Académique Documents
Professionnel Documents
Culture Documents
Neonatal Immunology
Transféré par
Rizwan AhmedCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Neonatal Immunology
Transféré par
Rizwan AhmedDroits d'auteur :
Formats disponibles
NEONATAL IMMUNOLOGY
CATEGORY: IMMUNE DEVELOPMENT
Neonatal Immunology
John Tregoning, St Georges University of London, UK
Introduction
The reduction in immune response leads to increased susceptibility to pathogens and to reduced
responses to vaccines that are effective in adults, necessitating research on infant-specific
formulations. The altered function of the neonatal immune response may also influence the
development of asthma and allergy in later life.
Importance
Five million infants die in the first year of life, 1.5 million of these deaths are due to infection. The
most common causes are respiratory infection and diarrhoea. Sadly, current vaccines are not as
effective in early life as they are in adulthood.
Development of the immune system
In many ways the immune system we are born with is the product of the immune environment
during pregnancy. In order to maintain the foetus the mother needs to ignore the foetal alloantigens
(half of the antigens being of paternal, and therefore of foreign origin). This leads to a scenario of
immunosuppression/regulation during pregnancy and this carries over into early life. (For more
about cellular development see: T-cell development in the thymus).
Transfer of protection from mother-to-child
The main component of immune protection transferred from mother to child is antibody. This is
transferred across the placenta to the foetus using the FcRn (neonatal Fc receptor). Antibody is
also transferred to the infant via breast milk. The main immunoglobulin class transferred is IgA, the
transferred IgA works at mucosal surfaces, where it is able to prevent pathogen entry. However
other important factors are transferred, including complement and commensal bacteria which
may provide protection against asthma and allergy in later life (see: Complement system).
Features of the neonatal immune system
Pattern recognition: Neonatal responses to pathogen associated molecular patterns (PAMPs) are
reduced compared to adults. However pattern recognition receptor (PRR)-expression levels are
similar. It appears that the molecules that transduce the signal (for example interferon response
factor 3 IRF3) have reduced function. This leads to reduced production of key inflammatory
mediators, for example interleukin-12 (IL-12) and interferon- (IFN). PRR function increases over
time, and the increase in capacity occurs in proportion to time since birth rather than gestational
age, suggesting that it is controlled by exposure to the environment and removal of maternal
influence.
Continued next page
The copyright for this work resides with the author
Like many other systems in the body, the immune system is not fully functional at birth and
therefore we are at an increased risk of infection. At the same time, the act of being born moving
from the sterile environment of the womb to the wider world, exposes us to a whole range of
pathogens that we have never encountered and have no protection against. To supplement this
period of immune immaturity and reduce the risk of infection, the mother transfers passive
protection to the child, mainly in the form of antibody.
The immune response in early life is dampened compared to adults. This in part is caused by the
immunosuppressive environment of the womb. Speculatively though it may also be an adaption to
the exposure to larges amounts of new antigens in early life. The immune response is carefully
regulated to ensure appropriate levels of immune response but avoiding inflammatory responses to
benign or harmless antigens. Since there are more new antigens in early life, it may be that the
response is skewed to suppression.
NEONATAL IMMUNOLOGY
CATEGORY: IMMUNE DEVELOPMENT
Neonatal Immunology
cont.
T-cell response: There is a well-documented skewing of the neonatal T-cell response towards T
helper 2 (Th2). This is associated with the reduction in IL-12 and IFN production by neonatal
antigen-presenting cells (APC). This may have an effect on the immune response to antigens seen
in early life possibly inducing an allergic type response.
B-cell response: Antibody production in early life is reduced. In particular the antibody response to
polysaccharide antigens is reduced. This is a particular problem with regards to bacterial infections,
to which newborn children are highly susceptible. This failure to produce antibody is associated
with several factors including reduced T cell help, fewer follicular dendritic cells and germinal
centres and reduced signalling through the CD40 ligand family members.
Downstream effects of the neonatal immune response
The immaturity of the neonatal immune response has an effect on three important areas:
1. Increased susceptibility to infection. The recognition of infectious agents is reduced in early life
and it is therefore easier for a pathogen to invade the host. Neonates are also less experienced so
have no immune memory against infection.
2. Decreased vaccine efficacy. In a similar fashion to infection, reduced recognition of vaccine
antigens as foreign means that induction of protective memory responses to vaccines are reduced.
There is also an effect of maternally derived antibody which may mask key epitopes of the vaccine.
3. Development of asthma and allergy. The Th2 skewing of the T cell response is hypothesised to
drive the development of allergic responses to antigen in early life.
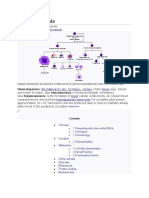
Input
Transduction
Harmless
Antigens Pathogens
Self
Vaccine
Antigens
Antigen
Pattern Recognition
Receptors (PRR) sense
PAMPS
Neonatal APC
Decreased Increased
Vaccine
Pathogen
Efficacy
Load
Sensing of
pathogens by
neonatal PRR is
compromised
kew
Downstream Effect
e
ns
po
s
Re
Reduced
Adaptor
Function
2S
lper
T he
After recognising pathogen,
the signal is passed on via
adaptor proteins
ed
uc
d
Re
Cells exposed to a
range of previously
unseen antigens.
Benign antigens need
to be tolerised and
pathogenic antigens
should initiate an
immune response
Asthma
Allergy
Autoimmunity
This altered PRR
function leads to
various
downstream
effects
Figure 1. Downstream effects of reduced antigen presenting cell function in early life. The neonatal immune
system is exposed to a large number of previously unseen antigens. The majority of these antigens are benign and
therefore should be tolerised but some are dangerous and therefore should induce an immune response. The
neonatal antigen presenting cells (APC) have reduced recognition of antigens regardless of source (self, benign,
pathogenic, vaccine). This is mediated at the level of pattern recognition receptors (PRR) or their adaptor molecules.
This leads to reduced immune responses to these antigens and has an impact on vaccine efficacy, disease
susceptibility and, possibly by skewing responses to Th2, the development of asthma and allergy.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Test Bank For Human Anatomy 9th Edition by MartiniDocument31 pagesTest Bank For Human Anatomy 9th Edition by MartiniAnthony Cohen100% (38)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- JIPMER MBBS BIOCHEMISTRYDocument18 pagesJIPMER MBBS BIOCHEMISTRYAsish Geiorge100% (1)
- BiorefinaryDocument6 pagesBiorefinaryRizwan AhmedPas encore d'évaluation
- Agglutination: Antibody Binding to Particles Causes ClumpingDocument19 pagesAgglutination: Antibody Binding to Particles Causes ClumpingRizwan AhmedPas encore d'évaluation
- FPSC AdvertDocument6 pagesFPSC AdvertFatima AhmedPas encore d'évaluation
- F.4 111 2015 - 07 04 16 PSDocument3 pagesF.4 111 2015 - 07 04 16 PSRizwan AhmedPas encore d'évaluation
- Cells 08 00724Document13 pagesCells 08 00724meltwithsnow163.comPas encore d'évaluation
- Pathogenesis of Autoimmune Disease: NephrologyDocument16 pagesPathogenesis of Autoimmune Disease: NephrologyHector PonsPas encore d'évaluation
- Overview of Complement Activation and RegulationDocument14 pagesOverview of Complement Activation and RegulationAnna SkrobińskaPas encore d'évaluation
- D652-Kowshik Kumar MDocument89 pagesD652-Kowshik Kumar MDr osama khamisPas encore d'évaluation
- Cells: Neurons: © Thomas Deerinck/Visuals Unlimited, IncDocument28 pagesCells: Neurons: © Thomas Deerinck/Visuals Unlimited, IncCierre WesleyPas encore d'évaluation
- UEP Biochemistry Module 1 IntroductionDocument24 pagesUEP Biochemistry Module 1 IntroductionCent VinPas encore d'évaluation
- Chemical Compounds R and RDocument1 pageChemical Compounds R and RchobynetPas encore d'évaluation
- List Down The Types of Connective Tissues and Their FunctionsDocument3 pagesList Down The Types of Connective Tissues and Their FunctionsZahir Jayvee Gayak IIPas encore d'évaluation
- Biology Olympiad Exam Syllabus (Final)Document4 pagesBiology Olympiad Exam Syllabus (Final)NumayrPas encore d'évaluation
- 04 - 2reproduction in ProtozoaDocument5 pages04 - 2reproduction in ProtozoaDipankar RoyPas encore d'évaluation
- Chapter 2 - Biology F4 (Cell)Document35 pagesChapter 2 - Biology F4 (Cell)Ismail ZuePas encore d'évaluation
- First Publication To Describe A Protocol For The Liquid Storage ofDocument4 pagesFirst Publication To Describe A Protocol For The Liquid Storage ofedilainePas encore d'évaluation
- MOLECULAR BASIS OF CANCERDocument29 pagesMOLECULAR BASIS OF CANCERdian.esterinaPas encore d'évaluation
- Glycolysis: Biochemistry of MetabolismDocument47 pagesGlycolysis: Biochemistry of MetabolismDozdiPas encore d'évaluation
- Cosmeceutical Peptides in The Framework of Sustainable Wellness EconomyDocument8 pagesCosmeceutical Peptides in The Framework of Sustainable Wellness EconomyNgọc NguyễnPas encore d'évaluation
- Centriole and Centrosome Structure and FunctionsDocument11 pagesCentriole and Centrosome Structure and FunctionsavishiPas encore d'évaluation
- Lipid DropletsDocument2 pagesLipid DropletsAaronmiguel27Pas encore d'évaluation
- Cell DivisionDocument48 pagesCell DivisionMichaelPas encore d'évaluation
- EicosanoidsDocument4 pagesEicosanoidsFrancis GathiraPas encore d'évaluation
- Experiment 1 - Staining OnionDocument5 pagesExperiment 1 - Staining OnionFatimatuzzahra' Binti Hardiyono FISPas encore d'évaluation
- ABO Blood Grouping Cbsebiology4uDocument14 pagesABO Blood Grouping Cbsebiology4uRahit BiswasPas encore d'évaluation
- Cell Division Is The Basis of Reproduction For Every OrganismDocument3 pagesCell Division Is The Basis of Reproduction For Every OrganismAlliah MendozaPas encore d'évaluation
- Bais Manish DVM PHD Nov 23sDocument3 pagesBais Manish DVM PHD Nov 23smanish.bais114017Pas encore d'évaluation
- Haematopoiesis: Jump To Navigation Jump To SearchDocument20 pagesHaematopoiesis: Jump To Navigation Jump To SearchJennie KimPas encore d'évaluation
- Endocrine 1 PageDocument3 pagesEndocrine 1 PagetimbitPas encore d'évaluation
- 1 WS1 Structure of ChromosomeDocument2 pages1 WS1 Structure of Chromosomegajendra. khandelwalPas encore d'évaluation
- Effects of Citicoline On Phospholipid and Glutathione Levels in Transient Cerebral IschemiaDocument6 pagesEffects of Citicoline On Phospholipid and Glutathione Levels in Transient Cerebral IschemiaMuhammad Ilham FarizPas encore d'évaluation
- Ibo (The International Biology Olympiad)Document6 pagesIbo (The International Biology Olympiad)RadpandjiPas encore d'évaluation