Académique Documents
Professionnel Documents
Culture Documents
Carson 2002
Transféré par
Jan BohemioCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Carson 2002
Transféré par
Jan BohemioDroits d'auteur :
Formats disponibles
TRANSFUSION PRACTICE
Mortality and morbidity in patients with very low
postoperative Hb levels who decline blood transfusion
Jeffrey L. Carson, Helaine Noveck, Jesse A. Berlin, and Steven A. Gould
BACKGROUND: Guidelines for allogeneic transfusion
emphasize minimizing use to avoid transmission of serious illness. However, there is little information on the
risks associated from withholding transfusion.
STUDY DESIGN AND METHODS: A retrospective cohort study of patients who declined RBC transfusions
for religious reasons was performed. This analysis was
restricted to consecutive patients 18 years old, who
underwent surgery in the operating room from 1981 to
1994 and had a postoperative Hb count of 8 g per dL
or less. The primary outcome was defined as any inhospital death occurring within 30 days of the surgery.
Secondary outcome was 30-day mortality or in-hospital
30-day morbidity. Morbidity was defined as myocardial
infarction, arrhythmia, congestive heart failure, or infection.
RESULTS: Of 2083 eligible patients, 300 had postoperative Hb counts of 8 g per dL or less. The study
population was predominantly female (70.3%) with a
mean age of 57 years (SD, 17.7). In patients with a
postoperative Hb level of 7.1 to 8.0, 0 died (upper 95%
CI, 3.7%), and 9.4 percent (95% CI, 4.4-17.0%) had a
morbid event. In patients with a postoperative Hb level
of 4.1 to 5.0, 34.4 percent (95% CI, 18.6-53.2%) died
and 57.7 percent (95% CI, 36.9-76.6%) had a morbid
event or died. After adjusting for age, cardiovascular
disease, and Acute Physiology and Chronic Health
Evaluation II score, the odds of death in patients with a
postoperative Hb level of 8 g per dL increased 2.5
times (95% CI, 1.9-3.2) for each gram decrease in Hb
level.
CONCLUSIONS: The risk of death was low in patients
with postoperative Hb levels of 7.1 to 8.0 g per dL, although morbidity occurred in 9.4 percent. As postoperative blood counts fall the risk of mortality and/or morbidity rises and becomes extremely high below 5 to 6 g
per dL.
he trend in blood management is to withhold
transfusion unless a patient has symptoms.
Very low transfusion triggers have been advocated. Many hospitals are developing bloodless
medicine and surgery programs. Data are needed to inform the medical community and public about the risks
of anemia after surgery.
Previous clinical studies provide limited information
on clinical consequences of very low blood counts. Physiologic studies suggest that young volunteers tolerate very
low blood counts, although fatigue and a decline in
memory and cognitive function have been documented.1,2 Clinical trials have not evaluated blood transfusion strategies with Hb levels less than 7 g per dL.3-9 An
analysis of case reports of Jehovahs Witness patients
concluded that nearly all deaths due to anemia occurred
in patients with Hb levels less than 5 g per dL.10 Carson et
al. 11,12 previously published two series of consecutive
Jehovahs Witness patients but restricted the analysis to
preoperative Hb levels and did not characterize outABBREVIATION: APACHE II, Acute Physiology and Chronic
Health Evaluation II; Hb = hemoglobin; OR = odds ratio.
From the Division of General Internal Medicine, Department
of Medicine, University of Medicine and Dentistry of New Jersey, Robert Wood Johnson Medical School, New Brunswick,
New Jersey; Center for Clinical Epidemiology and Biostatistics,
Department of Biostatistics and Epidemiology, University of
Pennsylvania School of Medicine, Philadelphia, Pennsylvania;
and Northfield Laboratories, Evanston, Illinois.
Address reprint requests to: Jeffrey L. Carson, MD, Division
of General Internal Medicine, Department of Medicine, University of Medicine and Dentistry of New Jersey, Robert Wood
Johnson Medical School, New Brunswick, NJ; e-mail:
carson@umdnj.edu.
Supported in part by a grant from Northfield Laboratories, Evanston, IL, and by Grant R01HL41523 from the National Heart, Lung, and Blood Institute.
Disclosure: One of the authors (SAG) owns stock in a
company that produces a Hb-based oxygen carrier.
Received for publication October 12, 2001; revision received January 10, 2002, and accepted February 12, 2002.
TRANSFUSION 2002;42:812-818.
812
TRANSFUSION
Volume 42, July 2002
PATIENT OUTCOME WITH VERY LOW Hb LEVEL
comes stratified by Hb levels below 6 g per dL. The risk
associated with postoperative anemia may be different
than preoperative anemia because surgery is completed
and the patient may be subject to different physiologic
stress. We now report on the subset of these patients with
postoperative Hb counts of 8 g per dL or less.
MATERIALS AND METHODS
Study design and patient population
We performed a retrospective cohort study of surgical
patients who refused RBC transfusions for religious reasons. These patients were drawn from two previously
published studies in Jehovahs Witness patients undergoing surgery.11,12 One study consisted of a consecutive series of 125 patients at Cooper Hospital/University Medical Center, Camden, New Jersey (single hospital). The
second study included 1958 consecutive patients from 12
hospitals enrolled in a multi-institutional study. All patients were hospitalized between 1981 and 1994. Inclusion criteria required that surgery be performed in the
operating room and the patient be at least 18 years of age.
Younger patients were excluded because transfusions can
be ordered by the court in minors. Patients undergoing
open heart procedures were also excluded from the
study.
Outcome variables
We defined mortality as in-hospital death occurring
within 30 days of the surgery. We did not identify deaths
that might have occurred following discharge but within
this 30-day window.
We evaluated postoperative morbidity only in the
multicenter cohort since the single-center cohort did not
identify the date of the morbid event. We defined postoperative morbidity as myocardial infarction, congestive
heart failure, arrhythmia, or infection (bacteremia, pneumonia, or deep wound infection) that occurred within 30
days of surgery. Myocardial infarction was defined by use
of the Atherosclerosis Risk in Communities Study criteria,
which are widely used in epidemiologic studies of myocardial infarction.13 We defined congestive heart failure
as a physician diagnosis of congestive heart failure or a
chest radiograph interpreted as new congestive heart failure in combination with treatment with diuretics, digoxin, or angiotensin-converting enzyme inhibitor. We
defined arrhythmia as ventricular tachycardia, ventricular fibrillation, new-onset atrial fibrillation, or Mobitz
type II or complete heart block requiring parenteral drug
treatment, pacer, or cardioversion. We defined bacteremia as a positive blood culture for an organism other
than that usually considered a contaminant (e.g., Staphylococcus epidermidis). We defined pneumonia as a new
pulmonary infiltrate on the chest radiograph and new
antibiotic treatment. We defined deep wound infection
by physician diagnosis and treatment with antibiotic.
Data collection
All data were collected from information recorded in the
medical charts by trained abstractors by use of explicit
abstraction instruments. These data included demographic information, past medical histories, preoperative
physical assessment, laboratory results, surgery that was
performed, and postoperative morbid events.
Preoperative Hb was the last value recorded prior to
surgery. The lowest postoperative Hb was the lowest
value recorded through the fourth week following surgery. In the single-hospital database the lowest postoperative Hb was recorded through the time of discharge
which was greater than 30 days for five patients. In patients with an outcome, the postoperative Hb level used
was the last value prior to death or the first morbid event.
In patients without an outcome, the postoperative Hb
used was the lowest postoperative value.
We collected information on many comorbid conditions. This included histories of cancer, diabetes, hypertension, chronic obstructive pulmonary disease, angina
pectoris, and congestive heart failure. Angina was defined
as a history of chest pain brought on by exertion or emotion or that was relieved by rest or nitroglycerin or a
history of angina noted in the medical chart. Congestive
heart failure was defined as a history of congestive heart
failure noted in the medical chart or a history of orthopnea, paroxysmal nocturnal dyspnea, or pulmonary
edema. We created a combined category of cardiovascular disease that included history of angina, congestive
heart failure, myocardial infarction, or peripheral vascular disease. A modification of the Acute Physiology and
Chronic Health Evaluation II (APACHE II) score, which is
predictive of in-hospital mortality for critically ill patients
was created.14 We excluded the Hb component of this
calculation because the Hb level was the primary variable
of interest. We classified surgical procedure in three
ways: 1) by primary system, for example, neurosurgery; 2)
as aortic, intrathoracic, intraperitoneal, or other which
has been previously shown to be an independent predictor of outcome;15 and 3) emergency operation. We recorded the type of anesthesia used and the clinical center
where the patient underwent surgery.
Statistical analysis
A descriptive analysis calculating the mortality and combined mortality or morbidity outcome by Hb levels (in
gram increments) with 95-percent Cis was performed.
We assessed the relationship between Hb level and outcome by use of the Cochran-Armitage Trend test.16 We
evaluated the linearity of the relationship between Hb
and outcome by testing the significance of a quadratic
Volume 42, July 2002 TRANSFUSION
813
CARSON ET AL.
(squared) term in the logistic model. As this term was not
significant, Hb was entered as a continuous variable in all
the logistic models. The unadjusted relationships between Hb level and postoperative mortality or morbidity
were assessed by use of a logistic regression model including Hb as the only independent variable, with the
calculation of odds ratio (ORs) and 95-percent confidence interval (CIs).16 We used logistic regression to
evaluate confounding by a fitting series of models that
included Hb level and each variable in Table 1, one at a
time. We examined the change in the OR for Hb level
after each variable was added to the model and defined
confounding as a 10-percent change in OR for Hb level.
The final model adjusted for the potential confounders of
age, cardiovascular disease, and APACHE II score (minus
the Hb component).17 Interaction between cardiovascular disease and Hb level was evaluated based on prior
studies, which indicated that the effect of anemia was
more pronounced in those with cardiovascular disease
than in those without cardiovascular disease.18 All analyses were performed with a computer program (SAS version 8.0, SAS Institute, Cary, NC).
RESULTS
Study population
Of the 2083 consecutive patients from the two study cohorts, 300 (14.4%) patients had postoperative Hb levels
8 g per dL or less. There were 263 patients from the multicenter cohort and 37 from the single-hospital cohort.
The study population was predominantly female (70.3%)
and the mean age was 57 years (SD, 17.7, range, 18-90).
Of the 300 patients, 123 (41%) had preoperative Hb levels
less than 8 g per dL. Table 1 displays the patient characteristics by gram increments of lowest recorded Hb. The
majority of surgeries were aortic, intrathoracic, or intra-
peritoneal (65.3%) and were performed with general anesthesia (85.0%). Emergency operations accounted for
19.0 percent of the total. Table 2 characterizes the surgical procedure and associated mortality.
Postoperative Hb levels and mortality
Of the 300 patients with nadir postoperative Hb levels
8 g per dL, 48 (16.0%; 95% CI, 12.0-20.7%) died in the
hospital within 30 days of operative procedure. Table 3
displays the number of deaths stratified by Hb level and
cardiovascular disease. There were no deaths in the 99
patients with nadir Hb levels between 7.1 and 8.0 g per dL
(upper 95% CI, 3.7%). Mortality rose from 8.9 percent in
those with Hb levels between 6.1 and 7.0 to 100 percent in
those with Hb levels between 1.1 and 2.0 g per dL. The
test for trend was significant (p < 0.01) and the unadjusted OR for each gram decrease in Hb was 2.4 (95% CI,
1.9-3.0). Adjustment for the factors in Table 1, type of
operation, and clinical center failed to change the OR for
Hb by more than 5 percent in either direction. Therefore,
the final model adjusted for age, cardiovascular disease
(the two variables for which adjustment produced the
largest changes in the OR for Hb), and APACHE II score
since it was one of the strongest predictors of outcome.
Adjustment for these three variables together had no appreciable effect on the OR for Hb level; the OR was 2.5
(95% CI, 1.9-3.2). The interaction between postoperative
Hb level and cardiovascular disease was not significant
(p = 0.19).
Postoperative Hb levels and mortality
and morbidity
The analysis of mortality and morbidity was limited to
the multicenter cohort. There were 263 patients with nadir postoperative Hb levels 8 g per dL. Seven patients
were excluded from this analysis because they developed
TABLE 1. Patient characteristics stratified by lowest postoperative Hb level (n = 300)
Female
Age (years)
18-59
60-74
75
History of cancer
Diabetes
History of hypertension
History of chronic obstructive pulmonary disease
Angina
Congestive heart failure
Cardiovascular disease
Intraperitoneal, intrathoracic, or aortic procedure
Emergency operation
General anesthesia
* Data reported as number (%).
814
TRANSFUSION
Volume 42, July 2002
1.1-2.0
(n = 7)
6 (85.7)
Lowest Hb level (g/dL) during postoperative period*
2.1-3.0
3.1-4.0
4.1-5.0
5.1-6.0
6.1-7.0
(n = 24)
(n = 28)
(n = 32)
(n = 54)
(n = 56)
16 (66.7)
22 (78.6)
19 (59.4)
37 (68.5)
37 (66.1)
7.1-8.0
(n = 99)
74 (74.7)
4 (57.1)
2 (28.6)
1 (14.3)
0
1 (14.3)
2 (28.6)
0
2 (28.6)
1 (14.3)
2 (28.6)
5 (71.4)
2 (28.6)
7 (100)
13 (54.2)
8 (33.3)
3 (12.5)
2 (8.3)
3 (12.5)
11 (45.8)
2 (8.3)
2 (8.3)
3 (12.5)
5 (20.8)
16 (66.7)
12 (50.0)
19 (79.2)
56 (56.6)
28 (28.3)
15 (15.2)
20 (20.2)
17 (17.2)
40 (40.4)
1 (1.0)
3 (3.0)
10 (10.1)
17 (17.2)
64 (64.6)
8 (8.1)
87 (87.9)
11 (39.3)
13 (46.4)
4 (14.3)
4 (14.3)
10 (35.7)
9 (32.1)
2 (7.1)
2 (7.1)
3 (10.7)
8 (28.6)
18 (64.3)
6 (21.4)
27 (96.4)
17 (53.1)
8 (25.0)
7 (21.9)
6 (18.8)
10 (31.3)
16 (50.0)
1 (3.1)
4 (12.5)
7 (21.9)
12 (37.5)
19 (59.4)
9 (28.1)
25 (78.1)
30 (55.6)
13 (24.1)
11 (20.4)
8 (14.8)
13 (24.1)
22 (40.7)
2 (3.7)
8 (14.8)
7 (13.0)
14 (25.9)
37 (68.5)
12 (22.2)
46 (85.2)
28 (50.0)
20 (35.7)
8 (14.3)
13 (23.2)
11 (19.6)
24 (42.9)
1 (1.8)
4 (7.1)
4 (7.1)
12 (21.4)
37 (66.1)
8 (14.3)
44 (78.6)
PATIENT OUTCOME WITH VERY LOW Hb LEVEL
TABLE 2. Classification of operation and risk
of mortality*
Operation
Breast
Genitourinary
Gastrointestinal
Gynecological
Miscellaneous
Neurosurgery
Orthopedic
Skin
Thoracic
Vascular
Intraperitoneal, intrathoracic,
or aortic procedure
Emergency surgery
Number (%)
3 (1.0%)
35 (11.7%)
116 (8.7%)
52 (17.3%)
6 (2.0%)
6 (2.0%)
33 (11.0%)
5 (1.7%)
4 (1.3%)
40 (13.3%)
Mortality
(number [%])
1 (33.3%)
6 (17.1%)
20 (17.2%)
6 (11.5%)
2 (33.3%)
1 (16.7%)
2 (6.1%)
0 (0%)
0 (0%)
10 (25.0%)
196 (65.3%)
57 (19.0%)
34 (17.4%)
13 (22.8%)
* The overall mortality rate was 16 percent.
a morbid event prior to their Hb falling to 8 g per dL. Of
the remaining 256 patients, 57 (22.3%; 95% CI, 17.327.9%) experienced a morbid event, and 74 (28.9%; 95%
CI, 23.4-34.9%) had the combined morbidity and mortality outcome. The most common postoperative complications were congestive heart failure (n = 24, 9.4%), arrhythmia (n = 19, 7.4%), and pneumonia (n = 17, 6.6%).
Bacteremia (n = 8, 3.1%), deep wound infection (n = 3,
1.2%), and myocardial infarction (n = 4, 1.6%) were uncommon outcomes.
The relationship between nadir postoperative Hb
level and mortality or morbidity is displayed in Table 4.
There was a sharp increase in the rates of mortality or
morbidity as the Hb value decreases (p for trend < 0.01).
The unadjusted OR for each gram decrease in Hb was 2.2
(95% CI, 1.8-2.8). After adjusting for age, cardiovascular
disease, and APACHE II score the OR for each gram decrease in Hb was 2.1 (95% CI, 1.7-2.6). The interaction
between postoperative Hb level and cardiovascular disease was consistent with prior studies, although not significant (p = 0.09)
DISCUSSION
We describe the mortality and morbidity in the largest
consecutive series (n = 300) in the published literature of
patients, with postoperative Hb levels 8 g per dL, who
declined blood transfusion for religious reasons. We
demonstrate that mortality rises as Hb falls. The odds of
death increase 2.5 times for each gram decrement in
postoperative Hb level. Interestingly, no deaths occurred
in 99 patients with postoperative Hb levels between 7.1
and 8.0 g per dL. The upper 95-percent CI is compatible
with a rate of death no greater than 3.7 percent. However,
the morbidity rate was significant, 9.4 percent (95% CI,
4.4-17.0%).
The study also found that mortality and morbidity
rose sharply below postoperative Hb level of 5 to 6 g per
dL. These results are consistent with an analysis of case
reports in humans. Furthermore, studies in young volunteers undergoing isovolemic hemodilution to a Hb level
of 5 g per dL suggest that most will tolerate this blood
level, although transient, asymptomatic electrocardiogram changes were found in 5 of 87 subjects.19,20 These
results are consistent with animal data as well.
We were unable to identify in the literature any other
consecutive series of patients who decline blood transfusion. An analysis of case reports involving Jehovahs Witnesses from 1970 through early 1993 found 61 reports of
patients with Hb levels 8 g per dL.10 Death occurred in
79 percent of patients and anemia was the designated
cause in nearly half of the patients. Nearly all of these
deaths occurred in patients with Hb levels 5 g/dL. We
chose not to try to classify the cause of death in this study
population because it may be inaccurate. There are several case reports since 1993 of medical and surgical patients surviving with Hb levels of 2.0 to 5.0 g per dL, often
with use of such extreme measures as hypotensive anesthesia, hypothermia, muscle paralysis, and sedation.21-26
Increased cardiac output, decreased peripheral vascular resistance, and increased release of oxygen by RBCs
are physiologic changes that occur in response to anemia.27-35 There are conflicting data regarding the level of
anemia of which these physiologic changes occur. Some
studies suggest that cardiac output rises when the Hb
level is in the range of 9 to 10 g per dL,36 while other data
suggest that the Hb level must be below 7 or 8 g per dL for
these changes to occur.19,37,38 It is likely that compensation begins at different Hb levels depending on age, comorbidity, volume status, and medications. Results from
this analysis suggest inadequate compensation at very
low blood counts.
Prior studies in animals and humans suggest that the
presence of cardiovascular disease increases the risk associated with anemia. In healthy animals, electrocardiograph changes consistent with ischemia are seen at Hb
below 5 g per dL, while lactate production, depressed
ventricular function, and deaths have been observed at
Hb levels of 3 g per dL or lower.39-41 However, in dogs
with experimentally induced coronary stenosis varying
from 50 to 80 percent, ST segment changes and/or locally
depressed cardiac function occurred at Hb levels in the
range of 7 to 10 g per dL.42 This finding in animals was
confirmed in the previous analysis of these data which
showed an interaction between preoperative Hb level
and cardiovascular disease. We did not replicate the findings of an interaction between cardiovascular disease and
Hb level.12,43-45 While the trend was consistent with prior
analyses, this study had far fewer subjects and therefore
less power to identify an association.
This study has several other limitations. First, it is
possible that we have not adequately controlled for differences between patients with different Hb levels despite adjusting for multiple factors including age, cardioVolume 42, July 2002 TRANSFUSION
815
CARSON ET AL.
TABLE 3. Mortality stratified by postoperative Hb level (n = 300)
Postoperative
Hb (g/dL)
1.1-2.0
2.1-3.0
3.1-4.0
4.1-5.0
5.1-6.0
6.1-7.0
7.1-8.0
Total study
population
7
24
28
32
54
56
99
30-day in-hospital
mortality*
7 (100)
13 (54.2)
7 (25.0)
11 (34.4)
5 (9.3)
5 (8.9)
0 (0)
No cardiovascular disease
(n = 230)
30-day in-hospital
Number
mortality, n (%)
5
5 (100)
19
10 (52.6)
20
2 (10.0)
20
4 (20.0)
40
3 (7.5)
44
5 (11.4)
82
0 (0)
Cardiovascular disease
(n = 70)
30-day in-hospital
Number
mortality*
2
2 (100)
5
3 (60.0)
8
5 (62.5)
12
7 (58.3)
14
2 (14.3)
12
0 (0)
17
0 (0)
* Results reported as number (%).
TABLE 4. Mortality or morbidity stratified by postoperative Hb level*
Postoperative
Hb (g/dL)
1.1-2.0
2.1-3.0
3.1-4.0
4.1-5.0
5.1-6.0
6.1-7.0
7.1-8.0
Total study
population
4
12
19
26
49
50
96
30-day in-hospital
mortality and/or morbidity
4 (100)
11 (91.7)
10 (52.6)
15 (57.7)
14 (28.6)
11 (22.0)
9 (9.4)
No cardiovascular disease
(n = 199)
30-day in-hospital
Number
mortality and/or morbidity
2
2 (100)
9
8 (88.9)
14
6 (42.9)
18
9 (50.0)
34
8 (23.5)
40
9 (22.5)
82
8 (9.8)
Cardiovascular disease
(n = 57)
30-day in-hospital
Number
mortality and/or morbidity
2
2 (100)
3
3 (100)
5
4 (80.0)
8
6 (75.0)
15
6 (40.0)
10
2 (20.0)
14
1 (7.1)
* Analysis limited to multicenter data (n = 256); postoperative Hb is prior to event.
Defined as arrhythmia, congestive heart failure; myocardial infarction, bacteremia, pneumonia, deep wound infection, or death; 74 patients
with at least one event. Data reported as number (%).
vascular disease, and APACHE II score (an overall
measure of physiologic state and comorbidity). Second,
42.8 percent of patients in the original cohorts never had
a postoperative Hb level recorded. Thus, it is possible that
patients who might have had a low postoperative Hb
level would have been missed because the test was not
performed in patients who were doing well. However, it is
improbable that many patients were missed because
postoperative Hb levels are routinely performed in patients with significant blood loss and the mortality was
very low is this subset of patients (0.8%). Third, patients
included in this analysis were hospitalized up to 20 years
ago. It is likely that perioperative care has improved during this time period so that a similar patient cared for
today might have lower mortality. However, even if modern care would reduce mortality by 20 percent, patients
with very low counts would still have a very high death
rate. Fourth, despite starting with 300 patients in this
study, the numbers of patients and outcomes in each of
the Hb level categories were relatively small, which reduces the precision of the estimate of risk. Fifth, it would
have been preferable to use 30-day mortality instead of
in-hospital mortality up to 30 days. This was necessary
because we did not have information on deaths after discharge in the single-hospital cohort. However, when we
compared the number of deaths by use of the two defi816
TRANSFUSION
Volume 42, July 2002
nitions in the multicenter cohort, the results were almost
identical. Sixth, we did not collect information on delirium or stroke which may be associated with anemia.
Seventh, it would have been preferable to control for time
of Hb level by use of time-dependent covariates, but this
was not possible since the necessary Hb values were not
performed. Finally, it is possible that the underlying illness that led to the low Hb level may be responsible for
the mortality or morbidity rather than the adverse effect
of anemia. Our analysis is adjusted for age, cardiovascular disease, and illness burden as measured by the
APACHE II score and suggests an increase in mortality
and morbidity as the nadir Hb falls. However, a clinical
trial in which patients receive transfusion to increase Hb
level would be necessary to definitively answer if anemia
is responsible for the rising mortality and morbidity.
We can only speculate if blood transfusion would
modify the mortality and morbidity, since none of these
patients accepted blood transfusion. However, it seems
likely, although unproven, that transfusion would improve outcome in patients with Hb levels less than 5 g per
dL. It is less clear if blood transfusion would have impacted outcome in patients with higher blood counts. In
patients with Hb levels between 5 and 7 g per dL, the
mortality was about 9 percent. Certainly, this death rate is
unacceptably high in most surgical patients. Even in pa-
PATIENT OUTCOME WITH VERY LOW Hb LEVEL
tients with Hb levels between 7 and 8 g per dL, in whom
we found no deaths, a morbidity rate of 9.4 percent is
much too high. One clinical trial in intensive care unit
patients found that mortality is not increased if transfusion is withheld down to Hb levels of 7 g per dL. Further
prospective randomized trials are needed in surgical patients to determine the transfusion threshold that minimizes mortality and morbidity and optimizes functional
recovery.
The trend in blood management is to minimize
blood use. Many hospitals are implementing bloodless
medicine and surgery programs. Data from this study can
be used to weigh risk from anemia and to inform patients
that mortality and morbidity are extremely high with very
low blood counts. Despite the impressive advances in
critical care, the physiology of progressive anemia remains clear. There is a level below which adequate compensation for reduced oxygen-carrying capacity is no
longer adequate, leading to ischemia and eventual death.
The essential observation is that mortality and morbidity
remain extremely high with very low Hb levels.
REFERENCES
1. Toy P, Feiner J, Viele MK, et al. Fatigue during acute isovolemic anemia in healthy, resting humans. Transfusion
2000;40:457-60.
2. Weiskopf RB, Kramer JH, Viele M, et al. Acute severe isovolemic anemia impairs cognitive function and memory
in humans. Anesthesiology 2000;92:1646-52.
10. Viele MK, Weiskopf RB. What can we learn about the
need for transfusion from patients who refuse blood? The
experience with Jehovahs Witnesses. Transfusion 1994;34:
396-401.
11. Carson JL, Poses RM, Spence RK, Bonavita G. Severity of
anaemia and operative mortality and morbidity. Lancet
1988;1:727-9.
12. Carson JL, Duff A, Poses RM, et al. Effect of anaemia and
cardiovascular disease on surgical mortality and morbidity. Lancet 1996;348:1055-60.
13. Crow RS, Prineas RJ, Jacobs DR Jr, Blackburn H. A new
epidemiologic classification system for interim myocardial
infarction from serial electrocardiographic changes. Am J
Cardiol 1989;64:454-61.
14. Knaus WA, Draper EA, Wagner DP, Zimmerman JE. An
evaluation of outcome from intensive care in major medical centers. Ann Intern Med 1986;104:410-8.
15. Goldman L, Caldera DL, Nussbaum SR, et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med 1977;297:845-50.
16. Fleiss JL. Statistical methods for rates and proportions.
New York: Wiley; 1981.
17. Kahn HA, Sempos CT. Statistical methods in epidemiology. New York: Oxford University Press; 1989.
18. Carson JL, Duff A, Berlin JA, et al. Perioperative blood
transfusion and postoperative mortality. JAMA 1998;279:
199-205.
randomized, controlled clinical trial of transfusion requirements in critical care: transfusion requirements in
19. Weiskopf RB, Viele MK, Feiner J, et al. Human cardiovascular and metabolic response to acute, severe isovolemic
anemia. JAMA 1998;279:217-21, erratum in JAMA 1998;
280:1404.
20. Leung JM, Weiskopf RB, Feiner J, et al. Electrocardiographic ST-segment changes during acute, severe isovolemic hemodilution in humans. Anesthesiology 2000;93:
1004-10.
21. Baker CE, Kelly GD, Perkins GD. Perioperative care of a
Jehovahs Witness with a leaking abdominal aortic aneurysm. Br J Anaesthesiol 1998;81:256-9.
22. Cullis JO, Duncombe AS, Dudley JM, et al. Acute leukaemia in Jehovahs Witnesses. Br J Haematol 1998;100:664-8.
23. McLoughlin PL, Cope TM, Harrison JC. Hyperbaric oxygen therapy in the management of severe acute anaemia
in a Jehovahs witness. Anaesthesia 1999;54:891-5.
24. Pivalizza EG, Tjia IM, Juneja HS, et al. Elective splenectomy in an anemic Jehovahs Witness patient with cirrhosis. Anesthesiol Analges 1998;87:529-30.
25. Rupp RE, Ebraheim NA, Saddemi SR, et al. Management
of a multiply injured Jehovahs Witness with severe acute
anemia. Orthop Rev 1993;22:847-50.
26. Victorino G, Wisner DH. Jehovahs Witnesses: unique
problems in a unique trauma population. J Am Coll Surg
1997;184:458-68.
Critical Care Investigators, Canadian Critical Case Trials
Group]. N Engl J Med 1999;340:409-17, erratum in N Engl
27. Fowler NO, Holmes JC. Blood viscosity and cardiac output in acute experimental anemia. J Appl Physiol 1975;39:
3. Topley E, Fisher MR. The illness of trauma. Br J Clin Pract
1956;10:770-6.
4. Blair SD, Janvrin SB, McCollum CN, et al. Effect of early
blood transfusion on gastrointestinal haemorrhage. Br J
Surg 1986;73:783-5.
5. Johnson RG, Thurer RL, Kruskall MS, et al. Comparison of
two transfusion strategies after elective operations for
myocardial revascularization. J Thorac Cardiovasc Surg
1992;104:307-14.
6. Hebert PC, Wells G, Marshall J, et al. Transfusion requirements in critical care: a pilot study. Canadian Critical
Care Trials Group. JAMA 1995;273:1439-44, erratum in
JAMA 1995;274:944.
7. Bush RL, Pevec WC, Holcroft JW. A prospective randomized trial limiting perioperative red blood cell transfusions
in vascular patients. Am J Surg 1997;174:143-8.
8. Carson JL, Terrin ML, Barton FB, et al. A pilot randomized trial comparing symptomatic vs. hemoglobin-leveldriven red blood cell transfusions following hip fracture.
Transfusion 1998;38:522-9.
9. Hebert PC, Wells G, Blajchman MA, et al. A multicenter,
J Med 1999;340:1056
453-6.
Volume 42, July 2002 TRANSFUSION
817
CARSON ET AL.
28. Geha AS. Coronary and cardiovascular dynamics and oxygen availability during acute normovolemic anemia. Surgery 1976;80:47-53.
29. Glick G, Plauth WH, Braunwald E. Role of the autonomic
nervous system in the circulatory response to acutely induced anemia in unanesthetized dogs. J Clin Invest 1964;
43:47-53.
30. Levine E, Rosen A, Sehgal L, et al. Physiologic effects of
acute anemia: implications for a reduced transfusion trigger. Transfusion 1990;30:11-4.
31. Messmer K, Sunder-Plassmann L, Jesch F, et al. Oxygen
supply to the tissues during limited normovolemic hemodilution. Res Exp Med (Berl) 1973;159:152-66.
37. Whitaker W. Some effects of severe chronic anemia on
the circulatory system. Q J Med 1956;25:175-83.
38. Varat MA, Adolph RJ. Fowler no. cardiovascular effects of
anemia. Am Heart J 1972;83:415-26.
39. Wilkerson DK, Rosen AL, Sehgal LR, et al. Limits of cardiac compensation in anemic baboons. Surgery 1988;103:
665-70.
40. Hagl S, Heimisch W, Meisner H, et al. The effect of hemodilution on regional myocardial function in the presence
of coronary stenosis. Basic Res Cardiol 1977;72:344-64.
41. Yoshikawa H, Powell WJ Jr, Bland JH, Lowenstein E. Effect
of acute anemia on experimental myocardial ischemia.
Am J Cardiol 1973;32:670-8.
32. Murray JF, Escobar E. Circulatory effects of blood viscosity: comparison of methemoglobinemia and anemia.
42. Anderson HT, Kessinger JM, McFarland WJ Jr, et al. Response of the hypertrophied heart to acute anemia and
J Appl Physiol 1968;25:594-9.
33. Murray JF, Rapaport E. Coronary blood flow and myocar-
coronary stenosis. Surgery 1978;84:8-15.
43. Nelson AH, Fleisher LA, Rosenbaum SH. Relationship be-
dial metabolism in acute experimental anaemia. Cardiovasc Res 1972;6:360-7.
34. Rodriguez JA, Chamorro GA, Rapaport E. Effect of isovolemic anemia on ventricular performance at rest and during exercise. J Appl Physiol 1974;36:28-33.
35. Wright CJ. The effects of severe progressive hemodilution
on regional blood flow and oxygen consumption. Surgery
1976;79:299-305.
36. Finch CA, Lenfant C. Oxygen transport in man. N Engl J
Med 1972;286:407-15.
tween postoperative anemia and cardiac morbidity in
high-risk vascular patients in the intensive care unit. Crit
Care Med 1993;21:860-6.
44. Hogue CW, Goodnough LT, Monk TG. Perioperative myocardial ischemic episodes are related to hematocrit level
in patients undergoing radical prostatectomy. Transfusion
1998;38:924-31.
45. Wu WC, Rathore SS, Wang Y, et al. Blood transfusion in
elderly patients with acute myocardial infarction. N Engl J
Med 2001;345:1230-6.
818
TRANSFUSION
Volume 42, July 2002
Vous aimerez peut-être aussi
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Spare Part PhilosophyDocument27 pagesSpare Part Philosophyavaisharma50% (2)
- Changed Report 2015 PDFDocument298 pagesChanged Report 2015 PDFAnonymous FKjeRG6AFnPas encore d'évaluation
- Guideline - Research ProposalDocument38 pagesGuideline - Research ProposalRASPas encore d'évaluation
- Art of War Day TradingDocument17 pagesArt of War Day TradingChrispen MoyoPas encore d'évaluation
- Bioinformatics Computing II: MotivationDocument7 pagesBioinformatics Computing II: MotivationTasmia SaleemPas encore d'évaluation
- SavannahHarbor5R Restoration Plan 11 10 2015Document119 pagesSavannahHarbor5R Restoration Plan 11 10 2015siamak dadashzadePas encore d'évaluation
- Sermon Manuscript Galatians 5:16-26Document9 pagesSermon Manuscript Galatians 5:16-26Nathaniel ParkerPas encore d'évaluation
- ET4254 Communications and Networking 1 - Tutorial Sheet 3 Short QuestionsDocument5 pagesET4254 Communications and Networking 1 - Tutorial Sheet 3 Short QuestionsMichael LeungPas encore d'évaluation
- Homeopatija I KancerDocument1 pageHomeopatija I KancermafkoPas encore d'évaluation
- Advocacy Firm Business Plan by SlidesgoDocument40 pagesAdvocacy Firm Business Plan by SlidesgoirinaPas encore d'évaluation
- Vieworks DR Panel BrochureDocument8 pagesVieworks DR Panel Brochuretito goodPas encore d'évaluation
- Natural Cataclysms and Global ProblemsDocument622 pagesNatural Cataclysms and Global ProblemsphphdPas encore d'évaluation
- Albert Roussel, Paul LandormyDocument18 pagesAlbert Roussel, Paul Landormymmarriuss7Pas encore d'évaluation
- EZ Water Calculator 3.0.2Document4 pagesEZ Water Calculator 3.0.2adriano70Pas encore d'évaluation
- RPH Week 31Document8 pagesRPH Week 31bbwowoPas encore d'évaluation
- Toshiba MotorsDocument16 pagesToshiba MotorsSergio Cabrera100% (1)
- Bgrim 1q2022Document56 pagesBgrim 1q2022Dianne SabadoPas encore d'évaluation
- Chapter 20 AP QuestionsDocument6 pagesChapter 20 AP QuestionsflorenciashuraPas encore d'évaluation
- Benjamin Franklin - The Indian Treaties (1938)Document450 pagesBenjamin Franklin - The Indian Treaties (1938)Spiritu SanctoPas encore d'évaluation
- Bubble Test Direct Pressure InserviceDocument3 pagesBubble Test Direct Pressure InserviceEdAlmPas encore d'évaluation
- Cool Fire Manual 45M620N2UK 01 PDFDocument198 pagesCool Fire Manual 45M620N2UK 01 PDFPaun MihaiPas encore d'évaluation
- A 138Document1 pageA 138pooja g pPas encore d'évaluation
- Coal Bottom Ash As Sand Replacement in ConcreteDocument9 pagesCoal Bottom Ash As Sand Replacement in ConcretexxqPas encore d'évaluation
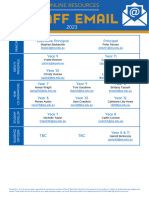
- 2023 Teacher Email ListDocument5 pages2023 Teacher Email ListmunazamfbsPas encore d'évaluation
- Eapp Melc 12Document31 pagesEapp Melc 12Christian Joseph HerreraPas encore d'évaluation
- Microwave EngineeringDocument2 pagesMicrowave Engineeringசுந்தர் சின்னையா0% (9)
- Impact of Government Policies and EthicsDocument24 pagesImpact of Government Policies and EthicsGunveen AbrolPas encore d'évaluation
- PetrifiedDocument13 pagesPetrifiedMarta GortPas encore d'évaluation
- Analytics Designer - Comment Deletion - SAP CommunityDocument6 pagesAnalytics Designer - Comment Deletion - SAP CommunityARPITA BISWASPas encore d'évaluation
- Fortigate Firewall Version 4 OSDocument122 pagesFortigate Firewall Version 4 OSSam Mani Jacob DPas encore d'évaluation