Académique Documents
Professionnel Documents
Culture Documents
Chiropex 001
Transféré par
SnehaTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Chiropex 001
Transféré par
SnehaDroits d'auteur :
Formats disponibles
An open clinical study to evaluate the
efficacy and safety of Chiropex in Plantar
Xerosis
JAYASRI DAS PRAMANIK, PADMANABHA RUGVEDI
ABSTRACT:
Dryness of the skin is a common condition in many systemic conditions and due to dryness in the
environment. Dryness of foot or plantar Xerosis in particular can lead to pruritus, hardness, cracks and
fissures in the skin if left untreated. Aim: The study was conducted to evaluate the safety and efficacy
of Chiropex in plantar Xerosis. Materials and methods: This was an open clinical study conducted
in subjects of plantar Xerosis after getting an approval from the ethical committee. Hundred subjects
including both male and female, aged between 18-50 years clinically diagnosed to have plantar Xerosis
after physical and systemic examination not associated with any pre existing systemic illness and who
were willing to give an informed written consent were considered for the study. All the subjects were
advised to wash the feet and then apply a small quantity of Chiropex cream on the affected area
twice daily for the period of 2 weeks. All subjects were followed at weekly intervals for a period of 2
weeks. Assessment parameters included cracks in heels, dryness of soles, pain in the heel, soothing and
moisturizing effect Results: All the hundred subjects completed the study period. Results have shown
beneficial effect of Chiropex for all the parameters with a significance of p<0.001 as compared to
values at entry and week 1 values and there were no adverse effects either observed or reported during
the clinical study and overall compliance to treatment was found to be good. Conclusion: Therefore, it
may be concluded that, Chiropex is effective and safe and is faster in the management of individuals
suffering from Plantar Xerosis.
Key words: Plantar Xerosis, Chiropex,
Introduction:
The loss of moisture from the
stratum corneum and intercellular
matrix leads to dry skin, or
xerosis.1 Dry skin or xerosis is a
common condition that frequently
requires therapeutic intervention.
Xerosis is characterized by
aggregated
desquamating
corneocytes with the appearance
of fine white scales; clinically, it
is often accompanied by decreased
mechanical flexibility of the
stratum corneum, fine fissures,
inflammation, and sensations of
itching and burning. The condition
is believed to stem from impaired
water-binding capability in the
Dr. Jayasri Das Pramanik DVD.MD,
Assistant Professor, Department of Dermatology,
School of Tropical Medicine, Kolkota-700073.
Dr Padmanabha Rugvedi MD(Ayu)
Research Associate
Clinical Pharmacology & Publication, R&D Centre
The Himalaya Drug Company Makali, Bengaluru
Specially Contributed to "The Antiseptic"
Vol. 109 No. 12 & P : 607 - 611
December 2012
stratum corneum. It is aggravated
by exposure to low temperatures
and low indoor humidity in
winter months commonly found
in northern climates. Furthermore,
other adverse environmental
conditions such as exposure to
detergents and solvents, subclinical
dyskeratotic disorders and age
support the clinical manifestation
of xerosis2.
Clinically dry skin appears
rough, uneven, and cracked. Raised
or uplifted skin edges (scaling),
desquamation (flaking), chapping,
and pruritus may be present. A
person who has a decrease or loss
of function of the sweat glands
on the plantar surface of the foot
will experience xerosis of the feet
or plantar xerosis.1 This can be a
painful condition that can cause
bleeding. The incidence of xerosis
increases with age, exposure to
dry environmental conditions, like
living in a dry climate, obesity
THE ANTISEPTIC
consistently walking barefoot or
wearing sandals or open-backed
shoes, and physiological changes
that alter circulatory supply to the
lower extremities. Plantar Xerosis
can become more dangerous if
they go untreated and become
deep or infected. This is especially
dangerous for people with diabetes
or compromised immune systems.
Other factors can be poor feet
structures, abnormal gait that
produces calluses on the heel,
Thyroid disease, Psoriasis etc.
Among systemic diseases, primary
biliary cirrhosis is one commonly
associated with xerosis3. Drugs
like EGFR inhibitors can also
produce xerosis as an adverse
event.4
People with diabetes have
a high incidence of xerosis of
the feet, especially on the heels.
While assessing for predictors
of foot lesions in patients with
diabetes, one study found that
607
82.1% of the patients had skin
with dryness, cracks, or fissures.5
Dry skin often leads to cracks
and fissures, which can serve as a
portal of entry for bacteria. These
cracks and fissures are associated
with an increased risk of cellulitis
and foot ulceration 6,7 that, if
left unchecked, can eventually
necessitate amputation. Areas of
dry, thick skin in the plantar aspect
of the foot can raise pressure in
that area. 8 Callus formation is
the result of the body's protective
response to areas of high pressure.
Unfortunately, this protective
mechanism can become a vicious
cycle. An area of dry skin or
high pressure causes the body to
develop callus, increasing pressure
to that area; the body's response
to this increased pressure is to
build even more callus. High foot
pressures have been associated
with high risk of developing
foot ulcers in patients who have
diabetes9; in addition, high plantar
foot pressure has a high specificity
for predicting the development
of foot ulceration.10 Though not
well studied, the sheer force in
the feet also may be a risk factor
for developing a foot ulcer. The
soft, elastic skin may reduce
pathological shear force; thereby,
preventing ulceration.
The importance of examining
patients' feet and offering
instruction in preventive foot
care by physicians and diabetes
educators is often overlooked.
Xerosis can be controlled with
moisturizers. Moist, elastic skin,
resulting from using a moisturizer,
can help prevent further foot
complications.1
Numerous humidifying topical
preparations containing emollients
and humectants have been used
over the years for the treatment
of dry skin, as well as for more
acute dermatological disorders
including ichthyosis, psoriasis,
actinic damage, eczema, and
the like which exhibit dry skin
608
symptoms. Many such preparations
primarily affect the skin's outer
layer, the stratum corneum, and
act as a partial replacement for
the damaged stratum corneum2.
investigator retained the original
copy of the signed informed
consent and the subject received
a copy of the signed informed
consent.
Chiropex is a polyherbal
formulation containing potent
herbs possessing moisturizing,
anti-microbial, analgesic, and
wound healing activities. Chiropex
was evaluated for its efficacy
and safety in individuals suffering
from Plantar Xerosis.
Inclusion Criteria:
Aim:
This study was planned to
evaluate the clinical efficacy and
safety (short-term) of Chiropex in
Plantar Xerosis.
Materials and Method:
Hundred subjects who are
willing to participate in the study
were given detailed description
about the investigational product,
nature and duration of the study.
Also subjects responsibilities after
entering the study were explained.
Subjects were pre screened by
the investigators for the criteria
indicated in the subject selection
section. Only subjects who met the
requirements of this section, have
signed an informed consent form
and subjects who were willing to
follow instructions given by the
investigator and have an updated
medical history on file with the
investigator were entered in the
study.
Informed consent process:
A written informed consent by the
subject was obtained from each
study subject. The investigator
provided information about the
study verbally as well as using
a patient information sheet, in a
language that is non technical and
is understandable by the study
subject. The investigator gave
adequate time for the subject to
read it before the informed consent
is signed. The subjects consent
was obtained in writing using an
informed consent form. The
THE ANTISEPTIC
Hundred subjects of both
sexes, from the age group of
18-50 years, who were clinically
diagnosed with Plantar Xerosis
with symptoms like the hard, dry
and flaky cracking of the skin of
the heels, and who were willing
to give informed consent were
enrolled in the study
Exclusion criteria:
Subjects with conditions of
dermatitis due to medication &
skin infection were excluded
from the study. Also subjects
with pre-existing systemic
disease necessitating longterm medications, endocrinal
disorders, subjects with known
history or present condition of
allergic response to any cosmetic/
pharmaceutical products, toiletries
or its components or ingredients
in the test products and those who
refused to give informed consent,
were excluded from the study.
Pregnant and lactating women
were also excluded from the study.
Study procedure:
All enrolled subjects underwent
a thorough physical and local skin
examination; hundred subjects
received Chiropex cream. All
subjects were advised to wash
the feet and then apply a small
quantity of Chiropex cream on the
affected area in a circular motion
over the dry and cracked heels
twice daily for the period of 2
weeks. All subjects were followed
at weekly intervals for a period
of 2 weeks.
Follow-up and assessment
Subjects were assessed at entry,
week 1 and week 2. Assessment
parameters included cracks in
heels, dryness of soles, pain in the
heel, soothing and moisturizing
effect. Assessment of parameters
December 2012
was done on the basis of following
grading scale: -Cracks in heels: 0:
No cracks, 1:Dry soles with one or
two cracks., 2: 5-7 cracks, 3: Many
superficial cracks with slight
pain, 4: Slight deep cracks with
moderate pain, 5: Deep cracks
with severe pain and bleeding
which causes difficulty in walking.
Dryness of sole- 0: No dryness,
1: Slight dryness, 2: Dryness only
at the cracks, 3: Dryness over
the entire sole. Pain in the heel
was expressed in a scale of 0-3
where 0-nil to 3- severe. Soothing
effect and moisturizing effect was
expressed in a scale of 0-4, where
0-Poor, 1- fair, 2 moderate,3Good, 4-excellent. The scoring was
in turn correlated with response to
the treatment as follows: 0: no
improvement, 1: Poor response, 2:
Fair response, 3: Good response,
4: Excellent response. Soothing
and moisturizing effect- 1: No
change, 2: Fair, 3: Good, 4: Very
good, 5-Excellent.
At each follow-up visit,
the investigator recorded any
information about intercurrent
illness, therapeutic interventions
and concomitant medication/s.
All the adverse events reported
or observed by patients were
recorded with information about
severity, date of onset, duration,
and action taken regarding the
study drug.
Adverse event assessment
At each follow-up visit, the
investigator recorded information
about intercurrent illness or
infections and concomitant
medication. All the adverse
events reported or observed
by patients were recorded with
information about severity, date of
onset, duration, and action taken
regarding the study drug.
Relation of adverse events to
study medication was predefined as
Unrelated (a reaction that does
December 2012
not follow a reasonable temporal
sequence from the administration
of the drug), Possible (follows
a known response pattern to the
suspected drug, but could have
been produced by the subjects
clinical state or other modes
of therapy administered to the
subject), and Probable (follows
a known response pattern to the
suspected drug that could not
be reasonably explained by the
known characteristics of the
subjects clinical state).
Primary
points:
and
secondary
end
The predefined primary
efficacy endpoints were clinical
improvement and symptomatic
control in Plantar Xerosis. The
predefined secondary endpoints
for short-term safety were assessed
by incidence of adverse events
during the study period, and
overall compliance to the drug
treatment.
Statistical Analysis
All values are expressed as
compared to At entry as Mean
SD. Results were analyzed
statistically by Repeated Measures
of ANOVA using Friedman test
followed by Dunnetts multiple
comparison test to find out the
level of significance. Analysis was
performed using Graphpad prism
software Version 4.03, San Diego,
California, USA.
RESULTS:
A total 100 subjects were
enrolled in the study. The
demographic details of the subjects
at entry are listed in Table 1.
100 subjects showed reduction
in the cracks and other symptoms,
which is summarized in Table 2.
The improvement trend was seen
from week 1 till the end of the
study. There were no clinically
significant adverse reactions,
either reported or observed, during
the entire study period and overall
compliance to the treatment was
good.
THE ANTISEPTIC
The evaluation of various
parameters on the effect of
Chiropex has been shown in
table 2. Reduction of cracks in
heels at entry was 2.930.33 which
after treatment with Chiropex
reduced to 1.930.26 at week 1
and further reduced to 0.810.47
at week 2. Similarly reduction in
dryness of soles was noted from
2.920.34 at entry to 1.860.38
at week 1 and further reduced
to 0.650.58 at week 2 with the
treatment of Chiropex. Pain in
heels reduced from 2.050.22 at
entry to 1.580.46 at 1st week
and 0.720.34 at 2nd week. Cracks
in the heels, dryness of soles
and Pain in the heels showed a
significant improvement at the
end of 2 weeks as compared to
values at entry (p<0.001) as well
as compared to week 1 values
(p<0.001). Similarly soothing
and moisturising effect was also
showed significance of p<0.001 at
2 weeks as compared to values at
entry and at week 1 values.
Soothing effect improved from
2.030.56 at entry to 2.610.67
at week 1 and 3.270.33 at week
2. Similarly moisturising effect
also showed improvement from
2.060.49 at entry to 2.720.67
at week 1 and further it increased
to 3.470.26 at week 2.
Statistical analysis conducted
has shown that all the parameters
had shown beneficial effect on
Chiropex with a significance of
p<0.001 as compared to values
at entry and week 1 values.
There were no adverse effects
either observed or reported during
the clinical study and overall
compliance to treatment was found
to be good.
DISCUSSION:
Chirpopex cream is a polyherbal
cream that contains natural
moisturising factors, essential
fatty acids and vitamin E. After its
application, easily gets absorbed
in all types of skin including
609
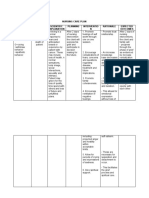
Table 1: Demographic details at entry (n=100)
Age MeanSD (in years)
Diet Veg: Non-Veg
Males: Females
Smokers: non smokers
36.729.59
94:6
2:98
1: 99
Table 2: Evaluation of various parameters on the effect of Chiropex
Sl. Parameter
Score(MeanSD)
No.
At entry
Week 1
Week 2
1 Cracks in heels
2.930.33
1.930.26
0.810.47
2 dryness of soles
2.920.34
1.860.38
0.650.58
3 Pain in heels
2.050.22
1.580.46
0.720.34
4 Soothing effect
2.030.56
2.610.67
3.270.33
5 Moisturising effect 2.060.49
2.720.67
3.470.26
Note: a Significance at week 2 as compared to values at entry and
b
is Significance at week 2 as compared to week 1 values
dry, and thick skin. It gets faster
absorbed and gives relief faster. It
absorbs and retains moisture and
relieves dryness and itching. Its
regular applications smoothen and
soften the skin. It is non-greasy
and non-staining as well.
Chiropex cream contains
Madhu (Honey), Oils of Atasi
(Linum usitatissimum), Karanja
(Pongamia pinnata), Ushira
(Vetiveria zizonioides), Barbari
(Ocimum basilicum), Jambira
(Citrus limon) and Peppermint
satva (Trachyspermum ammi).
Clinical observations suggest
that honey holds significant
promise as an effective treatment
for a number of medical
conditions and particularly in
the management of non-healing
wounds11-12. Chrysin is a natural,
biologically active compound
extracted from honey possesses
potent anti-inflammatory, and
anti-oxidation properties13. Honey
610
acts mainly as hyperosmolar
medium and prevents bacterial
growth. Due to this, it helps to
rapid absorption of edema fluid
from the soggy wounds. Due to
high viscosity of honey, it forms
a physical barrier that prevents
bacterial colonization in wounds
and creating a moist environment,
which helps to accelerate the
wound healing process. The
nutrient contents of honey such
as laevulose, and fructose improve
local substrate supply and help
epithelialization14.
Oil of Linum usitatissimum
contains 57.83%, -linolenic
acid, and Omega-3-fatty acid in
major. The fixed oil of Linum
usitatissimum inhibits PGF2leukotrine, histamine, and
bradykinin induced inflammation.
The oil has also been reported
to reduce arachidonic induced
inflammation,
suggesting
its capacity to inhibit both
cyclooxygenase and lipoxygenase
THE ANTISEPTIC
Statistical
Significance
a
p<0.001
b
p<0.001
a
p<0.001
b
p<0.001
a
p<0.001
b
p<0.001
a
p<0.001
b
p<0.001
a
p<0.001
b
p<0.001
pathways
of
arachidonate
metabolism. These activities are
suggested due to the presence of
-linolenic acid and omega-3fatty acid15. The seed oil has skin
conditioning activity that is used to
create special effects on skin and
enhances the appearance of dry
or damaged skin and sustantative
materials which adhere to the
skin to reduce flaking and restore
suppleness16.
Oils from Pongamia pinnata
are rich source of fatty oil
and have been reported with
antimicrobial activity against
common pathogens. In Ayurvedic
practice, the seed-oil of Pongamia
pinnata is used in itches, abscess
and other skin diseases. Various
extracts of the seed are used
in other skin conditions like
leucoderma, and leprosy17. The
seed oil has skin conditioning
activity that reduces the flaking
and dryness of skin and restores
the skin texture.
December 2012
Oil from Vetiver contains
sesquiterpenes including their
derivatives like vetivone ,
khusimol in major and has
reported with antimicrobial and
refrigerant activities19-20.
Oil of Ocimum basilicum is
rich in chavicol methyl ether or
estragole, linalool and eugenol.
The studies in literatures suggest
Linalool has been reported with
antibacterial activity21. Salmah et
al in their trial have reported about
the wound healing potential of
Ocimum basilicum extract after
topical application 14. Ocimum
basilicum oil has skin conditioning
activity that reduces the symptoms
associated with dry skin to regain
its suppleness.
Limonene present in Citrus
limon oil has reported with
antibacterial and anti-fungal
activities23. Lemon Oil has skin
conditioning activity that keeps
skin healthy and promotes the
protective functions of the skin.
The seed extract of Trachyspermum
ammi has been reported with
wound healing promoter activity
on repeated use25. Traditionally,
the seed extract is also used in
hemorrhagic septicemia26.
Chiropex cream has the
above described potent herbs
with
moisturizing,
antimicrobial, analgesic, and wound
healer promotive activities.
Its moisturizing activity helps
to smoothen and soften the
skin. Its anti-microbial activity
helps to prevent from common
contaminations. Its analgesic
activity helps to reduce pain. Its
wound-healing promoter activity
helps to heal the Plantar Xerosis
faster.
CONCLUSION:
This clinical study clearly
shows that significant symptomatic
relief was observed with Chiropex
cream in individual suffering
December 2012
from Plantar Xerosis. Statistical
significant beneficial effect was
observed with Chiropex treatment
in the parameters like cracked
heels, dryness of soles, pain
in the heels, Soothing effect
and Moisturising effect. There
were no adverse effects either
observed or reported during the
clinical study. All the subjects
completed the study and overall
compliance to treatment was found
to be good. Therefore, it may
be concluded that, Chiropex is
effective and safe and is faster
in the management of individuals
suffering from Plantar Xerosis.
REFERENCES:
1. Pham HT et al, A prospective, randomized,
controlled double-blind study of a
moisturizer for xerosis of the feet in
patients with diabetes. Ostomy Wound
Manage. 2002 May;48(5):30-6
2. Moshe Arkin, Kfar Shmaryahu
(IL)
Topical compositions of urea and
ammonium lactate; US 2005/0037040
A1 (patent application)
3. Meri Koulentaki MD, Dermatological
Manifestations in Primary Biliary Cirrhosis
Patients: A Case Control Study The
American Journal of Gastroenterology
(2006) 101, 541546; doi:10.1111/j.15720241.2006.00423.x
4. Samer H. Ghosn, Abdul-Ghani Kibbi,
Cutaneous manifestations of liver diseases
5. Litzelman DK, Marriott DJ, Vinicor F.
Independent physiological predictors of
foot lesions in subjects with NIDDM.
Diabetes Care. 1997;20(8):1273-1278.
6. Koutkia P, Mylonakis E, Boyce J. Cellulitis:
evaluation of possible predisposing factors
in hospitalized subjects. Diagn Microbiol
Infect Dis. 1999;34(4):325-327.
7. Mackool BT, Lowitt MH, Dover JS. Skin
manifestations of diabetes mellitus. In:
Kahn CR, Weir GC, eds. Joslin's Diabetes
Mellitus, 13th ed. Philadelphia, Pa.; Lea
and Febiger: 1994;900-911.
8. Young MJ, Cavanagh PR, Thomas G,
Johnson MM, Murray H, Boulton AJ. The
effect of callus removal on dynamic plantar
foot pressures in diabetic patients. Diabet
Med. 1992;9(1):55-57.
9. Frykberg RG, Lavery LA, Pham H,
Harvey C, Harkless L, Veves A. Role of
neuropathy and high foot pressures in
diabetic foot ulceration. Diabetes Care.
1998;21(10):1714-1719.
10.
P ham H, Armstrong DG, Harvey C,
Harkless LB, Giurini JM, Veves A.
Screening techniques to identify people
a high risk for diabetic foot ulceration:
a prospective multicenter trial. Diabetes
Care. 2000;23(5):606-611
11.
Dunford C. The use of honey-derived
dressings to promote effective wound
management.
Prof
Nurse.
2005
Apr;20(8):35-8.
THE ANTISEPTIC
12.
Kingsley A. The use of honey in the
treatment of infected wounds: case
studies. Br J Nurs. 2001 Dec;10(22
Suppl):S13-6, S18, S20.
13. Woo KJ, Jeong YJ, Inoue H, Park JW, Kwon
TK. Chrysin suppresses lipopolysaccharide
-induced cyclooxygenase-2 expression
through the inhibition of nuclear factor for
IL-6 (NF-IL6) DNA-binding activity. FEBS
Lett. 2005 Jan 31;579(3):705-11.
14. Salmah et al. Synergistic effect of alcoholic
extract of sweet basil (Ocimum basilicum
L) leaves and honey on cutaneous wound
healing in rats. Int Journal of molecular
medicine and advance sciences. 1(3).
2005. 220-224.
15. Gaurav Kaithwas et al. Anti-inflammatory,
analgesic, and antipyretic activities of
Linum usitatissimum L. (flaxseed/linseed)
fixed oil. Ind J Exp Biology. 49. 2011.
932-938.
16.
Tara E Gottschalck et al. International
Cosmetic Ingredient Dictionary and
Handbook. The cosmetic toiletry and
Fragrance association. Washington. 12th
Edition. 2008. 1465.
17.
S.R. Arote et al. Pongamia pinnata L:
A Comprehensive Review. International
Journal of PharmTech Research. Vol.2,
No.4, pp 2283-2290, Oct-Dec 2010
18.
Tara E Gottschalck et al. International
Cosmetic Ingredient Dictionary and
Handbook. The cosmetic toiletry and
Fragrance association. Washington. 12th
Edition. 2008. 2149
19.
S avarimuthu Ignacimuthu. In vitro
antibacterial activity of some plant
essential oils. BMC Complementary and
Alternative Medicine 2006, 6:39. 1-8.
20. K.J. Thara Saraswathi et al. Comparitive
Study on Essential Oil in Natural and
In vitro Regenerated Plants of Vetiveria
zizanioides (Linn.) Nash. AmericanEurasian J. Agric. & Environ. Sci., 10
(3): 458-463, 2011
21. Amir Mohammad Daneshian Moghaddam
et al. Antimicrobial activity of essential oil
extract of Ocimum basilicum L. leaves on
a variety of pathogenic bacteria. Journal
of Medicinal Plants Research Vol. 5(15),
pp. 3453-3456, 4 August, 2011
22.
Tara E Gottschalck et al. International
Cosmetic Ingredient Dictionary and
Handbook. The cosmetic toiletry and
Fragrance association. Washington. 12th
Edition. 2008. 1680
23.
Y uangang Zu et al. Activities of Ten
Essential Oils towards Propionibacterium
acnes and PC-3, A-549 and MCF-7 Cancer
Cells. Molecules 2010, 15, 3200-3210
24.
Tara E Gottschalck et al. International
Cosmetic Ingredient Dictionary and
Handbook. The cosmetic toiletry and
Fragrance association. Washington. 12th
Edition. 2008. 617
25.
Jaiswal S et al. Plants used for tissue
healing of animals. Natural products
radiance. 3(4). July-August. 2004. 284292.
26. Prasant kumar singh et al. Ethnoveterinary
healthcare practices in marihan subdivision of district mirzapur,uttar pradesh,
india. Life sciences leaflets 16:561 569,
2011
611
Vous aimerez peut-être aussi
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Course SyllabusDocument5 pagesCourse SyllabusjuyjuyalcalaPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- The Process of Strength and Conditioning For GolfersDocument0 pageThe Process of Strength and Conditioning For GolfersadriansmithbizPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Synopsis de Addiction CenterDocument2 pagesSynopsis de Addiction CenterNishana100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- CSP - Groin LumpDocument39 pagesCSP - Groin LumpAnnisa SakilaPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Material Safety Data Sheet: 1 IdentificationDocument6 pagesMaterial Safety Data Sheet: 1 IdentificationGio Ibarra MolinaPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Insulin IndexDocument13 pagesInsulin IndexbookbookpdfPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Caries PPT - ppt11Document109 pagesCaries PPT - ppt11dr parveen bathlaPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- U.S. Department of Health and Human Services National Institutes of HealthDocument8 pagesU.S. Department of Health and Human Services National Institutes of HealthP D SpencerPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- AT & Complicated GriefDocument4 pagesAT & Complicated GriefCarolina BertaPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Axsos 3 Titanium: Monoaxial Locking Plate SystemDocument28 pagesAxsos 3 Titanium: Monoaxial Locking Plate SystemalexPas encore d'évaluation
- Avipattikar ChurnaDocument3 pagesAvipattikar ChurnadrbhaveshpPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Personal Hygiene: Didik S AtmojoDocument25 pagesPersonal Hygiene: Didik S AtmojoRetno BeniPas encore d'évaluation
- Introduction To STYEDocument10 pagesIntroduction To STYESumit KumarPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Science of Addiction (Drugs and The Brain)Document84 pagesThe Science of Addiction (Drugs and The Brain)cacker4140100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- KK Tunnel Route MapDocument1 pageKK Tunnel Route MapHonolulu Star-AdvertiserPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- NCP Case StudyDocument2 pagesNCP Case StudyGerome Isaiah RabangPas encore d'évaluation
- Child Health Program Oral Health: Guidance DocumentDocument30 pagesChild Health Program Oral Health: Guidance Documentanubhutigupta1404Pas encore d'évaluation
- Nikki Sison CVDocument2 pagesNikki Sison CVyeng botzPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Classification Des MédicamentsDocument28 pagesClassification Des MédicamentsGustyl KolinsPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- EGYPT Registered Products Update 22-10-09 1Document103 pagesEGYPT Registered Products Update 22-10-09 1Anuj MairhPas encore d'évaluation
- Jarvis 2012 Practical UroflowmetryDocument2 pagesJarvis 2012 Practical UroflowmetryFoxglove83Pas encore d'évaluation
- Nursing Care Plan For Osteomyelitis: Nursing Diagnosis For Osteomyelitis and Nursing Interventions For OsteomyelitisDocument43 pagesNursing Care Plan For Osteomyelitis: Nursing Diagnosis For Osteomyelitis and Nursing Interventions For Osteomyelitisabe abdiPas encore d'évaluation
- ClubfootDocument9 pagesClubfootLorebell100% (5)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Katalog Pavna ANG Siebec-03-WEBDocument24 pagesKatalog Pavna ANG Siebec-03-WEBzanjan98Pas encore d'évaluation
- Mnemonic DeviceDocument12 pagesMnemonic DeviceJonathan ObañaPas encore d'évaluation
- Auto Urine TherapyDocument130 pagesAuto Urine TherapyBashu Poudel100% (3)
- StrategicDocument79 pagesStrategicpradnya7289Pas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Integrated Therapeutics IiiDocument16 pagesIntegrated Therapeutics IiiSalahadinPas encore d'évaluation
- Types and Complication of C-SectionDocument13 pagesTypes and Complication of C-SectionMeghaUnniPas encore d'évaluation
- Aromatherapy & DepressionDocument3 pagesAromatherapy & DepressionTheMothershipPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)