Académique Documents
Professionnel Documents
Culture Documents
Urinary
Transféré par
أحمدالشحاتCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Urinary
Transféré par
أحمدالشحاتDroits d'auteur :
Formats disponibles
What are the four parts of the
urinary system?
What are the 7 functions of the
urinary system?
Kidneys
Ureters
Bladder
Urethra
1. Regulation of water, electrolyte, and acid-base balance
2. Excretion of metabolic wastes, excess water, and excess
electrolytes in urine
3. Excretion of bioactive substances, including many drugs
4. Regulation of arterial blood pressure by secretion of renin
5. Secretion of erythropoietin
6. Conversion of the steroid prohormone vitamin D (produced in
the epidermis) into the active form (1,25-dihydroxycholcalciferol
or calcitrol or vitamin D3)
7. Gluconeogenesis during starvation or fasting
What structures are present at
the hilum of the kidney?
Adipose tissue in the renal
sinus, renal artery and vein,
renal pelvis branching into
major calyces
What does a renal lobe consist
of?
A renal (medullary) pyramid plus
the cortical tissue at its base
and along its sides (the renal
columns or columns of Bertin)
What does a renal lobule
consist of?
A medullary ray plus the
attached cortical tissue
What is the tip of each
medullary pyramid called?
Trace the path of blood flow
through the kidney.
Renal papilla
Renal artery --> Segmental artery --> Interlobar
artery --> Arcuate artery --> Interlobular artery
(cortical radial artery) --> Afferent arteriole -->
Glomerular capillaries --> Efferent arteriole -->
Peritubular capillaries OR Vasa recta --> Stellate
vein --> Interlobular vein --> Arcuate vein -->
Interlobar vein --> Segmental vein --> Renal vein
Glomerulonephritis
What is inflammation within the
glomerulus called?
Caused by humoral immune reactions -->
deposition of circulating antibody-antigen
complexes within the glomerulus OR binding of
circulating antibodies to glomerular antigens or
extraneous antigens depositied in the glomerulus
--> local inflammatory response
What are the two poles of a
renal corpuscle?
Vascular pole
Tubular pole
Describe the outer parietal layer
of the glomerular capsule.
Simple squamous epithelium
supported by a basal lamina
At the tubular pole, this epithelium
changes to the simple cuboidal
epithelium of the PCT.
Describe the visceral layer of
the glomerular capsule.
What are slit diaphragms?
Describe the basement
membrane of the glomerulus.
What are the 3 parts of the
filtration barrier?
Stellate (star-shaped) podocytes with primary
processes curving around lengths of
glomerular capillary; many parallel,
interdigitating pedicels (secondary processes)
extend from each primary process; filtration
slit pores exist between the pedicels and are
covered with slit diaphragms
Modified and specialized occluding or tight
junctions composed of nephrins, other proteins,
glycoproteins, and proteoglycans; projecting
from the cell membrane on either side of the
filtration slit, these polyanionic glycoproteins and
proteoglycans interact to form a series of
openings within the slit diaphragm, with a surface
that is negatively charged
Fusion of capillary- and podocyte-produced basal
laminae
Laminin and fibronectin connect to integrins of both
the podocyte and the endothelial cell membranes
Meshwork of corss-linked type IV collagen and large
proteoglycans restricts passage of large proteins
Polyanionic GAGs restrict filtration of organic anions
1. Fenestrations of the capillary endothelium =
block blood cells and platelets
2. Thick combined basal lamina (glomerular
basement membrane) = restricts large proteins
and some organic anions
3. Filtration slit diaphragms between pedicels =
restrict some small proteins and some organic
anions
1. Physical support of capillaries within the glomerulus
What are the functions of the
mesangium?
2. Contract in response to blood pressure changes, helping to
maintain optimal filtration rate
3. Phagocytosis of protein aggregates adhering to the glomerular
filter, including antibody-antigen complexes
4. Secretion of cytokines, prostaglandins, and other factors
important for immune defense and repair in the glomerulus
Describe the histological
features of the PCT.
Simple cuboidal epithelium; central nuclei;
cells well-stained with numerous
mitochondria (acidophilic, mostly associated
with basal foldings), prominent basal folds,
and lateral interdigitations; apical pits and
vesicles; long apical microvilli (brush border);
lumens often occluded
Which cells hydroxylate vitamin
D?
Proximal tubule cells
hydroxylate vitamin D and
release it to the capillaries.
Which cells produce
erythropoietin?
Fibroblastic interstitial cells in
cortical areas near the proximal
tubules
Describe the histological
features of the thin limbs of the
loop of Henle.
Simple squamous epithelium;
few mitochondria or organelles;
prominent lumens
Describe the histological
features of the thick ascending
limb of the loop of Henle.
Simple cuboidal epithlium; no
microvilli; many mitochondria
Describe the histological
features of the DCT.
Describe the histological
features of the collecting
system.
What is the thickening and loss
of function of the glomerular
basement membrane called?
What is sickle cell nephropathy?
Describe cells of the macula
densa.
Simple cuboidal epithelium; cells flatter
and smaller than in PCT; short microvilli
and basolateral folds but no brush
border; emptier lumens; more nuclei
seen in a section than in PCT (due to
smaller cell size); fewer mitochondria
than PCT, so less acidophilic
Principal cells = most abundant, cuboidal to
columnar; basolateral foldings; few organelles
and sparse microvilli with a primary cilium; palestaining, distinct cell membranes
Intercalated cells = few and scattered; slightly
darker staining; more abundant mitochondria
and projecting apical folds
Diabetic glomerulosclerosis
Produced as part of the systemic
microvascular sclerosis in diabetes mellitus
Leading cause of irreversible end-stage kidney
disease in the United States
Treatment requires transplant or artificial
hemodialysis
One of the most common problems caused
by sickle cell disease
Occurs when the affected erythrocytes sickle
in the vasa recta because of the low oxygen
tension there
Nephropathy results from renal infarcts,
usually within the renal papillae or pyramids
Columnar and closely packed; apical
nuclei, basal Golgi complexes, and a
more elaborate and varied system
of ion channels and transporters
than other DCT cells
Describe juxtaglomerular (JG)
cells.
What is the third cell type,
besides macula densa cells and
JG cells, that is part of the
juxtaglomerular apparatus?
Modified smooth muscle cells of the
tunica media of the afferent arteriole
where it contacts the macula densa
Secretory phenotype including more
rounded nuclei, rough ER, Golgi
complexes, and zymogen granules with
renin
Lacis cells = extraglomerular
mesangial cells that have many of
the same supportive, contractile,
and defensive functions as
mesangial cells within the
glomerulus
How do macula densa cells
respond to high GFR and high
luminal Na+ and Clconcentrations?
Release ATP, adenosine, and other
vasoactive compounds that trigger
constriction of the afferent
arteriole, lowering the glomerular
pressure and decreasing the GFR
Describe the interstitium of the
medulla.
Contains sparse myofibroblastlike cells in a matrix very rich in
hydrophilic hyaluronate
What is lithotripsy?
A procedure that uses focused
ultrasonic shock waves to
disintegrate kidney stones; can
cause significant renal damage
Define pyelonephritis.
Inflammation of the renal pelvis and
calyces caused by bacterial infections of
the urinary tract
Bacteria often move from one or more
minor calyx into the associated renal
papilla, causing accumulation of
neutrophils in the collecting ducts
What type of epithelium do the
calyces, renal pelvis, ureter, and
bladder have?
Stratified transitional epithelium
or urothelium
What are the 3 layers of
urothelium?
1. Single layer of small basal cells resting on a very
thin basement membrane
2. Intermediate region containing from one to
several layers of more columnar cells
3. Superficial layer of very large, bulbous cells
(umbrella cells) that are occasionally bi- or
multinucleated and are highly differentiated to
protect underlying cells against the cytotoxic effects
of hypertonic urine
Describe the apical membranes
of umbrella cells. What special
protein do they contain?
Asymmetric unit membranes where regions of the outer
lipid layer appear twice as thick as the inner leaflet;
these regions are composed of lipid rafts containing
mostly integral membrane proteins called uroplakins
that assemble into paracrystalline arrays of stiffened
plaques; these membranous plaques are impermeable
to water and protect the cytoplasm and underlying cells
from the hyperosmotic effects of urine; plaques are
hinged together by narrow regions of typical membrane
How does the urothelium
change when the bladder goes
from full to empty and vice
versa?
Full --> Empty
Mucosa folds extensively; individual umbrella cells decrease their
apical surface area by folding their membranes at the hinge
regions and internalizing the folded plaques in discoidal vesicles
Empty --> Full
Mucosa unfolds; discoidal vesicles rejoin the apical membranes of
umbrella cells, increasing their surface area as the cell shape
changes from round to flat; urothelium thins out as intermediate
cells are pushed and pulled laterally to accomodate the increased
volume of urine
What surrounds urothelium?
What is the muscle layer of the
bladder called?
Folded lamina propria
Submucosa
Dense sheath of interwoven
smooth muscle layers
Adventitia
Detrusor muscle
Cystitis
What is inflammation of the
bladder mucosa called?
What can chronic cystitis cause?
How do the ureters and the
urethra appear in cross section?
Can be caused by UTI,
immunodeficiency, urinary
catheterization, radiation, or
chemotherapy
Unstable urothelium with benign
urothelial changes involving
hyperplasia or metaplasia; bladder
cancer is usally some sort of
transitional cell carcinoma arising from
unstable urothelium
The prominent longitudinal folds of
these tubes appear as numerous
large projections into the lumen
such that the lumen border is thick
and wavy or squiggly
What are the three segments of
the male urethra?
Describe the prostatic urethra
Describe the membranous
urethra
Describe the spongy urethra
Describe the female urethra
1. Prostatic urethra
2. Membranous urethra
3. Spongy urethra
3-4 cm, extends through
prostate gland, lined by
urothelium
Short segment, passes through
an external sphincter of striated
muscle and is lined by stratified
columnar and pseudostratified
epithelium
About 15 cm long, enclosed within the
erectile tissue of the penis; lined with
stratified columnar and
pseudostratified columnar epithelium
with stratified squamous epithelium
distally
4-5 cm long, lined initially with
transitional epithelium, then by
stratified squamous epithelium and
some areas of pseudostratified
columnar epithelium; middle part is
surrounded by the external striated
muscle sphincter
What is infection of the urethra
called?
Urethritis
Often leads to cystitis in women
due to short urethra
What bacteria is usually the
culprit in a UTI?
Coliform bacteria or Chlamydia
What is pain or difficulty during
urination called?
Dysuria
Vous aimerez peut-être aussi
- اشهر اسئله لدكتور دينا شكرىDocument6 pagesاشهر اسئله لدكتور دينا شكرىأحمدالشحاتPas encore d'évaluation
- Wdhllohb Ihbknjk KJJGKJVM, MBJHV.L ., KBKJB, NGKJV,,.N, V HJKDocument1 pageWdhllohb Ihbknjk KJJGKJVM, MBJHV.L ., KBKJB, NGKJV,,.N, V HJKأحمدالشحاتPas encore d'évaluation
- OphthslDocument1 pageOphthslأحمدالشحاتPas encore d'évaluation
- MSSBDocument1 pageMSSBأحمدالشحاتPas encore d'évaluation
- Ent CaseDocument1 pageEnt CaseأحمدالشحاتPas encore d'évaluation
- MNBDocument1 pageMNBأحمدالشحاتPas encore d'évaluation
- New Text DocumentDocument3 pagesNew Text DocumentأحمدالشحاتPas encore d'évaluation
- New Text DocumentDocument6 pagesNew Text DocumentأحمدالشحاتPas encore d'évaluation
- New Text DocumentDocument1 pageNew Text DocumentأحمدالشحاتPas encore d'évaluation
- MCQ Bacteriology 31Document9 pagesMCQ Bacteriology 31أحمدالشحات100% (1)
- New Text DocumentDocument7 pagesNew Text DocumentأحمدالشحاتPas encore d'évaluation
- Accessory GI OrgansDocument10 pagesAccessory GI OrgansأحمدالشحاتPas encore d'évaluation
- Physiology of The Kidey NMMMMMMMMM N, MBNV NMBNN NMBNMBNDocument1 pagePhysiology of The Kidey NMMMMMMMMM N, MBNV NMBNN NMBNMBNأحمدالشحاتPas encore d'évaluation
- New Text DocumentDocument3 pagesNew Text DocumentأحمدالشحاتPas encore d'évaluation
- FalcoDocument1 pageFalcoأحمدالشحاتPas encore d'évaluation
- MRCP Material Drive PDFDocument2 pagesMRCP Material Drive PDFأحمدالشحات100% (1)
- Cell Injury and AdaptationDocument33 pagesCell Injury and AdaptationأحمدالشحاتPas encore d'évaluation
- Orthostatic HypotensionDocument9 pagesOrthostatic HypotensionأحمدالشحاتPas encore d'évaluation
- New Text DocumentDocument2 pagesNew Text DocumentأحمدالشحاتPas encore d'évaluation
- New Text DocumentDocument10 pagesNew Text DocumentأحمدالشحاتPas encore d'évaluation
- UsbnvDocument1 pageUsbnvأحمدالشحاتPas encore d'évaluation
- PharmacologyDocument9 pagesPharmacologyRVDPas encore d'évaluation
- Pass & SketchyDocument1 pagePass & Sketchyأحمدالشحات100% (1)
- New Text DocumentDocument4 pagesNew Text DocumentأحمدالشحاتPas encore d'évaluation
- Set 3c271ab3Document12 pagesSet 3c271ab3أحمدالشحاتPas encore d'évaluation
- SkinDocument6 pagesSkinأحمدالشحاتPas encore d'évaluation
- RespiratoryDocument14 pagesRespiratoryأحمدالشحاتPas encore d'évaluation
- ReproductiveDocument28 pagesReproductiveأحمدالشحاتPas encore d'évaluation
- GitDocument20 pagesGitأحمدالشحاتPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- S35 - Anil Kumar Pandey (J.K. Pathology) Near V Mart, Gandhi Ground, BADAUN243601 9058494498 / 8755328670Document6 pagesS35 - Anil Kumar Pandey (J.K. Pathology) Near V Mart, Gandhi Ground, BADAUN243601 9058494498 / 8755328670Satyabhan SinghPas encore d'évaluation
- Aborigines and Native Americans - A Compare and Contrast EssayDocument6 pagesAborigines and Native Americans - A Compare and Contrast Essaytwihard9360% (5)
- Prepared By: Dagdagan, Jeanne Frances SDocument12 pagesPrepared By: Dagdagan, Jeanne Frances SRachel Marie M. GaniaPas encore d'évaluation
- Immunization SchedulesDocument12 pagesImmunization SchedulesAnjali ThakurPas encore d'évaluation
- Scrub Typhus GuidelinesDocument40 pagesScrub Typhus GuidelinesnarasimhahanPas encore d'évaluation
- Pathogen Environmental Monitoring BookDocument54 pagesPathogen Environmental Monitoring BookAngga Prasetyo100% (1)
- A To Z Diseases LISTS For NEETPGDocument5 pagesA To Z Diseases LISTS For NEETPGQworldPas encore d'évaluation
- CBSE Class 9 Science Revision Notes Chapter - 13 Why Do We Fall Ill?Document3 pagesCBSE Class 9 Science Revision Notes Chapter - 13 Why Do We Fall Ill?pdf.downloadPas encore d'évaluation
- 1.mekanisme System Imun Sal. Cerna & Infeksi Rongga Mulut - KBKDocument32 pages1.mekanisme System Imun Sal. Cerna & Infeksi Rongga Mulut - KBKtyahudisaputriPas encore d'évaluation
- HPV Vaccination Against Cervical Cancer in Women Above 25 Years of AgeDocument9 pagesHPV Vaccination Against Cervical Cancer in Women Above 25 Years of Agegringo6969Pas encore d'évaluation
- Annual GAD Accomplishment Report 2014Document7 pagesAnnual GAD Accomplishment Report 2014jpllanesPas encore d'évaluation
- Bulb Mite Found in Garlic FieldsDocument2 pagesBulb Mite Found in Garlic FieldsRuni Ayu PPas encore d'évaluation
- The Main Themes of MicrobiologyDocument31 pagesThe Main Themes of MicrobiologyJhon VincentPas encore d'évaluation
- Sts FinalDocument6 pagesSts FinalNadine VilloserPas encore d'évaluation
- Anatomy and Phsyiology of MeningococcemiaDocument2 pagesAnatomy and Phsyiology of MeningococcemiaKevin Comahig100% (1)
- Guarino 2014Document21 pagesGuarino 2014ChangPas encore d'évaluation
- Covid-19 (Sars-Cov-2 Rna RT-PCR) : Result: Not Detected Remark: Individual Specimens Reference Range: Not DetectedDocument2 pagesCovid-19 (Sars-Cov-2 Rna RT-PCR) : Result: Not Detected Remark: Individual Specimens Reference Range: Not DetectedRonni PricePas encore d'évaluation
- Multisystem & Genetic - BoardsDocument10 pagesMultisystem & Genetic - BoardsSoojung NamPas encore d'évaluation
- 2 Antiviral ImmunityDocument23 pages2 Antiviral ImmunityVlad SmithPas encore d'évaluation
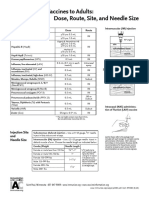
- Administering Vaccines To Adults: Dose, Route, Site, and Needle SizeDocument1 pageAdministering Vaccines To Adults: Dose, Route, Site, and Needle SizeAkashPas encore d'évaluation
- Ascaris LumbricoidesDocument33 pagesAscaris LumbricoidesRosi Gustina100% (5)
- Diagnosis Hepatitis PDFDocument18 pagesDiagnosis Hepatitis PDFYuendri IrawantoPas encore d'évaluation
- Spiritual Meaning of DiseasesDocument5 pagesSpiritual Meaning of DiseasesstudiocrocPas encore d'évaluation
- Reverse Vaccinology Basics and Applications 2157 7560.1000194Document5 pagesReverse Vaccinology Basics and Applications 2157 7560.1000194Yooobsan Nii barriitiPas encore d'évaluation
- Ambulance Activation PlanDocument14 pagesAmbulance Activation PlanticticPas encore d'évaluation
- PAT 202 Manual - 2009-10Document138 pagesPAT 202 Manual - 2009-10Ananda PreethiPas encore d'évaluation
- Introduction To Food Microbiology ADocument66 pagesIntroduction To Food Microbiology AoreaPas encore d'évaluation
- Understand How To Vaccines Work PDFDocument2 pagesUnderstand How To Vaccines Work PDFVonny RiskaPas encore d'évaluation
- Skin Infections and InfestationsDocument37 pagesSkin Infections and InfestationsAremu OlatayoPas encore d'évaluation
- Failure of Polio Eradication in PakistanDocument4 pagesFailure of Polio Eradication in PakistanAamir BugtiPas encore d'évaluation