Académique Documents
Professionnel Documents
Culture Documents
Risk Factors For Predicting Diarrheal Duration
Transféré par
Dini NanamiTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Risk Factors For Predicting Diarrheal Duration
Transféré par
Dini NanamiDroits d'auteur :
Formats disponibles
Indian J Pediatr (April 2012) 79(4):472477
DOI 10.1007/s12098-011-0561-3
ORIGINAL ARTICLE
Risk Factors for Predicting Diarrheal Duration
and Morbidity in Children with Acute Diarrhea
Archana B. Patel & Ronithung Ovung &
Neetu B. Badhoniya & Michael J. Dibley
Received: 19 October 2010 / Accepted: 12 September 2011 / Published online: 24 September 2011
# Dr. K C Chaudhuri Foundation 2011
Abstract
Objective To identify baseline risk factors for prolonged
diarrheal duration and subsequent complications in children
aged 6 to 59 mo with acute diarrhea who participated in a
micronutrient clinical trial in a tertiary care hospital.
Methods The adjusted odds ratio or incidence risk ratios (IRR)
of the baseline variables for prolongation of diarrheal duration
(cox proportional hazard model), diarrhea >7 d (multiple
logistic regressions), severe dehydration experienced after
hospitalization (poisson regression models) was estimated.
Results Fever (OR 1.10, 95% CI 1.021.19, p=0.02), dehydration (OR 1.32, 95% CI 1.101.59, p=0.003), dysentery
(OR 1.41 95% CI 1.091.82, p=0.008), those who received
medications (OR 1.19, 95% CI 1.031.39, p=0.02), and
A. B. Patel
Department of Pediatrics,
Indira Gandhi Government Medical College,
Nagpur, India
A. B. Patel : N. B. Badhoniya
Lata Medical Research Foundation,
Nagpur, India
R. Ovung
Indira Gandhi Government Medical College,
Nagpur, India
N. B. Badhoniya
Department of Biostatistics, Public Health Foundation of India,
New Delhi, India
weight for age Z-score 2 (OR 1.25, 95% CI 1.071.46,
p=0.004) were at a greater risk of prolonged diarrhea.
Diarrhea >7 d was associated with younger age (OR 1.08,
95% CI 1.031.14, p=0.003), female child (OR 2.33, 95% CI
1.194.55, p=0.013), diarrheal duration before enrolment (OR
1.06, 95% CI 1.041.09, p<0.001), fever (OR 1.7, 95% CI
1.232.49, p=0.002) and the weight for age Z-score 2 (OR
4.32, 95% CI 2.039.16, p<0.001). Severe dehydration after
hospitalization was associated with dehydration at baseline
(OR 6.7, 95% CI 23.0, p<0.001), incomplete immunization
(OR 3.33, 95% CI 1.57.69, p<0.001), failure to receive any
medication(OR 3.03, 95% CI 1.267.14, p=0.01).
Conclusions Few studies assess risk factors for diarrheal
morbidity prospectively. The present study showed that
children of acute diarrhea with above risk factors need stricter
monitoring for complications to reduce diarrheal mortality.
Keywords Acute diarrhea . Morbidity . Risk factors .
Duration . Children
Abbreviations
IV
Intravenous
ORS
Oral rehydration solution
Pl
Placebo
RH
Relative hazards
WHO
World Health Organization
Zinc
Zn
Zn+Cu Zinc and copper
M. J. Dibley
The Sydney School of Public Health, University of Sydney,
Sydney, Australia
A. B. Patel (*)
125, Raj Nagar, Opposite Tidke Vidyalay, Katol Road,
Nagpur 440 013, MS, India
e-mail: dr_apatel@yahoo.com
Introduction
Diarrheal disease causes an estimated 1.8 million deaths per
year [1]. Despite evidence of reduction in mortality over the
Indian J Pediatr (April 2012) 79(4):472477
last 50 y, diarrheal disease continues to be a major killer of
children aged less than 5 y and a principal cause of
morbidity for most impoverished children of the world [2, 3].
One third of the hospital admissions in developing
countries are due to diarrhea related diseases, with 17%
mortality [4, 5]. In India, 9% of children under five had
diarrhea and 1% of these children had blood in their stools
in two wk preceding the third National Family Health
Survey (20056) [6]. Although the majority of episodes of
diarrhea are self-limited, the proportions that experience
mortality are due to dehydration and complications due to
prolongation of diarrhea [7]. Identification of risk factors for
prolongation of acute diarrhea in children can help in the
management, planning and prevention of complications due
to acute diarrhea and subsequent mortality. Although there
are many studies that report epidemiological risk factors for
acute diarrhea in children, there are few that identify the
risks of prolongation of the episode and its complications in
a cohort of children with acute diarrhea. If children with
these risk factors are provided greater medical attention, it
may be possible to reduce childhood morbidity and
mortality. The aim of the present study was to identify
baseline factors in the study population that are associated
with prolonged duration of acute diarrhea.
473
intake of anti-diarrheal or antimicrobial agents, type of
rehydration practiced at home, and hemoglobin concentration (Hemocue method) [9, 10]. The household wealth index,
water and hand sanitation scores were composite indices
derived by scoring different factors that contributed to these
indices using principal component analysis [11]. Factors
assessed for the household wealth index were ownership
of electricity, radio, television, refrigerator, bicycle, scooter
and land, main material used for dwelling floor and fuel
used for cooking. For the water safety score the main
source of drinking water, water storage and treatment of
drinking water before use were assessed, and for the hand
sanitation score washing of hands by soap and water, mud,
plain water or not washed before feeding the child and after
going to latrine were assessed. Nutritional status was
assessed by measuring weight and height using standard
methods and calculating weight for age and, weight for
height Z-scores using the World Health Organization 2005
Anthro software [12]. Weight was measured to nearest 100 g
using an electronic scale (Wedderburn Tanita HD-316). For
children <2 y the length was measured in supine position
on a wooden sliding board, those over 2 y had stature
measured using a height board.
Monitoring of Participants
Material and Methods
In the present study the authors determined the risk factors
that predicted diarrheal duration and subsequent morbidity
in 6 to 59-mo-old children, participating in a randomized
control trial which evaluated the effect of zinc and copper
in treatment of acute diarrhea, admitted at the Indira Gandhi
Government Medical College, Nagpur India [8]. This study
was a part of a micronutrient clinical trial of three arms
namely, placebo (Pl), zinc (Zn) only, and zinc and copper
(Zn+Cu) arms, in 808 children aged 6 to 59 mo of acute
diarrhea, which received ethical clearance from both the
involved institutes. The detailed methods for the trial have
been reported elsewhere [8]. Here the authors report the
baseline characters, nutritional status and etiological agent
of acute diarrhea in children aged 6 mo to 59 mo that
predict the diarrheal duration.
Baseline Assessment
At enrolment, the study research physician collected
information from the mother about: age, gender, duration
of illness (fever, vomiting, diarrhea), dehydration (present
or absent), blood in stools (dysentery or not), immunization
status (as per schedule), any breast feeding, maternal
education in years, number of children in the household,
household assets and facilities, water safety hand sanitation,
The patients were monitored for dehydration, complications
(severe dehydration, electrolyte imbalance, hemolytic uremic syndrome, septicemia, co-morbidities such as severe
anemia, malaria, pneumonia, meningitis, and death), and
the need for unscheduled intravenous fluids (use of IV
fluids on appearance of severe dehydration despite appropriate ORS administration) and its volume (ml) till
discharge. ORS and water were supplied in a container of
known volume capacity and the total amount consumed
from start of the study to the cessation of diarrhea was
calculated in ml. Patients were discharged only after
cessation of diarrhea. A child was discontinued from the
study for any of the following reasons: complications such
as electrolyte imbalance, azotemia, convulsion, acidosis,
congestive heart failure, hemolytic uremic syndrome,
septicemia, unconscious, death, preventing the child from
taking oral fluids or medications, occurrence of a serious
adverse event, parents or guardian withdrawal of consent,
or if the patient left against medical advice.
Statistical Analysis
Data was entered each day into pre-programmed Microsoft
Access software database. STATA 10/IC (STATA Corporation, College Station, TX) software was used for statistical
analysis. Anthropometric indicators were calculated using
World Health Organizations 2005 Anthro software. Uni-
474
Indian J Pediatr (April 2012) 79(4):472477
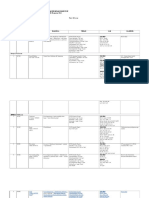
Table 1 Baseline characteristics of the children enrolled in the trial
Characteristics
n=808
Age mo, mean (SD)
Male Gender N (%)
17.9 (11.1)
477 (59.03)
Mothers education schooling yrs, mean (SD)
7 (4.249967
Immunization complete to-date N (%)
Breast feeding/complimentary feeds N (%)
549 (68)
453 (56.1)
Duration of diarrhea, h, mean (SD)
35.4 (20.4)
Number of stool before enrolment mean (SD)
Duration of vomiting before mean (SD)
8.5 (4.2)
20.3 (20.8)
Temperature C, mean (SD)
98.8 (1)
Dehydration N (%)
Dysentery N (%)
174 (21.5)
78 (9.6)
Rota virus diarrhea N (%)
169 (21.1)
Received any other medications N (%)
Weight for age Z-score 2N (%)
365 (45.2)
426 (52.7)
Household wealth index mean (SD)
0.0001 (1)
Water safety score mean (SD)
Hand washing score mean (SD)
1.8 (0.93)
1.2 (1.04)
Serum zinc g/dl, mean (SD)
Serum Copper g/dl, mean (SD)
71.2 (32.5)
123.5 (36.4)
Hemoglobin% g/dl, mean (SD)
9.7 (1.9)
Table 2 Relative hazards for
continuation of diarrhea in
children
variate analysis was carried out by estimating regression
coefficient or odds ratios (OR) or incidence risk ratios
(IRR) and their 95% confidence interval (CI) for all the risk
factors for diarrheal duration. Cox proportional hazards
model was used to estimate the relative hazards (RH) of
continuation of diarrhea of the baseline covariates. Using
intention to treat analysis, the unadjusted and adjusted OR
or IRR of the baseline variables for three additional
outcomes (a) diarrhea longer than 7 d from onset(multiple
logistic regression), (b) complications in hospital, and (c)
severe dehydration experienced in hospital after enrolment
was estimated using poisson regression models. A full
model of multiple logistic regression (MLR) and multiple
poisson regression (MPR) included all risk factors measured in the present study. However, the final model
included the risk factors which were significant in the full
model at level of 0.25. The level of significance was
fixed at =0.05, for judging the significance of that
covariate in the final model. Baseline risk factors considered were age, gender, maternal education, immunization,
any breastfeeding, prior duration of diarrhea, duration of
vomiting, stool frequency per day, stool type, any medication received, weight for age 2, dehydration status,
temperature, water safety score, wealth index, hand
washing score, serum zinc and copper level, hemoglobin
Baseline variables
Unadjusted
Adjusted
OR (95% CI)
Zinc
Zinc and Copper
Age (mo)
Female Gender
1.05
1.02
0.98
1.07
(0.90, 1.22)
(0.88, 1.18)
(0.98,0.99)
(0.92,1.23)
0.57
0.81
<0.001
0.39
Mothers education schooling(y)
Immunization complete to-date
Breast feeding/complimentary feeds
Duration of diarrhea before enrolment (h)
Number of stool before enrolment
0.99
1.00
1.32
1.00
1.01
(0.97,1.00)
(0.86,1.16)
(1.15,1.53)
(1.00,1.01)
(1.00,1.03)
0.1
0.97
<0.001
0.01
0.11
Duration of vomiting before enrolment h
Temperature (C)
Dehydration
Dysentery
Rota virus diarrhea
Received any other medications
Weight for age Z-score 2
Household wealth index
Water safety score
Hand washing score
Serum zinc(g/dl)
Serum Copper (g/dl)
Hemoglobin% (g/dl)
1.00
1.13
1.31
1.26
1.21
1.31
1.14
0.91
1.10
1.01
1.00
1.00
0.96
(1.00,1.01)
(1.04,1.22)
(1.10,1.58)
(0.98,1.61)
(1.02,1.44)
(1.13,1.51)
(0.99,1.32)
(0.84,0.98)
(1.02,1.19)
(0.94,1.07)
(1.00,1.00)
(1.00,1.00)
(0.92,0.99)
0.16
<0.001
<0.001
0.07
0.03
<0.001
0.07
0.01
0.01
0.88
0.81
0.02
0.02
OR (95% CI)
0.98(0.97, 0.99)
1.14(0.98,1.32)
<0.001
0.09
0.99 (0.97,1.01)
1.10 (0.95,1.28)
0.15
0.25
1.00 (1.00,1.01)
0.05
1.10 (1.02,1.19)
1.32 (1.10,1.59)
1.41 (1.09,1.82)
0.02
<0.001
0.01
1.19
1.25
0.92
1.06
0.02
<0.001
0.06
0.13
(1.03,1.39)
(1.07,1.46)
(0.85,1.00)
(0.98,1.15)
1.00 (1.00,1.00)
0.08
Indian J Pediatr (April 2012) 79(4):472477
475
and ELISA test (Premier Rotaclane) was used for rotavirus
antigen detection.
significantly more likely to experience severe dehydration. Children dehydrated at admission were also at
increased risk of complications (OR 5.25, 95% CI 2.4011.4,
p<0.001).
Results
The baseline characteristics of the study population are
shown in Table 1. The univariate and multivariate hazard
ratios of baseline variables associated with continuation of
diarrhea are shown in Table 2 and that for diarrhea >7 d is
shown in Table 3. Clinical indicators such as younger age
(increased risk for continuation of diarrhea by 24% for age
reduction by each year), fever, blood in stools, weight for
age Z-score 2, duration of diarrhea at enrolment were
common risk factors for continuation of diarrhea and for
diarrhea >7 d. It is important to note that receiving zinc
supplement, lower sanitation (water safety and hand
washing) score, baseline zinc and anemia had no impact
on duration of diarrhea. Those children who were dehydrated (6.69, 95% CI 2 3.01, 14.85, p<0.001) at baseline
were more likely to experience severe dehydration even
after admission. Incompletely immunized children (OR
3.33, 95% CI 1.57.69, p<0.001) and those receiving
medications (OR 3.03, 95% CI 1.267.14, P 0.01) were
Discussion
This is a prospective study in 808 children with mean age
17.9+11.1 mo at the government hospital. The mean
maternal literacy was low with an average of 7 y of
education and over half the children had weight for age Zscore 2 (52.7%). Prolongation in duration of acute
diarrhea was associated with the following clinical indicators: younger age, fever, dehydration, blood in stools, those
who received any medication, duration of diarrhea at
enrolment and weight for age Z-score 2 (Table 2). There
was also a tendency towards prolonged diarrhea in children
with lower wealth index. Studies have shown that diarrheal
incidence is high in toddlers, however, this study shows
that even the diarrheal duration is longer in younger
children [13, 14]. The reason for their susceptibility for
prolongation could be their poorly challenged immune
system. A study from Hong Kong that retrospectively
Table 3 Risk factor associated with diarrheal duration >7 d from onset
Factors influencing diarrheal duration >7 d from onset
Unadjusted
OR (95% CI)
Adjusted
P
OR (95% CI)
1.77 (0.89,3.50)
Zinc
1.58 (0.77, 3.25)
0.215
0.102
Zinc and Copper
Age mo
1.11 (0.53, 2.38)
0.94 (0.90, 0.98)
0.795
0.005
0.93 (0.88,0.97)
0.003
Male gender
0.52 (0.29,0.94)
0.03
0.43 (0.22,0.84)
0.013
Mothers education schooling yrs
Immunization complete to-date
Breast feeding/complimentary feeds
Duration of diarrhea before enrolment h
Number of stools before enrolment
Duration of vomiting before
Temperature C
Dehydration
Dysentery
Rota virus diarrhea
Received any other medications
Weight for age Z-score 2
Household wealth index
Water safety score
Hand washing score
Serum zinc g/dl
Serum Copper g/dl
0.990.92,1.06)
1.18 (0.62, 2.24)
0.62 (0.33,1.15)
1.05 (1.04,1.07)
1.00 (0.93,1.07)
1.01 (0.99,1.02)
1.25 (0.95,1.65)
1.08 (0.53,2.23)
2.40 (1.11,5.18)
1.23 (0.62,2.41)
2.44 (1.33,4.49)
2.08 (1.11,3.90)
0.87 (0.63,1.19)
1.36 (1.01,1.83)
0.91 (0.68,1.22)
1.00 (1.00,1.00)
1.00 (1.00,1.00)
0.803
0.611
0.126
<0.001
0.973
0.389
0.114
0.828
0.026
0.557
0.004
0.022
0.379
0.04
0.522
0.087
0.093
1.56 (0.76,3.21)
0.223
Hemoglobin% g/dl
0.95 (0.81,1.11)
0.527
1.06
0.95
0.99
1.75
(1.04,1.09)
(0.87,1.03)
(0.97,1.00)
(1.23,2.49)
<0.001
0.216
0.106
0.002
2.50
1.84
1.72
4.32
(0.99,6.29)
(0.82,4.14)
(0.86,3.45)
(2.03,9.16)
0.052
0.138
0.125
<0.001
1.29 (0.90,1.85)
0.171
1.00 (1.00,1.00)
0.241
476
reviewed inpatient gastro-enteritis management found that
children with mucus and blood in their stools, fever on
admission and received antibiotics were more likely to have
bacterial pathogen with longer duration of stay in the
hospital. This is consistent with the findings of the present
prospective study and other studies worldwide [1517].
Malnutrition was also a risk factor in the present study.
Prolonged diarrhea is a recognized risk factor for malnutrition in the low income countries and vice versa malnutrition
can be a risk factor for dehydration and prolongation of
diarrhea [18, 19]. In the present study 52.7% of the study
children had weight for age Z-score 2 and the risk of
continued diarrhea in this population was 25% more than
children with no malnutrition. Protein energy malnutrition
retards the repair of the damaged intestinal epithelium and
can prolong diarrhea [20]. Duration of diarrhea at admission
is also of clinical importance to monitor diarrheal severity.
The severity of diarrhea at enrolment was the most
important predictor for prolongation of diarrhea >4 d in
another study that evaluated the effect of zinc and copper
mixed with ORS for treatment of acute diarrhea [21].
Similarly, presence of dehydration at enrolment could also
reflect severity of diarrhea and have been recognized to
increase the duration of diarrhea [22]. The only additional risk
factor for diarrhea >7 d was gender. Females had a higher
risk of experiencing diarrhea >7 d. This could be a regional
observation as the epidemiology of prolonged diarrhea
differs across studies [2328].
The risk factors for severe dehydration after admission
were some dehydration, incomplete immunization and no
medication received at enrolment. These are the children who
would be experiencing more frequent stools or vomiting or
have not received adequate ORS or medical attention early in
the course of the illness. Despite treatment and monitoring in
hospital they were still susceptible to severe dehydration and
complications. This indicates that children with diarrhea who
receive early attention and adequate management even at
home are less likely to suffer either prolongation of diarrhea,
severe dehydration or its complications. Another case control
study from this region found similar baseline risk factors of
younger age, malnutrition and severity of illness for moderate
or severe dehydration [26].
Conclusions
Few prospective studies have identified baseline clinical
risk factors that predict morbidity in a cohort of children
with acute diarrhea for better monitoring of these children.
It was observed that clinical indicators such as younger
children, those malnourished, having fever, diarrhea with
blood, received no medications, longer duration of diarrhea
at admission and those with dehydration at the time of
Indian J Pediatr (April 2012) 79(4):472477
hospitalization need to be carefully monitored as they are at
risk for prolonged diarrhea.
Acknowledgements The authors extend their thanks to all the
women, children and their families who participated in the trial, also
thank the following members of the research team who contributed to
the successful implementation of the study: Mr. Hussaini Ali and Mr.
Gadkari (Universal Medicaments Pharmacists), Ms. Smita Puppulwar
and Ms. Shubhangi Puranik. Authors are grateful to Prof. Catherine
DEste, Dr. AV Shrikhande and Dr. Nitin Kimmatkar, the members of
the treatment effects monitoring committee, who reviewed the
unexpected trial events and conducted an interim analysis. The project
was supported by a Wellcome Trust Collaborative Research Initiative
Grant (number 068664/Z/02/Z).
Contributions AP:developed the study protocol, questionnaires and
clinical trial procedures, directed the conduct of the trial, data analysis,
data interpretation and wrote the first draft of the paper; RO: helped in
reviewing literature, drafting and editing the paper; NB: helped with
data analysis and editing the manuscript; MJD: contributed to the
development of the protocol, helped in the development of study
questionnaires and trial procedures, contributed to the data analysis,
data interpretation and edited the paper. All authors reviewed drafts of
the manuscript, read and approved the final draft.
Conflict of Interest None.
Role of Funding Source Wellcome Trust Collaborative Research
Initiative Grant.
References
1. Bryce J, Boschi-Pinto C, Shibuya K, Black RE, WHO Child
Health Epidemiology Reference Group. WHO estimates of the
causes of death in children. Lancet. 2005;365:114752.
2. Kosek M, Bern C, Guerrant RL. The global burden of diarrheal
disease, as estimated from studies published between 1992 and
2000. Bull World Health Organ. 2003;81:197204.
3. Keusch GT, Fontaine O, Boschi-Pinto C, Bhutta ZA, Gotuzzo E.
Diarrheal diseases. In: Jamison JT, Measham AR, Alleyne G, et
al., editors. Disease control priorities in developing countries. 2nd
ed. Washington: World Bank; 2006. p. 37187.
4. World Health Organization. Persistent diarrhea in children in
developing countries: memoranda from a WHO meeting. Bull
WHO. 1988;66:70927.
5. World Health Organization WHO. Division of diarrheal and acute
respiratory disease control. Rational management of diarrhea in
children. Essent Drugs Monit. 1991;11:101.
6. International Institute for Population Sciences (IIPS) and ORC
Macro. National Family Health Survey (NFHS-3), 200506:
India. Mumbai: IIPS; 2006.
7. Gyimah S. Interaction effects of maternal education and household facilities on childhood diarrhea in Sub-Saharan Africa. J
Health Popul Dev Ctries. 2003 (13 November, 2003).
8. Patel A, Dibley MJ, Mamtani M, Badhoniya N, Kulkarni H. Zinc
and copper supplementation in acute diarrhea in children: a
double-blind randomized controlled trial. BMC Med. 2009;7:22.
9. WHO. The treatment of diarrhea: a manual for physicians and
other senior health workers. Vol. WHO/CDD/SER/80.2. Geneva:
World Health Organization; 2005.
Indian J Pediatr (April 2012) 79(4):472477
10. HemoCue Blood Hemoglobin Photometer Operating Manual.
[http://www.hemocue.com/files/900138_GB.pdf].
11. Filmer D, Pritchett LH. Estimating wealth effects without
expenditure data or tears: an application to educational enrolments
in States of India. Demography. 2001;38:11532.
12. WHO. WHO Anthro. 2005: Geneva, Switzerland.
13. Karim AS, Akhter S, Rahman MA, Nazir MF. Risk factors of
persistent diarrhea in children below five years of age. Indian J
Gastroenterol. 2001;20:5961.
14. Faanha MC, Pinheiro AC. Acute diarrhea treated by health care
services in Fortaleza, Cear State, Brazil, from 1996 to 2001. Cad
Saude Publica. 2005;21:4954.
15. Thapa BR, Ventkateswarlu K, Malik AK, Panigrahi D. Shigellosis
in children from north India: a clinicopathological study. J Trop
Pediatr. 1995;41:3037.
16. Uhnoo I, Olding-Stenkvist E, Kreuger A. Clinical features of
acute gastroenteritis associated with rotavirus, enteric adenoviruses,
and bacteria. Arch Dis Child. 1986;61:7328.
17. Lins MD, Silva GA. Diarrheal disease in hospitalized children
importance of the persistent diarrhea. J Pediatr (Rio J). 2000;76:3743.
18. Mach O, Lu L, Creek T, et al. Population-based study of a
widespread outbreak of diarrhea associated with increased
mortality and malnutrition in Botswana, JanuaryMarch, 2006.
Am J Trop Med Hyg. 2009;80:8128.
19. Schmidt WP, Cairncross S, Barreto ML, Clasen T, Genser B. Recent
diarrheal illness and risk of lower respiratory infections in children
under the age of 5 years. Int J Epidemiol. 2009;38:76672.
477
20. Riveron Corteguera R. Persistent diarrhea. Arch Domin Pediatr.
1993;29:5862.
21. Patel AB, Dhande LA, Rawat MS. Therapeutic evaluation of zinc
and copper supplementation in acute diarrhea in children: double
blind randomized trial. Indian Pediatr. 2005;42:43342.
22. Bhattacharya SK, Bhattacharya MK, Manna B, et al. Risk
factors for development of dehydration in young children with
acute watery diarrhea: a case-control study. Acta Paediatr.
1995;84:1604.
23. Banerjee B, Hazra S, Bandyopadhyay D. Diarrhea management
among under fives. Indian Pediatr. 2004;41:25560.
24. Staat MA, Morrow AL, Reves RR, Bartlett AV, Pickering LK.
Diarrhea in children newly enrolled in day-care centers in
Houston. Pediatr Infect Dis J. 1991;10:2826.
25. Cruz JR, Bartlett AV, Mendez H, Sibrian R. Epidemiology of
persistent diarrhea among Guatemalan rural children. Acta
Paediatr Suppl. 1992;381:226.
26. Zodpey SP, Deshpande SG, Ughade SN, Hinge AV, Shirikhande
SN. Risk factors for development of dehydration in children aged
under five who have acute watery diarrhea: a case-control study.
Public Health. 1998;112:2336.
27. El Samani FZ, Willett WC, Ware JH. Predictors of simple diarrhea
in children under 5 yearsa study of a Sudanese rural
community. Soc Sci Med. 1989;29:106570.
28. Ahmed M, Billoo AG, Murtaza G. Risk factors of persistent
diarrhea in children below five years of age. J Pak Med Assoc.
1995;45:2902.
Vous aimerez peut-être aussi
- Parade OK 3 07 June 2017Document9 pagesParade OK 3 07 June 2017Dini NanamiPas encore d'évaluation
- Ocular Trauma SlideDocument49 pagesOcular Trauma SlideRizky FajriPas encore d'évaluation
- Mapping RabuDocument6 pagesMapping RabuDini NanamiPas encore d'évaluation
- Rekap Pasien Bedah Digestive Minggu, 13 November 2016: Nama Dokter MudaDocument6 pagesRekap Pasien Bedah Digestive Minggu, 13 November 2016: Nama Dokter MudaDini NanamiPas encore d'évaluation
- 29.full BolehDocument7 pages29.full BolehDini NanamiPas encore d'évaluation
- Theron Et Al 2011Document9 pagesTheron Et Al 2011Dini NanamiPas encore d'évaluation
- Jurnal TB 1Document18 pagesJurnal TB 1Dini NanamiPas encore d'évaluation
- Soal Uts Lp3iDocument1 pageSoal Uts Lp3iDini NanamiPas encore d'évaluation
- Rekap Pasien Bedah Digestive Selasa, 08 November 2016: Nama Dokter MudaDocument6 pagesRekap Pasien Bedah Digestive Selasa, 08 November 2016: Nama Dokter MudaDini NanamiPas encore d'évaluation
- ABC of DermatologyDocument149 pagesABC of DermatologyAndreea Alexandru100% (14)
- No TBDocument8 pagesNo TBDini NanamiPas encore d'évaluation
- No Agak TBDocument9 pagesNo Agak TBDini NanamiPas encore d'évaluation
- Tuberculosis 140515184439 Phpapp01Document47 pagesTuberculosis 140515184439 Phpapp01Veronica Wong Huey ShinPas encore d'évaluation
- Tuberculosis 140515184439 Phpapp01Document47 pagesTuberculosis 140515184439 Phpapp01Veronica Wong Huey ShinPas encore d'évaluation
- Treatment of Complicated Parapneumonic Pleural Medscimonit 2012Document7 pagesTreatment of Complicated Parapneumonic Pleural Medscimonit 2012DianaWilderPas encore d'évaluation
- Jurnal TB 2Document6 pagesJurnal TB 2Dini NanamiPas encore d'évaluation
- Pone 0149258Document16 pagesPone 0149258Dini NanamiPas encore d'évaluation
- Jurnal 3Document11 pagesJurnal 3Dini NanamiPas encore d'évaluation
- Jurnal TB 1Document18 pagesJurnal TB 1Dini NanamiPas encore d'évaluation
- Slide Dini JurnalDocument22 pagesSlide Dini JurnalDini NanamiPas encore d'évaluation
- Slide Dini JurnalDocument34 pagesSlide Dini JurnalDini NanamiPas encore d'évaluation
- Theron Et Al 2011Document9 pagesTheron Et Al 2011Dini NanamiPas encore d'évaluation
- Radiological Features of BronchiectasisDocument24 pagesRadiological Features of BronchiectasisOxana TurcuPas encore d'évaluation
- The God Factor - The Role of Religious Involvement On DepressionDocument122 pagesThe God Factor - The Role of Religious Involvement On DepressionDini NanamiPas encore d'évaluation
- Chronic Diarrhea GuideDocument14 pagesChronic Diarrhea GuideDini NanamiPas encore d'évaluation
- Art:10.1007/s00431 007 0419 XDocument8 pagesArt:10.1007/s00431 007 0419 XDini NanamiPas encore d'évaluation
- Functional Diarrhea in Toddlers (Chronic Nonspeci Fi C Diarrhea)Document4 pagesFunctional Diarrhea in Toddlers (Chronic Nonspeci Fi C Diarrhea)Dini NanamiPas encore d'évaluation
- DissertationDocument228 pagesDissertationDini NanamiPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5783)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Ethical Issues in Nursing Research:: Deontological PerspectiveDocument11 pagesEthical Issues in Nursing Research:: Deontological PerspectiveJM JavienPas encore d'évaluation
- Multi-Specialty Hospital: Ram Sharada Healthcare Pvt. LTDDocument48 pagesMulti-Specialty Hospital: Ram Sharada Healthcare Pvt. LTDsubhash goelPas encore d'évaluation
- William Obstetric 24th Study GuideDocument447 pagesWilliam Obstetric 24th Study GuideNizam Kunong100% (2)
- Memo No. 2022-59 - Submission of Updated PHIC and PRC License of Medical SpecialistsDocument8 pagesMemo No. 2022-59 - Submission of Updated PHIC and PRC License of Medical SpecialistsPaul Rizel LedesmaPas encore d'évaluation
- Effectiveness of Information, Education and Communication Package On Knowledge On Developmental Care Among Mothers of Low Birth Weight BabiesDocument12 pagesEffectiveness of Information, Education and Communication Package On Knowledge On Developmental Care Among Mothers of Low Birth Weight Babiesiaset123Pas encore d'évaluation
- 1) Community PharmacyDocument17 pages1) Community PharmacyDr. Zirwa AsimPas encore d'évaluation
- 75 5056am0703 614 623Document10 pages75 5056am0703 614 623Rizkhy WahyuPas encore d'évaluation
- A Brief History of EndodonticsDocument5 pagesA Brief History of EndodonticsDidi PascalauPas encore d'évaluation
- A Multidisciplinary Care Map For A Woman in Preterm Labor LazaletaDocument3 pagesA Multidisciplinary Care Map For A Woman in Preterm Labor Lazaletablythe RiveroPas encore d'évaluation
- The Generics ActDocument19 pagesThe Generics ActCJ Halasan100% (1)
- Small But Intriguing The Unfolding Story of Homeopathic Medicine PDFDocument7 pagesSmall But Intriguing The Unfolding Story of Homeopathic Medicine PDFweb3351Pas encore d'évaluation
- End of Life Summit FICA References PDFDocument2 pagesEnd of Life Summit FICA References PDFTejas PatilPas encore d'évaluation
- Emp Master 09042015Document80 pagesEmp Master 09042015Joe SalisPas encore d'évaluation
- Teaching Faculty For Allied Health Sciences - 2021Document9 pagesTeaching Faculty For Allied Health Sciences - 2021jamoonPas encore d'évaluation
- Hepatitis B InfectionDocument8 pagesHepatitis B Infectionto van quyenPas encore d'évaluation
- Research On Prison HealthcDocument87 pagesResearch On Prison HealthcptsievccdPas encore d'évaluation
- Rapid Is 2015Document11 pagesRapid Is 2015José Cunha CoutinhoPas encore d'évaluation
- Contoh Format Laporan SoapDocument5 pagesContoh Format Laporan SoapAchmad Triwidodo AmoePas encore d'évaluation
- Ayushman Bharat PMJAY Branding GuidelinesDocument10 pagesAyushman Bharat PMJAY Branding GuidelinesalkaPas encore d'évaluation
- Routine Health Information System: by Atsede Mazengia (BSC, MPH) Uog-2022Document374 pagesRoutine Health Information System: by Atsede Mazengia (BSC, MPH) Uog-2022Birhanu GirmaPas encore d'évaluation
- Children's Services Job DescriptionDocument11 pagesChildren's Services Job DescriptionMuhammad Dian Luthfy LubisPas encore d'évaluation
- Final Report On The Audit of Peace Corps Panama IG-18-01-ADocument32 pagesFinal Report On The Audit of Peace Corps Panama IG-18-01-AAccessible Journal Media: Peace Corps DocumentsPas encore d'évaluation
- Student'S Health Information Form: (E.g. Frequency, Extent, Duration, Ongoing Therapy, Etc.)Document2 pagesStudent'S Health Information Form: (E.g. Frequency, Extent, Duration, Ongoing Therapy, Etc.)Susan Loida SorianoPas encore d'évaluation
- Petrosea Klinik Medical Services AgreementDocument29 pagesPetrosea Klinik Medical Services AgreementChaqhim YvciPas encore d'évaluation
- Rebekah Antoine: WORK EXPERIENCEDocument6 pagesRebekah Antoine: WORK EXPERIENCEapi-416398178Pas encore d'évaluation
- Ess 7Document4 pagesEss 7api-582020074Pas encore d'évaluation
- B.Sc. Handbook 2018-21Document59 pagesB.Sc. Handbook 2018-21Manisha NishaPas encore d'évaluation
- ASHP Guidelines On PNTCDocument10 pagesASHP Guidelines On PNTCNosheen KhizarPas encore d'évaluation
- NEW m1m2 Reporting FormDocument24 pagesNEW m1m2 Reporting FormDeyeck Verga100% (8)
- IRMNCH Nutrition ServicesDocument26 pagesIRMNCH Nutrition ServicesAftab AlmaniPas encore d'évaluation