Académique Documents
Professionnel Documents
Culture Documents
Journal Trig Neuralgia
Transféré par
marhayudi15Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Journal Trig Neuralgia
Transféré par
marhayudi15Droits d'auteur :
Formats disponibles
ORIGINAL RESEARCH ARTICLE
CNS Drugs 2011; 25 (10): 847-857
1172-7047/11/0010-0847/$49.95/0
2011 Adis Data Information BV. All rights reserved.
Topiramate versus Carbamazepine
for the Treatment of Classical
Trigeminal Neuralgia
A Meta-Analysis
Qiang-ping Wang and Min Bai
Department of Neurosurgery, Dujiangyan Peoples Hospital, Dujiangyan Medical Center, Dujiangyan, China
Abstract
Background: Carbamazepine is currently the drug of first choice in the
treatment of trigeminal neuralgia. However, it is reported as efficacious in
only 7080% of patients, and can be associated with adverse effects such as
drowsiness, confusion, nausea, ataxia, nystagmus and hypersensitivity, which
may necessitate discontinuation of medication. Therefore, alternative drugs
such as oxcarbazepine, baclofen and topiramate are also used to treat the
disease.
Objectives: The aim of this study was to compare the effectiveness and safety
of topiramate with carbamazepine in the treatment of classical trigeminal
neuralgia.
Methods: We searched the Cochrane Central Register of Controlled Trials
(CENTRAL) [Issue 3 of 12, March 2011], MEDLINE, EMBASE, the
Chinese Biomedical Database (CBM), the Chinese National Knowledge Infrastructure (CNKI) and the Chinese Science and Technique Journals
Database (VIP) for the period January 1998 to March 2011, and we also
manually searched all relevant journals. We included all confirmed randomized controlled trials treating trigeminal neuralgia with topiramate and carbamazepine. We evaluated the risk of bias of the included trials according to
the Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.
The Cochrane Collaborations software RevMan 5.1 was used for the metaanalysis.
Results: A total of six randomized controlled trials with poor methodological
quality were included. All trials were conducted in China. Altogether, they
included 354 patients with trigeminal neuralgia. The results of the metaanalysis showed that topiramate was more effective than carbamazepine after
a treatment duration of 2 months (relative risk [RR] = 1.20, 95% CI 1.04, 1.39,
p = 0.01). However, no difference was found in the effectiveness rate after a
treatment duration of 1 month (RR = 1.00, 95% CI 0.87, 1.14, p = 0.94), in the
remission rate after a treatment duration of 1 month (RR = 1.06, 95% CI 0.83,
Wang & Bai
848
1.36, p = 0.63), in the remission rate after a treatment duration of 2 months
(RR = 1.31, 95% CI 0.96, 1.80, p = 0.09) or in adverse events when comparing
topiramate with carbamazepine.
Conclusions: Present trials comparing topiramate with carbamazepine are all
poor in methodological quality. A meta-analysis of these studies showed that
the overall effectiveness and tolerability of topiramate did not seem to differ
from carbamazepine in the treatment of classical trigeminal neuralgia.
However, the meta-analysis yielded a favourable effect of topiramate compared with carbamazepine after a treatment duration of 2 months. Results
were limited due to the poor methodological quality and the geographic localization of the randomized controlled trials identified. Therefore, large,
international, well conducted, randomized controlled trials are needed to
further assess the relative efficacy and tolerability of topiramate and carbamazepine in this indication.
Background
Trigeminal neuralgia is the most common
neuralgia and is often defined as sudden, severe,
brief, stabbing, usually unilateral, recurrent episodes of pain in the distribution of one or more
branches of the trigeminal nerve.[1] The annual
incidence of trigeminal neuralgia is 45/100 000[2]
and it can be classified into classical and symptomatic trigeminal neuralgia.[3] Symptomatic trigeminal neuralgia includes all cases of trigeminal
neuralgia secondary to a tumour, multiple sclerosis,
structural abnormalities of the skull base, etc.
whereas the diagnosis of classical trigeminal
neuralgia can only be made in cases without an
established aetiology, i.e. idiopathic, as well as in
cases with potential vascular compression of the
fifth cranial nerve, according to the latest classification of the International Headache Society.[3]
There is a distinct difference between the
treatment of classical trigeminal neuralgia and
symptomatic trigeminal neuralgia. CT or MRI is
primarily considered to determine whether there
are structural causes in patients with trigeminal
neuralgia.[4] The primary disease should be managed first in patients with symptomatic trigeminal neuralgia. There are many methods for the
treatment of classical trigeminal neuralgia, including pharmacotherapy, a block or destruction
of portions of the trigeminal nerve, cryotherapy,
2011 Adis Data Information BV. All rights reserved.
pharmaceutical injection, peripheral acupuncture,
radiofrequency thermocoagulation, g knife surgery
and other surgery options. The efficacies of Gasserian ganglion percutaneous techniques and microvascular decompression for classical trigeminal
neuralgia have been demonstrated;[4] however, they
should be reserved for when there is a decrease in
efficacy or tolerability of medication because they
are destructive processes.[5] Other treatments such
as g knife surgery, cryotherapy, pharmaceutical
injection and peripheral acupuncture show some
degree of therapeutic effectiveness, but they also
present various kinds of adverse effects or limits.[6]
Therefore, drugs still play the most important role
in the treatment of classical trigeminal neuralgia
especially in patients who have been newly diagnosed. Carbamazepine is considered a first-line
treatment for classical trigeminal neuralgia, and
it has been demonstrated to achieve a reduction
in attacks in up to 88% of patients.[4,7-9] However,
the efficacy of carbamazepine is compromised by
poor tolerability of severe adverse effects such
as drowsiness, confusion, nausea and ataxia.[10]
Oxcarbazepine has also been shown to be effective and is considered a second-line treatment for
trigeminal neuralgia,[4,11] but it is expensive. Baclofen, lamotrigine, pimozide and some other
drugs are also used in the treatment of trigeminal
neuralgia; however, the efficacy of these drugs
remains uncertain.[4]
CNS Drugs 2011; 25 (10)
Topiramate vs Carbamazepine for Classical Trigeminal Neuralgia
Topiramate, a sulfamate-substituted monosaccharide, was first identified as an antiepileptic
drug. Compared with other antiepileptics, this
drug acts at different neural transmission levels
such as sodium channels and enhances GABA
levels, and has been termed a neurostabilizer.[12]
It is used to treat CNS conditions such as neuropathies, eating disorders, alcohol and drug
dependence, migraine, nerve injury, restless leg
syndrome, essential tremor and psychiatric diseases.[13-15] Topiramate is generally well tolerated
at low doses[16] but at high doses it may cause
various kinds of adverse effects including paraesthesia, dysphasia, fatigue, confusion and insomnia.[17] Topiramate is also used for the treatment
of classical trigeminal neuralgia, but its efficacy
remains controversial. Great disparities in results
have been obtained among research into the efficacy of topiramate for classical trigeminal neuralgia.[18-26] In order to determine the effectiveness
and safety of topiramate for classical trigeminal
neuralgia, we conducted a systematic review to
critically evaluate all of the currently available,
randomized controlled trials that compared topiramate with carbamazepine in the treatment of
classical trigeminal neuralgia.
Methods
Data Sources
The following electronic databases were searched
from January 1998 to March 2011: Cochrane Central Register of Controlled Trials (CENTRAL)
[Issue 3 of 12, March 2011], MEDLINE, EMBASE,
the Chinese Biomedical Database (CBM), the
Chinese National Knowledge Infrastructure
(CNKI) and the Chinese Science and Technique
Journals Database (VIP). The first search term
was tic douloureux, trigeminal neuralgia, trigeminal neuropathy or facial pain, the second
search term was carbamazepine or tegretol,
and the third search term was topiramate or
topamax. We combined these three terms for the
electronic search. Corresponding Chinese terms
were also searched. There were no language restrictions. In addition, we also manually searched
all relevant journals. References were addressed
2011 Adis Data Information BV. All rights reserved.
849
in original articles, and reviews were further
searched for relevant studies. Dissertations and
abstracts were also included.
Study Selection
All randomized controlled trials comparing
topiramate with carbamazepine in the treatment
of classical trigeminal neuralgia were considered.
Trigeminal neuralgia had to have been diagnosed
according to a standardized criterion such as the
classification of the International Headache
Society,[3] and classical trigeminal neuralgia had
to have been confirmed by CT or MRI. To be
included in our analysis, trials were required to
have similar baseline characteristics in both study
groups. Trials that involved patients with other
diseases such as organic pain, psychiatric diseases
or other kinds of facial pain were excluded. Trials
using any other medications were also excluded.
Outcome Measures
The main outcomes were the number of participants who responded to treatment, the number of participants who achieved remission and
the number of adverse events reported. We extracted and classified the outcomes of the selected
trials according to the authors original definitions only when they met explicit criteria such as
the system proposed by Spacek et al.[27] If appropriate, we classified the outcomes according
to an explicit criterion when the authors original
definitions did not.
Data Extraction and Quality Assessment
The two authors of this article (Qiang-ping
Wang and Min Bai) independently identified every
potential article and assessed its methodological
quality. Data from all articles were validated and
extracted according to predefined criteria (table I).
Risk of bias was assessed according to the latest
Cochrane classification.[29] Disagreements were
resolved by discussion between the two authors.
Data Synthesis
To compare the effectiveness and safety
of topiramate with carbamazepine we used the
CNS Drugs 2011; 25 (10)
Wang & Bai
2011 Adis Data Information BV. All rights reserved.
a Structural causes were observed by CT or MRI.
b Patients presented with organic pain, mental disease or other facial pain.
c The diagnosis standard proposed by Zheng and Deng.[28]
d Patients presented with impaired sensory or motor function, or with focal neurological signs.
bid = twice daily; ICHD = International Classification of Headache Disorders, 2nd edition;[3] ID = initial dosage; MD = maximal dosage; NR = not reported; tid = three times daily;
VAS = Visual Analogue Scale.
NR
ID: 0.2 g tid
MD: 0.6 g/day
22/21
Structurala
Neurologicald
Zhengc
Xia,[26] 2010
4871
15
NR
ID: 25 mg bid
MD: 200 mg/day
NR
ID: 0.1 g tid
MD: 0.8 g/day
33/33
Structural
Neurologicald
Zheng
Li et al.,[25] 2010
4073; mean: 49.2
30
942;
median: 12
ID: 25 mg bid
MD: 400 mg/day
NR
ID: 0.1 g tid
MD: 0.6 g/day
33/33
Structurala
NR
Gong,[24] 2010
4078; mean: 49.7
45
842;
median: 12
ID: 25 mg bid
MD: 600 mg/day
NR
ID: 0.1 g tid
MD: 1.1 g/day
34/31
Structurala
Neurologicald
Zhengc
Zeng and
Chen,[23] 2009
5073
TPM: mean: 57.4 15.6
CBZ: mean: 58.2 14.9
30 (16/14)
NR
ID: 25 mg bid
MD: 400 mg/day
VAS
ID: 0.2 g tid
MD: 0.6 g/day
Pain
ICHD
Dong et al.,[22]
2008
23/23
4078
TPM: mean: 56 10
CBZ: mean: 54 7
22 (11/11)
NR
ID: 25 mg bid
MD: 200 mg/day
NR
ID: 0.1 g tid
MD: 1.0 g/day
38/30
NR
Chen,[21] 2008
Structurala
5082
35
NR
ID: 25 mg bid
MD: 400 mg/day
Method for outcome
assessment
Treatment
duration (mo)
Dosage
regimen (CBZ)
Dosage regimen
(TPM)
Disease
duration (mo)
Male patients
(TPM/CBZ)
Age (y)
No. in group
(TPM/CBZ)
Exclusion
criteria
Inclusion
criteria
Study, year
Table I. General information from randomized controlled trials comparing topiramate (TPM) with carbamazepine (CBZ) in the treatment of classical trigeminal neuralgia
850
Cochrane Collaborations software RevMan 5.1
(The Nordic Cochrane Centre, The Cochrane
Collaboration, 2011, Copenhagen, Denmark) to
abstract the risk estimates (relative risk: RR) and
the 95% confidence intervals (CI). For studies
without sufficient information, we contacted the
primary authors in order to acquire and verify
data when necessary. In order to ensure clinical
homogeneity, we divided trials into two subgroups
according to the duration of the intervention. The
chi-square (w2) test and the Higgins I2 test were used
to assess heterogeneity. We then pooled the data
across studies using fixed effects models if statistical
heterogeneity did not exist. If appropriate, a metaanalysis was conducted using random effects models when statistical heterogeneity did exist.
Results
Study Description and Quality
The literature search revealed 93 articles, of
which 87 studies were excluded (figure 1). Six
trials met our inclusion criteria, and their general
information is listed in table I. All trials originated from China, and all articles were published
in Chinese. No article published in another language was found. Only one trial[22] included
patients with the diagnosis of classical trigeminal
neuralgia according to the International Classification of Headache Disorders (ICHD) that was
formulated by the Headache Classification Subcommittee of the International Headache Society.[3]
Three trials[23,25,26] included patients diagnosed according to a Chinese criterion that was published
by Zheng and Deng.[28] The following main points
were proposed by Zheng and Deng[28] to aid in the
diagnosis of trigeminal neuralgia:
! The pain is always located in the distribution
of the trigeminal nerve.
! The pain is always unilateral.
! The pain is provoked by touching a relevant
trigger point but attacks of pain can also be
spontaneous.
! The pain is recurrent; each single burst of pain
lasts under 2 minutes on average.
! There is no pain between bursts of pain, and
most patients will have complete remission of
pain for weeks or months, at least initially.
CNS Drugs 2011; 25 (10)
Topiramate vs Carbamazepine for Classical Trigeminal Neuralgia
Potentially relevant articles
identified (n = 93)
Articles excluded by screening the
title and abstract (n = 76):
not relevant to this study (n = 55)
duplicated studies (n = 2)
case report (n = 7)
not a clinical trial (n = 12)
Further evaluation
(n = 17)
Articles excluded after reading the
full text (n = 11):
non-randomized controlled trials
(n = 2)
uncontrolled trials (n = 3)
mixing CTN with other neuralgia (n = 1)
no usable information for meta-analysis
and authors uncontactable (n = 3)
comparing TPM with placebo (n = 2)
851
tensity by more than 50%, and remission was
defined as the disappearance of the symptoms of
trigeminal neuralgia. A reduction of <50% or no
change was considered ineffective therapy.
The quality assessment of the trials is shown in
table II. All trials had a high risk of bias. Details
of how patients were randomized were only given
in two trials,[23,25] and detailed information on
randomization and allocation concealment was not
provided in other studies. The method of blinding
of patients and assessors was not reported in any
of the trials. The baseline characteristics were
similar between groups in all trials (p > 0.05), as
mentioned, but detailed information with respect
to sex, age or severity of clinical status was not
presented in most trials. Details of follow-up and
the number of dropouts or withdrawals were not
clearly reported in any of the trials.
Outcomes
Effectiveness Rate
Trials met the inclusion
criteria (n = 6)
Fig. 1. Flowchart of trial selection process. CTN = classical trigeminal neuralgia; TPM = topiramate.
! Other unilateral facial pains such as toothache, temporomandibular disorders, postherpetic neuralgia and traumatic neuropathic
trigeminal pain have been excluded.
Altogether, a total of 354 patients were included
in the six trials. All patients were adults, and the
duration of disease ranged from 8 to 42 months.
All topiramate groups were given an initial dosage of 25 mg twice per day, and the dosage was
gradually increased according to clinical symptoms. The maximal dosage ranged from 200 to
600 mg/day among trials. Duration of treatment
in three of the trials was 1 month,[21,22,24] and it
was 2 months in the other trials.[23,25,26] There
was only one trial[22] that assessed the results
using the Visual Analog Scale (VAS).[27] Details
of how the outcomes were measured were not
given in other trials. Outcomes in all trials were
classified according to the system proposed by
Spacek et al.[27] Response to treatment was defined as a reduction in both frequency and in 2011 Adis Data Information BV. All rights reserved.
The number of patients who responded to the
therapy was provided in all trials. A small degree
of heterogeneity between the trials was observed
(w2 = 8.33, p = 0.14, I2 = 40%), so we conducted
a meta-analysis using random effects models
(figure 2). We found no significant differences
between the two groups in a pooled analysis
(RR = 1.08, 95% CI 0.96, 1.21, p = 0.20). In subgroup analyses, there were also no significant differences between groups after a treatment duration
of 1 month (RR = 1.00, 95% CI 0.87, 1.14, p = 0.94,
heterogeneity: w2 = 3.04, p = 0.22, I2 = 34%). However, the meta-analysis showed statistically significantly superior effectiveness of topiramate
compared with carbamazepine after a treatment
duration of 2 months (RR = 1.20, 95% CI 1.04,
1.39, p = 0.01, heterogeneity: w2 = 0.24, p = 0.89,
I2 = 0%). Even though the CI of the summary estimates in the two subgroups overlapped to a
small degree, substantial differences were observed between the two subgroups with different
therapy durations (w2 = 3.41, p = 0.06, I2 = 70.7%).
Remission Rate
The number of patients who gained remission
after treatment was provided in all trials. No
heterogeneity between the trials was observed
CNS Drugs 2011; 25 (10)
Wang & Bai
852
Table II. Methodological quality of randomized controlled trials comparing topiramate with carbamazepine in the treatment of classical
trigeminal neuralgia, using Cochrane criteria for assessment of bias[29]
Study, year
Allocation
concealment
Random
sequence
generation
Blinding of
participants
and personnel
Incomplete
outcome data
Blinding of
outcome
assessment
Selective
reporting
Other bias
(outcome
assessment)
Chen,[21] 2008
Unclear
Unclear
Unclear
Unclear
Unclear
Unclear
High
Dong et al.,[22] 2008
Unclear
Unclear
Unclear
Unclear
Unclear
Unclear
Low
High
Zeng and Chen,[23] 2009
Lowa
Unclear
Unclear
Unclear
Unclear
Unclear
Gong,[24] 2010
Unclear
Unclear
Unclear
Unclear
Unclear
Unclear
High
Li et al.,[25] 2010
Lowb
Unclear
Unclear
Unclear
Unclear
Unclear
High
Xia,[26] 2010
Unclear
Unclear
Unclear
Unclear
Unclear
Unclear
High
Coin tossing.
Drawing of lots.
High = high risk of bias; Low = low risk of bias; Unclear = unclear risk of bias.
(w2 = 2.14, p = 0.83, I2 = 0%, figure 3). We conducted
a meta-analysis using fixed effects models. The
meta-analysis showed no significant differences
between the two groups in a pooled analysis
(RR = 1.17, 95% CI 0.96, 1.42, p = 0.12). No significant differences were yielded between the two
Topiramate
Study or subgroup, year events total
groups after a treatment duration of 1 month
(RR = 1.06; 95% CI 0.83, 1.36, p = 0.63, heterogeneity: w2 = 0.60, p = 0.74, I2 = 0%) or after a
treatment duration of 2 months (RR = 1.31, 95% CI
0.96, 1.80, p = 0.09, heterogeneity: w2 = 0.21, p = 0.90,
I2 = 0%) via subgroup analyses. There were no
Carbamazepine
Risk ratio
total Weight M-H, random, 95% CI
events
Risk ratio
M-H, random, 95% CI
Effectiveness rate (1 month)
Chen,[21] 2008
Dong et al.,[22] 2008
Gong,[24] 2010
Subtotal (95% CI)
33
20
29
38
23
33
94
22
21
31
30
23
33
86
14.4%
18.6%
24.4%
57.5%
1.18 [0.92, 1.52]
0.95 [0.78, 1.17]
0.94 [0.80, 1.09]
1.00 [0.87, 1.14]
33
21
31
85
17.7%
11.6%
13.3%
42.5%
1.24 [1.00, 1.53]
1.13 [0.85, 1.52]
1.20 [0.92, 1.57]
1.20 [1.04, 1.39]
74
82
Total events
Heterogeneity: 2 = 3.04, df = 2 (p = 0.22); I 2 = 34%
Test for overall effect: Z = 0.07 (p = 0.94)
Effectiveness rate (2 months)
33
25
31
Li et al.,[25] 2010
22
16
19
Xia,[26] 2010
34
22
29
Zeng and Chen,[23] 2009
89
Subtotal (95% CI)
63
79
Total events
Heterogeneity: 2 = 0.24, df = 2 (p = 0.89); I 2 = 0%
Test for overall effect: Z = 2.51 (p = 0.01)
171 100.0%
183
Total (95% CI)
137
161
Total events
Heterogeneity: 2 = 8.33, df = 5 (p = 0.14); I 2 = 40%
Test for overall effect: Z = 1.28 (p = 0.20)
Test for subgroup differences: 2 = 3.41, df = 1 (p = 0.06); I 2 = 70.7%
1.08 [0.96, 1.21]
0.2
0.5
1
Favours
carbamazepine
2
Favours
topiramate
Fig. 2. Forest plot of the effectiveness rate of topiramate vs carbamazepine for classical trigeminal neuralgia. df = degrees of freedom;
M-H = Mantel-Haenszel test.
2011 Adis Data Information BV. All rights reserved.
CNS Drugs 2011; 25 (10)
Topiramate vs Carbamazepine for Classical Trigeminal Neuralgia
Topiramate
Study or subgroup, year events total
Carbamazepine
events total Weight
853
Risk ratio
M-H, fixed, 95% CI
Risk ratio
M-H, fixed, 95% CI
Remission rate (1 month)
20
38
Chen,[21] 2008
13
14
23
Dong et al.,[22] 2008
15
22
Gong,[24] 2010
33
21
Subtotal (95% CI)
94
56
Total events
49
Heterogeneity: 2 = 0.60, df = 2 (p = 0.74); I 2 = 0%
Test for overall effect: Z = 0.48 (p = 0.63)
30
23
33
86
16.8%
17.4%
24.3%
58.6%
1.21 [0.73, 2.02]
0.93 [0.60, 1.45]
1.05 [0.74, 1.49]
1.06 [0.83, 1.36]
33 17.4%
21 8.3%
31 15.8%
85 41.4%
1.40 [0.89, 2.20]
1.36 [0.64, 2.91]
1.19 [0.70, 2.03]
1.31 [0.96, 1.80]
171 100.0%
1.17 [0.96, 1.42]
Remission rate (2 months)
21
Li et al.,[25] 2010
33
15
Xia,[26] 2010
10
22
7
Zeng and Chen,[23] 2009
17
34
13
Subtotal (95% CI)
89
48
Total events
35
Heterogeneity: 2 = 0.21, df = 2 (p = 0.90); I 2 = 0%
Test for overall effect: Z = 1.69 (p = 0.09)
Total (95% CI)
Total events
183
104
84
Heterogeneity: 2 = 2.14, df = 5 (p = 0.83); I 2 = 0%
Test for overall effect: Z = 1.54 (p = 0.12)
Test for subgroup differences: 2 = 1.08, df = 1 (p = 0.30); I 2 = 7.7%
0.1
0.2
0.5
1
Favours
carbamazepine
2
5
Favours
topiramate
10
Fig. 3. Forest plot of the remission rate of topiramate vs carbamazepine for classical trigeminal neuralgia. df = degrees of freedom;
M-H = Mantel-Haenszel test.
significant differences between the two subgroups
(w2 = 1.08, p = 0.30, I2 = 7.7%).
Safety
Detailed information about adverse events
was provided in all trials. Among participants
allocated to receive topiramate, 29 of 183 (15.8%)
experienced some adverse events, mainly manifested as somnolence (8), dizziness (7), nausea (7),
ataxia (2) and confusion (2). 36 of 171 (21.1%)
participants allocated to receive carbamazepine
presented with adverse events, mainly manifested
as dizziness (12), somnolence (6), nystagmus (5),
ataxia (4), nausea (3) and fatigue (2) [table III].
The meta-analysis on individual adverse events
such as dizziness (figure 4), nausea and somnolence showed no significant differences between
the two groups (table III). However, participants
allocated to carbamazepine groups might be more
likely to experience adverse effects such as nystagmus, fatigue and rash, which were not recorded
in the topiramate groups, although our analysis
2011 Adis Data Information BV. All rights reserved.
did not reveal significant differences between
treatments for these events.
Discussion
We conducted a systematic review and metaanalysis of all available randomized controlled
trials on the comparative efficacy and adverse
events of topiramate compared with carbamazepine.
The results showed equally favourable effectiveness and acceptable tolerability of topiramate compared with carbamazepine in the treatment of
classical trigeminal neuralgia, which differed from
the conclusions of some authors and guidelines.[4-11]
We considered that there were two possible explanations for these findings as follows: topiramate
might indeed be effective, or existing studies might
have been inadequately designed and the effects of
topiramate might have been overestimated.
There were many limitations in our analysis,
precluding a firm conclusion on the effectiveness
of topiramate for classical trigeminal neuralgia.
CNS Drugs 2011; 25 (10)
Wang & Bai
0.49
0.27
0.46
0.33
0.07
0.62
0.32
0.45
0.33
0.18
0.59
0.13, 70.02
0.01, 3.67
0.01, 7.22
0.04, 3.11
0.04, 1.17
0.23, 12.29
0.23, 91.66
0.20, 2.05
0.56, 5.50
0.22, 1.33
95% CI of RR
0.49, 3.42
3.00
0.18
0.30
0.33
0.20
1.67
4.57
0.64
1.30
1.76
0.54
RR
0/0
0/0
0/0
0/0
0/2
0/0
0/0
0/1
3/2
1/0
1/2
2011 Adis Data Information BV. All rights reserved.
p-Value
RR = relative risk.
22/21
Xia,[26] 2010
0/0
0/0
0/0
0/1
0/0
1/1
0/0
1/0
0/2
1/2
1/2
33/33
2010
Li et al.,
0/0
0/0
0/0
0/0
0/0
1/0
0/0
1/0
1/1
1/1
0/1
33/33
Gong,[24] 2010
[25]
0/0
0/2
0/1
0/0
0/1
0/0
2/0
1/1
2/0
1/1
34/31
Zeng and Chen,[23]
2009
0/1
1/0
0/0
0/0
0/1
0/0
0/0
0/0
2/2
0/0
0/0
23/23
Dong et al.,[22] 2008
0/0
0/0
0/0
0/0
0/0
0/2
0/0
0/0
1/4
2/0
4/0
38/30
Chen,[21] 2008
0/2
Rash
Fatigue
Weight loss
(TPM/CBZ) (TPM/CBZ) (TPM/CBZ)
Leukopenia
(TPM/CBZ)
Nystagmus
(TPM/CBZ)
Ataxia
Confusion
Xerostomia
(TPM/CBZ) (TPM/CBZ) (TPM/CBZ)
No. in group Dizziness
Nausea
Somnolence
(TPM/CBZ) (TPM/CBZ) (TPM/CBZ) (TPM/CBZ)
Study, year
Table III. General information and meta-analysis results of adverse events reported in randomized controlled trials comparing topiramate (TPM) with carbamazepine (CBZ) in the
treatment of classical trigeminal neuralgia
854
All of the trials had a high risk of bias. None of
the trials estimated the appropriate sample size,
and smaller samples are more likely to suffer from
selection bias. Detailed information with respect
to sex, age, characteristics of pain and duration
or severity of clinical status was not presented in
most trials. Although randomization was mentioned, details of the randomization methods
were not clearly described in most trials. Blinding
method, allocation concealment, follow-up or
dropouts were not reported in any of the trials.
Details on how outcomes were measured were
not given in most trials. As described in the six
trials, the outcome assessments were conducted
at the end of treatment. However, the outcome
should be measured over a period of time rather
than at one timepoint. Sometimes pain relief can
occur for a short period of time but cannot be
maintained long term, so positive results might
have been obtained by chance in these trials. Moreover, all of the trials included were conducted in
China where most studies performed are reported
as positive.[30] Although all of the studies had positive results, it is likely that the effects were overestimated due to the low quality of these trials.
We found that there were very few studies to
compare topiramate with carbamazepine in the
treatment of classical trigeminal neuralgia. Although great efforts were made to seek out all
relevant studies, we could only find eligible randomized controlled trials published in the Chinese
language. Is topiramate known to be ineffective
or less effective than carbamazepine in the treatment of classical trigeminal neuralgia? We did not
find evidence to support this hypothesis within the
published literature. The Chinese studies might
indeed be inadequately designed and the effects
of topiramate might be exaggerated, but could all
six trials make the same mistake and yield similar
results? Or are there any known differences in response to topiramate or carbamazepine between
Chinese and non-Chinese populations? We performed a literature search in order to clarify this,
but satisfying answers were not found. Zhao et al.[31]
studied the pharmacokinetic characteristics of
topiramate in Chinese volunteers and compared
the results with Western studies. They found that
Chinese volunteers achieved a faster time-to-peak
CNS Drugs 2011; 25 (10)
Topiramate vs Carbamazepine for Classical Trigeminal Neuralgia
Study, year
855
Topiramate Carbamazepine
Risk ratio
events total events total Weight M-H, fixed, 95% CI
Chen,[21] 2008
38
30 35.6%
0.20 [0.02, 1.67]
Dong et al.,[22] 2008
23
23 15.9%
1.00 [0.15, 6.51]
Gong,[24] 2010
33
33
Li et al.,[25] 2010
33
33 15.9%
0.50 [0.05, 5.25]
Xia,[26] 2010
22
21 16.3%
0.48 [0.05, 4.88]
Zeng and Chen,[23] 2009 1
34
31
Total events
8.0% 1.00 [0.07, 15.33]
8.3% 0.91 [0.06, 13.96]
171 100.0%
183
Total (95% CI)
Risk ratio
M-H, fixed, 95% CI
0.54 [0.22, 1.33]
12
Heterogeneity: 2 = 1.62, df = 5 (p = 0.90); I 2 = 0%
Test for overall effect: Z = 1.34 (p = 0.18)
0.01
0.1
1
Favours
carbamazepine
10
Favours
topiramate
100
Fig. 4. Forest plot of the adverse event of dizziness reported for topiramate compared with carbamazepine. df = degrees of freedom;
M-H = Mantel-Haenszel test.
and higher peak serum topiramate concentrations. A longer plasma elimination half-life was
also found in Chinese compared with Western populations. However, this pharmacokinetic study
could not support such an important conclusion
that topiramate was more effective for classical
trigeminal neuralgia in Chinese than in Western
populations. Therefore, any differences in therapeutic response to topiramate or carbamazepine
between Chinese and non-Chinese populations
still need to be examined in high-quality trials.
Due to the adverse effect profile of carbamazepine, more effective and safer alternative drugs need
to be found to treat classical trigeminal neuralgia.
Our study found equally favourable effectiveness
and acceptable tolerability of topiramate compared with carbamazepine in the treatment of
classical trigeminal neuralgia. However, we could
not draw an affirmative conclusion due to the
poor methodological quality and localized population of the trials included. Therefore, this
study aimed at presenting the available results
and providing a reference point for future studies,
with the expectation that future large, international, well conducted, randomized controlled
trials will precisely assess the effectiveness of topiramate for classical trigeminal neuralgia.
There are some suggestions for future studies.
First, patients included in trials should be diagnosed according to strict criteria such as those of
2011 Adis Data Information BV. All rights reserved.
the IHCD. As trigeminal neuralgia is characterized by occasional attacks and remission phases
in its natural history, especially in its initial phases,
adequate selection of the clinical phase and detailed
records of the history are important. Second,
adequate randomization and allocation concealment methods should be used. Third, participants
and outcome assessors should be blinded with adequate methods. Furthermore, rigorous approaches
should be used in outcome measurement to make
sure the results are objective and authentic. As
pain is inherently difficult to measure because of
its subjective nature and the strong influence of
social context, emotion and other nonphysiological
variables,[32] an objective, authentic and standardized instrument for outcome measurement such
as the VAS, the multi-institutional Initiative on
Methods, Measurement, and Pain Assessment in
Clinical Trials (IMMPACT)[33] or the Brief Pain
Inventory-Facial[34] is obligatory. Moreover, an
intent-to-treat analysis should be applied to reduce the impact of dropouts or withdrawals.
Conclusions
Current trials comparing topiramate with carbamazepine are all poor in terms of methodological quality. The meta-analysis of these studies
showed that the overall effectiveness and tolerability of topiramate does not seem to differ from
CNS Drugs 2011; 25 (10)
Wang & Bai
856
carbamazepine in the treatment of classical trigeminal neuralgia. However, the meta-analysis
yielded a favourable effect of topiramate compared
with carbamazepine after a treatment duration of
2 months. Results are limited by the poor methodological quality and localized population of
the trials included. Therefore, large, international,
well conducted, randomized controlled trials are
needed to further assess the relative efficacy and
tolerability of topiramate and carbamazepine in
this indication.
Acknowledgements
We thank Dr Ding Lei for providing valuable advice for
this article. We also thank all staff members of the Cochrane
Collaboration for providing Cochrane methodology and the
Cochrane RevMan 5.1 programme that was used in this article. No sources of funding were used to prepare this study. All
authors agree with the opinions and conclusions expressed in
this manuscript and have no conflicts of interest.
References
1. Merskey H, Bogduk N. Classification of chronic pain: descriptions of chronic pain syndromes and definitions of
pain terms. Seattle (WA): IASP Press, 1994: 59-71
2. Katusic S, Williams DB, Beard CM, et al. Epidemiology and
clinical features of idiopathic trigeminal neuralgia and
glossopharyngeal neuralgia: similarities and differences,
Rochester, Minnesota, 1945-1984. Neuroepidemiology
1991; 10: 276-81
3. Headache Classification Subcommittee of the International
Headache Society. The International Classification of Headache Disorders. 2nd ed. Cephalalgia 2004; 24 Suppl. 1: 9-160
4. Cruccu G, Gronseth G, Alksne J, et al. AAN-EFNS guidelines on trigeminal neuralgia management. Eur J Neurol
2008; 15: 1013-28
5. Zakrzewska JM, McMillan R. Trigeminal neuralgia: the
diagnosis and management of this excruciating and poorly
understood facial pain. Postgrad Med J 2011; 87: 410-6
6. Zakrzewska JM. Assessment and treatment of trigeminal
neuralgia. Br J Hosp Med 2010; 71 (9): 490-4
7. Rockcliff BW, Davis EH. Controlled sequential trials of
carbamazepine in trigeminal neuralgia. Arch Neurol 1996;
15: 129-36
8. Attal N, Cruccu G, Haanpaa M, et al. EFNS guidelines on
pharmacological treatment of neuropathic pain. Eur J
Neurol 2006; 13 (11): 1153-69
9. Gronseth G, Cruccu G, Alksne J, et al. Practice parameter:
the diagnostic evaluation and treatment of trigeminal
neuralgia (an evidence-based review): report of the Quality
Standards Subcommittee of the American Academy of
Neurology and the European Federation of Neurological
Societies. Neurology 2008; 71 (15): 1183-90
10. Sindrup SH, Jensen TS. Pharmacotherapy of trigeminal
neuralgia. Clin J Pain 2002; 18 (1): 22-7
2011 Adis Data Information BV. All rights reserved.
11. Jorns TP, Zakrzewska JM. Evidence-based approach to the
medical management of trigeminal neuralgia. Br J Neurosurg 2007; 21 (3): 253-61
12. Maryanoff BE. Pharmaceutical gold from neurostabilizing agents: topiramate and successor molecules. J Med
Chem 2009; 52: 3431-40
13. Tucker P, Trautman RP, Wyatt DB, et al. Efficacy and
safety of topiramate monotherapy in civilian posttraumatic
stress disorder: a randomized, double-blind, placebo controlled study. J Clin Psychiatry 2007; 68: 201-6
14. van Passel L, Arif H, Hirsch L, et al. Topiramate for the
treatment of epilepsy and other nervous system disorders.
Expert Rev Neurother 2006; 6: 19-31
15. Johnson BA, Capece JA, Wiegand F, et al. Topiramate for
treating alcohol dependence: a randomized controlled trial.
JAMA 2007; 298: 1641-51
16. Zvartau-Hind M, Din MU, Gilani A, et al. Topiramate relieves refractory trigeminal neuralgia in MS patients.
Neurology 2000; 55: 1587-8
17. Weintraub D, Buchsbaum R, Spencer HT, et al. Cognitive
side effects from the Columbia anti-epileptic drug database
[abstract]. Neurology 2004; 63 Suppl. 5: A311
18. Domingues RB, Kuster GW, Aquino CC. Treatment of
trigeminal neuralgia with low doses of topiramate. Arq
Neuropsiquiatr 2007; 65 (3B): 792-4
19. Solaro C, Uccelli MM, Brichetto G, et al. Topiramate relieves idiopathic and symptomatic trigeminal neuralgia.
J Pain Symptom Manage 2001; 21 (5): 367-8
20. Gilron I, Booher SL, Rowan JS, et al. Topiramate in trigeminal neuralgia: a randomized, placebo-controlled multiple crossover pilot study. Clin Neuropharmacol 2001; 24 (2):
109-12
21. Chen JB. Effectiveness of topiramate in the treatment of
primary trigeminal neuralgia. J Pract Med 2008; 24 (21):
3738-9
22. Dong BN, Yuan YL, Zhao HH, et al. Observation on effectiveness and safety of topiramate in the treatment of
primary trigeminal neuralgia. Chin J Diffic Compl Cas
2008; 7 (11): 680-1
23. Zeng XJ, Chen QT. Clinical observation on effectiveness of
topiramate in the treatment of primary trigeminal neuralgia. Guang Dong Med 2009; 30 (4): 631-2
24. Gong JJ. A randomized controlled trial of 3 drugs in the
treatment of primary trigeminal neuralgia. J Trad Chinese
Med 2010; 2 (12): 74
25. Li MQ, Huang XY, Zhu CL, et al. Topiramate and carbamazepine in the treatment of primary trigeminal neuralgia:
a randomized controlled trial. China Mod Med 2010; 17 (2):
52-3
26. Xia YJ. Observation on efficacy of topiramate in the treatment of primary trigeminal neuralgia. Prim Med Care
Forum 2010; 14 (3): 241-2
27. Spacek A, Hanl G, Groiss O, et al. Acupuncture and ganglionic local opioid analgesia in trigeminal neuralgia. Wien
Med Wochenschr1998; 148 (19): 447-9
28. Zheng F, Deng F. Therapeutics of pain [M]. Shanghai:
Shanghai Science and Technology Press, 1996: 55-8
29. Higgins JPT, Altman DG, Sterne JAC. Assessing risk of bias
in included studies. In: Higgins JPT, Green S, editors. West
CNS Drugs 2011; 25 (10)
Topiramate vs Carbamazepine for Classical Trigeminal Neuralgia
30.
31.
32.
33.
Sussex: Cochrane Handbook for Systematic Reviews of
Interventions, 2011 Mar
Vickers A, Goyal N, Harland R, et al. Do certain countries
produce only positive results? A systematic review of controlled trials. Control Clin Trials 1998; 19: 159-66
Zhao RS, Huang J, Yang L, et al. Pharmacokinetics and
bioequivalence of topiramate tablets in healthy volunteers.
Chin J Clin Pharmacol 2005; 21 (6): 441-4
Chen HI, Lee JY. The measurement of pain in patients with
trigeminal neuralgia. Clin Neurosurg 2010; 57: 129-33
Dworkin RH, Turk DC, Wyrwich KW, et al. Interpreting
the clinical importance of treatment outcomes in chronic
2011 Adis Data Information BV. All rights reserved.
857
pain clinical trials: IMMPACT recommendations. J Pain
2008; 9 (2): 105-21
34. Lee JY, Chen HI, Urban C, et al. Development of and psychometric testing for the Brief Pain Inventory-Facial in patients
with facial pain syndromes. J Neurosurg 2010; 113 (3): 516-23
Correspondence: Dr Qiang-ping Wang, Department of
Neurosurgery, Dujiangyan Peoples Hospital, Dujiangyan
Medical Center, Baolian street no.1, Dujiangyan 611830,
China.
E-mail: 187317846@qq.com
CNS Drugs 2011; 25 (10)
Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.
Vous aimerez peut-être aussi
- Critical Appraisal of A CaseDocument2 pagesCritical Appraisal of A Casemarhayudi15Pas encore d'évaluation
- Critical Apraisal CitaDocument4 pagesCritical Apraisal Citamarhayudi15Pas encore d'évaluation
- Coass III EsophagologyDocument26 pagesCoass III Esophagologymarhayudi15Pas encore d'évaluation
- Jurnal Mata 1Document9 pagesJurnal Mata 1marhayudi15Pas encore d'évaluation
- Jurnal 4nDocument4 pagesJurnal 4nmarhayudi15Pas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Q3-Las-Health10-Module 3-Weeks 6-8Document6 pagesQ3-Las-Health10-Module 3-Weeks 6-8MA TEODORA CABEZADAPas encore d'évaluation
- Starlight ProgramsDocument12 pagesStarlight Programsllacara@nncogannett.comPas encore d'évaluation
- Physical Education Essential Learning Out Comes and Learning TargetsDocument8 pagesPhysical Education Essential Learning Out Comes and Learning TargetsJessa May RapadasPas encore d'évaluation
- About The Heart and Blood Vessels Anatomy and Function of The Heart ValvesDocument4 pagesAbout The Heart and Blood Vessels Anatomy and Function of The Heart ValvesdomlhynPas encore d'évaluation
- Pengaruh Pijat Bayi Terhadap Frekuensi Dan Durasi Menyusu BayiDocument11 pagesPengaruh Pijat Bayi Terhadap Frekuensi Dan Durasi Menyusu BayiIzmi NasutionPas encore d'évaluation
- Soy Estrogen Myth False - DR Mercola Caught by Federal Authorities Spreading False Health Info - (Soy Found Not To Contain Estrogen, Soy Does Not Lower Men's Testosterone, Fraudulent Claims)Document10 pagesSoy Estrogen Myth False - DR Mercola Caught by Federal Authorities Spreading False Health Info - (Soy Found Not To Contain Estrogen, Soy Does Not Lower Men's Testosterone, Fraudulent Claims)FRAUDWATCHCOMMISSIONPas encore d'évaluation
- (Handbook) Exchanges ProfileDocument20 pages(Handbook) Exchanges ProfileHouda MahfoudiPas encore d'évaluation
- Clinico-Pathological Conference: Presented by The Department of Internal MedicineDocument3 pagesClinico-Pathological Conference: Presented by The Department of Internal MedicineCloudy ClaudPas encore d'évaluation
- 5.3.1 Distinguish Between Learning and Performance: Skill in SportDocument48 pages5.3.1 Distinguish Between Learning and Performance: Skill in SportAiham AltayehPas encore d'évaluation
- Platelet Analysis - An Overview: HistoryDocument7 pagesPlatelet Analysis - An Overview: HistoryPieter Du Toit-EnslinPas encore d'évaluation
- 16 MSDS NaHSO3Document6 pages16 MSDS NaHSO3Furqan SiddiquiPas encore d'évaluation
- Redfern Mianscum LetterDocument6 pagesRedfern Mianscum LettermediaindigenaPas encore d'évaluation
- Chapter 1Document62 pagesChapter 1Ashenafi PaulosPas encore d'évaluation
- Project ProposalDocument3 pagesProject ProposalSkrrtt SkrrttPas encore d'évaluation
- Development and in Vitro-In Vivo Evaluation of Gastro Retentive Drug Delivery of Nizatidine Using Natural and Semi - Synthetic PolymersDocument17 pagesDevelopment and in Vitro-In Vivo Evaluation of Gastro Retentive Drug Delivery of Nizatidine Using Natural and Semi - Synthetic PolymersShyamlaPas encore d'évaluation
- National Programme For Prevention and Control of FluorosisDocument49 pagesNational Programme For Prevention and Control of FluorosisveereshPas encore d'évaluation
- Deborah Falla The Role of Motor Learning and Neuroplasticity in Designing RehabilitationDocument5 pagesDeborah Falla The Role of Motor Learning and Neuroplasticity in Designing RehabilitationDago Angel Prieto PalavecinoPas encore d'évaluation
- Centrifugal ChillerDocument24 pagesCentrifugal ChillerARUL SANKARANPas encore d'évaluation
- 1PE 4 Q3 Answer Sheet March 2024Document3 pages1PE 4 Q3 Answer Sheet March 2024Chid CabanesasPas encore d'évaluation
- Coca Cola Fairlife CaseDocument4 pagesCoca Cola Fairlife Caseapi-315994561Pas encore d'évaluation
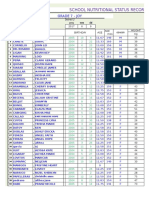
- School Nutritional Status Record: Grade 7 - JoyDocument4 pagesSchool Nutritional Status Record: Grade 7 - JoySidPas encore d'évaluation
- Public Opinion On Idea of Digitalising Rural CommunityDocument11 pagesPublic Opinion On Idea of Digitalising Rural CommunityINSTITUTE OF LEGAL EDUCATIONPas encore d'évaluation
- PHIL 125: Practical Logic: University of Alberta Sam Hillier, Fall 2013Document12 pagesPHIL 125: Practical Logic: University of Alberta Sam Hillier, Fall 2013Harry WeiPas encore d'évaluation
- Stages of LaborDocument3 pagesStages of Laborkatzuhmee leePas encore d'évaluation
- Psychiatric Disability AssessmentDocument19 pagesPsychiatric Disability AssessmentDivya ThomasPas encore d'évaluation
- Social Science Class 10 Understanding Economic DevelopmentDocument93 pagesSocial Science Class 10 Understanding Economic DevelopmentkannansesPas encore d'évaluation
- Resume 3Document2 pagesResume 3api-458753728Pas encore d'évaluation
- Republic of The Philippines Davao Oriental State College of Science and TechnologyDocument4 pagesRepublic of The Philippines Davao Oriental State College of Science and Technologydinheadnursing09Pas encore d'évaluation
- Branksome Hall Asia Code of ConductDocument9 pagesBranksome Hall Asia Code of Conductapi-246218373Pas encore d'évaluation
- Normal GFR in ChildDocument8 pagesNormal GFR in ChildbobbypambudimdPas encore d'évaluation