger retro-molar defects
using pedicled buccal pad of fat flap is frequently insufficient and may
be oncologically unsafe when the tumor is abutting or infiltrating the
buccal pad of fat [11-15]. Pedicled and free myocutaneous flaps albeit
safe and robust, are not suitable options due to additional, unnecessary
muscle bulk. The pectoralis major myocutaneous flap carries about
15% flap related complications with the disadvantages of being
bulky, the need of a second stage for pedicle division, unacceptable
donor site scar in females [16,17]. Thus, RMT defects too wide to be
covered with local flaps and are best served with regional or distant
fasciocutaneous flap reconstruction. Defects of such size are typically
covered with a free fasciocutaneous flap; the most commonly used of
which are the radial forearm flaps (RFFF). The research was designed
to test the safety and efficacy of submental island flap as one stage
reconstructive procedure for large post-surgical RMT oral defects.
We evaluated this technique in comparison with the RFFF as an
accepted standard of care for similar cases.
Patients and Methods
This is a retrospective evaluation of prospectively collected
patients data that was carried out from August 2010 to May 2014 for
patients with buccal mucosal cancer originating in or extending to the
RMT region and presenting to our clinic in Mansoura University Can
cer Center in Egypt (Figure 1). We enrolled all cases with predicted
post-resectional defects 4cm in greatest dimension. Pure soft tissue
resection and marginal mandibular resections were included in the
study. Patients with metastatic disease, poor performance, fully
thickness bony defects necessitating mandibular reconstruction and
Figure 1: Preoperative photo of a large ulcerating SCC in the retromolartrigone
(arrow).
Citation: Roshdy S, Hafez MT, El Zahaby IA, Hussein O, Shahatto F, et al. (2015) Retro-Molar Trigonal Reconstruction and Oncologic Outcomes after
Resection of Large Malignant Ulcers in Elderly Patients. Arch Otolaryngol Rhinol 1(2): 052-056. DOI: 10.17352/2455-1759.000010
052
Roshdy, et al. (2015)
patients who are salvaged by surgery after concurrent chemotherapy
and/or radiotherapy were excluded from this study. All clinical
procedures were conducted in accordance with the guidelines of the
ethics committee of the Faculty of Medicine, Mansoura University,
and after obtaining the written informed consent of the patients.
All patients were evaluated preoperatively by medical history,
physical examination, CT scans and/or MRI from the skull base to the
clavicle and biopsy from the primary lesion. Panorex films were done
when mandibular infiltration was suspected. Patients with tumors
extended to anterior tonsillar pillar or reached the adjacent part of
the tongue base required neoadjuvant chemotherapy that consisted of
cisplatin (60-100 mg/m2/day) on day 1 and 5-FU (1000 mg/m2/day)
on days 1-4 for 3 cycles 21days interval between cycles.
Surgical procedure involves wide local excision of the RMT cancer
including underlying buccinator muscle trans-orally with or without
lip split and sent for frozen section to ensure adequate safety margins
(more than 5mm) (Figure 2). When evident mandibular invasion was
encountered, marginal mandibulectomy was carried out to achieve
clear safety margins. Prophylactic tracheostomy was needed when
there was airway compromise especially in cases extending to anterior
tonsillar pillar and/or the tongue base.
Ipsilateral selective neck dissection (Level I-IV) was done for
clinically node positive cases or radically for large, high grade and
deeply infiltrative tumors. In cases where the base of the tongue is
infiltrated or when the patient presents clinically with bilateral nodal
disease, ipsilateral modified radical neck dissection is done and
contralateral selective node dissection was done. Modified block neck
dissection was indicated if matted lymph nodes or extensive cervical
lymph nodes involvement is found preoperatively and if level IV
nodes are positive on frozen section.
The resulting large surgical defect was reconstructed by submental
island flap or radial forearm free flap (RFFF) (Figures 3a,3b). Choice
of either reconstructive procedure was based on elderly age, or
associated co-morbidities as diabetes mellitus and ischemic heart
diseases and constrictive lung conditions that contraindicate RFFF
reconstruction.
All patients were managed in the ICU for one or two days,
for assuring safety of the airway and vital data, before transfer to
the surgical ward. They received intra-operative antibiotics with
induction of anaesthesia continued for 7 days thereafter. Tube feeding
was used for 5 days before resumption of oral feeding. All our patients
were referred to Clinical Oncology and Nuclear medicine department
for adjuvant therapy recommendations.
Adjuvant therapy
Postoperative radiotherapy: External beam radiotherapy was
used in patients with pathologically nodal positive disease (more
than one lymph node, extra capsular infiltration), T3and T4a; 60Gy
in 30 fractions was given to the primary site and bilateral neck lymph
nodes, single fraction /day /5 settings /week using linear accelerator
6mev photon, 2 parallel opposed field. Spinal cord excluded after
45Gy.
The patients were followed monthly in the first 6 months,
053
Figure 2: Shows the post-resection defect (blue arrow) and the harvested
submental island flap (red arrow).
Figure 3a: Submental flap inset at the defect after passing through a tunnel in
the vestibule of the oral cavity (arrow).
Figure 3b: Radial forarm free flap inset at retromolartrigone defect after
resection of a large SCC (green arrow) with completed arterial anastomosis
(red arrow) and venous anastomosis (blue arrow).
then 3 months in the first 2 years then every six months thereafter.
During follow up visit, patients were examined clinically and by neck
US. Biopsy from suspected lesion was taken for histopathological
examination. Cosmesis and oral functions regarding speech,
swallowing and occlusion were assessed in every visit. CT or MRI
neck every 3 month (Figures 4a,4b).
Statistics
Descriptive data are presented as number and percentages.
Functional outcome of submental flap versus RFFF was compared
using Fisher exact test.
Results
Fifty-three eligible patients were enrolled in the study. Mean age
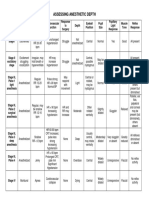
of patients was 57 (7.15) years. Table 1 shows patients characteristics
and tumors description. Out of 53 patients, four had histologically
positive margins by frozen section and subjected to re-excision.
Marginal mandibulectomy was needed in two patients due to evident
cortical infiltration. Nine cases showed extension to anterior tonsillar
Citation: Roshdy S, Hafez MT, El Zahaby IA, Hussein O, Shahatto F, et al. (2015) Retro-Molar Trigonal Reconstruction and Oncologic Outcomes after
Resection of Large Malignant Ulcers in Elderly Patients. Arch Otolaryngol Rhinol 1(2): 052-056. DOI: 10.17352/2455-1759.000010
Roshdy, et al. (2015)
the pectoralis major myocutaneous flap are often bulky with difficult
inset in this posteriorly located defect [16-19].
Figure 4a: Four months postoperative view of a submental island flap
reconstruction of a retromolartrigone defect (arrow).
Figure 4b: Fourteen Months postoperative view of a radial forarm free flap
reconstruction of a retromolartrigone defect (arrow).
pillar and three cases reached the adjacent part of the tongue base and
required excision.
Selective neck dissection (level I-IV) was done for 47 patients;
however modified radical neck dissection was needed in six patients
with clinically overt neck disease. The size of the post resection defect
varied from 4x4 to 5x6 cm. Reconstruction of the resulting defects was
carried out by submental island flap in 46 patients and with RFFF in
seven cases. All patients had smooth hospital stay and postoperative
course except for 5 cases with submental island flap reconstruction
had partial flap necrosis resulting in minor salivary leak which was
managed conservatively. Two out of 7 cases reconstructed by RFFF
suffered complete flap loss with subsequent major salivary leak and
those patient required re-surgery and were backed-up by pectoralis
major myocutaneous flap. Table 2 shows operative data and flap
related complications, cosmetic and functional outcome. Locoregional recurrence was detected in 7 cases (13.2) % during the first
year of the follow up, 5 cases after submental flap reconstruction
and 2 after RFFF. These lesions were large enough that mandate reexcision and postoperative radiotherapy. Fourteen patients received
neoadjuvant chemotherapy, 33 patients received postoperative
radiotherapy. The 2-year disease free survival among patients received
postoperative radiotherapy was 72.7% (Figure 5).
Discussion
The decision making regarding the reconstructive approach after
oral cancer extirpation, especially the retro-molar trigone, remains
a clinical dilemma, which is complicated by the enormous array of
procedures suitable for a given defect, each one offering pros and
cons.
However, when dealing with a large retro-molar trigonal defects
there is limited reconstructive options as nearby local mucosal or
palatal flaps that are usually insufficient, and could result in large
denuded areas [9,10], and other pedicled regional or distant flaps as
054
The commonly used reconstructive procedure for those large
retro-molar trigone defects are the microvascular free flaps especially
the radial forearm free flap which becomes the state of the art
reconstructive method for almost all oral defects being thin, pliable,
wide caliber and long vascular pedicle [20-23], nevertheless, this
Table 1:
patients).
Patients
characteristics
and
Tumor
description"
Characteristics
No.(%)
Gender
Males
Females
40(75.5)
13(24.5)
Associated comorbidities
Diabetes mellitus
Ischemic heart disease
Chronic obstructive chest disease
Chronic compensated liver disease
34 (64)
10 (18.8)
2 (3.8)
13 (24.5)
Tumor pathology
G1-2 SCC
G3 SCC
48(90.6)
5 (9.4)
Primary tumor site
- RMT
- Buccal mucosa extending to RMT.
33(62.3)
20(37.7)
Defect anatomy
Vestibular mucosa only
Tonsillar pillar
Tongue base
Mandibular periosteum
Mandibular cortex
37 (68.8)
9 (16.9)
3 (5.6)
2 (3.7)
2 (3.7)
T stage (AJCC)
T2
T3
T4a
31(58.5)
20(37.7)
2(3.8)
cN stage (AJCC)
N0
N1
N2a
N2b
9 (17)
25(47.2)
13(24.5)
6(11.3)
Neo-adjuvant chemotherapy
14 (26.4)
Postoperative radiotherapy
33 (62.3)
Loco regional recurrence
7(13.2)
(N=53
AJCC: American Joint Committee on Cancer staging manual.
Table 2: Operative details,flap-related complications, Cosmesis and functional
outcomes".
Type of reconstruction
Submental island
P value (Fisher
RFFF (N=7)
flap (N=46)
test)
Operative details
Flap harvest time in min 45+ 10
Surgical teams
Single
90+ 20
Two
Flap necrosis
Partial 015
Complete
5
0
0
2
P=NS
P=0.015
Salivary leak
P=NS
Cosmesis
Good
Excellent
Oral function
Mouth occlusion
Mastication
Swallowing
Satisfactory
Not disturbed
Easy
Satisfactory
Not disturbed
Easy
Citation: Roshdy S, Hafez MT, El Zahaby IA, Hussein O, Shahatto F, et al. (2015) Retro-Molar Trigonal Reconstruction and Oncologic Outcomes after
Resection of Large Malignant Ulcers in Elderly Patients. Arch Otolaryngol Rhinol 1(2): 052-056. DOI: 10.17352/2455-1759.000010
Roshdy, et al. (2015)
In the present study the 2-year DFS was 72.2 and this result is
similar to that of Ghoshal et al. [32], who reported 2-year DFS in
radically treated patients 76.4%.
Conclusion
Judicious use of submental island flap offers an easy way to
reconstruct large intra-oral defects. We believe thatfree flaps in head
and neck reconstruction are an ideal procedure but need advanced
surgical skills and not suitable for most of our patients in Oncology
Center- Mansoura University, and we suggest that the submental
flap should be present in the reconstructive surgeon armamentarium
when dealing with large retro-molar trigonal defect.
References
1. Jemal AR, Siegel E, Ward T, Murray JQ, Xu C, et al. (2006) Cancer statistics.
CA Cancer J Clin 56: 106-130.
Figure 5: Disease Free Survival among cases received post-operative RT.
microvascular techniques require good patient performance, expertise
and facilities. Therefore, not all patients or centers are candidate for
this sophisticated and lengthy micro-surgical techniques.
The submental island flap had emerged as a simple, secure,
easy, versatile reconstructive technique for those large retro-molar
trigonal defects and other oral and perioral defects with comparable
oncological and functional outcome [24-27]. In addition to, anterior
belly of digastric muscle taken within flap ensures closing of
dead space and gives support to cheek especially after resection of
buccinator muscle. Postoperative radiotherapy has no effect on flap
viability or its texture. Removing excess submental skin redundancy
with primary closure of donor site gives cosmetic improvement. In
our study we found no cases of complete submental island flap loss
even in elderly patients with associated co-morbidities, so it is suitable
for nearly all cases of the study. On the contrary, radial forearm free
flap was selected only for those fit patients, required longer operative
time, prolonged hospital stay, continued anticoagulant therapy for at
least 6 months and showed higher rate of total flap loss and donor site
morbidities.
The only disadvantage of the submental island flap is hair bearing
inside oral cavity in male patients and might be the proposed concept
of its interference with sound oncologic neck dissection.
As regard lymphadenectomy, proper neck node staging is done
for all the cases by resecting at least ten lymph nodes in positive cases
to achieve accurate pN stage [28].
But there is still controversy about interference of SMIF harvesting
with sound oncologic lymph node dissection [29].
In our study the local recurrence reported in 13.2% of our
patients. Coppen et al. [30], reported 25% a local relapse, Diaz et al.
[31], reported an overall recurrence rate of 45% (54/119) and a local
recurrence rate of 32% (38/119). Ghoshal et al. [32], documented a
2% regional recurrence rate while Bachar et al. [33], reported that
regional recurrence occurred in six patients and local and regional
recurrence in four patients (70 patients included in this study) also
Hakeem et al. [34], reported a local recurrence in (9.6%).
055
2. Mignogna MDS, Fedele L, Lo Russo (2004) The World Cancer Report and
the burden of oral cancer. European Journal of Cancer Prevention 13: 139142.
3. Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics 2002.
CA Cancer J Clin 55: 74-108.
4. Mehanna H, Paleri V, West CM, Nutting C (2011) Head and neck cancer-Part
1: Epidemiology, presentation, and preservation. Clin Otolaryngol 36: 65-68.
5. El-Mofty S, (2010) Early detection of oral cancer. Egypt J Oral Maxillofac Surg
1: 25-31.
6. Wood WC, Moore S, Staley C, Skandalakis JE (2010) Anatomic Basis of
Tumor Surgery: Springer.
7. Moore MA, Ariyaratne Y, Badar F, Bhurgri Y, Datta K, et al. (2010) Cancer
Epidemiology in South Asia - Past, Present and Future. Asian Pac J Cancer
Prev 11: 49-66.
8. Bhurgri Y (2005) Cancer of the oral cavity - trends in Karachi South (19952002). Asian Pac J Cancer Prev 6: 22-26.
9. Guven O, (1998) A clinical study on oroantral fistulae. J Craniomaxillofac
Surg 26: 267-271.
10. el-Hakim IE, el-Fakharany AM (1999) The use of the pedicled buccal fat pad
(BFP) and palatal rotating flaps in closure of oroantral communication and
palatal defects. J Laryngol Otol 113: 834-838.
11. Zhang HM, Yan YP, Qi KM, Wang JQ, Liu ZF (2002) Anatomical structure of
the buccal fat pad and its clinical adaptations. Plast Reconstr Surg 109: 25192520.
12. Mohan S, Kankariya H, Harjani B (2012) The use of the buccal fat pad for
reconstruction of oral defects: review of the literature and report of cases. J
Maxillofac Oral Surg 11: 128-131.
13. Hazrati EF, Loh, H Loh (1992) Use of the buccal fat pad for correction of
intraoral defects. Plastic and Reconstructive Surgery 90: 151.
14. Bither SR, Halli, Kini Y (2013) Buccal fat pad in intraoral defect reconstruction.
Journal of maxillofacial and oral surgery 12: 451-455.
15. Hao SP (2000) Reconstruction of oral defects with the pedicled buccal fat pad
flap. Otolaryngology-Head and Neck Surgery: 863-867.
16. Mehta S, Sarkar S, Kavarana N, Bhathena H, Mehta A (1996) Complications
of the Pectoralis Major Myocutaneous Flap in the Oral Cavity: A Prospective
Evaluation of 220 Cases. Plastic and Reconstructive Surgery 98: 31-37.
17. Hsing CY, Wong YK, Wang CP, Wang CC, Jiang RS, et al. (2011) Comparison
between free flap and pectoralis major pedicled flap for reconstruction in oral
cavity cancer patients A quality of life analysis. Oral Oncology 47: 522-527.
18. Liu HL, Chan JYW, Wei WI (2010) The changing role of pectoralis major
Citation: Roshdy S, Hafez MT, El Zahaby IA, Hussein O, Shahatto F, et al. (2015) Retro-Molar Trigonal Reconstruction and Oncologic Outcomes after
Resection of Large Malignant Ulcers in Elderly Patients. Arch Otolaryngol Rhinol 1(2): 052-056. DOI: 10.17352/2455-1759.000010
Roshdy, et al. (2015)
flap in head and neck reconstruction. European Archives of Oto-RhinoLaryngology 267: 1759-1763.
19. Shah JP, Haribhakti V, Loree TR, Sutaria P (1990) Complications of the
pectoralis major myocutaneous flap in head and neck reconstruction. The
American Journal of Surgery 160: 352-355.
20. Cheng YS, Li WL, Xu L, Xu ZF, Liu FY, et al. (2013) Assessment of quality
of life of oral cancer patients after reconstruction with radial forearm free
flaps. Zhonghua kou qiang yi xue za zhi = Zhonghua kouqiang yixue zazhi =
Chinese journal of stomatology 48:161-164.
21. Shah JP, Gil Z (2009) Current concepts in management of oral cancer-surgery. Oral Oncol 45: 394-401.
22. Eckardt A, Meyer A, Laas U, Hausamen JE (2007) Reconstruction of defects
in the head and neck with free flaps: 20 years experience. British Journal of
Oral and Maxillofacial Surgery 45: 11-15.
27. Elzahaby IA, Mohammed OH, Hafez MT, Abd Elaziz SR, Mosbah MM, et al.
(2013) Reconstruction of the lip commissure with upper and lower lip fullthickness defects using submental and nasolabial flaps: a case report. Annals
of Oral & Maxillofacial Surgery 13: 27.
28. Edge S, Byrd D, Compton C, Fritz A, Greene F & Trotti A (2010) Lip and
Oral Cavity American Joint Cancer Committee (AJCC) staging Manual, 7th
edition, Springer-Verlag New York 31.
29. Elzahaby IA, Roshdy S, Shahatto F, Hussein O (2015) The adequacy of
lymph node harvest in concomitant neck block dissection and submental
island flap reconstruction for oral squamous cell carcinoma; a case series
from a single Egyptian institution. BMC Oral Health.
30. Coppen C, de Wilde PC, Pop LA, van den Hoogen FJ, Merkx MA (2006)
Treatment results of patients with a squamous cell carcinoma of the buccal
mucosa. Oral Oncology 42: 795-799.
23. Blanchaert RH (2012) Survival after free flap reconstruction in patients with
advanced oral squamous cell carcinoma. J Oral Maxillofac Surg 70: 460.
31. Diaz EM Jr, Holsinger FC, Zuniga ER, Roberts DB, Sorensen DM
(2003) Squamous cell carcinoma of the buccal mucosa: one institutions
experience with 119 previously untreated patients.Head Neck25: 267273.
24. Chen WL, Yang ZH, Huang ZQ, Wang YY, Wang YJ, et al. (2007) [Reverse
facial artery-submental artery island myocutaneous flap for reconstruction
of oral and maxillofacial defects following cancer ablation]. Zhonghua Kou
Qiang Yi Xue Za Zhi 42: 629-30.
32. Ghoshal S, Mallick I, Panda N, Sharma SC (2006) Carcinoma of the
buccal mucosa: analysis of clinical presentation, outcome and prognostic
factors.Oral Oncol42:533539.
25. Merten SL, Jiang RP, Caminer D (2002) The submental artery island flap for
head and neck reconstruction. Anz Journal of Surgery 72: 121-124.
33. Bachar G, Goldstein DP, Barker E, Lea J, OSullivan B, et al. (2012)
Squamous cell carcinoma of the buccal mucosa: Outcomes of Treatment in
the modern era. The Laryngoscope 122: 1552-1557.
26. Martin D, Pascal JF, Baudet J, Mondie JM, Farhat JB, et al. (1993) The
submental island flap: a new donor site. Anatomy and clinical applications as
a free or pedicled flap. Plastic and reconstructive surgery 92: 867-873.
34. Hakeem AH, Pradhan SA, Tubachi J, Kannan R (2013) Outcome of per
oral wide excision of T1-2 N0 localized squamous cell cancer of the buccal
mucosa--analysis of 156 cases. Laryngoscope 123: 177-180.
Copyright: 2015 Roshdy S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
056
Citation: Roshdy S, Hafez MT, El Zahaby IA, Hussein O, Shahatto F, et al. (2015) Retro-Molar Trigonal Reconstruction and Oncologic Outcomes after
Resection of Large Malignant Ulcers in Elderly Patients. Arch Otolaryngol Rhinol 1(2): 052-056. DOI: 10.17352/2455-1759.000010
Vous aimerez peut-être aussi
- A Survey of Solid Waste Management in Chennai (A Case Study of Around Koyambedu Market and Madhavaram Poultry Farms)Document4 pagesA Survey of Solid Waste Management in Chennai (A Case Study of Around Koyambedu Market and Madhavaram Poultry Farms)Peertechz Publications Inc.100% (1)
- Angiosarcoma of The Scalp and Face: A Hard To Treat TumorDocument4 pagesAngiosarcoma of The Scalp and Face: A Hard To Treat TumorPeertechz Publications Inc.Pas encore d'évaluation
- MEK Inhibitors in Combination With Immune Checkpoint Inhibition: Should We Be Chasing Colorectal Cancer or The KRAS Mutant CancerDocument2 pagesMEK Inhibitors in Combination With Immune Checkpoint Inhibition: Should We Be Chasing Colorectal Cancer or The KRAS Mutant CancerPeertechz Publications Inc.Pas encore d'évaluation
- Fishing Condition and Fishers Income: The Case of Lake Tana, EthiopiaDocument4 pagesFishing Condition and Fishers Income: The Case of Lake Tana, EthiopiaPeertechz Publications Inc.Pas encore d'évaluation
- PLGF, sFlt-1 and sFlt-1/PlGF Ratio: Promising Markers For Predicting Pre-EclampsiaDocument6 pagesPLGF, sFlt-1 and sFlt-1/PlGF Ratio: Promising Markers For Predicting Pre-EclampsiaPeertechz Publications Inc.Pas encore d'évaluation
- International Journal of Aquaculture and Fishery SciencesDocument4 pagesInternational Journal of Aquaculture and Fishery SciencesPeertechz Publications Inc.Pas encore d'évaluation
- Imaging Journal of Clinical and Medical SciencesDocument7 pagesImaging Journal of Clinical and Medical SciencesPeertechz Publications Inc.Pas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- 7 AHM Antibiotic PolicyDocument98 pages7 AHM Antibiotic PolicyfaisalPas encore d'évaluation
- Data 14-12-2021 Formulir TB TerbaruDocument1 pageData 14-12-2021 Formulir TB TerbaruAksaPas encore d'évaluation
- Chronic Inflammatory Demyelinating PolyradiculoneuropathyDocument5 pagesChronic Inflammatory Demyelinating PolyradiculoneuropathyDiego Fernando AlegriaPas encore d'évaluation
- Allergic Contact DermatitisDocument12 pagesAllergic Contact DermatitisAzis BoenjaminPas encore d'évaluation
- Disorders of Immunity Hypersensitivity Reactions: Dr. Mehzabin AhmedDocument25 pagesDisorders of Immunity Hypersensitivity Reactions: Dr. Mehzabin AhmedFrances FranciscoPas encore d'évaluation
- Curriculum Vitae: School of Regeneration and Encouragement KEMA FK UNPADDocument7 pagesCurriculum Vitae: School of Regeneration and Encouragement KEMA FK UNPADReki PebiPas encore d'évaluation
- Rachel Bray - ResumeDocument2 pagesRachel Bray - Resumeapi-625221885Pas encore d'évaluation
- Anesthesia-Assessing Depth PDFDocument1 pageAnesthesia-Assessing Depth PDFAvinash Technical ServicePas encore d'évaluation
- Sports DrinksDocument2 pagesSports DrinksMustofaPas encore d'évaluation
- A Silent KillerDocument3 pagesA Silent KillerLinhNguyePas encore d'évaluation
- The GINA 2019 Asthma Treatment Strategy For Adults and Adolescents 12... Download Scientific DiagramDocument1 pageThe GINA 2019 Asthma Treatment Strategy For Adults and Adolescents 12... Download Scientific DiagramFatih AryaPas encore d'évaluation
- Ok - Effect of Melatonin On Broiler ChicksDocument12 pagesOk - Effect of Melatonin On Broiler ChicksOliver TalipPas encore d'évaluation
- COVID-19 and Pregnancy: A Review of Clinical Characteristics, Obstetric Outcomes and Vertical TransmissionDocument20 pagesCOVID-19 and Pregnancy: A Review of Clinical Characteristics, Obstetric Outcomes and Vertical TransmissionDra Sandra VèlezPas encore d'évaluation
- Acute Gastritis CiciDocument43 pagesAcute Gastritis CiciDwi Rezky AmaliaPas encore d'évaluation
- Annotated BibliographyDocument4 pagesAnnotated BibliographyJuanPas encore d'évaluation
- Vitamin and Mineral Supplementation During PregnanDocument4 pagesVitamin and Mineral Supplementation During PregnanEvi RachmawatiPas encore d'évaluation
- Drugs Used in Heart FailureDocument33 pagesDrugs Used in Heart FailureLynx Kee Bayating100% (1)
- Insights and Images: Vascular Channel Mimicking A Skull FractureDocument2 pagesInsights and Images: Vascular Channel Mimicking A Skull Fracturethariq mubarakPas encore d'évaluation
- Secukinumab: First Global ApprovalDocument10 pagesSecukinumab: First Global ApprovalAri KurniawanPas encore d'évaluation
- DKA Handout1Document59 pagesDKA Handout1alePas encore d'évaluation
- He2011 TMJ ANKYLOSIS CLASSIFICATIONDocument8 pagesHe2011 TMJ ANKYLOSIS CLASSIFICATIONPorcupine TreePas encore d'évaluation
- Patient Wellbeing Assessment and Recovery Plan - Children and AdolescentsDocument12 pagesPatient Wellbeing Assessment and Recovery Plan - Children and AdolescentsSyedaPas encore d'évaluation
- National NORCET Test-9Document106 pagesNational NORCET Test-9SHIVANIIPas encore d'évaluation
- Exercise #1 10Document10 pagesExercise #1 10John Paul FloresPas encore d'évaluation
- Medical Symptoms QuestionnaireDocument29 pagesMedical Symptoms QuestionnaireOlesiaPas encore d'évaluation
- NephrologyDocument9 pagesNephrologyEliDavidPas encore d'évaluation
- Lesson Plan On Spina BifidaDocument24 pagesLesson Plan On Spina BifidaPriyaPas encore d'évaluation
- Gujarat Technological University: W.E.F. AY 2017-18Document3 pagesGujarat Technological University: W.E.F. AY 2017-18raj royelPas encore d'évaluation
- Foundations of Operative Surgery An Introduction To Surgical TechniquesDocument165 pagesFoundations of Operative Surgery An Introduction To Surgical TechniquesTeodora-Valeria TolanPas encore d'évaluation
- Hydatidiform MoleDocument2 pagesHydatidiform MoleIrfan HardiPas encore d'évaluation