Académique Documents
Professionnel Documents
Culture Documents
Exercise Dose and The Heart
Transféré par
César Ayala GuzmánTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Exercise Dose and The Heart
Transféré par
César Ayala GuzmánDroits d'auteur :
Formats disponibles
CHEST AND ABDOMINAL CONDITIONS
Exercise and the Heart V the Harm
of Too Little and Too Much
Carl J. Lavie, MD1; James H. OKeefe, MD2; and Robert E. Sallis, MD, FACSM3
there is a fallible logic that if some
exercise is good, then more must be
better (18). Certainly there are a substantial number of individuals exercising for many hours and on many
days while regularly competing in long
road races, such as marathons, or long
bicycle and swimming races, such as
triathlons, and even multiday events
(18,27Y30). Although most are of the
belief that participation in high levels
of PA is good for heart health, there
is evolving evidence that a high level of
EEE may be associated with risk of
cardiotoxicity.
In this review, we discuss the evidence
proving the tremendous CV benefit of
regular exercise along with the more recent and evolving evidence that high levels of ET may provide similar or even less overall benefit compared with that
provided by low doses of ET. Additionally, we review the
evidence that high levels of ET may be associated with increased risk of atrial fibrillation (AF), coronary artery
disease (CAD), and malignant ventricular arrhythmias
(VA). Furthermore this evidence suggests that acute bouts
of EEE may lead to cardiac dilatation and dysfunction,
especially on the right side of the heart and ventricular
septum, in turn leading to the release of cardiac biomarkers, such as cardiac troponin and brain natriuretic
peptide (BNP), resulting in VA and increased risk of sudden
cardiac death (SCD).
Abstract
Physical activity and exercise training are underutilized by much of Westernized society, and physical inactivity may be the greatest threat to health
in the 21st century. Many studies have shown a linear relationship between
ones activity level and heart health, leading to the conclusion that if some
exercise is good, more must be better. However, there is evolving evidence that high levels of exercise may produce similar or less overall cardiovascular (CV) benefits compared with those produced by lower doses of
exercise. Very high doses of exercise may be associated with increased risk
of atrial fibrillation, coronary artery disease, and malignant ventricular arrhythmias. These acute bouts of excessive exercise may lead to cardiac
dilatation, cardiac dysfunction, and release of troponin and brain natriuretic
peptide. The effects of too little and too much exercise on the heart are
reviewed in this article, along with recommendations to optimize the dose
of exercise to achieve heart health.
Introduction
Considerable evidence indicates the profound benefits of
physical activity (PA), exercise training (ET), and higher
levels of cardiorespiratory fitness (CRF) on lowering morbidity and mortality from heart disease (11,38,40). Recent
studies have focused on the fact that PA levels do not meet
national guidelines in a substantial percentage of the population in the United States, probably in 50% to 80% of the
population, and most of the world (11,38,40), and physical
inactivity may represent one of the greatest threats to health
in the 21st century (5).
Although excessive endurance exercise (EEE), defined as
ET 9 60 to 90 min per session, is not nearly as prevalent as
low levels of PA, occurring in 2% to 5% of the population,
1
Department of Cardiovascular Diseases, John Ochsner Heart and Vascular
Institute, Ochsner Clinical School, University of Queensland School of Medicine, New Orleans, LA; 2St. Lukes Mid America Heart Institute, University of
Missouri, Kansas City, MO; and 3Department of Family Medicine, Kaiser
Permanente Medical Center, Fontana, CA
Address for correspondence: Carl J. Lavie, MD, Cardiac Rehabilitation,
Exercise Laboratories, John Ochsner Heart and Vascular Institute,
Ochsner Clinical School, University of Queensland School of Medicine,
1514 Jefferson Highway, New Orleans, LA 70121Y2483;
E-mail: clavie@ochsner.org.
1537-890X/1402/104Y109
Current Sports Medicine Reports
Copyright * 2015 by the American College of Sports Medicine
104
Volume 14 & Number 2 & March/April 2015
Exercise and Heart Health
Beginning in the 1950s with the seminal work of Morris
et al. (23,24) and continuing in the 1970s with early
studies by Paffenbarger et al. (31), the positive effects of
exercise on heart health have been established clearly
(11,38,40). Regular moderate exercise has been shown to
be helpful for both the primary and secondary prevention
of CVD in both men and women. For this and other reasons, the U.S. PA Guidelines recommend that all Americans
engage in 30 min of moderate exercise (like a brisk walk) for 5
dIwkj1 or more, which equates to 150 minIwkj1 (11,38,40).
The guidelines also point out that similar benefits can be
Exercise Dose and the Heart
Copyright 2015 by the American College of Sports Medicine. Unauthorized reproduction of this article is prohibited.
obtained by engaging in more strenuous exercise (like
jogging) for shorter periods of time, such that 15 min of
jogging done 5 dIwkj1 (or 75 minIwkj1) appears to provide equivalent benefit to doing 150 minIwkj1 of walking.
Risk of SCD with EEE
The risk associated with EEE has been noted for centuries
and evident recently with high-profile cases (18,27Y30,32).
During the Greco-Persian war in 490 BBC, Pheidippides,
a 40-year-old Greek herald, ran almost 150 miles during a
2-d period to deliver urgent military messages. On the third
day, he ran the 26 miles (actually 24.8, which may be significant because most cardiac events during marathons occur
in the last mile) (29,32) from the battlefield near Marathon to
Athens to deliver news of a momentous Greek victory. As per
the legend, upon arriving, Pheidippides explained to the
Athenians, Victory is ours!, and then he immediately collapsed and died. Now 2,500 years later, there are numerous
examples of SCD associated with EEE, and in the best-selling
book, Born to Run (Christopher McDougall, Knopf Publishers, 2009), Micah True is the mythical long distance
runner, Caballo Blanco, who runs as far as 100 miles on
some days. In 2012, while out on a relatively routine 12-mile
training run, he died suddenly, presumably from a lethal
arrhythmia. It is likely that the heart of this 58-year-old
veteran endurance athlete showed manifestations of the
Pheidippides cardiomyopathy (32).
The number of Americans participating in marathons
has increased by more than 25-fold over the past 40 years
(27,29). Certainly high levels of CRF are generally associated
with considerable cardioprotection and reduction in CVD.
However, this is not translated into better reduction in CV or
all-cause mortality among runners. Paradoxically, long-term
marathon runners in some studies have been associated with
increased, rather than decreased, CAD (18,27,29).
However, perhaps the most serious consequence of EEE is
SCD; although these relatively rare events often generate
considerable publicity in major EEE events, SCD remains
relatively uncommon (18,27Y30,32).
In fact, a recent study reviewed all marathons and halfmarathons in the United States during a 10-year period
(10.9 million runners and 59 cardiac arrests) and reported
that SCD occurred in only 1 of 200,000 participants (0.54/
100,000 participants) (13). However other studies suggest
that the true occurrence may be two- to four-fold higher
than this because the data from the study of Kim et al. (13)
may be contaminated by a large number of half-marathoners
and only accounted for SCD during the race itself and not
soon afterwards (18,34,35). Nevertheless, the fatalities in
marathons are still relatively uncommon, although the fatality rate in triathlons may be two-fold higher than runningonly races, largely because of the increased CV events and
SCD during the swim portion of the race (18,29,32);
however, the data in marathons, as opposed to triathlons,
are certainly more robust. The high-catecholamine state of
such EEE competitions superimposed on preexisting ETinduced structural myocardial abnormalities is the most
logical explanation for cases of SCD after common causes
(hypertrophic cardiomyopathy, CAD, anomalous coronaries, channelopathies, and other causes) are excluded.
www.acsm-csmr.org
Effects on CV Structure and Function
There are many potential adverse effects with EEE on cardiac structure and function (Fig. 1) (29). In a recent animal
study, rats were trained to run strenuously for 60 consecutive
minutes daily for 16 wk (3). The ET rats, compared with
controls, developed left ventricular (LV) hypertrophy, right
ventricular (RV) hypertrophy, diastolic ventricular dysfunction, dilation of both the left and right atria (LA and RA,
respectively), as well as considerable collagen deposition within
the cardiac chambers. Serious VA were inducible in 42% of
the running rats compared with only 6% of controls (P = 0.05).
After detraining, however, these adverse structural changes,
as well as VA, largely reversed (3). Many previous animal
studies also have found acute adverse CV effects of prolonged
(up to 6 h) EEE, sometimes employing a rat model of cold
water swimming, in which the animals were forced to swim
to avoid drowning, thus reducing the clinical relevance due
to excessive emotional strain in addition to the EEE (29,33).
However, similar adverse structural remodeling following EEE have been noted in humans (18,27Y30,32). Accumulating evidence suggests that the adverse effects of both
short-term intense PA and cumulative EEE are most evident
in the right-side cardiac chambers (RV and RA). At rest,
average cardiac output in an average size human is approximately 5 LIminj1, and this typically increases by five-fold to
about 25 LIminj1 during vigorous ET. During chronic longterm exposure to prolonged, high-intensity ET, this increased
cardiac output may place more strain on the thinner wall,
smaller, right-side cardiac chambers compared with the left
side of the heart. Following a marathon, for example, approximately 30% of runners develop acute dilation of cardiac structures, especially the RV and RA, and dysfunction of
the RV and ventricular septum. During the postrace period,
the cardiac geometric dimensions are restored, but with this
recurrent stretch of the chambers and reestablishment of
chamber geometry, some individuals may be prone to the
development of chronic structural changes, including chronic
dilation of the LA, RA, and RV, as well as patchy myocardial
scarring in response to the recurrent volume load and
Figure 1: Proposed pathogenesis of cardiomyopathy in endurance athletes. BNP, B-type natriuretic peptide; CK-MB, creatine kinase MB. Reproduced with permission from OKeefe et al. (29).
Current Sports Medicine Reports
Copyright 2015 by the American College of Sports Medicine. Unauthorized reproduction of this article is prohibited.
105
excessive cardiac strain. Although these abnormalities are
typically asymptomatic and resolve over 24 to 72 h, if they
accrue over many years, they may predispose to potentially
serious arrhythmias, such as AF and/or VA (18,27Y30,32).
In one prospective study of 25 runners (12 men and 13
women), Trivax et al. (39) found that running a marathon
caused acute dilation of the RA and RV, with a sudden fall
in RV ejection fraction (EF). Similarly La Gerche et al. (14)
studied 40 highly trained aerobic athletes after competing in
EEE events (marathons, mean time 3 h; half Ironman triathlons, mean time 5.5 h; full Ironman, mean time 11 h; and
Alpine Cycling race, mean time 8 h). On postrace echocardiograms, they noted increases in RV volume and reduced
RVEF (but not LVEF) (Fig. 2) and found elevations in biomarkers (troponin and BNP), which correlated with the fall
in RVEF. These abnormalities in cardiac structure returned
entirely to baseline within the first few weeks and are noted
more typically in races of long duration. Of this cohort, 5
of the 40 (12.5%) had myocardial scarring detected on
cardiac magnetic resonance imaging (MRI), as demonstrated
by late gadolinium enhancement (LGE). Therefore these
studies suggest that intense EEE induces RV dysfunction,
which largely spares the LV (except for possibly the ventricular
septum shared by both ventricles). Even when short-term RV
recovery appears to be complete, potentially long-term ET and
competition in EEE races may lead to myocardial fibrosis
eventually, which potentially could predispose malignant VA.
Another study by Ector et al. (8) reported that the reduction in RVEF seemed less significant in asymptomatic athletes
compared with that in EEE competitors who have symptoms
of arrhythmias, in which RV dilation and reductions in RVEF
Figure 2: Differential effect of prolonged intense exercise on RV
and LV volumes. Baseline volumes are shown on the left, and the
changes in volume after the race are shown on the right. RV volumes
increased in the postrace setting, whereas LV volumes decreased,
resulting in a decrease in RVEF but not in LVEF. Reproduced with
permission from La Gerche et al. (14).
106
Volume 14 & Number 2 & March/April 2015
were more pronounced. In another study, those endurance athletes had a 12% prevalence of RV abnormalities by MRI (6).
Other studies also have confirmed the long-term adverse
effects on myocardial structure (18,27Y30,32), including one
study suggesting that the CAD event rate during 2-year followup was significantly higher in the athletes than that in controls (P G 0.0001) (6).
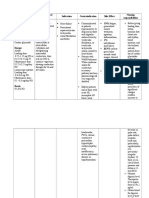
Impact of EEE on CAD
Recent studies have suggested that long distance runners
may have increased levels of atherosclerosis and CAD (18,37).
In a study 6 years ago, male marathon runners had paradoxically increased coronary artery calcification (CAC) as measured by computed tomography (CT) CAC scoring (21). A
very recent study of men who completed at least one marathon yearly for 25 consecutive years (n = 50) compared with
23 sedentary controls demonstrated increased total plaque
volume (P G 0.01), calcified plaque volume (P G 0.0001), and
noncalcified plaque volume (P = 0.04) compared with those
with EEE (Fig. 3) (37). Despite the fact that runners have
better overall CAD risk profiles, these results underscore the
potential for very heavy EEE to increase the severity of CAD
through mechanisms largely independent of the traditional
CAD risk factors.
A very recent study by Mohlenkamp et al. (22) assessed
108 marathon runners and 864 age-matched controls as well
as 216 age- and risk factor-matched controls. Recreational
marathon runners with myocardial fibrosis by MRI-LGE had
higher troponin release than those without LGE. Higher
CAC scores and LGE, as opposed to troponin release (which
was present in 37% of the marathoners), predicted subsequent
CAD events, which were overall similar between marathoners
and risk factor-matched nonmarathon controls.
Impact of ET on Risk of AF
We recently evaluated various risk factors, including
metabolic factors, for the risk of AF (19,20). Certainly
many epidemiologic and observational studies, although
not all (26), have reported a strong statistically significant
association between chronic high-intensity ET and elevated
risk of AF (1,19,20). The impact of habitual PA and ET on
the risk of AF appears to be nonlinear, with lower rates of
AF among moderately active individuals compared with
those among sedentary controls, whereas an increased risk
of AF was noted among individuals performing EEE or long
bouts of high-intensity ET (18,27Y30,32). The mechanism
of AF with high ET is uncertain, but this may involve acute
fluxes in cathecholamines and autonomic tone, atrial stretch,
and RV cardiomyopathy.
In a study of 44,410 Swedish men, intense ET of 95
hIwkj1 at age 30 years increased the risk of AF later in life,
whereas moderate-intensity PA reduced the risk of AF (7).
In a study of 5,446 older athletes (mean age, 73 years),
again low- and moderate-intensity PA progressively reduced
the risk of AF, whereas the rate slightly increased in those
with high-intensity PA (slightly more risk than light intensity but still lower than nonexercisers) (25). In nearly
53,000 long distance cross country skiers from Sweden, there
was more AF with the greater amount of cross-country races
and the fastest finishing times (2). However, with detraining
Exercise Dose and the Heart
Copyright 2015 by the American College of Sports Medicine. Unauthorized reproduction of this article is prohibited.
Figure 3: Marathoners had significantly more total coronary
plaque volume, noncalcified plaque volume, and calcified plaque
volume compared with those of control subjects. Reproduced with
permission from Schwartz et al. (37).
and moderation of ET dose, there is atrial remodeling and
normalization of autonomic tone and reduction of AF risk.
Recent Running Studies and U-Shaped Curve
Three very recent running studies have demonstrated the
U-shaped relationship between running doses and CV diseases and all-cause mortality (15,36,41).
The Copenhagen City Heart Study followed 1,878 runners and 10,158 nonrunners for up to 35 years (28,36). The
runners had an impressive 44% lower risk of mortality
during follow-up, with an average 6-year extension in life
expectancy. However, a U-shaped curve was apparent for
mortality with respect to running dose, with the peak benefit noted with slow-to-moderate running speeds, frequency
of about 3 times per week, and 1 to 2 hIwkj1 of running.
Very high doses of running, however, were associated with
trends of worse survival compared with either nonrunners or groups of low- and moderate-dose runners.
Data from 55,000 people from the Aerobic Center Longitudinal Study, including 13,000 runners and 42,000 nonrunners, followed for an average of 15 years, have been
reported recently (15). During follow-up, runners had impressive reductions in all-cause and CV mortality of 30%
and 45%, respectively, with an average increase in life expectancy of 3 years. Persistent runners had the greatest event
reduction, whereas those who began running and stopped or
vice versa received about half of the full beneficial effect.
However, when dividing runners into quintiles of doses
(milesIwkj1, running days per week, minIwkj1, and running
speed), with the exception of speed (faster running always
had a trend for better survival), quintile 1 (G6 milesIwkj1, 1
to 2 times per week, G51 minIwkj1) had similar mortality
reductions as those in quintiles 2 to 4 and a trend to slightly
greater benefit than those in quintile 5 (Fig. 4). The individuals performing higher running doses generally have
higher levels of CRF; and in almost all studies in the literature, higher levels of CRF are associated with lower CV and
all-cause mortality rates. However, among runners (who already have high levels of CRF even when running at lower
volumes), low doses of running provide maximal protection
against all-cause and CV mortality (15).
Additionally, in a study of 24,000 patients with CAD
with a history of myocardial infarction, those doing more
Figure 4: Central illustration: hazard ratios (HR) of all-cause and CV mortality by running characteristic (weekly running time, distance,
frequency, total amount, and speed). Participants were classified into six groups: nonrunners (reference group) and five quintiles of each running
characteristic. All HR were adjusted for baseline age (yr), sex, examination year, smoking status (never, former, or current), alcohol consumption
(heavy drinker or not), other physical activities except running (0, 1 to 499, or 500 METIminIwkj1), and parental history of CV disease (yes or no).
All P values for HR across running characteristics were G0.05 for all-cause and CV mortality except for running frequency of six times a week
(P = 0.11) and speed of G6.0 miles/hyperlipidemia (P = 0.10) for CV mortality. Reproduced with permission from Lee et al. (15).
www.acsm-csmr.org
Current Sports Medicine Reports
Copyright 2015 by the American College of Sports Medicine. Unauthorized reproduction of this article is prohibited.
107
ET had progressive reductions in CV mortality, up to a point
(Figs. 5 and 6) (41). At running doses of 930 milesIwkj1
(or walking 946 milesIwkj1), there appears to be partial loss
of the ET benefit on CV mortality (41).
These studies all point to the fact that more does not
appear to be better and low-to-moderate doses of running
seem to be ideal for conferring long-term CV health and
enhanced longevity (15,18,27Y30,32,36,41).
Nevertheless, over a decade ago, a study on more than
73,000 participants, mostly nonelite skiers, who had competed in a major ski race in Sweden demonstrated that participants had lower mortality from all causes, CV diseases,
and cancers compared with age-adjusted mortality rates (10).
Another recent study indicates that participants in the
Olympics and professional sports also were associated with
long-term protection against mortality from all causes, CV
diseases, and cancers, suggesting that previous sports stardom
is associated with overall excellent long-term prognosis (12).
Optimal ET Dosing
As Hippocrates said centuries ago, Everything in excess
is opposed to nature (9). From a population perspective,
lack of PA is much more prevalent than excessive ET.
The PA Federal Guidelines call for 150 minIwkj1 of moderate PA or 75 minIwkj1 of vigorous PA. The Institute of
Medicine suggests 60 minIdj1 of some PA. Recent evidence
Figure 5: Categorical model. Cox proportional survival analyses
of the risk of CVD-related mortality vs MET-hours per day run or
walked. Relative risk is calculated for 1.07 to 1.8, 1.8 to 3.6, 3.6 to
5.4, 5.4 to 7.2, and 7.2 METIhIdj1 or more relative to the inadequate exercisers (G1.07 METIhIdj1). All CVD-related mortality
includes both CVD as an underlying cause and CVD as a contributing cause for some other underlying cause. Significance
levels are coded as follows: a P e 0.05; b P e 0.01; and c P e .001.
The significance levels for 7.2 METIhIdj1 or more vs less than 1.07
METIhIdj1 were all nonsignificant, that is, P = 0.99 for all-cause
mortality, P = 0.68 for all CVD-related mortality, and P = 0.46 for
CVD as the underlying cause of death. METIhIdj1, metabolic
equivalent of task-hours per day. Reproduced with permission from
Williams et al. (41).
108
Volume 14 & Number 2 & March/April 2015
Figure 6: Continuous model. Cox proportional survival analyses
of the risk of CVD-related mortality vs MET-hours per day run or
walked. In the model > METIhIdj1trimmed (METIhIdj1 if METIhIdj1 e
7.2, 7.2 otherwise) + A indicator function (1 = METIhIdj1 Q 7.2,
0 otherwise) + covariates, the hypothesis A = 0 tests whether
the HR is increased significantly above 7.2 METIhIdj1 relative to the
HR at 7.2. Shown is the 15.4% average decrease in the risk for
CVD-related mortality per MET-hours per day between 0 and 7.2
(95% confidence interval (CI), 8.9%Y21.5%; P G 0.001) and a
2.62-fold risk increase above 7.2 METIhIdj1 relative to the risk at
7.2 METIhIdj1 (95% CI, 1.29- to 5.06-fold; P = 0.009). Reproduced
with permission from Williams et al. (41).
has suggested that very few are meeting these minimal
requirements (11,38,40), and we have made a call to action
that all clinicians should be promoting PA throughout the
health care system (40).
Evidence is mounting, however, that indicates a substantial number of individuals (perhaps 2% or 5% of the population) may be overdoing ET, at least from a health
standpoint. If the current mantra exercise is medicine is
embraced, PA/ET may be analogous to a drug, with indications and contraindications as well as issues related to
underdosing and overdosing (27). The recent running articles certainly raise the idea that running doses of less than
the PA guidelines may produce maximal protection from
all-cause and CV mortality (15,36). On the other hand, very
high doses of ET could have adverse effects by increasing
the risk of arrhythmias (especially VA and AF) but also with
acute bouts of high-volume, high-intensity ET increasing
release of troponin and BNP and causing acute cardiac dilation and dysfunction of cardiac chambers. Returning to
high bouts of ET before cardiac recovery could prove to be
particularly toxic to the heart. Chronic EEE can produce
myocardial scarring and potentially produce cardiomyopathies and substrate for sustained and life-threatening VA.
The Other Side of the Story V Providing Fair Balance
Others feel that the evidence that years of high-intensity
ET accelerates atherosclerosis or causes cardiac fibrosis is
relatively weak, and given the known benefits of competitive ET, discussed previously, on both cardiac and vascular
structure and function, this may not be clinically important
Exercise Dose and the Heart
Copyright 2015 by the American College of Sports Medicine. Unauthorized reproduction of this article is prohibited.
(4,16,17). Although there is no argument that EEE can be
potentially harmful, it may be inappropriate to overly
frighten individuals who want to participate in competitive
ET, even EEE, such as marathons, triathlons, or even ultraendurance races (16). In fact, very high levels of ET may
prevent the decreased compliance and dispensability observed with healthy, sedentary aging (4,17).
Summary and Conclusions
On the basis of multiple studies, it would seem most advisable, at least from a population-wide public health standpoint, to limit vigorous ET to no more than 60 minIdj1, and
indeed it is likely that near-maximal health benefits occur at
even much lower doses (15,27,36). On the other hand, people participate in vigorous ET for non-health reasons, including
competition/challenge, fun/exhilaration, ego, psychological
benefits, friendships, etc. These individuals should recognize
that there may be some increased risk, although relatively
small, of such vigorous EEE. Ideally, however, a weekly cumulative dose of vigorous ET of not more than 5 h may be
ideal, including taking 1 to 2 dIwkj1 off from vigorous and
high-intensity ET (27).
Finally as Hippocrates noted centuries ago, If we could
give every individual the right amount of nourishment and
exercise, not too little and not too much, we would have
found the safest way to health (9). These words from 2,500
years ago still seem prudent and wise today.
The authors declare no conflicts of interest and do not
have any financial disclosures.
References
12. Garatachea N, Santos-Lozano A, Sanchis-Gomar F, et al. Former elite athletes live longer than the general population: a meta-analysis. Mayo Clin.
Proc. 2014; 89:1195Y200.
13. Kim JH, Malhotra R, Chiampas G, et al. Cardiac arrest during long-distance
running races. N. Engl. J. Med. 2012; 366:130Y40.
14. La Gerche A, Burns AT, Mooney DJ, et al. Exercise-induced right ventricular
dysfunction and structural remodelling in endurance athletes. Eur. Heart J.
2012; 33:998Y1006.
15. Lee D-C, Pate RR, Lavie CJ, et al. Leisure-time running reduces all-cause and
cardiovascular mortality risk. J. Am. Coll. Cardiol. 2014; 64:472Y81.
16. Levine BD. Can intensive exercise harm the heart? The benefits of competitive
endurance training for cardiovascular structure and function. Circulation.
2014; 130:987Y91.
17. Lew WY. Exercise: commitment to a young heart. J. Am. Coll. Cardiol. 2014;
64:1267Y9.
18. McCullough PA, Lavie CJ. Coronary artery plaque and cardiotoxicity as a
result of extreme endurance exercise. Mo. Med. 2014; 111:9Y94.
19. Menezes AR, Lavie CJ, DiNicolantonio JJ, et al. Atrial fibrillation in the 21st
century: a current understanding of risk factors and primary prevention
strategies. Mayo Clin. Proc. 2013; 88:394Y409.
20. Menezes AR, Lavie CJ, DiNicolantonio JJ, et al. Cardiometabolic risk factors and atrial fibrillation. Rev. Cardiovasc. Med. 2013; 14:e73Y81.
21. Mohlenkamp S, Lehmann N, Breuckmann F, et al. Running: the risk of
coronary events: prevalence and prognostic relevance of coronary atherosclerosis in marathon runners. Eur. Heart J. 2008; 29:1903Y10.
22. Mohlenkamp S, Leineweber K, Lehmann N, et al. Coronary atherosclerosis
burden, but not transient troponin elevation, predicts long-term outcome in
recreational marathon runners. Basic Res. Cardiol. 2014; 109:391.
23. Morris JN, Heady, JA, Raffle, et al. Coronary heart-disease and physical
activity of work. Lancet. 1953; 265:1053Y7.
24. Morris JN, Heady, JA, Raffle PA, et al. Coronary heart-disease and physical
activity of work. Lancet. 1953; 265:1111Y20.
25. Mozaffarian D, Furberg CD, Psaty BM, Siscovick D. Physical activity and
incidence of atrial fibrillation in older adults: the cardiovascular health study.
Circulation. 2008; 118:800Y7.
26. Ofman P, Khawaja O, Rahilly-Tierney CR, et al. Regular physical activity
and risk of atrial fibrillation: a systematic review and meta-analysis. Circ.
Arrhythm. Electrophysiol. 2013; 6:252Y6.
27. OKeefe JH, Franklin B, Lavie CJ. Exercising for health and longevity vs peak
performance: different regimens for different goals. Mayo Clin. Proc. 2014;
89:1171Y5.
1. Abdulla J, Nielsen JR. Is the risk of atrial fibrillation higher in athletes than
in the general population? A systematic review and meta-analysis. Europace.
2009; 11:1156Y9.
28. OKeefe JH, Lavie CJ. Run for your life I at a comfortable speed and not
too far. Heart. 2013; 99:516Y9.
2. Andersen K, Farahmand B, Ahlbom A, et al. Risk of arrhythmias in 52,755
long-distance cross-country skiers: a cohort study. Eur. Heart J. 2013; 34:
3624Y31.
29. OKeefe JH, Patil HR, Lavie CJ, et al. Potential adverse cardiovascular effects from excessive endurance exercise. Mayo Clin. Proc. 2012; 87:
587Y95.
3. Benito B, Gay-Jordi G, Serrano-Mollar A, et al. Cardiac arrhythmogenic
remodeling in a rat model of long-term intensive exercise training. Circulation. 2011; 123:13Y22.
4. Bhella PS, Hastings JL, Fujimoto N, et al. Impact of lifelong exercise dose
on left ventricular compliance and distensibility. J. Am. Coll. Cardiol. 2014;
64:1257Y66.
5. Blair SN. Physical inactivity: the biggest public health problem of the 21st
century. Br. J. Sports Med. 2009; 43:1Y2.
6. Breuckmann F, Mohlenkamp S, Nassenstein K, et al. Myocardial late gadolinium enhancement: prevalence, pattern, and prognostic relevance in marathon runners. Radiology. 2009; 251:50Y7.
7. Drca N, Wolk A, Jensen-Urstad M, Larsson SC. Atrial fibrillation is associated with different levels of physical activity levels at different ages in men.
Heart. 2014; 100:1037Y42.
8. Ector J, Ganame J, van der Merwe N, et al. Reduced right ventricular
ejection fraction in endurance athletes presenting with ventricular arrhythmias: a quantitative angiographic assessment. Eur. Heart J. 2007; 28:
345Y53.
9. Everything in excess is opposed to nature [Internet]. Hippocrates. Available
from: http://www.brainyquote.com/quotes/quotes/h/hippocrate118541.html.
2014. Accessed June 23, 2014.
, et al. Mortality amongst participants
10. Farahmand BY, Ahlbom A, Ekblom O
in Vasaloppet: a classical long-distance ski race in Sweden. J. Intern. Med.
2003; 253:276Y83.
11. Franklin BA, Lavie CJ, Squires RW, Milani RV. Exercise-based cardiac rehabilitation and improvements in cardiorespiratory fitness: implications regarding patient benefit. Mayo Clin. Proc. 2013; 88:431Y7.
www.acsm-csmr.org
30. OKeefe JH, Schnohr P, Lavie CJ. The dose of running that best confers
longevity. Heart. 2013; 99:588Y90.
31. Paffenbarger RS, Hyde RT, Wing AL, Hsieh CC. Physical activity, all-cause
mortality, and longevity of college alumni. N. Engl. J. Med. 1986; 314:
605Y13.
32. Patil HR, OKeefe JH, Lavie CJ, et al. Cardiovascular damage resulting from
chronic excessive endurance exercise. Mo. Med. 2012; 109:312Y21.
33. Praphatsorna P, Thong-Ngama D, Kulaputanaa O, Klaikaewb N. Effects of
intense exercise on biochemical and histological changes in rat liver and
pancreas. Asian Biomed. 2010; 4:619Y25.
34. Redelmeier DA, Greenwald JA. Competing risks of mortality with marathons: retrospective analysis. BMJ. 2007; 335:1275Y7.
35. Roberts WO, Roberts DM, Lunos S. Marathon related cardiac arrest risk
differences in men and women. Br. J. Sports Med. 2013; 47:168Y71.
36. Schnohr P, Marott JL, Lange P, et al. Longevity in male and female joggers:
the Copenhagen City Heart Study. Am. J. Epidemiol. 2013; 177:683Y9.
37. Schwartz RS, Kraus SM, Schwartz JG, et al. Increased coronary artery plaque
volume among male marathon runners. Mo. Med. 2014; 111:85Y90.
38. Swift DL, Lavie CJ, Johannsen NM, et al. Physical activity, cardiorespiratory
fitness, and exercise training in primary and secondary coronary prevention.
Circ. J. 2013; 77:281Y92.
39. Trivax JE, Franklin BA, Goldstein JA, et al. Acute cardiac effects of marathon running. J. Appl. Physiol. (1985). 2010; 108:1148Y53.
40. Vuori IM, Lavie CJ, Blair SN. Physical activity promotion in the health care
system. Mayo Clin. Proc. 2013; 88:1446Y61.
41. Williams P, Thompson P. Increased cardiovascular disease mortality from excessive exercise in heart attack survivors. Mayo Clin. Proc. 2014; 89:1187Y94.
Current Sports Medicine Reports
Copyright 2015 by the American College of Sports Medicine. Unauthorized reproduction of this article is prohibited.
109
Vous aimerez peut-être aussi
- Breast Cancer RiskDocument7 pagesBreast Cancer RiskCésar Ayala GuzmánPas encore d'évaluation
- Sleep and PerformanceDocument7 pagesSleep and PerformanceCésar Ayala Guzmán100% (1)
- Training Loads DifferentlyDocument13 pagesTraining Loads DifferentlyCésar Ayala GuzmánPas encore d'évaluation
- Akkus 2012 SnatchDocument9 pagesAkkus 2012 SnatchCésar Ayala GuzmánPas encore d'évaluation
- Nutrition For Athletes - IOC PDFDocument66 pagesNutrition For Athletes - IOC PDFCésar Ayala GuzmánPas encore d'évaluation
- Ying-Chen 2015 - WeightliftingDocument4 pagesYing-Chen 2015 - WeightliftingCésar Ayala GuzmánPas encore d'évaluation
- Borg Scale in Strength TrainingDocument11 pagesBorg Scale in Strength TrainingCésar Ayala Guzmán100% (1)
- Viorel 2014 - Clean & JerkDocument6 pagesViorel 2014 - Clean & JerkCésar Ayala GuzmánPas encore d'évaluation
- Ikeda 2012 SnatchDocument15 pagesIkeda 2012 SnatchCésar Ayala GuzmánPas encore d'évaluation
- Sexual Activity Before CompetitionDocument8 pagesSexual Activity Before CompetitionCésar Ayala GuzmánPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Rendam Kaki Dengan Rebusan Jahe Merah Dapat Mencegah Terjadinya EklamsiaDocument8 pagesRendam Kaki Dengan Rebusan Jahe Merah Dapat Mencegah Terjadinya EklamsiaMellwandariskPas encore d'évaluation
- The Adult Chain of Survival Module1Document1 pageThe Adult Chain of Survival Module1Mariam E.Pas encore d'évaluation
- Chapter 14 - Dyslipidemia - Afraid of Another Attack Level IIDocument6 pagesChapter 14 - Dyslipidemia - Afraid of Another Attack Level IIfarah amranePas encore d'évaluation
- 10.1038@s41572 019 0090 3Document20 pages10.1038@s41572 019 0090 3sari100% (1)
- 5-Heart FailureDocument12 pages5-Heart FailureJericho De GuzmanPas encore d'évaluation
- New Microsoft Word DocumentDocument18 pagesNew Microsoft Word Documentapi-427712934Pas encore d'évaluation
- Echocardiography in Fontan PhysiologyDocument30 pagesEchocardiography in Fontan PhysiologyNavojit ChowdhuryPas encore d'évaluation
- Chapter 13: The Heart and Heart DiseaseDocument3 pagesChapter 13: The Heart and Heart Diseasetrbrown2011Pas encore d'évaluation
- HypovolCardiSepsisShock PDFDocument11 pagesHypovolCardiSepsisShock PDFloysstormPas encore d'évaluation
- BuaDocument3 pagesBuaAnonymous xyaZgBmRPas encore d'évaluation
- Harvard Step Test: SkillslabDocument32 pagesHarvard Step Test: SkillslabRozman SepeaiPas encore d'évaluation
- Hallmark AssignmentDocument12 pagesHallmark AssignmentMulwa MutungaPas encore d'évaluation
- Pharmacology - Mnemonics PDFDocument140 pagesPharmacology - Mnemonics PDFItharshan Indreswaran76% (17)
- Say No To Code Blue, Say YesDocument36 pagesSay No To Code Blue, Say YesTheodorus PY PranotoPas encore d'évaluation
- Module-17 - CPR and AED PDFDocument28 pagesModule-17 - CPR and AED PDFJithinShankarPas encore d'évaluation
- MCQS Pathology, Rawalpindi Medical CollegeDocument8 pagesMCQS Pathology, Rawalpindi Medical CollegeZahid QamarPas encore d'évaluation
- Cardio QuizDocument100 pagesCardio QuizEvidence ChaibvaPas encore d'évaluation
- Cavafix Mono 04.08Document6 pagesCavafix Mono 04.08Frunk Gonk ZendenPas encore d'évaluation
- Zoghbi ASE Guidelines MR AR FINAL - Updated - 0Document34 pagesZoghbi ASE Guidelines MR AR FINAL - Updated - 0DenisseRangelPas encore d'évaluation
- Lesson Plan On CPRDocument9 pagesLesson Plan On CPRAngelica Mercado SirotPas encore d'évaluation
- GE Responder 2000 - User ManualDocument142 pagesGE Responder 2000 - User ManualPedro Nel Cifuentes RodriguezPas encore d'évaluation
- Acute Myocardial InfarctionDocument13 pagesAcute Myocardial InfarctionSajjad KabirPas encore d'évaluation
- Adult Immediate Post Cardiac Arrest Care Algorithm 2015 UpdateDocument1 pageAdult Immediate Post Cardiac Arrest Care Algorithm 2015 UpdateRyggie Comelon0% (1)
- CVS PrecordiumDocument20 pagesCVS PrecordiumSarahPas encore d'évaluation
- Vital Sign #1: Body TemperatureDocument5 pagesVital Sign #1: Body TemperaturePrimelift Safety Resources LimitedPas encore d'évaluation
- A New Era in Acute Ischaemic Stroke Treatment A Review of Uk and European Thrombectomy GuidelinesDocument8 pagesA New Era in Acute Ischaemic Stroke Treatment A Review of Uk and European Thrombectomy GuidelinesJavieraAlondraDiazPas encore d'évaluation
- Ezx 314Document29 pagesEzx 314Adventa 91Pas encore d'évaluation
- Syntax Score Calculation SimulationDocument66 pagesSyntax Score Calculation SimulationTahari Bargas PrakosoPas encore d'évaluation
- Respiratory System Muamar Aldalaeen, RN, Mba, HCRM, Cic, Ipm, MSN, PHD - Haneen Alnuaimi, MSNDocument46 pagesRespiratory System Muamar Aldalaeen, RN, Mba, HCRM, Cic, Ipm, MSN, PHD - Haneen Alnuaimi, MSNAboodsha ShPas encore d'évaluation
- DigoxinDocument4 pagesDigoxinJaessa FelicianoPas encore d'évaluation