Académique Documents
Professionnel Documents
Culture Documents
WHO RHR 14.18 Eng
Transféré par
Sasi KumarDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
WHO RHR 14.18 Eng
Transféré par
Sasi KumarDroits d'auteur :
Formats disponibles
ACTIVE MANAGEMENT OF THE THIRD
STAGE OF LABOUR
New WHO Recommendations Help to Focus Implementation1
WHO Recommendations for Active Management of the
Third Stage of Labour (AMTSL), 2012
The use of uterotonics for the prevention of postpartum haemorrhage (PPH)
during the third stage of labour is recommended for all births.
Oxytocin (10 IU, IV/IM) is the recommended uterotonic drug for the prevention of
PPH.
In settings where skilled birth attendants are available, controlled cord traction
(CCT) is recommended for vaginal births if the care provider and the parturient
woman regard a small reduction in blood loss and a small reduction in the
duration of the third stage of labour as important.
In settings where skilled birth attendants are unavailable, CCT is not
recommended.
Sustained uterine massage is not recommended as an intervention to prevent
PPH in women who have received prophylactic oxytocin.
Postpartum abdominal uterine tonus assessment for early identification of uterine
atony is recommended for all women.
CCT is the recommended method for removal of the placenta in caesarean
section.
In early 2012, the World Health Organization (WHO) held a technical consultation to review global evidence
related to the prevention and management of postpartum haemorrhage (PPH), which is still the most common
cause of death for women during pregnancy. Since 2007, WHO recommendations have supported active
management of the third stage of labour (AMTSL) as a critical intervention for PPH prevention. AMTSL has
become a central component of the PPH reduction strategies of governments around the world. As a result of the
2012 meeting, WHO has issued new recommendations regarding AMTSL, which can be used to strengthen and
focus the implementation of this lifesaving intervention.
What Is New and Different about AMTSL in These Recommendations?
AMTSL as a prophylactic intervention is composed of a package of three components or steps: 1) administration
of a uterotonic, preferably oxytocin, immediately after birth of the baby; 2) controlled cord traction (CCT) to
deliver the placenta; and 3) massage of the uterine fundus after the placenta is delivered. In 2012, the results of
a large WHO-directed, multi-centred clinical trial2 were published and showed that the most important AMTSL
component was the administration of a uterotonic.
The WHO trial also demonstrated that the addition of CCT did almost nothing to reduce haemorrhage. The
women who received CCT bled 10 mL less (on average) than women who delivered their placenta by their own
effort. There was a real difference, however, in terms of the length of the third stage: third stage was an average
of six minutes longer among those women who did not receive CCT. The authors acknowledged that this can be
an important amount of time, not so much for the woman, but for the management of busy labour and delivery
units.
Considering data from this trial and the existing evidence concerning the role of routine uterine massage in the
prevention of PPH, the WHO issued new recommendations clarifying that although administration of a
uterotonic remains central to the implementation of AMTSL, the performance of CCT and immediate fundal
massage are optional components.
World Health Organization. WHO recommendations for the prevention and treatment of postpartum haemorrhage. 2012. WHO: Geneva, Switzerland.
Gulmezoglu AM et al. Active management of the third stage of labour with and without controlled cord traction: a randomised, controlled, noninferiority trial. Lancet 2012; March 6, 2012. DOI:10.1016/S0140-6736(12)60206-2.
1
2
2013
WHO/RHR/14.18
Frequently Asked Questions about New AMTSL Recommendations
Does this mean that AMTSL is now something different or should be called by a new name?
No, it is not necessary to change the name or thinking about AMTSL, since the main components have not
changed and AMTSL is so widely understood and practiced. Such a change might result in confusion that could
slow down programme expansion. Instead, as programmes expand and improve the use of AMTSL, they should
put greater emphasis on the first component, the administration of a uterotonic.
Should national policies regarding AMTSL now be
changed?
National policies should continue to promote AMTSL and ensure
that systems are in place to monitor and track its
implementation. Policies should support the practice of AMTSL
in all maternity facilities of the health system and by all cadres
with midwifery skills. Policies should also direct the routine
availability of high-quality oxytocin and encourage storage of
oxytocin in a cool environment.
Should training materials and pre-service education
programmes be amended to reflect the new
recommendations?
Training and education programmes should continue to train
providers in all the elements of AMTSL, since CCT and fundal
massage remain important techniques that providers may need
to perform in other situations, for example, in the management
of retained placenta or PPH resulting from uterine atony. CCT
decreases the time to the delivery of the placenta, and therefore
may be important in busy labour wards or for a single provider.
A Refocused Approach to Prevention of PPH
Using AMTSL
Uterotonic: Ensure that every woman is offered a
uterotonic immediately after the delivery of the
baby. Oxytocin is the preferred drug to prevent
PPH.
Delayed cord clamping: Delay clamping the cord
for at least 1-3 minutes to reduce rates of infant
anaemia.
CCT: Perform CCT, if required.
Postpartum vigilance: Immediately assess
uterine tone to ensure a contracted uterus;
continue to check every 15 minutes for 2 hours.
If there is uterine atony, perform fundal massage
and monitor more frequently.
Oxytocin quality and supply: Ensure a continuous
supply of high-quality oxytocin. Maintain the cool
chain for oxytocin, and remember that potency is
reduced if oxytocin is exposed to heat for long
periods.
What does this mean for non-skilled providers?
Because of the clear evidence that the administration of a uterotonic is the most important component in
AMTSL, ministries of health should put in place policies and programmes to ensure that every woman is offered
a uterotonic immediately after birthwhether she delivers in a facility with a skilled provider or at home in the
presence of a non-skilled provider. This can be done through the promotion of AMTSL in facilities and the
development of community-based programmes for the use of misoprostol for women who deliver at home. These
kinds of efforts can increase coverage to ensure that close to 100% of pregnant women are protected from lifethreatening PPH.
If we have a concern about the quality of oxytocin in our facilities, what should we do?
Oxytocin potency deteriorates when it is exposed to temperatures greater than 30C for prolonged periods of
time. For this reason, oxytocin should be distributed and stored along a cool chain. Oxytocin can be stored at
room temperature in the labour unit for limited periods, as long as health managers routinely check and rotate
stock and monitor drug quality.
Implications for Policy, Training and Service Delivery
AMTSL has not changed.
Although these new WHO recommendations highlight the importance of the
Instead, there is now a
greater emphasis on the use
administration of a uterotonic in the prevention of PPH, they in fact do not
of a uterotonic at every birth.
suggest that there should be a change in how providers are trained in AMTSL
or how AMTSL is implemented in health care facilities that provide delivery
services. These recommendations clarify the most important components of AMTSL and suggest that there
should be an expanded emphasis on ensuring that every woman, regardless of where she delivers, is offered a
high-quality uterotonic at the time of birth. This emphasis can both increase coverage, by expanding the
number of women who can be provided a uterotonic and thus be protected from PPH, and increase quality, by
allowing programme managers and supervisors to focus on the most effective components in the package of care.
This report was made possible by the generous support of the American people through the United States Agency for International
Development (USAID), under the terms of the Leader with Associates Cooperative Agreement GHS-A-00-08-00002-00. The contents are the
responsibility of the Maternal and Child Health Integrated Program (MCHIP) and do not necessarily reflect the views of USAID or the United
States Government.
The Maternal and Child Health Integrated Program (MCHIP) is the USAID Bureau for Global Healths flagship maternal, neonatal and child
health (MNCH) program. MCHIP supports programming in maternal, newborn and child health, immunization, family planning, malaria,
nutrition, and HIV/AIDS, and strongly encourages opportunities for integration. Cross-cutting technical areas include water, sanitation,
hygiene, urban health and health systems strengthening.
For further information on this brief, please contact info@mchip.net.
For further information on the WHO guidelines, please contact reproductivehealth@who.int.
Vous aimerez peut-être aussi
- AMTSL BrieferDocument2 pagesAMTSL BrieferNewborn2013Pas encore d'évaluation
- PPH Briefer (Amtsl)Document2 pagesPPH Briefer (Amtsl)Lina AbuarqoubPas encore d'évaluation
- International Journal of Gynecology and Obstetrics: Özge Tunçalp, João Paulo Souza, Metin GülmezogluDocument3 pagesInternational Journal of Gynecology and Obstetrics: Özge Tunçalp, João Paulo Souza, Metin GülmezogluDaniel Ramirez QuintanaPas encore d'évaluation
- WHO 2013 PPH HighlightsDocument4 pagesWHO 2013 PPH HighlightsNimeJi B'leaf 윤 재Pas encore d'évaluation
- Postpartum Hemorrhage in Emergency Medicine Treatment & Management - Approach Considerations, Prehospital Care, Emergency Department CareDocument6 pagesPostpartum Hemorrhage in Emergency Medicine Treatment & Management - Approach Considerations, Prehospital Care, Emergency Department CareLUTFI ANNUR W A - 056Pas encore d'évaluation
- RHL - WHO Recommendation On The Use of Uterine Massage For The Treatment of Postpartum Haemorrhage - 2018-04-04Document4 pagesRHL - WHO Recommendation On The Use of Uterine Massage For The Treatment of Postpartum Haemorrhage - 2018-04-04tamiPas encore d'évaluation
- Figo PPHDocument14 pagesFigo PPHBima GhovaroliyPas encore d'évaluation
- Research Proposal o NishaDocument14 pagesResearch Proposal o NishaNishaThakuri100% (1)
- WHO Labour Care GuideDocument34 pagesWHO Labour Care GuideAnkita Singh100% (1)
- Evidenced Based Practice and Research PrioritiesDocument20 pagesEvidenced Based Practice and Research Prioritiesjyoti dhangalPas encore d'évaluation
- Current Trends in ObstetricsDocument6 pagesCurrent Trends in ObstetricsShyrra Edades Pinder100% (1)
- FFPRHC Guidance (July 2004) Contraceptive Choices For Breastfeeding WomenDocument9 pagesFFPRHC Guidance (July 2004) Contraceptive Choices For Breastfeeding Womenastuti susantiPas encore d'évaluation
- Chapter 3 EincDocument31 pagesChapter 3 EincHaru YukiPas encore d'évaluation
- Guideline On Anaesthesia and Sedation in Breastfeeding Women 2020 Guideline From The Association of AnaesthetistsDocument12 pagesGuideline On Anaesthesia and Sedation in Breastfeeding Women 2020 Guideline From The Association of Anaesthetistsantonio123valenciaPas encore d'évaluation
- Anaesthesia - 2020 - Mitchell - Guideline On Anaesthesia and Sedation in Breastfeeding Women 2020Document12 pagesAnaesthesia - 2020 - Mitchell - Guideline On Anaesthesia and Sedation in Breastfeeding Women 2020ANGELICAPas encore d'évaluation
- Hyperstimulation Management SBUHB 2022 Final CElisDocument7 pagesHyperstimulation Management SBUHB 2022 Final CElisantidius johnPas encore d'évaluation
- WHO PPHDocument62 pagesWHO PPHAchyut SharmaPas encore d'évaluation
- Souza - New WHO PPH GuidelinesDocument21 pagesSouza - New WHO PPH GuidelinesDhaka2012Pas encore d'évaluation
- Tun-Alp Et al-2017-BJOG ANCguidelinecommentaryDocument3 pagesTun-Alp Et al-2017-BJOG ANCguidelinecommentaryFitria NurwulansariPas encore d'évaluation
- FIGO Statement Uterine Atony Uterotonics PPH ENDocument5 pagesFIGO Statement Uterine Atony Uterotonics PPH ENSOFIA MORALESPas encore d'évaluation
- Prevention of Postpartum HemorrhageDocument6 pagesPrevention of Postpartum HemorrhageMarco TahirPas encore d'évaluation
- Preoperative FastingDocument14 pagesPreoperative FastingBrenda BernalPas encore d'évaluation
- WHO Recommendations On Antenatal Care For A Positive Pregnancy Experience 1Document14 pagesWHO Recommendations On Antenatal Care For A Positive Pregnancy Experience 1Thessa Yunisio PutriPas encore d'évaluation
- Guidelines On 8 Key Evidence Based Practices During Labour - 353Document35 pagesGuidelines On 8 Key Evidence Based Practices During Labour - 353National Child Health Resource Centre (NCHRC)Pas encore d'évaluation
- Management of Postpartum Haemorrhage (C-Obs 43) Amended May 2015Document13 pagesManagement of Postpartum Haemorrhage (C-Obs 43) Amended May 2015Emmanuel RecodoPas encore d'évaluation
- Addendum ALSO Tanzania RevisedDocument43 pagesAddendum ALSO Tanzania RevisedviaereaPas encore d'évaluation
- Retained Placenta Guideline For The Diagnosis and Management ofDocument8 pagesRetained Placenta Guideline For The Diagnosis and Management ofPamelaPas encore d'évaluation
- Management of Postpartum Haemorrhage (C-Obs 43) Review March 14Document13 pagesManagement of Postpartum Haemorrhage (C-Obs 43) Review March 14Simon AhmadpourPas encore d'évaluation
- Um - Haemorrhage/cd001337 - Diazv - Com/en/: SumberDocument4 pagesUm - Haemorrhage/cd001337 - Diazv - Com/en/: SumberrifkialbanaPas encore d'évaluation
- Antenatal Care BJOGDocument3 pagesAntenatal Care BJOGBusyra HanimPas encore d'évaluation
- ThesisDocument11 pagesThesispriyankaPas encore d'évaluation
- Induction of Labor 1Document36 pagesInduction of Labor 1Jessy JoltuwuPas encore d'évaluation
- Carbetocin For The Prevention of Postpartum Hemorrhage A Systematic ReviewDocument7 pagesCarbetocin For The Prevention of Postpartum Hemorrhage A Systematic ReviewOscar Gregorio Coronado MacdanielPas encore d'évaluation
- Acute TocolysisDocument6 pagesAcute Tocolysisverogalung100% (1)
- AO 2009 0025 Essential Newborn CareDocument15 pagesAO 2009 0025 Essential Newborn Carejulesubayubay542895% (21)
- Prolonged LaborDocument8 pagesProlonged LaborMisnariahIdrusPas encore d'évaluation
- Evaluates Administration of Oxytocin Drug in Maternity and Its Implications: Short Article ReviewDocument7 pagesEvaluates Administration of Oxytocin Drug in Maternity and Its Implications: Short Article Reviewindex PubPas encore d'évaluation
- International Midwives DayDocument48 pagesInternational Midwives Daymikegrace02Pas encore d'évaluation
- WHO Recommendations On Antenatal Care For A Positive Pregnancy Experience: SummaryDocument10 pagesWHO Recommendations On Antenatal Care For A Positive Pregnancy Experience: SummaryShalim BagusPas encore d'évaluation
- Induction of Labour Techniq SADocument18 pagesInduction of Labour Techniq SAPujanaWiaktaPas encore d'évaluation
- Benefits & Issues With Birth Control - Based On The Teachings Of Dr. Andrew Huberman: A Double-Edged Sword – Discovering The Positives And PitfallsD'EverandBenefits & Issues With Birth Control - Based On The Teachings Of Dr. Andrew Huberman: A Double-Edged Sword – Discovering The Positives And PitfallsPas encore d'évaluation
- Integrated Essential Maternal and Newborn CareDocument8 pagesIntegrated Essential Maternal and Newborn Carekhatedeleon100% (1)
- Advancement in Partograph WHO's Labor Care GuideDocument7 pagesAdvancement in Partograph WHO's Labor Care GuideSujan ThapaPas encore d'évaluation
- Tocolytic Treatment in PregnancyDocument21 pagesTocolytic Treatment in PregnancyxxdrivexxPas encore d'évaluation
- Two Up Cont CPG Intrapartum PDFDocument98 pagesTwo Up Cont CPG Intrapartum PDFjojolilimomoPas encore d'évaluation
- WHO Recommendation On Techniques For Preventing Perineal Trauma During Labour - RHL PDFDocument19 pagesWHO Recommendation On Techniques For Preventing Perineal Trauma During Labour - RHL PDFsaksPas encore d'évaluation
- Active Management of 3RD Stage of LaborDocument7 pagesActive Management of 3RD Stage of LaborFarheen khanPas encore d'évaluation
- A Study On Active Management of Third Stage of Labour As Per WHO Guidelines: Efficacy and ComplicationsDocument4 pagesA Study On Active Management of Third Stage of Labour As Per WHO Guidelines: Efficacy and ComplicationsAudioBhaskara TitalessyPas encore d'évaluation
- MCN Lab WRDocument101 pagesMCN Lab WRMaui TabuzoPas encore d'évaluation
- Different Modalities in First Stage Enhancement of LaborDocument4 pagesDifferent Modalities in First Stage Enhancement of LaborTI Journals PublishingPas encore d'évaluation
- A Descriptive Study To Assess The Knowledge and Practice of Nurses Regarding Active Management of Third Stage of Labour at The Selected Hospitals of PunjabDocument4 pagesA Descriptive Study To Assess The Knowledge and Practice of Nurses Regarding Active Management of Third Stage of Labour at The Selected Hospitals of PunjabEditor IJTSRDPas encore d'évaluation
- Manajemen Kala III PDFDocument2 pagesManajemen Kala III PDFWiwik'RatnaSariPratiwi'Pas encore d'évaluation
- Antenatal Corticosteroids BriefDocument2 pagesAntenatal Corticosteroids BriefNewborn2013Pas encore d'évaluation
- ACS Advocacy BrieferDocument2 pagesACS Advocacy BrieferNewborn2013Pas encore d'évaluation
- Sagesorg-Guidelines For The Use of Laparoscopy During PregnancyDocument32 pagesSagesorg-Guidelines For The Use of Laparoscopy During PregnancyLuis Acosta CumberbatchPas encore d'évaluation
- Guidelines For Diagnosis, Treatment, and Use of Laparoscopy For Surgical Problems During Pregnancy PDFDocument23 pagesGuidelines For Diagnosis, Treatment, and Use of Laparoscopy For Surgical Problems During Pregnancy PDFMilton Baltodano SánchezPas encore d'évaluation
- Preconception Health and Care: A Life Course ApproachD'EverandPreconception Health and Care: A Life Course ApproachJill ShawePas encore d'évaluation
- Exercise and Sporting Activity During Pregnancy: Evidence-Based GuidelinesD'EverandExercise and Sporting Activity During Pregnancy: Evidence-Based GuidelinesRita Santos-RochaPas encore d'évaluation
- Bioche TopicsDocument4 pagesBioche TopicsSasi KumarPas encore d'évaluation
- Total Number of Questions: 2433 + 250 2683: Lippincott Target Jipmer 2 Edition - Adrplexus Medical Coaching CentreDocument2 pagesTotal Number of Questions: 2433 + 250 2683: Lippincott Target Jipmer 2 Edition - Adrplexus Medical Coaching CentreSasi KumarPas encore d'évaluation
- 80 (3) 210Document7 pages80 (3) 210Sasi KumarPas encore d'évaluation
- Errata List-I (1 - 10 Subjects) - Target Jipmer 2 EditionDocument9 pagesErrata List-I (1 - 10 Subjects) - Target Jipmer 2 Editiondhanj1921Pas encore d'évaluation
- Psychiatry TOPICS (21 No.) (2 Pages)Document2 pagesPsychiatry TOPICS (21 No.) (2 Pages)Sasi KumarPas encore d'évaluation
- Murray Sample ChapterDocument47 pagesMurray Sample ChapterSasi KumarPas encore d'évaluation
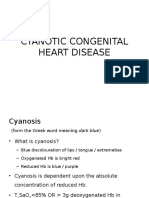
- Cyanotic Congenital Heart DiseaseDocument50 pagesCyanotic Congenital Heart DiseaseSasi KumarPas encore d'évaluation
- Plab PDFDocument18 pagesPlab PDFSasi Kumar100% (1)
- Sustainable Development Goals 2016Document3 pagesSustainable Development Goals 2016Sasi KumarPas encore d'évaluation
- LUNG 71 (1) Pp. 3-10Document8 pagesLUNG 71 (1) Pp. 3-10Sasi KumarPas encore d'évaluation
- Proposal For Sustainable Development Goals .Document13 pagesProposal For Sustainable Development Goals .Sasi KumarPas encore d'évaluation
- GeneDocument1 pageGeneSasi KumarPas encore d'évaluation
- MDGDocument1 pageMDGSasi KumarPas encore d'évaluation
- Ect in PregncyDocument13 pagesEct in PregncySasi KumarPas encore d'évaluation
- Minimal Change DiseaseDocument7 pagesMinimal Change DiseaseSasi KumarPas encore d'évaluation
- SPM Epidemiology of Infectious DiseasesDocument79 pagesSPM Epidemiology of Infectious DiseasesMUHAMMAD HASAN NAGRAPas encore d'évaluation
- Fundamental Critical Care Support Course (Structured Course of Society of Critical Care Medicine-USA)Document1 pageFundamental Critical Care Support Course (Structured Course of Society of Critical Care Medicine-USA)Sasi KumarPas encore d'évaluation
- DSM-5 (Table of Contents)Document9 pagesDSM-5 (Table of Contents)ParticipantObserver100% (1)
- AcarboseDocument6 pagesAcarboseSasi KumarPas encore d'évaluation
- Active Management Third Stage LaborDocument1 pageActive Management Third Stage LaborSasi KumarPas encore d'évaluation
- Acute Headache in The ED Evidence-Based Evaluation and Treatment OptionsDocument32 pagesAcute Headache in The ED Evidence-Based Evaluation and Treatment OptionsSasi KumarPas encore d'évaluation
- NRHMDocument17 pagesNRHMRithanya Shree Jaya100% (1)
- Orthopedics MCQs With AnswersDocument32 pagesOrthopedics MCQs With AnswerslanghalilafaPas encore d'évaluation
- Menckhoff - Orthopedic Pearls and Pitfalls Handout 3-25-13Document34 pagesMenckhoff - Orthopedic Pearls and Pitfalls Handout 3-25-13Sasi KumarPas encore d'évaluation
- 520Document28 pages520Sasi KumarPas encore d'évaluation
- 031CME06Document6 pages031CME06Sasi KumarPas encore d'évaluation
- E. Coli, Proteus, Pseudomonas, Klebsiella, Serratia, StaphylococciDocument1 pageE. Coli, Proteus, Pseudomonas, Klebsiella, Serratia, StaphylococciSasi KumarPas encore d'évaluation
- New Microsoft Word DocumentDocument25 pagesNew Microsoft Word DocumentSasi KumarPas encore d'évaluation
- 05 Special SitDocument32 pages05 Special SitSasi KumarPas encore d'évaluation
- Complete ES1 2023 Vol1Document334 pagesComplete ES1 2023 Vol1Chandu SeekalaPas encore d'évaluation
- FOB Price (Free On Board) - What Is FOB PriceDocument3 pagesFOB Price (Free On Board) - What Is FOB PriceFarooq BhuttaPas encore d'évaluation
- Amazon Go ReportDocument3 pagesAmazon Go ReportkatyaPas encore d'évaluation
- Our American HeritageDocument18 pagesOur American HeritageJeremiah Nayosan0% (1)
- Quotes For Essay and Ethics CompilationDocument5 pagesQuotes For Essay and Ethics CompilationAnkit Kumar SinghPas encore d'évaluation
- Notes: 1 Yorùbá Riddles in Performance: Content and ContextDocument25 pagesNotes: 1 Yorùbá Riddles in Performance: Content and ContextDofono ty NísèwèPas encore d'évaluation
- Auguste Comte - PPT PresentationDocument61 pagesAuguste Comte - PPT Presentationmikeiancu20023934100% (8)
- Safe Disposal of Hazardous Wastes Vol IDocument290 pagesSafe Disposal of Hazardous Wastes Vol IRodrigo BartoloPas encore d'évaluation
- Tallado V. ComelecDocument3 pagesTallado V. ComelecLorelain ImperialPas encore d'évaluation
- Par Vol2i10Document66 pagesPar Vol2i10Bakhita MaryamPas encore d'évaluation
- Group Floggers Outside The Flogger Abasto ShoppingDocument2 pagesGroup Floggers Outside The Flogger Abasto Shoppingarjona1009Pas encore d'évaluation
- 03 - UndercityDocument28 pages03 - UndercityJames Bayhylle100% (1)
- Vidrine Racism in AmericaDocument12 pagesVidrine Racism in Americaapi-512868919Pas encore d'évaluation
- How I Have Experienced The 2020: LockdownDocument3 pagesHow I Have Experienced The 2020: LockdownГеоргий КузнецовPas encore d'évaluation
- Philippine Law A Tapestry of Justice and HeritageDocument2 pagesPhilippine Law A Tapestry of Justice and HeritageKaren Faith MallariPas encore d'évaluation
- An Introduction To The "Mantra Śãstra": By: S.E. Gop ĀlāchārluDocument25 pagesAn Introduction To The "Mantra Śãstra": By: S.E. Gop ĀlāchārluKuldeep SharmaPas encore d'évaluation
- Income Tax CalculatorDocument11 pagesIncome Tax Calculatorsaty_76Pas encore d'évaluation
- BrochureDocument10 pagesBrochureSaurabh SahaiPas encore d'évaluation
- Hho Dry DiagramDocument7 pagesHho Dry Diagramdesertbloom100% (2)
- Against Open Merit: Punjab Public Service CommissionDocument2 pagesAgainst Open Merit: Punjab Public Service CommissionSohailMaherPas encore d'évaluation
- Jazzed About Christmas Level 2-3Document15 pagesJazzed About Christmas Level 2-3Amanda Atkins64% (14)
- G.R. No. 187512 June 13, 2012 Republic of The Phils Vs Yolanda Cadacio GranadaDocument7 pagesG.R. No. 187512 June 13, 2012 Republic of The Phils Vs Yolanda Cadacio GranadaDexter Lee GonzalesPas encore d'évaluation
- (Outstanding) (DDI) 9 Talent Management Best Practices - DDIDocument12 pages(Outstanding) (DDI) 9 Talent Management Best Practices - DDINguyen Thanh-LoanPas encore d'évaluation
- University Institute of Legal Studies: Jurisprudence-Austin'S Analytical Positivism 21LCT114Document15 pagesUniversity Institute of Legal Studies: Jurisprudence-Austin'S Analytical Positivism 21LCT114Harneet KaurPas encore d'évaluation
- P 141Document1 pageP 141Ma RlPas encore d'évaluation
- Contrast and Compare Napoleon (Animal Farm) and Big Brother (1984) Characters in George Orwell's MasterpiecesDocument2 pagesContrast and Compare Napoleon (Animal Farm) and Big Brother (1984) Characters in George Orwell's MasterpiecesTogay Balik100% (1)
- Suffixes in Hebrew: Gender and NumberDocument11 pagesSuffixes in Hebrew: Gender and Numberyuri bryanPas encore d'évaluation
- Levi Strass and Co v. Papikan Enterprises Trademark MSJDocument12 pagesLevi Strass and Co v. Papikan Enterprises Trademark MSJNorthern District of California BlogPas encore d'évaluation
- Moodys SC - Russian Banks M&ADocument12 pagesMoodys SC - Russian Banks M&AKsenia TerebkovaPas encore d'évaluation
- Journal Jul Dec14 Art4Document16 pagesJournal Jul Dec14 Art4paromita bhattacharjeePas encore d'évaluation