Académique Documents
Professionnel Documents
Culture Documents
Assisted Suicide
Transféré par
Amal B ChandranDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Assisted Suicide
Transféré par
Amal B ChandranDroits d'auteur :
Formats disponibles
ACTION ON ELDER ABUSE (AEA)
ASSISTED DYING BILL
BRIEFING NOTE JULY 2014
Introduction:
Action on Elder Abuse (AEA) focuses upon challenging and preventing the
abuse of older people, whether in the community or institutions. The charity
has been in existence for 21 years.
AEA has no objection to the principle of assisted dying (physician assisted
suicide). This is a moral debate that is not in itself abusive. However, it is the
process, and the associated safeguards, that dictate whether or not the reality
becomes abusive, and it is this that we have addressed in the Bill proposed
by Lord Falconer.
As it stands, we believe that the current Assisted Dying Bill lacks any
meaningful safeguards to protect the interests of people who will be in
the most vulnerable of situations, and we recommend that it should be
opposed in its current form.
The key issues for AEA relate to:
(a)
(b)
(c)
(d)
how individuals may self elect for assisted dying;
how external pressures, including coercion or feelings of family
obligation, may influence a decision to hasten death and what
weight is given to such pressures;
who is nominated to validate that a decision is taken voluntarily, on
an informed basis and without coercion or duress; and
how that validation is undertaken.
This is exclusively about ensuring that people are not coerced, either overtly
or covertly, into self-electing to commit suicide with assistance, that they
understand the implications and options, and have had the opportunity to
consider their decision in an environment that ensures it is genuinely free of
coercion or duress.
Starting Point:
We recognise that the Assisted Dying Bill is focused upon adults who are
terminally ill, and as a consequence of that terminal illness, are reasonably
expected to die within six months. Consequently, as it is drafted, it would not
apply to people simply as a consequence of age or disability.
But this raises a question about the approach adopted and what the Bill is
seeking to address. It is not linked to advance decisions associated with other
factors (e.g. some people might strongly wish to trigger assisted suicide if they
feared a loss of capacity through dementia at some future date). Nor is it
linked to levels of pain or suffering, but seems to focus exclusively on the
likelihood of dying within a short timeframe.
This is not to imply or suggest that other circumstances should be included.
But it raises the question as to whether a diagnosis/prognosis of a terminal
illness, with likely death within six months, is sufficient criterion by itself for
assisted suicide particularly when such prognosis can only be subjectively
established.
Validation of the decision
The witness:
The Bill indicates that the person should sign a declaration in the presence of
a witness who is not a relative or involved in their care/treatment.
What is the purpose of the witness, is it simply to confirm that it really was the
person who signed the declaration? If so, what is the point, as that will
become apparent at the next stage of the declaration?
To be effective, a witness would need to be independent (i.e. not the next
door neighbor or friend who is due to inherit in the Will), able to confirm that
there was no coercion or duress applied and that the decision was free and
genuine. That would be a huge responsibility, with major questions around
how it could be performed effectively. It is akin to the role of an Independent
Mental Capacity Advocate in levels of complexity.
As defined, the witness role seems superfluous to the process and would not
provide any safeguard. It is effectively of no value.
The Medical Practitioners:
The Bill indicates that the medical practitioner from whom the person has
requested assistance, and another medical practitioner independent of the
family and the original practitioner, should countersign the declaration. These
practitioners are to confirm that the person is terminally ill; has the capacity to
make the decision; and voluntarily wishes to end their life on an informed
basis and without coercion or duress.
The prerequisites for undertaking this role are that the doctor holds a
qualification or has experience in respect of the diagnosis and management of
terminal illness.
The Secretary of State may issue a code of practice on assessing whether the
person has capacity to make such a decision; and on recognising and taking
account of the effects of depression or other psychological disorders that may
impair a persons decision-making.
This approach toward validation is exclusively a medical model i.e. it only
considers if someone has mental capacity, or whether they are affected by
cognitive issues that may influence decision-making. However, the
practitioners are not required to be trained in assessing capacity, just the
management of terminal illness, so it is unclear as to how this would be
effectively undertaken in the context of the Mental Capacity Act 2005?
The Bill makes reference to - but does not address coercion, undue
influence or duress, which are major factors in elder abuse, and these issues
do not appear to be considered within the parameters of the Bill. It is unclear
as to how the persons decision would be validated to ensure that it is
genuinely free of coercion or duress? By who? Over what time period?
There are currently major concerns around the potential misuse of Do Not
Attempt Resuscitation notices by medical practitioners in hospitals, and
ageist approaches that are discriminatory in terms of denying treatment based
on age. The spectre of Dr Shipman still haunts the profession. The linking of
this assisted suicide process to a profession that is aimed at healing the sick
is a dangerous one in terms of the messages it sends to people who are frail
or sick; it challenges the basis of the trust that must be integral to the
relationship between the physician and the patient.
Are medical practitioners the best people to undertake this role, or is this
something that should be undertaken by specialists?
To be comfortable with a proposal for assisted suicide, the safeguards need
to be clearly defined in advance, be meaningful and proportionate, and
address a range of factors additional to those affecting mental heath or
capacity. It is about getting to know ad understand the person, their
circumstances, and the external and internal pressures on them. All of this
takes time to do effectively.
The Assisted Dying Bill falls short of meeting these goals in its entirety.
Timeframes:
Medicines will be delivered after a period of not less than 14 days, unless the
doctors agree that a persons death is reasonably expected to occur within
one month in which case this timeframe is reduced to six days.
We understand the reasons why timeframes are short within this proposal.
However
a) this would be insufficient to allow anyone to adequately establish that
coercion or undue influence was not occurring;
b) it would be difficult if not impossible to establish that the decision was a
genuinely informed one, that all suitable alternatives had been
explained, and that it was consequently an informed choice.
The timeframes increase the need for the earlier processes to be robust, that
there is an identified method and process for establishing the actual
circumstances affecting the decision, and for adequate investigation to ensure
the decision is genuinely free of coercion etc.
As it stands, we believe that the current Assisted Dying Bill lacks any
meaningful safeguards to protect the interests of people who will be in
the most vulnerable of situations, and we recommend that it should be
opposed in its current form.
Vous aimerez peut-être aussi
- NotesDocument102 pagesNotesCasey MillerPas encore d'évaluation
- PASSMED MRCP MCQs-DERMATOLOGY PDFDocument53 pagesPASSMED MRCP MCQs-DERMATOLOGY PDFFatima Ema100% (5)
- Vulnerable Adults: Assessing Capacity To ConsentDocument7 pagesVulnerable Adults: Assessing Capacity To ConsentDr Suzanne Conboy-HillPas encore d'évaluation
- Legal and Ethical Issues in Pediatric NursingDocument18 pagesLegal and Ethical Issues in Pediatric NursingTanvi100% (4)
- PPM Informed Consent in Anesthesia WITH FORMSDocument10 pagesPPM Informed Consent in Anesthesia WITH FORMSbalab2311Pas encore d'évaluation
- Cns 780 Know The LawDocument7 pagesCns 780 Know The Lawapi-582911813Pas encore d'évaluation
- Perceived Stress Scale (PSS-10)Document3 pagesPerceived Stress Scale (PSS-10)Amal B Chandran0% (1)
- How To Avoid Ever Having To Write Poor Historian'Document4 pagesHow To Avoid Ever Having To Write Poor Historian'Anyone who wants to download a file...Pas encore d'évaluation
- End of Life Choice Bill - DraftDocument21 pagesEnd of Life Choice Bill - DraftStuff Newsroom100% (1)
- Autonomy & VeracityDocument3 pagesAutonomy & VeracityLovie Japhet LopezPas encore d'évaluation
- Ethical Issues in Geriatric MedicineDocument5 pagesEthical Issues in Geriatric MedicineSPas encore d'évaluation
- Fiel Angelo G. Mallari, RNDocument68 pagesFiel Angelo G. Mallari, RNfiel mallariPas encore d'évaluation
- Ethical Problem in HIV CounselingDocument3 pagesEthical Problem in HIV CounselingandikayusufPas encore d'évaluation
- 1.01. Bioethical PrinciplesDocument26 pages1.01. Bioethical PrinciplesAbi Tabares100% (1)
- Ewbank Opposed To Expanded Civil Commitment Law Oregon SB 187Document38 pagesEwbank Opposed To Expanded Civil Commitment Law Oregon SB 187mary engPas encore d'évaluation
- Legal and Ethical Issues in Pediatric NursingDocument18 pagesLegal and Ethical Issues in Pediatric NursingTanvi0% (1)
- Ethical Issues in Dementia PDFDocument9 pagesEthical Issues in Dementia PDFRebeccaJuryPas encore d'évaluation
- Medical Ethics and Case Studies Part1Document12 pagesMedical Ethics and Case Studies Part1denver cayagaPas encore d'évaluation
- Eol 5 - Arihan Gupta 1Document5 pagesEol 5 - Arihan Gupta 1api-529369011Pas encore d'évaluation
- Decision MakingDocument13 pagesDecision Makingsyafi'udinPas encore d'évaluation
- DNR GuidelinesDocument20 pagesDNR GuidelinesVirendar Pal SinghPas encore d'évaluation
- Ethical Issues in Palliative CareDocument16 pagesEthical Issues in Palliative CarevassalliPas encore d'évaluation
- Module 15: Contemporary Issues in PsychopathologyDocument5 pagesModule 15: Contemporary Issues in PsychopathologyLiz EvermorePas encore d'évaluation
- Decision Making in Incompetent PatientDocument2 pagesDecision Making in Incompetent PatientilhamokPas encore d'évaluation
- Activity CareDocument2 pagesActivity CareJaysette SNPas encore d'évaluation
- Module Ethical Issues of Elder CareDocument18 pagesModule Ethical Issues of Elder CareAlan Roque0% (1)
- Legal and Legislative IssuesDocument24 pagesLegal and Legislative IssuesÀhmâd ÂqéłPas encore d'évaluation
- 17 Living WillsDocument8 pages17 Living WillsKenneth Vercammen, Esq.Pas encore d'évaluation
- Clinical-Legal Issues in PsychiatryDocument26 pagesClinical-Legal Issues in PsychiatrypaulraviPas encore d'évaluation
- Ethical Issues For PLAB 2Document16 pagesEthical Issues For PLAB 2Somchai PtPas encore d'évaluation
- ##2022 Informed Consent NotesDocument11 pages##2022 Informed Consent NotesSANTHIYA A/P MOHANA SUNDARAM MoePas encore d'évaluation
- The Principle of Non MaleficenceDocument1 pageThe Principle of Non MaleficenceClaire Esic PontanarPas encore d'évaluation
- ME Lecture 1, Sept. 5, 20231Document50 pagesME Lecture 1, Sept. 5, 20231Helen Ziqi ZhangPas encore d'évaluation
- What Is Informed ConsentDocument2 pagesWhat Is Informed ConsentMerva LaurentePas encore d'évaluation
- The Principle of Beneficence Written ReportDocument4 pagesThe Principle of Beneficence Written ReportQuin CusayPas encore d'évaluation
- Informed ConsentDocument24 pagesInformed ConsentNoona PlaysPas encore d'évaluation
- Roviech HomeworkDocument3 pagesRoviech HomeworkLegallyPas encore d'évaluation
- Pro Debate - AGDocument3 pagesPro Debate - AGAkilah GilzenePas encore d'évaluation
- Legal and Ethical IssuesDocument22 pagesLegal and Ethical IssuesUdaya Sree100% (4)
- Ethical Legal IssuesDocument29 pagesEthical Legal IssueslisalovPas encore d'évaluation
- Writing Sample 1Document18 pagesWriting Sample 1Shivam TiwaryPas encore d'évaluation
- Penerapan Advokasi Pada Konflik Hukum Kesehatan PreliminaryDocument7 pagesPenerapan Advokasi Pada Konflik Hukum Kesehatan PreliminaryyeniPas encore d'évaluation
- Running Head: Principles of Ethics 1Document7 pagesRunning Head: Principles of Ethics 1mahu2236Pas encore d'évaluation
- Jeselo O. Gorme, RNDocument25 pagesJeselo O. Gorme, RNcoosa liquorsPas encore d'évaluation
- Ethical Issues in The Care of Older PersonsDocument3 pagesEthical Issues in The Care of Older PersonsGodwin Babista GonzalesPas encore d'évaluation
- Elective Patient RightsDocument6 pagesElective Patient Rightsapril punzalanPas encore d'évaluation
- Principles of BioethicsDocument5 pagesPrinciples of Bioethicsbanyenye25Pas encore d'évaluation
- Informed ConsentDocument4 pagesInformed Consentnnaesor_1091Pas encore d'évaluation
- This I Believe 1Document3 pagesThis I Believe 1api-709406220Pas encore d'évaluation
- Major Bioethical PrinciplesDocument44 pagesMajor Bioethical PrinciplesDr. Liza Manalo50% (2)
- HPCA Chapter 3 v6Document14 pagesHPCA Chapter 3 v6saonone100% (1)
- Assisted Suicide Literature ReviewDocument4 pagesAssisted Suicide Literature Reviews1bebopalyn2Pas encore d'évaluation
- PCEP-PC Module 3 NotesDocument22 pagesPCEP-PC Module 3 NotesMan MedPas encore d'évaluation
- 08 PDFDocument16 pages08 PDFMădălina RădulescuPas encore d'évaluation
- AutonomyDocument3 pagesAutonomyMae Jane AuzaPas encore d'évaluation
- MARCOS - Legal Issues of ElderlyDocument2 pagesMARCOS - Legal Issues of ElderlyArian May MarcosPas encore d'évaluation
- Implications of Demographic AgingDocument2 pagesImplications of Demographic Agingjanelle tapiruPas encore d'évaluation
- Implications of Demographics of AgingDocument5 pagesImplications of Demographics of AgingAndrei SubidoPas encore d'évaluation
- Advance Directives 230752 7Document47 pagesAdvance Directives 230752 7api-198352965100% (1)
- Ethical Issues in GeriatricsDocument31 pagesEthical Issues in GeriatricslakshmiPas encore d'évaluation
- Physician Integrity: Why It Is InviolableDocument3 pagesPhysician Integrity: Why It Is InviolableAndrea Villagran100% (1)
- Bioethics Lesson 3Document11 pagesBioethics Lesson 3Jewell Nivera CarpioPas encore d'évaluation
- Non Experimental DesignDocument52 pagesNon Experimental DesignAmal B Chandran100% (1)
- Somatoform DisordersDocument37 pagesSomatoform DisordersAmal B ChandranPas encore d'évaluation
- Mental Health Problems in Old AgeDocument3 pagesMental Health Problems in Old AgeAmal B ChandranPas encore d'évaluation
- Disaster NursingDocument7 pagesDisaster NursingAmal B Chandran100% (1)
- 01 Manajemen Risiko Klinik (MRK)Document32 pages01 Manajemen Risiko Klinik (MRK)irmaPas encore d'évaluation
- Rehabilitation Protocol For Achilles Tendon RepairDocument10 pagesRehabilitation Protocol For Achilles Tendon Repairckpravin7754Pas encore d'évaluation
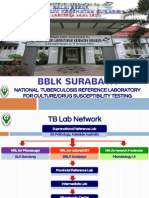
- BBLK Surabaya: National Tuberculosis Reference Laboratory For Culture/Drug Susceptibility TestingDocument12 pagesBBLK Surabaya: National Tuberculosis Reference Laboratory For Culture/Drug Susceptibility TestingMas Paijo PeloukPas encore d'évaluation
- Diass InfographicDocument1 pageDiass InfographicMichaer AmingPas encore d'évaluation
- Pathophysiology DKADocument2 pagesPathophysiology DKALovely CacapitPas encore d'évaluation
- Anatomic Therapy English PDFDocument339 pagesAnatomic Therapy English PDFBabou Parassouraman100% (3)
- List of ClinicsDocument44 pagesList of ClinicswoodksdPas encore d'évaluation
- My Personal Health and Wellness PlanDocument2 pagesMy Personal Health and Wellness PlanLeighsen VillacortaPas encore d'évaluation
- Infliximab: Drug Treatment InformationDocument7 pagesInfliximab: Drug Treatment InformationAlin-Ionuț SălcianuPas encore d'évaluation
- Module 2 (EED119) : Romel Dave Abajar BEED 3-BDocument6 pagesModule 2 (EED119) : Romel Dave Abajar BEED 3-BSkarzy Abajar100% (1)
- Complex Trauma Inventory (CTI) With Scoring Protocol and Psychometric InformationDocument4 pagesComplex Trauma Inventory (CTI) With Scoring Protocol and Psychometric InformationKhoyrunnisaa AnnabiilahPas encore d'évaluation
- Guards Performance Appraisal Form by ClientsDocument3 pagesGuards Performance Appraisal Form by ClientsAMBE B. AMBEPas encore d'évaluation
- Empirically Supported Complexity: Rethinking Evidence-Based Practice in PsychotherapyDocument6 pagesEmpirically Supported Complexity: Rethinking Evidence-Based Practice in PsychotherapyPedro VargasPas encore d'évaluation
- Assessing Cognitive Impairment in Patients With SchizophreniaDocument5 pagesAssessing Cognitive Impairment in Patients With SchizophreniaShifa TifarinPas encore d'évaluation
- Omeprazole Drug StudyDocument8 pagesOmeprazole Drug StudyJe Michelle LoayonPas encore d'évaluation
- Canadas Food Guide Serving SizesDocument2 pagesCanadas Food Guide Serving SizesVictor EstradaPas encore d'évaluation
- DKA-FBF2007-#04-Prometheus BooksDocument71 pagesDKA-FBF2007-#04-Prometheus Booksapi-3766294100% (1)
- Physical Examination ScoliosisDocument7 pagesPhysical Examination Scoliosisyosua_edwinPas encore d'évaluation
- BrufenDocument4 pagesBrufensofronije2005Pas encore d'évaluation
- EFG Healthcare - BrochureDocument2 pagesEFG Healthcare - BrochuremikewiesenPas encore d'évaluation
- Doctors Progress Note - Module 5Document4 pagesDoctors Progress Note - Module 5adrian nakilaPas encore d'évaluation
- PPT-Leukemic Retinopathy Upload 1Document4 pagesPPT-Leukemic Retinopathy Upload 1Herisa RahmasariPas encore d'évaluation
- Name: Ponce, Christian Neil P. Subject: CHN2 Course and Year: Bsn3 Block1. Code:N113Document3 pagesName: Ponce, Christian Neil P. Subject: CHN2 Course and Year: Bsn3 Block1. Code:N113Novelyn PuaPas encore d'évaluation
- Acute Herpetic Gingivostomatitis Associated With Herpes Simplex Virus 2Document4 pagesAcute Herpetic Gingivostomatitis Associated With Herpes Simplex Virus 2Ayu KartikaPas encore d'évaluation
- Final Exam Review NutritionDocument9 pagesFinal Exam Review Nutritionjenm1228Pas encore d'évaluation
- Procedural Dermatology CmeDocument3 pagesProcedural Dermatology CmePadmapriya SrinivasanPas encore d'évaluation
- Fundamentals of NursingDocument268 pagesFundamentals of Nursinguhta100% (1)
- Molluscum ContagiosumDocument15 pagesMolluscum ContagiosumАминаа ТавинбэхPas encore d'évaluation