Académique Documents
Professionnel Documents
Culture Documents
Endodontic Topics Volume 31 Issue 1 2014 (Doi 10.1111/etp.12066) Baba, Nadim Z. Goodacre, Charles J. - Restoration of Endodontically Treated Teeth - Contemporary Concepts and
Transféré par
ardeleanoanaTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Endodontic Topics Volume 31 Issue 1 2014 (Doi 10.1111/etp.12066) Baba, Nadim Z. Goodacre, Charles J. - Restoration of Endodontically Treated Teeth - Contemporary Concepts and
Transféré par
ardeleanoanaDroits d'auteur :
Formats disponibles
bs_bs_banner
Endodontic Topics 2014, 31, 6883
All rights reserved
2014 John Wiley & Sons A/S.
Published by John Wiley & Sons Ltd
ENDODONTIC TOPICS
1601-1538
Restoration of endodontically
treated teeth: contemporary
concepts and future perspectives
NADIM Z. BABA & CHARLES J. GOODACRE
The concept of using a root for the restoration of a missing crown is not new. Through continuous research, our
understanding of the causes of failure has improved. Recent research on endodontically treated teeth has changed
contemporary views concerning some principles while consolidating others. Clinical success in restoring
endodontically treated teeth depends on our ability to use the latest materials available in conjunction with sound
clinical methods. A number of articles have discussed the major factors that play a key role in the long-term
survival of endodontically treated teeth and associated restorations. The purpose of this article is to identify key
principles that affect tooth and restoration survival and to present expectations regarding optimal future solutions
for the long-term retention of endodontically treated teeth.
Received 23 September 2014; accepted 2 October 2014.
Various methods and materials have been proposed
over the years for restoring pulpless teeth (13). Root
fractures and other difficulties encountered with these
early treatments led to the development of cast post
and cores that continue to be used today. Recently,
in response to an increased demand for esthetic allceramic restorations, a variety of non-metallic
prefabricated tooth-colored post systems have been
introduced as an alternative to metal posts. Today, the
prosthodontic and endodontic aspects of restoring
endodontically treated teeth (ETT) have appreciably
advanced and a significant body of scientific
knowledge on which to base our clinical treatment
decisions
is
available.
However,
retaining
endodontically treated teeth throughout life requires
careful restoration and adherence to available
evidence.
Although the collaboration between different
specialties coupled with modern therapies allows
patients to retain severely compromised teeth for
longer periods of time, the restoration of such teeth
remains a challenge. Despite a number of innovations
and decades of research on posts, failures can still
68
occur when endodontically treated teeth are restored
(Fig. 1) (4). Fortunately the failure rate is relatively
low, but it could be even lower. As professionals,
it is our obligation to do everything possible to
minimize complications. Some of the post
complications encountered clinically are pos
loosening, root fracture (Fig. 2), endodontic failure
(Fig. 3), root perforation (Fig. 4), post fracture
(Fig. 5), caries, and periodontal failure. The most
common post complications have been identified as
post loosening and root fracture (4). Several authors
(510) discussed the multifactorial origins of the
causes of cracks and fractures in ETT. Loss of tooth
structure, the use of endodontic irrigants and
instrumentation, a reduced level of proprioception,
changes in dentin, and the restorative procedures are
the main factors proposed as causes of fracture (i.e.
post placement). In addition, different variables, such
as the arch position, the presence of opposing occlusal
contacts, periodontal tissue support, endodontic
status, and the amount of remaining dentin, play an
important role in the prognosis of ETT. A number of
articles have discussed the major factors that play a key
Restoration of endodontically treated teeth: contemporary concepts and future perspectives
a
Fig. 1. (a) A separated instrument within the mesial root canal of a mandibular right second molar. (b) Perforation
of the roots of a mandibular second molar, the result of post space preparation with instruments not held parallel to
the root canals. (c) A radiograph of a fractured maxillary lateral with a prefabricated non-metallic post.
role in the long-term survival of endodontically
treated teeth and associated restorations (11,12). The
purpose of this article is to identify key principles that
affect tooth and restoration survival and to present
expectations regarding optimal future solutions for the
long-term retention of endodontically treated teeth.
Effect of endodontic treatment on
the tooth
Fig. 2. Radiograph displaying a very short post in the
root of a maxillary first bicuspid that caused root
fracture.
When performing root canal therapy, the access cavity
opening causes loss of coronal tooth substance (Fig. 6)
(13,14). In addition, root canal treatment as well as
retreatment can cause damage to the root dentin. A
study looked at the influence of retreatment
procedures on the appearance of defects on the root
canal walls (15). It was concluded that retreatment
caused more defects in dentin than initial treatment.
During initial treatment, craze lines and cracks can be
formed in the dentin. The latter can develop into
69
Baba & Goodacre
Fig. 3. Radiograph displaying an inadequate root canal
therapy that caused a radiolucent apical lesion.
Fig. 5. Radiograph of a fractured maxillary lateral
incisor with a prefabricated screw post.
Fig. 4. Inappropriate placement of a screw post created
a perforation in the pulpal floor of the maxillary first
molar.
Fig. 6. Excessive enlargement of the access cavity
following root canal therapy.
fractures during retreatment and under the functional
stresses applied to the tooth during chewing and
parafunction. Several studies (16,17) compared the
effect of hand files and rotary files on dentin after canal
preparation. They concluded that rotary instruments
caused more dentinal defects, such as craze lines and
cracks, which possibly could develop into fractures
after restorative treatment.
Several methods have been proposed for detecting
cracks and fractures when they are not visible clinically.
The most commonly used techniques are transillumination (Fig. 7), occlusal tests, endodontic
microscopes, dyes, and quantitative percussion
diagnostics (1822). Recently, cone beam computed
tomography (CBCT) has been suggested as a tool to
diagnose fractures, perforations, or suspected cracks
(23,24).
Another factor that could affect the mechanical
properties of dentin is the use of endodontic irrigants
70
Restoration of endodontically treated teeth: contemporary concepts and future perspectives
a
d
c
Fig. 7. (a) Clinical photo shows a crack line on the occlusal surface of a maxillary first molar. (b) The amalgam
restorations were replaced with new ones and the tooth was prepared to receive a partial coverage restoration. (c) A
trans-illumination picture shows the crack running between the amalgams across the transverse ridge. (d) Occlusal
view of the 3/4 crown showing that it encompassed the buccal cusps.
and medications (2527). Following contact with
these products, chemical degradation of dentin is
evident and the dentin becomes weaker because of a
reduction in microhardness. However, the degree of
dentin change is related to the amount and duration of
contact between products and dentin. Other irrigation
agents such as mineral trioxide aggregate and bioactive
glass do not seem to affect the flexural strength of root
dentin (2829).
In addition to the use of irrigants and medications,
Ferrari et al. showed that 10 to 12 years after
endodontic treatment, there is progressive degradation
of the demineralized collagen matrices (30). The aging
dentin becomes sclerotic and exhibits very limited
yielding before failure. The fracture toughness is lower,
and the stressstrain response is characteristic of brittle
behavior (31). Most importantly, there is a reduction in
the stiffness and elasticity of dentin and a reduced
resistance to crack propagation (6,13,32,33).
These factors can affect the prognosis of the
endodontically treated tooth. As a consequence,
practitioners should strive to use restorative materials
with properties similar to that of dentin, along with
sound clinical principles to counteract the changes in
71
Baba & Goodacre
mechanical properties of dentin as well as the loss of
tooth structure following root canal treatment (RCT).
A systematic review investigated tooth survival after
RCT (34); 14 studies met the inclusion criteria. Four
key factors were identified as enhancing the survival
of teeth after RCT: the presence of interproximal
contacts, no plans for using the treated teeth as
abutments for fixed or removable partial dentures,
tooth type, and crown restoration.
The restorative dentist plays an important role in the
success and failure of endodontic treatment. Before
endodontic treatment is contemplated, the restorative
dentist should: (i) have an overall treatment plan
for the patient based on their chief complaint
and desires; (ii) assess the restorability of the tooth,
which may involve the removal of all existing
restorations and/or caries to determine the tooths
restorability, and examine the tooth for the presence of
cracks; and (iii) evaluate the need for any periodontal
treatment and appraise the periodontal prognosis of
the tooth to be restored. After endodontic treatment
has been performed, the dentist should minimize
recontaminating the root canal system.
A study by Balto et al. (35) found that all of the
provisional materials they tested in post-prepared root
canals failed to prevent coronal leakage when used for
an average of 30 days. Similarly, delayed placement of
the definitive restoration had an impact on the
prognosis of ETT. These teeth had a higher success
rate when they were restored with a definitive
restoration than with a provisional coronal access
restoration (36). An in vitro study looking at bacterial
penetration of coronally unsealed endodontically
treated teeth found that defective restorations could
cause reinfection of the root canal system within 19
days (37). A combination of poor endodontic
treatment and poor restoration caused a high failure
rate for ETT (38). In comparing endodontic
treatment quality with restoration quality, Tronstad
et al. (39) found that the quality of root canal
treatment is more crucial than that of the coronal
restoration for the survival of ETT.
A well-fitting provisional restoration followed by a
post and core and a definitive coronal restoration
should be planned and cemented in as short a time as
possible. Avoiding reinfection of the root canal and
preventing mechanical failures such as fractures
enhances the survival of ETT (40,41). In a
retrospective study, Willershausen et al. (42) evaluated
72
775 ETT in 508 patients and found a higher survival
rate for teeth restored within 2 weeks.
If immediate restoration of the tooth is not possible,
it is recommended to protect the root canal system by
sealing the orifice of the canals and the floor of the
pulp chamber with intracoronal barriers (4345).
Among the suggested materials to be used are flowable
composite resin, mineral trioxide aggregate (MTA),
glass ionomer, fissure sealant, and conventional
restorative composite resin. This type of treatment has
mostly been suggested to protect the root canal system
from contamination during the provisionalization
period.
The use of digital impressions and CAD/CAM
fabrication can help the restorative dentist to seal the
filled root canal system and protect the tooth as soon
as possible, either with a provisional or definitive
restoration.
Principles that enhance success
when restoring endodontically
treated teeth
The prognosis of ETT does not depend solely on the
quality of the RCT or the quality and time required
for definitive restoration (38,46). Survival of the
restoration also depends on several basic principles
that affect tooth and restoration survival.
Cuspal coverage
ETT can benefit from the placement of crowns. An
epidemiological study in a large patient population
found that while 97% of teeth were retained in the oral
cavity 8 years after initial non-surgical endodontic
treatment, an analysis of the teeth that were extracted
(< 3%) revealed that 85% of them had no full coronal
coverage (47). Aquilino & Caplan reported that ETT
with cuspal coverage had a six times greater rate of
survival than those without cuspal coverage (48).
Another prospective study (49) of the factors affecting
outcomes of non-surgical RCT found that ETT which
were restored with a crown had a better survival rate
than those that were not. Vire (50), in a study of failed
teeth, demonstrated that ETT without crowns were
lost after an average time of 50 months whereas ETT
with crowns were lost after an average of 87 months.
In a systematic review, Stavropolou & Koidis (51)
concluded that ETT restored with crowns had a
Restoration of endodontically treated teeth: contemporary concepts and future perspectives
higher long-term survival rate compared to those not
restored with crowns (Figs. 8 and 9). A retrospective
cohort study found that the 5-year survival rate of
teeth without cuspal coverage was 36% (52). However,
while crowns significantly improved the success of
endodontically treated posterior teeth, they did not do
so for anterior teeth (53). Intact endodontically
treated anterior teeth only require a crown when they
are weakened by large or multiple existing restorations
or when they require significant changes to their form
or color that are not manageable by conservative
restorations.
Fig. 8. Occlusal view showing the fractured buccal cusp
of an endodontically treated mandibular left first molar
without cuspal coverage.
Fig. 9. Fracture of the palatal cusp of a maxillary right
first molar with significant amount of tooth structure
missing restored with a composite resin and without
cuspal coverage.
Several studies (5456) indicated that ETT with
intact coronal surfaces (except for the access opening)
can be successfully restored using composite resin
restorations. However, the survival rate of ETT will
likely be lower when ETT have lost excessive amounts
of tooth structure. Sedgley & Messer (57) concluded
that the loss of axial dentin walls weakens the teeth.
Composite resin is a popular core buildup material
because of its ease of use, and the possibility of
preparing and finishing it immediately (46). Some
clinicians consider composite resin as an esthetic
replacement for cuspal coverage crowns. Composite
resin appears to be an acceptable core material when
substantial coronal tooth structure remains but a poor
choice when a significant amount of tooth structure is
missing (56,58,59). The authors believe that if less
than 50% of the coronal tooth structure of an
endodontically treated tooth remains, a post should be
used to retain the core material. The choice of buildup
material depends on the remaining adjacent teeth,
occlusion, and the planned definitive restoration. One
disadvantage of composite resin is that it is
dimensionally unstable (60). The setting shrinkage
during polymerization causes stress on the adhesive
bond resulting in cuspal strain with a disruption of the
bond, and gap formation that might contribute to
long-term bond failure followed by microleakage and
recurrent caries (54,55). The amount of shrinkage is
related to the amount of filler content in the
composite resin. A reduced amount of filler will cause
greater shrinkage. For this reason it is necessary to
avoid using flowable composite resins as buildup
materials because of their low filler content and their
reduced mechanical properties (61).
A recent systematic review looking at the effects of
the restoration of ETT by crowns versus conventional
filing materials concluded that there is no evidence to
support or refute the effectiveness of crowns over
filling materials for the restoration of ETT (46).
After considering the available contrasting data, the
authors acknowledge the potential benefits of using
composite resin to restore posterior teeth that are
intact except for a conservative access opening.
However, when occlusal wear, heavy forces, or parafunctional habits are present in the mouth, more
clinical data are required to determine the long-term
survival of these teeth when large composite resin
restorations are present. For this reason, we
recommend that endodontically treated teeth which
73
Baba & Goodacre
have been previously restored and weakened by prior
tooth structure removal be restored with a crown that
encompasses the cusps. Conversely, it may be possible
to avoid crowns on some previously restored posterior
teeth with only a conservative access opening and
little-to-no wear present that would indicate the
presence of detrimental occlusal forces.
It is highly recommended that a rubber dam be
placed when a composite resin is used as the core
buildup material. Composite resin is a technically
demanding material that requires careful adherence to
material-handling protocols. To ensure success, the
use of low-shrinkage composite resin (62), the buildup
of the core in small increments (63), and the use of
liners (64) has been advocated.
The high demand for esthetic restorations, the need
for an occlusal material stiffer than dentin, and the
benefit of covering the cusps has caused some
clinicians to use all-ceramic onlays and crowns as a
conservative and effective treatment modality to
restore ETT (6567). A suggested conservative
technique to restore ETT is the use of an endocrown
(6870). This restoration consists of an onlay or
crown with the core material in a single unit (Fig. 10).
The core material engages in a cavity prepared into the
pulp chamber. A study by Magne et al. (68) found that
an endocrown fabricated from a resin nanoceramic has
a favorable mode of failure when ETT with no buildup
material are used. These crowns were found to be
more resistant to failure than teeth that had been
restored with a post, composite resin core, and a
ceramic crown (69,70). It is unknown whether this
type of conservative restoration will produce the same
problems as the one-piece crownpost combinations
made using metal. Also, the impact of their subsequent
removal upon structure integrity is unknown.
Tooth preservation
Maximum preservation of coronal and radicular tooth
structure is a guiding principle for the restoration of
ETT. As clinicians we should preserve intact tooth
structure whenever possible in order to maintain an
adequate retention and resistance form of the final
restoration. The position of the tooth in the arch,
the presence of opposing occlusal contacts, the
periodontal tissue support, the endodontic status, and
the amount of remaining dentin aids in selecting
the appropriate material for the definitive restoration.
The authors believe that gold onlays or crowns are
excellent restorations where esthetics is not of major
concern, on teeth with limited interocclusal space, and
when restoring heavy bruxers.
Cervical ferrule
Fig. 10. All-ceramic restoration consisting of a crown
with a core material in a single unit.
74
A ferrule can be established by the crown
encompassing sound tooth structure (Fig. 11) (71
76). The data indicates that cervical ferrules increase
the tooths resistance to fracture (71,72,77). In spite
of the data supporting the benefit of cervical ferrules,
not all practitioners recognize their value. A survey
published by Morgano et al. (78) evaluated the
percent of respondents who felt that a ferrule increased
a tooths resistance to fracture: 56% of general dentists,
67% of prosthodontists, and 73% of board-certified
prosthodontists felt that core ferrules increased a
tooths fracture resistance.
Different lengths and forms of the ferrule have been
studied (71,73,74,79) and are essential factors for
the success of the ferrule effect. When possible,
encompassing 2.0 mm of intact tooth structure
around the entire circumference of a core creates an
optimally effective crown ferrule. Grasping larger
amounts of tooth structure further enhances ferrule
effectiveness. The amount of tooth structure engaged
Restoration of endodontically treated teeth: contemporary concepts and future perspectives
a
Fig. 11. A ferrule will be created by the overlying crown
engaging tooth structure. The final restoration is at least
2 mm apical to the junction core/tooth.
by the overlying crown appears to be more important
than the length of the post in increasing a tooths
resistance to fracture.
If insufficient cervical tooth structure remains to
develop a ferrule, surgical crown lengthening or
orthodontic extrusion should be considered to expose
more tooth structure.
In some situations where teeth have been extensively
restored, have been subject to trauma, or have
substantial caries, it will be difficult to obtain a ferrule.
In such cases it may be prudent to extract the tooth
and replace it with an implant and crown. Extraction
of ETT may also be required when crown lengthening
would create an unacceptable esthetic environment or
produce a furcation defect, or when a short root is
present that would not permit an appropriate post
length to be developed (80).
Studies have shown that a uniform ferrule produces
significantly greater fracture resistance than a nonuniform ferrule (74,76,81), with the greatest variation
in failure load associated with the absence of portions
of the crown ferrule. The presence of a 2-mm ferrule
on the facial, lingual, distal, and mesial surfaces of the
tooth produces the most favorable resistance to tooth
fracture and decreases the weakening effect of a post
(Fig. 12) (76).
Need for a post
Studies have compared the fracture resistance of
endodontically treated extracted teeth without posts
Fig. 12. Post and crown loosened from maxillary canine
a few months after placement. (a) Both the post/
prefabricated post and the crown came off. (b) Clinical
photo shows the absence of cervical tooth structure
(ferrule) for retention of the crown.
or crowns with the fracture resistance of teeth restored
with posts and cores and crowns. Maxillary incisors
without posts resisted higher failure loads than the
other groups with posts and crowns (82) and
mandibular incisors with intact natural crowns
exhibited greater resistance to transverse loads than
teeth with posts and cores (83). These studies have
shown no evidence of a strengthening reinforcement
effect of posts. However, several studies showed a
relatively high failure rate of endodontically treated
teeth that were restored with a composite resin filling
without a post (8486). The failures occurred when
the teeth had small and curved roots. A study by Salvi
et al. (87) evaluated ETT restored with and without
post and cores in a specialist practice. They concluded
that there was no significant difference between teeth
restored with or without posts provided that at least
two-thirds of the dentin remained. They also found
75
Baba & Goodacre
a
Fig. 13. (a) Radiograph of a broken mesial root of an endodontically treated mandibular right molar restored with
a crown and no post. (b) Extracted tooth showing the fractured mesial root.
that 11 out of 13 failures in mandibular molars were
due to fractures (Fig. 13).
Clinical studies have failed to provide definitive
support for the concept that posts strengthen
endodontically treated teeth (53,85,87). An analysis of
data from multiple clinical studies noted that 3% of
teeth with posts fractured with no evidence that posts
enhanced the survival of teeth (88). Posts have had
little enhancing effect on the clinical survival of fixed
partial denture abutments, but they did improve
the clinical survival of removable partial denture
abutments compared to endodontically treated
abutments where no posts were used (53).
Because clinical and laboratory data indicate teeth
are not strengthened by posts, their purpose is for the
retention of a core that will provide adequate retention
and support for the definitive crown or prosthesis.
When enough tooth structure is present in an
endodontically treated molar, there is absolutely no
need for a post (Fig. 14). The presence of adequate
dentin coupled with no preparation of a post space
helps avoid weakening the tooth, eliminates the risk of
perforation during post preparation, and aids in
preventing the development of cracks that could be
detrimental to the ETT. In endodontically treated
molars, buildup materials usually have sufficient
retention from the pulp chamber, divergent coronal
portions of the root canals, and undercuts created in
the pulp chamber during removal of caries and RCT.
For endodontically treated anterior teeth and
premolars, if sufficient tooth structure remains to
76
Fig. 14. (a) Occlusal view of a maondibular second
molar showing the presence of enough tooth structure
to retain the core. (b) Radiograph of the root canal
treatment.
Restoration of endodontically treated teeth: contemporary concepts and future perspectives
retain the core, the use of a post is not required;
bonding a core buildup material to dentin is sufficient.
However, if a substantive amount of tooth structure is
missing in these teeth, a post is needed in order to
retain the core and optimize the resistance form. The
best prognosis is obtained when a 2-mm ferrule
encompasses intact tooth structure around the entire
circumference of the core no matter what type of post
is used. Because posts do not reinforce a tooth, they
should only be used when the core cannot be retained
by some other means.
Types and properties of posts
In recent years, prefabricated posts have become quite
popular and a wide variety of systems are now
available. In response to a need for tooth-colored
posts, several non-metallic posts such as zirconia, glass
fiber-reinforced epoxy resin (GFR), and ultra-high
polyethylene fiber-reinforced posts are available; early
data indicates that they can be acceptable alternatives
to metallic posts. However, gold alloys, titanium, and
chromecobalt are still clinically viable and are widely
used.
Among the non-metallic posts, GFR posts are the
most popular. They are available in different shapes:
cylindrical, cylindroconical, or conical. An in vitro
assessment of several GF post systems indicated that
parallel-sided GF posts are more retentive than tapered
GFR posts (89). These posts could be made from glass
or silica fibers (white or translucent) but the most
commonly used fibers are silica based. The matrix
for this post is an epoxy resin. The fibers are in the
vicinity of 14 m in diameter and uniformly
embedded in the epoxy resin matrix. The fibers are
stretched before injection of the resin matrix to
maximize the physical properties of the post. When
compared to metallic posts, GFR posts have a low
modulus of elasticity and are more flexible (90). This
flexibility induces more stress cervically, which, in the
case of minimal or no ferrule, causes a higher risk of
post fracture, debonding of the core, and loss of
retention of the post followed by microleakage and
secondary caries (Fig. 15). Several studies (91,92)
have determined that there is a 40% decrease in the
strength of GFR posts after thermocycling and cyclic
loading. In addition, contact of the post with oral
fluids (short- and long-term) reduced their flexural
strength. While failure with fiber posts might be less
Fig. 15. (a) A radiograph of a fractured mandibular
second premolar with a prefabricated non-metallic post.
(b) Crown with broken post.
likely to produce root fracture, post removal may
damage the root, and the cost to the patient versus
time of service before failure is a concern.
In contrast, metallic posts are stiffer than dentin and
can take more load than GFR posts. Their stiffness can
induce more stress apically, causing catastrophic root
fractures (Fig. 16). Similarly to GFR posts, metal posts
also undergo a process of cement failure during cyclic
loading (93). Metal posts have a longer lifespan than
GFR posts and they fracture less; but when they fail,
the failure is non-restorable (94).
A comprehensive review of the English literature was
conducted on evaluating the clinical performance of
GFP in order to seek evidence for the treatment of
teeth with non-metallic posts (95). Clinical research
articles showed that non-metallic posts have favorable
77
Baba & Goodacre
Fig. 16. A radiograph of a fractured maxillary second
premolar with a metallic prefabricated post.
mechanical and physical properties and the studies
presented with a wide range of reported failure
percentages, from 0% after a mean of 2.3 years to
11.4% after 2 years. Post debonding, post fracture,
crown debonding, and root fracture were the most
commonly reported complications. Post debonding
was reported in 16 of the 23 studies. A 10-year
prospective study on GFR posts found that the overall
failure rate of these posts was 37%, of which 11% were
due to post debonding (96). From these results, it can
be concluded that the failure might be due to
weaknesses in the bonding of composite resin to
the post and/or to the dentin. Studies (9799)
demonstrated that radicular dentin is different from
coronal dentin. It contains fewer tubules and forms a
thinner hybrid layer than coronal dentin. The efficacy
of bonding to radicular dentin could be compromised.
It is strongly recommended that chemical or dual-cure
composite resin cement be used to ensure complete
polymerization of the cement in the canal.
Another reason for post debonding could be the lack
of retention between the composite resin cement and
the surface of the GFR post. Studies have shown that
there is a low bond strength (5 to 6 MPa) between the
GFR posts and composite resin (100,101). Differences
exist among brands of GFR posts in term of structural
characteristics and fatigue resistance (102,103). GFR
posts could present with voids and irregularities within
the resin and discontinuity at the interface between the
fibers and the matrix. It is recommended to condition
the surface of GFR posts prior to cementation with
soft air abrasion (2 bars) and the application of silane
(104,105).
78
Post debonding could be due to the polymerization
shrinkage of the composite resin cement, the
technique-sensitive cementation process, the difficult
access and visibility during cementation, the lack of a
clear and universal cementation protocol, the lack of
ferrule effect, or an inadequate choice in the type of
post for the given clinical situation and tooth. The
wide range of failure percentages reported with GFR
posts may also be indicative of variations amongst
clinicians and differences in their experiences/
restorative techniques. It appears that more long-term
clinical data is needed in order to determine the
efficacy of fiber-reinforced posts.
A 10-year retrospective study of the survival rate of
teeth restored with metal prefabricated posts and cast
metal posts and cores found that their overall failure
rate was 15.4% and 17.4%, respectively (106). When
we compare these results to the high overall failure rate
of non-metallic post, the authors believe that the GFR
posts are not superior to metallic or cast posts.
There are challenges related to the use of cylindrical
prefabricated posts when restoring teeth with ovoid,
wide, or particularly tapered canals. The lack of
intimate adaptability of these posts to the tooth
structure compromises their retention in the canal.
In addition, the low success rate of GFR posts
encouraged researchers to look for alternative
materials to restore ETT. Polyethylene fiber-reinforced
(PFR) posts made out of ultrahigh-molecular weight
polyethylene woven fiber ribbon (Ribbond, Seattle,
WA) have been proposed. It is not a post and core in
the traditional sense. It is a polyethylene woven fiber
ribbon that is coated with a dentin bonding agent and
packed in the canal, where it is then light polymerized
into position (107). Another proposed material is a
customized glass-fiber post (108,109). Costa et al.
(108) compared the root fracture strength of singlerooted premolars restored with GFR posts to the ones
restored with customized GFR posts. They concluded
that the customized GFR posts did not show
improved fracture resistance or differences in failure
patterns when compared to GFR posts. Some authors
suggested combining PFR with a customized GFR
post to restore ETT (110). Custom-milled zirconia
posts have also been suggested as an alternative
material to GFR posts in anterior teeth where the use
of a custom post is indicated. An in vitro study
comparing a one-piece milled zirconia post and core
to different core systems concluded that the mean
Restoration of endodontically treated teeth: contemporary concepts and future perspectives
load-bearing capacity of the one-piece milled zirconia
post and core was comparable to that of a cast gold
post and core (111). One explanation as to why
these post behaved similarly to cast post and core is the
absence of an interface between the post and the core,
which eliminates the debonding of the core evidenced
with GFR posts and cores.
The authors believe that until more long-term
clinical data becomes available, fiber-reinforced resin
posts should be used with caution because of the wide
range of reported failure rates in available clinical
studies.
Future directions
In the future, we foresee that the advancement of
CAD/CAM technology, milling, and laser printing
along with an improvement in digital impression
technology will make it possible to more easily and
accurately fabricate customized post and cores from
several different materials. In addition, more
conservative endodontic treatment procedures are
likely to emerge and reduce the need for posts and
crowns. Pulpal regeneration procedures may even
eliminate or substantially reduce the need for the use
of crowns and posts and cores.
In future studies of ETT and new technologies, we
believe in vitro studies should be performed using
fatigue loading and chewing simulation conditions.
Summary
Based on this review of available evidence, the
following clinical recommendations are proposed:
1. When performing root canal therapy, the tooth
needs to be evaluated for the presence of cracks and
craze lines using several of the diagnostic tools
available. The restorability of the tooth needs to be
assessed along with the periodontal prognosis.
2. Following root canal therapy, the tooth needs to be
restored with a definitive restoration in as short a
time as possible. If immediate restoration is not
possible, it is recommended to seal the orifice of the
canals and the floor of the pulp chamber with
intracoronal barriers.
3. Crowns are not needed on many endodontically
treated posterior teeth to enhance their long-term
survival because their structural integrity is often
compromised. There is some data indicating
4.
5.
6.
7.
posterior teeth that are intact except for the access
opening can be satisfactorily restored with
composite resin rather than a crown. However, the
long-term success of this more conservative
treatment is not known in the presence of heavy
occlusal forces.
Posts weaken teeth and they should only be used
when the core cannot be adequately retained by
some other means.
When crowns are placed on endodontically treated
teeth, they should encompass 2.0 mm of tooth
structure apical to the core whenever possible since
crown ferrules increase the resistance of teeth to
fracture.
Until more long-term clinical data becomes
available, fiber-reinforced resin posts should be
used with caution due to the wide range of
reported failure rates in available clinical studies.
Procedures will become available that preserve or
regenerate pulp vitality and may reduce or even
eliminate the need for restorations. For those teeth
that need RCT, even more conservative endodontic
procedures will be developed; and when combined
with new materials it may not be necessary to place
crowns on these teeth. When posts are needed due
to tooth condition, digital technologies will make it
possible to fabricate customized posts and cores
from a variety of materials.
References
1. Prothero JH. Prosthetic Dentistry, 2nd edn. Chicago:
Medico-Dental Publishing, 1916: 1116, 11521162.
2. Harris CA. The Dental Art. Baltimore: Armstrong and
Berry, 1839: 305347.
3. Richardson J. A Practical Treatise on Mechanical
Dentistry. Philadelphia: Lindsay and Blakiston, 1880:
148149, 152153.
4. Goodacre CJ, Baba NZ. Restoration of endodontically
treated teeth. In: Ingle JI and Bakland LK, eds.
Endodontics, 6th edn. Toronto, Canada: BC Decker
Inc., 2008.
5. Meyenberg K. The ideal restoration of endodontically
treated teethstructural and esthetic consideration: a
review of the literature and clinical guidelines for the
restorative clinician. Eur J Esthet Dent 2013: 8:
238268.
6. Kishen A. Mechanisms and risk factors for fracture
predilection in endodontically treated teeth. Endod
Topics 2006: 13: 5783.
7. Bier CA, Shemesh H, Tanomaru-Filho M, Wesselink
PR, Wu MK. The ability of different nickeltitanium
79
Baba & Goodacre
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
80
rotary instruments to induce dentinal damage during
canal preparation. J Endod 2009: 35: 236238.
Goldsmith M, Gulabivala K, Knowles JC. The effect of
sodium hypochlorite irrigant concentration on tooth
surface strain. J Endod 2002: 28: 575579.
Perez F, Rouqueyrol-Pourcel N. Effect of a lowconcentration EDTA solution on root canal walls: a
scanning electron microscopic study. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod 2005: 99:
383387.
Randow K, Glantz PO. On cantilever loading of vital
and non-vital teeth. An experimental clinical study.
Acta Odontol Scan 1986: 44: 271277.
Baba NZ, Goodacre CJ, Daher T. The restoration of
endodontically treated teeth: the seven keys to success.
Gen Dent 2009: 57: 596603.
Baba NZ, Goodacre CJ. Key principles that enhance
success when restoring endodontically treated teeth.
Roots 2011: 7: 3035.
Reeh ES, Messer HH, Douglas WH. Reduction in
tooth stiffness as a result of endodontic and restorative
procedures. J Endod 1989: 15: 512516.
Gonzlez Lpez S, De Haro-Gasquet F, Vlchez-Daz
MA, Ceballos L, Bravo M. Effect of restorative
procedures and occlusal loading on cuspal deflection.
Oper Dent 2006: 31: 3338.
Shemesh H, Roeleveld AC, Wesselink PR, Wu MK.
Damage to root dentin during retreatment
procedures. J Endod 2011: 37: 6366.
Yoldas O, Yilmaz S, Atakan G, Kuden C, Kasan Z.
Dentinal microcrack formation during root canal
preparations by different NiTi rotary instruments
and the self-adjusting file. J Endod 2012: 38:
232235.
Liu R, Kaiwar A, Shemesh H, Wesselink PR, Hou B,
Wu MK. Incidence of apical root cracks and apical
dentinal detachments after canal preparation with hand
and rotary files at different instrumentation lengths.
J Endod 2013: 39: 129132.
Wright HM Jr, Loushine RJ, Weller RN. Identification
of resected root-end dentinal cracks: a comparative
study of transillumination and dyes. J Endod 2004: 30:
712715.
Rubinstein R. The anatomy of the surgical operating
microscope and operating positions. Dent Clin North
Am 1997: 41: 391413.
Slaton CC, Loushine RJ, Weller RN, Parker WH,
Kimbrough WF, Pashley DH. Identification of
resected root-end dentinal cracks: a comparative study
of visual magnification. J Endod 2003: 29: 519522.
Clark DJ, Sheets CG, Paquette JM. Definitive
diagnosis of early enamel and dentinal cracks based on
microscopic evaluation. J Esthet Restor Dent 2003: 15:
391401.
Sheets CG, Stewart DL, Wu JC, Earthman JC. An in
vitro comparison of quantitative percussion diagnostics
with a standard technique for determining the
presence of cracks in natural teeth. J Prosthet Dent
2014: 112: 267275.
23. Ozer SY. Detection of vertical root fractures of
different thicknesses in endodontically enlarged teeth
by cone beam computed tomography versus digital
radiography. J Endod 2010: 36: 12451249.
24. Shemesh H, Cristescu RC, Wesselink PR, Wu MK.
The use of cone-beam computed tomography and
digital periapical radiographs to diagnose root
perforations. J Endod 2011: 37: 513516.
25. Oliveira LD, Carvalho CA, Nunes W, Valera MC,
Camargo CH, Jorge AO. Effects of chlorhexidine and
sodium hypochlorite on the microhardness of root
canal dentin. Oral Surg Oral Med Oral Pathol Oral
Radiol Endod 2007: 104: e125128.
26. Sayin TC, Serper A, Cehreli ZC, Otlu HG. The effect
of EDTA, EGTA, EDTAC, and tetracycline-HCl with
and without subsequent NaOCl treatment on the
microhardness of root canal dentin. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod 2007: 104:
418424.
27. Ballal NV, Mala K, Bhat KS. Evaluation of the effect of
maleic acid and ethylenediaminetetraacetic acid on the
microhardness and surface roughness of human root
canal dentin. J Endod 2010: 36: 13851388.
28. Hatibovic-Kofman S, Raimundo L, Zheng L, Chong
L, Friedman M, Andreasen JO. Fracture resistance and
histological findings of immature teeth treated with
mineral trioxide aggregate. Dent Traumatol 2008: 24:
272276.
29. Marending M, Stark WJ, Brunner TJ, Fischer J,
Zehnder M. Comparative assessment of time-related
bioactive glass and calcium hydroxide effects on
mechanical properties of human root dentin. Dent
Traumatol 2009: 25: 126129.
30. Ferrari M, Mason PN, Goracci C, Pashley DH, Tay FR.
Collagen degradation in endodontically treated teeth
after clinical function. J Dent Res 2004: 83: 414419.
31. Kinney JH, Nalla RK, Pople JA, Breunig TM, Ritchie
RO. Age-related transparent root dentin: mineral
concentration, crystallite size, and mechanical
properties. Biomaterials 2005: 26: 33633376.
32. Kruzic JJ, Nalla RK, Kinney JH, Ritchie RO. Crack
blunting, crack bridging and resistance-curve fracture
mechanics in dentin: effect of hydration. Biomaterials
2003: 24: 52095221.
33. Nalla RK, Kinney JH, Ritchie RO. On the fracture of
human dentin: is it stress- or strain-controlled?
J Biomed Mater Res A 2003: 67: 484495.
34. Ng YL, Mann V, Gulabivala K. Tooth survival
following non-surgical root canal treatment: a
systematic review of the literature. Int Endod J 2010:
43: 171189.
35. Balto H, Al-Nazhan S, Al-Mansour K, Al-Otaibi M,
Siddiqu Y. Microbial leakage of Cavit, IRM, and Temp
Bond in post-prepared root canals using two methods
of gutta-percha removal: an in vivo study. J Contemp
Dent Pract 2005: 6: 5361.
36. Safavi KE, Dowen WE, Langeland K. Influence of
delayed coronal permanent restoration on endodontic
prognosis. Endod Dent Traumatol 1987: 3: 187191.
Restoration of endodontically treated teeth: contemporary concepts and future perspectives
37. Torabinejad M, Ung B, Kettering JD. In vitro bacterial
penetration of coronally unsealed endodontically
treated teeth. J Endod 1990: 16: 566569.
38. Ray HA, Trope M. Periapical status of endodontically
treated teeth in relation to the technical quality of the
root filling and the coronal restoration. Int Endod J
1995: 28: 1218.
39. Tronstad L, Asblornsen K, Doving L, Pedersen I,
Eriksen HM. Influence of coronal restorations on the
periapical health of endodontically treated teeth.
Endod Dent Traumatol 2000: 16: 218221.
40. Lynch CD, Burke FM, N Rordin R, Hannigan A.
The influence of coronal restoration type on the
survival of endodontically treated teeth. Eur J
Prosthodont Restor Dent 2004: 12: 171176.
41. Tang W, Wu Y, Smales RJ. Identifying and reducing
risks for potential fractures in endodontically treated
teeth. J Endod 2010: 36: 609617.
42. Willershausen B, Tekyatan H, Krummenauer F,
Briseno Marroquin B. Survival rate of endodontically
treated teeth in relation to conservative vs post
insertion techniquesa retrospective study. Eur J Med
Res 2005: 10: 204208.
43. Sauia TS, Gomes BP, Pinheiro ET, Zaia AA, Ferraz
CC, Souza-Filho FJ. Microleakage evaluation of
intraorifice sealing materials in endodontically treated
teeth. Oral Surg Oral Med Oral Pathol Oral Radiol
Endod 2006: 102: 242246.
44. Malik G, Bogra P, Singh S, Smara RK. Comparative
evaluation of intracanal sealing ability of mineral
trioxide aggregate and glass ionomer cement: an in
vitro study. J Conserv Dent 2013: 16: 540545.
45. Bayram HM, Celikten B, Bayram E, Bozkurt A. Fluid
flow evaluation of coronal microleakage intraorifice
barrier materials in endodontically treated teeth. Eur J
Dent 2013: 7: 359362.
46. Fedorowicz Z, Carter B, de Souza RF, Chaves CA,
Nasser M, Sequeira-Byron P. Single crown versus
conventional fillings for the restoration of root filled
teeth. Cochran Database Syst Rev 2012: 5: CD
009109.
47. Salehrabi R, Rotstein I. Endodontic treatment
outcomes in a large patient population in the USA: an
epidemiological study. J Endod 2004: 30: 846850.
48. Aquilino SA, Caplan DJ. Relationship between crown
placement and the survival of endodontically treated
teeth. J Prosthet Dent 2002: 87: 256263.
49. Ng YL, Mann V, Gulabivala K. A prospective study of
the factors affecting outcomes of non-surgical root
canal treatmentpart 2: tooth survival. Int Endod J
2011: 44: 610625.
50. Vire DE. Failure of endodontically treated teeth:
classification and evaluation. J Endod 1991: 17:
338342.
51. Stavropoulou AF, Koidis PT. A systematic review of
single crowns on endodontically treated teeth. J Dent
2007: 35: 761767.
52. Nagasiri R, Chitmongkolsuk S. Long-term survival
of endodontically treated molars without crown
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
63.
64.
65.
66.
67.
coverage: a retrospective cohort study. J Prosthet Dent
2005: 93: 164170.
Sorensen JA, Martinoff JT. Endodontically treated
teeth as abutments. J Prosthet Dent 1985: 53:
631636.
Mannocci F, Bertelli E, Sherriff M, Watson TF, Ford
TR. Three-year clinical comparison of survival of
endodontically treated teeth restored with either full
cast coverage or with direct composite restoration.
J Prosthet Dent 2002: 88: 297301.
Mannocci F, Qualtrough AJ, Worthington HV,
Watson TF, Pitt Ford TR. Randomized clinical
comparison of endodontically treated teeth restored
with amalgam or with fiber posts and resin composite:
five-year results. Oper Dent 2005: 30: 915.
Nagasiri R, Chitmongkolsuk S. Long-term survival
of endodontically treated molars without crown
coverage: a retrospective cohort study. J Prosthet Dent
2005: 93: 164170.
Sedgley CM, Messer HH. Are endodontically treated
teeth more brittle? J Endod 1992: 18: 332335.
Costa LC, Pegoraro LF, Bonfante G. Influence of
different metal restorations bonded with resin on
fracture resistance of endodontically treated maxillary
premolars. J Prosthet Dent 1997: 77: 365369.
Steele A, Johnson BR. In vitro fracture strength of
endodontically treated premolars. J Endod 1999: 25:
68.
Nagem Filho H, Nagem HD, Francisconi PA, Franco
EB, Mondelli RF, Coutinho KQ. Volumetric
polymerization shrinkage of contemporary composite
resins. J Appl Oral Sci 2007: 15: 448452.
Attar N, Tam LE, McComb D. Flow, strength,
stiffness and radiopacity of flowable resin composites.
J Can Dent Assoc 2003: 69: 516521.
Palin WM, Fleming GJ, Nathwani H, Burke FJ, Randall
RC. In vitro cuspal deflection and microleakage of
maxillary premolars restored with novel low-shrink
dental composites. Dent Mater 2005: 21: 324335.
Visvanathan A, Ilie N, Hickel R, Kunzelmann KH.
The influence of curing times and light curing
methods on the polymerization shrinkage stress of a
shrinkage-optimized composite with hybrid-type
prepolymer fillers. Dent Mater 2007: 23: 777784.
Alomari QD, Reinhardt JW, Boyer DB. Effect on cusp
deflection and gap formation in composite
restorations. Oper Dent 2001: 26: 406411.
Magne P, Belser UC. Porcelain versus composite
inlays/onlays: effects of mechanical loads on stress
distribution, adhesion, and crown flexure. Int J
Periodontics Restorative Dent 2003: 23: 543555.
Beier US, Kapferer I, Burtscher D, Giesinger JM,
Dumfahrt H. Clinical performance of all-ceramic inlay
and onlay restorations in posterior teeth. Int J
Prosthodont 2012: 25: 395402.
Guess PC, Selz CF, Steinhart YN, Stampf S, Strub JR.
Prospective clinical split-mouth study of pressed and
CAD/CAM all-ceramic partial-coverage restorations:
7-year results. Int J Prosthodont 2013: 26: 2125.
81
Baba & Goodacre
68. Magne P, Carvalho A, Bruzi G, Anderson R, Maia H,
Giannini M. Influence of no-ferrule and no-post
buildup design on the fatigue resistance of
endodontically treated molars restored with resin
nanoceramic CAD/CAM crowns. Oper Dent 2014:
39: 595602.
69. Biacchi GR, Basting RT. Comparison of fracture
strength of endocrowns and glass fiber post-retained
conventional crowns. Oper Dent 2012: 37: 130136.
70. Dejak B, Motkowski A. 3D-finite element analysis of
molars restored with endocrowns and posts during
masticatory simulation. Dent Mater 2013: 29:
e309317.
71. Libman WJ, Nicholls JI. Load fatigue of teeth restored
with cast posts and cores and complete crowns. Int J
Prosthodont 1995: 8: 155161.
72. Milot P, Stein RS. Root fracture in endodontically
treated teeth related to post selection and crown
design. J Prosthet Dent 1992: 68: 428435.
73. Pereira JR, de Ornelas F, Conti PC, do Valle AL. Effect
of a crown ferrule on the fracture resistance of
endodontically
treated
teeth
restored
with
prefabricated posts. J Prosthet Dent 2006: 95: 5054.
74. Ng CCH, Dumbrigue HB, Al-Bayat MI, Griggs JA,
Wakefield CW. Influence of remaining coronal tooth
structure location on the fracture resistance of restored
endodontically treated anterior teeth. J Prosthet Dent
2006: 95: 290296.
75. Akkayan B. An in vitro study evaluating the effect of
ferrule length on fracture resistance of endodontically
treated teeth restored with fiber-reinforced and
zirconia dowel systems. J Prosthet Dent 2004: 92:
155162.
76. Tan PL, Aquilino SA, Gratton DG, Stanford CM, Tan
SC, Johnson WT, Dawson D. In vitro fracture
resistance of endodontically treated central incisors
with varying ferrule heights and configurations.
J Prosthet Dent 2005: 93: 331336.
77. Sorensen JA, Engelman MJ. Ferrule design and
fracture resistance of endodontically treated teeth.
J Prosthet Dent 1990: 63: 529536.
78. Morgano SM, Hashem AF, Fotoohi K, Rose L. A
nationwide survey of contemporary philosophies and
techniques of restoring endodontically treated teeth.
J Prosthet Dent 1994: 72: 259267.
79. Zhi-Yue L, Yu-Xing Z. Effects of post-core design and
ferrule on fracture resistance of endodontically treated
maxillary central incisors. J Prosthet Dent 2003: 89:
368373.
80. Baba NZ, Goodacre CJ, Kattadiyil MT. Tooth
retention through toot canal treatment or tooth
extraction and implant placement: a prosthodontic
perspective. Quintessence Int 2014: 45: 405416.
81. Naumann M, Preuss A, Rosentritt M. Effect of
incomplete crown ferrules on load capacity of
endodontically treated maxillary incisors restored
with fiber posts, composite build-ups, and all-ceramic
crowns: an in vitro evaluation after chewing
simulation. Acta Odontol Scand 2006: 64: 3136.
82
82. Pontius O, Hutter JW. Survival rate and fracture
strength of incisors restored with different post and
core systems and endodontically treated incisors
without coronoradicular reinforcement. J Endod 2002:
28: 710715.
83. Gluskin AH, Radke RA, Frost SL, Watanabe LG. The
mandibular incisor: rethinking guidelines for post and
core design. J Endod 1995: 21: 3337.
84. Tamse A, Fuss Z, Lustig J, Kaplavi J. An evaluation of
endodontically treated vertically fractured teeth.
J Endod 1999: 25: 506508.
85. Tour B, Faye B, Kane AW, Lo CM, Niang B, Boucher
Y. Analysis of reasons for extraction of endodontically
treated teeth: a prospective study. J Endod 2011: 37:
15121515.
86. Fokkinga WA, Le Bell AM, Kreulen CM, Lassila LV,
Vallittu PK, Creugers NH. Ex vivo fracture resistance
of direct resin composite complete crowns with and
without posts on maxillary premolars. Int Endod J
2005: 38: 230237.
87. Salvi GE, Siegrist Guldener BE, Amstad T, Joss A,
Lang NP. Clinical evaluation of root filled teeth
restored with or without post-and-core systems in a
specialist practice setting. Int Endod J 2007: 40:
209215.
88. Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY.
Clinical complications in fixed prosthodontics. J
Prosthet Dent 2003: 90: 3141.
89. Teixeira ECN, Teixeira FB, Piasick JR, Thompson JY.
An in vitro assessment of prefabricated fiber
post systems. J Am Dent Assoc 2006: 137:
10061012.
90. Plotino G, Grande NM, Bedini R, Pameijer CH,
Somma F. Flexural properties of endodontic posts
and human root dentin. Dent Mater 2007: 23:
11291135.
91. Lassila LV, Tanner J, Le Bell AM, Narva K, Vallittu
PK. Flexural properties of fiber reinforced root canal
posts. Dent Mater 2004: 20: 2936.
92. Lassila LVJ, Nohrstrm T, Vallitu P. The influence of
short-term water storage on the flexural properties of
unidirectional glass fiber-reinforced composites.
Biomaterials 2002: 23: 22212229.
93. Baldissara P, Di Grazia V, Palano A, Ciocca L. Fatigue
resistance of restored endodontically treated teeth: a
multiparametric analysis. Int J Prosthodont 2006: 19:
2527.
94. Torbjrner A, Fransson B. A literature review on the
prosthetic treatment of structurally compromised
teeth. Int J Prosthodont 2004: 17: 369376.
95. Baba NZ, Golden G, Goodacre CJ. Nonmetallic
prefabricated dowels: a review of compositions,
properties, laboratory, and clinical test results.
J Prosthodont 2009: 18: 527536.
96. Naumann M, Koelpin M, Beuer F, Meyer-Lueckel H.
10-year survival rate evaluation for glass-fibersupported postendodontic restoration: a prospective
observational clinical study. J Endod 2012: 38:
432435.
Restoration of endodontically treated teeth: contemporary concepts and future perspectives
97. Mjr IA, Smith MR, Ferrari M, Mannocci F. The
structure of dentine in the apical region of human
teeth. Int Endod J 2001: 34: 346353.
98. Mannocci F, Pilecki P, Bertelli E, Watson TF. Density
of dentinal tubules affects the tensile strength of root
dentin. Dent Mater 2004: 20: 293296.
99. Ferrari M, Mannocci F, Vichi A, Cagidiaco MC,
Mjr IA. Bonding to root canal: structural
characteristics of the substrate. Am J Dent 2000: 13:
255260.
100. Goracci C, Tavares AU, Fabianelli A, Monticelli F,
Raffaelli O, Cardoso PC, Tay F, Ferrari M. The
adhesion between fiber posts and root canal walls:
comparison between microtensile and push-out bond
strength measurements. Eur J Oral Sci 2004: 112:
353361.
101. Perdigao J, Geraldeli S, Lee IK. Push-out bond
strengths of tooth-colored posts bonded with
different adhesive systems. Am J Dent 2004: 17:
422426.
102. Seefeld F, Wenz HJ, Ludwig K, Kern M. Resistance to
fracture and structural characteristics of different fiber
reinforced post systems. Dent Mater 2007: 23:
265271.
103. Grandini S, Goracci C, Monticelli F, Tay FR, Ferrari
M. Fatigue resistance and structural characteristics of
fiber posts: three-point bending test and SEM
evaluation. Dent Mater 2005: 21: 7582.
104. Valandro LF, Yoshiga S, de Melo RM, Galhano GA,
Mallmann A, Marinho CP, Bottino MA. Microtensile
105.
106.
107.
108.
109.
110.
111.
bond strength between a quartz fiber post and a resin
cement: effect of post surface conditioning. J Adhes
Dent 2006: 8: 105111.
Zicari F, De Munck J, Scotti R, Naert I, Van Meerbeek
B. Factors affecting the cementpost interface. Dent
Mater 2012: 28: 287297.
Gmez-Polo M, Llid B, Rivero A, Del Ro J, Celemn
A. A 10-year retrospective study of the survival rate of
teeth restored with metal prefabricated posts versus
cast metal posts and cores. J Dent 2010: 38: 916920.
Ayna B, Celenk S, Atakul F, Uysal E. Three-year
clinical evaluation of endodontically treated anterior
teeth restored with polyethylene fibre-reinforced
composite. Aust Dent J 2009: 54: 136140.
Costa RG, De Morais EC, Campos EA, Michel MD,
Gonzaga CC, Correr GM. Customized fiber glass
posts. Fatigue and fracture resistance. Am J Dent
2012: 25: 3538.
da Costa RG, de Morais EC, Leo MP, Bindo MJ,
Campos EA, Correr GM. Three-year follow up of
customized glass fiber esthetic posts. Eur J Dent 2011:
5: 107112.
Kimmel SS. Restoration and reinforcement of
endodontically treated teeth with a polyethylene
ribbon and prefabricated fiberglass post. Gen Dent
2000: 48: 700706.
Bittner N, Hill T, Randi A. Evaluation of a one-piece
milled zirconia post and core with different post-andcore systems: an in vitro study. J Prosthet Dent 2010:
103: 369379.
83
Vous aimerez peut-être aussi
- Practice: Failures in Implant DentistryDocument7 pagesPractice: Failures in Implant DentistryhmsatPas encore d'évaluation
- Maxillofacial Prosthetics: Kamolphob Phasuk,, Steven P. HaugDocument11 pagesMaxillofacial Prosthetics: Kamolphob Phasuk,, Steven P. Hauglaura sanchez avilaPas encore d'évaluation
- The Prosthodontic Management of Endodontically Treated Teeth - A Literature Review. Part I. SuccesDocument8 pagesThe Prosthodontic Management of Endodontically Treated Teeth - A Literature Review. Part I. SucceskochikaghochiPas encore d'évaluation
- In-Situ MetallographyDocument22 pagesIn-Situ MetallographyAmalia Tri WPas encore d'évaluation
- Regressive Changes of TeethDocument45 pagesRegressive Changes of TeethNader AlaizariPas encore d'évaluation
- CADCAM Review 2018 PDFDocument5 pagesCADCAM Review 2018 PDFAya Ibrahim YassinPas encore d'évaluation
- Jung 2018Document11 pagesJung 2018Sebastien MelloulPas encore d'évaluation
- Treatment Planning Single Maxillary Anterior Implants for DentistsD'EverandTreatment Planning Single Maxillary Anterior Implants for DentistsPas encore d'évaluation
- Shubharambh Banquets HL - All Halls 26-5-2017Document5 pagesShubharambh Banquets HL - All Halls 26-5-2017calvin.bloodaxe4478Pas encore d'évaluation
- Rethinking FerruleDocument10 pagesRethinking FerruleteodudePas encore d'évaluation
- Supra-Gingival Minimally Invasive Dentistry: A Healthier Approach to Esthetic RestorationsD'EverandSupra-Gingival Minimally Invasive Dentistry: A Healthier Approach to Esthetic RestorationsÉvaluation : 5 sur 5 étoiles5/5 (1)
- Cosmetic Dentistry CSD 2013Document3 pagesCosmetic Dentistry CSD 2013Rodrigo Daniel Vela RiveraPas encore d'évaluation
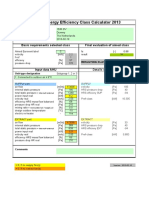
- Eurovent Energy Efficiency CalculatorDocument1 pageEurovent Energy Efficiency CalculatorPradeep Sukumaran100% (1)
- Posterior Composite Restoration UpdateDocument10 pagesPosterior Composite Restoration UpdateBianca IovoaiaPas encore d'évaluation
- ImplantDocument4 pagesImplantSaraPas encore d'évaluation
- Emergency Profile ManagementDocument13 pagesEmergency Profile ManagementCristian PazPas encore d'évaluation
- The Dahl Concept Past Present and FutureDocument9 pagesThe Dahl Concept Past Present and FuturevivigaitanPas encore d'évaluation
- Endodontic Management of Traumatic InjuriesDocument6 pagesEndodontic Management of Traumatic InjuriesMehwish MunawarPas encore d'évaluation
- Guidelines BookDocument16 pagesGuidelines BookAdel ElaroudPas encore d'évaluation
- Werm Ker 2014Document7 pagesWerm Ker 2014Alice EmailsPas encore d'évaluation
- The Biologic WidthDocument21 pagesThe Biologic WidthDrKrishna DasPas encore d'évaluation
- Avoiding and Treating Dental Complications: Best Practices in DentistryD'EverandAvoiding and Treating Dental Complications: Best Practices in DentistryDeborah A. TermeiePas encore d'évaluation
- Restoration of The Worn Dentition. Part 2Document7 pagesRestoration of The Worn Dentition. Part 2Isharajini Prasadika Subhashni GamagePas encore d'évaluation
- Advance in MaterialsDocument10 pagesAdvance in Materialssami robalinoPas encore d'évaluation
- Regenerative Endodontics Barriers and Strategies For Clinical Translation 2012 Dental Clinics of North AmericaDocument11 pagesRegenerative Endodontics Barriers and Strategies For Clinical Translation 2012 Dental Clinics of North AmericaCaioSelaimenPas encore d'évaluation
- Topical Fluorides and Decalcification ArDocument164 pagesTopical Fluorides and Decalcification ArArinaPas encore d'évaluation
- Additive Contour of Porcelain Veneers A Key Element in Enamel PreservationDocument13 pagesAdditive Contour of Porcelain Veneers A Key Element in Enamel PreservationPablo BenitezPas encore d'évaluation
- The Success of Endodontic Therapy Healing and Functionality Friedman PDFDocument11 pagesThe Success of Endodontic Therapy Healing and Functionality Friedman PDFizeldien5870Pas encore d'évaluation
- A Restrospective Periodontal Assessment of 137 Teeth After Featheredge Preparation and GingittageDocument11 pagesA Restrospective Periodontal Assessment of 137 Teeth After Featheredge Preparation and GingittageBelen AntoniaPas encore d'évaluation
- Clin DSDDocument5 pagesClin DSDAlfred OrozcoPas encore d'évaluation
- Periodontal-Restorative Interactions: A Review: DentistryDocument7 pagesPeriodontal-Restorative Interactions: A Review: DentistrySahana RangarajanPas encore d'évaluation
- Relationship Between Bruxism and Temporomandibular Disorders: A Systematic Review of Literature From 1998 To 2008Document25 pagesRelationship Between Bruxism and Temporomandibular Disorders: A Systematic Review of Literature From 1998 To 2008AARON DIAZ RONQUILLOPas encore d'évaluation
- Advances in Extraction TechniquesDocument13 pagesAdvances in Extraction TechniquesashajangamPas encore d'évaluation
- The Single-Tooth RestorationDocument5 pagesThe Single-Tooth Restorationumerjaved86Pas encore d'évaluation
- HTTP WWW - Styleitaliano.org Esthetic Dentistry in PaediatricsDocument9 pagesHTTP WWW - Styleitaliano.org Esthetic Dentistry in PaediatricsAmee PatelPas encore d'évaluation
- The Ideal Restoration of Endodontically Treated Teeth Structural and Esthetic Considerations A Review of The Literature and Clinical Guidelines For The Restorative ClinicianDocument31 pagesThe Ideal Restoration of Endodontically Treated Teeth Structural and Esthetic Considerations A Review of The Literature and Clinical Guidelines For The Restorative ClinicianLuis Alberto Carpio MorenoPas encore d'évaluation
- Dent Update 2016 Resin-Bonded-Bridge-DesignDocument11 pagesDent Update 2016 Resin-Bonded-Bridge-DesignSmriti VermaPas encore d'évaluation
- Dental Caries A DiseaseDocument57 pagesDental Caries A Diseaseasti finda100% (1)
- MagnificationDocument52 pagesMagnificationSiva KumarPas encore d'évaluation
- Managing The Unstable CDDocument8 pagesManaging The Unstable CDNajeeb UllahPas encore d'évaluation
- 1 Cbct-Evaluation of Remaining Dentin Thickness and Fracture Resistance of Conventional and Conservative Access and Biomechanical Preparation in Molars Using Cone-beam Computed Tomography- An in Vitro StudyDocument4 pages1 Cbct-Evaluation of Remaining Dentin Thickness and Fracture Resistance of Conventional and Conservative Access and Biomechanical Preparation in Molars Using Cone-beam Computed Tomography- An in Vitro StudyalbertaugustinePas encore d'évaluation
- Surgical Vs Non-Surgical Approach in PeriodonticsDocument13 pagesSurgical Vs Non-Surgical Approach in PeriodonticsBea DominguezPas encore d'évaluation
- Dental Implant Treatment Planning for New Dentists Starting Implant TherapyD'EverandDental Implant Treatment Planning for New Dentists Starting Implant TherapyÉvaluation : 4 sur 5 étoiles4/5 (1)
- The Use of Separating Rings in The Placement of Class II Composite ResinsDocument9 pagesThe Use of Separating Rings in The Placement of Class II Composite ResinsLeslie MorrowPas encore d'évaluation
- Papper PeriodDocument12 pagesPapper PeriodLoretoReyesMoralesPas encore d'évaluation
- Journal of EndodonticsDocument220 pagesJournal of EndodonticsFauzan100% (2)
- Bonnick - 2011 - Dental Clinics of North America PDFDocument14 pagesBonnick - 2011 - Dental Clinics of North America PDFKranti PrajapatiPas encore d'évaluation
- Modern Anterior Endodontic Access and Directed Dentin Conservation David Clark & John Khademi PDFDocument5 pagesModern Anterior Endodontic Access and Directed Dentin Conservation David Clark & John Khademi PDFizeldien5870Pas encore d'évaluation
- Prolonged Retention, Ankylosis and Infraocclusion of Deciduous Teeth Ok OkDocument5 pagesProlonged Retention, Ankylosis and Infraocclusion of Deciduous Teeth Ok OkRahulLife'sPas encore d'évaluation
- 2013 Direct Anterior Composites A Practical GuideDocument16 pages2013 Direct Anterior Composites A Practical Guidemaroun ghalebPas encore d'évaluation
- Minimally Invasive Endodontics A Promising Future Concept A Review Article - 2017Document7 pagesMinimally Invasive Endodontics A Promising Future Concept A Review Article - 2017izeldien5870Pas encore d'évaluation
- An Introduction To Fixed ProsthodonticsDocument6 pagesAn Introduction To Fixed Prosthodonticsمؤمل رياض سعد كاظمPas encore d'évaluation
- Optimizing Gingival EstheticsDocument8 pagesOptimizing Gingival EstheticsThe Bioclear Clinic100% (1)
- 2 Nonsurgical Periodontal Therapy - Pocket DentistryDocument14 pages2 Nonsurgical Periodontal Therapy - Pocket DentistryRizki OktavianiPas encore d'évaluation
- 31 SJ BDJ 2014 953Document7 pages31 SJ BDJ 2014 953Juan Augusto Fernández TarazonaPas encore d'évaluation
- Denture Related StomatitisDocument8 pagesDenture Related StomatitisLike OliviaPas encore d'évaluation
- The Effect of Access Cavity Design On Fracture Resistance of Endodontically Treated First Molars in Vitro Study PDFDocument9 pagesThe Effect of Access Cavity Design On Fracture Resistance of Endodontically Treated First Molars in Vitro Study PDFLina SaadPas encore d'évaluation
- Biologic WidthDocument39 pagesBiologic Widthsharanya chekkarrajPas encore d'évaluation
- Deep Margin ElevationDocument1 pageDeep Margin ElevationJazPas encore d'évaluation
- Open Drainage or NotDocument6 pagesOpen Drainage or Notjesuscomingsoon2005_Pas encore d'évaluation
- Material Options For Class II Composite Restorations - Varied Clinical Parameters Require Different TechniquesDocument6 pagesMaterial Options For Class II Composite Restorations - Varied Clinical Parameters Require Different TechniquesMohammed NabeelPas encore d'évaluation
- Root Canal SealersDocument14 pagesRoot Canal SealerskerminkPas encore d'évaluation
- Endodontic Therapy On A Dentition Exhibiting Multiple Periapical Radiolucencies Associated With DDocument3 pagesEndodontic Therapy On A Dentition Exhibiting Multiple Periapical Radiolucencies Associated With Djihan_joePas encore d'évaluation
- The Management of Periapical Lesions in Endodontically Treated TeethDocument14 pagesThe Management of Periapical Lesions in Endodontically Treated TeethardeleanoanaPas encore d'évaluation
- Radiographic and Rheological Properties of A New Endodontic SealerDocument4 pagesRadiographic and Rheological Properties of A New Endodontic SealerardeleanoanaPas encore d'évaluation
- Determination of Root Canal Curvatures Before and After Canal Preparation (Part IIDocument10 pagesDetermination of Root Canal Curvatures Before and After Canal Preparation (Part IIjihan_joePas encore d'évaluation
- Effect of Waterlase Laser Retrograde Root-End Cavity Preparation On The Integrity of Root ApicesDocument5 pagesEffect of Waterlase Laser Retrograde Root-End Cavity Preparation On The Integrity of Root ApicesRăican AlexandruPas encore d'évaluation
- British Dental JournalDocument5 pagesBritish Dental JournalardeleanoanaPas encore d'évaluation
- 1806 4760 BDJ 27 01 00046Document6 pages1806 4760 BDJ 27 01 00046ardeleanoanaPas encore d'évaluation
- 0103 6440 BDJ 26 03 00222Document6 pages0103 6440 BDJ 26 03 00222ardeleanoanaPas encore d'évaluation
- 1806 4760 BDJ 26 06 00619Document5 pages1806 4760 BDJ 26 06 00619ardeleanoanaPas encore d'évaluation
- DentalPressEndodontics v2n4 Oct-Dec 2012Document72 pagesDentalPressEndodontics v2n4 Oct-Dec 2012ardeleanoanaPas encore d'évaluation
- DentalPressEndodontics v1n3 Oct-Dec 2011Document96 pagesDentalPressEndodontics v1n3 Oct-Dec 2011ardeleanoanaPas encore d'évaluation
- Dentina Como SustratoDocument28 pagesDentina Como SustratoCdcgs PWinPas encore d'évaluation
- Endodontic Topics Volume 18 Issue 1 2008 (Doi 10.1111/j.1601-1546.2011.00260.x) YUAN-LING NG KISHOR GULABIVALA - Outcome of Non-Surgical Re-TreatmentDocument28 pagesEndodontic Topics Volume 18 Issue 1 2008 (Doi 10.1111/j.1601-1546.2011.00260.x) YUAN-LING NG KISHOR GULABIVALA - Outcome of Non-Surgical Re-TreatmentardeleanoanaPas encore d'évaluation
- Endodontic Topics Volume 19 Issue 1 2008 (Doi 10.1111/j.1601-1546.2011.00253.x) CHANKHRIT SATHORN PETER PARASHOS - Monitoring The Outcomes of Root Canal Re-TreatmentsDocument10 pagesEndodontic Topics Volume 19 Issue 1 2008 (Doi 10.1111/j.1601-1546.2011.00253.x) CHANKHRIT SATHORN PETER PARASHOS - Monitoring The Outcomes of Root Canal Re-TreatmentsardeleanoanaPas encore d'évaluation
- Drilling Fluid Technology: Performances and Environmental ConsiderationsDocument32 pagesDrilling Fluid Technology: Performances and Environmental ConsiderationsAli EttehadiPas encore d'évaluation
- Characterization of Iron Oxide Thin Film Prepared by The Sol-Gel MethodDocument2 pagesCharacterization of Iron Oxide Thin Film Prepared by The Sol-Gel MethodBryan Anders AguilarPas encore d'évaluation
- INDENTIFICATIONDocument6 pagesINDENTIFICATIONMomina HaiderPas encore d'évaluation
- E 1652 - 03 - Rte2ntiDocument8 pagesE 1652 - 03 - Rte2ntiLemir LopezPas encore d'évaluation
- Plastics - Polyacrylamide Materials - Designation System and SpecificationDocument20 pagesPlastics - Polyacrylamide Materials - Designation System and SpecificationDevesh Kumar PandeyPas encore d'évaluation
- Sand To Silicon 22nm VersionDocument18 pagesSand To Silicon 22nm VersionDavid Rubio SaezPas encore d'évaluation
- Wave Induced AccelerationDocument6 pagesWave Induced AccelerationAnonymous g5FCwMRPas encore d'évaluation
- 13.9 Numerical Procedures For Binary, Ternary LLE: Excel ProcedureDocument2 pages13.9 Numerical Procedures For Binary, Ternary LLE: Excel ProcedureAlyssaRamosPas encore d'évaluation
- Steel MetallurgyDocument8 pagesSteel MetallurgyEswarPas encore d'évaluation
- Class II Methodology For Drag EstimationDocument80 pagesClass II Methodology For Drag EstimationBrian XistosPas encore d'évaluation
- BetaDocument3 pagesBetacrg1234Pas encore d'évaluation
- Effect of Eccentricity On Analysis and Design of Isolated FootingsDocument18 pagesEffect of Eccentricity On Analysis and Design of Isolated Footingsप्रभु नाथ सिंहPas encore d'évaluation
- TilesDocument84 pagesTilesgagan raoPas encore d'évaluation
- Assignment 2Document4 pagesAssignment 2blackbeauty14Pas encore d'évaluation
- Earth Wire FittingsDocument11 pagesEarth Wire FittingsWeber HahnPas encore d'évaluation
- Why Kinetics Is Very Important in PharmacyDocument13 pagesWhy Kinetics Is Very Important in PharmacyRavi KantPas encore d'évaluation
- Synthesis of UiO 66 OH Zirconium Metal Organic FrameworkDocument7 pagesSynthesis of UiO 66 OH Zirconium Metal Organic FrameworkFilozofijaPalePas encore d'évaluation
- Robustness of The QAL2 Calibration EN14181 UncertaDocument10 pagesRobustness of The QAL2 Calibration EN14181 UncertaAnaibar TarikPas encore d'évaluation
- Bond Work IndexDocument7 pagesBond Work IndexJaime Alberto Sanchez CardonaPas encore d'évaluation
- Microbial Identification in The Pharmaceutica IndustryDocument11 pagesMicrobial Identification in The Pharmaceutica IndustrySurendar KesavanPas encore d'évaluation
- Properties EpoxyCOMPOSITEDocument9 pagesProperties EpoxyCOMPOSITESanket AntrePas encore d'évaluation
- DegassingDocument11 pagesDegassingMKOZERDEMPas encore d'évaluation
- Sierra Megonnell and Kyle Lovisone ExpDocument1 pageSierra Megonnell and Kyle Lovisone Expapi-528179516Pas encore d'évaluation
- ADVANTAGES. of Polymer Insulator PDFDocument1 pageADVANTAGES. of Polymer Insulator PDFviksoniPas encore d'évaluation
- Que BankDocument12 pagesQue BankAbhishek VishwakarmaPas encore d'évaluation
- Transparent Films On Polymers For Photovoltaic Applications: J. Herrero, C. Guill !enDocument6 pagesTransparent Films On Polymers For Photovoltaic Applications: J. Herrero, C. Guill !enAnand Sreekantan ThampyPas encore d'évaluation
- 9869 0099 01e Grouting Solutions Technical Specification EnglishDocument7 pages9869 0099 01e Grouting Solutions Technical Specification Englishignacio.garcia11Pas encore d'évaluation