Académique Documents
Professionnel Documents
Culture Documents
Circumcision 1
Transféré par
Irsyad ArraisCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Circumcision 1
Transféré par
Irsyad ArraisDroits d'auteur :
Formats disponibles
1
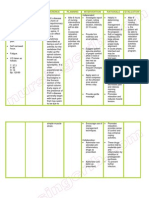
CIRCUMCISION
A circumcision performed in Central Asia, c.18651872
Male circumcision (from Latin circumcidere, meaning "to cut around")[1] is the
surgical removal of the foreskin (prepuce) from the human penis.[2][3][4] In a typical
procedure, the foreskin is opened and then separated from the glans after
inspection. The circumcision device (if used) is placed, and then the foreskin is
removed. Topical or locally injected anesthesia may be used to reduce pain and
physiologic stress.[5] For adults, general anesthesia is an option, and the procedure
is often performed without a specialized circumcision device. The procedure is
most often elected for religious reasons or personal preferences,[1] but may be
indicated for both therapeutic and prophylactic reasons. It is a treatment option for
pathological phimosis, refractory balanoposthitis and chronic urinary tract
infections (UTIs);[2][6] it is contraindicated in cases of certain genital structure
abnormalities or poor general health.[3][6]
The positions of the world's major medical organizations range from considering
neonatal circumcision as having no benefit and significant risks to having a modest
health benefit that outweighs small risks. No major medical organization
recommends either universal circumcision for all infant males (aside from the
recommendations of the World Health Organization for parts of Africa), or banning
the procedure.[7] Ethical and legal questions regarding informed consent and
autonomy have been raised over non-therapeutic neonatal circumcision.[8][9]
A 2009 Cochrane meta-analysis of studies done on sexually active heterosexual
men in Africa found that circumcision reduced their acquisition of HIV by 3866%
over a period of 24 months.[10] The WHO recommends considering circumcision as
part of a comprehensive HIV program in areas with high endemic rates of HIV,
such as sub-Saharan Africa,[11][12] where studies have concluded it is cost-effective
against HIV.[11] Circumcision reduces the incidence of HSV-2 infections by 28%,[13]
and is associated with reduced oncogenic HPV prevalence[14] and a reduced risk of
both UTIs and penile cancer,[5] but routine circumcision is not justified for the
prevention of those conditions.[2][15] Studies of its potential protective effects
against other sexually transmitted infections have been inconclusive. A 2010
review of literature worldwide found circumcisions performed by medical
providers to have a median complication rate of 1.5% for newborns and 6% for
older children, with few instances of severe complications. [16] Bleeding, infection
and the removal of either too much or too little foreskin are the most common
complications cited.[16][17] Circumcision does not appear to have a negative impact
on sexual function.[18]
About one-third of males worldwide are circumcised. [1][16] The procedure is most
prevalent in the Muslim world and Israel (where it is near-universal), the United
States and parts of Southeast Asia and Africa; it is relatively rare in Europe, Latin
America, parts of Southern Africa and most of Asia.[1] The origin of circumcision is
not known with certainty; the oldest documentary evidence for it comes from
ancient Egypt.[1] Various theories have been proposed as to its origin, including as a
religious sacrifice and as a rite of passage marking a boy's entrance into adulthood.
[19]
It is part of religious law in Judaism[20] and is an established practice in Islam,
Coptic Christianity and the Ethiopian Orthodox Church.[1][21][22]
Indications and contraindications
Routine or elective
Neonatal circumcision is often elected for non-medical reasons, such as for
religious beliefs or for personal preferences possibly driven by societal norms. [6]
Outside the parts of Africa with high prevalence of HIV/AIDS, the positions of the
world's major medical organizations on non-therapeutic neonatal circumcision
range from considering it as having a modest net health benefit that outweighs
small risks to viewing it as having no benefit with significant risks for harm. No
major medical organization recommends non-therapeutic neonatal circumcision,
and no major medical organization calls for banning it either. The Royal Dutch
Medical Association, which expresses the strongest opposition to routine neonatal
circumcision, does not call for the practice to be made illegal out of their concern
that parents who insist on the procedure would turn to poorly trained practitioners
instead of medical professionals. This argument to keep the procedure within the
purview of medical professionals is found across all major medical organizations.
In addition, the organizations advise medical professionals to yield to some degree
to parents' preferences, commonly based in cultural or religious views, in the
decision to agree to circumcise.[7]
Owing to the HIV/AIDS epidemic there, sub-Saharan Africa is a special case. The
finding that circumcision significantly reduces female-to-male HIV transmission
has prompted medical organizations serving the affected communities to promote
circumcision as an additional method of controlling the spread of HIV.[7] The
World Health Organization (WHO) and UNAIDS (2007) recommend
circumcision as part of a comprehensive program for prevention of HIV
transmission in areas with high endemic rates of HIV.[12]
Medical indications
Circumcision may be medically indicated in children for pathological phimosis,
refractory balanoposthitis and chronic, recurrent urinary tract infections (UTIs) in
males who are chronically susceptible to them.[2][6] The World Health
Organization promotes circumcision as a preventive measure for sexually
active men in populations at high risk for HIV.[12]
Contraindications
Circumcision is contraindicated in infants with certain genital structure
abnormalities, such as a misplaced urethral opening (as in hypospadias and
epispadias), curvature of the head of the penis (chordee), or ambiguous genitalia,
because the foreskin may be needed for reconstructive surgery. Circumcision is
contraindicated in premature infants and those who are not clinically stable and in
good health.[3][6][23] If an individual, child or adult, is known to have or has a family
history of serious bleeding disorders (hemophilia), it is recommended that the
blood be checked for normal coagulation properties before the procedure is
attempted.[6][23]
Technique
Circumcision surgery with hemostats and scissors
Before (left) and after (right) an adult circumcision, undertaken to treat
phimosis. The glans is exposed even when the penis is flaccid.
The foreskin extends out from the base of the glans and covers the glans when the
penis is flaccid. Proposed theories for the purpose of the foreskin are that it serves
to protect the penis as the fetus develops in the mother's womb, that it helps to
preserve moisture in the glans, or that it improves sexual pleasure. The foreskin
may also be a pathway of infection for certain diseases. Circumcision removes the
foreskin at its attachment to the base of the glans.[1]
Removal of the foreskin
For infant circumcision, devices such as the Gomco clamp, Plastibell and Mogen
clamp are commonly used in the USA.[5] These follow the same basic procedure.
First, the amount of foreskin to be removed is estimated. The practitioner opens the
foreskin via the preputial orifice to reveal the glans underneath and ensures it is
normal before bluntly separating the inner lining of the foreskin (preputial
epithelium) from its attachment to the glans. The practitioner then places the
circumcision device (this sometimes requires a dorsal slit), which remains until
blood flow has stopped. Finally, the foreskin is amputated.[5] For adults,
circumcision is often performed without clamps,[24] and non-surgical alternatives
such as the elastic ring controlled radial compression device are available.[25]
Pain management
The circumcision procedure causes pain, and for neonates this pain may interfere
with mother-infant interaction or cause other behavioral changes,[26] so the use of
analgesia is advocated.[5][27] Ordinary procedural pain may be managed in
pharmacological and non-pharmacological ways. Pharmacological methods, such
as localized or regional pain-blocking injections and topical analgesic creams, are
safe and effective.[5][28][29] The ring block and dorsal penile nerve block (DPNB)
are the most effective at reducing pain, and the ring block may be more effective
than the DPNB. They are more effective than EMLA (eutectic mixture of local
anesthetics) cream, which is more effective than a placebo.[28][29] Topical creams
have been found to irritate the skin of low birth weight infants, so penile nerve
block techniques are recommended in this group.[5]
For infants, non-pharmacological methods such as the use of a comfortable,
padded chair and a sucrose or non-sucrose pacifier are more effective at reducing
pain than a placebo,[29] but the American Academy of Pediatrics (AAP) states that
such methods are insufficient alone and should be used to supplement more
effective techniques.[5] A quicker procedure reduces duration of pain; use of the
Mogen clamp was found to result in a shorter procedure time and less pain-induced
stress than the use of the Gomco clamp or the Plastibell. [29] The available evidence
does not indicate that post-procedure pain management is needed.[5] For adults,
general anesthesia is an option,[30] and the procedure requires four to six weeks of
abstinence from masturbation or intercourse to allow the wound to heal.[23]
Effects
Sexually transmitted diseases
Human immunodeficiency virus
There is strong evidence that circumcision reduces the risk of HIV infection in
heterosexual men in high-risk populations.[10][31] Evidence among heterosexual men
in sub-Saharan Africa shows an absolute decrease in risk of 1.8% which is a
relative decrease of between 38 percent and 66 percent over two years,[10] and in
this population studies rate it cost effective.[11] Whether it is of benefit in developed
countries is undetermined.[32]
There are plausible explanations based on human biology for how circumcision
can decrease the likelihood of female-to-male HIV transmission. The superficial
skin layers of the penis contain Langerhans cells, which are targeted by HIV;
removing the foreskin reduces the number of these cells. When an uncircumcised
penis is erect during intercourse, any small tears on the inner surface of the
foreskin come into direct contact with the vaginal walls, providing a pathway for
transmission. When an uncircumcised penis is flaccid, the pocket between the
inside of the foreskin and the head of the penis provides an environment conducive
to pathogen survival; circumcision eliminates this pocket. Some experimental
evidence has been provided to support these theories.[33]
The WHO and the Joint United Nations Programme on HIV/AIDS (UNAIDS)
state that male circumcision is an efficacious intervention for HIV prevention, but
should be carried out by well-trained medical professionals and under conditions of
informed consent (parents' consent for their infant boys).[1][12][34] The WHO has
judged circumcision to be a cost-effective public health intervention against the
spread of HIV in Africa, although not necessarily more cost-effective than
condoms.[1] The Centers for Disease Control and Prevention (CDC) has calculated
that newborn circumcision is cost-effective against HIV in the US.[35] The joint
WHO/UNAIDS recommendation also notes that circumcision only provides partial
protection from HIV and should not replace known methods of HIV prevention.[12]
The available evidence does not indicate that circumcision provides HIV protection
for heterosexual women.[5][36] Data is lacking regarding the effect circumcision may
have on the transmission rate of men who engage in anal sex with a female partner.
[34][37]
It is undetermined whether circumcision benefits men who have sex with
[38][39]
men.
Human papillomavirus
Human papillomavirus (HPV) is the most commonly transmitted sexually
transmitted disease, affecting both men and women. While most infections are
asymptomatic and are cleared by the immune system, some types of the virus
cause genital warts, and other types, if untreated, cause various forms of cancer,
including cervical cancer and penile cancer. Genital warts and cervical cancer are
the two most common problems resulting from HPV.[40]
Circumcision is associated with a reduced prevalence of oncogenic types of
HPV infection, meaning that a randomly selected circumcised man is less likely to
be found infected with cancer-causing types of HPV than an uncircumcised man. [14]
It also decreases the likelihood of multiple infections.[41] No strong evidence
indicates that it reduces the rate of new HPV infection, [41][42][43] but the procedure is
associated with increased clearance of the virus by the body,[41][42] which can
account for the finding of reduced prevalence.[41]
Although genital warts are caused by a type of HPV, there is no statistically
significant relationship between being circumcised and the presence of genital
warts.[42][43]
Other infections
Studies evaluating the effect of circumcision on the incidence of other sexually
transmitted infections have reached conflicting conclusions. A 2006 meta-analysis
found that circumcision was associated with lower rates of syphilis, chancroid
and possibly genital herpes.[44] A 2010 review of clinical trial data found that
circumcision reduced the incidence of HSV-2 (herpes simplex virus, type 2)
infections by 28%. The researchers found mixed results for protection against
trichomonas vaginalis and chlamydia trachomatis and no evidence of protection
against gonorrhea or syphilis.[13] Among men who have sex with men, reviews have
found poor evidence for protection against sexually transmitted infections other
than HIV,[38][45] with the possible exception of syphilis.[38]
Phimosis, balanitis and balanoposthitis
Phimosis is the inability to retract the foreskin over the glans penis. At birth, the
foreskin cannot be retracted due to adhesions between the foreskin and glans, and
this is considered normal (physiological phimosis). Over time, the foreskin
naturally separates from the glans, and a majority of boys are able to retract the
foreskin by age four. If the inability to do so becomes problematic (pathological
phimosis), which is commonly due to the skin disease balanitis xerotica obliterans
(BXO), circumcision is the preferred treatment option. [2][46] The procedure may also
be used prophylactically to prevent the development of phimosis.[6]
An inflammation of the glans penis and foreskin is called balanoposthitis; that
affecting the glans alone is called balanitis. [47][48] Most cases of these conditions
occur in uncircumcised males,[49] affecting 411% of that group.[50] The moist,
warm space underneath the foreskin is thought to facilitate the growth of
pathogens, particularly when hygiene is poor. Yeasts, especially Candida albicans,
are the most common penile infection and are rarely identified in samples taken
from circumcised males.[49] Both conditions are usually treated with topical
antibiotics (metronidazole cream) and antifungals (clotrimazole cream) or lowpotency steroid creams.[47][48] Circumcision is a treatment option for refractory or
recurrent balanoposthitis, but in recent years the availability of these other
treatments have made it less necessary.[47][48]
Urinary tract infections
A UTI affects parts of the urinary system including the urethra, bladder, and
kidneys. There is about a 1% risk of UTIs in boys under two years of age, and the
majority of incidents occur in the first year of life. There is good but not ideal
evidence that circumcision reduces the incidence of UTIs in boys under two years
of age, and there is fair evidence that the reduction in incidence is by a factor of 3
10 times,[5][51] but prevention of UTIs does not justify routine use of the procedure.
[2]
Circumcision is most likely to benefit boys who have a high risk of UTIs due to
anatomical defects,[5][51] and may be used to treat recurrent UTIs.[2]
There is a plausible biological explanation for the reduction in UTI risk after
circumcision. The orifice through which urine passes at the tip of the penis (the
urinary meatus) hosts more urinary system disease-causing bacteria in
uncircumcised boys than in circumcised boys, especially in those under six months
of age. As these bacteria are a risk factor for UTIs, circumcision may reduce the
risk of UTIs through a decrease in the bacteria population.[5][52]
Cancers
Circumcision has a protective effect against the risks of penile cancer in men, and
cervical cancer in the female sexual partners of heterosexual men. Penile cancer is
rare, with about 1 new case per 100,000 people per year in developed countries,
and higher incidence rates per 100,000 in sub-Saharan Africa (for example, 1.6 in
Zimbabwe, 2.7 in Uganda and 3.2 in Swaziland).[53] Penile cancer development can
be detected in the carcinoma in situ (CIS) cancerous precursor stage and at the
more advanced invasive squamous cell carcinoma stage. [5] Childhood or adolescent
circumcision is associated with a reduced risk of invasive squamous cell carcinoma
in particular.[5][53] There is an association between adult circumcision and an
increased risk of invasive penile cancer; this is believed to be from men being
circumcised as a treatment for penile cancer or a condition that is a precursor to
cancer rather than a consequence of circumcision itself.[53] Penile cancer has been
observed to be nearly eliminated in populations of males circumcised neonatally.[50]
Important risk factors for penile cancer include phimosis and HPV infection, both
of which are mitigated by circumcision.[53] The mitigating effect circumcision has
on the risk factor introduced by the possibility of phimosis is secondary, in that the
removal of the foreskin eliminates the possibility of phimosis. This can be inferred
from study results that show uncircumcised men with no history of phimosis are
equally likely to have penile cancer as circumcised men.[5][53] Circumcision is also
associated with a reduced prevalence of cancer-causing types of HPV in men [41]
and a reduced risk of cervical cancer (which is caused by a type of HPV) in female
partners of men.[6] Because penile cancer is rare (and may get more rare with
increasing HPV vaccination rates), and circumcision has risks, the practice is not
considered to be valuable solely as a prophylactic measure against penile cancer
in the United States.[5][15][50]
Adverse effects
Neonatal circumcision is generally safe when done by an experienced practitioner.
[54]
The most common acute complications are bleeding, infection and the
removal of either too much or too little foreskin.[5][17] These complications occur
in less than 1% of procedures, and constitute the vast majority of all acute
circumcision complications in the United States. [17] Minor complications are
reported to occur in 3% of procedures. [54] A specific complication rate is difficult to
determine due to scant data on complications and inconsistencies in their
classification.[5] Complication rates are greater when the procedure is performed by
an inexperienced operator, in unsterile conditions, or when the child is at an older
age.[16] Significant acute complications happen rarely,[5][16] occurring in about 1 in
500 newborn procedures in the United States. [5] Severe to catastrophic
complications are sufficiently rare that they are reported only as individual case
reports.[5] The death rate due to circumcision is estimated at 1 in every 500,000
neonatal procedures conducted within the United States.[17] Other possible
complications include concealed penis, skin bridges, urethral fistulas, and
meatal stenosis.[55] These complications may be avoided with proper technique,
and are most often treatable without requiring a hospital visit.[55]
10
Circumcision does not appear to decrease the sensitivity of the penis, harm sexual
function or reduce sexual satisfaction.[18][56] The Royal Dutch Medical Association's
2010 Viewpoint mentions that "complications in the area of sexuality" have been
reported.[57] Additionally, the procedure may carry the risks of heightened pain
response for newborns and dissatisfaction with the result.[26]
Prevalence
Prevalence of circumcision by country
Circumcision is probably the world's most widely performed procedure. [58]
Approximately one-third of males worldwide are circumcised, most often for
reasons other than medical indication.[1][16] It is commonly practiced between
infancy and the early twenties.[1] The WHO estimated in 2007 that 664,500,000
males aged 15 and over were circumcised (30% global prevalence), almost 70% of
whom were Muslim.[1] Circumcision is most prevalent in the Muslim world, Israel,
South Korea, the United States and parts of Southeast Asia and Africa. It is
relatively rare in Europe, Latin America, parts of Southern Africa and Oceania and
most of Asia. Prevalence is near-universal in the Middle East and Central Asia. [1][59]
Non-religious circumcision in Asia, outside of the Republic of Korea and the
Philippines, is fairly rare,[1] and prevalence is generally low (less than 20%) across
Europe.[1][60] Estimates for individual countries include Taiwan at 9% [61] and
Australia 58.7%.[62] Prevalence in the United States and Canada is estimated at
11
75% and 30% respectively.[1] Prevalence in Africa varies from less than 20% in
some southern African countries to near universal in North and West Africa.[59]
The rates of routine neonatal circumcision over time have varied significantly by
country. In the United States, hospital discharge surveys estimated rates at 64.7%
in the year 1980, 59.0% in the year 1990, 62.4% in the year 2000, and 58.3% in the
year 2010.[63] These estimates are lower than the overall rates, as they do not
account for non-hospital circumcisions,[63] or for procedures performed for medical
need;[1][63] community surveys have reported higher neonatal prevalence. [1] Canada
has seen a slow decline since the early 1970s, possibly influenced by statements
from the AAP and the Canadian Pediatric Society issued in the 1970s saying that
the procedure was not medically indicated.[1] In Australia, the rate declined in the
1970s and 80s, but has been increasing slowly as of 2004. [1] In the United
Kingdom, prevalence was roughly 25% in the 1940s, but declined dramatically
after the National Health Service (NHS) did not cover the costs of the procedure.[1]
The prevalence in South Korea has increased markedly in the second half of the
20th century, rising from near zero around 1950 to about 60% in 2000, with the
most significant jumps in the last two decades of that time period. [1] This is
probably due to the influence of the United States, which established a trusteeship
for the country following World War II.[1]
Medical organizations can affect the neonatal circumcision rate of a country by
influencing whether the costs of the procedure are borne by the parents or are
covered by insurance or a national health care system. Policies that require the
costs to be paid by the parents yield lower neonatal circumcision rates. The decline
in the rates in the UK is one example; another is that in the United States, the
individual states where insurance or Medicaid covers the costs have higher rates.
Changes to policy are driven by the results of new research, and moderated by the
politics, demographics, and culture of the communities.[7]
History
Circumcision is the world's oldest planned surgical procedure, suggested by
anatomist and hyperdiffusionist historian Grafton Elliot Smith to be over 15,000
years old, pre-dating recorded history. There is no firm consensus as to how it
came to be practiced worldwide. One theory is that it began in one geographic area
and spread from there; another is that several different cultural groups began its
practice independently. In his 1891 work History of Circumcision, physician Peter
Charles Remondino suggested that it began as a less severe form of emasculating a
captured enemy: penectomy or castration would likely have been fatal, while some
12
form of circumcision would permanently mark the defeated yet leave him alive to
serve as a slave.[19][64]
The history of the migration and evolution of the practice of circumcision is
followed mainly through the cultures and peoples in two separate regions. In the
lands south and east of the Mediterranean, starting with Sudan and Ethiopia, the
procedure was practiced by the ancient Egyptians and the Semites, and then by the
Jews and Muslims, with whom the practice traveled to and was adopted by the
Bantu Africans. In Oceania, circumcision is practiced by the Australian Aborigines
and Polynesians.[64] There is also evidence that circumcision was practiced among
the Aztec and Mayan civilizations in the Americas,[1] but little detail is available
about its history.[19][58]
Middle East, Africa and Europe
Evidence suggests that circumcision was practiced in the Arabian Peninsula by the
4th millennium BCE, when the Sumerians and the Semites moved into the area
that is modern-day Iraq.[58] The earliest historical record of circumcision comes
from Egypt, in the form of an image of the circumcision of an adult carved into the
tomb of Ankh-Mahor at Saqqara, dating to about 24002300 BCE. Circumcision
was done by the Egyptians possibly for hygienic reasons, but also was part of their
obsession with purity and was associated with spiritual and intellectual
development. No well-accepted theory explains the significance of circumcision to
the Egyptians, but it appears to have been endowed with great honor and
importance as a rite of passage into adulthood, performed in a public ceremony
emphasizing the continuation of family generations and fertility. It may have been
a mark of distinction for the elite: the Egyptian Book of the Dead describes the sun
god Ra as having circumcised himself.[19][64]
Circumcision features prominently in the Hebrew Bible. The narrative in Genesis
chapter 17 describes the circumcision of Abraham and his relatives and slaves,
making him the first named individual to undergo the procedure. In the same
chapter, Abraham's descendants are commanded to circumcise their sons on the
eighth day of life. Many generations later, Moses was raised by the Egyptian elite,
so circumcision was doubtless familiar to him. For the Jews of the time,
circumcision was not as much a spiritual act as it was a physical sign of their
covenant with God, and a prerequisite for the fulfillment of the commandment to
produce offspring. In addition to proposing that circumcision was taken up by the
Jews purely as a religious mandate, scholars have suggested that Judaism's
patriarchs and their followers adopted circumcision to make penile hygiene easier
13
in hot, sandy climates; as a rite of passage into adulthood; or as a form of blood
sacrifice.[58][64][65]
Alexander the Great conquered the Middle East in the 4th century BCE, and in the
following centuries ancient Greek cultures and values came to the Middle East.
The Greeks abhorred circumcision, making life for circumcised Jews living among
the Greeks (and later the Romans) very difficult. Antiochus Epiphanes outlawed
circumcision, as did Hadrian, which helped cause the Bar Kokhba revolt. During
this period in history, Jewish circumcision called for the removal of only a part of
the prepuce, and some Hellenized Jews attempted to look uncircumcised by
stretching the extant parts of their foreskins. This was considered by the Jewish
leaders to be a serious problem, and during the 2nd century CE they changed the
requirements of Jewish circumcision to call for the complete removal of the
foreskin, emphasizing the Jewish view of circumcision as intended to be not just
the fulfillment of a Biblical commandment but also an essential and permanent
mark of membership in a people.[64][65]
Keks dancing at the circumcision celebration of Sultan Ahmed III's sons
(1720); miniature from the Surname-i Vehbi, Topkap Palace, Istanbul
A narrative in the Christian Gospel of Luke makes a brief mention of the
circumcision of Jesus, but the subject of physical circumcision itself is not part of
the received teachings of Jesus. Paul the Apostle reinterpreted circumcision as a
spiritual concept, arguing the physical one to be no longer necessary. The teaching
that physical circumcision was unnecessary for membership in a divine covenant
was instrumental in the separation of Christianity from Judaism. Although it is not
explicitly mentioned in the Quran (early 6th century CE), circumcision is
considered essential to Islam, and it is nearly universally performed among
Muslims. The practice of circumcision spread across the Middle East, North Africa
and Southern Europe with Islam.[66]
14
Circumcision knife from the Congo; wood, iron; late 19th/early 20th century
The practice of circumcision is thought to have been brought to the Bantu-speaking
tribes of Africa by either the Jews after one of their many expulsions from
European countries, or by Muslim Moors escaping after the 1492 conquest of
Spain. In the second half of the 1st millennium CE, inhabitants from the North East
of Africa moved south and encountered groups from Arabia, the Middle East and
West Africa. These people moved south and formed what is known today as the
Bantu. Bantu tribes were observed to be upholding what was described as Jewish
law, including circumcision, in the 16th century. Circumcision and elements of
Jewish dietary restrictions are still found among Bantu tribes.[58]
Indigenous peoples of Australia, the Pacific and Americas
Circumcision is practised by some groups amongst Australian Aboriginal peoples,
Polynesians, and Native Americans. Little information is available about the
origins and history of circumcision among these peoples, compared to
circumcision in the Middle East.
For Aboriginal Australians and Polynesians, circumcision likely started as a blood
sacrifice and a test of bravery, and became an initiation rite with attendant
instruction in manhood in more recent centuries. Often seashells were used to
remove the foreskin, and the bleeding was stopped with eucalyptus smoke.[58][67]
Christopher Columbus reported circumcision being practiced by native Americans.
[citation needed]
It was also practiced by the Incas, Aztecs and Mayans. It probably
started among South American tribes as a blood sacrifice or ritual mutilation to test
bravery and endurance, and its use later evolved into a rite of initiation.[58]
Modern times
15
Circumcision did not become a common medical procedure until the late 19th
century.[68] At that time, British and American doctors began recommending it
primarily as a deterrent to masturbation.[68][69] Prior to the 20th century,
masturbation was believed to be the cause of a wide range of physical and mental
illnesses including epilepsy, paralysis, impotence, gonorrhea, tuberculosis,
feeblemindedness, and insanity.[70][71]
One of the first modern physicians to advocate the procedure was Lewis Sayre, a
founder of the American Medical Association. In 1870, Sayre began using
circumcision as a purported cure for several cases of young boys presenting with
paralysis or significant motor problems. He thought the procedure ameliorated
such problems based on a "reflex neurosis" theory of disease, which held that
excessive stimulation of the genitals was a disturbance to the equilibrium of the
nervous system and a cause of systemic problems. [68] The use of circumcision to
promote good health also fit in with the germ theory of disease, which saw
validation during the same time period: the foreskin was seen as harboring
infection-causing smegma (a mixture of shed skin cells and oils). Sayre published
works on the subject and promoted it energetically in speeches. Contemporary
physicians picked up on Sayre's new treatment, which they believed could prevent
or cure a wide-ranging array of medical problems and social ills. Its popularity
spread with publications such as Peter Charles Remondino's History of
Circumcision. By the turn of the century, in both America and Great Britain, infant
circumcision was nearly universally recommended.[19][72]
After the end of World War II, Britain moved to a nationalized health care system,
and so looked to ensure that each medical procedure covered by the new system
was cost-effective. Douglas Gairdner's 1949 article "The Fate of the Foreskin"
argued persuasively that the evidence available at that time showed that the risks
outweighed the known benefits. The procedure was not covered by the national
health care system, and circumcision rates dropped in Britain and in the rest of
Europe. In the 1970s, national medical associations in Australia and Canada issued
recommendations against routine infant circumcision, leading to drops in the rates
of both of those countries. In the United States, the American Academy of
Pediatrics has, over the decades, issued a series of policy statements regarding
circumcision, sometimes positive and sometimes negative.[19][72]
An association between circumcision and reduced heterosexual HIV infection rates
was suggested in 1986.[19] Experimental evidence was needed to establish a causal
relationship, so three randomized controlled trials were commissioned as a means
to reduce the effect of any confounding factors.[73] Trials took place in South
16
Africa, Kenya and Uganda.[10] All three trials were stopped early by their
monitoring boards on ethical grounds, because those in the circumcised group had
a lower rate of HIV contraction than the control group. [10] Subsequently, the World
Health Organization promoted circumcision in high-risk populations as part of an
overall program to reduce the spread of HIV,[12] although some have challenged the
validity of the African randomized controlled trials, prompting a number of
researchers to question the effectiveness of circumcision as an HIV prevention
strategy.[74][75][76][77] The Male Circumcision Clearinghouse website was formed by
WHO, UNAIDS, FHI and AVAC to provide current evidence-based guidance,
information and resources to support the delivery of safe male circumcision
services in countries that choose to scale up the procedure as one component of
comprehensive HIV prevention services.[78][79]
Society and culture
Cultures and religions
In some cultures, males must be circumcised shortly after birth, during childhood
or around puberty as part of a rite of passage. Circumcision is commonly practiced
in the Jewish and Islamic faiths.
Judaism
Preparing for a Jewish ritual circumcision with a Mogen shield
(on the table, next to the scalpel)
Circumcision is very important to Judaism, with over 90% of adherents having the
procedure performed as a religious obligation. The basis for its observance is found
in the Torah of the Hebrew Bible, in Genesis chapter 17, in which a covenant of
circumcision is made with Abraham and his descendants. Jewish circumcision is
part of the brit milah ritual, to be performed by a specialist ritual circumciser (a
17
mohel) on the eighth day of a newborn son's life (with certain exceptions for poor
health). Jewish law requires that the circumcision leave the glans bare when the
penis is flaccid. Converts to Judaism must also be circumcised; those who are
already circumcised undergo a symbolic circumcision ritual. Circumcision is not
required by Judaism for one to be considered Jewish, but adherents foresee serious
negative spiritual consequences if it is neglected.[20][80]
Islam
Children in Turkey wearing traditional circumcision costumes
Although there is some debate within Islam over whether it is a religious
requirement, circumcision (called khitan) is practiced nearly universally by
Muslim males. Islam bases its practice of circumcision on the Genesis 17 narrative,
the same Biblical chapter referred to by Jews. The procedure is not explicitly
mentioned in the Quran, however it is a tradition established by Islam's prophet
Muhammad directly (following Abraham), and so its practice is considered a
sunnah (prophet's tradition) and is very important in Islam. For Muslims,
circumcision is also a matter of cleanliness, purification and control over one's
baser self (nafs). There is no agreement across the many Islamic communities
about the age at which circumcision should be performed. It may be done from
soon after birth up to about age 15; most often it is performed at around six to
seven years of age. The timing can correspond with the boy's completion of his
recitation of the whole Quran, with a coming-of-age event such as taking on the
responsibility of daily prayer or betrothal. Circumcision may be celebrated with an
associated family or community event. Circumcision is recommended for, but is
not required of, converts to Islam.[22][81][82]
Christianity
18
The New Testament chapter Acts 15 records that Christianity does not require
circumcision. Christianity does not forbid it either; the Gospel of Luke mentions
that Jesus himself was circumcised.[83] In 1442, the leadership of the Catholic
Church declared that circumcision was not necessary.[84] Coptic Christians practice
circumcision as a rite of passage.[1][21][85][86] The Ethiopian Orthodox Church calls
for circumcision, with near-universal prevalence among Orthodox men in Ethiopia.
[1]
In South Africa, some Christian churches disapprove of the practice, while
others require it of their members.[1]
African cultures
Certain African cultural groups, such as the Yoruba and Igbo of Nigeria,
customarily circumcise their infant sons. The procedure is also practiced by some
cultural groups or individual family lines in the Sudan, Zaire, Uganda and in
southern Africa. For some of these groups, circumcision appears to be purely
cultural, done with no particular religious significance or intention to distinguish
members of a group. For others, circumcision might be done for purification, or it
may be interpreted as a mark of subjugation. Among these groups, even when
circumcision is done for reasons of tradition, it is often done in hospitals.[87]
Australian cultures
Some Australian Aborigines use circumcision as a test of bravery and self-control
as a part of a rite of passage into manhood, which results in full societal and
ceremonial membership. It may be accompanied by body scarification and the
removal of teeth, and may be followed later by penile subincision. Circumcision is
one of many trials and ceremonies required before a youth is considered to have
become knowledgeable enough to maintain and pass on the cultural traditions.
During these trials, the maturing youth bonds in solidarity with the men.
Circumcision is also strongly associated with a man's family, and it is part of the
process required to prepare a man to take a wife and produce his own family.[87]
Ethical and legal issues
19
A protest against infant circumcision
There is a long-running and vigorous debate over ethical concerns regarding
circumcision, particularly neonatal circumcision for reasons other than intended
direct medical benefit. There are three parties involved in the decision to
circumcise a minor: the minor as the patient, the parents (or other guardians) and
the physician. The physician is bound under the ethical principles of beneficence
(promoting well-being) and non-maleficence ("first, do no harm"), and so is
charged with the responsibility to promote the best interests of the patient while
minimizing unnecessary harms. Those involved must weigh the factors of what is
in the best interest of the minor against the potential harms of the procedure.[8]
With a newborn involved, the decision is made more complex due to the principles
of respect for autonomy and consent, as a newborn cannot understand or engage in
a logical discussion of his own values and best interests. [8][9] A mentally more
mature child can understand the issues involved to some degree, and the physician
and parents may elicit input from the child and weigh it appropriately in the
decision-making process, although the law may not treat such input as legally
informative. Ethicists and legal theorists also state that it is questionable for parents
to make a decision for the child that precludes the child from making a different
decision for himself later. Such a question can be raised for the decision by the
parents either to circumcise or not to circumcise the child.[8]
Generally, circumcision on a minor is not ethically controversial or legally
questionable when there is a clear and pressing medical indication for which it is
the accepted best practice to resolve. Where circumcision is the chosen
intervention, the physician has an ethical responsibility to ensure the procedure is
performed competently and safely to minimize potential harms. [8][9] Worldwide,
most legal jurisdictions do not have specific laws concerning the circumcision of
20
males,[1] but infant circumcision is considered legal under the existing laws in
countries such as Australia, Canada, New Zealand, the UK and the US. [88] A few
countries have passed legislation on the procedure: Germany allows nontherapeutic circumcision under certain conditions,[89] while non-religious routine
circumcision is illegal in South Africa and Sweden.[1][88]
Societally, circumcision is often considered for reasons other than medical need.
Public health advocates of circumcision consider it to be a net benefit overall, and
therefore feel increasing the circumcision rate to be an ethical imperative. They
recommend performing the procedure during the neonatal period, when it is less
expensive and has a lower risk of complications. [9] While studies show there is a
modest epidemiological benefit to circumcision, critics argue that the number of
circumcisions that would have be performed would yield an overall negative public
health outcome due to the resulting number of complications or other negative
effects (such as pain). Pinto (2012) writes "sober proponents and detractors of
circumcision agree that there is no overwhelming medical evidence to support
either side."[9] This type of cost-benefit analysis is highly dependent on the kinds
and frequencies of health problems in the population under discussion and how
circumcision affects those health problems.[8]
Parents are assumed to have the child's best interests in mind. Ethically, it is
imperative that the medical practitioner inform the parents about the benefits and
risks of the procedure and obtain informed consent before performing it.
Practically, however, many parents come to a decision about circumcising the child
before he is born, and a discussion of the benefits and risks of the procedure with a
physician has not been shown to have a significant effect on the decision. Some
parents request to have their newborn or older child circumcised for nontherapeutic reasons, such as the parents' desires to adhere to family tradition,
cultural norms or religious beliefs. In considering such a request, the physician
may consider (in addition to any potential medical benefits and harms) such nonmedical factors in determining the child's best interests and may ethically perform
the procedure. Equally, without a clear medical benefit relative to the potential
harms, a physician may take the ethical position that non-medical factors do not
contribute enough as benefits to outweigh the potential harms and refuse to
perform the procedure. Medical organization such as the British Medical
Association state that their member physicians are not obliged to perform the
procedure in such situations.[8][9]
Economic considerations
21
The cost-effectiveness of circumcision has been studied to determine whether a
policy of circumcising all newborns or a policy of promoting and providing
inexpensive or free access to circumcision for all adult men who choose it would
result in lower overall societal healthcare costs. As HIV/AIDS is an incurable
disease that is expensive to manage, significant effort has been spent studying the
cost-effectiveness of circumcision to reduce its spread in parts of Africa that have a
relatively high infection rate and low circumcision prevalence. [90] Several analyses
have concluded that circumcision programs for adult men in Africa are costeffective and in some cases are cost-saving. [11] In Rwanda, circumcision has been
found to be cost-effective across a wide range of age groups from newborn to
adult,[43][91] with the greatest savings achieved when the procedure is performed in
the newborn period due to the lower cost per procedure and greater timeframe for
HIV infection protection.[32][91] Circumcision for the prevention of HIV
transmission in adults has also been found to be cost-effective in South Africa,
Kenya and Uganda, with cost savings estimated in the billions of US dollars over
20 years.[90] Hankins et al. (2011) estimated that a $1.5 billion investment in
circumcision for adults in 13 high-priority African countries would yield $16.5
billion in savings.[92]
The overall cost-effectiveness of neonatal circumcision has also been studied in the
United States, which has a significantly different cost setting from Africa in areas
such as public health infrastructure, availability of medications, and medical
technology and the willingness to use it. [93] A study by the CDC suggests that
newborn circumcision would be societally cost-effective in the United States based
on circumcision's efficacy against the heterosexual transmission of HIV alone,
without considering any other cost benefits.[5] The American Academy of Pediatrics
(2012) recommends that neonatal circumcision in the United States be covered by
third-party payers such as Medicaid and insurance.[5] A Johns Hopkins study (2012)
that considered reported benefits of circumcision such as reduced risks from HIV,
HPV, HSV-2 and UTIs calculated that if the circumcision rate in the United States
were to drop from 55% to 10% (the rate in Europe), it would "increase lifetime
health care costs by $407 per male and $43 per female." [94] The cost of the
procedure is more expensive for an older male than a newborn.[95]
References
1.
"Male circumcision: Global trends and determinants of prevalence,
safety and acceptability" (PDF). World Health Organization. 2007.
22
2.
Lissauer T, Clayden G (October 2011). Illustrated Textbook of
Paediatrics, Fourth edition. Elsevier. pp. 352353. ISBN 978-0-7234-35655.
3.
Rudolph C, Rudolph A, Lister G, First L, Gershon A (18 March 2011).
Rudolph's Pediatrics, 22nd Edition. McGraw-Hill Companies, Incorporated.
p. 188. ISBN 978-0-07-149723-7.
4.
Sawyer S (November 2011). Pediatric Physical Examination &
Health Assessment. Jones & Bartlett Publishers. pp. 555556. ISBN 978-14496-7600-1.
5.
American Academy of Pediatrics Task Force on Circumcision (2012).
"Technical Report". Pediatrics 130 (3): e756e785. doi:10.1542/peds.20121990. ISSN 0031-4005. PMID 22926175.
6.
Hay W, Levin M (25 June 2012). Current Diagnosis and Treatment
Pediatrics 21/E. McGraw Hill Professional. pp. 1819. ISBN 978-0-07177971-5.
7.
Jacobs, Micah; Grady, Richard; Bolnick, David A. (2012). "Current
Circumcision Trends and Guidelines". In Bolnick, David A.; Koyle, Martin;
Yosha, Assaf. Surgical Guide to Circumcision. London: Springer. pp. 38.
doi:10.1007/978-1-4471-2858-8_1. ISBN 978-1-4471-2857-1. Retrieved
April 6, 2014. (subscription required (help)).
8.
Caga-anan EC, Thomas AJ, Diekema DS, Mercurio MR, Adam MR (8
September 2011). Clinical Ethics in Pediatrics: A Case-Based Textbook.
Cambridge University Press. p. 43. ISBN 978-0-521-17361-2.
9.
Pinto K (August 2012). "Circumcision controversies". Pediatric
clinics of North America 59 (4): 977986. doi:10.1016/j.pcl.2012.05.015.
PMID 22857844.
10.
Siegfried N, Muller M, Deeks JJ, Volmink J (2009). "Male
circumcision for prevention of heterosexual acquisition of HIV in men". In
Siegfried, Nandi. Cochrane Database of Systematic Reviews (2): CD003362.
doi:10.1002/14651858.CD003362.pub2. PMID 19370585.
11.
Uthman OA, Popoola TA, Uthman MM, Aremu O (2010). "Economic
evaluations of adult male circumcision for prevention of heterosexual
23
acquisition of HIV in men in sub-Saharan Africa: a systematic review". In
Van
Baal,
Pieter
H.
M.
PLoS
ONE
5
(3):
e9628.
doi:10.1371/journal.pone.0009628. PMC 2835757. PMID 20224784.
12.
"WHO and UNAIDS announce recommendations from expert
consultation on male circumcision for HIV prevention". World Health
Organization. March 2007.
13.
Wetmore CM, Manhart LE, Wasserheit JN (April 2010). "Randomized
controlled trials of interventions to prevent sexually transmitted infections:
learning from the past to plan for the future". Epidemiol Rev 32 (1): 12136.
doi:10.1093/epirev/mxq010. PMC 2912604. PMID 20519264.
14.
See: Larke et al. "Male circumcision and human papillomavirus
infection in men: a systematic review and meta-analysis" (2011), Albero et
al. "Male Circumcision and Genital Human Papillomavirus: A Systematic
Review and Meta-Analysis" (2012), Rehmeyer "Male Circumcision and
Human Papillomavirus Studies Reviewed by Infection Stage and Virus
Type" (2011).
15.
"Can penile cancer be prevented?". Learn About Cancer: Penile
Cancer: Detailed Guide. American Cancer Society. Retrieved 2012-10-25.
16.
Weiss HA, Larke N, Halperin D, Schenker I (2010). "Complications
of circumcision in male neonates, infants and children: a systematic review".
BMC Urol 10: 2. doi:10.1186/1471-2490-10-2. PMC 2835667.
PMID 20158883.
17.
"Circumcision: Position Paper on Neonatal Circumcision". American
Academy of Family Physicians. 2007. Retrieved 2007-01-30.
18.
The American Academy of Pediatrics Task Force on Circumcision
"Technical Report" (2012) addresses sexual function, sensitivity and
satisfaction without qualification by age of circumcision. Sadeghi-Nejad et
al. "Sexually transmitted diseases and sexual function" (2010) addresses
adult circumcision and sexual function. Doyle et al. "The Impact of Male
Circumcision on HIV Transmission" (2010) addresses adult circumcision
and sexual function. Perera et al. "Safety and efficacy of nontherapeutic
male circumcision: a systematic review" (2010) addresses adult circumcision
and sexual function and satisfaction.
24
19.
Alanis MC, Lucidi RS (May 2004). "Neonatal circumcision: a review
of the world's oldest and most controversial operation". Obstet Gynecol Surv
59 (5): 37995. doi:10.1097/00006254-200405000-00026. PMID 15097799.
20.
Glass JM (January 1999). "Religious circumcision: a Jewish view".
BJUI. 83 Suppl 1: 1721. doi:10.1046/j.1464-410x.1999.0830s1017.x.
PMID 10349410.
21.
"Circumcision". Columbia Encyclopedia. Columbia University Press.
2011.
22.
Clark M (10 March 2011). Islam For Dummies. John Wiley & Sons.
p. 170. ISBN 978-1-118-05396-6.
23.
"Manual for male circumcision under local anaesthesia". World
Health Organization. December 2009.
24.
McClung, Chris; Voelzke, Bryan (2012). "Adult Circumcision". In
Bolnick, David A.; Koyle, Martin; Yosha, Assaf. Surgical Guide to
Circumcision. London: Springer. pp. 165175. doi:10.1007/978-1-44712858-8_14. ISBN 978-1-4471-2857-1. Retrieved April 6, 2014.
(subscription required (help)).
25.
Use of devices for adult male circumcision in public health HIV
prevention programmes: Conclusions of the Technical Advisory Group on
Innovations in Male Circumcision (PDF). World Health Organization. 2012.
26.
Perera CL, Bridgewater FH, Thavaneswaran P, Maddern GJ (2010).
"Safety and efficacy of nontherapeutic male circumcision: a systematic
review". Annals of Family Medicine 8 (1): 6472. doi:10.1370/afm.1073.
PMC 2807391. PMID 20065281.
27.
Professional Standards and Guidelines Circumcision (Infant Male)
(PDF). College of Physicians and Surgeons of British Columbia. September
2009. Retrieved 2012-09-11.
28.
Lonnqvist P (Sep 2010). "Regional anaesthesia and analgesia in the
neonate". Best Pract Res Clin Anaesthesiol 24 (3): 30921.
doi:10.1016/j.bpa.2010.02.012. PMID 21033009.
25
29.
Shockley RA, Rickett K (April 2011). "Clinical inquiries. What's the
best way to control circumcision pain in newborns?". J Fam Pract 60 (4):
233ab. PMID 21472156.
30.
Wolter C, Dmochowski R (2008). "Circumcision". Handbook of
Office Urological Procedures. Springer. pp. 88. ISBN 978-1-84628-523-3.
31.
Krieger JN (May 2011). "Male circumcision and HIV infection risk".
World Journal of Urology 30 (1): 313. doi:10.1007/s00345-011-0696-x.
PMID 21590467.
32.
Kim H, Li PS, Goldstein M, Howard H; Li, Philip S; Goldstein, Marc
(November 2010). "Male circumcision: Africa and beyond?". Current
Opinion in Urology 20 (6): 5159. doi:10.1097/MOU.0b013e32833f1b21.
PMID 20844437.
33.
Weiss HA, Dickson KE, Agot K, Hankins CA (2010). "Male
circumcision for HIV prevention: current research and programmatic
issues".
AIDS.
24
Suppl
4:
S619.
doi:10.1097/01.aids.0000390708.66136.f4. PMID 21042054.
34.
"New Data on Male Circumcision and HIV Prevention: Policy and
Programme Implications" (PDF). World Health Organization. March 28,
2007.
35.
Sansom SL, Prabhu VS, Hutchinson AB, et al. (2010). "Costeffectiveness of newborn circumcision in reducing lifetime HIV risk among
U.S. males". In Kissinger, Patricia. PLoS ONE 5 (1): e8723.
doi:10.1371/journal.pone.0008723. PMC 2807456. PMID 20090910.
36.
Dinh MH; Fahrbach KM; Hope TJ (March 2011). "The role of the
foreskin in male circumcision: an evidence-based review". Am J Reprod
Immunol. doi:10.1111/j.1600-0897.2010.00934.x. PMID 21114567.
37.
"Male Circumcision and Risk for HIV Transmission and Other Health
Conditions: Implications for the United States". Centers for Disease Control
and Prevention. 7 February 2008. Retrieved 15 July 2011.
38.
Templeton DJ, Millett GA, Grulich AE (February 2010). "Male
circumcision to reduce the risk of HIV and sexually transmitted infections
among men who have sex with men". Current Opinion in Infectious
26
Diseases
23
(1):
PMID 19935420.
4552.
doi:10.1097/QCO.0b013e328334e54d.
39.
Wiysonge CS, Kongnyuy EJ, Shey M, et al. (2011). "Male
circumcision for prevention of homosexual acquisition of HIV in men". In
Wiysonge, Charles Shey. Cochrane Database of Systematic Reviews (6):
CD007496. doi:10.1002/14651858.CD007496.pub2. PMID 21678366.
40.
"STD facts Human papillomavirus (HPV)". CDC. Retrieved
September 12, 2012.
41.
Rehmeyer C, CJ (2011). "Male Circumcision and Human
Papillomavirus Studies Reviewed by Infection Stage and Virus Type". J Am
Osteopathy Assoc 111 (3 suppl 2): S11S18. PMID 21415373.
42.
Larke N, Thomas SL, Dos Santos Silva I, Weiss HA (November
2011). "Male circumcision and human papillomavirus infection in men: a
systematic review and meta-analysis". J. Infect. Dis. 204 (9): 137590.
doi:10.1093/infdis/jir523. PMID 21965090.
43.
Albero G, Castellsagu X, Giuliano AR, Bosch FX (February 2012).
"Male Circumcision and Genital Human Papillomavirus: A Systematic
Review and Meta-Analysis". Sex Transm Dis 39 (2): 104113.
doi:10.1097/OLQ.0b013e3182387abd. PMID 22249298.
44.
Weiss HA, Thomas SL, Munabi SK, Hayes RJ (April 2006). "Male
circumcision and risk of syphilis, chancroid, and genital herpes: a systematic
review and metaanalysis". Sexually Transmitted Infections 82 (2): 1019;
discussion
110.
doi:10.1136/sti.2005.017442.
PMC 2653870.
PMID 16581731.
45.
Millett GA, Flores SA, Marks G, Reed JB, Herbst JH (October 2008).
"Circumcision status and risk of HIV and sexually transmitted infections
among men who have sex with men: a meta-analysis". JAMA 300 (14):
167484. doi:10.1001/jama.300.14.1674. PMID 18840841.
46.
Becker K (January 2011). "Lichen sclerosus in boys". Dtsch Arztebl
Int 108 (4): 538. doi:10.3238/arztebl.2011.053. PMC 3036008.
PMID 21307992.
27
47.
Leber M, Tirumani A (June 8, 2006). "Balanitis". EMedicine.
Retrieved 2008-10-14.
48.
Osipov V, Acker S (November 2006). "Balanoposthitis". Reactive and
Inflammatory Dermatoses. EMedicine. Retrieved 2006-11-20.
49.
Aridogan IA, Izol V, Ilkit M (August 2011). "Superficial fungal
infections of the male genitalia: a review". Crit. Rev. Microbiol. 37 (3): 237
44. doi:10.3109/1040841X.2011.572862. PMID 21668404.
50.
Hayashi Y, Kojima Y, Mizuno K, Kohri K (2011). "Prepuce: phimosis,
paraphimosis, and circumcision". ScientificWorldJournal 11: 289301.
doi:10.1100/tsw.2011.31. PMID 21298220.
51.
Jagannath VA, Fedorowicz Z, Sud V, Verma AK, Hajebrahimi S
(2012). "Routine neonatal circumcision for the prevention of urinary tract
infections in infancy". In Fedorowicz, Zbys. Cochrane Database of
Systematic Reviews 11: CD009129. doi:10.1002/14651858.CD009129.pub2.
PMID 23152269.
52.
Jagannath VA, Fedorowicz Z, Sud V, Verma AK, Hajebrahimi S
(2011). "Routine neonatal circumcision for the prevention of urinary tract
infections in infancy (Protocol)". In Fedorowicz, Zbys. Cochrane Database
of Systematic Reviews (5): CD009129. doi:10.1002/14651858.CD009129.
53.
Larke NL, Thomas SL, Dos Santos Silva I, Weiss HA (August 2011).
"Male circumcision and penile cancer: a systematic review and metaanalysis". Cancer Causes Control 22 (8): 1097110. doi:10.1007/s10552011-9785-9. PMC 3139859. PMID 21695385.
54.
American Urological Association. "Circumcision". Retrieved 200811-02.
55.
Krill, Aaron J.; Palmer, Lane S.; Palmer, Jeffrey S. (2011).
"Complications of Circumcision". The Scientific World JOURNAL 11: 2458
2468. doi:10.1100/2011/373829. ISSN 1537-744X.
56.
Morris BJ, Waskett JH, Banerjee J, Wamai RG, Tobian AA, Gray RH,
Bailis SA, Bailey RC, Klausner JD, Willcourt RJ, Halperin DT, Wiswell TE,
Mindel A (2012). "A 'snip' in time: what is the best age to circumcise?".
BMC Pediatr 12: 20. doi:10.1186/1471-2431-12-20. PMC 3359221.
28
PMID 22373281. "Circumcision in adolescence or adulthood may evoke a
fear of pain, penile damage or reduced sexual pleasure, even though
unfounded."
57.
"Non-therapeutic circumcision of male minors (2010)". KNMG. 12
June 2010.
58.
Doyle D (October 2005). "Ritual male circumcision: a brief history".
The journal of the Royal College of Physicians of Edinburgh 35 (3): 279
285. PMID 16402509.
59.
Drain PK, Halperin DT, Hughes JP, Klausner JD, Bailey RC (2006).
"Male circumcision, religion, and infectious diseases: an ecologic analysis of
118 developing countries". BMC Infectious Diseases 6: 172.
doi:10.1186/1471-2334-6-172. PMC 1764746. PMID 17137513.
60.
Klavs I, Hamers FF (February 2008). "Male circumcision in Slovenia:
results from a national probability sample survey". Sexually Transmitted
Infections 84 (1): 4950. doi:10.1136/sti.2007.027524. PMID 17881413.
61.
Ko MC, Liu CK, Lee WK, Jeng HS, Chiang HS, Li CY (April 2007).
"Age-specific prevalence rates of phimosis and circumcision in Taiwanese
boys". Journal of the Formosan Medical Association=Taiwan Yi Zhi 106 (4):
3027. doi:10.1016/S0929-6646(09)60256-4. PMID 17475607.
62.
Richters J, Smith AM, de Visser RO, Grulich AE, Rissel CE (August
2006). "Circumcision in Australia: prevalence and effects on sexual health".
Int J STD AIDS 17 (8): 54754. doi:10.1258/095646206778145730.
PMID 16925903.
63.
Owings M et al. (August 22, 2013). "Trends in Circumcision for Male
Newborns in U.S. Hospitals: 19792010". Centers for Disease Control and
Prevention. Retrieved 22 January 2014.
64.
65.
66.
Gollaher (2001), ch. 1, The Jewish Tradition, pp. 1-30
"Circumcision". Encyclopaedia Judaica (2 ed.). USA: Macmillan
Reference. 2006. ISBN 978-0-02-865928-2.
Gollaher (2001), ch. 2, Christians and Muslims, pp. 31-52
29
67.
Gollaher (2001), ch. 3, Symbolic Wounds, pp. 53-72
68.
Darby, Robert (Spring 2003). "The Masturbation Taboo and the Rise
of Routine Male Circumcision: A Review of the Historiography". Journal of
Social History 36 (3): 737757.
69.
Gollaher, David L. (2000). Circumcision: A History of the World's
Most Controversial Surgery. New York: Basic Books. pp. 101104.
ISBN 0465026532.
70.
Bullough, Vern L.; Bonnie Bullough (1994). Human Sexuality: An
Encyclopedia. New York: Garland. p. 425. ISBN 0824079728.
71.
Conrad, Peter; Joseph W. Schneider (1992). Deviance and
Medicalization: From Badness to Sickness. Philadelphia: Temple University
Press. p. 212. ISBN 0877229996.
72.
Gollaher (2001), ch. 4, From Ritual to Science, pp. 73-108
73.
Siegfried N, Muller M, Volmink J, et al. (2003). "Male circumcision
for prevention of heterosexual acquisition of HIV in men". In Siegfried,
Nandi. Cochrane Database of Systematic Reviews (3): CD003362.
doi:10.1002/14651858.CD003362. PMID 12917962.
74.
Boyle GJ, Hill G (2011). "Sub-Saharan African randomised clinical
trials into male circumcision and HIV transmission: methodological, ethical
and legal concerns". J Law Med 19 (2): 31634. PMID 22320006.
75.
Dowsett GW, Couch M (May 2007). "Male circumcision and HIV
prevention: is there really enough of the right kind of evidence?".
Reproductive Health Matters 15 (29): 3344. doi:10.1016/S09688080(07)29302-4. PMID 17512372.
76.
Darby R, Van Howe R (2011). "Not a surgical vaccine: there is no
case for boosting infant male circumcision to combat heterosexual
transmission of HIV in Australia". Australian and New Zealand Journal of
Public Health 35 (5): 459465. doi:10.1111/j.1753-6405.2011.00761.x.
PMID 21973253.
30
77.
Frisch M et al. (2013). "Cultural Bias in the AAP's 2012 Technical
Report and Policy Statement on Male Circumcision". Pediatrics 131 (4):
796800. doi:10.1542/peds.2012-2896. PMID 23509170.
78.
McNeil, Jr., Donald G. (March 3, 2009). "AIDS: New Web Site Seeks
to Fight Myths About Circumcision and H.I.V.". The New York Times. p. D6.
Retrieved February 1, 2012.
79.
AVAC: Global Advocacy for HIV Prevention. "About male
circumcision". Retrieved December 2012.
80.
Bolnick, David A.; Katz, Kenneth E. (2012). "Jewish Ritual
Circumcision". In Bolnick, David A.; Koyle, Martin; Yosha, Assaf. Surgical
Guide to Circumcision. London: Springer. pp. 265274. doi:10.1007/978-14471-2858-8_23. ISBN 978-1-4471-2857-1. Retrieved April 6, 2014.
(subscription required (help)).
81.
al-Sabbagh, Muhammad Lutfi (1996). Islamic ruling on male and
female circumcision. World Health Organization. p. 16. ISBN 92-9021-2160.
82.
El-Sheemy, Mohamed S.; Ziada, Ali M. (2012). "Islam and
Circumcision". In Bolnick, David A.; Koyle, Martin; Yosha, Assaf. Surgical
Guide to Circumcision. London: Springer. pp. 275280. doi:10.1007/978-14471-2858-8_24. ISBN 978-1-4471-2857-1. Retrieved April 6, 2014.
(subscription required (help)).
83.
http://gracecommentary.com/luke-2_21-24/
84.
Pope Eugene IV's bull Cantate Domino says that "The sacrosanct
Roman Church" "commands all who glory in the name of Christian, at
whatever time, before or after baptism, to cease entirely from circumcision,
since, whether or not one places hope in it, it cannot be observed at all
without the loss of eternal salvation."
85.
Thomas Riggs (2006). "Christianity: Coptic Christianity". Worldmark
Encyclopedia of Religious Practices: Religions and denominations.
Thomson Gale. ISBN 978-0-7876-6612-5.
86.
Adams, Gregory; Adams, Kristina (2012). "Circumcision in the Early
Christian Church: The Controversy That Shaped a Continent". In Bolnick,
31
David A.; Koyle, Martin; Yosha, Assaf. Surgical Guide to Circumcision.
London: Springer. pp. 291298. doi:10.1007/978-1-4471-2858-8_26.
ISBN 978-1-4471-2857-1. Retrieved April 6, 2014. (subscription required
(help)).
87.
"Circumcision". Encyclopedia of Religion (2 ed.). Gale. 2005.
88.
"Circumcision of Infant Males". The Royal Australasian College of
Physicians. Sep 2010. Retrieved 11 September 2013.
89.
"Circumcision remains legal in Germany". Deutsche Welle. 12 Dec
2012. Retrieved 11 September 2013.
90.
Doyle S, Kahn J, Hosang N, Carroll P (2010). "The Impact of Male
Circumcision on HIV Transmission". Journal of Urology 183 (1): 2126.
doi:10.1016/j.juro.2009.09.030. PMID 19913816.
91.
Binagwaho A, Pegurri E, Muita J, Bertozzi S (Jan 2010). "Male
circumcision at different ages in Rwanda: a cost-effectiveness study". In
Kalichman, Seth C. Public Library of Science 7 (1): e1000211.
doi:10.1371/journal.pmed.1000211. PMC 2808207. PMID 20098721.
92.
Hankins C, Forsythe S, Njeuhmeli E (Mar 2012). "Voluntary medical
male circumcision: an introduction to the cost, impact, and challenges of
accelerated scaling up". In Sansom, Stephanie L. Arch Pediatr Adolesc Med
8 (11): e1001127. doi:10.1371/journal.pmed.1001127. PMC 3226452.
PMID 22140362.
93.
Xu X, Patel DA, Dalton VK, Pearlman MD, Johnson TR (Mar 2009).
"Can routine neonatal circumcision help prevent human immunodeficiency
virus transmission in the United States?". American journal of men's health
3
(1):
7984.
doi:10.1177/1557988308323616.
PMC 2678848.
PMID 19430583.
94.
Kacker S, Frick KD, Gaydos CA, Tobian AA (Aug 2012). "Costs and
Effectiveness of Neonatal Male Circumcision". Public Library of Science
166 (10): 19. doi:10.1001/archpediatrics.2012.1440. PMC 3640353.
PMID 22911349.
95.
Sadeghi-Nejad H, Wasserman M, Weidner W, Richardson D,
Goldmeier D (January 2010). "Sexually transmitted diseases and sexual
32
function". J Sex Med 7 (1 Pt 2): 389413. doi:10.1111/j.17436109.2009.01622.x. PMID 20092446.
Bibliography
Bolnick D A, Koyle M, Yosha A (September 2012). Surgical Guide to
Circumcision. Springer. ISBN 978-1-4471-2857-1.
Gollaher D (February 2001). Circumcision: A History Of The World's Most
Controversial Surgery. Basic Books. ISBN 978-0-465-02653-1.
This page was last modified on 21 May 2014 at 08:09.
Circumcision surgical procedure
Circumcision with a clamp
The surgical procedure of male circumcision may involve one of various devices
such as the Circumplast, Gomco clamp, Plastibell, and Mogen clamp.
With all these devices, the same basic procedure is followed. First, the amount of
foreskin to be removed is estimated. The foreskin is opened via the preputial
orifice to reveal the glans underneath and ensure it is normal. The inner lining of
the foreskin (preputial epithelium) is bluntly separated from its attachment to the
glans. The device is placed (this sometimes requires a dorsal slit) and remains there
until blood flow has stopped. Finally, the foreskin is amputated. [1] Sometimes, the
frenulum band may need to be broken or crushed and cut from the corona near the
urethra to ensure that the glans can be freely and completely exposed.[2]
Devices
33
Circumplast
With the Circumplast, once the glans is freed, the Circumplast is placed over the
glans, and the foreskin is placed over the Circumplast. A ligature is then tied firmly
around the foreskin and tightened into a groove in the Circumplast to achieve
hemostasis. Foreskin distal to the ligature is excised and the handle is snapped off
the Circumplast device. The Circumplast falls from the penis after the wound has
healed, typically in four to six days.
Gomco clamp
With a Gomco clamp, a section of skin is dorsally crushed with a hemostat and
then slit with scissors. The foreskin is drawn over the bell shaped portion of the
clamp and inserted through a hole in the base of the clamp. The clamp is tightened,
"crushing the foreskin between the bell and the base plate." The crushed blood
vessels provide hemostasis. The flared bottom of the bell fits tightly against the
hole of the base plate, so the foreskin may be cut away with a scalpel from above
the base plate.[3]
Plastibell
Plastibell circumcision day 6 post operation
With the Plastibell, once the glans is freed, the Plastibell is placed over the glans,
and the foreskin is placed over the Plastibell. A ligature is then tied firmly around
the foreskin and tightened into a groove in the Plastibell to achieve hemostasis.
Foreskin distal to the ligature is excised and the handle is snapped off the Plastibell
device. The Plastibell falls from the penis after the wound has healed, typically in
four to six days.[4]
Mogen clamp
With a Mogen clamp, the foreskin is pulled dorsally with a straight hemostat, and
lifted. The Mogen clamp is then slid between the glans and hemostat, following the
angle of the corona to "avoid removing excess skin ventrally and to obtain a
34
superior cosmetic result" to Gomco or Plastibell circumcisions. The clamp is
locked, and a scalpel is used to cut the skin from the flat (upper) side of the clamp.
[5][6]
References
1.
"Circumcision policy statement. American Academy of Pediatrics. Task Force on
Circumcision". Pediatrics 103 (3): 68693. March 1999. doi:10.1542/peds.103.3.686.
PMID 10049981.
2.
"Neonatal Circumcision: An Audiovisual Primer". Stanford School of Medicine.
3.
Peleg D, Steiner A (September 1998). "The Gomco circumcision: common
problems and solutions". American Family Physician 58 (4): 8918. PMID 9767725.
4.
Barrie H, Huntingford PJ, Gough MH (July 1965). "The Plastibell Technique for
Circumcison". British Medical Journal 2 (5456): 2735. doi:10.1136/bmj.2.5456.273.
PMC 1845746. PMID 14310205.
5.
Fowler, Grant C.; Pfenninger, John L. (2003). Pfenninger and Fowler's
procedures for primary care. St. Louis: Mosby. ISBN 978-0-323-00506-7.[page needed]
6.
Reynolds RD (July 1996). "Use of the Mogen clamp for neonatal circumcision".
American Family Physician 54 (1): 17782. PMID 8677833.
This page was last modified on 3 February 2014 at 19:23.
Gomco clamp
A Gomco clamp, otherwise known as a Yellen clamp,[1][2] is a specialized clamp
for performing circumcisions. It was invented by Hiram S. Yellen and Aaron
Goldstein in 1934-1935.[3][4] Gomco stands for the GOldstein Medical COmpany,
the original manufacturer of the clamp.[2] In a 1998 study, it was the preferred
circumcision technique of 67% of US physicians.[5]
Method
35
A 22-year-old Canadian man being circumcised with a Gomco clamp.
The technique is as follows:[6]
1. Anesthetic should be applied (though it is an historically recent addition,
dating only to approximately the early 1990s).
2. The foreskin is gripped with two hemostats (tissue holders) and a probe is
inserted between the foreskin and glans to break any adhesion.[7]
3. Once separated, a hemostat is used to crush the foreskin lengthwise in order
to reduce bleeding.[7]
4. Next, the foreskin is cut lengthwise where it was crushed to allow space to
insert the clamp.[7]
5. The bell of the clamp is placed over the glans, and the foreskin is pulled over
the bell.
6. The base of the clamp is placed over the bell, and the clamp's arm is fitted.
7. After the surgeon confirms correct fitting and placement, and the amount of
foreskin to be excised, the nut on the Gomco clamp is tightened, causing the
clamping of nerves and blood flow to the foreskin.
8. The clamp is left in place for about five minutes to allow clotting to occur,
then the foreskin is severed using a scalpel.
9. The clamp's base and bell are then removed from the penis.
Advantages
The circumcision scar is straight.
36
Most of the inner foreskin can be removed.
The circumcision is relatively quick compared to the more recent Plastibell.
Disadvantages
Involves several small parts, all of which must be sterile so as to ensure the
safety of the patient and minimize the risk of infection.
Procedure takes longer than the traditional Jewish Shield or Mogen Clamp
techniques.
The scar is more visible.
Prevalence
Distinctive brown ring scar resulting from neonatal circumcision using the Gomco clamp
method
Probably over 75% of circumcised American men born between 1950 and 1980
were circumcised with a Gomco clamp or a variant. The presence of a light brown
ring, typically one inch behind the corona, probably indicates a Gomco
circumcision.
Notes and references
1.
Warner, E; Strashin, E (1981). "Benefits and risks of circumcision". Canadian
Medical Association journal 125 (9): 96776, 992. PMC 1862490. PMID 7037142.
2.
Gelbaum, I (1993). "Circumcision Refining a traditional surgical technique".
Journal of Nurse-Midwifery 38 (2): 18S30S. doi:10.1016/0091-2182(93)90093-V.
PMID 8387102.
37
3.
Hodges, Frederick (1997). "A Short History of the Institutionalization of
Involuntary Sexual Mutilation in the United States". In Denniston, George C.; Milos,
Marilyn Fayre. Sexual mutilations: a human tragedy. Springer. p. 26. ISBN 978-0-30645589-6.
4.
Alanis, Mark C.; Lucidi, Richard S. (2004). "Neonatal Circumcision: A Review of
the World's Oldest and Most Controversial Operation". Obstetrical & Gynecological
Survey 59 (5): 37995. doi:10.1097/00006254-200405000-00026. PMID 15097799.
5.
Stang, H. J.; Snellman, L. W. (1998). "Circumcision Practice Patterns in the
United States". Pediatrics 101 (6): e5. doi:10.1542/peds.101.6.e5. PMID 9606247.
6.
Peleg, David; Steiner, Ann (1998). "The Gomco Circumcision: Common
Problems and Solutions". American Family Physician 58 (4): 8918. PMID 9767725.
7.
HealthWise Medical Reference, Available online at:
http://children.webmd.com/tc/circumcision-what-happens-during-a-circumcision Last
Updated: February 19, 2008.
Surgical instruments
Laser scalpel
RF knife
Lancets
Liston knife
Catlin
Von Graefe knife
Bandage scissors
Mayo scissors
Metzenbaum scissors
Tenotomy scissors
Scalpels
Dissecting
Surgica
l
scissors
:
38
Rongeur
Curette
Osteotome
Drill bits
Rasps
Trocars
Drills
Dermatomes
Other:
Bulldogs forceps
Hemostat
Obstetric
Vulsellum
Tenaculum
Debakey forceps
Foerster clamp
Hemostat
Pennington clamp
Aortic cross-clamp
Gomco clamp
Grasping (forceps)
Clamping
39
Retracting/viewin
g
Allis clamp
Retractors: Senn retractor
Rib spreader
Dilators
Specula
Fiber optic endoscopes
Head mirror
Yankauer suction tip
rulers and calipers
Jackson-Pratt drain
Penrose drain
Surgical staplers
Periodontal probe
Surgical suture
Examination/prep:
Suction:
Irrigation and injection needles
Accessory/other
Measurement devices:
Drain:
Other:
This page was last modified on 2 December 2013 at 03:38.
40
The Gomco Circumcision:
Common Problems and Solutions
DAVID PELEG, M.D., and ANN STEINER, M.D., University of Iowa Hospitals and Clinics,
Iowa City, Iowa
Am Fam Physician. 1998 Sep 15;58(4):891-898.
Circumcision performed using the Gomco clamp is usually quick and effective,
and results in very little bleeding. However, every clinician performing
circumcision occasionally has concerns or questions regarding the procedure.
Some of the more common concerns regarding the use of the Gomco clamp are
technique-related, including choosing the correct size of the Gomco bell and clamp
for the procedure, choosing the right method of getting the foreskin properly
through the hole of the Gomco base plate, and assessing how much foreskin to
remove. Other concerns include poor cosmetic results, contraindications to routine
circumcision, and circumcision in an infant whose mother has human
immunodeficiency virus. This article reviews the technique of circumcision using
the Gomco clamp and answers some of the more common questions.
The Gomco clamp has become one of the leading instruments used in the
performance of non-ritual circumcision in the United States. This device is popular
because of its safety record in preventing injury and bleeding.
Technique
The procedure can be started after informed consent is obtained from the parents
and the infant is properly identified. After the infant is restrained, the penis,
scrotum and groin area are cleaned with a disinfecting solution and are inspected
for anatomic abnormalities (Figure 1). The Gomco clamp is checked to make sure
the bell is the right size for the clamp and that there are no defects (Figure 2). The
area is prepped and a dorsal penile nerve block is administered, if desired (Figure
3a and 3b), unless a topical anesthetic cream (such as 2.5 percent prilocaine and
2.5 percent lidocaine [Emla]) has been used. A drape is used if desired.
41
FIGURE 1.
Schematic representation of normal neonatal penile anatomy.
FIGURE 2.
The Gomco circumcision clamp.
FIGURE 3A.
Correct points to inject dorsal penile nerve block.
42
FIGURE 3B.
Cross section anatomy of the penis.
The foreskin is grasped on either side of the midline with two hemostats, taking
care to avoid the urethral meatus, and a third hemostat or other instrument is
carefully inserted into the preputial ring down to the level of the corona. The
instrument should be used to tent the foreskin away from the glans to avoid the
urethral meatus. The hemostat is swept around the glans on both the right and left
sides, avoiding the ventral frenulum. This separates most of the adhesions between
the inner mucosal layer and the glans. The hemostat is removed and is then used to
create a crush line on the dorsal aspect not closer than 1 cm to the coronal sulcus in
the foreskin. The crushed skin is cut with blunt scissors, taking care to avoid the
glans (Figure 4a).
FIGURE 4A.
Dorsal crush and slit.
The foreskin is then retracted proximally using the hemostats, exposing the glans.
Any remaining adhesions are bluntly divided using a blunt probe or gauze until the
entire coronal sulcus is visible. Care should be taken to avoid the ventral frenulum
to prevent bleeding. The foreskin is then drawn over the glans, and the bell of the
43
Gomco clamp is inserted over the glans (Figure 4b). Several methods to pull the
foreskin through the hole of the base plate around the bell are described later in this
article. The stem of the bell is then maneuvered through the hole along with the
foreskin after the amount of foreskin to be removed has been determined (Figure
4c). The amount of remaining shaft skin is evaluated and may be adjusted for
length and symmetry (Figure 4d).
FIGURE 4B.
Insertion of the bell over the glans.
FIGURE 4C.
Grasping the edges of the dorsal slit and inserting the arms of the bell
through the hole of the plate.
44
FIGURE 4D.
Pulling the foreskin upwards and adjusting the bell and base plate.
The rocker arm (top plate) of the Gomco clamp is then attached (if this has not
been done previously) and brought around into the notch of the base plate. The
arms of the bell are settled into the yoke, and the nut is tightened, crushing the
foreskin between the bell and the base plate (Figure 4e). A scalpel is then used to
excise the foreskin at the level of the base plate (Figure 4f). The nut is then
loosened, and the top and base plate are removed from the bell. The shaft skin is
then eased off the bell at the line of incision using a gauze with mild traction, to
take its place below the corona.
FIGURE 4E.
Final assembly.
45
FIGURE 4F.
Excising the foreskin.
The penis should be inspected following the procedure for signs of bleeding, with
special attention to the ventral frenulum region. A dressing of petroleum jelly or
petroleum gauze should be gently applied. The parents should be counseled about
the healing process. Gentle retraction of the shaft skin may be necessary if it
encroaches on the glans. Petroleum jelly may be applied liberally at diaper changes
until the glans re-epithelializes.
Answers to Frequently Asked Questions
1. Is routine circumcision contraindicated in some male infants?
Several anatomic variations or abnormalities prohibit routine circumcision without
proper consultation with a urologist. They include hypospadias, epispadias,
megaurethra or abnormally short penile shaft (Figure 5). If, when placing the index
and middle finger at the base of the penis and pushing down, there is less than 1
cm of penile shaft visible, then a Gomco circumcision should not be performed.
Careful inspection of the infant's anatomy is important before beginning the
procedure.
FIGURE 5.
Examples of an infant with an abnormally short penile shaft. Circumcision should be
deferred until after consultation with a urologist.
Circumcision in infants who are ill or premature should be delayed until they are well or
ready for discharge from the hospital.
2. Should a dorsal penile nerve block be used?
46
The dorsal penile nerve block was first described in 1978.1 Since then, more than
2,000 newborns undergoing circumcision and receiving dorsal penile nerve blocks
have been reported without any major complications.17 The nerve block is a
simple procedure that can be easily performed. Typically, 0.4 mL of 1 percent
lidocaine is injected into the subcutaneous tissue at the base of the penis at each of
the points indicated in Figure 3a for a total of 0.8 mL.
Some physicians prefer to use a single mid-line injection, but this has not been well
studied or described. A small amount (0.1 to 0.2 mL) of 1 percent sodium
bicarbonate pre-mixed with lidocaine can decrease the pain caused by the acidic
pH of the lidocaine solution. To avoid intravascular injection, negative pressure
should be applied frequently to check for the absence of blood. Some clinicians
prefer to administer the block before draping the area, and then to gently massage
the area while waiting approximately five minutes required for maximum effect of
the anesthetic to occur.
A low rate of minor complications such as local bruising, hematoma and excessive
bleeding at the injection site have been reported.1,35 Theoretic but unreported
complications include lidocaine toxicity, lidocaine effect, delay in voiding and
interference with erectile function. The most serious complication that has been
reported occurred in 1990,6 and involved a two-day-old infant who received a
dorsal penile nerve block with an inadvertent injection of 1:1,000 epinephrine. The
infant had a brief hemodynamic response followed by a profound vasoconstriction
and ischemia of the genitalia. This was resolved by inserting a caudal catheter and
establishing a sympathetic block. The use of epinephrine is contraindicated in any
procedure involving the penile shaft.
In 1991, concerns were raised regarding the safety of the dorsal penile nerve block
because of the limited number of case reports at that time.8 Concern centered on
the potential risk of lidocaine in the dorsal vein causing systemic effects in the
central nervous system or heart, or systemic absorption from the tissues (which
could lead to toxicity). Thus far, these complications have not been reported.
A common complication of the dorsal penile nerve block is its failure to provide
adequate analgesia. This complication may be the result of a lack of experience on
the part of the clinician and the failure to wait five minutes after the block is
administered.9,10
Multiple studies2,5,7,11 have documented a decrease in pain perceived by the
neonate during routine circumcision when a dorsal penile nerve block is used.
47
Because of the reported lack of major complications in over 2,000 infants receiving
this analgesic block, it is reasonable to recommend that physicians performing
routine newborn circumcision should become familiar and proficient with this
technique.
There has been interest in a lidocaine-prilocaine cream for use in circumcision. In
one small trial,12 this cream was shown to be more effective than placebo.
Although the manufacturer warns against its use in infants less than one month of
age because of the potential risk of methemoglobinemia, this concern may be
unwarranted.
3. What size of Gomco bell should be used? Does it have to
completely cover the glans?
The size of the Gomco bell used for the circumcision is dependent on the diameter
of the glans rather than on the length of the penile shaft. The bell should
completely cover the glans penis without overly distending the foreskin. Too small
a bell will fail to protect the glans and will cause the foreskin to be redundant as it
is pulled through the base plate. If a bell is selected that does not fulfill these
criteria, the physician should choose a different clamp and bell to get the best fit.
Care should be taken to assure that the bell is the correct size for the plate and arm
being used.
4. What technique should be used for getting the foreskin properly
through the hole of the Gomco base plate after the bell has been
applied?
Multiple techniques have been used to secure the foreskin in order to bring it
through the hole of the base plate. The most important element of this procedure is
to make sure that the bell stays under the foreskin and over the glans and that equal
amounts of mucosa and foreskin are brought through the base plate. In addition,
the apex of the dorsal slit must be visible above the plate before putting the arms in
the yoke and excising the foreskin. A small safety pin may be used to bring the
edges of the dorsal slit together over the flare of the bell before bringing the draw
stud through the base plate. The safety pin should be inserted through both the
foreskin and the mucosa so that care is taken not to omit the mucosal layer. In
addition, the clinician must take special care to make sure that the sharp end of the
safety pin does not cause inadvertent injury to the clinician or the infant. Once the
safety pin is satisfactorily inserted through the foreskin and underlying mucosa, the
base plate can be placed over the draw stud, followed by the safety pin holding the
48
foreskin and the mucosa. The level at which the foreskin is to be excised can then
be adjusted before placing the arms of the draw stud into the yoke.
A second method for bringing the foreskin through the base plate involves placing
the bell between the glans and the foreskin, and then placing a hemostat directly
through the hole in the base plate. The hemostat is then used to draw the edges of
the dorsal slit together over the flare of the bell. The hemostat can then be pulled
back through the hole in the base plate, bringing the draw stud and foreskin with it
(Figure 4c and d). Once again, care must be taken to make sure that equal amounts
of foreskin and underlying mucosa are brought through and excised. This approach
limits the number of operative steps involved in performing the procedure.
A third method, and one that we prefer, involves clamping the edges of the dorsal
slit together with a hemostat over the flare of the bell after it has been placed over
the glans penis. This assures that the bell will stay in place. The draw stud is then
brought through the hole of the base plate and two separate hemostats are then
used to grasp the corners of the dorsal slit at the level of the preputial opening
(Figure 6). The original hemostat is then removed from the foreskin at the level of
the flare of the bell, and the two hemostats above the base plate can then be used to
draw the foreskin and draw stud through the base plate hole. This technique allows
exact adjustment of the angle of the bell as it lies over the glans and allows
adjustment of the amount of foreskin and mucosa to be removed. Once again, care
is taken to make sure that the foreskin and mucosa are within the clamps and that
equal amounts are removed.
FIGURE 6.
Pulling the skin and mucosa through the hole in the base plate using hemostats.
5. What should be done if the physician notices that the urethral
meatus is displaced, and that the infant has either an epispadias or
hypospadias after the dorsal slit has been made and the foreskin has
been pulled proximally, exposing the glans?
At this point, the procedure should be terminated since any repair of these
congenital anomalies may involve the use of foreskin tissue. If there is bleeding
from the dorsal slit, the edges should be whipstitched using a fine chromic suture,
or the dorsal slit may be closed using a interrupted fine chromic suture. In one
49
study of complications resulting from circumcision,13 22 (0.4 percent) of 5,882
newborns studied were noted to have some type of hypospadias. One third of these
infants had completion of the procedure despite the presence of an anomaly.
6. What should be done if the edges of the dorsal midline incision are
bleeding persistently, making the procedure difficult?
Care must be taken at the time of creating the dorsal slit to stay within the crushed
area of tissue and not to extend the dorsal slit past the apex of the area of crushed
tissue. This will limit the amount of bleeding from the edges of the dorsal slit.
Should bleeding occur, it is best to proceed with the circumcision because once the
Gomco clamp is in place, bleeding from the dorsal slit will stop. If the bleeding
interferes with continuing the procedure, a hemostat can be used to create a second
area of crushed tissue overlying the area of bleeding. As long as the area of crushed
tissue is within the portion of the foreskin that is to be removed during the
circumcision, this will not change the cosmetic outcome of the procedure. If
generalized bleeding persists without an obvious source, consideration should be
given to the possibility of a bleeding disorder.
7. How can the bell be kept from falling off the glans while trying to
get the draw stud through the hole of the base plate?
Failure to keep the bell in place while pulling the draw stud and the foreskin
through the base plate can happen for a number of reasons: the preputial opening
may be dilated, the dorsal slit may be too long or the bell being used may be too
small. The immediate problem can be solved by changing the size of the Gomco
clamp and bell, or by using a hemostat to draw the edges of the dorsal slit together
across the flare of the bell while grasping the tissue around the dorsal slit on either
side widely, thus creating tension on the foreskin across the flare of the bell.
8. What if, after everything is in place but before the Gomco nut has
been closed, the physician is uncertain whether there is too much or
too little foreskin above the base plate?
The amount of penile shaft skin that should remain after circumcision should be
assessed before the actual circumcision. One way to do this is to mark the
circumference of the shaft skin with a marker, typically at the coronal ridge. In
addition, when the dorsal slit is created, the clinician should have an idea about
how much shaft skin should remain below the base plate. Equal amounts of skin
and mucosa must be pulled through the bevel hole. Inadequate separation of the
50
mucous membrane from the glans may result in adhesions or phimosis. If a
decision is made to adjust the amount of foreskin to be removed after the Gomco
clamp is in place, it is important to disassemble the draw stud arms from the yoke
and to pull the bell away from the base plate. If an attempt is made to adjust the
amount of foreskin while the clamp and bell are still assembled, there is a risk that
vessels between the foreskin and the underlying mucosa will be sheared off and
will retract. The vessels will not be sealed when foreskin excision occurs and may
be at risk for bleeding, causing wound dehiscence at the line of incision.
9. What if it appears that too little foreskin has been removed after
the circumcision has been completed?
Once the circumcision has been performed by the clinician, it may become
apparent that too little foreskin and/or underlying mucosa was removed, requiring
another procedure. If the glans is not exposed following the circumcision, then this
is probably the case. Failure to remove enough of these tissues is likely to be due to
the lack of enough tissue being pulled through the base plate rather than using a
clamp that is too small. Any subsequent procedure should be referred to a
urologist.
10. What if the nurse checks the infant's penis 30 minutes after the
procedure and reports that the glans is no longer visible?
If not enough foreskin or underlying mucosa is removed during circumcision, a
condition known as concealed penis can occur. In this situation, the penile shaft
and glans are pushed back into the scrotal fat and the penis is buried. As long as the
baby is able to urinate without obstruction, there is no need for further procedure at
this time. However, a revision of the circumcision may be necessary at a later time.
This procedure should be performed by a pediatric urologist.
11. What is the most common reason for a poor cosmetic result?
Failure to completely free mucosal adhesions from the glans penis so that the entire
coronal sulcus is exposed is the most common reason for a poor cosmetic result.
The most common place for this to occur is at the coronal sulcus just lateral to the
ventral frenulum. If the adhesions are not completely separated, not enough
mucosa will be removed and the glans will not be completely exposed. Phimosis
may result. In one study,14 this occurred in 2 percent of patients undergoing
circumcision.
51
12. What if the parents want to take the infant home but he hasn't
urinated yet?
Most nurseries require that the infant urinate before undergoing circumcision.
However, barring complications during circumcision, there is no reason that the
infant needs to stay in the hospital after circumcision until micturition occurs.
13. Should the physician perform a circumcision on an infant whose
mother has HIV infection?
The HIV status of the mother should not affect the physician's decision to perform
newborn circumcision unless she has thrombocytopenia. In that situation, the
physician would first make sure that the baby has a normal platelet count. The staff
involved in performing the circumcision should use universal precautions, as they
should when performing any circumcision. We are not aware of any data regarding
newborn circumcision in sons of HIV-positive mothers.
14. What if the parents request a Jewish ritual circumcision (known
as Berit Mila)?
Fulfillment of the covenant of Berit Mila by people of the Jewish faith is one of
their oldest rituals, dating back 5,000 years to Abraham. This ceremony usually
occurs on the eighth day of an infant's life and is usually performed by a ritual
circumciser known as a Mohel or Mohelet. Premature infants or infants who are ill
may have the ceremony deferred until they are able to safely undergo circumcision.
In a community with a large Jewish population, the Mohel or Mohelet is readily
available. In a small town without a significant Jewish population, a Mohel or
Mohelet may be harder to find and parents may have to locate one in a larger town
or travel to the larger community themselves. Checking with a local Rabbi is
probably the best way to find out what services or alternatives are available to a
Jewish family.
The Authors
DAVID PELEG, M.D., is a fellow in maternal-fetal medicine at the University of
Iowa Hospitals and Clinics, Iowa City. Dr. Peleg received a medical degree from
Hebrew UniversityHadassah Medical School, Jerusalem, and completed training
at the Central Emek Hospital, Afula, Israel.
52
ANN STEINER, M.D., is associate clinical professor of obstetrics and gynecology
at the University of Iowa Hospitals and Clinics. Dr. Steiner received a medical
degree from Case Western Reserve University School of Medicine, Cleveland, and
completed a residency in obstetrics and gynecology at the University of California,
San Francisco, School of Medicine. She is also a Mohelet certified by the Berit
Mila Board of Reform Judaism.
Address correspondence to David Peleg, M.D., Dept. of Obstetrics and
Gynecology, University of Iowa Hospitals and Clinics, 200 Hawkins Dr., Iowa
City, IA 52242-1080. Reprints are not available from the authors.
The authors thank Edward Bell, M.D., and Charles Hawtrey, M.D., both professors
from the University of Iowa Hospitals and Clinics, for reviewing the manuscript.
REFERENCES
1. Kirya C, Werthmann MW. Neonatal circumcision and penile dorsal nerve block: a painless
procedure. J Pediatr. 1978;92:9981000.
2. Arnett RM, Jones JS, Horger EO 3d. Effectiveness of 1 percent lidocaine dorsal penile nerve
block in infant circumcision. Am J Obstet Gynecol. 1990;163:10748.
3. Fontaine P, Dittberner D, Scheltema KE. The safety of dorsal penile nerve block for neonatal
circumcision. J Fam Pract. 1994;39:2438.
4. Mintz MR, Grillo R. Dorsal penile nerve block for circumcision. Clin Pediatr. 1989;28:5901.
5. Williamson PS, Williamson ML. Physiologic stress reduction by a local anesthetic during
newborn circumcision. Pediatrics. 1983;71:3640.
6. Berens R, Pontus SP Jr. A complication associated with dorsal penile nerve block. Reg Anesth.
1990;15:30910.
7. Stang HJ, Gunnar MR, Snellman L, Condon LM, Kestenbaum R. Local anesthesia for
neonatal circumcision. Effects on distress and cortisol response. JAMA. 1988;259:150711.
8. Schoen EJ, Fischell AA. Pain in neonatal circumcision. Clin Pediatr. 1991;30:42932.
9. Ryan CA, Finer NN. Changing attitudes and practices regarding local analgesia for newborn
circumcision. Pediatrics. 1994;94:2303.
10. Wellington N, Rieder MJ. Attitudes and practices regarding analgesia for newborn
circumcision. Pediatrics. 1993;92:5413.
53
11. Maxwell LG, Yaster M, Wetzel RC, Niebyl JR. Penile nerve block for newborn circumcision.
Obstet Gynecol. 1987;70:4159.
12. Taddio A, Stevens B, Craig K, Rastogi P, Ben-David S, Shennan A, et al. Efficacy and safety
of lidocaine-prilocaine cream for pain during circumcision. N Engl J Med. 1997;336:1197201.
13. Gee WF, Ansell JS. Neonatal circumcision: a ten-year overview: with comparison of the
Gomco clamp and the Plastibell device. Pediatrics. 1976;58:8247.
14. Fraser IA, Allen MJ, Bagshaw PF, Johnstone M. A randomized trial to assess childhood
circumcision with the Plastibell device compared to a conventional dissection technique. Br J
Surg. 1981;68:5935.
Copyright 1998 by the American Academy of Family Physicians.
Copyright 2014 American Academy of Family Physicians.
Plastibell
54
A 6 day old Plastibell Circumcision Device on a one month old infant.
The Plastibell Circumcision Device is a clear plastic ring with a deep groove
running circumferentially designed for circumcising infant males. The Plastibell is
placed onto the head of the penis during a 10 minute surgical procedure, and the
device will fall off within 3 to 7 days. The Plastibell was invented by Hollister Inc
in 1950, and first reported on in 1953.[1][2]
Surgical description
A baby midway through a Plastibell circumcision.
The Plastibell Circumcision Device is a clear plastic ring with handle designed
for male neonatal circumcision that has a deep groove running circumferentially.
The elective minimally invasive surgical procedure to install the Plastibell device
may be performed by an OB/GYN, a pediatrician, a urologist, a family physician
or a pediatric surgeon. The important issue is that the medical practitioner is
trained in the procedure.
The adhesions between glans and foreskin are divided with a probe. Then the
foreskin is cut longitudinally to allow it to be retracted and the glans (the head of
penis) to be exposed. The Plastibell comes in 6 sizes. The appropriate one is
55
chosen and applied to the head (the circumcision pictured at right is in this stage).
The ring is then covered over by the foreskin. A ligature is tied firmly around the
foreskin, crushing the skin against the groove in the Plastibell. Then the excess
skin protruding beyond the ring is trimmed off. Finally, the handle is broken off at
the end of the procedure. The entire procedure takes five to ten minutes, depending
on the experience and skill of the surgeon.[3]
As with all circumcisions, the procedure should involve adequate anaesthesia,
using either EMLA cream,[4] dorsal penile nerve block, penile ring block, or a
combination of these prior to operation. The ring falls off in 3 to 7 days leaving a
circumferential wound that will heal over the following week. Typically, the glans
will appear red or yellow until it has cornified.
Advantages
The glans is protected during the procedure by the ring. Hemostasis (control of
bleeding) is effective due to the ligature tie. Cosmetically, a predictable result is
obtained due to the straight line of the ligature that causes the wound. It is a quick
procedure for the physician to performonce mastered.
No bandage is required, allowing easy monitoring for infection.
Healing occurs while the edges of the prepuce are secured in the ring, making skin
bridges (where the foreskin's end heals to the glans' corona) unlikely.
Cosmetically, there will be little to no circumcision scar, though as usual with any
circumcision, there will be a color change where the (formerly) inner and outer
layers of foreskin meet.
Disadvantages
The ring must fall off before final healing can occur. Rarely, the tip of the glans
may protrude through the ring and become swollen, trapping the ring in place.
Blood transfusion risk 1 in 30,000 procedures (Wiswell).[citation needed]
One study of 2000 Plastibell circumcisions found a complication rate of 1.8%.[5]
The foreskin must be slit and forced from the glans to allow entry for the plastic
dome.
56
Furthermore, because convalescence depends on a (temporarily) affixed medical
device, risks of infection or hemorrhage due to the bell slipping or otherwise
failing are greater[6] than a Gomco clamp or similar entirely-supervised
circumcision. There are several reports in the literature of urinary retention after
circumcision with the Plastibell device.[7] Death has been reported.[8][9][10]
Other disadvantages include the risk of infection, with cases of impetigo,[11] as well
as necrotizing fasciitis.[12][13] There have also been cases of necrosis of the glans
penis following circumcision with the Plastibell instrument.[14]
Prevalence
The Plastibell device is one of the three most common devices used for neonatal
circumcision in the United States, the other two being the Mogen clamp and the
Gomco clamp.[15]
Notes and references
1.
Miller, RL; Snyder, DC (1953). "Immediate circumcision of the newborn male".
American journal of obstetrics and gynecology 65 (1): 111. PMID 13016660.
2.
Kariher, DH; Smith, TW (1956). "Immediate circumcision of the newborn".
Obstetrics and gynecology 7 (1): 503. PMID 13280246.
3.
Barrie, H.; Huntingford, P. J.; Gough, M. H. (1965). "The Plastibell Technique for
Circumcison". BMJ 2 (5456): 2735. doi:10.1136/bmj.2.5456.273. PMC 1845746.
PMID 14310205.
4.
Russell, CT; Chaseling, J (1996). "Topical anaesthesia in neonatal circumcision: A
study of 208 consecutive cases". Australian family physician. Suppl 1: S304.
PMID 9479796.
5.
Izzidien Al-Samarrai A.Y., Mofti A. Crankson S. J The Use of Plastibell in
Neonatal Circumcision. Review of 2000 cases. Surg. Gyne & Obst.167: 341-343,
1988[verification needed]
6.
Brennae, Mark (June 13, 2007). "Ontario boy dies after complications from
circumcision". The Vancouver Sun (CanWest News Service). Retrieved 2008-07-16.
7.
Ly, L; Sankaran, K (2003). "Acute venous stasis and swelling of the lower
abdomen and extremities in an infant after circumcision". CMAJ 169 (3): 2167.
PMC 167126. PMID 12900483.
57
8.
Paediatrics & Child Health, Home[dead link]
9.
http://www.austlii.edu.au/cgi-bin/sinodisp/au/cases/vic/VCAT/2010/1772.html?
stem=0&synonyms=0&query=anaesthetic[full citation needed]
10.
Paediatric Death Review Committee: Office of the Chief Coroner of Ontario
(2007). "Circumcision: A minor procedure?". Paediatrics & child health 12 (4): 3112.
PMC 2528673. PMID 19030377.
11.
Stranko, J; Ryan, ME; Bowman, AM (1986). "Impetigo in newborn infants
associated with a plastic bell clamp circumcision". Pediatric infectious disease 5 (5):
5979. PMID 3763425.
12.
Bliss, David P.; Healey, Patrick J.; Waldhausen, John H.T. (1997). "Necrotizing
fasciitis after Plastibell circumcision". The Journal of Pediatrics 131 (3): 45962.
doi:10.1016/S0022-3476(97)80078-9. PMID 9329429.
13.
Woodside, JR (1980). "Necrotizing fasciitis after neonatal circumcision".
American journal of diseases of children 134 (3): 3012.
doi:10.1001/archpedi.1980.02130150055015. PMID 6444778.
14.
Bode, C.O.; Ikhisemojie, S.; Ademuyiwa, A.O. (2010). "Penile injuries from
proximal migration of the Plastibell circumcision ring". Journal of Pediatric Urology 6
(1): 237. doi:10.1016/j.jpurol.2009.05.011. PMID 19570722.
15.
"Circumcision policy statement. American Academy of Pediatrics. Task Force on
Circumcision". Pediatrics 103 (3): 68693. 1999. doi:10.1542/peds.103.3.686.
PMID 10049981.
This page was last modified on 24 May 2014 at 07:46.
Plastibell
Last updated: 08 March 2014, 18:48 UTC
This page includes images of child patients. The Plastibell is only made in
child sizes, therefore it is not possible for us to illustrate its use with
reference to an adult patient.
Description and commercial history of the device
58
Originally marketed in 1955, the Plastibell is a disposable plastic bell-shaped
object with a groove close to its edge. The bell is inserted into the preputial cavity
(over the glans and under the foreskin) and the foreskin is tied around it with a
tight string. Blood flow to the prepuce is thereby ceased and the prepuce forward
of the string is cut off. The handle is then snapped off. After several days, the
prepuce caught under the string necrotizes and falls off, providing a bloodless
circumcision with no open wound to become irritated or infected.
It took in excess of seven years for a patent to be granted. Why that is so is a matter
of some debate; one possibility is that there was doubt about the true novelty of the
device. The same technique of strangulation with a tied cord can be found in the
Ross Ring dating from 1939; the two clamps differ only in respect of the material
used to make them and the design of their respective handles. The US Patent
Office may have taken the view that the Utility Model (the fundamental principle
of operation) of the Plastibell was the same as that of the Ross Ring and therefore
not eligible for protection of Intellectual Property Rights. That said, the differences
between the Ross Ring and the Plastibell remained eligible for patent protection
and it was those features (the use of plastic to facilitate the novel break-off handle)
that were the subject of the grant of a patent in October 1962.
Even in the mid-1950s anybody could mimic Rosss utility model, intellectual
property rights to the fundamental concept having already expired due to passage
of
time.
The patent in respect of the Plastibell expired in the 1970s. Thus there is now a
free-for-all as regards copying the original design as marketed by Hollister. Several
companies currently manufacture such circumcision devices. However, the trade
name Plastibell should be used only to describe the product of the current
trademark owner. The trademark was originally registered to Hollister Inc.
(incorporated in Illinois, USA), 2000 Hollister Drive, Libertyville, IL 60048. As at
January 2011 the "Last Listed Owner" (renewed September 2006) is Briggs
Manufactured Products LLC (incorporated in Delaware, USA), 7300 Westown
59
Parkway,
West
Des
Moines,
IA
50266.
CIRCLIST is aware of several manufacturing sources, listed below. Not all are
accredited by the USFDA (the United States Food and Drug Administration),
despite the simplicity of applying for such accreditation via the substantial
equivalence fast track procedure. Those not yet accredited are encouraged to
apply. Some suppliers offer enhancements to the original design, such as elastic
(Spandex) string in place of the traditional original inelastic material.
The Plastibell circumcision technique
Because of the danger of the plastic ring being pulled back behind the glans, only
the foreskin that naturally covers the glans can be safely removed using the
Plastibell.
Hence
it
usually
results
in
a
loose
circumcision.
The Plastibell is used in nearly 60% of all routine infant circumcisions in the US
with the majority of the rest being done by the Gomco Clamp method.
60
For some 40 years the Plastibell was the only disposable child circumcision device
in use, until the appearance of the Tara KLamp in 1995.
Case study, United Kingdom, March/April 1980
The left-hand image shows an 8-year old boy with a long, tight
foreskin, who was circumcised during the Easter school holidays,
1980. The right-hand image shows the same boy with a Plastibell
device in place and the overhang of foreskin excised. Applied to a boy
of this age, the bell, ligature and necrotic foreskin remnant are likely
to remain in place for approximately 7 days before falling off - usually
in the bath.
Legal Notes: In April 2013 an anonymous complaint was made to the
Internet Watchdog NCMEC suggesting that publication of the lefthand image constituted child exploitation. That assertion was
initially upheld by NCMEC but later withdrawn following appeal by
the editor of this website. TAKE NOTE that the images are therefore
deemed to be legal for public display in a medical-educational
context, but in some countries it may nevertheless be illegal to possess
retained copies without good cause. Therefore you are advised NOT
to download these images to personal off-line storage. Both the above
images are copyright and appear here with the knowledge and
consent of the original photographer who was present at the
circumcision by arrangement with the surgeon, the late Dr. Oswald
Burnett Gibson, MB, BS, FFARCS (1930-1981).
61
During the 5 to 10 days that the device remains attached, it is pulled tight against
the glans by the foreskin trying to retract back to its unstretched position. For this
reason, Hollister recommend that the foreskin should not be pulled too far forward
before being trapped by the thread around the Plastibells groove. This results in a
necessarily looser circumcision than can be achieved with the Gomco clamp; the
Plastibell is wholly unsuitable for tight styles. Furthermore, the position of the scar
line behind the glans is determined only by the distance from the back of the glans
to the groove in the bell. For a given glans circumference (and hence Plastibell
size) the longer the boys glans the further back the resulting scar line will be and
the
looser
the
circumcision
will
be.
If the Plastibell is fixed too tightly then the front of it can dig into the glans and
cause problems, including obstruction of the urethra. The photo above shows the
Plastibell properly applied immediately after the procedure; the final result was
most satisfactory with no loose foreskin covering the boys glans when flaccid.
The largest Plastibell generally available in the United States and Great Britain is
designed to fit the average 11-12 year old boy. Well-developed boys of this age
may have too large a glans to use the Plastibell, whereas very late developers may
be able to be circumcised with it up to 14 or so years old. It is very important that
the correct size bell is used to avoid damage to the glans.
The Plastibell can be applied quickly and easily under local anaesthesia. Within the
time that the anaesthesia remains effective, not only has the blood supply been cut
off from the foreskin but also the nerve endings at, and forward of, the thread are
rendered ineffective. All the boy will feel is a slight pressure from the bell on the
glans.
Because no stitches are used with a Plastibell there is no need for dressings,
antibiotics, etc which makes things very much simpler, especially with young
children who cannot easily co-operate. Pain from the circumcision site is, to a great
extent, related to the degree of desire for the operation. A boy who actively
requests and wants it will not notice the pain as much as one who actively opposed
the operation, or who simply wasnt consulted.
62
Absence of adult sizes
The device is not produced in adult sizes. Post-puberty, the foreskin is simply too
tough to be adequately strangled by a string ligature alone. Inadequate isolation
of the necrotic tissue can be very dangerous, potentially leading to severe infection.
Historically speaking, overcoming this constraint appears to have been the
motivation behind the development of the Zhenxi Ring and the Shang Ring.
Articles in the medical press about the Plastibell
Pediatr Surg Int. 2006 Oct 6
Palit V, Menebhi DK, Taylor I, Young M, Elmasry Y and Shah T. A unique service in UK
delivering Plastibell circumcision: review of 9-year results.
Muslim infants undergo circumcision for religious reasons and Bradford has a high
Muslim population. The National Health Service in UK does not provide religious
circumcision, so in1996 a nurse-delivered circumcision service led by consultant
urologists was set up at a no-profit and cost-only basis. Plastibell circumcision was
offered to all infants between 6 and14 weeks old and performed under local
anaesthesia. Information leaflets and videotapes about the procedure were
available to parents prior to the procedure. A three monthly audit of the service was
undertaken. Between July 1996 and June 2005 (9 years) 1,129 circumcisions were
performed. The common complications were problems with the ring (3.6%) and
63
bleeding(3%). Overall, there was 96% satisfaction rate among the service users.
The Plastibell technique for circumcision is a simple method and can be safely
performed by trained nurses with acceptable complication rates.
J Pediatr Urol. 2009 Jun 12.
Samad A, Khanzada TW and Kumar B (Department of Surgery, Isra University, Hyderabad,
Pakistan). Plastibell circumcision: A minor surgical procedure of major importance.
OBJECTIVE: To determine the number of days taken by the Plastibell to fall off
after circumcision and the Plastibell impaction rate in various age groups.
METHODS: This was a prospective cohort study of male babies who underwent
circumcision using the Plastibell technique. Patients were followed up 1 week
postoperatively as well as soon after the Plastibell had fallen off. RESULTS: Mean
age was 14.3 months and mean weight 8.2kg at time of surgery. The average time
taken for the Plastibell to fall off after circumcision for babies under 3 months was
8.7 days; this period gradually increased to 16.8 days for children over 5 years of
age. The overall complication rate was 7.4%. Plastibell impaction was the
commonest complication, encountered after 6.1% of procedures, and was managed
by cutting the Plastibell. The impaction rate was only 2.3% for babies under 3
months, but gradually increased to 26.9% for children over 5 years.
CONCLUSION: The time taken by the Plastibell to fall off spontaneously as well
as the Plastibell impaction rate increases gradually with age. In view of the overall
safety, comfort and absence of any long-term complication, this procedure justifies
recommendation in all children aged under 1 year, but its use is debatable in older
children.
Latest
News
Glossary & Considering Styles &
Anatomy Circumcision? Results
Preferences
Femcirc
Rites &
Circumcision
&
and
Traditions and the Law
Experiences
FGM
History of Photography Academic
Site
Circumcision
advice
Corner
Map
Mogen clamp
Instruments
&
Techniques
Statistical
Surveys
Resources
elsewhere
64
The Mogen clamp, one of the three most common circumcision devices, was
invented by Rabbi Harry Bronstein in 1954.[1] It has two flat blades that open
approximately 3 mm.[2] The name "Mogen clamp" is a general term for a style of
clamp; there are several different manufacturers of specific models.[citation needed]
History and prevalence
Rabbi Harry Bronstein, a mohel from Brooklyn, invented the Mogen clamp in
1954. The name "Mogen" was derived from the Hebrew word ( magen), which
means shield. Bronstein hoped to standardize circumcision equipment for mohels
and doctors.[1] Medical literature reports that the Mogen clamp is (probably) the
third most popular circumcision clamp (after Plastibell and Gomco) used by
medical practitioners in hospitals.[3]
Procedure
The hospital circumcision procedure with the Mogen clamp is as follows:
1. Apply local anesthetic
2. Use hemostats to draw the foreskin forward
3. Break any adhesions from the foreskin to the glans penis
4. Place the Mogen clamp over the foreskin following the angle of the corona,
ensuring the glans is not trapped
5. Use the Mogen clamp arm to close the clamp, crushing the foreskin along a
line that is 1mm wide
6. Excise the foreskin distal to the clamp
7. Release the clamp arm and remove the clamp
8. Liberate the glans by pulling the crush line apart
9. Bandage[4][5]
The hospital procedure usually takes three to four minutes and is virtually
bloodless.[5]
65
Newborn post-procedure care
Remove the bandage 48 hours after the procedure
Clean the penis by washing gently with water several times per day[6]
Advantages
Fastest:[3] Procedure with Mogen clamp has been found to be from 2.5
times[7] to over ten times[8] faster than with Gomco clamp and almost two
times faster than with the PlastiBell technique[9]
Preferred by hospital residents and interns vs. PlastiBell in one institution in
San Francisco [9]
Does not leave a foreign body at the circumcision site vs. Plastibell [5]
Least likely to lead to infection[10]
Allows full visualization of exactly how much foreskin to remove[3]
Disadvantages
Device does not directly protect the glans during the procedure[5]
It is not possible to remove as much inner foreskin as with the Gomco clamp
The glans is not visualized before removal of the foreskin[3]
Complications specific to the Mogen clamp
A 1984 study of 313 circumcisions using the Mogen clamp states "Circumcision
using the Mogen clamp is a simple quick, and safe procedure." The study showed
that the "complication rate was low (1.6%)."[11]
66
If the Mogen clamp is placed inappropriately,[12] or is otherwise used in a way
outside the manufacturer's specifications,[13] injury to or removal of a portion of the
glans penis is possible; several cases of this occurring have been reported.[3][12][14]
Lawsuits
A Massachusetts lawsuit regarding a circumcision performed using Mogen
Circumcision Instruments' clamp resulted in a $7.5 million judgement against
Mogen Circumcision Instruments of New York in 2007. This judgment caused
Mogen to go into default.[15]
In a case in which 85% of a child's glans penis was accidentally amputated, and
could not be reattached, a lawsuit was filed against Miltex Inc., Miltex Inc.'s parent
company Integra Life Sciences Holding Corp., and the doctor who performed the
circumcision. Miltex Inc. and Integra Life Sciences Holding Corp. were ordered to
pay the child and his mother $4.6 million. The lawsuit against the doctor was
dismissed.[1][16][17]
References
1.
2.
Molly Hennessy-Fiske (2011-09-26). "Injuries linked to circumcision clamps".
Los Angeles Times.
Ellsworth, Pamela et al. (2012-02-08). "Circumcision Devices". eMedicine.
3.
Strimling, BS (1996). "Partial amputation of glans penis during Mogen clamp
circumcision". Pediatrics 97 (6 Pt 1): 9067. PMID 8657537.
4.
Reynolds, RD (1996). "Use of the Mogen clamp for neonatal circumcision".
American family physician 54 (1): 17782. PMID 8677833.
5.
Dr. Brendan Duterte, performing physician; Janelle Aby, MD, producer.
Circumcision -- Mogen Technique. Stanford School of Medicine.
6.
"Newborn Circumcision Information". Kaiser Permanente. p. 2. Retrieved April
30, 2012.
7.
Kurtis, P. S.; Desilva, H. N.; Bernstein, B. A.; Malakh, L.; Schechter, N. L.
(1999). "A Comparison of the Mogen and Gomco Clamps in Combination with Dorsal
Penile Nerve Block in Minimizing the Pain of Neonatal Circumcision". Pediatrics 103
(2): e23. doi:10.1542/peds.103.2.e23. PMID 9925869.
67
8.
"Less Painful Newborn Circumcision". Harvard Medical School Family Health
Guide. June 2000. Retrieved April 30, 2012.
9.
Taeusch, H William; Martinez, Alma M; Partridge, J Colin; Sniderman, Susan;
Armstrong-Wells, Jennifer; Fuentes-Afflick, Elena (2002). "Pain During Mogen or
PlastiBell Circumcision". Journal of Perinatology 22 (3): 2148.
doi:10.1038/sj.jp.7210653. PMID 11948384.
10.
By Healthwise Staff, reviewed by Adam Husney, MD and Peter Anderson, MD,
FRCS(C) - Pediatric Urology (January 29, 2010). "Mogen clamp for circumcision".
WebMD. Retrieved April 30, 2012.
11.
Kaweblum, YA; Press, S; Kogan, L; Levine, M; Kaweblum, M (1984).
"Circumcision using the Mogen clamp". Clinical pediatrics 23 (12): 67982.
doi:10.1177/000992288402301204. PMID 6499347.
12.
"Complications of Circumcision". Stanford School of Medicine -- Department of
Pediatrics. Retrieved April 30, 2012.
13.
David W. Feigal, Jr., MD, MPH (August 29, 2000). "Potential for Injury from
Circumcision Clamps". FDA. Retrieved April 30, 2012.
14.
Patel, HI; Moriarty, KP; Brisson, PA; Feins, NR (2001). "Genitourinary injuries in
the newborn". Journal of pediatric surgery 36 (1): 2359. doi:10.1053/jpsu.2001.20062.
PMID 11150473.
15.
Molly Hennessy-Fiske (September 26, 2011). "Injuries linked to circumcision
clamps". Retrieved Jul 30, 2012.
16.
"$4.6M Settlement in Botched Circumcision Lawsuit My Fox LA, Published July
18, 2011
17.
Boy's Family To Receive $4.6M For Botched Circumcision CBS Los Angeles,
Published July 18, 2011
Surgical instruments
Scalpels
Laser scalpel
RF knife
Dissecting
68
Surgica
l
scissors
:
Lancets
Liston knife
Catlin
Von Graefe knife
Bandage scissors
Mayo scissors
Metzenbaum scissors
Tenotomy scissors
Rongeur
Curette
Osteotome
Drill bits
Rasps
Trocars
Drills
Dermatomes
Other:
Grasping (forceps)
Bulldogs forceps
Hemostat
Obstetric
69
Vulsellum
Tenaculum
Debakey forceps
Foerster clamp
Hemostat
Pennington clamp
Aortic cross-clamp
Gomco clamp
Allis clamp
Retractors: Senn retractor
Rib spreader
Clamping
Retracting/viewin
g
Accessory/other
Dilators
Specula
Fiber optic endoscopes
Head mirror
Yankauer suction tip
rulers and calipers
Examination/prep:
Suction:
Irrigation and injection needles
Measurement devices:
70
Jackson-Pratt drain
Penrose drain
Surgical staplers
Periodontal probe
Surgical suture
Drain:
Other:
This page was last modified on 10 April 2014 at 04:29.
Circumcision clamp
A circumcision clamp is a device which is used specifically for performing
circumcision. Some clamps may only be used by infants, young children, or adults.
Some circumcision clamps are disposable. Circumcision clamps for both males and
females are available on the market.
Types
Alisklamp[1]
Circumplast[2]
Gomco clamp (Trademark held by Allied Healthcare Products, Inc.)[3]
Harris clamp (patented 1933)[4]
Ismail clamp[5]
Kantor clamp[citation needed]
71
Leff clamp[citation needed]
Maryan clamp[6]
Mogen clamp
Nutech Clamp[citation needed]
Rathmann clamp (for females)[7]
RapideClamp[8]
Sheldon clamp[9]
Smart Klamp[10]
Tara KLamp (single-use disposable)[11]
Turner clamp[12]
Winkelmann clamp
References
1.
"About alisklamp". Retrieved April 18, 2012.
2.
"About Circumplast". Retrieved Sep 9, 2013.
3.
"Gomco Circumcision Clamps". Retrieved April 18, 2012.
4.
"Patent 1918700". Retrieved April 18, 2012.
5.
"Ismail Clamp". Retrieved April 18, 2012.
6.
Maryan, HO (1954). "Maryan's improved bloodless circumcision clamp".
American journal of obstetrics and gynecology 67 (2): 4426. PMID 13124427.
7.
Rathmann, WG (1959). "Female circumcision, indications and a new technique".
GP 20: 11520. PMID 14436410.
8.
"About RapideClamp". Retrieved Nov 29, 2013.
72
9.
Sheldon, D (1953). "Circumcision clamp". American journal of obstetrics and
gynecology 65 (3): 675. PMID 13030606.
10.
"510(K) Summary - PrePex". Retrieved April 18, 2012.
11.
"Tara KLamp". Retrieved April 18, 2012.
12.
US patent 2601470, Turner, John J, "Circumcision clamp", issued June 24, 1952
This page was last modified on 22 February 2014 at 20:57.
Vous aimerez peut-être aussi
- All You Need To Know About SwimmingDocument10 pagesAll You Need To Know About SwimmingHumaira AhmadPas encore d'évaluation
- The Army ValuesDocument10 pagesThe Army ValuesMylesPas encore d'évaluation
- Organizational Psychology Case Writing FormatDocument4 pagesOrganizational Psychology Case Writing Format3Idiots MediaPas encore d'évaluation
- Remaining Awake Through A Great RevolutionDocument15 pagesRemaining Awake Through A Great RevolutionRobert Bui100% (1)
- PACO507D01 ComparisonPaper2 TevisDocument10 pagesPACO507D01 ComparisonPaper2 TevisRob Tevis100% (3)
- 2020 White Paper Series Resetting The World With Wellness RevisedDocument84 pages2020 White Paper Series Resetting The World With Wellness Revisedreachss990100% (1)
- Gender Bias in Psychological ResearchDocument11 pagesGender Bias in Psychological ResearchRangothri Sreenivasa Subramanyam100% (2)
- (PIECE) Building Happiness, Resilience and Motivation in Adolescents: A Positive Psychology Curriculum For Well-BeingDocument60 pages(PIECE) Building Happiness, Resilience and Motivation in Adolescents: A Positive Psychology Curriculum For Well-BeingGiorgi DograshviliPas encore d'évaluation
- Lesson StudyDocument35 pagesLesson StudyEnan LimPas encore d'évaluation
- Solution Manual For Psychology For Living Adjustment, Growth, and Behavior Today 11Document16 pagesSolution Manual For Psychology For Living Adjustment, Growth, and Behavior Today 11David50% (2)
- Schizotypal Personality DisorderDocument3 pagesSchizotypal Personality DisorderjoycePas encore d'évaluation
- Asperger's Syndrome 1Document9 pagesAsperger's Syndrome 1api-303293059Pas encore d'évaluation
- Abortion Abortion Is The Termination of A Pregnancy by The Removal or Expulsion From The Uterus of A Fetus or EmbryoDocument11 pagesAbortion Abortion Is The Termination of A Pregnancy by The Removal or Expulsion From The Uterus of A Fetus or EmbryoJennifer CalicaPas encore d'évaluation
- Dilation and CurettageDocument4 pagesDilation and CurettageMary Grace MasPas encore d'évaluation
- Https:emedicine Medscape Com:article:2047080-PrintDocument5 pagesHttps:emedicine Medscape Com:article:2047080-Printmiss beePas encore d'évaluation
- Abortion Assignment Legal AspectDocument57 pagesAbortion Assignment Legal AspectDelphy VarghesePas encore d'évaluation
- AbortionDocument20 pagesAbortionJan Louie GatilloPas encore d'évaluation
- Birth ControlDocument11 pagesBirth ControljabezPas encore d'évaluation
- AbortionDocument57 pagesAbortionThanga Durai100% (1)
- Neonatal Child MC UNAIDSDocument108 pagesNeonatal Child MC UNAIDSgwamakaPas encore d'évaluation
- YULIYANTODocument5 pagesYULIYANTOadehendriePas encore d'évaluation
- AbortionDocument18 pagesAbortionfadhli-bin-hj-ahmad-3390Pas encore d'évaluation
- Abortion Nt3aDocument15 pagesAbortion Nt3aanon-220635Pas encore d'évaluation
- Induced AbortionDocument17 pagesInduced AbortionMwenemutapa FernandoPas encore d'évaluation
- Consenso Buenas Practicas Anticoncepción Intrauterina en FranciaDocument10 pagesConsenso Buenas Practicas Anticoncepción Intrauterina en FranciaJuly López LeitonPas encore d'évaluation
- BioethicsDocument4 pagesBioethicschristianashleye7Pas encore d'évaluation
- Participate IN Various Programmes VasectomyDocument6 pagesParticipate IN Various Programmes Vasectomyvenkat krishnanPas encore d'évaluation
- Awareness and Utilization of Emergency Contraceptives Among Female Nursing Students at KIU, Western Campus, Bushenyi DistrictDocument13 pagesAwareness and Utilization of Emergency Contraceptives Among Female Nursing Students at KIU, Western Campus, Bushenyi DistrictKIU PUBLICATION AND EXTENSIONPas encore d'évaluation
- Amnio ReductionDocument5 pagesAmnio ReductionNovhy Ganggut100% (1)
- Diverse Definitions of Prolonged Labour and Its Consequences With Sometimes Subsequent Inappropriate TreatmentDocument11 pagesDiverse Definitions of Prolonged Labour and Its Consequences With Sometimes Subsequent Inappropriate TreatmentrosaliaPas encore d'évaluation
- Types: Ortion Is The Termination of ADocument17 pagesTypes: Ortion Is The Termination of AedenpearlcastilloPas encore d'évaluation
- Circumcision in Baby BoysDocument6 pagesCircumcision in Baby BoysJbl2328Pas encore d'évaluation
- Male - Contraceptive WikiDocument11 pagesMale - Contraceptive WikiUnggul YudhaPas encore d'évaluation
- Abortion: Continuing Education ActivityDocument12 pagesAbortion: Continuing Education ActivityAffah MustafaPas encore d'évaluation
- The Long Acting Reversible Contraceptive (LARC) GuidelineDocument20 pagesThe Long Acting Reversible Contraceptive (LARC) GuidelineYinlerLeePas encore d'évaluation
- Ajol File Journals - 421 - Articles - 95078 - Submission - Proof - 95078 5017 245193 1 10 20131010Document7 pagesAjol File Journals - 421 - Articles - 95078 - Submission - Proof - 95078 5017 245193 1 10 20131010Sunat Khitan SoloPas encore d'évaluation
- KodefDocument45 pagesKodefWann FarhannaPas encore d'évaluation
- Birth - Control WikiDocument36 pagesBirth - Control WikiUnggul YudhaPas encore d'évaluation
- Episiotomy and Repair: BackgroundDocument4 pagesEpisiotomy and Repair: Backgroundtongam siahaanPas encore d'évaluation
- Postoperative Peritoneal Adhesions in Adults and Their Prevention - UpToDateDocument17 pagesPostoperative Peritoneal Adhesions in Adults and Their Prevention - UpToDateDesak PramestiPas encore d'évaluation
- Surgical Uterus Gynecologist Fundus Cervix: Types of HysterectomyDocument3 pagesSurgical Uterus Gynecologist Fundus Cervix: Types of HysterectomyMary Ann LunnayPas encore d'évaluation
- Physical Therapy Management (Current Best Evidence) : "Facilitating Cell"Document1 pagePhysical Therapy Management (Current Best Evidence) : "Facilitating Cell"Robert MariasiPas encore d'évaluation
- Neonatal CIrcumcision For HIV Prevention (FINAL)Document14 pagesNeonatal CIrcumcision For HIV Prevention (FINAL)Carol WIngfieldPas encore d'évaluation
- Emergency Contraception in South Africa A Literature ReviewDocument7 pagesEmergency Contraception in South Africa A Literature Reviewgw11pm8hPas encore d'évaluation
- Restricted Episiotomy and Perineal Repair: By: Surakshya Bhattarai WHD, MN 1 Year BHNC, Nams Roll No: 10Document70 pagesRestricted Episiotomy and Perineal Repair: By: Surakshya Bhattarai WHD, MN 1 Year BHNC, Nams Roll No: 10Surakshya BhattaraiPas encore d'évaluation
- Chapter 4 - Reproductive Health NotesDocument5 pagesChapter 4 - Reproductive Health NotesShagufta100% (1)
- Misoprostol For Treatment of Incomplete AbortionDocument32 pagesMisoprostol For Treatment of Incomplete AbortionAde Vella Feliza RaufPas encore d'évaluation
- Appendicitis: QuestionsDocument9 pagesAppendicitis: QuestionsPaúl AndradePas encore d'évaluation
- Management of Intra-Abdominally Translocated Contraceptive Devices, Is Surgery The Only Way To Treat This Problem?Document8 pagesManagement of Intra-Abdominally Translocated Contraceptive Devices, Is Surgery The Only Way To Treat This Problem?Rezky amalia basirPas encore d'évaluation
- Uncoiling The Tightening Obesity SpiralDocument5 pagesUncoiling The Tightening Obesity SpiralasclepiuspdfsPas encore d'évaluation
- 2019 Article 2376Document13 pages2019 Article 2376ade lydia br.siregarPas encore d'évaluation
- 18 AbortionDocument1 page18 AbortionSasa NovkovicPas encore d'évaluation
- Incidence and Factors Associated With Early Adverse Outcomes of Testicular Torsion Among Patients With Acute Scrotum in Western UgandaDocument17 pagesIncidence and Factors Associated With Early Adverse Outcomes of Testicular Torsion Among Patients With Acute Scrotum in Western UgandaKIU PUBLICATION AND EXTENSIONPas encore d'évaluation
- AbortionDocument19 pagesAbortionjeza_nolasco100% (2)
- Operative Management of Cryptorchidism Guidelines and RealityDocument9 pagesOperative Management of Cryptorchidism Guidelines and RealityRichard QiuPas encore d'évaluation
- 2guia en EmbarazoDocument13 pages2guia en EmbarazoCecilia Quispe JaureguiPas encore d'évaluation
- Anesthesia For Ivf PDFDocument11 pagesAnesthesia For Ivf PDFdr raghav guptaPas encore d'évaluation
- Birth Control - WikipediaDocument280 pagesBirth Control - Wikipediaishantmarkam24Pas encore d'évaluation
- Notes Chap 04Document8 pagesNotes Chap 04umamahfarooq75Pas encore d'évaluation
- A Potential Siddha Mineral Drug Pavala ParpamDocument8 pagesA Potential Siddha Mineral Drug Pavala Parpamjmanuel108yahoo.co.ukPas encore d'évaluation
- ST Peter, 2014, BI-Annual DR-TB Performance Report To AAHB, 15 March 2022. JohnDocument43 pagesST Peter, 2014, BI-Annual DR-TB Performance Report To AAHB, 15 March 2022. Johnሀይደር ዶ.ርPas encore d'évaluation
- Nursing Care Plan Pott's DiseaseDocument2 pagesNursing Care Plan Pott's Diseasederic95% (21)
- Neurology & Pupils (No 467)Document231 pagesNeurology & Pupils (No 467)Mohamed GaberPas encore d'évaluation
- Caffein Intox PDFDocument3 pagesCaffein Intox PDFSejahtera SurbaktiPas encore d'évaluation
- Seatone InfoDocument7 pagesSeatone InfoJugal ShahPas encore d'évaluation
- Maret 18 PDFDocument178 pagesMaret 18 PDFAnonymous vLgCd0U7Pas encore d'évaluation
- Ultimate Guide To Surviving in The WildDocument175 pagesUltimate Guide To Surviving in The WildSal Ot100% (1)
- Science 6 Endocrine SystemDocument39 pagesScience 6 Endocrine Systemcharmaine_olivia_1100% (1)
- Nursing Process Fon Chap 1Document20 pagesNursing Process Fon Chap 1Saqlain M.Pas encore d'évaluation
- Unknown Bacteria Lab ReportDocument13 pagesUnknown Bacteria Lab Reportapi-529628802Pas encore d'évaluation
- Fever of Unknown OriginDocument26 pagesFever of Unknown OriginFiona Yona Sitali100% (1)
- Lecture 32 - Nutritional DisordersDocument43 pagesLecture 32 - Nutritional Disordersapi-3703352100% (3)
- Final Coaching NP4 Set 1Document13 pagesFinal Coaching NP4 Set 1STEFFI GABRIELLE GOLEZPas encore d'évaluation
- Access To Primary Health Care Services For Indigenous PeopleDocument9 pagesAccess To Primary Health Care Services For Indigenous PeopleLawrence Ryan DaugPas encore d'évaluation
- Burdens of Family Caregiving at The End of LifeDocument6 pagesBurdens of Family Caregiving at The End of LifeNurul ShahirahPas encore d'évaluation
- Feed Additives, Antibodies, Poultry Vaccines 2023.3Document6 pagesFeed Additives, Antibodies, Poultry Vaccines 2023.3Bruce YangPas encore d'évaluation
- Home Quarantine Compliance 2022 1Document1 pageHome Quarantine Compliance 2022 1Puting KahoyPas encore d'évaluation
- Illich 1982Document5 pagesIllich 1982CsscamposPas encore d'évaluation
- Critical Care of Children With Heart Disease 2010Document735 pagesCritical Care of Children With Heart Disease 2010Haikel Mhamed100% (1)
- Group 4 Environmental Pollution and Impacts On Public HealthDocument10 pagesGroup 4 Environmental Pollution and Impacts On Public HealthBen KuPas encore d'évaluation
- Contact Lens Complications and ManagementDocument10 pagesContact Lens Complications and Managementstrawberry8832850% (2)
- Multiple Pulp Polyps Associated With Deciduous TeethDocument4 pagesMultiple Pulp Polyps Associated With Deciduous TeethJea Ayu YogatamaPas encore d'évaluation
- Structural Organisation in Animals - IIDocument70 pagesStructural Organisation in Animals - IIMay HarukaPas encore d'évaluation
- Breast Cancer Staging SystemDocument4 pagesBreast Cancer Staging SystemGabriella PatriciaPas encore d'évaluation
- Narcissistic MothersDocument11 pagesNarcissistic MothersSeraph100% (7)
- CystsDocument5 pagesCystsranindita maulyaPas encore d'évaluation
- Full Download Test Bank Health Assessment For Nursing Practice 6th Edition Wilson PDF Full ChapterDocument36 pagesFull Download Test Bank Health Assessment For Nursing Practice 6th Edition Wilson PDF Full Chapterbeatermany.imubd2100% (19)
- Theory ApplicationDocument38 pagesTheory ApplicationAnusha VerghesePas encore d'évaluation
- Robertslevc2015 - Auditory AgnosiaDocument15 pagesRobertslevc2015 - Auditory AgnosiaErick SolisPas encore d'évaluation