Académique Documents
Professionnel Documents
Culture Documents
Abnormalities in Estrogen
Transféré par
Néstor MirelesCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Abnormalities in Estrogen
Transféré par
Néstor MirelesDroits d'auteur :
Formats disponibles
Abnormalities in Estrogen, Androgen,
and Insulin Metabolism in Idiopathic
Hemochromatosis"
WOLFGANG STREMMEL," C L A U S NIEDERAU,&
MICHAEL BERGER," H A N S - K U N O K L E Y , d
HANS-LUDWIG KRUSKEMPER," A N D
GEORG S T R O H M E Y E R ~
Divisions of hGastroenterology, "Metabolism
and Nutrition, and dEndocrinology
Dusseldorf University Medical Center
Dusseldorf, Federal Republic of Germany
INTRODUCTION
Impotence and diabetes mellitus are two prominent clinical features of idiopathic hemochromatosis. Since the major complication of iron overload disease is
cirrhosis of the liver, it might be assumed that the pathogenesis of these metabolic
alterations may be secondary to impaired liver function. Patients with advanced
liver disease frequently show glucose intolerance and male cirrhotics often suffer
from impotence, revealing testicular atrophy and evidence of feminization. It is
conceivable that clearance of insulin and estrogens is impaired by a reduction in
the functional liver cell mass, producing insulin resistance as well as hypogonadism and feminization. However, this hypothesis has been challenged by several
studies that evaluated the clinical features and patterns of hormone disturbances
in different types of chronic liver disease.'.2 The underlying cause of the liver
disease, rather than hepatic dysfunction per se, has been shown to determine the
endocrine and metabolic alteration^.^ In this paper the various factors in the
development of hypogonadism and diabetes in idiopathic hemochromatosis will
be evaluated and compared to other chronic liver diseases such as alcoholic
cirrhosis.
HYPOGONADISM
As shown in a large series of patients with various types of cirrhosis, loss of
libido was found in 80% of the patients with idiopathic hemochromatosis and in
71% of the patients with alcoholic cirrhosis, whereas in cirrhosis due to chronic
active hepatitis or in cryptogenic cirrhosis (unknown etiology) this symptom was
only present in 3% and 7% of the cases, respectively.' Similarly, testicular atrophy was shown to be a prominent feature in idiopathic hemochromatosis and
alcoholic cirrhosis, whereas it was almost absent in chronic active hepatitis (FIG.
l ) , ' One interesting finding was that in 44 nonalcoholic male patients with hemochromatosis, who were diagnosed in an early stage, 25% already suffered from
This work was supported by grant no. IV B 5-40200287 from the Minister fur Wissenschaft und Forschung des Landes Nordrhein-Westfalen.
209
210
ANNALS NEW YORK ACADEMY OF SCIENCES
impotence in the absence of any histological or biochemical evidence of liver
di~ease.~
Since there was no correlation between the severity of histological alteration
in liver architecture and the degree of the observed endocrinopathy, it was concluded that impotence is not secondary to hepatic dysfunction. In order to determine the underlying metabolic abnormality leading to testicular atrophy in idiopathic hemochromatosis, the effect of iron overload disease on gonadal function
was analyzed in these male patients.
Physiology of Sexual Hormone Metabolism in Men
Sexual hormone metabolism is organized along the hypothalamic-pituitarygonadal axis (FIG.2).4 The hypothalamus integrates numerous stimuli from higher
centers in the brain as well as hormonal signals in the form of sex steroid concentrations. Accordingly, luteinizing hormone releasing factor (LHRH) is excreted,
which stimulates the pituitary gland to synthesize and release gonadotropins.
Follicle-stimulating hormone (FSH) promotes spermatogenesis in the reproductive component of the gonads, the seminiferous tubules, whereas luteinizing hormone (LH) stimulates the endocrine component of the testes, the Leydig cells, to
secrete testosterone. Products of both of these gonadal components circulate and
inhibit the release of hypothalamic LHRH and pituitary gonadotropin secretion.
Under physiologic conditions some testosterone is secreted also by the adrenal
cortex, and a small amount is converted by peripheral tissues (liver, adipose, and
neural tissue) from androstendione (FIG.2). Primary failure of the testes is characterized by atrophy of the germinal epithelium and reduced peripheral sexual
hormone concentrations, but is associated with increased gonadotropin levels.
Primary failure of the hypothalamus or pituitary, in contrast, is characterized by
reduced levels of gonadotropins as well as evidence of gonadal failure.
FIGURE 1. Loss of libido and testicular atrophy in 414 patients with various types of liver
cirrhosis (modified from data of Powell er a/.').
STREMMEL el 01.: ENDOCRINE ABNORMALITIES
211
I I
Plannm
Tmtatora
I
SprmOt~OO
FIGURE 2. The hypothalamic-pituitary-gonadalaxis and origins of circulating testosterone
in a normal man. (From Morgan and Pratt4. Reprinted with permission from the British
Medical Bulletin.)
Gonadal Histology
Histologic studies of the testicular tissue obtained from patients with idiopathic hemochromatosis and a history of severe loss of libido usually demonstrate
a variable degree of atrophy of the seminiferous tubules with scanty mitoses,
absent spermatozoa and spermatids, and thickening of the tubular walls (FIG.3).*
Leydig cells are present in reduced numbers or absent. Similar histological alterations are observed in male alcoholics.' However, while in patients with chronic
alcohol consumption testicular atrophy is known to be primarily caused by the
direct toxic effect of alcohol or acetaldehyde,6there was no indication of primary
testicular destruction due to iron overload of the tissue. In fact, stainable iron was
either absent or found in only slight amounts, predominantly localized in the
blood vessel walls, regardless of whether or not the hemochromatosis had been
treated by venesection.
Plasma Sexual Hormone and Gonadotropin Concentrations
For further evaluation of whether impotence in idiopathic hemochromatosis
originates from testicular or hypothalamic-pituitary dysfunction, plasma sexual
hormone and gonadotropin concentrations were determined. In nonalcoholic hemochromatotic males, impairment of sexual function was accompanied by a sig-
212
ANNALS NEW YORK ACADEMY OF SCIENCES
nificant decrease in plasma testosterone levels to 2.79 5 0.79 ng/ml, compared to
5.90 & 1.20 ng/ml in healthy control^.^ Since the sex steroid binding protein
(SHBG) was found to be in the normal
it is obvious that the free, biologically active testosterone concentration is also very low. Similar results were
obtained in chronic alcoholics. However, SHBG levels were significantly increased, indicating that the biologically active free testosterone is even more
depressed in alcoholic liver disease than in idiopathic hemochromato~is.~~~
However, there was a distinct difference in plasma levels of gonadotropins in
the two diseases (FIG.4). In chronic alcoholics, LH and FSH were found to be
increased.z@ When critically assessed, however, these elevated concentrations
seem inappropriately low for the degree of gonadal failure present and suggest
that, in addition to a primary gonadal failure, an element of hypothalamic-pituitary failure also exists in such men. This is confirmed by an inadequate response
to LHRH and clomiphene in the majority of chronic alcoholic^.^^^ In contrast,
FIGURE 3. Photomicrograph of a testicular biopsy from a hemochromatotic male with
testicular atrophy.
two-thirds of the nonalcoholic patients with idiopathic hemochromatosis revealed
a decrease in plasma FSH and LH levels with little or no response to clomiphene
or LHRH.&I4Furthermore, patients with idiopathic hemochromatosis and deficient gonadotropin secretion were reported to have an impaired prolactin response to thyrotropin-releasing hormone (TRH).l2-l4 Depressed gonadotropin levels and lack of response by hypothalamic stimulation could result from iron
deposition in the pituitary, which was shown to occur in 86% of a series of 57
autopsy cases. I5 In fact, iron was preferentially localized in the gonadotropic cells
of hemochromatotic patients, as shown by a combined immunocytochemicaland
Prussian blue staining technique (FIG. 5).16 Only a minority of thyrotropic,
corticotropic or somatotropic cells contained iron. I6 Therefore, panhypopituitarism with hypothyroidism and adrenal cortical insufficiency is a rare event in
hemochromatosis.l4
The preceding observation indicates that testicular atrophy in patients with
STREMMEL ef al.: ENDOCRINE ABNORMALITIES
213
basal
maximal
UIITROL
basal
max I MaI
HYlCHRMlTOSlS
YCMlllC CIRR)(OsIS
FIGURE 4. Luteinizing hormone (LH) levels after stimulation with LH-releasing hormone
(LHRH) in healthy controls and in patients with idiopathic hemochromatosis and alcoholic
cirrhosis. Values are means 2 SD.8
FIGURE 5. Immunocytochemical and Prussian blue staining of iron deposits in gonadotropic cells of the pituitary gland from a patient with idiopathic hemochromatosis (immunoperoxidase technique for P-LH and Prussian blue reaction, magnification 400x, black-andwhite reproduction). Dark iron-positive granules are apparent in many gonadotrophs. (From
Bergeron and Kovacs.I6 Reprinted with permission from the American Journal of Pafhology.)
ANNALS NEW YORK ACADEMY OF SCIENCES
214
idiopathic hemochromatosis is due to insufficient gonadotropin secretion caused
by the selective accumulation of iron in gonadotropic cells of the pituitary gland,
whereas in alcoholic cirrhosis testicular destruction is predominant. A marked
difference between these two diseases is further evident with regard to estrogen
metabolism. Hyperestrogenism is clinically apparent as feminization of male patients. Gynecomastia, vascular spiders, and changes in body hair and fat distribution are frequent features of hyperestrogenism, and are commonly observed in
alcoholic cirrhosis. Gynecomastia has been reported in up to 66% of alcoholics,
irrespective of the presence of liver d i s e a ~ e . ~ .Biochemical
I~-~~
evidence of hyperestrogenism in such men is documented by an increase in estrogen-responsive
proteins, such as prolactin, sex steroid binding protein (SHBG), and estrogenresponsive neurophysin.18,20,2~29 Gynecomastia in patients with idiopathic hemochromatosis is less common than in other forms of cirrhosis, especially alcoholic c i r r h ~ s i s . ~ In
- ~the
* ~ 60
* ~of our male patients suffering from impotence, none
was found to have gynecoma~tia.~
The same was true for the frequency of spider
naevi as well as for the concentrations of estrogen-responsive protein^.^^^*'^ Since
patients with idiopathic hemochromatosis had no clinical signs of hyperestrogenism, it was of particular interest to measure the actual estrogen concentration and
its formation in these nonalcoholic men. As is evident from FIGURE6, these
patients have normal levels of estron (El) and estradiol (E2).7Furthermore, metabolic clearance rates of estrogens were unaltered and the ratios of peripheral
conversion from androgens to estrogens were the same as for the control group
(FIG.7).' In contrast, a significant increase in estrogen formation was observed in
alcoholic men.7This increase resulted from ethanol-induced stimulation of aromatase activity, an enzyme that converts androgens to estrogens. The elevation of
the precursor androgen androstendione, which is hypersecreted in response to
alcohol stimulation, contributes to this increase in estrogen
ESTROWE
p<O.Ol
ESTRAOIU.
.I
MwTtiUS
FIGURE 6. Plasma concentrations of estrone and estradiol in healthy controls and in
patients with hemochromatosis and alcoholic cirrhosis. Values are means 2 SD.'
215
STREMMEL el a/.: ENDOCRINE ABNORMALITIES
p ' 0.01
_
.
IK
Lc
IK
u:
IK
LC
IK
u:
FIGURE 7. Conversion ratio of testosterone (T) and androstendione (A) to estrone (El)and
estradiol (E2) in patients with idiopathic hemochromatosis (IHC) and alcoholic cirrhosis
(AC) and in healthy controls ( C ) . Values are means SD.'
Although both iron overload disease and chronic alcohol consumption significantly reduce free plasma testosterone levels, independently of accompanying
liver disease, studies of plasma estrogen concentration have often shown variable
results. Therefore, it was suggested that the severity of liver disease might have
some additional impact on peripheral estrogen levels. A clue to this problem was
given by the observation that not liver disease or even cirrhosis per se, but portal
hypertension, a potential consequence of any kind of cirrhosis, might contribute
to hyperestrogenism in such patients.jOIn the rat model experimentally induced
portal hypertension leads to a 70% increase of plasma E2 levels, even in the
absence of liver damage.3 The following underlying pathogenetic mechanism was
proposed (FIG.8).jl Physiologically, only a small fraction of androgens circulate
to sex-steroid-dependent tissues, whereas a larger fraction is metabolized by the
liver, excreted into bile, deconjugated in the intestinal lumen, reabsorbed, and
returned to the liver, where it is efficiently removed and reenters the enterohepatic circulation. As a consequence of portosystemic shunting, a larger proportion of androgens escape the hepatic recycling process and are distributed to
peripheral sex-steroid-dependent tissues, where they are converted to estrogens.
Further studies are needed to confirm this hypothesis.
Therapeutic Consequences
Impotence, a common early symptom of idiopathic hemochromatosis, is one
of the few clinical features of the disease that often cannot be improved by
venesection therapy.32The reason remains a subject of speculation. Symptomatic
treatment with testosterone has been proposed and shown to be b e n e f i ~ i a l . ~ ,In
'.~~
216
ANNALS NEW YORK ACADEMY OF SCIENCES
FIGURE 8. Enterohepatic circulation of sex steroids under (a)
normal circumstances and (b) as
it occurs with portosystemic
shunting due to portal hypertension. (From Van Thiel el aL6 Reprinted with permission from
Thieme-Stratton, Inc.)
view of the predominant hypothalamic-pituitar'y failure, the lack of feminization,
and undisturbed estrogen metabolism, treatment with testosterone in patients
with hemochromatosis is not expected to be associated with hyperestrogenism as
a side effect. In contrast, administration of testosterone to patients with alcoholic
cirrhosis revealed a significant additional increase in estrogen levels, provoking
prominent feminization, and should therefore be avoided.34The aim of androgen
therapy in hypogonadal men with hemochromatosis is to restore or improve secondary sexual characteristics and male sexual behavior, and to mimic the hormonal effects on somatic development. The parenteral application of a long-acting
testosterone ester, such as 250 mg testosterone enanthate, at 3- to 4-week intervals results in a sustained increase in plasma testosterone towards the normal
range for males. Altough androgens do not restore spermatogenesis in hypogonadal states, resumption of normal sexual activity is to be expected following
adequate replacement.
There are also several reports of hemochromatosis in young female patients.3s
STREMMEL er al.: ENDOCRINE ABNORMALITIES
217
In most of these patients amenorrhea was the leading symptom. In contrast to
male patients, endocrine abnormalities in females may sometimes respond to iron
removal. However, the exact nature of the endocrine abnormalities in female
patients has not as yet been thoroughly studied.
PATHOLOGIC GLUCOSE TOLERANCE
As stated above, impotence in idiopathic hemochromatosis is characterized by
insufficient gonadotropin secretion due to iron deposition in the gonadotropic
cells of the pituitary gland. Disturbance in carbohydrate metabolism in hemochromatotic patients is also related to the specific pattern of iron accumulation in the
organism. The close association between diabetes mellitus and hemochromatosis
is well known. In most of the recent studies, the prevalence of diabetes in idiopathic hemochromatosis is reported to be about 50-60%.3s39In our own series of
166 patients with idiopathic hemochromatosis, 54.5% had overt diabetes. Of the
remaining patients, 10.3% had a pathologic glucose tolerance test, while 45.5% of
the patients revealed normal carbohydrate m e t a b ~ l i s m . ~
Liver Disease and Carbohydrate Intolerance
It is well established that liver disease per se and particularly cirrhosis with
portosystemic shunting is associated with glucose intolerance. Although the
mechanism of this impaired glucose utilization is still controversial, it was suggested that an alteration in the handling of insulin may be of importance. Physiologically, 50% of the insulin secreted by the pancreas is removed by its first
passage through the l i ~ e r . ~In. ~cirrhosis
'
and in fatty liver the capacity for insulin
extraction is markedly reduced, while insulin secretion remains unaltered.4246
Thus, peripheral circulating insulin levels are increased. Despite elevated plasma
insulin concentrations, hyperglycemia is common, suggesting that peripheral insulin resistance is responsible for the observed glucose intolerance. Whether
diminished glucose utilization is due to the presence of yet unidentified insulin
antagonists, to alterations in the insulin receptor status, or to a postreceptor event
is still ~ n k n o w n . ~ '
However, the prevalence of diabetes varies considerably among the various
types of liver disease leading to c i r r h o ~ i s . ' . ~In
* *a~ ~study of 414 patients with
hepatic cirrhosis, 49.3% (203) presented glycosuria at the time of diagnosis.'
Carbohydrate intolerance occurred in 19.1% of patients with a history of chronic
alcohol consumption. It was found in 5.3% of patients with chronic active hepatitis, and in 25% of patients with cryptogenic cirrhosis. In contrast, in iron overload
disease (either genetically induced as in idiopathic hemochromatosis or in secondary forms, mainly due to frequent transfusions) glucose intolerance and overt
diabetes was observed in 72.3% of the patients. This is significantly more frequent
than one would expect from the degree of liver disease in these iron overload
diseases. 1.37.48.49
Specific Eflects of Iron Overload Disease on Insulin Metabolism
There are two main pathogenetic factors that contribute to carbohydrate intolerance in hemochromatosis: (1) impaired insulin secretion caused by accumulation of excess iron in B-cells of the pancreas, and (2) insulin resistance due to
ANNALS NEW YORK ACADEMY OF SCIENCES
218
hepatocellular dysfunction. On the basis of carefully conducted family studies37.5s52and the observation that glucose intolerance is as frequent in secondary
as in idiopathic h e m o c h r o m a t ~ s i s ,the
~ ~ *suggestion
~~
of an additional genetic
factor in the development of diabetes seems highly unlikely.
In advanced stages of iron overload disease, impaired insulin secretion is the
main diabetogenic event.38.5s57A study by Stocks and Powell showed that in
patients with hemochromatosis and diabetes insulin response to oral glucose was
very poor and even less than in patients with idiopathic diabetes mellitus (FIG.
9).38This impaired insulin secretion is caused by selective deposition of excess
It is conceivable that the specific
iron in the B-cells of the pancreas (FIG.
distribution pattern of transferrin receptors is responsible for the selective effect
on B-cells, while A-cells remained unchanged. Accordingly, plasma glucagon
levels were reported to be in the normal range.59Moreover, other contrainsulinemic hormones such as growth hormone were not found to be increased.60
Furthermore the enteroinsulinaraxis, represented by the plasma concentration of
gastric inhibitory polypeptide (GIP), remained unaltered by iron overload disease.61
Impaired secretion of insulin in advanced hemochromatosis is accompanied by
diminished glucose utilization. There had been a long controversy over whether
this is due to insulin resistance commonly observed in cirrhosis of the liver or
represents a specific effect of iron overload disease. A clue to this problem became apparent when carbohydrate and insulin metabolism was evaluated in noncirrhotic patients with hemochromatosis and normal serum glucose concentratiom6' Characteristically, after an oral glucose load (100 g) these patients
revealed normal glucose tolerance but significant hyperinsulinemia compared to
healthy controls (FIG.11). In the presence of normal pancreatic insulin secretion,
determined by C peptide concentrations, and in the absence of disturbances in
glucagon, growth hormone, and GIP metabolism, these high plasma insulin concentrations result from diminished clearance of insulin by the liver or other insulin-dependent tissues.6' Most likely, iron accumulation in hepatocytes may be
responsible for the impaired degradation of insulin. Whether a reduced number of
A
IDlDPAlHlC DIAETES
M-
#/'
- z
--____
____---------
,r-OC#OO
/-.O----
-5 *-
,0--
/'
*/-*-*-*
P-*"
i -
a
d
0-
LEUITUS
HMC~TOSIS
n - /*'
o'
I *
STREMMEL ct ul.: ENDOCRINE ABNORMALITIES
219
FIGURE 10. Selective accumulation of excess iron in pancreatic B-cells in a patient with
idiopathic hemochromatosis and insulin-dependent diabetes mellitus. Double staining technique of pancreatic tissue: Frussian blue method for iron detection and peroxidase-antiperoxidase technique with anti-insulin serum. In this black-and-while reproduction the dark
cytoplasmatic staining represents iron deposits in pancreatic B-cells. (From Rahier er aI.*
Reprinted with permission from Diahetologia.)
insulin receptors or postbinding events compatible with insulin resistance are
responsible for this phenomenon remains to be established. Thus, it appears that
not only severe structural changes of the liver architecture with intra- and extrahepatic shunting, but also distinct functional alterations due to the specific effects
of intrahepatic iron deposition, contribute to the observed alteration in insulin
metabolism. This hypothesis is further supported by the observation that in those
noncirrhotic patients with idiopathic hemochromatosis, who revealed elevated
insulin concentrations after an oral glucose load at the time of diagnosis, increased insulin concentrations gradually returned to normal values with depletion
of the body iron stores. After 18 months of phlebotomy treatment none of these
patients revealed impaired insulin clearance or pathologic glucose tolerance after
an oral glucose load (unpublished observation). Moreover, also in the patients
with hyperglycemia, a significant improvement of carbohydrate metabolism was
achieved solely by venesection therapy. Although insulin-dependent diabetes was
not reversible, due to the destruction of the B-cells of the pancreas, in 33% of
these patients the insulin dose could be significantly reduced (by a mean of 8.6 U/
day) after complete iron depletion had been achieved. In the remaining patients
with glucose intolerance (non-insulin-dependent diabetes, impaired glucose tolerance) carbohydrate metabolism could be improved in about half of the patients by
phlebotomy treatment.
CONCLUSION
Impotence and disturbance in carbohydrate metabolism in idiopathic hemochromatosis are caused by the specific distribution pattern of excess iron in the
ANNALS NEW YORK ACADEMY OF SCIENCES
220
20 1
GLUCOSE
1oog glucor.
p.0.
TIME
[min]
C PEPTIDE
-10 0
"7
"
30
100g glucose
P.O.
90
60
TIME
120
180
[min]
INSULIN
-10 0
t
10og glucor.
30
60
90
120
180
TIME [min]
FIGURE 11. Circulating concentrations of glucose, C peptide, and insulin after a 100-g oral
glucose load in patients with noncirrhotic hemochromatosis (solid lines) and sex-, age-,
weight-, and height-matched healthy controls (dashed lines).6'
STREMMEL el al.: ENDOCRINE ABNORMALITIES
221
organism. Testicular atrophy results from insufficient gonadotropin secretion due
to iron accumulation in gonadotropic cells of the pituitary gland. The pathogenetic
factors in the development of diabetes include impaired insulin secretion caused
by the selective deposition of iron in the B-cells of the pancreas and insulin
resistance due to iron accumulation in the liver. Structural alteration of liver
architecture and porto-systemic shunting in advanced iron overload disease may,
in addition, contribute to the observed endocrinopathies.
SUMMARY
Of 44 male patients with idiopathic hemochromatosis who were diagnosed at
an early stage without morphological or biochemical evidence of liver disease,
25% suffered from impotence and 34% manifested glucose intolerance. Impotence
was correlated with a 50% reduction in plasma testosterone, resulting from a 63%
decrease in testosterone production. Testicular atrophy was caused by insufficient secretion of gonadotropins due to the selective accumulation of iron in
gonadotropic cells of the pituitary gland. However, peripheral sexual hormone
metabolism, in particular the conversion of androgens to estrogens, remained
unaltered. It was therefore possible to employ substitution therapy successfully
with testosterone in these men, and hyperestrogenism was not observed as a side
effect. The pathogenetic factors in the development of diabetes mellitus in patients with idiopathic hemochromatosis include impaired insulin secretion caused
by the selective deposition of iron in B-cells of the pancreas and insulin resistance
due to iron accumulation in the liver. In particular, the insulin resistance is markedly improved after depletion of body iron stores by phlebotomy treatment, resulting in lower insulin requirements in patients with insulin-dependent diabetes
as well as improvement of carbohydrate metabolisms in about half of the patients
with non-insulin-dependent diabetes. We have concluded that hypogonadism and
carbohydrate intolerance are caused by the specific distribution pattern of excess
iron in the organism, accompanied by functional impairment of affected parenchymal cells.
REFERENCES
I . POWELL,L. W., R. MORTIMER
& 0. D. HARRIS.1971. Med. J. Aust. 1: 941-950.
2. STREMMEL,
W., H. K. KLEY,H. L. KROSKEMPER
& G. STROHMEYER.
1985. Semin.
Liver Dis. 5: 84-93.
3. NIEDERAU,
A. SONNENBERG,
W. STREMMEL,
H. J. TRAMPISCH
& G.
C., R. FISCHER,
STROHMEYER.
1985. N. Engl. J . Med. 313: 1256-1262.
4. MORGAN,
M. Y. & 0. E. PRATT.1982. Br. Med. Bull. W. 43-52.
5. VAN THIEL,D. H., R. LESTER& R. J. SHERINS.
1974. Gastroenterology 67: 1188-1 199.
6. V A N THIEL,D. H. , J. S. GAVALER
& R. R. SCHADE.1985. Semin. Liver Dis. 5: 35-45.
7. KLEY,H. K., C. NIEDERAU,
W. STREMMEL,
R. LAX, G. STROHMEYER
& H. L.
KROSKEMPER.
1985. J. Clin. Endocrinol. Metab. 61: 1-6.
8. KLEY,H. K., W. STREMMEL,
C. NIEDERAU,
R. HEHRMANN,
0. SHAMS,G. STROHMEYER & H. L. KRUSKEMPER.
1985. Hepatology 5: 251-256.
9. MOVAT,N. A. G., C. R. W. EDWARDS,
R. FISHER,A. S. MCHEILLY,
J. R. B. GREEN
& A. M. DAWSON.1976. Gut 17: 345-350.
10. TOURNIARE,
J., M. FEVRE,
B. MAZENOD& G. PONSIN.1974. J. Clin. Endocrinol.
Metab. 39: 1122-1 124.
11. BEZWODA,
W. R.,T. H. BOTHWELL,
L. A. VAN DER WALT,S. KRONHEIM
& B. L.
PIMSTONE.
1977. Clin. Endocrinol. 6 377-385.
ANNALS NEW YORK ACADEMY OF SCIENCES
222
12. WALTON,C., W. F. KELLY,I. LAING& D. E. BULLOCK.
1983. Q.J. Med. 52: 99-110.
J. P., T. DARRAGON,
J. CAROFF& J. LE ROY. 1979. Semin. Hop. Paris 55:
13. BERCOVICI,
1606- 1612.
14. MCNEIL,L. W., L. C. MCKEE,D. LORBER& D. RABIN.1983. Am. J. Med. Sci. 185:
7-13.
R. A. & G. K. MALLORY.1960. Arch. Intern. Med. 105: 686-700.
15. MACDONALD,
C. & K. KOVACS.1978. Am. J. Pathol. 93:295-306.
16. BERGERON,
17. KLEY,H. K., E. NIESCHLAG,
W. WIEGELMANN
& H. G. SOLBACH.
1975. Acta Endocrinol. (Copenhagen) 79: 275-285.
18. VAN THIEL,D. H. & R. LESTER.1979. Hypothalamic-pituitary-gonadal dysfunction in
patients with alcoholic liver disease. In Problems in Liver Disease. C. S. Davidson,
Ed.: 286-298. Stratton Intercontinental Medical Book Corporation. New York.
J., N. FABRICIUS-BJERRE,
N. BAHNSEN,
P. BOISEN,L. BANGSTRUP,
M.
19. LINDHOLM,
& L. HAGEN.1978. Eur. J. Clin. Invest. 8: 269-272.
LAVPEDERSEN
J. S., D. H. VAN THIEL& R. LESTER.1980. Alcoholism (New York) 4: 27120. GAVALER,
276.
BAKER,H. W. G., H. G. BURGER,
D. M. DE KRETSER,A. DULMARIS,
B. HUDSON,S.
OCONNOR,
C. A. PAULSEN,
H. PURCELL,
G. C. RENNIE,C. S.SEAH,H. P. TAFT&
C. WANG.1976. Q. J. Med. 45: 145-178.
W. H. J., C. S. DAVIDSON,J. H. DIBLE,G.K. MALLORY,
S. SHER22. SUMMERSKILL,
LOCK,M. D. TURNER
& S.J. WOLFE.1960. N. Engl. J. Med. 262 1-10.
23. GALVAO-TELES,
A., D. C. ANDERSON,
C. W. BURKE,J. C. MARSHALL,
C. S. CORKER,
R. L. BROWN& M. L. CLARK.1973. Lancet 1: 173-177.
24. CHOPRA,J. D., D. TULCHINSKY
& F. L.GREENWAY.
1973. Ann. Intern. Med. 79: 198-
21.
203.
L. A,, J. SAGEL,B. DUBOWITZ,G. KAY,P. J. CARR,M. KATZ& M. C.
25. DISTILLER,
KEW. 1976. Horn. Metab. Res. 8: 461-465.
26. FARNSWORTH,
W. E., A. H. CAVANOUGH,
J. R. BROWN,I. ALVAREZ& L. M.
LEWANDOWSKI.
1978. Arch. Androl. 1: 193-195.
27. LIEGEL,J., L. F. FABRE,P. Y.HOWARD
& R. W. FARMER.
1972. Physiologist 15: 198.
28. LINDHOLM,
J., N. FABRICIUS-BIERRE,
M. BAHNSEN,P. BOJESEN,C. HAGAN& T.
CHRISTENSEN.
1978. Eur. J. Clin. Invest. 8: 273-276.
29. VANTHIEL,D. H., J. S.GAVALER,
R. LESTER,D. L. LORIAUX
& G. D. BRAUNSTEIN.
1975. Metabolism 24: 1015-1019.
30. VAN THIEL,D. H., J. S. GAVALER,
F. L. SLONE,C. F. COBB,W. I. SMITH,K. M.
BRON& R. LESTER.1980. Gastroenterology 78: 81-91.
31. VAN THIEL,D. H. 1982. Mechanism for feminization occurring in chronic alcoholic
men. In The Endocrines and the Liver. M. Langer, L. Chiandussi. I. J. Chopra & L.
Martini, Eds.: 147-151. Academic Press. New York.
C., W. STREMMEL
& G. STROHMEYER.
1981. Internist 2 2 546-554.
32. NIEDERAU,
1955. Medicine 34: 381-430.
33. FINCH,S. C. & C. A. FINCH.
34. KLEY,H. K., G. STROHMEYER
& H. L. KRUSKEMPER.
1979. Gastroenterology 7 6
234-241.
35. LAMON,J. M., S. P. MARYNICK,
R. ROSENBLATT
& S. DONNELLY.
1979. Gastroenterology 7 6 178-184.
36. BALCERZAK,
S. P., D. H. MINTZ& M. P. WESTERMANN.
1968. Am. J. Med. Sci. 255:
53-62.
37. DYMOCK,
W. & R. WILLIAMS.
1971. Postgrad. Med. J. 47(Suppl.): 79-83.
38. STOCKS,A. E. & L. W. POWELL.1973. Q. J. Med. 42: 733-749.
39. NIEDERAU,
C., W. STREMMEL
& G. STROHMEYER.
1981. Internist 22: 546-554.
E., J. ZAVARONI,
C. COSCELLI&I U. BUTTURINI.
1983. Metabolism 32: 43840. BONORA,
446.
41. SAMOL,E. & J. A. RYDER.1%1. J. Clin. Invest. 40.2092-2102.
42. OLEFSKY,J. M. 1982. Gastroenterology 83: 1313-1318.
A,, D. G. JOHNSTON,
K. G. M. M. ALBERTI,N. NATTRASS
& R. WRIGHT.
43. STEWARD,
1983. Eur. J. Clin. Invest. W: 397-403.
D. G. & K. G. M. M. ALBERTI.1976. Clin. Endocrinol. Metab. 5: 657-702.
44. JOHNSTON,
G. 1979. Z. Gastroenterol. 17: 462-468.
45. SMITH-LAING,
STREMMEL et af.: ENDOCRINE ABNORMALITIES
223
46. GRECO,A. V.,G. FEDELI,G. GHIRLANDA,
F. CRUCITTI,R. MANNA,L. ALTOMONTE,
A. G. REBUZZI& A. BERTOLI.1979. Diabetologia 17: 23-28.
47. PETRIDES,A. S . & G. STROHMEYER.
1986. Gastroenterol. 24: 403-415.
48. MEGYESI,K., E. SAMOLS& V. MARKS.1967. Lancet 2: 1051-1055.
W., H. FRERICHS
& K. SICKINGER.
1970. Prog. Liver Dis. 3: 371-407.
49. CREUTZFELDT,
1974. Clin. Genet. 5: 242-247.
50. SADDI, R. & J. FEINGOLD.
J. R. WRIGHT,J. TOBIN&
51. ROWE,J. W., J. R. WANDS,E. MEZEY,L. A. WATERBURY,
R. ANDRES.1977. Medicine (Baltimore) 5 6 197-211.
I. A. KOURIDES&
52. FELLER,E. R., A. PONT,J. A. WANDS,E. A. CARTER,G. FOSTER,
K. J. ISSELBACHER.
1977. N. Engl. J. Med. 2 % 1422-1426.
K., B. MOLINAR,A. HIRT, P. IMBACH,E. GUGLER,0. T ~ N &
Z R. P.
53. ZUPPINGER,
ZURBROGG.1979. Helv. Paediatr. Acta 34: 197-207.
54. COSTIN,G., M. D. KOGUT,C. HYMAN& J. A. ORTEGA.1977. Diabetes 26: 230-240.
W. STAUFFACHER
& D. POMETTA.1973. Eur.
55. BIERENSDE HAAN,B., J.-C. SCHERRER.
J. Clin. Invest. J: 179-187.
J. W., J. CASSAR,D. A. PYKE,W. G. OAKLEY& R. WILLIAMS.1972. Am. J.
56. DYMOCK,
Med. 5 2 203-210.
M., M. LINDEMANN,
C. ROSAK,K. SCHALK,P. KALTWASSER
& P. H.
57. NEUBAUER,
ALTHOFF. 1982. Inn. Med. 9 151-158.
58. RAHIER,J., S. LOOZEN,R. M. GOEBBELS& M. ABRAHEM.1987. Diabetologia 30: 512.
MOLLER,W. A., M. BERGER,H. J. COPPERS,P. BERCHTOLD,
G. STROHMEYER,
A. E.
RENOLD,J. R. HOFSTETTER& J. H. GONVERS.1979. Gut 20: 200-204.
60. PASSA,P., F. ROUSSELIE,C. GAUVILLE& J. CANIVET.1977. Diabetes 26: 113-120.
61. NIEDERAU,C., M.BERGER,W. STREMMEL,
A. STARKE,
G. STROHMEYER,
R. EBERT,
E. SIEGEL
& W. CREUTZFELDT.1984. Diabetologia 26: 441-444.
59.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Keeping Birth Normal: Position StatementDocument3 pagesKeeping Birth Normal: Position StatementCatur ErtyPas encore d'évaluation
- List of Students Eligibile For Gold Medal AwardDocument8 pagesList of Students Eligibile For Gold Medal AwardVpsm SinghPas encore d'évaluation
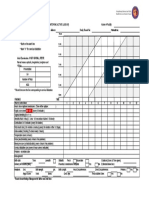
- Partograph: (Use This Form For Monitoring Active Labour)Document1 pagePartograph: (Use This Form For Monitoring Active Labour)Omar Khalif Amad PendatunPas encore d'évaluation
- INTRAPARTUMDocument18 pagesINTRAPARTUMMICHELLE FACTOPas encore d'évaluation
- My Resume...Document5 pagesMy Resume...Kat TangonanPas encore d'évaluation
- Medical ChaperoneDocument8 pagesMedical ChaperoneMd Anwar ShahadatPas encore d'évaluation
- 4 Steps: Instrument PassingDocument3 pages4 Steps: Instrument PassingGwyn Leen CagasPas encore d'évaluation
- Jurnal Tetes MataDocument6 pagesJurnal Tetes MataSyafiraPas encore d'évaluation
- O&G LO SlidesDocument60 pagesO&G LO Slideskatherine nunnPas encore d'évaluation
- Hioerplasia Mamaria GestacionalDocument9 pagesHioerplasia Mamaria GestacionalOctavio LeyvaPas encore d'évaluation
- Innovative, Micro Catheters - Unknown - Setting A New StandardDocument8 pagesInnovative, Micro Catheters - Unknown - Setting A New StandardMetehan AgacaPas encore d'évaluation
- Procedures in Obstetrics and Gynaecology TextbookDocument272 pagesProcedures in Obstetrics and Gynaecology TextbookPriyaPas encore d'évaluation
- 501k StrykerDocument12 pages501k StrykerFrancisco100% (1)
- Chemistry - I: TEST(s) Normal UNIT(s)Document1 pageChemistry - I: TEST(s) Normal UNIT(s)Muhammad SuhaibPas encore d'évaluation
- Prepping and Draping The PatientDocument26 pagesPrepping and Draping The Patientjosphinenthenya001Pas encore d'évaluation
- Handouts For Normal PediatricsDocument54 pagesHandouts For Normal Pediatricsapi-3842758Pas encore d'évaluation
- PREMATURIIDocument91 pagesPREMATURIIAdriana MelnicPas encore d'évaluation
- Meet Khyati RupaniDocument9 pagesMeet Khyati RupaniKhyati RupaniPas encore d'évaluation
- Female Welfare ProgrammeDocument6 pagesFemale Welfare ProgrammeAnnapurna DangetiPas encore d'évaluation
- CholecystitisDocument12 pagesCholecystitisMariela HuertaPas encore d'évaluation
- Eu Directive Annex 5 - List of Qualifications PDFDocument10 pagesEu Directive Annex 5 - List of Qualifications PDFIbrahim ZainabPas encore d'évaluation
- Women Factory Employees Facilities As Per Factory ActDocument25 pagesWomen Factory Employees Facilities As Per Factory ActNaveen Kumar SharmaPas encore d'évaluation
- ABORTIONDocument23 pagesABORTIONCristyl Shine BariaoPas encore d'évaluation
- Pain Assessment in PediatricDocument4 pagesPain Assessment in PediatricfitriaPas encore d'évaluation
- Intestin Gros Si AnorectalDocument282 pagesIntestin Gros Si AnorectalPatricia IoanaPas encore d'évaluation
- Mindray M7 Portable Ultrasound Review and Video: Brian Gill's Ultrasound Machine Reviews, News, and AdviceDocument10 pagesMindray M7 Portable Ultrasound Review and Video: Brian Gill's Ultrasound Machine Reviews, News, and AdvicerovoPas encore d'évaluation
- Asha Monthly Reports - Aprial MonthDocument64 pagesAsha Monthly Reports - Aprial MonthSamuel SourabPas encore d'évaluation
- Women - S Health USA 2016-03Document170 pagesWomen - S Health USA 2016-03joan100% (1)
- Literature Review Ectopic PregnancyDocument4 pagesLiterature Review Ectopic Pregnancyakjnbowgf100% (1)
- E HEALTH SeminarDocument17 pagesE HEALTH SeminarDev jibreenPas encore d'évaluation