Académique Documents
Professionnel Documents
Culture Documents
Phase II Trial of Temozolomide Plus O6-Benzylguanine in Adults With Recurrent, Temozolomide-Resistant Malignant Glioma
Transféré par
Mariano PerezCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Phase II Trial of Temozolomide Plus O6-Benzylguanine in Adults With Recurrent, Temozolomide-Resistant Malignant Glioma
Transféré par
Mariano PerezDroits d'auteur :
Formats disponibles
VOLUME
27
NUMBER
MARCH
10
2009
JOURNAL OF CLINICAL ONCOLOGY
O R I G I N A L
R E P O R T
Phase II Trial of Temozolomide Plus O6-Benzylguanine in
Adults With Recurrent, Temozolomide-Resistant
Malignant Glioma
Jennifer A. Quinn, Sara Xiaoyin Jiang, David A. Reardon, Annick Desjardins, James J. Vredenburgh,
Jeremy N. Rich, Sridharan Gururangan, Allan H. Friedman, Darell D. Bigner, John H. Sampson,
Roger E. McLendon, James E. Herndon II, Amy Walker, and Henry S. Friedman
From the Departments of Surgery,
Pathology, Biostatistics, and Bioinformatics, Duke University Medical
Center, Durham, NC.
Submitted June 26, 2008; accepted
October 31, 2008; published online
ahead of print at www.jco.org on
February 9, 2009.
Supported by National Institute of
Neurological Disorders and Stroke
Grant No. 5P50 NS20023-25, National
Institutes of Health (NIH) Specialized
Program of Research Excellence Grant
No. 5P50 CA 108786-4, NIH Merit
Award R37 CA 011898-38, and NIH
Grant No. 1 R21 CA 101298-01; S.X.J.
was supported by NIH Grant No. TL1
RR024126.
Authors disclosures of potential conflicts of interest and author contributions are found at the end of this
article.
Clinical Trials registry information available at www.jco.org
Corresponding author: Henry S.
Friedman, MD, Duke University Medical Center, PO Box 3624, Durham,
NC 27710; e-mail: fried003@mc
.duke.edu.
Patients and Methods
Patients were accrued into two independent strata on the basis of histology: glioblastoma
multiforme (GBM) and anaplastic glioma. Both temozolomide and O6-BG were administered on
day 1 of a 28-day treatment cycle. Patients were administered a 1-hour O6-BG infusion at a dose
of 120 mg/m2 followed immediately by a 48-hour infusion at a dose of 30 mg/m2/d. Temozolomide
was administered orally within 60 minutes of the end of the 1-hour O6-BG infusion at a dose of 472
mg/m2. The primary end point was objective response rate. Secondary end points included
progression-free survival, overall survival, and safety.
Results
Sixty-six of 67 patients who enrolled were treated with temozolomide and O6-BG. One of 34
patients (3%) with GBM (95% CI, 0.1% to 15%) and five of 32 assessable patients (16%) with
anaplastic glioma (95% CI, 5% to 33%) were responders. The most commonly reported adverse
events were grade 4 hematologic events experienced in 48% of the patients.
Conclusion
O6-BG when added to a 1-day dosing regimen of temozolomide was able to restore temozolomide
sensitivity in patients with temozolomide-resistant anaplastic glioma, but there seemed to be no
significant restoration of temozolomide sensitivity in patients with temozolomide-resistant GBM.
J Clin Oncol 27:1262-1267. 2009 by American Society of Clinical Oncology
INTRODUCTION
0732-183X/09/2708-1262/$20.00
1262
Purpose
This phase II trial was designed to define the role of O6-benzylguanine (O6-BG) in restoring
temozolomide sensitivity in patients with recurrent or progressive, temozolomide-resistant malignant
glioma and to evaluate the safety of administering O6-BG in combination with temozolomide.
2009 by American Society of Clinical Oncology
DOI: 10.1200/JCO.2008.18.8417
Despite recent advances in therapeutic regimens, the
diagnosis of malignant glioma still carries a poor
prognosis. Although alkylators such as temozolomide and polifeprosan 20 with carmustine implant
(Gliadel, Guilford Pharmaceuticals-MGI Pharma,
Bloomington, MN) are US Food and Drug Administrationapproved for treatment of malignant glioma, their ability to prolong survival is short-lived.
Thus, innovative therapeutic agents and strategies
are imperative.
One novel approach to fighting this deadly disease is to target the mechanisms of resistance to
chemotherapy. Because O6-alkylguanine-DNA alkyltransferase (AGT) has been shown to be a major
factor in the resistance of tumor cells to alkylating
2009 by American Society of Clinical Oncology
agents such as carmustine and temozolomide,1-3
perhaps targeting this DNA repair protein can help
restore chemotherapy activity.
One such agent that can irreversibly inactivate
AGT is a low molecular weight substrate, O6benzylguanine (O6-BG). In vitro1,4,5 and in vivo6,7
studies using tumor cell lines and subcutaneous
brain tumor xenografts demonstrate that
O6-BG increases the therapeutic effectiveness
of temozolomide.
These studies suggest that combining O6-BG
with temozolomide may circumvent resistance
and restore chemotherapy sensitivity. However,
before one can combine these two agents, one
must answer the following two important questions: what dosing schedule of O6-BG is necessary to
completely suppress AGT activity in brain tumors
TMZ and O6-BG in Malignant Glioma
for at least 48 hours, and what is the maximum-tolerated dose (MTD)
of temozolomide in a 1-day dosing regimen that can be combined
with O6-BG?
Prior research endeavors have answered both of these questions.
Weingart et al8 answered this first question in a phase I trial of polifeprosan 20 with carmustine implant plus continuous infusion of intravenous O6-BG in adults with recurrent malignant glioma by
establishing the dose of O6-BG to be 120 mg/m2 for 1 hour followed by
a continuous infusion of 30 mg/m2/d for 2 days. Quinn et al9 answered
the second question in a phase I trial of temozolomide plus O6-BG in
adults with recurrent malignant glioma by establishing the MTD of
temozolomide to be 472 mg/m2 when administered as a single dose in
conjunction with the above dosing schedule of O6-BG.
The objectives of this phase II trial were twofold: to define the
role of O6-BG in restoring temozolomide sensitivity in patients
with recurrent or progressive, temozolomide-resistant malignant
glioma and to evaluate the safety of administering O6-BG in combination with temozolomide.
PATIENTS AND METHODS
Patients
Eligible patients had a histologically confirmed diagnosis of progressive
or recurrent glioblastoma multiforme (GBM) or anaplastic glioma (anaplastic
astrocytoma [AA], anaplastic oligodendroglioma [AO], or anaplastic mixed
AA and AO). These tumors must have shown resistance to temozolomide,
defined as a 25% increase in tumor growth on contrast-enhanced magnetic
resonance imaging (MRI) or computed tomography (CT) within 8 weeks of
the last dose of temozolomide. Furthermore, all patients who experienced
treatment failure with temozolomide as their most recent treatment were
immediately enrolled onto the trial using temozolomide plus O6-BG. Patients
were 18 years old and required to have a Karnofsky performance score of
60%. An interval of at least 2 weeks since prior surgical resection (if conducted) or 4 weeks since prior chemotherapy (6 weeks for a nitrosourea-based
regimen) had to have elapsed for the patient to be enrolled onto the clinical
trial. All patients had evidence of residual tumor on postoperative MRI before
starting temozolomide plus O6-BG. Additional enrollment criteria included
adequate pretreatment bone marrow function (hematocrit 29%, total granulocyte count 1,500 cells/L, platelets 100,000 cells/L), renal function
(serum creatinine 1.5 mg/dL, serum urea nitrogen 25 mg/dL), and
hepatic function (serum AST and bilirubin 1.5 upper limit of normal).
For patients receiving corticosteroids, a stable dose for 1 week before entry
onto the study was required, if clinically possible, with no escalation of dose
above entry dose level. Patients of reproductive potential were required to take
effective contraceptive measures for the duration of the study. The following
patients were excluded from the study: pregnant women, potentially fertile
women or men who were not using effective contraception method, and
patients taking immunosuppressive agents other than corticosteroids. The
protocol was reviewed and approved by the Duke University Health System
institutional review board. Each patient signed an informed consent form.
Study Design and Treatment
This was a phase II, open-label, single-center trial with accrual goals
defined within two separate strata: GBM and anaplastic glioma (AA or AO).
Both temozolomide and O6-BG were administered on day 1 of a 28-day
treatment cycle. First, patients were treated with a 1-hour bolus infusion of
O6-BG at a dose of 120 mg/m2 followed immediately by a 48-hour continuous
infusion of O6-BG at a dose of 30 mg/m2/d. Next, temozolomide was administered orally, in a fasting state, at a dose of 472 mg/m2 within 60 minutes of the
end of the 1-hour administration of O6-BG infusion.
Temozolomide was commercially available from Schering-Plough Research Institute (Kenilworth, NJ). O6-BG was supplied by AOI Pharmaceuticals Inc (New York, NY).
www.jco.org
Prophylactic antiemetics were permitted as needed. Neurologic stability
was provided with the lowest corticosteroid dose when required. Colonystimulating factors were permitted only for rescue from grade 4 neutropenia.
Surveillance and Follow-Up
The baseline examination included central review of tumor tissue, MRI
(or CT if MRI was medically contraindicated), CBCs and blood chemistry
tests, and a physical examination including a comprehensive neurologic examination. During therapy, weekly CBCs were obtained. Before subsequent
cycles of chemotherapy, patients were required to repeat CBCs, blood chemistry tests, and a physical examination. In addition, after every two cycles of
chemotherapy, patients were required to obtain repeat neuroimaging.
Toxicity was graded according to the National Cancer Institute Common Toxicity Criteria version 2.0. Repeat cycles of chemotherapy were administered on schedule only if the patient met the following re-treatment criteria:
total granulocyte count 1,500 cells/L, platelets 100,000/L, hematocrit 29 g/dL, AST 2.5 upper limit of normal, creatinine 1.5 upper
limit of normal, and total bilirubin within normal limits; all other toxicities
must have resolved to baseline or grade 1. Temozolomide dose was reduced by
25% in any patient with grade 3 nonhematologic or grade 4 hematologic
toxicity or if re-treatment was delayed by longer than 2 weeks because of any
grade toxicity. Patients who were delayed 3 weeks from treatment were removed from the trial unless there was evidence of tumor response.
Objective assessments of overall response were based on tumor assessment from MRI scans (CT if MRI was medically contraindicated) interpreted
in the light of corticosteroid use, as suggested by Macdonald et al,10 with
appropriate support from the neurologic examination. This drug combination was administered for a maximum of 16 months or until unacceptable
toxicity or tumor progression occurred.
Statistical Analysis
The primary end point was objective response rate (ORR) defined as the
percentage of patients with complete response (CR) or partial response (PR)
according to the modified Macdonald criteria. The secondary end points were
safety, 6-month, and median progression-free survival (PFS), and 6-month
and median overall survival (OS).
On the basis of a two-stage Simon minimax design11 with an level of
10% and 90% power, 32 patients (18 patients in stage 1 of the study and an
additional 14 patients in stage 2) within each stratum were required to test the
null hypothesis that the true ORR was 5% versus the alternative hypothesis
that the true ORR was 20%. At least one objective response within each
stratum was needed in stage 1 to allow expansion of the trial to stage 2. At the
end of the study, at least four objective responses within each stratum were
needed to reject the null hypothesis.
Efficacy and safety analyses included all patients who received at least
one dose of temozolomide and O6-BG. The number and proportion of
patients who achieved an objective response (CR or PR) was summarized,
along with the corresponding exact two-sided 95% CI, calculated by a
method derived from the binomial distribution. PFS, defined as the time
between initiation of treatment and the first occurrence of disease progression, disease, or death, and OS, defined as the time between initiation of
treatment and death, were summarized by using the Kaplan-Meier method.12 Estimates for the median event time and 6-month rates were generated within the Kaplan-Meier framework.
RESULTS
Patient Characteristics
Sixty-seven patients were enrolled. Sixty-six patients received at
least one dose of temozolomide and O6-BG. One patient with AA did
not receive any protocol treatment because of withdrawal of consent
and is excluded from all summaries. Patient demographics and baseline disease characteristics of the 66 patients who received protocol
treatment are listed in Table 1. Central pathologic review confirmed
that 34 patients had GBM, 28 patients had AA, and four patients had
2009 by American Society of Clinical Oncology
1263
Quinn et al
No. of Patients (N 66)
Characteristic
Age, years
Median
Range
Sex
Male
Female
Karnofsky performance score, %
70
70-80
90-100
No. of progressions
Median
Range
Time from diagnosis, weeks
Median
Range
Histological diagnosis
AA
AO
GBM
51
21-69
44
22
67
33
3
33
30
4
51
45
1.0
Progression-Free Survival (proportion)
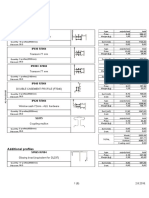
Table 1. Patient Demographics and Clinical Characteristics
0.9
0.8
0.7
0.6
0.5
0.4
0.3
AA/AO
0.2
0.1
2
1-5
GBM
100
200
Time (weeks)
60
12-702
Fig 1. Kaplan-Meier estimates of progression-free survival according to histology. AA, anaplastic astrocytoma; AO, anaplastic oligodendroglioma; GBM, glioblastoma multiforme.
28
4
34
42
6
52
Abbreviations: AA, anaplastic astrocytoma; AO, anaplastic oligodendroglioma; GBM, glioblastoma multiforme.
AO. The median age was 51 years, and the majority of patients were
male. Fifty-five percent of patients had a Karnofsky performance score
of 80. All patients had progressive or recurrent disease after prior
therapy with temozolomide, and the majority of patients (59%) had at
least two prior progressions. The median time from diagnosis to the
start of therapy with temozolomide plus O6-BG was 60 weeks (range,
12 to 72 weeks).
Response
The overall ORR for all histologies was 9% (95% CI, 3% to 19%).
One (3%) of 34 patients with GBM (95% CI, 0.1% to 15%) and five
(16%) of 32 patients with anaplastic glioma (95% CI, 5% to 33%) were
responders to the combination of temozolomide and O6-BG. Table 2
details the response in each histology subgroup. One patient died as a
result of a perforated cecum 2 days after treatment with this drug
combination. Five patients with anaplastic glioma who had a response
completed at least a full year of therapy. Of these five patients, disease
progression did not occur in three patients for 131, 93, and 89 weeks,
respectively, and the other two patients remain disease-free 185 and
164 weeks from enrollment, respectively. Of interest, one patient with
an anaplastic glioma who completed a year of therapy remained progression free for 143 weeks but never realized a response by the modified Macdonald criteria. However, this patients positron emission
tomography scan was hypometabolic on completion of a full year
of therapy.
PFS
The 6-month PFS was 17% overall (95% CI, 9% to 27%), 9% for
GBM (95% CI, 2% to 21%), and 25% for anaplastic glioma (95% CI,
12% to 41%). The median PFS was 7.9 weeks overall (95% CI, 7.6 to
9.6 weeks), 7.5 weeks for GBM (95% CI, 4.2 to 7.9 weeks), and 9.6
weeks for anaplastic glioma (95% CI, 7.9 to 16.1 weeks). There was a
significant statistical difference between the two histologies
(P .0049). The PFS data are illustrated by the Kaplan-Meier curve in
Figure 1.
OS
The 6-month OS was 47% (95% CI, 35% to 58%), 26% for GBM
(95% CI, 13% to 42%), and 69% for anaplastic glioma (95% CI, 50%
to 82%). The median OS was 24.7 weeks (95% CI, 20.9 to 31.0 weeks),
19.4 weeks for GBM (95% CI, 13.7 to 24.3 weeks), and 33 weeks for
anaplastic glioma (95% CI, 28.0 to 49.6 weeks). There was a significant
statistical difference between the two histologies (P .0004). The OS
data are presented as a Kaplan-Meier curve in Figure 2.
Table 2. Overall Survival, Progression-Free Survival, and Objective Response Rate According to Histology
Overall
Variable
Overall survival
Median, weeks
At 6 months, %
Progression-free survival
Median, weeks
At 6 months, %
Objective response rate, %
GBM
AA/AO
No. of Patients
95% CI
No. of Patients
95% CI
24.7
47
20.9 to 31.0
35 to 58
19.4
26
13.7 to 24.3
13 to 42
7.9
17
9
7.6 to 9.6
9 to 27
3 to 19
7.5
9
3
4.2 to 7.9
2 to 21
0.1 to 15
No. of Patients
95% CI
33
69
28 to 49.6
50 to 82
9.6
25
16
7.9 to 16.1
12 to 41
5 to 33
Abbreviations: AA, anaplastic astrocytoma; AO, anaplastic oligodendroglioma; GBM, glioblastoma multiforme.
There was a statistically significant difference between the two histologies.
1264
2009 by American Society of Clinical Oncology
JOURNAL OF CLINICAL ONCOLOGY
TMZ and O6-BG in Malignant Glioma
1.0
Overall Survival (proprotion)
0.9
0.8
0.7
0.6
0.5
0.4
0.3
AA/AO
0.2
GBM
0.1
0
50
100
150
200
Time (weeks)
Fig 2. Kaplan-Meier estimates of overall survival according to histology. AA,
anaplastic astrocytoma; AO, anaplastic oligodendroglioma; GBM, glioblastoma multiforme.
Toxicity
Table 3 summarizes the adverse events (AEs). The most commonly reported AEs were grade 4 hematologic events experienced in
48% of the patients, for whom a 25% temozolomide dose reduction
was required for subsequent dose administrations. The most frequent hematologic AEs were grade 4 neutropenia (47%), followed
by grade 4 thrombocytopenia (12%). One patient died as a result of
a perforated cecum 2 days after initiation of treatment with this drug
combination. This event was unlikely to be drug related, given that
before enrollment she complained of abdominal pain. One patient
was not assessable for toxicity because the patient never received this
drug combination.
DISCUSSION
Temozolomide and polifeprosan 20 with carmustine implant are both
US Food and Drug Administrationapproved drugs because of their
ability to prolong survival in patients diagnosed with malignant glioma. Unfortunately, all patients with this disease will eventually experience treatment failure with these agents.
Resistance to both temozolomide and carmustine is mediated in
part through the DNA repair protein AGT. Three clinical trials13-15
reported an inverse relationship between AGT levels and survival for
patients with malignant glioma treated with carmustine. Esteller et al16
also confirmed this relationship, albeit using methylation of the AGT
promoter gene in lieu of quantization of AGT levels. Likewise, this
same inverse relationship between AGT levels and response was seen
in patients with malignant glioma treated with preradiation temozolomide.17 Furthermore, Hegi et al18 have shown a relationship between inactivation of the AGT gene by promoter methylation and
survival in patients with newly diagnosed GBM treated with surgery,
radiotherapy, and temozolomide. These studies suggest that the efficacy of temozolomide and carmustine could be enhanced by depletion of tumor AGT.
Depletion of tumor AGT activity by a selective inhibitor, O6-BG,
enhances the cytotoxicity of chloroethylators and methylators including temozolomide and carmustine.1,4,7,17,19-21 However, the main limitation in systemic administration of alkylating agents in combination
with O6-BG is their potential for dose-related toxicity to the hematopoietic system. This was seen in animal studies22-24 and confirmed in a
phase I clinical trial,25 where systemic administration of O6-BG and
carmustine markedly enhanced myelosuppression and reduced the
carmustine MTD from 200 to 40 mg/m2, representing an 80% dose
reduction. This profound reduction in the carmustine dose was most
likely the underlying factor in the failure of this drug combination to
cause frank tumor regression in the phase II trial.26
Given that temozolomide is inherently less toxic than carmustine, particularly to hematopoietic cells, it was hypothesized that perhaps temozolomide in combination with O6-BG would produce less
myelosuppression than carmustine in combination with O6-BG.
Thus, a phase I clinical trial was performed in patients with malignant
glioma to determine the MTD of single-dose temozolomide in combination with O6-BG.9 When combined with O6-BG, the MTD of
temozolomide was found to be 472 mg/m2. The requirement for an
80% dose reduction seen with carmustine when combined with
O6-BG was seen to a lesser extent (50%) with temozolomide when
combined with O6-BG.
Thus, one of the aims of this study was to evaluate the safety of
administering O6-BG in combination with temozolomide, especially
to the hematopoietic system. As expected, myelosuppression was the
Table 3. Adverse Events
Grade 3
Adverse Event
Hematologic
Anemia
Lymphopenia
Thrombocytopenia
Neutropenia
Neutropenia, febrile
Nonhematologic
Infection without neutropenia
Seizure
Thrombosis/embolism
GI perforation
www.jco.org
No. of Patients
Grade 4
%
2
4
3
6
Grade 5
No. of Patients
1
1
8
31
1
1
12
47
No. of Patients
2009 by American Society of Clinical Oncology
1265
Quinn et al
most commonly reported AE. Grade 4 hematologic events were experienced in 48% of the patients for whom a 25% temozolomide dose
reduction was required for subsequent dose administrations. The
most frequent hematologic AEs were grade 4 neutropenia (47%)
followed by grade 4 thrombocytopenia (12%).
Another aim of this study was to identify the role of O6-BG in
restoring temozolomide sensitivity in patients with recurrent or progressive temozolomide-resistant malignant glioma. Unfortunately,
the lack of a clinical rationale to justify a biopsy at recurrence precluded quantitation of tumor AGT levels, which could have provided
insights if other non-AGT mechanisms of resistance were operational.
We determined that O6-BG when added to a 1-day dosing regimen of
temozolomide was able to restore temozolomide sensitivity in patients
with temozolomide-resistant anaplastic glioma, but there seemed to
be no significant restoration of temozolomide sensitivity in patients
with temozolomide-resistant GBM.
Despite the encouraging response to temozolomide and O6-BG
in patients with anaplastic glioma, it is somewhat disappointing that a
greater response and improvement in PFS and OS were not realized in
GBM, especially if AGT was indeed the primary mechanism responsible for tumor resistance to temozolomide. Although O6-BG in combination with temozolomide was able to reverse the resistance in a
minority of patients with recurrent or progressive, temozolomideresistant malignant glioma, it was unable to reverse this resistance in
the majority of these patients. The explanation for the inability of this
combination to reverse resistance may lie in the two following reasons.
First, the dose reduction in temozolomide necessary to avoid
hematologic toxicity when combined with O6-BG may be an underlying factor in the failure of this drug combination to restore sensitivity. As a 1-day dosing regimen, temozolomide required a 50% dose
reduction when delivered with O6-BG. Alternative routes of administration of either O6-BG or alkylators have been investigated in hopes of
reducing systemic toxicity while maximizing efficacy. Administration
of O6-BG locally by intracerebral infusion through an Ommaya reservoir with concomitant oral administration of temozolomide was attempted in one patient.27 This therapy was well tolerated and caused
tumor stabilization for four months, but its success at depleting AGT
and thus prolonging survival above and beyond the effect of temozolomide alone is unknown at this time. The administration of carmustine locally in the form of polifeprosan 20 with carmustine implant in
combination with systemic O6-BG was performed in a phase I8 and a
phase II clinical trial.28 Both of these trials support the idea that local
administration of carmustine in the form of polifeprosan 20 with
carmustine implant in combination with systemic O6-BG may mitigate the systemic toxicities of alkylators with improved efficacy.28
Second, combining O6-BG with a 5-day dosing regimen of temozolomide may be more effective than a 1-day dosing regimen, especially if the total dose of temozolomide can be increased. To optimize
a 5-day dosing regimen of temozolomide in combination with O6-BG,
one could hypothesize that suppressing AGT beyond 48 hours for at
least 5 days while administering temozolomide may improve efficacy.
Because we know that the above O6-BG regimen completely suppresses O6-BG for at least 48 hours, perhaps repeating this exact
regimen every 48 hours for a period of 5 to 7 days may optimize AGT
suppression while administering a 5-day dosing regimen of temozolomide. Although other O6-BG regimens have been used in combination with temozolomide29 and polifeprosan 20 with carmustine
1266
2009 by American Society of Clinical Oncology
implant,8 there is no evidence to suggest that these dosing regimens are
adequate to suppress AGT levels in brain tumors.
Although the current trial of O6-BG when added to a 1-day
dosing regimen of temozolomide was able to restore temozolomide
sensitivity in patients with temozolomide-resistant anaplastic glioma,
no significant restoration of temozolomide sensitivity was seen in
patients with temozolomide-resistant GBM. The limited response
seen in GBM propels the research in a direction that explores alternative dosing regimens of temozolomide and O6-BG and alternative
administration routes for chemotherapy. Thus, additional investigation in combining temozolomide and O6-BG in a 5-day dosing schedule needs to be undertaken in a phase I trial. Also, additional
exploration of the safety and efficacy of combining polifeprosan 20
with carmustine implant with O6-BG should be pursued. In addition,
the role of drug delivery needs to be addressed, given that it is possible
that potentially higher interstitial pressure seen in GBMs compared
with anaplastic gliomas may be limiting drug delivery. This question
might be addressed in future studies by incorporation of dynamic
contrast-enhanced MRIs to evaluate tumor blood flow and potentially
drug delivery.
AUTHORS DISCLOSURES OF POTENTIAL CONFLICTS
OF INTEREST
Although all authors completed the disclosure declaration, the following
author(s) indicated a financial or other interest that is relevant to the subject
matter under consideration in this article. Certain relationships marked with a
U are those for which no compensation was received; those relationships
marked with a C were compensated. For a detailed description of the
disclosure categories, or for more information about ASCOs conflict of interest
policy, please refer to the Author Disclosure Declaration and the Disclosures of
Potential Conflicts of Interest section in Information for Contributors.
Employment or Leadership Position: None Consultant or Advisory
Role: Henry S. Friedman, Keryx Biopharmaceuticals (C) Stock
Ownership: None Honoraria: David A. Reardon, Schering-Plough
Research Funding: Henry S. Friedman, Schering-Plough Expert
Testimony: None Other Remuneration: None
AUTHOR CONTRIBUTIONS
Conception and design: Jennifer A. Quinn, David A. Reardon, James J.
Vredenburgh, Darell D. Bigner, James E. Herndon, Henry S. Friedman
Financial support: Darell D. Bigner, Henry S. Friedman
Administrative support: Darell D. Bigner, Henry S. Friedman
Provision of study materials or patients: Jennifer A. Quinn, David A.
Reardon, Annick Desjardins, James J. Vredenburgh, Jeremy N. Rich,
Allan H. Friedman, John H. Sampson, Henry S. Friedman
Collection and assembly of data: Jennifer A. Quinn, Sara Xiaoyin
Jiang, David A. Reardon, James J. Vredenburgh, Jeremy N. Rich,
Sridharan Gururangan, Allan H. Friedman, John H. Sampson, Roger
E. McLendon, Amy Walker
Data analysis and interpretation: Jennifer A. Quinn, Sara Xiaoyin Jiang,
David A. Reardon, James J. Vredenburgh, Sridharan Gururangan, Darell
D. Bigner, Roger E. McLendon, James E. Herndon
Manuscript writing: Jennifer A. Quinn, Sara Xiaoyin Jiang,
James E. Herndon, Henry S. Friedman
Final approval of manuscript: Jennifer A. Quinn, Sara Xiaoyin Jiang,
David A. Reardon, Annick Desjardins, James J. Vredenburgh, Jeremy N.
Rich, Sridharan Gururangan, Allan H. Friedman, Darell D. Bigner, John
H. Sampson, Roger E. McLendon, James E. Herndon, Henry S. Friedman
JOURNAL OF CLINICAL ONCOLOGY
TMZ and O6-BG in Malignant Glioma
REFERENCES
1. Dolan ME, Mitchell RB, Mummert C, et al:
Effect of O6-benzylguanine analogues on sensitivity
of human tumor cells to the cytotoxic effects of
alkylating agents. Cancer Res 51:3367-3372, 1991
2. Hegi ME, Diserens A-C, Godard S, et al:
Clinical trial substantiates the predictive value of
O-6-methylguanine-DNA methyltransferase promoter methylation in glioblastoma patients treated
with temozolomide. Clin Cancer Res 10:1871-1874,
2004
3. Pegg AE, Dolan ME, Moschel RC: Structure,
function, and inhibition of O6-alkylguanine-DNA alkyltransferase. Prog Nucleic Acid Res Mol Biol 51:
167-223, 1995
4. Bobola MS, Tseng SH, Blank A, et al: Role of
O6-methylguanine-DNA methyltransferase in resistance of human brain tumor cell lines to the clinically
relevant methylating agents temozolomide and
streptozotocin. Clin Cancer Res 2:735-741, 1996
5. Wedge SR, Porteous JK, Newlands ES:
3-aminobenzamide and/or O6-benzylguanine evaluated as an adjuvant to temozolomide or BCNU
treatment in cell lines of variable mismatch repair
status and O6-alkylguanine-DNA alkyltransferase activity. Br J Cancer 74:1030-1036, 1996
6. Friedman HS, Dolan ME, Pegg AE, et al:
Activity of temozolomide in the treatment of central
nervous system tumor xenografts. Cancer Res 55:
2853-2857, 1995
7. Wedge SR, Porteus JK, May BL, et al: Potentiation of temozolomide and BCNU cytotoxicity by
O(6)-benzylguanine: A comparative study in vitro.
Br J Cancer 73:482-490, 1996
8. Weingart J, Grossman SA, Carson KA, et al:
Phase I trial of polifeprosan 20 with carmustine
implant plus continuous infusion of intravenous O6benzylguanine in adults with recurrent malignant
glioma: New Approaches to Brain Tumor Therapy
CNS Consortium trial. J Clin Oncol 25:399-404, 2007
9. Quinn JA, Desjardins A, Weingart J, et al:
Phase I trial of temozolomide plus O6-benzylguanine
for patients with recurrent or progressive malignant
glioma. J Clin Oncol 23:7178-7187, 2005
10. Macdonald DR, Cascino TL, Schold SC Jr, et
al: Response criteria for phase II studies of supratentorial malignant glioma. J Clin Oncol 8:12771280, 1990
11. Simon R: Optimal two-stage designs for
phase II clinical trials. Control Clin Trials 10:1-10,
1989
12. Kaplan E, Meier P: Nonparametric estimation
from incomplete observations. J Am Stat Assoc
53:29-41, 1958
13. Belanich M, Pastor M, Randall T, et al: Retrospective study of the correlation between the DNA
repair protein alkyltransferase and survival of brain
tumor patients treated with carmustine. Cancer Res
56:783-788, 1996
14. Hotta T, Saito Y, Fujita H, et al: O6alkylguanine-DNA alkyltransferase activity of human
malignant glioma and its clinical implications. J Neurooncol 21:135-140, 1994
15. Jaeckle KA, Eyre HJ, Townsend JJ, et al: Correlation of tumor O6 methylguanine-DNA methyltransferase levels with survival of malignant astrocytoma
patients treated with bis- chloroethylnitrosourea: A
Southwest Oncology Group study. J Clin Oncol 16:
3310-3315, 1998
16. Esteller M, Garcia-Foncillas J, Andion E, et al:
Inactivation of the DNA-repair gene MGMT and the
clinical response of gliomas to alkylating agents.
N Engl J Med 343:1350-1354, 2000
17. Friedman HS, McLendon RE, Kerby T, et al:
DNA mismatch repair and O6-alkylguanine-DNA alkyltransferase analysis and response to Temodal in
newly diagnosed malignant glioma. J Clin Oncol
16:3851-3857, 1998
18. Hegi ME, Diserens A-C, Gorlia T, et al: MGMT
gene silencing and benefit from temozolomide in
glioblastoma. N Engl J Med 352:997-1003, 2005
19. Baer JC, Freeman AA, Newlands ES, et al:
Depletion of O6-alkylguanine-DNA alkyltransferase
correlates with potentiation of temozolomide and
CCNU toxicity in human tumour cells. Br J Cancer
67:1299-1302, 1993
20. Felker GM, Friedman HS, Dolan ME, et al:
Treatment of subcutaneous and intracranial brain
tumor xenografts with O6-benzylguanine and 1,3-
bis(2-chloroethyl)-1-nitrosourea. Cancer Chemother
Pharmacol 32:471-476, 1993
21. Wedge SR, Newlands ES: O6-benzylguanine
enhances the sensitivity of a glioma xenograft with
low O6-alkylguanine-DNA alkyltransferase activity to
temozolomide and BCNU. Br J Cancer 73:10491052, 1996
22. Page J, Giles H, Phillips W: Preclinical toxicology study of O6-benzylguanine (NSC-637037) and
BCNU (carmustine, NSC0409962) in male and female beagle dogs. Proc Am Assoc Cancer Res 35,
1994 (abstr 1952)
23. Rodman L, Giles H, Tomaszewski J: Preclinical toxicology study of O6-benzylguanine (NSC637037) and 1,3-bis(2-chloroethyl)-1-nitrosourea
(NSC 409962) in mice. Proc Am Assoc Cancer Res
35, 1994 (abstr 1954)
24. Rogers T, Rodman L, Tomaszewski J: Preclinical toxicology and pharmacokinetic studies of O6benzylguanine in mice and dogs. Proc Am Assoc
Cancer Res 35, 1994 (abstr 1953)
25. Friedman HS, Pluda J, Quinn JA, et al: Phase
I trial of carmustine plus O6-benzylguanine for patients with recurrent or progressive malignant glioma. J Clin Oncol 18:3522-3528, 2000
26. Quinn JA, Pluda J, Dolan ME, et al: Phase II
trial of carmustine plus O6-benzylguanine for patients with nitrosourea-resistant recurrent or progressive malignant glioma. J Clin Oncol 20:22772283, 2002
27. Koch D, Hundsberger T, Boor S, et al: Local
intracerebral administration of O(6)-benzylguanine
combined with systemic chemotherapy with temozolomide of a patient suffering from a recurrent
glioblastoma. J Neurooncol 82:85-89, 2007
28. Quinn JA, Desjardins A, Reardon D, et al:
Phase II trial of temozolomide (Temodar) plus O6benzylguanine (O6-BG) in the treatment of patients
with temodar-resistant malignant glioma. NeuroOncology 6:380, 2004
29. Warren K, Aikin AA, Libucha M, et al: Phase I
study of O6-benzylguanine and temozolomide administered daily for 5 days to pediatric patients with
solid tumors. J Clin Oncol 23:7647-7653, 2005
www.jco.org
2009 by American Society of Clinical Oncology
1267
Vous aimerez peut-être aussi
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Peroxiredoxin Systems Structures and FunctionsDocument409 pagesPeroxiredoxin Systems Structures and FunctionsMariano PerezPas encore d'évaluation
- Protein Dna RecognitionDocument31 pagesProtein Dna RecognitionMariano PerezPas encore d'évaluation
- Disulfide Bond Formation and Cysteine Exclusion inDocument10 pagesDisulfide Bond Formation and Cysteine Exclusion inMariano PerezPas encore d'évaluation
- A Pathway For Disulfide Bond Formation in VivoDocument5 pagesA Pathway For Disulfide Bond Formation in VivoMariano PerezPas encore d'évaluation
- The Ubiquitin-Proteasome Proteolytic System From Classical Biochemistry To Human DiseasesDocument242 pagesThe Ubiquitin-Proteasome Proteolytic System From Classical Biochemistry To Human DiseasesMariano PerezPas encore d'évaluation
- Gyrase Inhibitors Induce An Oxidative Damage Cellular Death Pathway in Escherichia ColiDocument15 pagesGyrase Inhibitors Induce An Oxidative Damage Cellular Death Pathway in Escherichia ColiMariano PerezPas encore d'évaluation
- CHOP Induces Death by Promoting Protein Synthesis and Oxidation in The Stressed Endoplasmic ReticulumDocument13 pagesCHOP Induces Death by Promoting Protein Synthesis and Oxidation in The Stressed Endoplasmic ReticulumMariano PerezPas encore d'évaluation
- Redox Sensing by Escherichia Coli Effects of DithiothreitolDocument4 pagesRedox Sensing by Escherichia Coli Effects of DithiothreitolMariano PerezPas encore d'évaluation
- Contribution of Calcium Influx in Mediating Glucose-Stimulated Oxygen Consumption in Pancreatic IsletsDocument11 pagesContribution of Calcium Influx in Mediating Glucose-Stimulated Oxygen Consumption in Pancreatic IsletsMariano PerezPas encore d'évaluation
- Generation of Rho0 Cells Utilizing A Mitochondrially Targeted Restriction Endonuclease and Comparative AnalysesDocument10 pagesGeneration of Rho0 Cells Utilizing A Mitochondrially Targeted Restriction Endonuclease and Comparative AnalysesMariano PerezPas encore d'évaluation
- Microplate-Based Kinetic Method For Assay of Mitochondrial NADH - and Succinate - Cytochrome C Reductase ActivitiesDocument3 pagesMicroplate-Based Kinetic Method For Assay of Mitochondrial NADH - and Succinate - Cytochrome C Reductase ActivitiesMariano PerezPas encore d'évaluation
- Targeting Metabolism To Diagnose and TreatDocument4 pagesTargeting Metabolism To Diagnose and TreatMariano PerezPas encore d'évaluation
- A Molecular Mechanism of Pyruvate Protection Against Cytotoxicity of Reactive Oxygen SpeciesDocument11 pagesA Molecular Mechanism of Pyruvate Protection Against Cytotoxicity of Reactive Oxygen SpeciesMariano PerezPas encore d'évaluation
- Mitochondria/Cytosol Fractionation Kit: Sufficient For Analysis of 50 SamplesDocument8 pagesMitochondria/Cytosol Fractionation Kit: Sufficient For Analysis of 50 SamplesMariano PerezPas encore d'évaluation
- Protein Folding in The Bacterial PeriplasmDocument7 pagesProtein Folding in The Bacterial PeriplasmMariano PerezPas encore d'évaluation
- Selective Removal of Mitochondria Via MitophagyDocument7 pagesSelective Removal of Mitochondria Via MitophagyMariano PerezPas encore d'évaluation
- Mitochondria/Cytosol Fractionation Kit: Sufficient For Analysis of 50 SamplesDocument8 pagesMitochondria/Cytosol Fractionation Kit: Sufficient For Analysis of 50 SamplesMariano PerezPas encore d'évaluation
- Selective Removal of Mitochondria Via MitophagyDocument7 pagesSelective Removal of Mitochondria Via MitophagyMariano PerezPas encore d'évaluation
- Fluorescent Dyes Introduction Ratiometric AssaysDocument2 pagesFluorescent Dyes Introduction Ratiometric AssaysMariano PerezPas encore d'évaluation
- NAD+ and NADH in Cellular Functions and Cell DeathDocument3 pagesNAD+ and NADH in Cellular Functions and Cell DeathMariano PerezPas encore d'évaluation
- Oxidative Protein Folding Is DrivenDocument11 pagesOxidative Protein Folding Is DrivenMariano PerezPas encore d'évaluation
- Oxidative Protein Folding Is DrivenDocument11 pagesOxidative Protein Folding Is DrivenMariano PerezPas encore d'évaluation
- Reactive Oxygen Species in Cancer Cells Live by The Sword Die by The Sword 2006 Cancer CellDocument2 pagesReactive Oxygen Species in Cancer Cells Live by The Sword Die by The Sword 2006 Cancer CellMariano PerezPas encore d'évaluation
- The Rate of Oxygen Utilization by CellsDocument32 pagesThe Rate of Oxygen Utilization by CellsMariano PerezPas encore d'évaluation
- Ratiometric Calcium IndicatorsDocument1 pageRatiometric Calcium IndicatorsMariano PerezPas encore d'évaluation
- An Assessment of Prediction Algorithms For Nucleosome PositioningDocument1 pageAn Assessment of Prediction Algorithms For Nucleosome PositioningMariano PerezPas encore d'évaluation
- An Assessment of Prediction Algorithms For Nucleosome PositioningDocument1 pageAn Assessment of Prediction Algorithms For Nucleosome PositioningMariano PerezPas encore d'évaluation
- Ratiometric Calcium IndicatorsDocument1 pageRatiometric Calcium IndicatorsMariano PerezPas encore d'évaluation
- Antibiotic Efficacy Is Linked To Bacterial Cellular Respiration.Document8 pagesAntibiotic Efficacy Is Linked To Bacterial Cellular Respiration.Mariano PerezPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- S.I.M. InnovaDocument51 pagesS.I.M. InnovaPauline Karen ConcepcionPas encore d'évaluation
- Lista Materijala WordDocument8 pagesLista Materijala WordAdis MacanovicPas encore d'évaluation
- SOCI 223 Traditional Ghanaian Social Institutions: Session 1 - Overview of The CourseDocument11 pagesSOCI 223 Traditional Ghanaian Social Institutions: Session 1 - Overview of The CourseMonicaPas encore d'évaluation
- Bnblist3559 PDFDocument430 pagesBnblist3559 PDFJagroopSinghBalhraPas encore d'évaluation
- Worcester Vs Ocampo - DigestDocument1 pageWorcester Vs Ocampo - DigestMaria Raisa Helga YsaacPas encore d'évaluation
- Emcee - Graduation DayDocument5 pagesEmcee - Graduation DayBharanisri VeerendiranPas encore d'évaluation
- A Triumph of Surgery EnglishDocument13 pagesA Triumph of Surgery EnglishRiya KumariPas encore d'évaluation
- Disha Publication Previous Years Problems On Current Electricity For NEET. CB1198675309 PDFDocument24 pagesDisha Publication Previous Years Problems On Current Electricity For NEET. CB1198675309 PDFHarsh AgarwalPas encore d'évaluation
- Florentino Vs EncarnacionDocument2 pagesFlorentino Vs EncarnacionJay Mark Esconde50% (2)
- In Holland V Hodgson The ObjectDocument5 pagesIn Holland V Hodgson The ObjectSuvigya TripathiPas encore d'évaluation
- BreadTalk - Annual Report 2014Document86 pagesBreadTalk - Annual Report 2014Vicky NeoPas encore d'évaluation
- Message To St. MatthewDocument3 pagesMessage To St. MatthewAlvin MotillaPas encore d'évaluation
- Knapp TestDocument2 pagesKnapp TestGeorge Litu67% (3)
- Food Corporation of India Zonal Office (N) A-2A, 2B, SECTOR-24, NOIDADocument34 pagesFood Corporation of India Zonal Office (N) A-2A, 2B, SECTOR-24, NOIDAEpaper awaazPas encore d'évaluation
- Thermal ComfortDocument6 pagesThermal ComfortHoucem Eddine MechriPas encore d'évaluation
- Case Digest Labor DisputeDocument5 pagesCase Digest Labor DisputeMysh PDPas encore d'évaluation
- Africanas Journal Volume 3 No. 2Document102 pagesAfricanas Journal Volume 3 No. 2Gordon-Conwell Theological Seminary100% (2)
- Internship Report-2020Document77 pagesInternship Report-2020Hossen ImamPas encore d'évaluation
- Leseprobe Aus: "Multilingualism in The Movies" Von Lukas BleichenbacherDocument20 pagesLeseprobe Aus: "Multilingualism in The Movies" Von Lukas BleichenbachernarrverlagPas encore d'évaluation
- 89 Robinson V MirallesDocument1 page89 Robinson V MirallesMartin AlfonsoPas encore d'évaluation
- Reflection IntouchablesDocument2 pagesReflection IntouchablesVictoria ElazarPas encore d'évaluation
- WE) The Accentual Structure of English WordsDocument8 pagesWE) The Accentual Structure of English Wordszhannatagabergen2606Pas encore d'évaluation
- Educ 323 - The Teacher and School Curriculum: Course DescriptionDocument16 pagesEduc 323 - The Teacher and School Curriculum: Course DescriptionCherry Lyn GaciasPas encore d'évaluation
- A Re Ection On The Dominant Learning Theories: Behaviourism, Cognitivism and ConstructivismDocument13 pagesA Re Ection On The Dominant Learning Theories: Behaviourism, Cognitivism and Constructivismchill protocolPas encore d'évaluation
- FUNCTIONS of LANGUAGE L. HébertDocument7 pagesFUNCTIONS of LANGUAGE L. HébertGonzalo Muniz100% (2)
- A Terence McKenna Audio Archive - Part 1Document203 pagesA Terence McKenna Audio Archive - Part 1BabaYagaPas encore d'évaluation
- Formulating A PICOT QuestionDocument4 pagesFormulating A PICOT QuestionKarl RoblePas encore d'évaluation
- Review of Related LiteratureDocument5 pagesReview of Related LiteratureRJ PareniaPas encore d'évaluation
- Data Sheet Physics 1 Module 10BDocument2 pagesData Sheet Physics 1 Module 10BBryanHarold BrooPas encore d'évaluation
- A Scoping Literature Review of The Provision of Orthoses and Prostheses in Resource-Limited Environments 2000-2010. Part Two: Research and OutcomesDocument20 pagesA Scoping Literature Review of The Provision of Orthoses and Prostheses in Resource-Limited Environments 2000-2010. Part Two: Research and OutcomesGufron Abu MufadholPas encore d'évaluation