Académique Documents
Professionnel Documents
Culture Documents
Other Visual Disorders Reviewer
Transféré par
Wendy EscalanteCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Other Visual Disorders Reviewer
Transféré par
Wendy EscalanteDroits d'auteur :
Formats disponibles
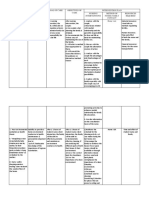
1 Other visual disorders (escalante-saac)
1. Retinal detachment
Retinas innermost layer of the eye
Serious and sight threatening event but is painless
Retina becomes separated from its underlying supportive tissue
*Degenerative causes
*Trauma
*Inflammation
*Tumor
*Diabetic retinopathy
*Cataract as complication
CAUSES
Light flashes
Wavy/watery vision
Veil/curtain obstructing vision
Shower/floater that resembles
spots, spider webs
Clinical manifestation
Glaucoma
Infxn of area
Complications
RISK FACTORS:
*Extremely near sighted
*Retinal detachment of other eye
*Fam hx of retinal detachment
D/E
*Indirect opthalmoscopy
*Slit lamp exam
*3-mirror ginoscopy
Reattach the detached part of the
retina
TREATMENT
4 Surgical procedures:
1. Cryotherapy laser
procedure/freeze treatment
2. Scleral buckle
3. Electrodiathermy
4. Protocoagulation
Most used method; localizing the position of all retina break w/ cryopobe; supporting all retina
breaks w/ scleral buckle
Electrode needle passed through sclera to allow subretinal fluid escape
Method of treating detachments of retina w/ argon laser
The high intensity beam of light from laser is converted into heat w/c forces protein molecule
in affected . . .
NURSING INTER:
*Assess hx of trauma
Post op nsg inter:
*Assess visual acuity
*Avoid bumping of head
*Encourage ambulation and independence
*Avoid rapid eye movements
*dRIVING IS RESTICTED
*Avoid straining/bending
*Apply clean water to eyes for 10 min
2. Diabetic Retinopathy
Complication of DM
-Damage of tiny blood vessels in eyes
-Often affected by increased blood sugar lvls
PATHO
*Develops when increased blood sugar lvl damage capillaries of retina. Blood vessels weaken
and are prone to rapture.
Eye painless
Partial/total loss vision
Blurred vision/lens opacity
CM
Macular edema
Severe vision loss
Blindness
Complications
*Maintain safety
*Miantain blood sugar lvls
*Laser therapy
TREATMENT
1. Aspirin
2. ACE inhibitor
MEDS
prevent or delay dvpt of diabetic retinopathy
Reduce risk of progression of diabetic retinopathy
HPN
Its recognized for risk factor for progression of DM retinopathy and DM vascular edema
*Impaired visual perception
DX
3. Macular degeneration
Leading cause of central vision loss, cells result to breakdown
*Macular degeneration test
*Retinal exam
*Fluorescein angiography
D/E
Amsler grid is used
*Age
*Obesity
*Inactivity
*Heredity
*HPN
*Smoking
*Toxic effects of drugs
Risk factors
Gradual dec of central vision
Black spots around central vision
NO CURE
CM
2 Other visual disorders (escalante-saac)
TREATMENT
4. Central artery/vein occlusion
Sudden painless and complete loss of vision in the eye
Branch artery occlusion
Sudden, painless, partial loss of vision in the eye
*Opthalmoscope
D/E
NO TREATMENT
TREATMENT
HPN, DM, Inc cholesterol, heart
disease, atherosclerosis, glaucoma
INC RISK FACTORS
RETINITIS PIGMENTOSA
No cure
Grp of genetic d/os that affect retina to respond to light
Diagnosis during childhood
BONS SPICULE SHAPE PIGMENTS DEPOSITS
CM
*Diff seeing in dimlighting
*Trips easily/bump into object
*Eye fatigue
*Loss of night vision
*Opthalmoscope
D/E
NONE
Treatment
CORNEAL D/OS
1. Keratititis
Inflammation of cornea, a transparent membrane that covers the colored part of the eye
-Both children and adult
CM
*Photophobia
*Loss of vision
*Diff opening of eye
*Inc tearing
Causes
*Poor contact lenses
*Overuse of contact lense
*Viral infxns
*Poor hygiene and nutrition
Glaucoma
Ulceration of cornea
Blindness
Complications
*Fluorescent staining w/ slit lamp
*Microscope
D/E
Identify the abrasion
1. Topical antiinfectives,
eyedrops/ointment
2. Analgesics
3. Corticosteroid
*Corneal transplant/Keratoplasty
PHARMA
SURGERY
Replacement if diseased cornea by healthy corneal tissue
PREVENTION
1. Use sterile lens in cleaning and disinfecting soln
2. Dont overwear contact lenses
3. Warm compress if theres pain
HEALTH ED
1. Teach pt to approp way to use topical antibiotics
2. Iritis/uveitis
Inflammation of the uvea, consist of 3 structures: iris. Ciliary
Anterior uveitis
Inflamm of front part of the eye
PATHO:
1. Anterior- involves iris and ciliary body
2. Intermediate- Involves ciliary body, vitreous & retina
3. Posterior uveitis- Involves retina, chloroid and optic nerve
4. Diffused uveitis- Involves front and back of the eye
Cataracts, glaucoma
Compications
P/E
Opthalmoscopy
Tenometry
D/E
1. Atropine eyedrops
2. Corticosteroids
3. Analgesic
TREATMENT
Dilate pupil and relieve spasm
Prevents inflamm
Reduce pain
EYELID AND CONJUNCTIVAL D/OS
1. Ectropion
Eyelid turned outward and doesnt come in contact w/ eyebal & inner surface is exposed
-Age of 60
-Sagging down of eyelid
-Most common in lower eyelid
ETIOLOGY
*Aging process and weakening of the connective tissue
*Contraction of the scar tissue from burns/bells palsy/ down syndrome
CM:
Epipion?
Outward turning of eyelid
TREAMENT
Outward tearing of the eye
*Daily eye cleaning w/ boiled water (PNSS)
*Artificial tears- prevent drying
3 Other visual disorders (escalante-saac)
*Antibiotic drops- treat inffection
*Palpebral conjuntiva thickens and
keratinizes
COMPLICATION
NONE
PREVENTION
Disturbed body image r/t changes
in appearance
NSG DX
2. Entropion
Eyelids turned and against eyeball
-Edge of 1 eyelid turned in
-Pts over 50 y.o.
1. Senile
2. Congenital
3. Spastic
4. Cicatricial
CLASSIFICATIONS:
Most common, disinserted
Upper eyelid
-Fold of skin that overlaps eyelids
Secondary to neurologic inflammatory/irritative process
Result of scarcification of palpebral conjunctiva w/ consequent inward/rotation of eyelid
margin
CM
*Excessive tearing,
*eye irritation (sandy gritting eye)
*burning,
*eye pain
P.E.
D/E
*Artificial teardrops
*Antibiotic
*Senile-eyelid retraction via tapng
TREATMENT
3. Pterygium
Also called as winged growth
-Fibrovascular proliferation of bulbar conjuntiva that grows toward the cornea
PATHO:
-Nourished by tiny capillaries that supply blood to tissue
Sun exposure
CAUSE
*Growth of tissue
*Dec vision
*Irritation, redness and scarring
CM
Artificial tears
Eye drops
TREATMENT
4. Ptosis
Drooping of upper eyelids
Drip droop only slightly
Weakness of levator muscles
5. Lagopthalmos
Eyelids dont close to cover the eye completely
result to dry eyes
If untreated, can lead to blindness
Stroke, infxn, facial paralysis
CAUSES
Artificial tears
Surgical tape
Flexible goggles
Tarsorrhaphy
TREATMENT
6. Blepharitis
Inflammation of the entire eyelid, caused by excess growth of bacteria in the area of eyes
CM
*Feeling like something in the eye
*Blurring of eye
*Blurred vision
MGT
*Proper lid hygiene
*Removing all make-up before bedtime
7. Hordeolum/Stye
Acute inflam/abscess involving glandular structure pfeyelids
-CAUSE: Staphylococcus bacteria eye infection
Acute, tender swelling
CM
MGT
*Warm, moist compress 4x a day
*Lid scrub/hygiene
*Darken rm
8. Conjunctivitis(pink eye)
Inflammation of the conjunctiva
Virus, bacteria, irritates, allergies
CAUSES
CM
*Redness in sclera, inc amnts of tears
*Thick yellow discharge that crust over eyeglasses
Rare procedure that eyelids are sutured together to narrow opening
Eye trauma
-In the eyelids
Blunt contussion, hyphemia, orbital CONDITIONS IN EYE TRAUMA
fracture, laceration
Facial xrays
CT scan
Antibiotic:
erythromycin/sulfacetomide
Detect orbital fracture
*Surgery
*Cosmetic surgery
For optic nerve decompression
Myopia
Nearsightedness
D/E:
SURGERY
4 Other visual disorders (escalante-saac)
-Light in front of the retina
CONCAVE LENS- TREATMENT
Hyperopia
Farsightedness
CONVEX LENS-TREATMENT
Astigmatism
Light cant focused to retina
-Uneven curvature
LASIK(Laser assisted in sitsu
ketantomileusis)
TREATMENT
Vous aimerez peut-être aussi
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Assessment of Kidneys PDFDocument1 pageAssessment of Kidneys PDFWendy EscalantePas encore d'évaluation
- NCP 2 MiDocument16 pagesNCP 2 MiWendy EscalantePas encore d'évaluation
- NCPDocument3 pagesNCPWendy EscalantePas encore d'évaluation
- Modifiable Risk Factors Non - Modifiable Risk Factors: LegendDocument2 pagesModifiable Risk Factors Non - Modifiable Risk Factors: LegendWendy Escalante100% (1)
- Drug StudyDocument14 pagesDrug StudyWendy EscalantePas encore d'évaluation
- Nasogastric Tube Management and CareDocument21 pagesNasogastric Tube Management and CareWendy EscalantePas encore d'évaluation
- PATHODocument2 pagesPATHOWendy EscalantePas encore d'évaluation
- Acid-Ash DietDocument10 pagesAcid-Ash DietWendy Escalante0% (1)
- Concept Map of Carotid Artery DiseaseDocument2 pagesConcept Map of Carotid Artery DiseaseWendy EscalantePas encore d'évaluation
- Caring For The Bedridden PatientDocument1 pageCaring For The Bedridden PatientWendy EscalantePas encore d'évaluation
- Assessment of KidneysDocument1 pageAssessment of KidneysWendy EscalantePas encore d'évaluation
- 02 Orig Art 02 PDFDocument3 pages02 Orig Art 02 PDFWendy EscalantePas encore d'évaluation
- Therapeutic DietDocument3 pagesTherapeutic DietWendy EscalantePas encore d'évaluation
- Drug Study FinalDocument8 pagesDrug Study FinalWendy EscalantePas encore d'évaluation
- Brat DietDocument8 pagesBrat DietWendy EscalantePas encore d'évaluation
- At DietDocument8 pagesAt DietWendy EscalantePas encore d'évaluation
- Concept Map of CKD Gastrointestinal SymptomsDocument4 pagesConcept Map of CKD Gastrointestinal SymptomsWendy Escalante0% (1)
- Fundamentals in NursingDocument9 pagesFundamentals in NursingWendy EscalantePas encore d'évaluation
- Pediatric NursingDocument16 pagesPediatric NursingWendy Escalante100% (1)
- Degenerative Joint DiseaseDocument35 pagesDegenerative Joint DiseaseWendy EscalantePas encore d'évaluation
- DM Report1Document16 pagesDM Report1Wendy EscalantePas encore d'évaluation
- Case Presentation: Group 2Document30 pagesCase Presentation: Group 2Wendy EscalantePas encore d'évaluation
- Integrated Management of Childhood Illness: Sick Child Age 2 Months Up To 5 YearsDocument78 pagesIntegrated Management of Childhood Illness: Sick Child Age 2 Months Up To 5 YearsWendy EscalantePas encore d'évaluation
- FNCP CommunityDocument4 pagesFNCP CommunityWendy EscalantePas encore d'évaluation
- Nursing Care For Patient With Neurological DiseaseDocument8 pagesNursing Care For Patient With Neurological DiseaseWendy EscalantePas encore d'évaluation
- Diabetes MellitusDocument5 pagesDiabetes MellitusWendy EscalantePas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Lesson Plan For Science 3Document6 pagesLesson Plan For Science 3Dinah DimagibaPas encore d'évaluation
- The PhosphotronDocument6 pagesThe PhosphotronteslatikaPas encore d'évaluation
- Lenticular TechnologyDocument22 pagesLenticular Technologyabihari2006100% (2)
- Chapter 12 The Sense Organs Anatomy and Physiology of Eye Ear Skin Tongue NoseDocument7 pagesChapter 12 The Sense Organs Anatomy and Physiology of Eye Ear Skin Tongue NoseSanketraje JadhavPas encore d'évaluation
- New FC ProjectDocument16 pagesNew FC ProjectVanshita GarudPas encore d'évaluation
- RTVue Overview SlidesDocument50 pagesRTVue Overview SlidesSanjay Mukherjee100% (1)
- Lens Luxation in DogsDocument4 pagesLens Luxation in DogsBernadhete Gaudia SabirosePas encore d'évaluation
- Atlas of Pathologic MyopiaDocument188 pagesAtlas of Pathologic MyopiayosafatPas encore d'évaluation
- Laser Worker Surveillance Flow ChartDocument3 pagesLaser Worker Surveillance Flow ChartOh2BSum1Pas encore d'évaluation
- How Much Astigmatism To Treat in Cataract SurgeryDocument5 pagesHow Much Astigmatism To Treat in Cataract SurgeryPaulaPas encore d'évaluation
- CataractDocument51 pagesCataractApoorva AgrawalPas encore d'évaluation
- Ping BeckettDocument11 pagesPing BeckettVanessa TrustPas encore d'évaluation
- MPSC ForDocument193 pagesMPSC ForAshish GaikwadPas encore d'évaluation
- Ocular Penetrans Trauma and It EditDocument11 pagesOcular Penetrans Trauma and It EditTamsilPas encore d'évaluation
- How To Draw Anime - Eyes, Mouths, Noses and EarsDocument4 pagesHow To Draw Anime - Eyes, Mouths, Noses and Earssoulbrain20011373Pas encore d'évaluation
- Filedate - 629download Ebook Veterinary Ophthalmic Surgery PDF Full Chapter PDFDocument67 pagesFiledate - 629download Ebook Veterinary Ophthalmic Surgery PDF Full Chapter PDFwarren.alvarez156100% (22)
- Peripheral Retinal Degenerations: EditorDocument241 pagesPeripheral Retinal Degenerations: EditorFelipe AlarcónPas encore d'évaluation
- Lecture Three Convergence and Accommodation (AC/A) : Mr. Natnael L. (Lecturer) April/2017Document33 pagesLecture Three Convergence and Accommodation (AC/A) : Mr. Natnael L. (Lecturer) April/2017henok birukPas encore d'évaluation
- Topic 13 - Entoptic PhenomenaDocument4 pagesTopic 13 - Entoptic PhenomenashadowosPas encore d'évaluation
- Human Eye 5Document7 pagesHuman Eye 5NanditaPas encore d'évaluation
- BiometryDocument7 pagesBiometrysandip shelakePas encore d'évaluation
- CHAPTER 3 - SensationDocument59 pagesCHAPTER 3 - Sensationflammy07100% (1)
- Signal Computing: Digital Signals in The Software Domain - Eric C. LarsonDocument206 pagesSignal Computing: Digital Signals in The Software Domain - Eric C. LarsonBcalh3Pas encore d'évaluation
- Expanded Content - 02 - Species - GM BinderDocument86 pagesExpanded Content - 02 - Species - GM Binderoriah renneyPas encore d'évaluation
- Astigmatism 2Document35 pagesAstigmatism 2Thanujaa Uvaraj0% (1)
- Example10 enDocument20 pagesExample10 enapi-279889431Pas encore d'évaluation
- Anatomy Grades 5-6 Book 3Document65 pagesAnatomy Grades 5-6 Book 3Miha MargineanPas encore d'évaluation
- 2019 Health Assessment Examination - EyesDocument2 pages2019 Health Assessment Examination - Eyesharley dela cruzPas encore d'évaluation
- Csec 2009-1990Document162 pagesCsec 2009-1990Shari OliverPas encore d'évaluation
- Ophtha SGD 1Document4 pagesOphtha SGD 1Richelle IgnacioPas encore d'évaluation