Académique Documents
Professionnel Documents
Culture Documents
Sedatives
Transféré par
alghashm001Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Sedatives
Transféré par
alghashm001Droits d'auteur :
Formats disponibles
I.
Sedative-Hypnotic Drugs: Overview
Sedatives, Hypnotics, Ethanol
PHTX 604
Include benzodiazepines, barbiturates, alcohols (ethanol, chloral hydrate)
L a u r a S i m -S e l l e y
Among the most widely prescribed drug classes
McGuire Hall, Room 324B
High doses depress respiration; additive with other CNS depressants
Chronic use can produce physical and psychological dependence
8 2 7 -0 4 6 4
ljsimsel@hsc.vcu.edu
General Depressants produce:
Learning Objectives
1. Differentiate among benzodiazepine and barbiturate classes regarding onset
and duration of action, mechanisms of action, route of administration, termination
of action and therapeutic indications
2. Describe advantages and disadvantages of benzodiazepine sedative hypnotics
in comparison with barbiturates
3. Describe dangers in sedative therapy and treatment of overdose
4. Discuss potential for abuse of sedative-hypnotics and prevention and treatment
of dependence
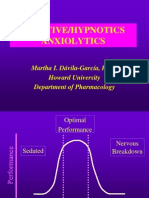
Sedation: decreases activity, modulates excitement, calms patient
produced by lowest doses of sedative-hypnotic drugs
Hypnosis (sleep): produce drowsiness and facilitate onset and
maintenance of sleep; ideally want sleep state that resembles natural and
from which patient can be easily aroused
all sedative hypnotics produce sleep at high doses
Therapeutic uses: anxiolytic, sleep-inducing; muscle relaxant, anticonvulsant
Therapeutic effects result from CNS actions
II. Mechanism of action: GABA A Receptor
GABA is the major inhibitory neurotransmitter in the CNS
Dose-dependent CNS depression that varies by drug
Lowest dose
sedation
Highest dose
hypnosis
anesthesia
coma
death
Linear for older sedative-hypnotics (barbiturates, ethanol)
Non-linear for newer drugs (benzodiazepines): requires proportionately increased
dose increments to get CNS depression therefore greater margin of safety
Biodisposition
Metabolized in the liver by P450 enzymes
phase I (oxidation): many have active metabolites with long half-lives
phase II (glucuronidation): excreted in urine
Pharmacokinetic properties differ for various benzodiazepines and affect their clinical
use
Affected by hepatic function (disease, age, increased/decreased enzyme activity)
3
Katzung; Basic & Clin. Pharm.
Mechanism of Action
III. Classes
Benzodiazepines and barbiturates bind to GABAA receptors
GABA receptor is also affected by general anesthetics, ethanol, inhaled drugs of
abuse, allopregnanolone (metabolite of progesterone)
A. Benzodiazepines
1. Characterized based on elimination half lives
a. short-acting (t1/2<6 hrs): short-lived or no active metabolites
triazolam (Halcion), midazolam (Versed)
Receptor
Ionotropic receptor composed of 5 subunits (pentamer) that assemble to
form a Cl- channel
Subunit diversity (8 classes with multiple isoforms = at least 18 subunits)
b. intermediate-acting (t1/2 6-24 hrs): short-lived or no active metabolites
temazepam (Restoril), lorazepam (Ativan), estazolam (Prosom)
c. : long-acting (t1/2 >24 hrs): long-lived active metabolites
flurazepam (Dalmane), diazepam (Valium), quazepam (Doral)
Isoforms have individual localizations in CNS
Receptor heterogeneity and in vivo data suggests that future drugs can be
developed to target specific effects (i.e. anxiolytic but not sedating)
2. Advantages over other sedative hypnotics
a. safety: limited capacity to produce profound and fatal CNS depression
b. less REM suppression
c. less tolerance and enzyme induction
Benzodiazepine drugs
3. Mechanism:
a. Benzodiazepine (BZ) site: potentiates GABA
actions
Anxiety:
Alprazolam (Xanax )
Chlordiazepoxide (Librium )
Chlorazepate (Tranxene )
Midazolam (Versed )
oral
intermediate
BZ sites: BZ1,BZ2,BZ3 (also referred to as
Omega1,2,3 )
short-acting
short-acting
most benzodiazepines bind to all types
zaleplon and zolpidem are BZ1-selective
Anxiety, sedation:
Diazepam (Valium )
Lorazepam (Ativan )
Insomnia:
Estazolam (Prosom )
Flurazepam (Dalmane )
Quazepam (Doral )
Temazepam (Restoril )
Triazolam (Halcion)
oral, i.v.
oral, i.v.
BZ site on the GABAA is receptor distinct from
the GABA binding site
long-acting
intermediate
Benzodiazepines do not directly activate the
receptor/channel, but increase the frequency of
Cl- channel opening produced by submaximal
oral
oral
intermediate
long-acting
long-acting
intermediate
short-acting
concentrations of GABA
Safety probably results from binding properties:
benzodiazepines do not have an effect on their
own, but require GABA
7
b. Drug Classification
Agonist: positive allosteric modulator that facilitates GABA actions by increasing Clconductance, shifts GABA concentration-response curve to left
Includes clinically useful benzodiazepines and endogenous agonist (endozepines)
Full agonist: produces maximal effect (i.e. diazepam)
Partial agonist: less than maximal effect (i.e. alpidem)
produce anti-anxiety effects with less sedation
4. Therapeutic Effects: CNS-mediated
a. Anxiety: general anxiety and panic disorders
b. Pre-Anesthetic (prep for surgery)
c. Anesthesia: diazepam, midazolam are used i.v. during anesthesia as adjuncts, but
do not produce anesthesia by themselves
d. Anti-convulsant
Inverse Agonist: negative allosteric modulators of GABA receptor function that
decrease Cl - conductance, shift GABA concentration-response curve to right
Example: -carbolines
Produce seizures and anxiety
e. Muscle relaxation
f. Alcohol Withdrawal Syndrome
g. Conscious sedation: i.v. diazepam, lorazepam, midazolam, produce muscle
relaxation and anterograde amnesia
Antagonist: flumazenil (Romazicon): has no effect on its own but blocks effects of
agonist/inverse agonist
Blocks benzodiazepines and zolpidem, but does not affect barbitu rates or
ethanol
Also endogenous compound (diazepam binding inhibitor (DBI))
Therapeutic uses: management of BZ overdose and reversal of sedative
effects produced by BZ during diagnostic/therapeutic procedures
Side Effects: agitation, confusion, dizziness, may precipitate withdrawal
Parenteral use associated with increased respiratory depression when used for
conscious sedation: monitor respiration and cardiovascular function
Parenteral diazepam can produce thrombophlebitis (due to vehicle for infusion:
polypropylene glycol); midazolam is water soluble therefore doesnt have this
effect
h. Insomnia: want to decrease sleep latency with minimal hangover
sedative-hypnotics usually decrease latency to sleep onset, increase duration of
stage 2 REM, decrease the duration of REM and slow-wave sleep
10
Long term treatment
side effects: BZ tolerance, next day confusion; may worsen sleep apnea
BZ and newer drugs preferred due to greater therapeutic index, less
Categories:
1. transient insomnia: <3 days, usually emotional or situational stressor
treatment: sleep hygiene, low dose hypnotics for 2-3 nights
note: use prior to event (i.e. exam) may impair performance
toxicity/overdose, less effect on sleep patterns, less abuse potential
short half life: patients with sleep onset insomnia but without significant
daytime anxiety (i.e. need to be effective all day)
2. short term insomnia 3 days- 3 weeks, usually personal stressor
treatment: sleep hygiene, adjunct hypnotic therapy (7-10 nights intermittently)
3. Long term insomnia >3 weeks, no specific stressor
non-pharm: sleep hygiene, exercise, relaxation training, behavioral modification
pharmacological: disadvantages tolerance, rebound insomnia after termination,
alters sleep patterns
BZ: decrease slow wave non -REM and REM (lesser)
barbiturates: decrease REM
11
long half life: patients with significant daytime anxiety who can tolerant
some sedation
To discontinue use after >2 weeks taper rather than withdraw
if using short half life BZ, switch to long half life BZ, then taper
may not have difficulty with zopiclone
12
5. Adverse Effects/Toxicity (may be increased in elderly)
D. Visual System: diplopia, nystagmus, blurred vision; contraindicated in narrow-
A. CNS depression : residual sedation, fatigue, drowsiness, confusion, ataxia
Anterograde amnesia: parenteral benzodiazepines (i.e. diazepam,
midazolam); oral triazolam has increased likelihood; flunitrazepam (Rohypnol)
Potentiates effects of other CNS depressants esp. problem with E TOH
impair driving and psychomotor skills
Paradoxical Stimulation: talkativeness, anxiety, nightmares,
tremulousness, hyperactivity, muscle spasms; more common in psychiatric patients
angle glaucoma (may be used with wide -angle glaucoma: more common type)
E. GI: cramps, pain
F. Reproduction: Sedative-hypnotics cross the placental barrier and are detectable
in breast milk
1st trimester: congenital malformations
Pre-delivery: large doses may produce hypothermia, hypotonia and mild
respiratory depression in neonate
B. Respiration: hypnotic doses of benzodiazepines dont depress respiration,
although higher doses may have some effect. Care should be taken in children,
those with impaired liver or lung function; additive effects with other CNS
depressants such as opioids or alcohol
C. Cardiovascular: minor in normal subjects; can decrease blood pressure
and heart rate at pre-anesthetic doses
13
6. Chronic Administration
14
c. Overdose: rare
a. Tolerance (decreased responsiveness to drug after repeated administration)
occurs with sedative-hypnotics
cross-tolerance to other CNS depressants
Treatment:
Emesis
Flumazenil (Romazicon): antagonist
i.v. administration (extensive 1st pass metabolism means that
effective oral dose can produce headache and dizziness)
may be incomplete reversal of respiratory depression; *note this
b. Dependence
Psychological dependence: most sedative-hypnotics are schedule III or IV
because of abuse liability due to anxiolysis, euphoria and disinhibition
could precipitate withdrawal in physically dependent individuals
7. Drug interactions:
Physiological dependence: chronic use of most sedative-hypnotics can lead to
dependence, characterized by a withdrawal syndrome (increased anxiety,
insomnia, and CNS excitability that can lead to convulsions)
abrupt withdrawal may produce irritability, dysphoria, tremors, anorexia,
dizziness esp. after sudden withdrawal
to avoid withdrawal, taper dose
additive depression with CNS depressants: alcohol, barbiturates, antipsychotics,
antidepressants, opiates, antihistamines, anticonvulsant
Cimetidine (Tagamet): inhibits metabolism of BZ
antagonist: flumazenil (Romazicon)
Smoking may decrease the effect of benzodiazepines (tar stim hepatic enzymes)
Benzodiazepines may
decrease the effect of levodopa
15
16
C. Barbiturates
*Due to their relative safety, benzodiazepines have largely replaced older
sedative-hypnotics (i.e. barbiturates)
Barbiturates: lack specificity in CNS, lower therapeutic index, frequent
tolerance, greater abuse liability, more drug interactions, no antagonist
1. Classes
a. ultrashort: <60 min
thiopental (Pentothal), methohexital (Brevital)
used as i.v. anesthetics
lipophilic = rapid onset of CNS effects, short duration of actions
b. short to intermediate
secobarbital (Seconal), pentobarbital (Nembutal)
oral or i.v. sedative hypnotic
c. long-acting
phenobarbital, mephobarbital (Mebaral), barbital
B. Novel benzodiazepine receptor agonists
structurally unrelated to benzodiazepines but bind to BZ binding site
1. Classes
a. zolpidem (Ambien)
BZ1(omega1)-selective
Used for short term management of insomnia
Minimal anticonvulsant or muscle relaxant effects
Additive with other CNS depressants
Less risk of tolerance and dependence than benzodiazepines
Side Effects: headache, drowsiness, dizziness
Fast onset; can be used as oral anxiolytic
Short acting : t1/2 ~2 hrs; effects last ~8hrs
b. zaleplon (Sonata)
BZ1 (omega1 )-selective
Decreases sleep latency but has little effect on sleep time or architecture
Rapid onset and short duration of action (t1/2 ~1hr); can use multiple doses
c. zolpicone (not in US)
increase the effect of digoxin, phenytoin, probenecid
17
2. Mechanism: facilitate GABA actions by increasing duration of channel opening
High doses may also directly open the channel
Promote BZ binding
Distinct from GABA and BZ sites
May also depress actions of excitatory neurotransmitters esp. glutamate (AMPA
receptors)
18
Therefore: overall effect to enhance inhibition and decrease exc itability
3. Pharmacological effects and clinical use
a. anesthesia (thiopental, methohexital)
b. anticonvulsant
c. sedative -analgesic combinations
sedatives do not produce analgesia, therefore may need combination
Fiorinal (butalbital/acetaminophen/caffeine)
Fiorinal #3 (butalbital/tylenol #3 (acetaminophen, codeine))
d. antagonize stimulant effects (ephedrine, dextroamphetamine, t heophylline)
e. sedative/hypnotic withdrawal (phenobarbital)
4. Factors affecting barbiturate action
a. lipid solubility (ultrashort > short > long)
b. interference with metabolism and excretion
c. drug interactions
1. additive with other CNS depressants
2. enzyme induction
5. Acute toxicity and treatment of overdose (often deliberate)
usually occurs at ~10X hypnotic dose (lower with ethanol)
a. dialysis: remove drug
b. supportive: maintain respiration, pH and fluid balance, body temp.
6. Tolerance
3-4 fold for hypnosis, less for lethality
cross dependence with other sedative hypnotics
pharmacodynamic (major) and pharmacokinetic (minor)
more tolerance two sedative and hypnotic effects than anticonvulsant and lethal
effects (i.e. therapeutic index decreases with tolerance)
7. Dependence and withdrawal
withdrawal: excitability, convulsions, delirium
also abuse potential
8. Contraindications
hepatic porphyria (defect in hemoglobin breakdown)
pulmonary disease
sensitivity
9. Drug interactions
CNS depression
additive CNS depression: most commonly ethanol
enzyme induction
19
20
D. Miscellaneous agents that resemble short-acting barbiturates
1. Chloral hydrate (Noctec, Somnos): active metabolite trichlo roethanol
2. Paraldehyde: treat delirium tremens in hospitalized patients
3. Meprobamate (Miltown, others): approved for anxiety, also used as night time
sedative
more similar to BZ, but greater abuse potential, decreased antianxiety effects
large doses: severe or fatal respiratory depression, hypotension, shock, heart
failure
meprobamate is a metabolite of carisoprodal (Soma)
4. Methaqualone (Quaalude)
5. Ethchlorvynol (Placidyl): short term treatment of insomnia
6. Bromide: first sedative-hypnotic agent (mid 19th century)
E. Misc. agents of lower efficacy
1. Antihistamines, Anticholinergics
a. less reliable as hypnotic
2. Melatonin: natural hormone, mild efficacy for sleep disorders and jet lag
3. Valerian, Kava kava: herbal product with sedative activity
21
Vous aimerez peut-être aussi
- Learning Hypnosis - Hypnosis Application for Coaches and TherapistsD'EverandLearning Hypnosis - Hypnosis Application for Coaches and TherapistsÉvaluation : 5 sur 5 étoiles5/5 (1)
- Antihypnotics and AnxiolyticsDocument12 pagesAntihypnotics and AnxiolyticsSabreena NordinPas encore d'évaluation
- SULPYCO Method: A New Quantum and Integrative Approach to DepressionD'EverandSULPYCO Method: A New Quantum and Integrative Approach to DepressionPas encore d'évaluation
- Sedative-Hypnotic Drugs: Dr. Hiwa K. Saaed, HD, Msc. PHDDocument51 pagesSedative-Hypnotic Drugs: Dr. Hiwa K. Saaed, HD, Msc. PHDHiwa Khidhir saaedPas encore d'évaluation
- Depression & Anxiety: What You Need To Know About Treatment with Medications, Herbs & SupplementsD'EverandDepression & Anxiety: What You Need To Know About Treatment with Medications, Herbs & SupplementsPas encore d'évaluation
- Sedative-Hypnotic Drugs: Department of Pharmacology Zhang YanmeiDocument30 pagesSedative-Hypnotic Drugs: Department of Pharmacology Zhang YanmeiKAVITA HOODAPas encore d'évaluation
- CNS Depressants: - Sedatives and Hypnotics - General Anesthetics - Narcotic AnalgesicsDocument118 pagesCNS Depressants: - Sedatives and Hypnotics - General Anesthetics - Narcotic Analgesicsbiruk getahunPas encore d'évaluation
- Sedative-Hypnotic DrugsDocument30 pagesSedative-Hypnotic DrugsdrfatimarizPas encore d'évaluation
- 2016 Pharmacology of Sedative-HypnoticDocument46 pages2016 Pharmacology of Sedative-HypnoticFansisca SiallaganPas encore d'évaluation
- Dr. Rahul Trivedi B.R.Nahata College of Pharmacy, Department of Pharmacy, Mandsaur UniversityDocument16 pagesDr. Rahul Trivedi B.R.Nahata College of Pharmacy, Department of Pharmacy, Mandsaur UniversityVampire VampirePas encore d'évaluation
- Anxiolytics Sedatives Hypnotics Pharm 3Document38 pagesAnxiolytics Sedatives Hypnotics Pharm 3Peter Harris100% (1)
- Anxiolytic DrugsDocument60 pagesAnxiolytic Drugsneleh grayPas encore d'évaluation
- Psychopharmacological AgentsDocument44 pagesPsychopharmacological Agentsbazet49Pas encore d'évaluation
- Sedative - HypnoticsDocument62 pagesSedative - HypnoticsvijayPas encore d'évaluation
- SEDATIVE - HYPNOTICS DRUGS - PharmaDocument66 pagesSEDATIVE - HYPNOTICS DRUGS - PharmaKenneth NuñezPas encore d'évaluation
- Sedative HynoticsDocument17 pagesSedative HynoticsAngel ShindePas encore d'évaluation
- Anxiolytic and Hypnotic DrugsDocument27 pagesAnxiolytic and Hypnotic DrugsEjaj SumitPas encore d'évaluation
- Pharmacology of Sedative-Hypnotics: DR - Datten Bangun, MSC, SPFK Dept - Farmakologi & Terapetik Fak - Kedokteran Uhn MedanDocument49 pagesPharmacology of Sedative-Hypnotics: DR - Datten Bangun, MSC, SPFK Dept - Farmakologi & Terapetik Fak - Kedokteran Uhn MedanGeorge AbrahamPas encore d'évaluation
- Sedative - HypnoticsDocument60 pagesSedative - HypnoticsNurul AinPas encore d'évaluation
- Anxiolytics & Hypnotics Drugs: Chapter FiveDocument21 pagesAnxiolytics & Hypnotics Drugs: Chapter FiveabrihamPas encore d'évaluation
- Lecture 28 - 3rd Asessment - Sedatives, HypnoticsDocument32 pagesLecture 28 - 3rd Asessment - Sedatives, Hypnoticsapi-3703352100% (1)
- Antianxiety SedativeDocument44 pagesAntianxiety Sedativemohsen mirdamadiPas encore d'évaluation
- 5 Sedative-Hypnotic DrugsDocument26 pages5 Sedative-Hypnotic DrugsDylan Panashe KwendaPas encore d'évaluation
- SedativeDocument15 pagesSedativeManul ShobujPas encore d'évaluation
- WEEK 6 7-CNS Medications StudentDocument83 pagesWEEK 6 7-CNS Medications Studentx8jdbj5gphPas encore d'évaluation
- Sedative & Hypnotics: Prof. Hanan Hagar Pharmacology Department Medical College King Saud UniversityDocument51 pagesSedative & Hypnotics: Prof. Hanan Hagar Pharmacology Department Medical College King Saud UniversityRose Ann Raquiza-PerantePas encore d'évaluation
- Sedative Hypnotic PoisoningDocument37 pagesSedative Hypnotic PoisoningDeepa WilliamPas encore d'évaluation
- Introduction To Cns PharmacologyDocument66 pagesIntroduction To Cns PharmacologyYazan Emad Salem100% (1)
- Nm-Lec15 - (Anxiolytics, Sedatives & Hypnotics)Document39 pagesNm-Lec15 - (Anxiolytics, Sedatives & Hypnotics)geng gengPas encore d'évaluation
- SedativeDocument35 pagesSedativeking_goldPas encore d'évaluation
- Sedative and HypnoticsDocument26 pagesSedative and HypnoticsZarish IftikharPas encore d'évaluation
- Cns Pharmacology: AJAYI AM Dept of Pharm & Tox, KIU-WC 1Document88 pagesCns Pharmacology: AJAYI AM Dept of Pharm & Tox, KIU-WC 1jaggwe rogers100% (1)
- Sedative-Hypnotics (SeH) and AnxiolyticsDocument101 pagesSedative-Hypnotics (SeH) and Anxiolyticsmatchees-gone roguePas encore d'évaluation
- Hypnotics and SedativesDocument22 pagesHypnotics and Sedativeskavya nainitaPas encore d'évaluation
- 13 Psychiatric DRUGSDocument42 pages13 Psychiatric DRUGSPande Indra PremanaPas encore d'évaluation
- AnxiolyticsDocument8 pagesAnxiolyticsHengky_FandriPas encore d'évaluation
- ReghDocument9 pagesReghreghpineda28Pas encore d'évaluation
- Sedatives and Hypnotics LectureDocument55 pagesSedatives and Hypnotics LectureOSAKA THOMASPas encore d'évaluation
- Pharma AnxietyDocument19 pagesPharma AnxietySomaia mohammedPas encore d'évaluation
- Chapter+14 +sedative HynoticsDocument32 pagesChapter+14 +sedative Hynoticsudaysingh98100% (2)
- Sedative-Hypnotic-Anxiolytics: Benzodiazepines & OthersDocument37 pagesSedative-Hypnotic-Anxiolytics: Benzodiazepines & OthersManWol JangPas encore d'évaluation
- Pharmacology Neurotropic Drugs 2015Document44 pagesPharmacology Neurotropic Drugs 2015Migz BrosasPas encore d'évaluation
- Central Nervous System Agents: Carmencita R. Pacis PHD, ManDocument52 pagesCentral Nervous System Agents: Carmencita R. Pacis PHD, ManTWINNY JOSSANNE CHEERISHANE MINIONPas encore d'évaluation
- 07.muscle RelaxanteDocument28 pages07.muscle RelaxanteLee BoborasPas encore d'évaluation
- Anxiolytics and HypnoticsDocument43 pagesAnxiolytics and HypnoticshamzabhayatPas encore d'évaluation
- CNS StimulantsDocument89 pagesCNS StimulantsMwanja Moses100% (1)
- Anxiolytic Sedative-Hypnotic DrugsDocument31 pagesAnxiolytic Sedative-Hypnotic DrugsRoman MamunPas encore d'évaluation
- Sedation and Analgesia in ICU FinalDocument68 pagesSedation and Analgesia in ICU FinalKrittin NaravejsakulPas encore d'évaluation
- Anxiolytic and Hypnotic DrugsDocument22 pagesAnxiolytic and Hypnotic DrugsAbdullah BhattiPas encore d'évaluation
- EMOS Farmacología I Sesion 17Document22 pagesEMOS Farmacología I Sesion 17rafaelPas encore d'évaluation
- Sedative HypnoticsDocument22 pagesSedative Hypnoticsmadeha goharPas encore d'évaluation
- Sedative-Hypnotic Drugs: Anita Q. Sangalang, MD, FPOGSDocument43 pagesSedative-Hypnotic Drugs: Anita Q. Sangalang, MD, FPOGSdave_1128Pas encore d'évaluation
- PM3102 Q2Document3 pagesPM3102 Q2rexlloydPas encore d'évaluation
- Drugs Affecting CNS & PNSDocument131 pagesDrugs Affecting CNS & PNSMj Briones100% (1)
- Central Nervous System StimulantsDocument20 pagesCentral Nervous System StimulantsAn LoPas encore d'évaluation
- Conscious Sedation: Hayel Gharaibeh, MD. Anesthesia ConsultantDocument84 pagesConscious Sedation: Hayel Gharaibeh, MD. Anesthesia ConsultantKhaled GharaibehPas encore d'évaluation
- F22 Sedative Hypnotic DrugsDocument37 pagesF22 Sedative Hypnotic DrugsJoyce SumagaysayPas encore d'évaluation
- Cns Depressants Sedative-Hypnotic Drugs: Dr. Hiwa K. Saaed, BSC, HD, Msc. PHDDocument42 pagesCns Depressants Sedative-Hypnotic Drugs: Dr. Hiwa K. Saaed, BSC, HD, Msc. PHDmiznahPas encore d'évaluation
- Drugs Acting On The CNS - 2Document41 pagesDrugs Acting On The CNS - 2Daniel OkakaPas encore d'évaluation
- Pharmacology - Central Nervous SystemDocument10 pagesPharmacology - Central Nervous System22bgu0805msPas encore d'évaluation
- Benzodiazepines: ProfileDocument4 pagesBenzodiazepines: Profilealghashm001Pas encore d'évaluation
- 12-Lead ECG Monitoring With EASI PDFDocument14 pages12-Lead ECG Monitoring With EASI PDFalghashm001Pas encore d'évaluation
- STAR Algorithm PDFDocument10 pagesSTAR Algorithm PDFalghashm001Pas encore d'évaluation
- STAR Arrhythmia Performance PDFDocument6 pagesSTAR Arrhythmia Performance PDFalghashm001Pas encore d'évaluation
- STAR Algorithm PDFDocument10 pagesSTAR Algorithm PDFalghashm001Pas encore d'évaluation
- 12-Lead ECG Monitoring With EASI PDFDocument14 pages12-Lead ECG Monitoring With EASI PDFalghashm001Pas encore d'évaluation
- Adelax: Only For The Use of Medical ProfessionalsDocument2 pagesAdelax: Only For The Use of Medical Professionalsparthibanemails5779Pas encore d'évaluation
- Efficacy and Safety of ClonazepamDocument7 pagesEfficacy and Safety of ClonazepamA. AlejandroPas encore d'évaluation
- NP5 Sample QuestionsDocument7 pagesNP5 Sample QuestionsIvan LouisePas encore d'évaluation
- Anxiety NotesDocument4 pagesAnxiety NotesketantchaudhariPas encore d'évaluation
- Amonoo 2019Document12 pagesAmonoo 2019zozPas encore d'évaluation
- FrenxitDocument2 pagesFrenxitIsrafil TamimPas encore d'évaluation
- Drug Prefixes Roots SuffixesDocument4 pagesDrug Prefixes Roots SuffixesElla LopezPas encore d'évaluation
- Chapter 14 BuspironeDocument10 pagesChapter 14 Buspironeleeperlhan2000Pas encore d'évaluation
- Topical Review ArticleDocument12 pagesTopical Review ArticleadnanjivrakPas encore d'évaluation
- Psychiatric BankDocument169 pagesPsychiatric BankThatcher M Lima100% (31)
- Pharmacology Cheat Sheet - Generic Drug Stems - NurseslabsDocument12 pagesPharmacology Cheat Sheet - Generic Drug Stems - NurseslabsKc Mea Paran BorjaPas encore d'évaluation
- Ch. 14 SlidesDocument64 pagesCh. 14 Slidesamericangurl1284681Pas encore d'évaluation
- Psycho P HarmDocument84 pagesPsycho P HarmEliPas encore d'évaluation
- Somatoform DisordersDocument18 pagesSomatoform Disordersapi-376421589% (9)
- Pharmacotherapy of Anxiety Disorders: Current and Emerging Treatment OptionsDocument21 pagesPharmacotherapy of Anxiety Disorders: Current and Emerging Treatment OptionsGabriel Vargas CuadrosPas encore d'évaluation
- Pharmacology QuestionsDocument33 pagesPharmacology QuestionsPurnimaPas encore d'évaluation
- Introduction To Cns PharmacologyDocument66 pagesIntroduction To Cns PharmacologyYazan Emad Salem100% (1)
- Flubromazolam in Brave New World BookDocument1 pageFlubromazolam in Brave New World BookShaolin105Pas encore d'évaluation
- Anxiety Disorder: College of NursingDocument10 pagesAnxiety Disorder: College of NursingAyr MasenasPas encore d'évaluation
- Guidance For CBRTDocument153 pagesGuidance For CBRTkbl27Pas encore d'évaluation
- Psychiatric Medication BasicsDocument16 pagesPsychiatric Medication BasicsCarmen HollidayPas encore d'évaluation
- SSC - 2020-06-15 - The Vision of Vilazodone and Vortioxetine - Slate Star CodexDocument20 pagesSSC - 2020-06-15 - The Vision of Vilazodone and Vortioxetine - Slate Star CodexKaroline MarxPas encore d'évaluation
- Anxiolytic, Sedative-Hypnotic DrugsDocument39 pagesAnxiolytic, Sedative-Hypnotic DrugsNina100% (1)
- Research Essay Final Draft 1Document10 pagesResearch Essay Final Draft 1api-548724051Pas encore d'évaluation
- Hosseinzadeh Et Al. 2008 - Anxiolytic and Hypnotic Effect of Crocus SativusDocument7 pagesHosseinzadeh Et Al. 2008 - Anxiolytic and Hypnotic Effect of Crocus SativusLaura DecockPas encore d'évaluation
- Pysch Nursing ReviewerDocument72 pagesPysch Nursing ReviewerKristeen Camille ValentinoPas encore d'évaluation
- How To Use Amino Acids Like To End Sugar Cravings and Ease AnxietyDocument8 pagesHow To Use Amino Acids Like To End Sugar Cravings and Ease AnxietySK100% (1)
- Anxiety and Anxiety Disorders PDFDocument7 pagesAnxiety and Anxiety Disorders PDFCsicsi KutyaPas encore d'évaluation
- Chapter 12Document12 pagesChapter 12MarissaCamposPas encore d'évaluation
- 02 Sedative Hypnotic and Anxiolytic DrugsDocument16 pages02 Sedative Hypnotic and Anxiolytic DrugsGilbert OsengoPas encore d'évaluation