Académique Documents
Professionnel Documents
Culture Documents
Lab Elisa
Transféré par
Reggy Amalia NurgammaTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Lab Elisa
Transféré par
Reggy Amalia NurgammaDroits d'auteur :
Formats disponibles
H.K. Dermatol. Venereol. Bull.
(2005) 13, xx-xx
Review Article
The use of ELISA in pemphigus
W Chan
ELISA for desmoglein 1 and 3 antibodies using recombinant Dsg 1 and 3 is a new, specific and
sensitive technique for diagnosing pemphigus vulgaris and foliaceus. It also provides quantitative
data which may later prove to be a valuable tool for monitoring of disease activity.
1
Keywords: ELISA, Pemphigus vulgaris
Introduction
Pemphigus is a group of autoimmune blistering
diseases. There had been abundant evidence that
antibodies against components within the
desmosomes were responsible for its pathogenesis.
The major antigens in pemphigus vulgaris and
pemphigus foliaceus are desmoglein 3 (130 kDa)
and desmoglein 1 (160 kDa) respectively. They
are glycoproteins belonging to the cadherin family
and form part of the transmembranous component
of the desmosomes.1 Conventionally, pemphigus
Department of Medicine & Therapeutics, Prince of
Wales Hospital, Hong Kong
W Chan, MRCP, MSc(Clinical Dermatology)
Correspondence to: Dr. W Chan
Department of Medicine & Therapeutics, Prince of Wales
Hospital, 30-32 Ngan Shing Street, Shatin, N.T., Hong Kong
vulgaris and pemphigus foliaceus are distinguished
by their differences in clinical and histological
features.
Investigation for anti-desmoglein
antibodies
Direct immunofluorescence performed on skin
biopsies would show epidermal intercellular
deposits of IgG and C3 in both pemphigus
vulgaris and foliaceus. The presence of the
circulating antibodies can be detected by indirect
immunofluorescence technique. Patients' serum is
incubated with appropriate substrates (e.g.
monkey oesophagus, guinea pig or human skin)
at serial dilutions. The sections are then washed
and incubated with fluorochrome-labelled
conjugate against human IgG. Finally, they are
examined under fluorescence microscope, with or
W Chan
without counter stain, after a second wash.
However, this method is time consuming, operator
dependent and difficult to perform on large
number of samples. The sensitivity also depends
on the availability of suitable substrate and ranged
from 83-90% in experienced centres.2 Monkey
oesophagus is more sensitive for the diagnosis of
pemphigus vulgaris and human skin is more
sensitive for pemphigus foliaceus.3 The use of two
substrates, namely monkey oesophagus, (rich in
desmoglein 3) and human skin (rich in desmoglein
1) is recommended to improve the sensitivity.2
Immunoblotting technique can be used to
characterise the pemphigus antigens according
to their molecular weight. Patient's serum and the
enzyme labelled anti-human IgG is added to
epidermal extract of normal skin. For example, if
anti-desmoglein 3 is present, a band would be
produced at the 130 kDa area and if antidesmoglein 1 is present, a band would be
produced at the 160 kDa area. Although this
technique can be used to identify the target
antigens, it is again time consuming and can only
produce qualitative results.
ELISA for desmogleins 3 and 1
In recent years recombinant desmoglein 3 and
desmoglein 1 had been produced using
baculovirus expression and these recombinant
desmogleins were used to develop specific ELISA
(enzyme linked immunosorbent assay) to detect
antibodies against them. The first report of ELISA
for diagnosis of pemphigus was in 1997 and it
suggested that the method was sensitive and
specific.4 It also provided a quantitative method
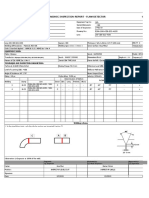
for measuring the antibodies levels. The principal
of the test is to measure anti-desmoglein-1 and
anti-desmoglein-3 antibodies present in the sera
by ELISA (Figure 1). Calibrators and patient sera
are added to microwells coated with desmoglein
1 and desmoglein 3 antigens, allowing antibodies
to react with the immobilised antigens. After
washing to remove any unbound serum proteins,
Sera added to microwells coated with
recombinant Dsg 1/3
Peroxidase conjugated
anti-human IgG antibodies
Chromogen added
and colour develops
Absorbance is
measured at 450 nm
and 620 nm
Figure 1. Schematic diagram of ELISA. (Dsg demoglein)
horseradish peroxidase conjugated IgG (Fab') is
added and incubated. Following another wash
step, the peroxidase substrate is added. Stop
solution is then added to each well to terminate
the enzyme reaction and to stabilise the colour
development. The assay can be quantified by
measuring the reaction photometrically and
plotting the results.
The use of ELISA was evaluated further in recent
years. In the study by Amagai, 97.9% of sera from
pemphigus foliaceus patients were positive in the
desmoglein 1 ELISA and 97.5% of sera from
pemphigus vulgaris patients were positive in the
desmoglein 3 ELISA.5 Only 1.1% and 2.2% of the
control sera were positive in desmoglein 1 and
desmoglein 3 ELISAs respectively. Harman et al
ELISA in pemphigus
recruited 82 patients with pemphigus vulgaris and
25 patients with pemphigus foliaceus who had
their diagnosis confirmed by clinical features,
histology, direct and indirect immunofluorescence.6
They also recruited 124 healthy controls and 193
disease controls (with mucous membrane
pemphigoid, lichen planus, other bullous and skin
diseases). The sensitivity of the desmoglein 3 ELISA
for diagnosing pemphigus vulgaris was 95%
overall and 100% in untreated patients. The
sensitivity of desmoglein 1 ELISA for diagnosing
pemphigus foliaceus was 92% overall and 100%
in untreated patients. Desmoglein 1 antibodies
were detected in 60% of pemphigus vulgaris
patients, while no desmoglein 3 antibodies were
detected in pemphigus foliaceus patients. The
specificity was as high as 98% or more. The overall
sensitivity of indirect immunofluorescence was
79% for pemphigus vulgaris and 84% for
pemphigus foliaceus respectively in this study.6
They concluded that ELISA was a sensitive and
specific diagnostic tool for pemphigus. Although
the level of sensitivity dropped when patients on
treatment were included, the figures were still far
better than the overall sensitivity of indirect
immunofluorescence.6 Using a combination of
desmoglein 1 and 3, it can also aid to distinguish
pemphigus vulgaris and pemphigus foliaceus. A
positive desmoglein 3 result is indicative of
pemphigus vulgaris, regardless of the associated
desmoglein 1 result. A negative desmoglein 3 and
a positive desmoglein 1 indicate a diagnosis of
pemphigus foliaceus.
Although the differentiation between pemphigus
vulgaris and foliaceus can usually be made without
detection of anti-desmoglein antibodies, ELISA
could be used as an aid in the occasion difficult
case. There had been reports on transition of
pemphigus vulgaris into foliaceus in a patient over
9 years period. The change in her phenotype was
mirrored in the level of desmoglein 3 and 1.7
The ELISA had several other advantages in
addition to high sensitivity and specificity. It
allowed samples to be tested in duplicates and
multiple samples to be tested without wasting
materials and reagents. The assay was simpler in
contrast to immunoblotting, required only 5 l of
serum and could be completed within one day,
allowing the analysis of large numbers of samples
in a relatively short time. The enzyme reaction in
ELISA when conjugated with anti-IgG antibodies
produced a colour change that could be measured
by absorbance which was indirectly related to the
quantity of antibodies. So it provides objective,
reproducible and quantitative data.6
Monitoring disease activity
Early studies suggested that antibodies titres
measured by indirect immunofluorescence could
be used as a marker of disease activity. However,
later studies gave conflicting results on the
reliability of this correlation, especially whether it
could be used as guide to therapy.8,9 This may
partly be due to the semi-quantitative and
subjective nature of the technique. With the
development of ELISA, this question had been
addressed again. In a study by Harman et al, 80
pemphigus vulgaris and 24 pemphigus foliaceus
patients were classified to quiescent, mild,
moderate or severe disease by a single
investigator.9 96-wells ELISA plates coated with
recombinant proteins of extracellular domain of
either desmoglein 1 or 3 were used. Antibodies
against desmoglein 3 and 1 in patients' serum
were detected by a standard method and
expressed as a percentage of a positive control
which arbitrarily contained 100 units of
desmoglein antibodies. The results showed that
the oral disease severity was related to desmoglein
3 antibody levels and skin disease severity to
desmoglein 1 antibodies level, regardless of
diagnosis. A 10-unit increase in desmoglein 1
ELISA value was associated with a 44% chance of
having a greater skin disease score in pemphigus
foliaceus cases (CI 20-73%, P<0.0005) and 33%
in pemphigus vulgaris cases (CI 23-44%, P<
0.005). A 10-unit increase in desmoglein 3 ELISA
W Chan
value was associated with a 20% chance of having
a greater oral disease score in pemphigus vulgaris
cases (CI 11-29%, P<0.0005). There was no
evidence of any effect of desmoglein 1 antibodies
on the severity of oral disease nor desmoglein 3
on skin disease.9 This was also consistent with the
'desmoglein compensation theory', which
explained the difference in phenotype between
pemphigus foliaceus, mucosal pemphigus vulgaris
and mucocutaneous pemphigus vulgaris (Figure
2).10 As desmoglein 1 is expressed more in upper
epidermis, acantholysis occurs in superficial
dermis. The mucous membrane and lower
epidermis is spared due to the co-expression of
desmoglein 3 in these sites. In pemphigus vulgaris,
acantholysis occurs in the mucous membrane due
to the distribution of desmoglein 3. If both
desmoglein 3 and 1 antibodies are present, there
tend to be more severe mucocutaneous disease.
The presence of desmoglein 1 antibodies in
pemphigus vulgaris patients predicted the
phenotype as well as a more severe disease
subgroup.11 It was suggested that the antibodies
to desmoglein 1 may be the result of epitope
spreading. However, some vulgaris patients did
not develop desmoglein 1 antibody despite long
standing disease. Proportion of patients with
desmoglein 1 antibodies were the same whether
they had treatment or not in the 79 patients
studied.11 Genetic factors may be important in
determining the autoantibody profile as
proportion of desmoglein 1 subjects was higher
in patients of Indian origin compared with white
northern Europeans.11
Despite the correlation, there were definitely
patients with high ELISA titres but clinically
quiescent disease. This may be due to nonpathological immunoglobulins (different subclass
or bind to epitopes that do not trigger disease) or
treatments. For patients with active disease but
low ELISA values, it is possible that there were
pathogenic antibodies to other epitopes which was
not detected.9 Preliminary data also suggested that
ELISA values were parallel to disease activity
Figure 2. Schematic diagram of desmoglein
compensation theory.
(unpublished data, Harman and Black). With
adequate normal and disease controls in a
population, studies are now being carried out to
see whether ELISA values may also reflect the
differences between different patients.
Other studies also produced similar conclusions.
It was also suggested that if the antibodies level
was very high, the reaction may saturate.
Appropriate dilution of the serum will be needed
to give a linear relationship and can provide
serological information on disease activity.12 There
is no data on the time lag between changes in
antibody titres and clinical symptoms and signs.
Sometimes increase in antibody titres may precede
clinical deterioration and this should alert the
clinician in management of the patient.
ELISA in pemphigus
The cost of testing a single sample in both the
desmoglein 1 and 3 ELISAs was UK13-18
(excluding labour, shipping costs and
consumables), depending on the number of
samples tested per batch.9 The manufacturer listed
certain limitations of the test: the test should be
interpreted in conjunction with clinical evaluation
of the patient along with other diagnostic
procedures, performance of these assays in the
paediatric population has not been established.
The assay performance characteristics have not
been established for matrices other than serum.
A positive result indicates the presence of
antibodies to recombinant desmoglein-1 or
desmoglein-3 and does not specifically identify a
certain type of pemphigus and a negative result
does not rule out the presence of all pemphigus
disease.13
ELISA had also been used to confirm the
transplacental transfer of antibodies by measuring
the desmoglein 3 antibodies level in serum from
mother with pemphigus vulgaris, cord blood and
the neonate.14 Currently ELISA for other conditions
are being developed such as BP 180 antigen for
the use in bullous pemphigoid.
In Hong Kong, the number of pemphigus patients
in each individual centre is limited. If ELISA for
desmoglein is to be introduced, it would probably
be more cost effective to have a regional centre
to collect all serum samples and perform the tests
as a batch. It would also be necessary to obtain
data on normal control within the population. The
frequency of test needed in each individual patient
for disease monitoring will depend on the severity
of his/her condition and clinical grounds.
Summary
The ELISA for desmoglein 1 and 3 antibodies
appears to be a highly specific and sensitive
technique for diagnosing pemphigus vulgaris
and foliaceus. The quantitative data provided
may also prove to be a valuable tool for
monitoring disease activity and even in guiding
patient management. However, it should be
emphasised that the patients and treatments
should be assessed primarily by clinical
improvement and only secondarily by laboratory
data.
References
1.
Hashimoto T. Recent advances in the study of the
pathophysiology of pemphigus. Arch Dermatol Res
2003;295 Suppl 1:S2-11.
2. Harman KE, Gratian MJ, Bhogal BS, Challacombe SJ,
Black MM. The use of two substrates to improve the
sensitivity of indirect immunofluorescence in the
diagnosis of pemphigus. Br J Dermatol 2000;142:
1135-9.
3. Kanitakis J. Indirect immunofluorescence microscopy
for the serological diagnosis of autoimmune blistering
skin diseases: a review. Clin Dermatol 2001;19:
614-21.
4. Ishii K, Amagai M, Hall RP, Hashimoto T, Takayanagi
A, Gamou S, et al. Characterization of autoantibodies
in pemphigus using antigen-specific enzyme-linked
immunosorbent assays with baculovirus-expressed
recombinant desmogleins. J Immunol 1997;159:
2010-7.
5. Amagai M, Komai A, Hashimoto T, Shirakata Y,
Hashimoto K, Yamada T, et al. Usefulness of enzymelinked immunosorbent assay using recombinant
desmogleins 1 and 3 for serodiagnosis of pemphigus.
Br J Dermatol 1999;140:351-7.
6. Harman KE, Gratian MJ, Seed PT, Bhogal BS,
Challacombe SJ, Black MM. Diagnosis of pemphigus
by ELISA: a critical evaluation of two ELISAs for the
detection of antibodies to the major pemphigus
antigens, desmoglein 1 and 3. Clin Exp Dermatol
2000;25:236-40.
7. Harman KE, Gratian MJ, Shirlaw PJ, Bhogal BS,
Challacombe SJ, Black MM. The transition of
pemphigus vulgaris into pemphigus foliaceus: a
reflection of changing desmoglein 1 and 3
autoantibody levels in pemphigus vulgaris. Br J
Dermatol 2002;146:684-7.
8. Creswell SN, Black MM, Bhogal B, Skeete MV.
Correlation of circulating intercellular antibody titres
in pemphigus with disease activity. Clin Exp Dermatol
1981;6:477-83.
9. Harman KE, Seed PT, Gratian MJ, Bhogal BS,
Challacombe SJ, Black MM. The severity of cutaneous
and oral pemphigus is related to desmoglein 1 and 3
antibody levels. Br J Dermatol 2001;144:775-80.
10. Mahoney MG, Wang Z, Rothenberger K, Koch PJ,
Amagai M, Stanley JR. Explanations for the clinical and
microscopic localization of lesions in pemphigus
W Chan
foliaceus and vulgaris. J Clin Invest 1999;103:461-8.
11. Harman KE, Gratian MJ, Bhogal BS, Challacombe SJ,
Black MM. A study of desmoglein 1 autoantibodies in
pemphigus vulgaris: racial differences in frequency and
the association with a more severe phenotype. Br J
Dermatol 2000;143:343-8.
12. Cheng SW, Kobayashi M, Kinoshita-Kuroda K,
Tanikawa A, Amagai M, Nishikawa T. Monitoring
disease activity in pemphigus with enzyme-linked
immunosorbent assay using recombinant desmogleins
1 and 3. Br J Dermatol 2002;147:261-5.
13. The RhiGene MESACUP DSG-1 & DSG-3 ELISA TEST
SYSTEM. Available from: http://www.corgenixonline.
com/package_inst.pdf/DSG%20INSERT%202.pdf
14. Okubo S, Sato-Matsumura KC, Abe R, Aoyagi S,
Akiyama M, Yokota K, et al. The use of ELISA to detect
desmoglein antibodies in a pregnant woman and fetus.
Arch Dermatol 2003;139:1217-8.
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Chapter - 2 Fish MongeryDocument10 pagesChapter - 2 Fish MongeryKrishna ChaudharyPas encore d'évaluation
- Optra - NubiraDocument37 pagesOptra - NubiraDaniel Castillo PeñaPas encore d'évaluation
- Polygon shapes solve complex mechanical problemsDocument6 pagesPolygon shapes solve complex mechanical problemskristoffer_mosshedenPas encore d'évaluation
- Securing Obligations Through Pledge and MortgageDocument4 pagesSecuring Obligations Through Pledge and MortgagePrincessAngelaDeLeon100% (1)
- Ôn tập và kiểm tra học kì Tiếng anh 6 ĐÁP ÁNDocument143 pagesÔn tập và kiểm tra học kì Tiếng anh 6 ĐÁP ÁNThùy TinaPas encore d'évaluation
- Pneapple Waste To Bioethanol Casabar - Et - Al-2019-Biomass - Conversion - and - BiorefineryDocument6 pagesPneapple Waste To Bioethanol Casabar - Et - Al-2019-Biomass - Conversion - and - Biorefineryflorian willfortPas encore d'évaluation
- Subtracting-Fractions-Unlike DenominatorsDocument2 pagesSubtracting-Fractions-Unlike Denominatorsapi-3953531900% (1)
- Boat DesignDocument8 pagesBoat DesignporkovanPas encore d'évaluation
- Entrepreneurial Intentions of Cavite Business StudentsDocument12 pagesEntrepreneurial Intentions of Cavite Business StudentsKevin Pereña GuinsisanaPas encore d'évaluation
- Ut ProcedureDocument2 pagesUt ProcedureJJ WeldingPas encore d'évaluation
- Jt20 ManualDocument201 pagesJt20 Manualweider11Pas encore d'évaluation
- Weakness and Hypotonia: Prepared by DR Hodan Jama MDDocument38 pagesWeakness and Hypotonia: Prepared by DR Hodan Jama MDabdisalaan hassanPas encore d'évaluation
- Drug Delivery Technologies and Future DirectionsDocument14 pagesDrug Delivery Technologies and Future Directionsraju1559405Pas encore d'évaluation
- Abinitio Interview QuesDocument30 pagesAbinitio Interview QuesVasu ManchikalapudiPas encore d'évaluation
- Vortex: Opencl Compatible Risc-V Gpgpu: Fares Elsabbagh Blaise Tine Priyadarshini Roshan Ethan Lyons Euna KimDocument7 pagesVortex: Opencl Compatible Risc-V Gpgpu: Fares Elsabbagh Blaise Tine Priyadarshini Roshan Ethan Lyons Euna KimhiraPas encore d'évaluation
- Bron 2017Document73 pagesBron 2017Anggia BungaPas encore d'évaluation
- Wicks Angela, Roethlein Christopher - A Satisfaction - Based Definition of QualityDocument1 pageWicks Angela, Roethlein Christopher - A Satisfaction - Based Definition of Qualityalfdjole0% (1)
- CONTACT DETAILS HC JUDGES LIBRARIESDocument4 pagesCONTACT DETAILS HC JUDGES LIBRARIESSHIVAM BHATTACHARYAPas encore d'évaluation
- ACCA P1 Governance, Risk, and Ethics - Revision QuestionsDocument2 pagesACCA P1 Governance, Risk, and Ethics - Revision QuestionsChan Tsu ChongPas encore d'évaluation
- Asset Valuation: Debt Investments: Analysis and Valuation: 1 2 N M 1 2 N MDocument23 pagesAsset Valuation: Debt Investments: Analysis and Valuation: 1 2 N M 1 2 N MSirSmirkPas encore d'évaluation
- Research Chapter 1Document7 pagesResearch Chapter 1Aryando Mocali TampubolonPas encore d'évaluation
- Explosive Loading of Engineering Structures PDFDocument2 pagesExplosive Loading of Engineering Structures PDFBillPas encore d'évaluation
- Chapter 4 and 5 - For StudentsDocument6 pagesChapter 4 and 5 - For Studentsdesada testPas encore d'évaluation
- Online JournalismDocument24 pagesOnline JournalismZandra Kate NerPas encore d'évaluation
- Pakistan Affairs Current Affairs 2016 MCQSDocument3 pagesPakistan Affairs Current Affairs 2016 MCQSMuhammad MudassarPas encore d'évaluation
- Ground Floor 40X80 Option-1Document1 pageGround Floor 40X80 Option-1Ashish SrivastavaPas encore d'évaluation
- TH255C Engine CAT PartsDocument134 pagesTH255C Engine CAT PartsKevine KhaledPas encore d'évaluation
- Me2404 Set1Document16 pagesMe2404 Set1sakthivelsvsPas encore d'évaluation
- Organization & Management: Manuel L. Hermosa, RN, Mba, Man, Edd, LPT, MaedcDocument32 pagesOrganization & Management: Manuel L. Hermosa, RN, Mba, Man, Edd, LPT, MaedcManny HermosaPas encore d'évaluation
- Arsh Final Project ReportDocument65 pagesArsh Final Project Report720 Manvir SinghPas encore d'évaluation