Académique Documents
Professionnel Documents
Culture Documents
Congenital Heart Disease in Infant PDF
Transféré par
Legina AromatikaTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Congenital Heart Disease in Infant PDF
Transféré par
Legina AromatikaDroits d'auteur :
Formats disponibles
Sandeep V.
Harshangi et al: Clinical study of congenital heart disease in infants
Journal of Pharmaceutical and Scientific Innovation
www.jpsionline.com
Research Article
CLINICAL STUDY OF CONGENITAL HEART DISEASE IN INFANTS IN TERTIARY CARE HOSPITAL
Sandeep V.Harshangi*1, Laxmi Nagaraj Itagi2, Venkatesh Patil3, Vijayanath.V4
1
Assistant Professor, Department of Pediatrics, M.R. Medical College, Gulbarga, Karnataka, India
2
Assistant Professor, Department of obstetrics & Gynecology, M.R. Medical College, Gulbarga, Karnataka, India
3
Associate professor, Department of Pharmacology, Navodaya Medical College, Raichur, Karnataka, India
4
Associate Professor, Department of Forensic Medicine & Toxicology, VMKV Medical College, Salem, Tamil Nadu, India
Received on: 08/01/13 Revised on: 05/02/13 Accepted on: 12/02/13
ABSTRACT
Congenital heart disease are primarily disease of neonates, infants and children. The burden of CHD in India is likely to be enormous due to very high birth
rate. The reported incidence is 8-10/ 1000 live births. Objective was to know the pattern of clinical presentation of various congenital heart disease in 0-1 year
age group. To study the different form of cyanotic and acyanotic congenital heart disease in present cases. 50 cases of CHD proven by 2D echocardiography
were studied for 2 years period. Present study included all infants in birth one year age group and excluded all preterm babies and patient with persistent
pulmonary hypertension. Out of the 50 cases of congenital heart disease, 34 were acyanotic CHD and 16 cases of cyanotic CHD. VSD (30%) was the
commonest acyanotic CHD while TOF (12%) was the commonest among cyanotic group. Growth retardation and CCF were the commonest complication. The
mortality rate was 18% with VSD as the leading cause of death among the CHD. The commonest cause of death among these patients was refractory CCF.
Most common CHD was acyanotic group with VSD being the commonest and among cyanotic the most common was TOF. A high index of suspicion,
detailed history, physical, cardiovascular and other systemic examination, chest X-ray and electrocardiogram along with the use of 2D echocardiography helps
us diagnose most of the cases of CHD. Children having murmurs should be screened unless thought to be physiological. A cardiac evaluation with
echocardiography is also necessary in all cases of LRTI and FTT. Early diagnosis, close monitoring and timely intervention in cases of CHD will go a long
way in reducing the morbidity and mortality to a large extent.
Keywords: Congenital heart disease; 2D echocardiography
INTRODUCTION
Congenital Heart Diseases (CHD) are primarily seen in
neonates, infants and children, although in our country it is
not uncommon to see adults with uncorrected CHD. The
burden of congenital heart disease in India is likely to be
enormous due to a very high birth rate. This heavy burden
emphasizes the importance of this group of heart diseases.
The reported incidence of CHD are 8-10/1000 live births
according to various studies from different parts of the
world.1 It is believed that this incidence has remained
constant worldwide.2
Nearly one-third of these CHD are critical requiring
intervention in the first year of life itself.3 Rapid advances
have taken place in the diagnosis and treatment of CHD over
the last six decades. There are diagnostic tools available
today by which an accurate diagnosis of CHD can be made
even before birth. With currently available treatment
modalities, over 75% of infants born with congenital heart
disease can survive beyond the first year of life and many can
lead normal lives thereafter. However, this privilege of early
diagnosis and timely management is restricted to children in
developed countries only. Unfortunately majority of children
born in developing countries with CHD do not get the
necessary care, leading to high morbidity and mortality.
There is no community based data for the incidence of
congenital heart disease at birth in India. Since a large
number of births in our country take place at home, mostly
unsupervised by a qualified doctor, hospital statistics are
unlikely be truly representative. The congenital heart disease
has been the subject of innumerable studies both regarding
prevalence and clinical features in western countries. The
few studies carried out in India were either community or
school based and they did not indicate the clinical profile of
CHD. It was therefore decided to carry out hospital based
study of clinical profile of congenital heart disease in infancy
at Basaveshwar Teaching & General Hospital and
Sangameshwar Teaching Hospital attached to M.R. Medical
College, Gulbarga.
OBJECTIVES
To know the pattern of clinical presentation of various
congenital heart disease in 0-1 year age group.
To study the different form of cyanotic and acyanotic
congenital heart disease in present cases.
METHODOLOGY
Methods of collection of data:
Infants presenting with features suggestive of congenital
heart disease and proven by 2D echocardiography were
studied over a period of 2 years from October 2005 to
September 2007 admitted in Sangameshwar Hospital,
Gulbarga and Basaveshwar Teaching & General Hospital,
Gulbarga. Study was carried out as per Institutional Ethical
committee clearance number: MRMC/ IEC/ 19/2005.
Inclusion Criteria:
All patients presenting with clinical features like
breathlessness, recurrent LRTI, failure to thrive, cyanotic
spells, congestive cardiac failure, murmur in the age group of
term neonates to first birthday.
Exclusion Criteria:
Preterm neonates.
More than one year.
Patients with persistent pulmonary hypertension.
RESULTS.
To study the different form of cyanotic and acyanotic
congenital heart disease in present cases.
JPSI 2 (1), Jan Feb 2013, 15-18
Sandeep V.Harshangi et al: Clinical study of congenital heart disease in infants
LRTI (60%), FTT (40%) cyanosis (26%, Fever (24%) and
6% were asymptomatic.
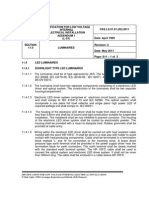
Table-1: Symptomatology of Various CHD
Symptomatology
No. of cases
Percent
Breathlessness
39
78.00
LRTI
30
60.00
FTT
20
40.00
Cyanosis
13
26.00
Fever
12
24.00
Asymptomatic
3
6.00
Signs GPE
Tachypnea
Tachycardia
Cyanosis
Fever
Edema
In the present study, when symptoms were taken into
consideration. It was found that breathlessness was the
commonest symptom seen in 39 cases (78%) followed by
Cardiac
lesion
Acyanotic
VSD
ASD
PDA
AVSD
Dextro
cardia
HOCM
COA
Cyanotic
TOF
TGV
TAPVC
Ebstein
DORV
Dextro
cardia with
pulmonary
atresia with
PDA
Dextro
cardia with
tricuspid
atresia with
ASD
Total
Cardiac size
Normal
Enlarged
Table-2: Signs of CHD
No. of cases
44
38
13
12
9
Percent
88.00
76.00
26.00
24.00
18.00
Commonest sign on general examination were tachypnea
(88%) and tachycardia in 76% followed by cyanosis in 26%
and fever in 24% of cases.
Table-3: X-Ray and ECG Findings and Murmur on Auscultation
Pulmonary vascularity
ECG
Increased
Decreased
Normal
Normal
LVH
RVH
BVH
PSM
Murmur
ESM
CM
Normal
15
8
5
2
2
-5
1
1
2
15
3
4
1
--
14
4
3
---
------
1
4
2
2
2
----2
2
-----
7
7
4
1
--
6
1
1
1
--
12
--1
--
3
8
-1
--
--5
---
----2
1
1
---
1
--
---
-1
1
--
-1
---
---
1
1
---
1
1
---
---
6
3
2
2
1
1
-1
2
----
-2
-2
1
1
-3
1
-1
--
6
----1
--1
2
---
---2
---
-----1
5
1
2
----
1
2
--1
--
-2
-----
6
1
2
2
1
1
-------
-------
--
--
--
--
--
--
--
--
--
Table-4: Associated Anomalies with CHD
Associated anomalies
No. of cases (n=12)
Percent
1. Musculoskeletal system
7
58.33
3
42.8
CTEV
Polydactyly
3
42.8
1
14.28
Webbed neck
2. Down syndrome
5
41.66
In the present study, associated anomalies were encountered
in 12 out of 50 patients with musculoskeletal system being
the commonest with 58.33% followed by Down syndrome
with 41.66%. Among the musculoskeletal system, the most
common were CTEV and polydactyly with 42.85% each and
one case of webbed neck.
Table-5: Complications of CHD
Complications
No. of cases
Percent
Growth retardation
28
56.00
CCF
28
56.00
11
22.00
Bronchopneumonia
Cyanotic Spell
3
6.00
Systemic Hypertension
1
2.00
No complications
7
14.00
In the present study, both growth retardation and CCF were
the commonest complication with 56% patient and next
common was bronchopneumonia with 22%.
Mortality in CHD:
Mortality rate was 18% (9 cases).
Table-6: Mortality in CHD
Cause of death
No. of cases
6
Refractory CCF
Complex CHD
2
Septicemia with infective endocarditis
1
Percent
66.6
22.2
11.1
Out of 50 patients, 9 patients expired giving a mortality rate
of 18%. Of all refractory CCF contributed the major cause of
death in about 66.66% cases followed by complex CHD with
22.22% of cases and only one patient (11.11%) expired
because of infective endocarditis with septicemia.
Symptoms:
In the present study, when symptoms were taken into
consideration, we found breathlessness to be commonest
symptom seen in 39 cases (78%) followed by LRTI (60%),
FTT (40%). Fever (24%). Present study showed similar
observation as shown by Tank S et al4 2004 and by other
Indian studies. Breathlessness was the commonest symptom
in both cyanotic and acyanotic CHD. LRTI and FTT were
maximally seen with VSD and these patients had large
defects. LRTI was also seen in ASD and PDA. FTT was seen
in 7 out of 15 cases of VSD, 4 of 8 cases of ASD, 3 out of 5
cases of PDA, 4 out of 6 cases of TOF, 1 out of 3 cases of
TGV. FTT is a major symptom of CHD, the reason being low
JPSI 2 (1), Jan Feb 2013, 15-18
Sandeep V.Harshangi et al: Clinical study of congenital heart disease in infants
energy intake, inadequate food intake, and malabsorption or
feeding difficulty. Tank S et al4 2004 reported 45%, while
Keith et al5 reported 35% of cyanotic spell.This was higher
than the incidence of cyanotic spell seen in the present study.
13 cases gave history of cyanosis and this was seen
commonly with TOF with all 6 patients giving history of
cyanosis and 3 patients had cyanotic spell. 26% cases of
CHD had cyanosis which were more common in cyanotic
CHD. 3 cases (6%) were asymptomatic and were picked up
on OPD basis.
Signs
Kasturi et al6 1999 reported among 108 cases of CHD, 63
(58%) were asymptomatic and 45 (42%) were symptomatic.
Common signs and symptoms were feeding difficulty,
cyanosis, tachypnoea, tachycardia, intercostals retraction and
CCF. Present study showed similar observation among the
signs. In a study by Linde ML et al7 1967 reported growth
retardation was present in children with acyanotic CHD but
was more pronounced in the cyanotic children. In the
acyanotic group, growth retardation was most prominent in
those with VSD. Present study reported 9 out of 15 cases of
VSD and 4 out of 6 cases of TOF had growth retardation.
This was in agreement with above study. In the present study
on general examination, we observed tachypnoea was the
commonest sign seen in 88% of cases, 76% of cases had
tachycardia, followed by cyanosis seen in 26% cases and
fever in 24% cases and dependent edema in 18% cases.
Tachypnoea and tachycardia were commonly found in VSD,
ASD and PDA i.e. left right shunt type of CHD. Cyanosis
were reported as commonest sign in cyanotic CHD patients.
X-Ray, ECG, Auscultatory Findings:
The finding of x-ray chest revealed cardiomegaly in 70.58%
patient of acyanotic CHD, of which VSD constituted 44.11%
followed by PDA with 11.76% and ASD(8.82%). Among
cyanotic CHD cardiomegaly was seen in 43.75% with 2
patients each of TGV and ebstein anomaly (12.5%).
Pulmonary plethora was seen in 21 patient (61.76%) of
acyanotic CHD with VSD accounting for 14 patients
(41.17%) followed by ASD with 4 patients (11.76%) and 3
patients of PDA (8.82%). Plethora was also seen in 5 patients
of cyanotic CHD (31.25%) with TGV with 3 patients
(18.75%). Pulmonary oligemia was seen in 7 patients
(43.75%) of cyanotic CHD with TOF accounting for 6
patients (37.5%) out of the 7 patients. Normal lung field was
visualized in 13 patients (38.23%) of acyanotic group and 4
patients (25%) of cyanotic group. Study done by Chadha et
al8 2001 showed normal ecg in 40% patients with important
ECG abnormalities being right ventricular dominance.
Present study also was in accordance with this study. On
looking at ECG, RVH was seen in 56% of cases while 28%
showed biventricular hypertrophy and 8% showing LVH or
normal ECG. On auscultation we found out PSM in 15
patients(30%) with VSD alone accounting for 12 patients
(80%). ESM was auscultated in 28 patients (56%) with ASD
accounting for 8 patients(28.57%) and TOF with 6
patients(21.42%) being the commonest. Continous murmur
was auscultated in 5 patients (10%) with all cases of PDA.
No murmur was heard in 2 cases (4%) of dextrocardia.
Extra Cardiac Associated Anomalies:
Khalil et al9 1994 reported an incidence of 17.9% of somatic
anomalies with down syndrome being the commonest seen in
9.3% of cases. Present study reported 10 % incidence of
down syndrome. Similar observation were reported by Kinare
et al10 1987. In the present study we found the incidence of
extra cardiac anomalies to be 24% (12 patient).
Musculoskeletal anomalies were the most frequent with 7
cases (58.33%). The musculoskeletal abnormalities
compromised of 3 cases (42.85%) of CTEV and polydactyly
and 1 case (14.28%) of webbed neck. Present study also
showed association of 5 cases (41.66%) of down syndrome.
Complication
Study by Rao VS et al11 1974, reported 72% with growth
retardation. Study by Jain et al12 1971 reported CCF as the
commonest complication. The present study shows 56%
patients with growth failure and CCF as the commonest
followed by 22% with bronchopneumonia, and 6% with
cyanotic spell and 2% with hypertension. The present study is
in concordance with the above study.
Mortality
Tank S et al4 2004 was reported overall 19.73% mortality
which was higher in CCHD, the causes being subacute
bacterial endocartitis, refractory failure, arrhythmias, sepsis
and complex congenital cyanotic heart disease. Mortality is
known to be higher in CHD. Observation in the present study
was mortality rate of 18% (9 case). Out of the 9 cases, 5 cases
of VSD, 2 complex CHD, 1 each of PDA and DORV. The
most common cause of death was refractory CCF accounting
for 66.66% and 22.22% mortality was because of complex
CHD per se. 11.11% case expired because of septicemia with
infective endocarditis. In the present study, refractory CCF
was the most commonest cause of death, which was not in
concordance with the above study, probably because of the
age group involved in the study.
CONCLUSION
Out of the 50 proven cases of congenital heart disease studied
from October 2005 to September 2007, the highest incidence
was noted in 1 month to 1 year age group. Out of the 50 cases
of congenital heart disease, 34 were acyanotic CHD and 16
cases of cyanotic CHD. VSD (30%) was the commonest
acyanotic CHD while TOF (12%) was the commonest among
cyanotic group
Breathlessness, LRTI, FTT, fever, tachypnea, tachycardia,
cyanosis were the common clinical presentation of majority
of cases. Male preponderance was noted in both cyanotic and
acyanotic CHD. These children were deprived of basic
medical care in the form of immunization. In our study 40%
reported complete immunization while 18% were partial
immunized and 42% were unimmunised.
Malnutrition was seen in 82% having less than 50th percentile
anthropometric data.Musculoskeletal anomalies were
commonest extra cardiac anomaly with Down syndrome the
next most common. Growth retardation and CCF were the
commonest complication. The mortality rate was 18% with
VSD as the leading cause of death among the CHD. The
commonest cause of death among these patients was
refractory CCF. All cases of CHD needs regular monitoring
and follow up so as to permit optimal growth and
development.
A high index of suspicion, detailed history, physical,
cardiovascular and other systemic examination, chest X-ray
and electrocardiogram along with the use of 2D
echocardiography helps us diagnose most of the cases of
CHD. Children having murmurs should be screened unless
thought to be physiological. A cardiac evaluation with
echocardiography is also necessary in all cases of LRTI and
FTT.
Early diagnosis, close monitoring and timely
JPSI 2 (1), Jan Feb 2013, 15-18
Sandeep V.Harshangi et al: Clinical study of congenital heart disease in infants
intervention in cases of CHD will go a long way in reducing
the morbidity and mortality to a large extent.
REFERENCES
1. Fyler DC, Buckley LP, Hellenbrand WE, Cohn HE. Report of the New
England Regional Infant Care program. Pediatrics. 1980; 65: Suppl:
375-461.
2. Abdullah R. What is the prevalence of congenital heart disease. Ped
Cardio. 1997; 18: 268.
3. Hoffman JI, Kaplan S. The incidence of congenital heart disease. J Am
Cardiol. 2002; 39: 1980-1900.
4. Tank S, Sushma M, Surekha J. Epidemiology of congenital heart
disease among hospitalized patients. www.bhj.org/ journal/ 2004 4602
april.html. epidemiol.
5. Keith JD, Rowe RD, Vlad P. Heart disease in infancy and childhood. 3rd
Edn., MacMillan NY, 1978; 365-40.
QUICK RESPONSE CODE
Kasturi L, Kulkarni AV, Amin A, Mashankar VA. Congenital heart
disease clinical spectrum. Indian J Pediatr. 1999; 36: 953.
7. Linde LM, Dunn OJ, Schireson R, Rasot B. Growth in children with
congenital heart diseasde. J Pediatr. 1967; 70: 413-419.
8. Chadha SL, Singh N, Shukla DK. Incidence of congenital heart disease.
Indian J Pediatr. 2001; 68: 507-510.
9. Khalil A, Aggarwal R, Thirupuram S, Arora R. Incidence of congenital
heart disease among hospital live births in India. Indian J Pediatr 1994;
31: 519-524.
10. Kinare SG, Sharma S. Congenital heart disease in first year of life (an
autopsy study of 270 cases). Indian J Pediatr. 1981; 48: 745-754.
11. Rao VS, Reddi YR. Profile of heart in children. Indian J Pediatr. 1974;
41: 244-248.
12. Jain KK, Sagar A, Beri S. Heart disease in children. Indian J Pediatr.
1971; 38: 441-48.
6.
ISSN (Online) : 2277 4572
Website
http://www.jpsionline.com
How to cite this article:
Sandeep V.Harshangi*, Laxmi Nagaraj Itagi, Venkatesh Patil, Vijayanath.V. Clinical study of congenital heart disease in infants in tertiary care hospital. J
Pharm Sci Innov. 2013; 2(1):15-18.
JPSI 2 (1), Jan Feb 2013, 15-18
Vous aimerez peut-être aussi
- Letter of Guarantee LPDP PDFDocument1 pageLetter of Guarantee LPDP PDFLegina AromatikaPas encore d'évaluation
- End of Study LetterDocument1 pageEnd of Study LetterLegina AromatikaPas encore d'évaluation
- Posttraumatic Epilepsy Among Epileptic Children Seen in A Pediatricneurology Clinic in Enugu Nigeriaa Descriptive Study Elj 1000105Document5 pagesPosttraumatic Epilepsy Among Epileptic Children Seen in A Pediatricneurology Clinic in Enugu Nigeriaa Descriptive Study Elj 1000105Legina AromatikaPas encore d'évaluation
- Ceem 14 029 PDFDocument11 pagesCeem 14 029 PDFLegina AromatikaPas encore d'évaluation
- Management of The Patient With Thermal Injuries PDFDocument15 pagesManagement of The Patient With Thermal Injuries PDFLegina AromatikaPas encore d'évaluation
- Sacralization and Herniated Nucleus Pulposus An Association Study 2165 7939 1000297Document7 pagesSacralization and Herniated Nucleus Pulposus An Association Study 2165 7939 1000297rosdaniaPas encore d'évaluation
- Jurnal Kulit 3Document8 pagesJurnal Kulit 3UmmulAklaPas encore d'évaluation
- Management of The Patient With Thermal Injuries PDFDocument15 pagesManagement of The Patient With Thermal Injuries PDFLegina AromatikaPas encore d'évaluation
- Evaluation and Management of Thermal Burns: Emergency Medicine Board Review ManualDocument11 pagesEvaluation and Management of Thermal Burns: Emergency Medicine Board Review ManualLegina AromatikaPas encore d'évaluation
- Termal InjuryyDocument6 pagesTermal InjuryyiswanlatifPas encore d'évaluation
- 9-Emergency MGMT of Burns - Peds Emerg Care 2005Document12 pages9-Emergency MGMT of Burns - Peds Emerg Care 2005Legina AromatikaPas encore d'évaluation
- Help Pedsurgeryafrica. 4Document4 pagesHelp Pedsurgeryafrica. 4Legina AromatikaPas encore d'évaluation
- C-Myc, Genome Instability, and Tumorigenesis PDFDocument35 pagesC-Myc, Genome Instability, and Tumorigenesis PDFLegina AromatikaPas encore d'évaluation
- 22-Urolithiasis. 3Document98 pages22-Urolithiasis. 3Legina AromatikaPas encore d'évaluation
- C-Myc, Genome Instability, and Tumorigenesis PDFDocument35 pagesC-Myc, Genome Instability, and Tumorigenesis PDFLegina AromatikaPas encore d'évaluation
- Bronchitis AkutDocument7 pagesBronchitis AkutLegina AromatikaPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Seismic Design Guide (2010)Document102 pagesSeismic Design Guide (2010)ingcarlosgonzalezPas encore d'évaluation
- Balzac and the Little Chinese Seamstress: A Journey During the Cultural RevolutionDocument4 pagesBalzac and the Little Chinese Seamstress: A Journey During the Cultural RevolutionRogona 123Pas encore d'évaluation
- The Power of Networking for Entrepreneurs and Founding TeamsDocument28 pagesThe Power of Networking for Entrepreneurs and Founding TeamsAngela FigueroaPas encore d'évaluation
- Ubc 2015 May Sharpe JillianDocument65 pagesUbc 2015 May Sharpe JillianherzogPas encore d'évaluation
- FAI - Assignment Sheet (Both Assignments)Document5 pagesFAI - Assignment Sheet (Both Assignments)Wilson WongPas encore d'évaluation
- 1 Starter WBDocument88 pages1 Starter WBHYOPas encore d'évaluation
- Valentine Gifting - Accessories EditionDocument25 pagesValentine Gifting - Accessories EditionPriyanath PaulPas encore d'évaluation
- The Golden HarvestDocument3 pagesThe Golden HarvestMark Angelo DiazPas encore d'évaluation
- July 4th G11 AssignmentDocument5 pagesJuly 4th G11 Assignmentmargo.nicole.schwartzPas encore d'évaluation
- Broom Manufacture Machine: StartDocument62 pagesBroom Manufacture Machine: StartHaziq PazliPas encore d'évaluation
- Cat IQ TestDocument3 pagesCat IQ TestBrendan Bowen100% (1)
- JKR Specs L-S1 Addendum No 1 LED Luminaires - May 2011Document3 pagesJKR Specs L-S1 Addendum No 1 LED Luminaires - May 2011Leong KmPas encore d'évaluation
- Independence Day Resurgence ScriptDocument60 pagesIndependence Day Resurgence ScriptdavidPas encore d'évaluation
- Explore Spanish Lesson Plan - AnimalsDocument8 pagesExplore Spanish Lesson Plan - Animalsapi-257582917Pas encore d'évaluation
- Timoshenko Beam TheoryDocument8 pagesTimoshenko Beam Theoryksheikh777Pas encore d'évaluation
- Pub - Perspectives On Global Cultures Issues in Cultural PDFDocument190 pagesPub - Perspectives On Global Cultures Issues in Cultural PDFCherlyn Jane Ventura TuliaoPas encore d'évaluation
- V60 Ventilator Specifications PDFDocument4 pagesV60 Ventilator Specifications PDFJonathan Issac Dominguez RamirezPas encore d'évaluation
- Antenatal AssessmentDocument9 pagesAntenatal Assessmentjyoti singhPas encore d'évaluation
- Assessing Student Learning OutcomesDocument20 pagesAssessing Student Learning Outcomesapi-619738021Pas encore d'évaluation
- Exploratory Data Analysis: M. SrinathDocument19 pagesExploratory Data Analysis: M. SrinathromaPas encore d'évaluation
- Liugong 938 Wheel Loader Parts ManualDocument20 pagesLiugong 938 Wheel Loader Parts Manualjonathan100% (49)
- Adjutant-Introuvable BASIC VERSIONDocument7 pagesAdjutant-Introuvable BASIC VERSIONfurrypdfPas encore d'évaluation
- TiONA 592 PDS - ENDocument1 pageTiONA 592 PDS - ENQuang VAPas encore d'évaluation
- Osprey, Men-At-Arms #008 The Black Watch (1971) (-) OCR 8.12Document48 pagesOsprey, Men-At-Arms #008 The Black Watch (1971) (-) OCR 8.12mancini100% (4)
- Project Cost ForecastDocument11 pagesProject Cost ForecastJames MendesPas encore d'évaluation
- Morpho Full Fix 2Document9 pagesMorpho Full Fix 2Dayu AnaPas encore d'évaluation
- Informed Consent: Ghaiath M. A. HusseinDocument26 pagesInformed Consent: Ghaiath M. A. HusseinDocAxi Maximo Jr AxibalPas encore d'évaluation
- OJT Form 03 Performance EvaluationDocument2 pagesOJT Form 03 Performance EvaluationResshille Ann T. SalleyPas encore d'évaluation
- Accounting Students' Attitude Towads AccountingDocument29 pagesAccounting Students' Attitude Towads AccountingSham Salonga Pascual50% (2)
- SFA160Document5 pagesSFA160scamalPas encore d'évaluation