Académique Documents
Professionnel Documents
Culture Documents
Choline Pet CT
Transféré par
scalpotTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Choline Pet CT
Transféré par
scalpotDroits d'auteur :
Formats disponibles
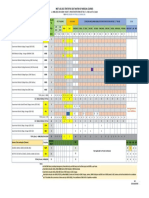
Vol. 187, No.
4S, Supplement, Wednesday, May 23, 2012
THE JOURNAL OF UROLOGY
e823
2040
DETECTION OF CONSOLIDATED DISEASE RECURRENCES OF
PROSTATE CANCER BY 11C-CHOLINE PET/SCAN: RESULTS
CONFIRMED BY SURGICAL RESECTION
Christopher Mitchell*, Eugene Kwon, Val Lowe, Joseph Hung,
Laureano Rangel, R. Jeffrey Karnes, Rochester, MN
Source of Funding: R01 Grant (5-RO1-CA-101734-02)
2039
IMPACT OF 11C-CHOLINE PET/CT SCAN ON DETECTION OF
RECURRENT PROSTATE CANCER IN MEN WITH BIOCHEMICAL
RECURRENCE FOLLOWING FAILED INITIAL TREATMENT
INTRODUCTION AND OBJECTIVES: To evaluate the accuracy of 11C-choline PET/CT scan in the diagnosis of consolidated
prostate cancer recurrences in men with biochemical failure after
primary treatment.
METHODS: Retrospective review was performed of all prostate
cancer patients who underwent evaluation using 11C-choline PET/CT
scan from 9/2007 to 11/2010 at Mayo Clinic.
RESULTS: Consolidated recurrences were identified in 36 patients who underwent salvage surgery. 28 patients underwent metastatectomy for isolated disease recurrences and 8 underwent salvage
prostatectomy. Mean and median PSA at the time of PET scan were
5.3 and 2.8 ng/ml respectively. In this setting 11C-choline PET/CT scan
yielded a sensitivity and PPV of 88% and 94% respectively. PET scan
was the only imaging modality to localize the site of recurrence in 14/36
(38.9%) patients. However, PET scan failed to identify metastatic
lesions in 4/35 patients (11%) all of whom were on androgen deprivation therapy at the time of PET scan. Negative surgical explorations
were performed in 2/35 patients (5.6%). 11C-choline PET/CT scan
failed to accurately quantify the disease burden in 4 patients who were
found to harbor co-existing microscopic nodal metastases.
CONCLUSIONS: 11C-choline PET/CT scan is an accurate diagnostic tool for the detection of localized disease recurrences which in
select cases are amenable to salvage surgical resection.
Christopher Mitchell*, Eugene Kwon, Val Lowe, Joseph Hung,
Laureano Rangel, R. Jeffrey Karnes, Rochester, MN
INTRODUCTION AND OBJECTIVES: Distinguishing localized
recurrence from systemic recurrence represents an important step in
optimizing prostate cancer treatment following primary treatment failure. We examined the performance of 11C-choline PET/CT scan for its
ability to delineate prostate cancer distribution and extent after failed
definitive therapy.
METHODS: Retrospective review was performed of all prostate
cancer patients who underwent evaluation using 11C-choline PET/CT
scan from 9/2007 to 11/2010 at Mayo Clinic. Analysis was restricted to
patients with biochemical recurrence following failed primary prostate
cancer treatment. Statistical analysis was performed to determine the
sensitivity, specificity, positive predictive value (PPV), and negative
predictive value (NPV).
RESULTS: During the study period 176 patients with biochemical recurrence after primary treatment failure underwent 11C-choline
PET/CT scan. In this setting 11C-choline PET scanning yielded a
sensitivity, specificity, PPV, and NPV of 93, 76, 91, and 81%, respectively. 56 of 166 (32%) PET scans performed were deemed clinically
useful as defined by their ability to detect treatable lesions, not
identified using conventional imaging, thereby triggering changes in
clinical management. The PSA cut-off at which PET scan was most
likely to be positive was 2.0ng/ml. On multivariate analysis, PSA at the
time of PET scan (HR1.37, 95% CI: 1.0-1.01, p0.04) and clinical
stage (HR5.19, 95% CI: 1.72-15.68, p0.0035) were significant
predictors of a positive 11C-choline PET/CT scan.
CONCLUSIONS: 11C-choline PET/CT scan performs well in
men with biochemical recurrence following primary treatment failure.
The optimal value for lesion detection is approximately 2.0mg/ml. We
find that 11C-choline PET/CT substantially enhances the rate of prostate cancer lesion detection by approximately 32% beyond what can be
garnered using conventional imaging technologies and has significant
potential to impact treatment of men with recurrent prostate cancer.
Source of Funding: None
Source of Funding: None
2041
LOCALIZATION OF RECURRENT PROSTATE CANCER AFTER
RADICAL PROSTATECTOMY BY ENDORECTAL COIL
MAGNETIC RESONANCE IMAGING
Brian Linder*, Akira Kawashima, Matthew Tollefson,
Laureano Rangel, Bernard King, Lance Mynderse, Rochester, MN
INTRODUCTION AND OBJECTIVES: To evaluate the predictive value of endorectal coil (e-coil) magnetic resonance imaging (MRI)
in identifying local recurrence of prostate cancer after prostatectomy.
METHODS: We identified 188 patients from 2002-2011 that
underwent e-coil MRI with dynamic gadolinium-contrast enhancement
followed by transrectal ultrasound (TRUS) guided biopsy of the prostatic fossa for evaluation of possible local prostate cancer recurrence.
All patients had undergone a radical prostatectomy as primary therapy.
Prior to fossa biopsy 25 patients received radiation therapy, 21 patients
received androgen deprivation therapy and 19 patients underwent both
modalities. A positive e-coil MRI for local recurrence was defined as the
depiction of enhancing nodules in the surgical bed. Local recurrence
was determined by a negative evaluation for distant metastatic disease,
in addition to a positive TRUS guided prostatic fossa biopsy, reduction
in prostate specific antigen (PSA) following external beam radiation
therapy, or increased size on serial e-coil MRI.
RESULTS: Local recurrence was identified in 138 patients. In
130 (94%) of these, e-coil MRI was positive for local recurrence. The
median PSA was 0.59 (range 0.1 to 13.1). The median length of
lesions seen on MRI was 1 cm (range 0.3-4.4 cm). Overall, the
sensitivity of MRI in detecting local recurrence was 94%, with a specificity of 42%. The positive predictive value was 82%, with a negative
predictive value of 72% (AUC-0.68). Local recurrence was identified in
44 of 55 patients (80%) with a PSA 0.4. Of these, 41 (93%) were
identified on e-coil MRI. In patients with a PSA 0.4, the sensitivity of
e-coil MRI was 93%, and specificity was 36%. The positive predictive
value was 85%, with a negative predictive value of 57% (AUC-0.65). In
patients with a lesion identified on MRI, the positive biopsy rate was
65%. The length of the lesion on MRI was a significant factor predicting
e824
THE JOURNAL OF UROLOGY
the likelihood of a positive biopsy. The positive biopsy rates were 57%,
72% and 88% when the lesion was 1 cm, 1-2 cm, or 2 cm,
respectively. For the length increase, the change in positive biopsy rate
for lesions from 1 cm to 1-2 cm using 1 cm as reference, and from
1-2 cm to 2 cm using 1-2 cm as a reference, the OR was 2.5
(1.35-4.45, p 0.003).
CONCLUSIONS: E-coil MRI has a high level of sensitivity in
identifying cases of local recurrence of prostate cancer, even at low
PSA levels. This imaging modality should be considered in the evaluation of biochemical recurrence to help guide TRUS prostatic fossa
biopsies and identify patients suitable for localized salvage therapy.
Source of Funding: None
2042
EVALUATION OF THE VESICOURETHRAL ANASTOMOSIS POST
RADICAL PROSTATECTOMY - TRANSRECTAL ULTRASOUND
VERSUS CYSTOGRAPHY
Andreas Bannowsky*, Nasim Mosaheb, Alexandra Raileanu,
Samer Schakaki, Isis Vollmer, Osnabruck, Germany;
Klaus-Peter Junemann, Kiel, Germany; Hermann van Ahlen,
Osnabruck, Germany
INTRODUCTION AND OBJECTIVES: Evaluation of the vesicourethral anastomosis after radical retropubic prostatectomy in prostate cancer is usually perfomed by cystography. The transrectal ultrasound of the prostate (TRUS) is mainly utilized to get anatomical
information like volume determination, tumor detection and extension.
In a prospective, two-institutional study we compared TRUS with
cystography after radical retropubic prostatectomy in the evaluation of
the vesicourethral anastomosis.
METHODS: In 212 patients the vesicourethral anastomosis
was evaluated by TRUS (7 MHz) followed immediately by cystography
on day 7-14 after radical prostatectomy. Sonographically all patients
were evaluated for hematomas, lymphoceles and leakages of the
anastomosis, controlled by irrigation (100 - 120 ml 0.9% saline solution)
during real time TRUS examination. All TRUS and x-ray findings,
duration of the examination and dose of radiation were separately
documented and compared. Leakages and hematomas (cystogram:
bladder displacements or impressions) were compared with the TRUS
findings and statistically evaluated.
RESULTS: 52 of the 212 patients (24.5%) showed an extravasation. In 39 cases (18.4%) this was seen by cystography and TRUS.
9 patients (4.2%) with leakage, were identified only by TRUS without
radiographic correlation. The topographic localisation of the leakage
was in 94% the dorsal part of the anastomosis. In 12 cases (5.6%)
hematomas were identified only by TRUS without any correlation in the
cystography, 5 in continuity with the anastomosis were responsible for
a persisting hematuria and 2 were the cause for temporary bladder
outlet obstruction. The source for bladder impressions due to paravesical lymphoceles could be identified by TRUS in 10 cases (4.7%). The
duration of examination differed significantly with 5.4 minutes for TRUS
vs. 8.7 minutes for cystography. No significant differences existed
between the two institutions.
CONCLUSIONS: In the evaluation of the anastomosis after
radical prostatectomy TRUS shows the same efficiency as the usually
perfomed cystography. It allows an online assessment of postoperative
topography, like hematomas or lymphoceles, and dynamic evaluation
(exact localisation and dimension) of inefficient anastomosis omitting
the cystography. The radiation exposition for the medical staff and
patient can be reduced by using TRUS. Treatment costs e.g. x-ray and
contrast medium are decreased. Due to the good results TRUS replaced the cystography at the two institutions participated in this study.
Source of Funding: None
Vol. 187, No. 4S, Supplement, Wednesday, May 23, 2012
2043
RELATIONSHIP BETWEEN PHYSICAL EXAMINATION, DYNAMIC
MRI, AND INTRA-OPERATIVE FINDINGS IN THE TREATMENT OF
PELVIC ORGAN PROLAPSE
Forrest Jellison*, Ngoc-Bich Le, A Lenore Ackerman,
Lisa Rogo-Gupta, Denise Chow, Karim Chamie, Steven Raman,
Larissa V Rodriguez, Shlomo Raz, Los Angeles, CA
INTRODUCTION AND OBJECTIVES: The purpose of this
study is to determine the relationship between physical examination
(PE), dynamic MRI, and operative findings in the surgical repair of
pelvic organ prolapse (POP).
METHODS: A cohort of 71 patients who underwent surgical
repair for anterior compartment prolapse between 2009 and 2011 were
selected for a retrospective analysis. Clinical symptoms were determined by validated questionnaires. Preoperative PE and dynamic MRI
findings were compared with the intraoperative findings of the anterior,
apical and posterior compartments. Dynamic MRI employed a previously described limited T2 weighted Haste sequence.
RESULTS: A total of 71 patients with a mean age of 64 (range
of 33-99, and median 65) were included. The median parity was 2
(range 0 9). The mean score of the PFDI-20 and PFIQ-8 were 125 and
269, respectively.
Anterior compartment repair was performed for the entire cohort with concomitant surgical repairs in 89% 49% had apical compartment repair and 74% had repair of the posterior compartment.
When dynamic MRI was compared to intraoperative findings,
detection of apical compartment prolapse (uterine or vault) had a
sensitivity of (100%, 100%), specificity (70%, 95%), and ROC (0.85,
0.97). In contrast, when PE was compared to intraoperative findings of
apical compartment prolapse (uterine or vault), detection rate had a
sensitivity of (42%, 33%), specificity (86%, 93%), and ROC (0.64,0.63),
respectively.
In evaluation of the posterior compartment, dynamic MRI and
PE had a sensitivity (76%, 85%), specificity (16%, 63%), and ROC
(0.16, 0.74) when compared to intraoperative findings.
Anterior compartment prolapse detection rates of (93%, 96%)
were similar when dynamic MRI and PE were compared to intraoperative findings.
Dynamic MRI had additional anatomical findings in 34% of the
patients (simple and complex ovarian cysts, nabothian cyst, uterine
fibroids, sacral cysts, umbilical and inguinal hernias, ureteral stone,
bladder thickening, and hydronephrosis of the kidney).
CONCLUSIONS: Dynamic MRI was able to predict prolapse for
all compartments, but is moderately less reliable for posterior compartment when compared with intraoperative findings. PE was able to
predict anterior compartment prolapse but is less reliable for apical and
posterior compartments when compared with intraoperative findings.
MRI predicted apical prolapse better than PE. Further investigation in
evaluation of posterior compartment is warranted.
Source of Funding: None
2044
DIFFUSION TENSOR MAGNETIC RESONANCE TRACTOGRAPHY
OF THE PROSTATE: FEASIBILITY FOR NEUROANATOMIC
MAPPING
David S. Finley*, Benjamin Ellingson, Shyam Natarajan, Taryar Zaw,
Steven Raman, Peter Schulam, Robert Reiter, Daniel Margolis, Los
Angeles, CA
INTRODUCTION AND OBJECTIVES: Present knowledge of
periprostatic neuroanatomy is based largely on gross dissection of the
prostate gland. We evaluated the feasibility of in-vivo diffusion tensor
magnetic resonance imaging (DTI) tractography of the prostate to
visualize and map periprostatic neurovascular anatomy.
METHODS: Eight men scheduled to undergo robot-assisted
radical prostatectomy underwent 3.0Tesla endorectal multiparametric
magnetic resonance imaging (MRI) of the prostate with DTI. Tract
Vous aimerez peut-être aussi
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Clinical Diagnosis of Alzheimer's Disease (1984, Neurology)Document8 pagesClinical Diagnosis of Alzheimer's Disease (1984, Neurology)robertokutcherPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Mortal Oscillatory Rates - Kook ScienceDocument20 pagesMortal Oscillatory Rates - Kook ScienceCarl MacCordPas encore d'évaluation
- The Haunted Self Structural Dissociation and The T PDFDocument7 pagesThe Haunted Self Structural Dissociation and The T PDFKomáromi PéterPas encore d'évaluation
- Food Safety Practices Among Street Food Vendors in Mayantoc PlazaDocument5 pagesFood Safety Practices Among Street Food Vendors in Mayantoc PlazaHACKER WiFI100% (2)
- Seminar On AphDocument46 pagesSeminar On AphKaruna KumariPas encore d'évaluation
- Bag TechniqueDocument4 pagesBag TechniqueCharlie Cotoner FalgueraPas encore d'évaluation
- Benign Breast DiseasesDocument35 pagesBenign Breast DiseasesBhim Nath KharelPas encore d'évaluation
- AFJMediareleasefinal 2Document2 pagesAFJMediareleasefinal 2Sam TormeyPas encore d'évaluation
- Gonorrhea Case StudyDocument2 pagesGonorrhea Case StudyDonna LLerandi100% (1)
- MED 251 Block 9 PHL Brochure and TarpDocument6 pagesMED 251 Block 9 PHL Brochure and TarpFerdinand Sta Ana Jr.Pas encore d'évaluation
- Of Active Medical Devices-Malaysia Standard MS 2058:2009 Syed Mustafa KamalDocument6 pagesOf Active Medical Devices-Malaysia Standard MS 2058:2009 Syed Mustafa KamalArif YamanPas encore d'évaluation
- 4 - Pharmaceutical ProcurementDocument12 pages4 - Pharmaceutical ProcurementRazak KiplangatPas encore d'évaluation
- Shafkat Jahan ThesisDocument164 pagesShafkat Jahan ThesisAzam StewartPas encore d'évaluation
- 1.17 (Surgery) Orthopedic History - Physical ExaminationDocument5 pages1.17 (Surgery) Orthopedic History - Physical ExaminationLeo Mari Go LimPas encore d'évaluation
- 2021 CPT CodesDocument8 pages2021 CPT CodesSundar RamanathanPas encore d'évaluation
- NEWBORN CAREPLAN - VEST - FISTULA SurgicalDocument16 pagesNEWBORN CAREPLAN - VEST - FISTULA SurgicalArchana SahuPas encore d'évaluation
- Acknowledgement, AbstractDocument3 pagesAcknowledgement, Abstractpratik borasePas encore d'évaluation
- Meal Planning 1Document12 pagesMeal Planning 1KHALEEL SALEHPas encore d'évaluation
- Medical Imaging WebquestDocument8 pagesMedical Imaging Webquestapi-262193618Pas encore d'évaluation
- DownloaderDocument1 pageDownloaderRizwan FarooqPas encore d'évaluation
- 8 Gene Therapy Alison M BeaneyDocument26 pages8 Gene Therapy Alison M BeaneyDharma DevPas encore d'évaluation
- PE Hyperventilation TopicDocument2 pagesPE Hyperventilation TopicJimmy Jr ChapapPas encore d'évaluation
- Diabetes Nursing AssignmentDocument3 pagesDiabetes Nursing Assignmentmed wardPas encore d'évaluation
- Transfusion-Associated Circulatory Overload (TACO) Draft Revised Reporting CriteriaDocument4 pagesTransfusion-Associated Circulatory Overload (TACO) Draft Revised Reporting CriteriaAarón LinaresPas encore d'évaluation
- Alert-Center Departement of Internal MedicineDocument4 pagesAlert-Center Departement of Internal Medicineሀይደር ዶ.ርPas encore d'évaluation
- A QUASI SynopsisDocument9 pagesA QUASI Synopsischaranjit kaurPas encore d'évaluation
- Rating Criteria: Prior To Woman'S Transfer To The DRDocument3 pagesRating Criteria: Prior To Woman'S Transfer To The DRPatricia Ann JaringPas encore d'évaluation
- Station 5Document25 pagesStation 5adi mustafaPas encore d'évaluation
- Horizontal Thinking in Healthcare Organizations - Edited.editedDocument5 pagesHorizontal Thinking in Healthcare Organizations - Edited.editedJamesPas encore d'évaluation
- HBP 2.0-For Website V2 PDFDocument26 pagesHBP 2.0-For Website V2 PDFapurva shahPas encore d'évaluation