Académique Documents
Professionnel Documents
Culture Documents
ARTIKEL 2 Hypertension
Transféré par
RitaSuzyantiCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
ARTIKEL 2 Hypertension
Transféré par
RitaSuzyantiDroits d'auteur :
Formats disponibles
Articles
Ecacy and safety of nebivolol and valsartan as xed-dose
combination in hypertension: a randomised, multicentre study
Thomas D Giles, Michael A Weber, Jan Basile, Alan H Gradman, David B Bharucha, Wei Chen, Manoj Pattathil, for the NAC-MD-01 Study Investigators*
Summary
Background The xed-dose combination of any two antihypertensive drugs from dierent drug classes is typically
more eective in reducing blood pressure than a dose increase of component monotherapy. We assessed the ecacy
and safety of a xed-dose combination of a vasodilating blocker (nebivolol) and an angiotensin II receptor blocker
(valsartan) in adults with hypertension.
Methods We did an 8-week, phase 3, multicentre, randomised, double-blind, placebo-controlled, parallel-group trial at
401 US sites. Participants (age 18 years) with hypertension but with blood pressure less than 180/110 mm Hg were
randomly assigned (2:2:2:2:2:2:2:1) by a 24-h interactive web response system in blocks of 15 to 4 weeks of double-blind
treatment with nebivolol and valsartan xed-dose combination (5 and 80 mg/day, 5 and 160 mg/day, or 10 and
160 mg/day), nebivolol (5 mg/day or 20 mg/day), valsartan (80 mg/day or 160 mg/day), or placebo. Doses were doubled
in weeks 58; results are reported according to the nal dose. Participants and research sta were masked to treatment
allocation. The primary and key secondary endpoints were changes from baseline to week 8 in diastolic and systolic
blood pressure, respectively. The primary statistical comparison was between the highest xed-dose combination dose
and the highest monotherapy doses; lower doses were then compared if this comparison was positive (Hochberg
method for multiple testing). Ecacy analyses were by intention to treat. Safety assessments included monitoring of
adverse events. Continuous ecacy parameters were analysed using an ANCOVA model; binary outcomes were
analysed using a logistic regression model. This study is registered with ClinicalTrials.gov, NCT01508026.
Findings Between Jan 6, 2012, and March 15, 2013, 4161 patients were randomly assigned (277 to placebo and 554555
to each active comparator group), 4118 of whom were included in the primary analysis. At week 8, the xed-dose
combination 20 and 320 mg/day group had signicantly greater reductions in diastolic blood pressure from baseline
than both nebivolol 40 mg/day (least-squares mean dierence 12 mm Hg, 95% CI 23 to 01; p=0030) and
valsartan 320 mg/day (44 mm Hg, 54 to 33; p<00001); all other comparisons were also signicant, favouring
the xed-dose combinations (all p<00001). All systolic blood pressure comparisons were also signicant (all p<001).
At least one treatment-emergent adverse event was experienced by 3036% of participants in each group.
Interpretation Nebivolol and valsartan xed-dose combination is an eective and well-tolerated treatment option for
patients with hypertension.
Lancet 2014; 383: 188998
See Editorial page 1861
See Comment page 1864
*Members listed in appendix
Department of Medicine,
Tulane University,
New Orleans, LA, USA
(Prof T D Giles MD); Division of
Cardiovascular Medicine,
State University of New York,
Downstate College of
Medicine, Brooklyn, NY, USA
(Prof M A Weber MD);
Department of Medicine,
Division of Cardiology, Medical
University of South Carolina,
Charleston, SC, USA
(Prof J Basile MD); Department
of Medicine, Temple University
School of Medicine, Pittsburgh,
PA, USA (Prof A H Gradman MD);
and Department of Clinical
Development
(D B Bharucha MD,
M Pattathil MSc) and
Department of Biostatistics
(W Chen PhD), Forest Research
Institute, Jersey City, NJ, USA
Correspondence to:
Prof Thomas D Giles,
109 Holly Drive, Metairie,
LA 70005, USA
tgiles4@cox.net
See Online for appendix
Funding Forest Research Institute.
Introduction
The combination of two antihypertensive drugs from
dierent classes is likely to cause a greater reduction in
blood pressure than would an increase in the monotherapy
dose.1 For patients who need more than one drug to
achieve blood pressure control, treatment should
commence with two drugs, either as separate entities or
as a xed-dose combination.2,3
The use of antihypertensive xed-dose combinations
compared with higher doses of the monotherapy
components has been associated with improved blood
pressure control,14 lower rates of adverse events, and
improved drug adherence.36 Moreover, xed-dose
combinations make the assessment of pharmacological
compatibility of the combined drugs easier for
prescribers, resulting in more predictable treatment
results compared with free combinations.
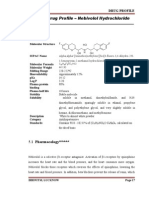
Nebivolol and valsartan are two antihypertensive drugs
with proven safety and tolerability.7,8 The mechanism of
www.thelancet.com Vol 383 May 31, 2014
action of nebivolola highly selective 1 adrenergic
receptor antagonistincludes a nitric-oxide-dependent
vasodilatory eect via 3receptor agonism and reduction
of oxidative stress, dierentiating it from traditional, nonvasodilatory 1 blockers (eg, atenolol).9,10 Valsartan is an
angiotensin II receptor blocker that also reduces oxidative
stress.11,12 We assessed the ecacy and safety of a new
xed-dose combination consisting of nebivolol and
valsartan compared with the monotherapy components
and placebo in patients with stage 1 or stage 2
hypertension.
Methods
Study design and participants
We did a phase 3, multicentre, randomised, double-blind,
placebo-controlled, parallel-group trial at 401 US sites. The
central laboratories were ACM Global Central Laboratory
(Rochester, NY, USA; clinical laboratory determinations),
Quest Diagnostics (San Juan Capistrano, CA, USA;
1889
Articles
genotyping), BioClinica (Princeton, NY, USA; ambulatory
blood pressure monitoring [ABPM] processing), and
Keystone Bioanalytical (North Wales, PA, USA;
processing of pharmacokinetic parameters). Men and
women aged 18 years or older were eligible to participate
if they had stage 1 or 2 hypertension (Seventh Report of
the Joint National Committee on Prevention, Detection,
Evaluation, and Treatment of High Blood Pressure
[JNC7] criteria2) with a recent diastolic blood pressure
measurement of at least 90 mm Hg and less than
110 mm Hg if receiving hypertension treatment or at
least 95 mm Hg and less than 110 mm Hg at screening if
untreated, a pulse rate of at least 55 beats per min (except
for those already taking a blocker), and a normal
physical examination at screening. Reasons for exclusion
included secondary hypertension; systolic blood pressure
at least 180 mm Hg or diastolic blood pressure at least
110 mm Hg; treatment with more than four
antihypertensive drugs (including components of xeddose combinations); contraindication to discontinuation
of present antihypertensive treatment; upper arm
circumference greater than 42 cm; presence of coronary
artery disease, reactive airway disease, chronic obstructive
pulmonary disease, second-degree or third-degree heart
block or sick sinus syndrome, heart failure, hypertensive
retinopathy (Keith-Wagener-Barker grade III or IV),
type 1 diabetes, poorly controlled type 2 diabetes (glycated
haemoglobin 8%), uncontrolled thyroid disease within
3 months of screening, inammatory bowel disease or
active gastritis, pancreatitis, or renal impairment
(estimated glomerular ltration rate <60 mL/min); and
pregnancy or breastfeeding. Other exclusion cirteria are
listed in the appendix.
This study was done in compliance with the
International Conference on Harmonisation of
Technical
Requirements
for
Registration
of
Pharmaceuticals for Human Use guidelines and the US
Food and Drug Administration (FDA) guidelines for
good clinical practice, and in accordance with the ethical
principles originating from the Declaration of Helsinki
and the US FDA Code of Federal Regulations Title 21,
section 312.120. All enrolled participants provided
voluntary, written informed consent and Health
Insurance Portability and Accountability Act
authorisation before participation in the study. The
institutional review boards of all participating centres
approved the study protocol, informed consent form,
and information sheet advertisements.
Randomisation and masking
After a 1-week screening period, participants entered a
6-week single-blind placebo run-in phase, which was
followed by an 8-week double-blind treatment period and
a 1-week double-blind down-titration phase. Participants
were randomly assigned if adherence to treatment in the
last two visits of the single-blind run-in phase averaged
80120% and diastolic blood pressure measurements
1890
were at least 95 mm Hg and less than 110 mm Hg at both
randomisation and the visit before randomisation, with
no more than a 10 mm Hg dierence between the two.
Adherence was assessed using pill counts.
Participants were randomly assigned (2:2:2:2:2:2:2:1) to
4 weeks of double-blind treatment with a nebivolol and
valsartan xed-dose combination (5 and 80 mg/day, 5 and
160 mg/day, or 10 and 160 mg/day), nebivolol
monotherapy (5 mg/day or 20 mg/day), valsartan
monotherapy (80 mg/day or 160 mg/day), or placebo.
Doses were doubled at the beginning of week 5 to xeddose combinations 10 and 160 mg/day, 10 and 320 mg/day,
and 20 and 320 mg/day; nebivolol 10 mg/day and
40 mg/day; and valsartan 160 mg/day and 320 mg/day.
Findings are reported according to the nal dose, unless
stated otherwise. The comparisons with 40 mg/day
nebivolol were done to satisfy the requirement by the US
FDA, as outlined in the applicable regulations13,14 and US
FDA discussions with the study sponsor, that the highest
approved doses of the component monotherapy drugs are
included. Randomisation codes were generated by the
Statistical Programming Department at the Forest
Research Institute (Jersey City, NJ, USA) and
implemented (including the maintenance of masking) by
a 24-h interactive web response system. Randomisation
was stratied by participation in a biomarker (plasma
renin activity and aldosterone concentration) and ABPM
substudy and by type 2 diabetes mellitus status, and was
done in blocks of 15. Tablets were identical in appearance,
taste, and smell, and participants and research sta were
masked to study drug treatment for the duration of
the trial.
Procedures
Blood pressure and pulse rate were measured using an
automatic monitoring device (Omron HEM-705CP,
Lake Forest, IL, USA). After a 5-min rest period, four
separate sitting blood pressure measurements were
taken at drug trough (the period at the end of the dosing
interval) with a 25 min interval between measurements.
The mean of the last three values constituted the blood
pressure value for the visit. Seated pulse rate was the
mean obtained at the same time the last three seated
blood pressure measurements were taken. A 24-h
ABPM was recorded from substudy participants at
week 0 and week 8 using a Spacelabs 90207 (Snoqualmie,
WA, USA) oscillometric device that was automatically
set to measure and record blood pressure. Blood
samples for assessment of biomarker levels were also
collected from substudy participants.
Outcomes
The primary ecacy endpoint was the change in trough
seated diastolic blood pressure from baseline to week 8
and the key secondary ecacy endpoint was change in
seated systolic blood pressure from baseline to week 8.
Other secondary ecacy parameters were changes from
www.thelancet.com Vol 383 May 31, 2014
Articles
baseline in mean trough seated diastolic and systolic
blood pressure at week 4 and changes in 24-h ABPM
values for diastolic and systolic blood pressure from
baseline to week 8 for participants assigned to the xeddose combination of 20 and 320 mg/day versus
40 mg/day nebivolol and 320 mg/day valsartan; diastolic
blood pressure responder rates at week 8 at levels less
than 90 mm Hg and less than 80 mm Hg, and systolic
blood pressure responder rates at week 8 at levels less
than 140 mm Hg and less than 130 mm Hg (20 and
320 mg/day xed-dose combination versus nebivolol
40 mg/day and valsartan 320 mg/day).
Additional prespecied ecacy parameters included
changes from baseline in mean trough seated diastolic
and systolic blood pressure at each visit, changes in
pulse rate at week 8, and proportions of participants
achieving treatment goal (blood pressure <140/90 mm Hg
without type 2 diabetes or <130/80 mm Hg with type 2
diabetes, consistent with JNC7 criteria2) at weeks 4 or 8.
A post-hoc ecacy assessment of pulse pressure from
baseline to week 8 was also done. Daytime and nighttime ABPM assessments and biomarker data will be
reported separately.
Subgroup analyses for the primary and key secondary
ecacy parameters were done according to participants
sex, body-mass index (<30 kg/m or 30 kg/m), ethnic
origin (Hispanic or not), race (black or non-black),
baseline diastolic blood pressure category (<median or
median), diabetes status (yes or no), and age (<65 years
or 65 years).
Safety and tolerability were assessed by recording
adverse events and monitoring vital signs at each visit; by
doing physical examinations and electrocardiograph
measurements at screening, baseline, and week 8; and
by measuring clinical laboratory parameters from blood
and urine taken at screening, baseline, and weeks 4
and 8.
Statistical analysis
Assuming a diastolic blood pressure mean treatment
dierence of 2 mm Hg (SD 8) between the xed-dose
combination 20 and 320 mg/day and the nebivolol
40 mg/day groups, and between the xed-dose
combination 20 and 320 mg/day and the valsartan
320 mg/day groups and on the basis of pairwise t test
comparisons, 500 participants would need to be
randomly assigned to each active-treatment group and
250 to placebo (total 3750 participants) to provide 95%
power to detect a 2 mm Hg (SD 8) treatment dierence
or greater at the two-tailed 5% signicance level. If the
study was positive, the study size would provide a further
90% power to detect a mean dierence of 2 mm Hg
(SD 8) between xed-dose combinations 10 and
160 mg/day and 10 and 320 mg/day and the
corresponding monotherapy groups, with multiplicity
adjustment using the Hochberg procedure,15 at the twotailed 5% signicance level.
www.thelancet.com Vol 383 May 31, 2014
Ecacy parameters were analysed based on the
intention-to-treat population, dened as all randomised
participants who took at least one dose of double-blind
drug and had at least one diastolic blood pressure
measurement after baseline, using the last-observationcarried-forward approach to impute missing data. The
primary ecacy parameter was analysed using an
ANCOVA model, with treatment group and diabetes
status as factors and baseline diastolic blood pressure
value as a covariate. The xed-dose combination 20 and
320 mg/day group was compared with the nebivolol
40 mg/day and valsartan 320 mg/day groups; if both
comparisons were statistically signicant (p<005), the
study was deemed to be positive and the xed-dose
combination 10 and 160 mg/day and 10 and 320 mg/day
groups were compared with their corresponding
monotherapy groups, with multiplicity controlled using
the Hochberg procedure15 on the adjusted p values (ie, the
maximum of pvalues for the comparisons of the xeddose combination group versus its corresponding
monotherapy groups).
For the key secondary ecacy parameter, each xeddose combination was compared with the respective
component monotherapy dose only if the primary
ecacy parameter comparison was signicant for the
xed-dose combination; comparisons were based on an
ANCOVA model similar to that used in the primary
analysis, with the baseline systolic blood pressure value
as a covariate. All other continuous parameters were
analysed using an ANCOVA model with treatment
group, diabetes status, subgroup factor, and treatmentgroup-by-subgroup factor interaction as factors and
baseline value as a covariate. The analyses of binary
outcomes were done using a logistic regression model
with treatment group as class variable and baseline blood
pressure (diastolic or systolic blood pressure, as
applicable) as a covariate.
Analyses of safety measures were based on the safety
population, dened as all randomly assigned participants
who took at least one dose of double-blind study drug,
and ndings are presented as descriptive statistics.
This study is registered with ClinicalTrials.gov,
NCT01508026.
Role of the funding source
The trial was designed jointly by the principal
investigator (TDG) and the study sponsor. The sponsor
was responsible for study monitoring, data management, inventory and distribution of clinical supplies,
and data collection and analysis. Three of the authors
are employees of the sponsor (DBB, MP, and WC) and
provided input into the data interpretation and writing
of the report; beyond that, the sponsor was not directly
involved in these aspects of the study. All authors
had full access to all the data in the study and
had nal responsibility for the decision to submit
for publication.
1891
Articles
13 250 patients assessed for eligibility
9089 ineligible
4161 randomised
277 assigned
to placebo
555 assigned
to 5 and
80 mg/day
FDC weeks
14 and 10
and
160 mg/day
weeks 58
33 discontinued
10 adverse
events
9 insucient
response
5 lost to
follow-up
2 protocol
violation
5 withdrew
consent
2 other
555 assigned
to 5 and
160 mg/day
FDC weeks
14 and 10
and
320 mg/day
weeks 58
65 discontinued
15 adverse
events
6 insucient
response
5 lost to
follow-up
12 protocol
violation
22 withdrew
consent
5 other
554 assigned
to 10 and
160 mg/day
FDC weeks
14 and 20
and
320 mg/day
weeks 58
59 discontinued
9 adverse
events
5 insucient
response
13 lost to
follow-up
4 protocol
violation
20 withdrew
consent
8 other
555 assigned
to 5 mg/day
nebivolol
weeks
14 and
10 mg/day
weeks 58
48 discontinued
9 adverse
events
3 insucient
response
9 lost to
follow-up
6 protocol
violation
12 withdrew
consent
9 other
555 assigned
to 20 mg/day
nebivolol
weeks
14 and
40 mg/day
weeks 58
50 discontinued
12 adverse
events
6 insucient
response
9 lost to
follow-up
4 protocol
violation
12 withdrew
consent
7 other
555 assigned
to 80 mg/day
valsartan
weeks
14 and
160 mg/day
weeks 58
76 discontinued
22 adverse
events
1 insucient
response
11 lost to
follow-up
11 protocol
violation
18 withdrew
consent
13 other
555 assigned to
160 mg/day
valsartan
weeks
14 and
320 mg/day
weeks 58
57 discontinued
10 adverse
events
12 insucient
response
9 lost to
follow-up
6 protocol
violation
13 withdrew
consent
7 other
58 discontinued
10 adverse
events
7 insucient
response
9 lost to
follow-up
11 protocol
violation
17 withdrew
consent
4 other
244 completed
the study
490 completed
the study
496 completed
the study
506 completed
the study
505 completed
the study
479 completed
the study
498 completed
the study
497 completed
the study
277 included in
ITT analysis
549 included in
ITT analysis*
548 included in
ITT analysis*
550 included in
ITT analysis*
552 included in
ITT analysis*
547 included in
ITT analysis*
548 included in
ITT analysis*
547 included in
ITT analysis*
Figure 1: Trial prole
FDC=xed-dose combination. ITT=intention-to-treat. *6, 7, 4, 3, 8, 7, and 8 patients were missing diastolic blood pressure measurements after baseline, respectively.
Results
Between Jan 6, 2012 (rst participant, rst visit), and
March 15, 2013 (last participant, last visit), 4161 participants were randomly assigned to receive double-blind
treatment, 4118 of whom were included in the intentionto-treat population (gure 1). Mean demographic and
clinical characteristics (table) and study completion rates
(gure 1) were comparable between treatment groups.
Consent withdrawal was the most frequent reason for
discontinuation in all active-treatment groups, with the
exception of nebivolol 40 mg/day (adverse events) and
nebivolol 10 mg/day (consent withdrawal; adverse events;
gure 1). Adherence at each visit was at least 99% for
every group.
The mean dierence in diastolic blood pressure
between baseline and week 8 ranged from 148 mm Hg
(SD 92) for the 10 and 160 mg/day xed-dose
combination to 157 mm Hg (96) for the 20 and
320 mg/day xed-dose combination; from 127 mm Hg
(90) for nebivolol 10 mg/day to 144 mm Hg (94) for
nebivolol 40 mg/day; and from 108 mm Hg (96) for
valsartan 160 mg/day to 112 mm Hg (93) for valsartan
320 mg/day (gure 2A). At week 8, the xed-dose
1892
combination 20 and 320 mg/day group had signicantly
greater reductions in diastolic blood pressure from
baseline than both nebivolol 40 mg/day (p=0030) and
valsartan 320 mg/day (p<00001; primary statistical
comparisons); all other comparisons were also
signicant, favouring the xed-dose combinations (all
p<00001). The least-squares mean dierence in the
primary endpoint between the xed-dose combination
and nebivolol ranged from 24 mm Hg (95% CI 34 to
13; p<00001) for the 10 and 160 mg/day xed-dose
combination compared with nebivolol 10 mg/day to 12
(23 to 01; p=0030) for the 20 and 320 mg/day xeddose combination compared with nebivolol 40 mg/day.
The least-squares mean dierence in the primary
endpoint between the xed-dose combination and
valsartan ranged from 37 mm Hg (95% CI 48 to
26; p<00001) for the 10 and 160 mg/day xed-dose
combination compared with valsartan 160 mg/day to
44 (54 to 33; p<00001) for the 20 and 320 mg/day
xed-dose combination compared with valsartan
320 mg/day.
The mean dierence in systolic blood pressure between
baseline and week 8 ranged from 177 mm Hg (SD 153)
www.thelancet.com Vol 383 May 31, 2014
Articles
Placebo
(n=277)
Age (years)
511 (104)
Nebivolol and valsartan xed-dose combination,
nal dose
10 and
160 mg/day
(n=555)
10 and
320 mg/day
(n=555)
20 and
320 mg/day
(n=554)
509 (101)
516 (98)
508 (97)
Nebivolol, nal dose
Valsartan, nal dose
10 mg/day
(n=555)
160 mg/day
(n=555)
320 mg/day
(n=554)
517 (99)
511 (107)
517 (102)
40 mg/day
(n=554)
515 (108)
Sex
Men
148 (53%)
300 (54%)
315 (57%)
313 (56%)
307 (55%)
297 (54%)
333 (60%)
295 (53%)
Women
129 (47%)
255 (46%)
240 (43%)
241 (44%)
248 (45%)
257 (46%)
222 (40%)
259 (47%)
White
231 (83%)
464 (84%)
475 (86%)
474 (86%)
452 (81%)
471 (85%)
481 (87%)
475 (86%)
Black
30 (11%)
56 (10%)
56 (10%)
52 (9%)
69 (12%)
54 (10%)
43 (8%)
51 (9%)
Other
16 (6%)
35 (6%)
24 (4%)
28 (5%)
34 (6%)
29 (5%)
31 (6%)
28 (5%)
Race
Ethnic origin
Hispanic
113 (41%)
252 (45%)
239 (43%)
231 (42%)
206 (37%)
220 (40%)
207 (37%)
216 (39%)
Non-Hispanic
164 (59%)
303 (55%)
316 (57%)
323 (58%)
349 (63%)
334 (60%)
348 (63%)
338 (61%)
Weight (kg)
936 (206)
911 (204)
922 (200)
922 (208)
924 (212)
913 (212)
923 (208)
Body-mass index (kg/m)
326 (60)
319 (63)
320 (60)
320 (65)
321 (63)
320 (63)
318 (60)
921 (208)
320 (60)
Type 2 diabetes
40 (14%)
81 (15%)
88 (16%)
89 (16%)
82 (15%)
86 (16%)
84 (15%)
88 (16%)
522 (94%)
535 (97%)
Previously diagnosed with hypertension
264 (95%)
532 (96%)
524 (94%)
533 (96%)
532 (96%)
526 (95%)
Antihypertensive treatment before enrolment*
212/264 (80%)
429/532 (81%)
420/524 (80%) 402/522 (77%)
408/533 (77%)
432/532 (81%)
420/526 (80%) 427/535 (80%)
Trough seated SBP (mm Hg)
1554 (112)
1546 (118)
1554 (111)
1546 (115)
1551 (118)
1551 (116)
1558 (121)
1551 (117)
Trough seated DBP (mm Hg)
998 (35)
996 (35)
996 (35)
999 (37)
999 (35)
998 (36)
998 (38)
997 (36)
Trough seated pulse ratio (beats per min)
780 (107)
778 (110)
773 (107)
782 (108)
770 (107)
776 (108)
775 (107)
Participation in the ABPM substudy
52 (19%)
108 (19%)
109 (20%)
110 (20%)
106 (19%)
109 (20%)
104 (19%)
771 (114)
107 (19%)
Data are mean (SD) or number (%). Some percentages do not total 100 because of rounding. ABPM=ambulatory blood pressure monitoring. DBP=diastolic blood pressure. SBP=systolic blood pressure.
*Percentages are relative to the numbers of patients previously diagnosed with hypertension. Intention-to-treat population.
Table: Demographics and clinical characteristics at baseline (safety population)
for the 10 and 160 mg/day xed-dose combination to
178 mm Hg (158) for the 20 and 320 mg/day xeddose combination; from 142 mm Hg (148) for nebivolol
10 mg/day to 151 mm Hg (165) for nebivolol
40 mg/day; and from 142 mm Hg (144) for valsartan
160 mg/day to 148 mm Hg (151) for valsartan
320 mg/day (gure 2B). At week 8, the xed-dose
combination 20 and 320 mg/day group had signicantly
greater reductions in systolic blood pressure from
baseline than both nebivolol 40 mg/day (p=0001) and
valsartan 320 mg/day (p=00005; primary statistical
comparisons); all other comparisons were also signicant,
favouring the xed-dose combinations (all p<001). The
least-squares mean dierence in the key secondary
endpoint between the xed-dose combination and
nebivolol ranged from 36 (95% CI 53 to 18;
p<00001) for the 10 and 160 mg/day xed-dose
combination compared with nebivolol 10 mg/day to 29
(47 to 11; p=0001) for the 20 and 320 mg/day xeddose combination compared with nebivolol 40 mg/day.
The least-squares mean dierence in the key secondary
endpoint between the xed-dose combination and
valsartan ranged from 39 (95% CI 57 to 21;
p<00001) for the 10 and 160 mg/day xed-dose
combination compared with valsartan 160 mg/day to 31
(49 to 14, p=00005) for the 20 and 320 mg/day
www.thelancet.com Vol 383 May 31, 2014
xed-dose combination compared with valsartan 320 mg/
day. A similar xed-dose combination eect was evident
at week 4: for both diastolic and systolic blood pressure, a
signicant advantage of xed-dose combinations 5 and
80 mg/day and 5 and 160 mg/day was noted for all
comparisons with their corresponding monotherapies
(nebivolol 5 mg/day and valsartan 80 mg/day or
160 mg/day; all p<0001), except for a dierence between
xed-dose combination 5 and 160 mg/day and valsartan
160 mg/day on systolic blood pressure (p=011; gure 2C
and 2D).
In the ABPM substudy, the reduction in 24-h diastolic
and systolic blood pressure at week 8 was signicantly
greater in the xed-dose combination 20 and 320 mg/day
group than in the valsartan 320 mg/day group, but was
not signicantly greater than in the nebivolol 40 mg/day
group (gure 3A and 3B). At week 8, blood pressure
control rates were signicantly greater in the xed-dose
combination 20 and 320 mg/day group (285 of 550 [52%])
than in the valsartan 320 mg/day group (195 of 547 [36%];
p<00001) and the nebivolol 40 mg/day group
(247 of 547 [45%]; p=0023; gure 3C).
For participants treated with a xed-dose combination,
changes in pulse rate from baseline to week 8 were similar
to those in participants treated with the corresponding
nebivolol monotherapies, and in participants taking
1893
Articles
Diastolic blood pressure, baseline to week 8 (primary endpoint)
Systolic blood pressure, baseline to week 8 (key secondary endpoint)
Mean change from baseline (mm Hg)
0
998
996
998
999
996
997
998
999
1554
1546
1558
1551
1554
1551
1546
4
6
8
10
12
14
16
p<00001
18
p<00001 p<00001
p<00001
p=0030
p<00001
p<00001
p<00001
bo
80
m 0a
g/ nd
da
y
16 Va
0 m lsa
g/ rtan
da
y
N
10 eb
m ivo
g/ lo
d l
FD ay
32 C
0 m 10
g/ and
da
y
V
32 a
0 m lsa
g/ rtan
da
y
40 Neb
i
m vo
g/ lo
da l
FD y
32 C
0 m 20
g/ and
da
y
C1
ce
p=0001
p=00005
Diastolic blood pressure
Week 4
Placebo
Valsartan 80 mg/day
Valsartan 160 mg/day
Nebivolol 5 mg/day
Nebivolol 20 mg/day
FDC 5 and 160 mg/day
FDC 5 and 80 mg/day
FDC 10 and 160 mg/day
0
2
4
6
Week 8
Placebo
Valsartan 160 mg/day
Valsartan 320 mg/day
Nebivolol 10 mg/day
Nebivolol 40 mg/day
FDC 10 and 160 mg/day
FDC 10 and 320 mg/day
FDC 20 and 320 mg/day
FDC 5 and 80 mg/day vs nebivolol 5, p<00001
FDC 5 and 80 mg/day vs valsartan 80, p<00001
FDC 5 and 160 mg/day vs nebivolol 5, p<00001
FDC 5 and 160 mg/day vs valsartan 160, p<00001
8
10
12
FDC 20 and 320 mg/day vs nebivolol 40, p=0030
FDC 20 and 320 mg/day vs valsartan 320, p<00001
FDC 10 and 160 mg/day vs nebivolol 10, p<00001
FDC 10 and 160 mg/day vs valsartan 160, p<00001
FDC 10 and 320 mg/day vs nebivolol 10, p<00001
FDC 10 and 320 mg/day vs valsartan 320, p<00001
14
16
18
p=0001
FD
Pla
bo
ce
FD
Pla
80 C 1
m 0a
g/ nd
da
y
16 Va
0 m lsa
g/ rtan
da
N y
10 eb
m ivo
g/ lo
da l
y
FD
32 C
0 m 10
g/ and
da
y
32 Va
0 m lsa
g/ rtan
da
y
40 Neb
m ivo
g/ lo
d l
F ay
32 DC
0 m 20
g/ and
da
y
p<00001
Least-squares mean change from baseline (mm Hg)
1551
Systolic blood pressure
Least-squares mean change from baseline (mm Hg)
2
0
2
4
6
FDC 5 and 80 mg/day vs nebivolol 5, p=00001
FDC 5 and 80 mg/day vs valsartan 80, p=00007
FDC 5 and 160 mg/day vs nebivolol 5, p<00001
FDC 5 and 160 mg/day vs valsartan 160, p=011
8
10
12
FDC 20 and 320 mg/day vs nebivolol 40, p=0001
FDC 20 and 320 mg/day vs valsartan 320, p=00005
FDC 10 and 160 mg/day vs nebivolol 10, p<00001
FDC 10 and 160 mg/day vs valsartan 160, p<00001
FDC 10 and 320 mg/day vs nebivolol 10, p<00001
FDC 10 and 320 mg/day vs valsartan 320, p=0001
14
16
18
0
4
Week
Figure 2: Changes in trough seated diastolic and systolic blood pressure from baseline to week 8 and visit by visit
Analyses were by intention to treat, last observation carried forward. All active-treatment groups were signicantly dierent from placebo at weeks 4 and 8 (p<0001
for all). Error bars are SEM. (A and B) Numbers in bars are mean values at baseline. FDC=xed-dose combination.
1894
www.thelancet.com Vol 383 May 31, 2014
Articles
24-h ABPM diastolic blood pressure, baseline to week 8
24-h ABPM systolic blood pressure, baseline to week 8
Mean change from baseline (mm Hg)
0
858
873
866
886
1373
4
1422
1408
1418
6
10
8
10
15
12
14
20
p<00001
Placebo
(n=52)
FDC
20 and 320
mg/day
(n=110)
Nebivolol
40 mg/day
(n=107)
Valsartan
320 mg/day
(n=105)
p<00001
p=00002
p<00001
50
p=0003
233
549
40
242
218 550
547
227
548
180
171
548
552
30
p=00005
Placebo
FDC 5 and 80 mg/day
Valsartan 80 mg/day
Nebivolol 5 mg/day
FDC 5 and 160 mg/day
Valsartan 160 mg/day
Nebivolol 20 mg/day
FDC 10 and 160 mg/day
FDC
20 and 320
mg/day
(n=110)
Nebivolol
40 mg/day
(n=107)
p=0001
p<00001 p<00001
p=00001
268
549
p=0023
285
550
256
548
213
200 552
548
174
547
20
10
Placebo
(n=52)
Blood pressure control rates, baseline to week 4 and week 8
60
Blood pressure control (%)
p=0003
247
547
Valsartan
320 mg/day
(n=105)
Placebo
FDC 10 and 160 mg/day
Valsartan 160 mg/day
Nebivolol 10 mg/day
FDC 10 and 320 mg/day
Valsartan 320 mg/day
Nebivolol 40 mg/day
FDC 20 and 320 mg/day
195
547
58
277
47
277
0
Week 4
Week 8
Figure 3: Changes in trough seated diastolic and systolic blood pressure in the ambulatory blood pressure monitoring substudy and blood pressure control
rates between baseline and week 8
Analyses were by intention to treat, last observation carried forward. (A and B) Numbers in bars are mean values at baseline. (C) Blood pressure control is dened as
blood pressure <130/80 mm Hg for individuals with type 2 diabetes or <140/90 mm Hg for those without. Numbers in bars are ratios of responders versus participants
in a given group. FDC=xed-dose combination.
valsartan only, mean pulse rate changes were similar to
those reported in participants receiving placebo (gure 4A).
In a post-hoc analysis, the decrease in pulse pressure with
the xed-dose combination 20 and 320 mg/day was greater
than the decrease noted with nebivolol 40 mg/day
(p=00053), but seemed to be smaller than the decrease
reported with valsartan 320 mg/day (p=0053; gure 4B).
Across all treatment groups, subgroup analyses
revealed no signicant interactions between treatment
and sex, race, diabetes status, or diastolic blood pressure
status at baseline (<median or median) when analysing
the primary or key secondary ecacy endpoints (baseline
to week 8 changes in diastolic or systolic blood pressure);
www.thelancet.com Vol 383 May 31, 2014
however, signicant interactions were noted between
treatment and Hispanic ethnic origin when analysing
diastolic (p=0004) and systolic blood pressure (p=0017),
and between treatment and age (p=0018) and treatment
and obesity status (p=0030) when analysing systolic
blood pressure. Findings from an exploratory post-hoc
assessment suggest that the signicant interactions
associated with the Hispanic ethnicity and age group
may have been driven by a higher placebo response
among Hispanics and those at least 65 years of age
(gure 5). The eects of the xed-dose combination
20 and 320 mg/day versus placebo were clinically
signicant across a range of patient phenotypes (gure 5).
1895
Articles
Pulse rate, baseline to week 8 (additional ecacy parameter)
Mean change from baseline (beats per min)
0
780
778
775
773
770
771
776
782
2
4
6
8
10
12
14
p<00001
p<00001
p<00001
Pulse pressure, baseline to week 8 (post-hoc analysis)
Mean change from baseline (mm Hg)
556
550
560
552
558
554
554
547
Discussion
p=0021
p=0052
p=00053
p=0053
Placebo
FDC
Valsartan Nebivolol
10 and 160 160 mg/day 10 mg/day
mg/day
FDC
Valsartan
Nebivolol
FDC
10 and 320 320 mg/day 40 mg/day 20 and 320
mg/day
mg/day
Figure 4: Mean changes in pulse rate and pulse pressure between baseline and week 8
Analyses were by intention to treat, last observation carried forward. Numbers in bars show mean values at
baseline. FDC=xed-dose combination.
During the 8-week treatment phase, discontinuation
rates because of an adverse event ranged from nine
of 555 (2%) for those in the 10 and 320 mg/day and 20 and
320 mg/day xed-dose combination groups to 22 of
555 (4%) in the nebivolol 40 mg/day group (gure 1). The
rates of experiencing at least one treatment-emergent
adverse event in the safety population were similar across
treatment groups: 100 of 277 (36%) in the placebo group,
193 of 555 (35%) in the xed-dose combination 10 and
160 mg/day group, 185 of 555 (33%) in the xed-dose
combination 10 and 320 mg/day group, 189 of 554 (34%) in
1896
the xed-dose combination 20 and 320 mg/day group,
196 of 555 (35%) in the nebivolol 10 mg/day group,
198 of 554 (36%) in the nebivolol 40 mg/day group, 165 of
555 (30%) in the valsartan 160 mg/day group, and 190
of 554 (34%) in the valsartan 320 mg/day group. Most
treatment-emergent adverse events were judged to be mild
or moderate in severity. The appendix lists treatmentemergent adverse events that occurred in at least 2% of the
safety population.
During double-blind treatment, 27 serious adverse
events were reported by three of 277 (1%) participants in
the placebo group (spontaneous abortion, cerebrovascular
accident, and transient ischaemic attack), two of
555 (<1%) in the xed-dose combination 10 and
160 mg/day group (ankle fracture and cerebrovascular
accident), two of 555 (<1%) in the xed-dose combination
10 and 320 mg/day group (acute myocardial infarction
and appendicitis), one of 554 (<1%) in the xed-dose
combination 20 and 320 mg/day group (diverticulitis),
two of 555 (<1%) in the nebivolol 10 mg/day group (acute
pyelonephritis and syncope), four of 554 (<1%) in the
nebivolol 40 mg/day group (hypotension, pancreatitis,
small intestinal obstruction, and thyroid cancer), four of
555 (<1%) in the valsartan 160 mg/day group (acute
respiratory failure, increased carbon dioxide, cerebral
infarction, intracranial aneurysm, mental status changes,
substance abuse, and suicide attempt), and ve of
554 (<1%) in the valsartan 320 mg/day group (acute
myocardial infarction, appendicitis, atrial brillation,
facial bone fracture, gastrointestinal haemorrhage, and
pneumonia). None of the serious adverse events were
judged to be related to treatment. Two deaths occurred
during the single-blind placebo run-in phase; both were
deemed not related to study drug. No deaths occurred
during double-blind treatment.
To our knowledge, this is the rst study to assess the
ecacy and safety of a xed-dose combination
consisting of a blocker and an angiotensin II receptor
blocker in patients with hypertension (panel).
Comparison between a xed-dose combination and the
highest approved doses of the monotherapy components is a regulatory requirement for assessment of
ecacy and safety.13 The data from this trial show a
signicant advantage of the xed-dose combination
consisting of 20 mg/day nebivolol and 320 mg/day
valsartan over monotherapy components at their
highest approved doses (40 mg/day nebivolol and
320 mg/day valsartan), including a greater reduction of
diastolic and systolic blood pressure and greater
proportions of participants who responded to treatment
or achieved blood pressure treatment goals. Other
nebivolol and valsartan xed-dose combinations
examined resulted in signicantly greater reductions
from baseline in diastolic and systolic blood pressure
compared with their monotherapy components.
www.thelancet.com Vol 383 May 31, 2014
Articles
FDC 20 and 320 mg/day
Placebo
Men
310
148
Women
240
129
Sex
BMI
30 kg/m2
310
177
<30 kg/m2
240
100
Ethnic origin
Hispanic
228
113
Non-Hispanic
322
164
Race
52
30
498
247
<65 years
509
250
65 years
41
27
Black
Non-black
Age (years)
Diabetes
Yes
89
40
No
461
237
Baseline diastolic blood pressure
<Median
239
121
Median
311
156
16 14 12 10 8 6 4 2 0 2 4
Systolic blood pressure (mm Hg),
LSMD (95% CI)
16 14 12 10 8 6 4 2 0 2 4
Diastolic blood pressure (mm Hg),
LSMD (95% CI)
Figure 5: Antihypertensive eects of xed-dose combination 20 and 320 mg/day (placebo-subtracted values) by subgroup
Analyses were by intention to treat, last observation carried forward. BMI=body-mass index. FDC=xed-dose combination. LSMD=least-squares mean dierence.
The absence of a dose response in the xed-dose
combination groups (gure 2) could be attributed to the
at dose responses for both nebivolol8 and valsartan.17 The
well-established tolerability of nebivolol8 and valsartan18
monotherapies was shown in a favourable tolerability
prole of the combination. Adverse events commonly
associated with -blocker use (eg, bradycardia, fatigue,
and dizziness)19,20 were noted with the highest nebivolol
dose (40 mg/day, which is rarely used in clinical practice
and is associated with a loss of 1 selectivity10), but not
with clinically common doses (520 mg/day; appendix).
Finally, post-hoc and exploratory ndings suggest that
the nebivolol and valsartan xed-dose combination has a
haemodynamic eect that includes reductions in both
pulse rate and pulse pressure (consistent with pharmacological properties of individual components)10,15 and that
this combination would be eective in a wide variety of
patients. The absence of a systolic blood pressure eect
in participants at least 65 years old is probably an artifact
of subdivision of the sample and the small number of
participants in that category.
Data interpretation is limited by several factors,
including the size of the ABPM substudy, which might
have been too small to capture a signicant dierence in
24-h ABPM data between the groups treated with xeddose combination 20 and 320 mg/day and nebivolol
40 mg/day. Moreover, available data suggest that both
increases in dose and treatment duration for nebivolol8
www.thelancet.com Vol 383 May 31, 2014
Panel: Research in context
Systematic review
We did not undertake a systematic review per se, but relied on ndings from relevant
meta-analyses. The benets of combining blood-pressure-lowering drugs from two
dierent drug classes for the eective management of hypertension have been reported
in many studies, including a meta-analysis of 42 trials with a total of 11 000 participants.1
In that analysis, the combination of two drugs from separate classes (a thiazide plus a
blocker; a thiazide plus an angiotensin-converting-enzyme inhibitor; a blocker plus an
angiotensin-converting-enzyme inhibitor; a blocker plus a calcium-channel blocker; and
a calcium-channel blocker plus an angiotensin-converting-enzyme inhibitor) resulted in
additive eects that were greater than those of a double dose of a single drug. Several
factors that might be useful when selecting drugs for combination therapy include
absence of a pharmacokinetic interaction, reduction in long-term adverse cardiovascular
incidences, and mechanisms of action that target dierent disease pathways.16 Doubts
have been raised previously about the eectiveness of a potential blocker and
angiotensin II receptor blocker combination because of a potential overlap in their
mechanism of action.16 To our knowledge, our study is the rst examination of a
combination consisting of a blocker and an angiotensin II receptor blocker in
participants with hypertension.
Interpretation
This study showed the potential of a nebivolol and valsartan combination. Better ecacy
and comparable tolerability of the xed-dose combination compared with its
monotherapy components suggests that nebivolol and valsartan in combination would
be an eective and safe treatment option for patients with hypertension but with systolic
and diastolic blood pressure less than 180/110 mm Hg.
1897
Articles
and valsartan21 would be expected to ultimately play a
part in ecacy. Additionally, a strong placebo response,
especially among Hispanics and participants at least
65 years old, and also among the small number of elderly
participants, makes assessment of the ecacy of the
combination in those subgroups dicult. Finally, a
design following a perfect Latin square, similar to the
one used in combination studies of nebivolol and hydrochlorothiazide,17,18 might have provided better insight
into a potential dose response of the nebivolol and
valsartan combination.
Contributors
TDG designed the study; collected, analysed, and interpreted data; and
wrote and reviewed the manuscript. MAW, JB, AHG, DBB, and
MP designed the study, interpreted data, and revised the manuscript.
WC designed the study, analysed data, and revised the manuscript.
Declaration of interests
In the past 36 months, TDG has received personal fees from Forest
Laboratories. MAW has received speaker, consultant, or research fees
from Forest, Boehringer-Ingelheim, Daiichi-Sankyo, Takeda, Medtronic,
Boston Scientic, AstraZeneca, and Arbor. JB has received consultant
fees from Forest. AHG has received grants, personal fees or non-nancial
support from Forest, Novartis, Daiichi-Sankyo, Takeda, the American
Society for Hypertension, and the American College of Cardiology.
DBB, WC, and MP are employees of Forest Research Institute.
Acknowledgments
Kristen Andersen, Autumn Kelly, Vojislav Pejovi, Leah Richmond, and
Bill Sterling of Prescott Medical Communications Group (Chicago, IL,
USA) assisted with literature searches, editing, creation of graphs and
tables, circulation of drafts among the authors, and formatting of the
manuscript for submission.
References
1
Wald DS, Law M, Morris JK, Bestwick JP, Wald NJ. Combination
therapy versus monotherapy in reducing blood pressure:
meta-analysis on 11,000 participants from 42 trials. Am J Med 2009;
122: 290300.
2
Chobanian AV, Bakris GL, Black HR, et al, and the Joint
NationalCommittee on Prevention, Detection, Evaluation, and
Treatment ofHigh Blood Pressure. National Heart, Lung, and
Blood Institute, and the National High Blood Pressure Education
Program Coordinating Committee. Seventh report of the Joint
National Committee on Prevention, Detection, Evaluation, and
Treatment ofHigh Blood Pressure. Hypertension 2003; 42: 120652.
3
Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC guidelines
for the management of arterial hypertension: the Task Force for the
Management of Arterial Hypertension of the European Society of
Hypertension (ESH) and of the European Society of Cardiology
(ESC). Eur Heart J 2013; 34: 2159219.
4
Salahuddin A, Mushtaq M, Materson BJ. Combination therapy
forhypertension 2013: an update. J Am Soc Hypertens 2013;
7: 40107.
5
Bangalore S, Kamalakkannan G, Parkar S, Messerli FH. Fixed-dose
combinations improve medication compliance: a meta-analysis.
Am J Med 2007; 120: 71319.
1898
9
10
11
12
13
14
15
16
17
18
19
20
21
Sherrill B, Halpern M, Khan S, Zhang J, Panjabi S. Singlepillvsfree-equivalent combination therapies for hypertension:
ameta-analysis of health care costs and adherence.
J Clin Hypertens (Greenwich) 2011; 13: 898909.
Imaizumi S, Miura S, Yahiro E, Uehara Y, Komuro I, Saku K.
Class- and molecule-specic dierential eects of angiotensin II
type 1 receptor blockers. Curr Pharm Des 2013; 19: 300208.
Weiss RJ, Saunders E, Greathouse M. Ecacy and tolerability
ofnebivolol in stage III hypertension: a pooled analysis of data
from three randomized, placebo-controlled monotherapy trials.
Clin Ther 2011; 33: 115061.
Gao Y, Vanhoutte PM. Nebivolol: an endothelium-friendly selective
1-adrenoceptor blocker. J Cardiovasc Pharmacol 2012; 59: 1621.
Vanhoutte PM, Gao Y. Beta blockers, nitric oxide, and
cardiovascular disease. Curr Opin Pharmacol 2013; 13: 26573.
Hussein O, Shneider J, Rosenblat M, Aviram M. Valsartan therapy
has additive anti-oxidative eect to that of uvastatin therapy
against low-density lipoprotein oxidation: studies in
hypercholesterolemic and hypertensive patients.
J Cardiovasc Pharmacol 2002; 40: 2834.
Ogawa S, Mori T, Nako K, Kato T, Takeuchi K, Ito S. Angiotensin II
type 1 receptor blockers reduce urinary oxidative stress markers in
hypertensive diabetic nephropathy. Hypertension 2006; 47: 699705.
ICH Expert Working Group. International Conference on
Harmonisation of Technical Requirements for Registration of
Pharmaceuticals for Human Use. Principles for Clinical Evaluation
of New Antihypertensive Drugs. 2000. http://www.fda.gov/
downloads/Drugs/GuidanceComplianceRegulatoryInformation/
Guidances/ucm073147.pdf (accessed Feb 1, 2014).
US Food and Drug Administration. Ttile 21. Code of Federal
Regulators. Section 310.545. Subchapter D: Drugs for Human Use,
Part 300, Subpart B-Combination Drugs. Washington, DC:
USDepartment of Health and Human Services, 2013.
Hochberg Y. A sharper Bonferroni procedure for multiple tests
ofsignicance. Biometrika 1988; 75: 80002.
Gradman AH, Basile JN, Carter BL, et al. Combination therapy
inhypertension. J Am Soc Hypertens 2010; 4: 9098.
Makani H, Bangalore S, Supariwala A, Romero J, Argulian E,
Messerli FH. Antihypertensive ecacy of angiotensin receptor
blockers as monotherapy as evaluated by ambulatory blood pressure
monitoring: a meta-analysis. Eur Heart J 2013; published online
Aug 21. DOI:10.1093/eurheartj/eht333.
Markham A, Goa KL. Valsartan. A review of its pharmacology and
therapeutic use in essential hypertension. Drugs 1997; 54: 299311.
Ambrosioni E, Borghi C. Tolerability of nebivolol in head-to-head
clinical trials versus other cardioselective -blockers in the
treatment of hypertension. High Blood Press Cardiovasc Prev 2005;
12: 2735.
Kountz DS. Are tolerability concerns a class eect of beta-blockers
in treating patients with hypertension? Postgrad Med 2009;
121: 1424.
Weir MR, Levy D, Crikelair N, Rocha R, Meng X, Glazer R.
Timetoachieve blood-pressure goal: inuence of dose of valsartan
monotherapy and valsartan and hydrochlorothiazide combination
therapy. Am J Hypertens 2007; 20: 80715.
www.thelancet.com Vol 383 May 31, 2014
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Nebesel LaunchPlDocument42 pagesNebesel LaunchPlPrithvi Raj100% (1)
- Drug Profile NebivololDocument6 pagesDrug Profile NebivololKrista ColePas encore d'évaluation
- Byscard DHTN Product PresentationDocument51 pagesByscard DHTN Product PresentationDr.abdul GhaffarPas encore d'évaluation
- Sympa T Holy TicsDocument30 pagesSympa T Holy TicsAhaisibwe GordonPas encore d'évaluation
- Nebilet ObukaDocument53 pagesNebilet ObukaDeni100% (1)
- Preferred Beta-Blockers For The Treatment of Heart FailureDocument7 pagesPreferred Beta-Blockers For The Treatment of Heart FailureAshutosh SinghPas encore d'évaluation
- Drug Study (CHF)Document9 pagesDrug Study (CHF)Ericka VillanuevaPas encore d'évaluation
- Drugs Interaction Basic & Clinical Pharmacology (PDFDrive) - 1170-1187Document18 pagesDrugs Interaction Basic & Clinical Pharmacology (PDFDrive) - 1170-1187Ismail Ali إسماعيل عليPas encore d'évaluation
- Aim and ObjectivesDocument3 pagesAim and ObjectivesDevvrat DubeyPas encore d'évaluation
- Nebivolol HydrochlorideDocument8 pagesNebivolol HydrochloridePrasad MungekarPas encore d'évaluation
- Nebivolol in HtaDocument16 pagesNebivolol in HtaCodruta Emanuela Maria VirsescuPas encore d'évaluation
- 4 - 2 Not All Beta Blocker Are The Same Out With The Old, in With The New - Prof - Romdoni, FIHADocument29 pages4 - 2 Not All Beta Blocker Are The Same Out With The Old, in With The New - Prof - Romdoni, FIHAsamuelidsPas encore d'évaluation
- Hypertension Management: Is Beta Blockers Still EffectiveDocument55 pagesHypertension Management: Is Beta Blockers Still EffectiveRidyahningtyas SintowatiPas encore d'évaluation
- Drug IndexDocument362 pagesDrug IndexsrhmdPas encore d'évaluation
- Nebivolol Versus Carvedilol or MetoprololDocument7 pagesNebivolol Versus Carvedilol or MetoprololRuslan RidcodubskiiPas encore d'évaluation
- Comparison of The Effects of Nebivolol and Bisoprolol On Systematic Vascular Resistance in Patients With Essential HypertensionDocument15 pagesComparison of The Effects of Nebivolol and Bisoprolol On Systematic Vascular Resistance in Patients With Essential HypertensionSherif KamalPas encore d'évaluation
- Adrenergic DrugsDocument22 pagesAdrenergic DrugsDan Mark Lavega OmadlePas encore d'évaluation
- Pharmacology Practical NotesDocument24 pagesPharmacology Practical NotesStefy BarranoPas encore d'évaluation
- Nebivolol Hydrochlorothiazide Prescribing InformationDocument7 pagesNebivolol Hydrochlorothiazide Prescribing InformationRaihan RakibPas encore d'évaluation