Académique Documents
Professionnel Documents
Culture Documents
AGREE Reporting Checklist 2016
Transféré par
Jimmy ZhangCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
AGREE Reporting Checklist 2016
Transféré par
Jimmy ZhangDroits d'auteur :
Formats disponibles
AGREE Reporting Checklist
2016
This checklist is intended to guide the reporting of clinical practice guidelines.
CHECKLIST ITEM AND DESCRIPTION
REPORTING CRITERIA
Page
#
DOMAIN 1: SCOPE AND PURPOSE
1. OBJECTIVES
Report the overall objective(s) of the
guideline. The expected health benefits
from the guideline are to be specific to the
clinical problem or health topic.
2. QUESTIONS
Report the health question(s) covered by
the guideline, particularly for the key
recommendations.
3. POPULATION
Describe the population (i.e., patients,
public, etc.) to whom the guideline is meant
to apply.
Health intent(s) (i.e., prevention, screening,
diagnosis, treatment, etc.)
Expected benefit(s) or outcome(s)
Target(s) (e.g., patient population, society)
Target population
Intervention(s) or exposure(s)
Comparisons (if appropriate)
Outcome(s)
Health care setting or context
Target population, sex and age
Clinical condition (if relevant)
Severity/stage of disease (if relevant)
Comorbidities (if relevant)
Excluded populations (if relevant)
DOMAIN 2: STAKEHOLDER INVOLVEMENT
4. GROUP MEMBERSHIP
Report all individuals who were involved in
the development process. This may include
members of the steering group, the
research team involved in selecting and
reviewing/rating the evidence and
individuals involved in formulating the final
recommendations.
5. TARGET POPULATION
PREFERENCES AND VIEWS
Report how the views and preferences of
the target population were
sought/considered and what the resulting
outcomes were.
6. TARGET USERS
Report the target (or intended) users of the
guideline.
Name of participant
Discipline/content expertise (e.g., neurosurgeon,
methodologist)
Institution (e.g., St. Peters hospital)
Geographical location (e.g., Seattle, WA)
A description of the members role in the
guideline development group
Statement of type of strategy used to capture
patients/publics views and preferences (e.g.,
participation in the guideline development group,
literature review of values and preferences)
Methods by which preferences and views were
sought (e.g., evidence from literature, surveys,
focus groups)
Outcomes/information gathered on patient/public
information
How the information gathered was used to inform
the guideline development process and/or
formation of the recommendations
The intended guideline audience (e.g.
specialists, family physicians, patients, clinical or
institutional leaders/administrators)
How the guideline may be used by its target
audience (e.g., to inform clinical decisions, to
inform policy, to inform standards of care)
DOMAIN 3: RIGOUR OF DEVELOPMENT
7. SEARCH METHODS
Report details of the strategy used to
search for evidence.
8. EVIDENCE SELECTION CRITERIA
Report the criteria used to select (i.e.,
include and exclude) the evidence. Provide
rationale, where appropriate.
9. STRENGTHS & LIMITATIONS OF THE
EVIDENCE
Describe the strengths and limitations of
the evidence. Consider from the
perspective of the individual studies and
the body of evidence aggregated across all
the studies. Tools exist that can facilitate
the reporting of this concept.
10. FORMULATION OF
RECOMMENDATIONS
Describe the methods used to formulate
the recommendations and how final
decisions were reached. Specify any areas
of disagreement and the methods used to
resolve them.
11. CONSIDERATION OF BENEFITS AND
HARMS
Report the health benefits, side effects,
and risks that were considered when
formulating the recommendations.
12. LINK BETWEEN
RECOMMENDATIONS AND EVIDENCE
Describe the explicit link between the
recommendations and the evidence on
which they are based.
Named electronic database(s) or evidence
source(s) where the search was performed (e.g.,
MEDLINE, EMBASE, PsychINFO, CINAHL)
Time periods searched (e.g., January 1, 2004 to
March 31, 2008)
Search terms used (e.g., text words, indexing
terms, subheadings)
Full search strategy included (e.g., possibly
located in appendix)
Target population (patient, public, etc.)
characteristics
Study design
Comparisons (if relevant)
Outcomes
Language (if relevant)
Context (if relevant)
Study design(s) included in body of evidence
Study methodology limitations (sampling,
blinding, allocation concealment, analytical
methods)
Appropriateness/relevance of primary and
secondary outcomes considered
Consistency of results across studies
Direction of results across studies
Magnitude of benefit versus magnitude of harm
Applicability to practice context
Recommendation development process (e.g.,
steps used in modified Delphi technique, voting
procedures that were considered)
Outcomes of the recommendation development
process (e.g., extent to which consensus was
reached using modified Delphi technique,
outcome of voting procedures)
How the process influenced the
recommendations (e.g., results of Delphi
technique influence final recommendation,
alignment with recommendations and the final
vote)
Supporting data and report of benefits
Supporting data and report of harms/side
effects/risks
Reporting of the balance/trade-off between
benefits and harms/side effects/risks
Recommendations reflect considerations of both
benefits and harms/side effects/risks
How the guideline development group linked and
used the evidence to inform recommendations
Link between each recommendation and key
evidence (text description and/or reference list)
Link between recommendations and evidence
summaries and/or evidence tables in the results
section of the guideline
13. EXTERNAL REVIEW
Report the methodology used to conduct
the external review.
14. UPDATING PROCEDURE
Describe the procedure for updating the
guideline.
Purpose and intent of the external review (e.g., to
improve quality, gather feedback on draft
recommendations, assess applicability and
feasibility, disseminate evidence)
Methods taken to undertake the external review
(e.g., rating scale, open-ended questions)
Description of the external reviewers (e.g.,
number, type of reviewers, affiliations)
Outcomes/information gathered from the external
review (e.g., summary of key findings)
How the information gathered was used to inform
the guideline development process and/or
formation of the recommendations (e.g.,
guideline panel considered results of review in
forming final recommendations)
A statement that the guideline will be updated
Explicit time interval or explicit criteria to guide
decisions about when an update will occur
Methodology for the updating procedure
DOMAIN 4: CLARITY OF PRESENTATION
15. SPECIFIC AND UNAMBIGUOUS
RECOMMENDATIONS
Describe which options are appropriate in
which situations and in which population
groups, as informed by the body of
evidence.
16. MANAGEMENT OPTIONS
Describe the different options for managing
the condition or health issue.
17. IDENTIFIABLE KEY
RECOMMENDATIONS
Present the key recommendations so that
they are easy to identify.
A statement of the recommended action
Intent or purpose of the recommended action
(e.g., to improve quality of life, to decrease side
effects)
Relevant population (e.g., patients, public)
Caveats or qualifying statements, if relevant
(e.g., patients or conditions for whom the
recommendations would not apply)
If there is uncertainty about the best care
option(s), the uncertainty should be stated in the
guideline
Description of management options
Population or clinical situation most appropriate
to each option
Recommendations in a summarized box, typed
in bold, underlined, or presented as flow charts
or algorithms
Specific recommendations grouped together in
one section
DOMAIN 5: APPLICABILITY
18. FACILITATORS AND BARRIERS TO
APPLICATION
Describe the facilitators and barriers to the
guidelines application.
Types of facilitators and barriers that were
considered
Methods by which information regarding the
facilitators and barriers to implementing
recommendations were sought (e.g., feedback
from key stakeholders, pilot testing of guidelines
before widespread implementation)
Information/description of the types of facilitators
and barriers that emerged from the inquiry (e.g.,
practitioners have the skills to deliver the
recommended care, sufficient equipment is not
available to ensure all eligible members of the
19. IMPLEMENTATION ADVICE/TOOLS
Provide advice and/or tools on how the
recommendations can be applied in
practice.
20. RESOURCE IMPLICATIONS
Describe any potential resource
implications of applying the
recommendations.
21. MONITORING/ AUDITING CRITERIA
Provide monitoring and/or auditing criteria
to measure the application of guideline
recommendations.
population receive mammography)
How the information influenced the guideline
development process and/or formation of the
recommendations
Additional materials to support the
implementation of the guideline in practice. For
example:
o Guideline summary documents
o Links to check lists, algorithms
o Links to how-to manuals
o Solutions linked to barrier analysis (see Item
18)
o Tools to capitalize on guideline facilitators
(see Item 18)
o Outcome of pilot test and lessons learned
Types of cost information that were considered
(e.g., economic evaluations, drug acquisition
costs)
Methods by which the cost information was
sought (e.g., a health economist was part of the
guideline development panel, use of health
technology assessments for specific drugs, etc.)
Information/description of the cost information
that emerged from the inquiry (e.g., specific drug
acquisition costs per treatment course)
How the information gathered was used to inform
the guideline development process and/or
formation of the recommendations
Criteria to assess guideline implementation or
adherence to recommendations
Criteria for assessing impact of implementing the
recommendations
Advice on the frequency and interval of
measurement
Operational definitions of how the criteria should
be measured
DOMAIN 6: EDITORIAL INDEPENDENCE
22. FUNDING BODY
Report the funding bodys influence on the
content of the guideline.
23. COMPETING INTERESTS
Provide an explicit statement that all group
members have declared whether they have
any competing interests.
The name of the funding body or source of
funding (or explicit statement of no funding)
A statement that the funding body did not
influence the content of the guideline
Types of competing interests considered
Methods by which potential competing interests
were sought
A description of the competing interests
How the competing interests influenced the
guideline process and development of
recommendations
From:
Brouwers MC, Kerkvliet K, Spithoff K, on behalf of the AGREE Next Steps Consortium. The AGREE Reporting Checklist: a tool to
improve reporting of clinical practice guidelines. BMJ 2016;352:i1152. doi: 10.1136/bmj.i1152.
For more information about the AGREE Reporting Checklist, please visit the AGREE Enterprise website at www.agreetrust.org.
Vous aimerez peut-être aussi
- A Practical Guide To Behavioral Research Tools and Techniques - Capítulo 01 PDFDocument9 pagesA Practical Guide To Behavioral Research Tools and Techniques - Capítulo 01 PDFdani_g_1987Pas encore d'évaluation
- Ebook PDF Theories of Personality 9th Edition by Jess Feist PDFDocument41 pagesEbook PDF Theories of Personality 9th Edition by Jess Feist PDFflossie.thompson26497% (29)
- Mukesh Chawla Mukesh ChawlaDocument62 pagesMukesh Chawla Mukesh Chawlajaideepjd06Pas encore d'évaluation
- Improving Healthcare Through Advocacy: A Guide for the Health and Helping ProfessionsD'EverandImproving Healthcare Through Advocacy: A Guide for the Health and Helping ProfessionsPas encore d'évaluation
- Patient ID and Safety PolicyDocument3 pagesPatient ID and Safety PolicyEva JaworskiPas encore d'évaluation
- FNMAP UDocument398 pagesFNMAP UAlicia Almeda-BaldiviaPas encore d'évaluation
- Enhancing Nurses Pain Assessment To Improve.11Document2 pagesEnhancing Nurses Pain Assessment To Improve.11Na d'Nazaie CodePas encore d'évaluation
- Standard of Service of Physiotherapy Final Draft.Document24 pagesStandard of Service of Physiotherapy Final Draft.Moges Baye100% (2)
- Practice Marketing Plan FinalDocument14 pagesPractice Marketing Plan Finalapi-317365152Pas encore d'évaluation
- Professionalism Core Values Self AssessmentDocument12 pagesProfessionalism Core Values Self Assessmentcait_s_georgePas encore d'évaluation
- What Is A PICO QuestionDocument3 pagesWhat Is A PICO QuestionBoid Gerodias100% (2)
- High Risk Consent Form: Doctor-In-Charge / Principal Surgeon / Principal InterventionistDocument5 pagesHigh Risk Consent Form: Doctor-In-Charge / Principal Surgeon / Principal InterventionistDrPraveen SharmaPas encore d'évaluation
- Quality Improvement PlanDocument49 pagesQuality Improvement PlanRob Willestone100% (1)
- Physiotherapy Manual GuidelinesDocument78 pagesPhysiotherapy Manual GuidelinesSaad ShafiqPas encore d'évaluation
- BCM-MS TPDocument2 pagesBCM-MS TPabdullahazrezarPas encore d'évaluation
- APTA Professionalism Core Values Self AssessmentDocument11 pagesAPTA Professionalism Core Values Self AssessmentJPPas encore d'évaluation
- JCI Standards Only 6th Ed HospitalDocument12 pagesJCI Standards Only 6th Ed HospitalHengkyPas encore d'évaluation
- Physical Therapy Documentation Templates PDFDocument6 pagesPhysical Therapy Documentation Templates PDFNellPas encore d'évaluation
- Home Care CompetencyDocument54 pagesHome Care Competencyapi-3002188600% (1)
- Quick Reference Guide-04Dec2019Document46 pagesQuick Reference Guide-04Dec2019adiangriawanPas encore d'évaluation
- Physiotherapy Manual of OperationsDocument20 pagesPhysiotherapy Manual of OperationsHbk RajneeshPas encore d'évaluation
- The Value of Healthcare AdministrationDocument3 pagesThe Value of Healthcare AdministrationKrizzella ShainaPas encore d'évaluation
- Check ListDocument44 pagesCheck ListManish KumarPas encore d'évaluation
- OT Code of Ethics 2015Document8 pagesOT Code of Ethics 2015Ays OlartePas encore d'évaluation
- CL489F Physiotherapy Reassessment ReportDocument4 pagesCL489F Physiotherapy Reassessment ReportnaeemullahPas encore d'évaluation
- Hospital Management ServicesDocument22 pagesHospital Management ServicesSpreading KnowledgePas encore d'évaluation
- DEVELOPING PHYSIOTHERAPY LED SHOULDER CLINICS: A PROPOSAL TO ADJUST SCOPE OF PRACTICE BY TENDAYI MUTSOPOTSI Bsc. HPT (Hons) MSc. ORTHO-MEDDocument15 pagesDEVELOPING PHYSIOTHERAPY LED SHOULDER CLINICS: A PROPOSAL TO ADJUST SCOPE OF PRACTICE BY TENDAYI MUTSOPOTSI Bsc. HPT (Hons) MSc. ORTHO-MEDPhysiotherapy Care SpecialistsPas encore d'évaluation
- Global Patient Safety Action Plan 2021-2030Document108 pagesGlobal Patient Safety Action Plan 2021-2030Leia MendesPas encore d'évaluation
- AMA HomeCarePhysiciansDocument74 pagesAMA HomeCarePhysiciansBruna Ortiz100% (1)
- Review of Compliance: Ms Marie Mccann Webber HouseDocument34 pagesReview of Compliance: Ms Marie Mccann Webber HouseSouthern Daily EchoPas encore d'évaluation
- Evidence-Based Practice Fact SheetDocument3 pagesEvidence-Based Practice Fact Sheetmohamedwhatever100% (2)
- Healthcare EthicsDocument30 pagesHealthcare EthicswetzelapulPas encore d'évaluation
- Ethics Medicolegal AspectDocument28 pagesEthics Medicolegal AspectRakesh shahPas encore d'évaluation
- Marketing Mix - The 4 P's of Marketing ExplainedDocument6 pagesMarketing Mix - The 4 P's of Marketing ExplainedDeepak Kalonia JangraPas encore d'évaluation
- Diagnosis and Treatment of Worker-Related Musculoskeletal Disorders of The Upper Extremity OmbroDocument705 pagesDiagnosis and Treatment of Worker-Related Musculoskeletal Disorders of The Upper Extremity OmbroDouglas GarciaPas encore d'évaluation
- Hospital Safety Officer Job DescriptionDocument1 pageHospital Safety Officer Job DescriptionSalvador Morales Obusan100% (1)
- Fall Prevention Guide Around the HomeDocument7 pagesFall Prevention Guide Around the Homepriyarajan007Pas encore d'évaluation
- National Accreditation Board For Hospitals and Healthcare ProvidersDocument104 pagesNational Accreditation Board For Hospitals and Healthcare ProviderssridhartrichyPas encore d'évaluation
- Medical History FormDocument2 pagesMedical History Formvhel05Pas encore d'évaluation
- Quality Control & Quality Improvement: Under SupervisionDocument20 pagesQuality Control & Quality Improvement: Under Supervisionheba abd elazizPas encore d'évaluation
- Patient Safety GoalsDocument59 pagesPatient Safety GoalsHarby Ongbay Abellanosa100% (1)
- Pediatric Physical AssessmentDocument5 pagesPediatric Physical Assessmentilovemaine0% (1)
- IHI Patient Family Experience of Hospital Care White Paper 2011Document34 pagesIHI Patient Family Experience of Hospital Care White Paper 2011Sorina VoicuPas encore d'évaluation
- Manager Interview PaperDocument8 pagesManager Interview Paperapi-301802746100% (2)
- Home Environmental AssessmentDocument2 pagesHome Environmental AssessmentSelvi Puspa SariPas encore d'évaluation
- List Policies and ProceduresDocument3 pagesList Policies and ProceduresJoeren GonzalesPas encore d'évaluation
- Leadership's Role in Quality ManagementDocument17 pagesLeadership's Role in Quality ManagementHadi Mohammed HamedPas encore d'évaluation
- JCI Accredited Apollo Hospitals Offer Quality Healthcare Management CourseDocument2 pagesJCI Accredited Apollo Hospitals Offer Quality Healthcare Management CourseGajendra TodakarPas encore d'évaluation
- Nursing Home Charges by Type & Care CategoryDocument67 pagesNursing Home Charges by Type & Care Categoryalmond2009Pas encore d'évaluation
- Physiotherapy Scope of Practice-Article PDFDocument3 pagesPhysiotherapy Scope of Practice-Article PDFeins_mptPas encore d'évaluation
- EBP: Formulating Clinical QuestionsDocument44 pagesEBP: Formulating Clinical QuestionsDiah agung100% (1)
- Preprocedure Check-In Sign-In Time-Out Sign-OutDocument2 pagesPreprocedure Check-In Sign-In Time-Out Sign-OutSyahri DzikriPas encore d'évaluation
- Patient Safety Organization A Complete Guide - 2020 EditionD'EverandPatient Safety Organization A Complete Guide - 2020 EditionPas encore d'évaluation
- Director Patient Experience in Metropolitan Atlanta GA Resume Stephanie TaylorDocument3 pagesDirector Patient Experience in Metropolitan Atlanta GA Resume Stephanie TaylorStephanie TaylorPas encore d'évaluation
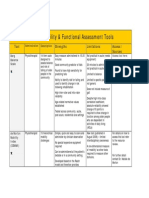
- Assessment Tools for Mobility & Functional IndependenceDocument4 pagesAssessment Tools for Mobility & Functional Independencesonya63265Pas encore d'évaluation
- Critical Appraisal PDFDocument5 pagesCritical Appraisal PDFwahyu nadiPas encore d'évaluation
- Group ProtocolDocument5 pagesGroup Protocolapi-455072421Pas encore d'évaluation
- Accreditation Council For Graduate Medical Education International Glossary of TermsDocument9 pagesAccreditation Council For Graduate Medical Education International Glossary of Termsdelap05Pas encore d'évaluation
- Preceptor Evaluation FormDocument2 pagesPreceptor Evaluation Formjenn1722Pas encore d'évaluation
- Gayatri Kalantri Community Health & RehabilitationDocument25 pagesGayatri Kalantri Community Health & RehabilitationGayatri KalantriPas encore d'évaluation
- Functional Assessment in PhysiotherapyDocument0 pageFunctional Assessment in PhysiotherapyDibyendunarayan BidPas encore d'évaluation
- Case Study 2Document3 pagesCase Study 2JoPaul Prado100% (2)
- Assessment and Management of PainDocument174 pagesAssessment and Management of PainKimkimkim EligioPas encore d'évaluation
- New Molecular Insights Into Inflammatory Bowel Disease Induced DiarrheaDocument12 pagesNew Molecular Insights Into Inflammatory Bowel Disease Induced DiarrheaJimmy ZhangPas encore d'évaluation
- Agree ToolDocument59 pagesAgree ToolCat NganPas encore d'évaluation
- OPDocument7 pagesOPAmishWarlordPas encore d'évaluation
- Agree ToolDocument59 pagesAgree ToolCat NganPas encore d'évaluation
- Proceedings LAMAS 5 2015 Edisi Revisi. Raheni Suhita, Djoko Sulaksono, Kenfitria Diah WDocument27 pagesProceedings LAMAS 5 2015 Edisi Revisi. Raheni Suhita, Djoko Sulaksono, Kenfitria Diah WAdam DamanhuriPas encore d'évaluation
- Talent Management in Malaysian UniversitDocument20 pagesTalent Management in Malaysian Universitحمب محمد نجمدنPas encore d'évaluation
- The Story About Ping Five in A Row GuideDocument5 pagesThe Story About Ping Five in A Row GuideEmPas encore d'évaluation
- HSBC Praise Team Self-Evaluations - Vocal/Instrumental/TechDocument3 pagesHSBC Praise Team Self-Evaluations - Vocal/Instrumental/TechEric Powell100% (2)
- 1890 Pgmedicalcqsecondphaseallotments201920Document60 pages1890 Pgmedicalcqsecondphaseallotments201920krishnaPas encore d'évaluation
- Estimated Time The Activity Is To Be Accomplished) : E.G. 56 HoursDocument9 pagesEstimated Time The Activity Is To Be Accomplished) : E.G. 56 HoursEarl Jeofrey LagarasPas encore d'évaluation
- Buku Prosiding-Lengkap PDFDocument196 pagesBuku Prosiding-Lengkap PDFfirdaPas encore d'évaluation
- Handouts IT of Education CompleteDocument523 pagesHandouts IT of Education CompleteNamtu LewanyPas encore d'évaluation
- Evaluation of English Textbook in Pakistan A Case Study of Punjab Textbook For 9th ClassDocument19 pagesEvaluation of English Textbook in Pakistan A Case Study of Punjab Textbook For 9th ClassMadiha ShehryarPas encore d'évaluation
- Master Thesis Support Vector MachineDocument5 pagesMaster Thesis Support Vector Machinednqjxbz2100% (2)
- Intimate RelationshipDocument3 pagesIntimate RelationshipMelody LiuPas encore d'évaluation
- MCHS 1965 YearbookDocument112 pagesMCHS 1965 YearbookMater Dei Catholic High SchoolPas encore d'évaluation
- Complexity Theory & Systems Theory - Schumacher CollegeDocument2 pagesComplexity Theory & Systems Theory - Schumacher Collegekasiv_8Pas encore d'évaluation
- Q1-M1 Ans (Eapp)Document9 pagesQ1-M1 Ans (Eapp)JD MartinPas encore d'évaluation
- Pancasila Character EducationDocument6 pagesPancasila Character EducationDaniel Prayoga D100% (1)
- Heat and Temperature (Asynchronous Class)Document4 pagesHeat and Temperature (Asynchronous Class)Noemi SalacsacanPas encore d'évaluation
- Non-Verbal Communication: by V P BhagatDocument14 pagesNon-Verbal Communication: by V P BhagatSat SharmaPas encore d'évaluation
- Outside State Colleges Email DetailsDocument84 pagesOutside State Colleges Email Detailsuniquerealestate098Pas encore d'évaluation
- Cable TestingDocument4 pagesCable TestingbinodePas encore d'évaluation
- 1.4 Components of Ethology: InstinctDocument7 pages1.4 Components of Ethology: InstinctAndreea BradPas encore d'évaluation
- Is LINUS truly solving illiteracyDocument10 pagesIs LINUS truly solving illiteracyAlex LimPas encore d'évaluation
- Unit 2 Expressing Like and Dislike A. Spoken Activity Exercise 1Document3 pagesUnit 2 Expressing Like and Dislike A. Spoken Activity Exercise 1Faeruz Nur KhaerunnisaPas encore d'évaluation
- Presentacin Intro Distribucin Por Variables A Taste of The MoonDocument8 pagesPresentacin Intro Distribucin Por Variables A Taste of The MoonClemente TorresPas encore d'évaluation
- Session Plan FBSDocument17 pagesSession Plan FBSorabelle punoPas encore d'évaluation
- Improve Group Project PerformanceDocument15 pagesImprove Group Project PerformanceВаля БоберськаPas encore d'évaluation
- Test English - Prepare For Your English ExamDocument3 pagesTest English - Prepare For Your English ExamDrumsoPas encore d'évaluation
- 9701 w13 QP 35 2 PDFDocument12 pages9701 w13 QP 35 2 PDFNeural Spark Physics CiePas encore d'évaluation