Académique Documents
Professionnel Documents
Culture Documents
Cardio Anapyhy Session1
Transféré par
Louise Anne Agnazata GayoCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Cardio Anapyhy Session1
Transféré par
Louise Anne Agnazata GayoDroits d'auteur :
Formats disponibles
9/18/2014
Cardiovascular System
Anatomy & Physiology
Beryl Ben C. Mergal, RN, MSN
DEVOTIONAL
Quiz #1
Label the Different Parts of the Heart.
Integration of Faith and
Learning
Proverbs 4:23
Keep thy heart with all
diligence; for out of it
are the issues of life..
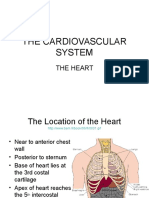
Anatomy of the Heart
Location and Structure
Hollow, Muscular
Organ
Delivers oxygenated
blood to body through
arteries
When blood returns
through veins, pumps
it to lungs to be
reoxygenated
Lies obliquely in chest,
behind sternum in
mediastinum.
Located between the
lungs in front of spine.
Varies in size
depending on the
persons body size.
Estimated around 5 in
long and 3.5 in wide.
9/18/2014
Location and Structure
Location and Structure
MEDIASTINUM
-the central section
of the thorax
(chest cavity)
2/3 lies left of
MSL
Changes in the Heart
In older adult, becomes slightly smaller
and loses contractile strength and
efficiency.
By 70, cardiac output at rest has
diminished by about 30% to 35% in
many people.
Q: What is Oxygenation?
transport of O to all body
parts & the removal of CO.
Q: 4 Components of this Process:
1. Hgb O2 carrier
2. Blood vessels transporting network
3. Heart the pump
4. Lungs oxygenate blood
The flat, broader part.
The blunt rounded point of
the cone
Major Function of the
Cardiovascular System
Circulation of blood
_________
Delivery of O, nutrients,
_______
hormones & enzymes to
the body
Removal of CO and
________
other products of metabolism
Physiology of Oxygenation
1. Ventilation
2. Alveolar Gas
Exchange (oxygen
uptake or external
respiration)
3. 02 Transport &
Delivery
4. Cellular Respiration
3.
9/18/2014
1. Ventilation
Regulators of Ventilation
1. respiratory control centers in
the pons & medulla oblongata.
2. changes in the concentration of
pH & CO2 in the bodys fluid
The 1st step in the process of oxygenation.
The movement of air into and out of the lungs
for the purpose of delivering fresh air into the lungs
alveoli.
2. Alveolar Gas Exchange
3. Decrease in blood O2
concentration (hypoxemia)
2. Alveolar Gas Exchange
Once fresh air reaches the lungs alveoli, the 2nd step in
the process of oxygenation begins.
OXYGEN UPTAKE (external respiration) the exchange
of O2 from the alveolar space into the pulmonary capillary
blood.
3. O2 Transport & Delivery
3 FACTORS INFLUENCE THE CAPACITY OF
BLOOD TO CARRY O2:
1. The amount of O2 dissolved in
plasma
2. The amount hemoglobin
3. The tendency of hemoglobin to
bind with O2
4. Cellular respiration
Gas exchange at the cellular level
(also called internal respiration)
takes place via diffusion in response to
concentration gradient.
O2 diffuses fr the blood to the tissues,
while CO2 moves fr the tissues to the
blood
Then blood is reoxygenated by the lungs
9/18/2014
4. Cellular respiration
Heart Wall
Three Layers
1. Epicardium outermost layer and made up of
squamous epithelial cells
Gaseous Exchange
Heart Wall
Three Layers
2. Myocardium middle and thickest layer.
Made up of Myocardial cells.
Nodal cells - for pacemaker functions.
Purkinje cells-found in bundle of His, Left Bundle
Branch(LBB) & Right Bundle Branch(RBB).
Heart Wall
Heart Wall
Three Layers
3. Endocardium innermost layer, consisting of thin layer
of endothelial tissue that lines heart valves and
chambers.
Pericardium
Fluid-filled sac that envelops heart and acts as tough,
protective coating.
Consists of fibrous pericardium (tough, white, fibrous
tissue) and serous pericardium (two layers
<parietal,visceral>)
9/18/2014
Heart Wall
Heart Wall
Pericardium
Pericardial space separates the visceral and parietal layers
and contains 10-20ml of thin, clear, lubricating
pericardial fluid.
The 4 Heart Chambers
Functions of the Pericardial Fluid
Protects & cushions the heart & great vessels.
Provides barrier to infectious processes in
adjacent structures.
The Heart Chambers
RA receives deoxygenated blood returning
from body.
LA receives oxygenated blood from lungs.
RV receives deoxygenated blood from RA,
pumping it to the lungs for reoxygenation.
LV receives oxygenated blood from LA,
pumping it into the systemic circulation.
ATRIA are reservoirs for ventricles (thinner
walls than ventricles).
Which chamber is the thickest & why?
RA 2mm
LA 3mm
Q: What separates the
heart chambers?
Septum (a muscular wall)
RV 3-5mm
LV 13-15mm
1. INTERATRIAL septum
separates the atria
2. INTERVENTRICULAR septum
separates the ventricles
9/18/2014
The Heart Valves
Chordae Tendinae
Atrio-ventricular
valves:AV valves
1. Tricuspid
2. Mitral or bicuspid
Small tendinous cords
anchored to the
papillary muscles that
holds the cusps or
leaflets of the valves.
Prevents the cusps
from bulging
backward into atria
during ventricular
contraction.
Semi-lunar valves:
1. Pulmonary
2. Aortic valves
The Heart Valves
The Heart Valves
AV Valves
Tricuspid valve separates RA fr RV; mitral
valve separates LA fr LV.
Closure of AV valves associated with S1
sound.
The Heart Valves
Ventricular Diastole
Semilunar Valves
Pulmonic valve, located where pulmonary
artery meets right ventricle.
Aortic valve, located where left ventricle
meets aorta.
Closure of semilunar valves associated with
S2 sound.
ATRIOVENTRICULAR VALVES OPEN
9/18/2014
Ventricular Systole
Q: What causes the valves to
open and close?
Increased pressure within the ventricles
during ventricular systole causes the
pulmonic and aortic valves to open,
allowing ejection of blood into the
pulmonary and systemic circulation.
Loss of pressure as the ventricular
chambers empty causes the valves to
close.
SEMILUNAR VALVES OPEN
Atrial and Ventricular
Pressure
Blood Flow to the Heart
Pulmonary Circulation
Mitral
Valve
Systemic
Circulation
Circulation through the Heart
Circulation through the Heart
9/18/2014
Coronary Blood Supply
Main coronary arteries
lie on surface of heart.
Heart receives its
blood supply almost
entirely through
coronary arteries.
Coronary Blood Supply
Coronary Blood Supply
Right Coronary Artery
Supplies blood to right
atrium, right ventricle,
and inferior wall of left
ventricle.
Posterior descending
artery supplies posterior
wall of left ventricle.
Coronary Blood Supply
Left Coronary Artery
Left Coronary Artery
Splits into two major
branches: left anterior
descending, left circumflex.
Left anterior descending
supplies blood to anterior
wall of left ventricle,
anterior interventricular
septum, bundle of His,
right bundle branch, and
anterior fasciculus of left
bundle branch.
Left circumflex provides
blood to lateral wall of left
ventricle and left atrium.
Coronary Blood Supply
Coronary Circulation
Heart receives its
blood supply during
ventricular relaxation
or diastole.
9/18/2014
Coronary Blood Supply to the
Heart
Cardiac Veins
About 75% of total
coronary venous blood
flow leaves left
ventricle by way of
coronary sinus.
The Circulation of Blood
TERMINAL
ARTERIOLE
The artery, capillary and vein and
its layers.
POSTCAPILLARY
VENULE
CAPILLARY
BED
CAPILLARY
TUNICA EXTERNA
TUNICA MEDIA
VALVE
TUNICA INTIMA
LUMEN
TISSUE CELLS
PRECAPILLARY
SPHINCTER
TRUE
CAPILLARIES
VASCULAR
SHUNT
Arteries
DIAMETER
LOCATION
ELASTIC
>1 cm
aorta
w/ extensive ELASTIC
Pulmonary
FIBERS at tunica media
common
Serve as pressure
carotid
reservoir
subclavian
Propels blood onward
common iliac
even if the LV is relaxed
0.1 10 mm
VEIN
Arterioles
TYPES
MUSCULAR
ARTERY
DESCRIPTION
Brachial (in
w/ more SMOOTH
the arm)
MUSCLE at tunica media
Radial (in the Capable of greater
forearm
vasoconstriction &
vasodilation.
Diameter: 10-100 micrometer
w/ high proportion of vascular
smooth muscles.
offer the greatest resistance to
blood flow.
a change in diameter affects
blood pressure.
9/18/2014
Arterioles
Capillaries
The ff can cause
vasoconstriction or vascular
smooth muscle contraction:
1. Epinephrine
2. Norepinephrine
3. Angiotensin II
Microscopic vessels (microcirculation)
Diameter: 4-10 micrometer
Consist of tunica intima or
endothelium
Function: allows exchange of
materials between blood & tissues.
Exchange vessels
Capillaries
Venules
High BP results to the ff:
1. rupture fragile capillaries
2. force solute-containing
fluids out into the interstitial
space.
Angiogeneis
angio = blood vessel
genesis = production
Growth of new blood vessels
- during wound healing
- during endurance exercise
training
Diameter: 10-100 micrometer
Function:
collect blood from capillaries &
deliver it to veins
w/ phagocytic WBCs
Veins
Diameter: 0.1 mm - >1mm
characterized by high volume &
low pressure
Function: volume storage
contain 70% of the circulating
blood volume
w/ valves
10
9/18/2014
Cardiac Physiology
Autonomic
Innervation of the
Heart
Sympathetic nerve
stimulation causes
release of
norepinephrine, which
increases heart rate
and accelerates AV
node conduction.
Autonomic
Innervation of the
Heart
Role of Baroreceptors and
Chemoreceptors in Response to Blood
Loss
Parasympathetic
Nerve stimulation
causes release of
acetylcholine, which
slows heart rate and
conduction through
the AV node.
Control of Blood
Pressure by
Baroreceptors
Baroreceptors are
stretch receptors in
the wall of some blood
vessels. They are
involved in the
control of arterial
pressure through the
discharge of impulses
to the cardiovascular
centre when there is
distension due to a
change in the blood
pressure.
Control of Blood
Pressure by
Chemoreceptors
They are sensitive to
any change in the
chemical composition
of the blood, such as a
decrease in oxygen
level and pH of the
blood or an increase
in the carbon
dioxide level.
11
9/18/2014
Effects of Blood Pressure to the
Heart
Chemoreceptor Stimulation
and the Hearts Response
Decreased Blood O2
Increased CO2
Decreased blood Ph
Decreased
Parasympathetic
Stimulation
Increased
Sympathetic
Stimulation
Increased
Heart Rate
Increased SV
Increased BP
Transmission of Electrical
Impulses
Transmission of Electrical
Impulses
In order for the heart to contract and pump
blood to the rest of the body, an electrical
stimulus needs to occur first.
Generation and transmission of electrical
impulses depend on the four key
characteristics of cardiac cells:
automaticity, excitability, conductivity
and contractility.
Four Key Cell Characteristics
1. Automaticity cells ability to
spontaneously initiate an electrical
impulse.
2. Excitability cells ability to respond to
an electrical impulse.
3. Conductivity cells ability to transmit
an electrical impulse from cell to another.
4. Contractility cells ability to contract.
Cardiac Conduction System
Impulses travel from
SA node (hearts
pacemaker) through
internodal tracts and
Bachmans bundle to
AV node.
From AV node,
impulses travel through
bundle of His, bundle
branches, and to
Purkinje fibers.
Cardiac Conduction System
1. Sinoatrial Node
(SA Node)
Located in the RA where
the superior vena cava joins
the atrial tissue mass.
Pacemaker of the heart.
Generates impulses about
60-100 b/min (resting
conditions).
Impulses travel on specific
path but dont travel in
backward or retrograde
direction.
12
9/18/2014
Cardiac Conduction System
2. Atrioventricular Node
(AV
Node)
Located in the inferior right
atrium near ostium of the
coronary sinus.
Does not possess
pacemaker cells but the
surrounding tissue does.
AV node conducts impulses
to the ventricles.
Firing rate of 40-60 b/min.
Cardiac Conduction System
Cardiac Conduction System
3. Bundle of His
Divided into 2 branches ;
RBB & LBB
RBB extends down the right
side of the interventricular
septum and through the
right ventricle.
LBB extends down the left
side of the interventricular
septum and through the left
ventricle.
Firing rate 30-40 b/min
Cardiac Conduction System
4. Purkinje Fibers
Composed of a diffuse
muscle fiber network
beneath the endocardium
that transmits impulses
quicker than any other part
of the conduction system.
Usually doesnt fire unless
SA and AV nodes fail to
generate or when impulse is
blocked in both BB.
Firing rate 20-40 b/min
Cardiac Conduction Times
SA
(60-100/min)
AV
(40-60/min)
BUNDLE OF HIS
(30-40/min)
PURKINJE FIBERS
(20-30/min)
13
9/18/2014
Abnormal Impulse Conduction
Causes include:
Altered Automaticity
Retrograde Conduction of Impulses
Reentry Abnormalities and Ectopy
Major Electrolytes That Affect
Cardiac Function
1. K
2. Na
3. Ca
Depolarization & Repolarization
(Action Potential)
Depolarization and repolarization are
electrical activities which cause muscular
activity.
Depolarization- generation of an electrical
impulse by an electrical cell which then causes
the ions to cross the cell membrane and
causes the action potential.
Repolarization - is the return of the ions to
their previous resting state, which corresponds
with relaxation of the myocardial muscle.
2 Types Of Ion Channels:
1. Na-K pump
the fast sodium channels
2. Na-Ca pump
Slow Ca channels
Sodium-Potassium Pump
Sodium-Potassium Pump
moves Na ions back out of the
cell in exchange for an inward
movement of K ions & viceversa.
Both ions are moving against
a concentration gradient
the ratio is 3 Na : 2 K
powered by ATP
Digoxin blocks Na-K pump
Epinephrine & insulin
stimulate it, causing uptake
of K to cells.
14
9/18/2014
Sodium-Potassium Pump
The Na-K Pump
give glucose and insulin to
hyperkalemic patients
Epinephrine and insulin is
associated with hypokalemia
Sodium-Calcium Pump
POLARIZATION
resting potential
Calcium ions move into the cell to
activate contraction.
Moves Ca back into the ECF
The energy stored in the Na
gradient powers the movement of Ca.
DEPOLARIZATION
(action potential)
REPOLARIZATION
(the recovery phase)
15
9/18/2014
The Pacemaker Potential
The Cardiac Muscle Potential
Depolarization-Repolarization
Depolarization-Repolarization
Action Potential of a Cardiac Muscle
Action Potential of a Cardiac Muscle
Phase 0: Rapid Depolarization
Na moves rapidly into cell.
Ca moves slowly into cell.
Cell receives stimulus from a
neighboring cell.
Myocardical contraction occurs
Phase 1: Early Repolarization
Na channels close
Na stops flowing into the cell.
Cell is in absolute refractory
period (no stimulus, no matter
how strong, can excite the
cell).
Depolarization-Repolarization
Depolarization-Repolarization
Phase 2: Plateau Phase
Ca channels open
K channels close
Calcium continues to flow in.
Potassium continues to flow
out.
Cell is in absolute refractory
period (no stimulus, no matter
how strong, can excite the
cell).
Phase 3: Rapid Repolarization
Occurs as the cell returns to its
original state.
Ca channels close.
K flows out rapidly.
Active transport via the Na-K
pump begins restoring K to the
inside of the cell and Na to the
outside of the cell.
Cell is in relative refractory
period; however, strong
stimulus can depolarize it.
Action Potential of a Cardiac Muscle
Action Potential of a Cardiac Muscle
16
9/18/2014
Depolarization-Repolarization
Action Potential of a Cardiac Muscle
Basic Electrocardiogram
(ECG)
Phase 4: Resting Phase
Cell membrane is impermeable
to Na.
K moves out of the cell.
Cell is ready for another
stimulus.
The ECG machine is designed to recognise and
record any electrical activity within the heart.
A standard ECG is printed at 25mm per second or
25 small squares per second.
Basic Electrocardiogram
(ECG)
Basic Electrocardiogram
(ECG)
Normal Sinus Rhythm
The P Wave
Normal Sinus rhythm occurs when an impulse starts in
the sinus node and progresses to the ventricles through a
normal conduction pathway from Sinus Node, Atria, AV
node, bindle of His, to the bundle branches, and on to the
Purkinje fibers.
P wave - represents atrial depolarisation.
Location: precedes the QRS complex
Amplitude: 2-3 mm high
Duration: 0.06-0.12 sec
Basic Electrocardiogram
Basic Electrocardiogram
(ECG)
The PR Interval
PR Interval Tracks atrial impulse from atria to AV node,
bundle of His, and RBB and LBB.
Location: from beginning of P wave to the beginning of the
QRS complex.
Duration: 0.12-0.60 sec
(ECG)
The Q Wave
Q wave and represents depolarisation in the septum.
Whilst the electrical stimulus passes through the bundle
of His, and before it separates down the two bundle
branches, it starts to depolarise the septum from left to
right.
17
9/18/2014
Basic Electrocardiogram
(ECG)
The R Wave
(ECG)
The S Wave
R wave represents the electrical stimulus as it passes
through the main portion of the ventricular walls
(Ventricular Depolarization).
Basic Electrocardiogram
Basic Electrocardiogram
(ECG)
The QRS Complex
S wave and represents depolarisation in the Purkinje
fibres.
The S wave travels in the opposite direction to the large R
wave because, the Purkinje fibres spread throughout the
ventricles from top to bottom and then back up through
the walls of the ventricles.
Basic Electrocardiogram
(ECG)
The ST Segment
QRS Complex represents depolarization of
ventricles.
Location: follows PR interval
Amplitude: 5-30 mm high (differs for each lead used)
Duration: 0.06-0.10 sec
The ST segment represents end of ventricular
depolarization and onset of ventricular
repolarization.
Location: extends from the S wave to the beginning of the
T wave.
Duration: 0.08 sec
Basic Electrocardiogram
Basic Electrocardiogram
(ECG)
The T Wave
T wave represents relative refractory period of
repolarization or ventricular recovery.
Location: follows ST segment
Amplitude: 0.5 mm in leads I, II, and III and up to 10 mm
in precordial leads
Duration: 0.06-0.12 sec
(ECG)
The QT Interval
QT Interval measures timed needed for ventricular
depolarizaton and repolarization.
Location: extends from beginning of QRS complex to the
end of the T wave.
Duration: varies; usually lasts 0.36-0.44 sec
18
9/18/2014
Basic Electrocardiogram
ECG Waveform
COmponents
(ECG)
The U wave
U wave represents repolarization of His-purkinje
system.
The U wave may not appear on an ECG. A prominent U
wave may be due to hypercalcemia, hypokalemia, or
digoxin toxicity.
Cardiac Contraction
The Physiology of the
CARDIAC CYCLE
Basic Phases of the Cardiac
Cycle
Relaxation
Atria Ventricles
AV Node delays impulses
travelling from Atria to
Ventricles.
Ventricular Systole
Contraction
Contraction
Filling
Ejection
SYSTOLE
Muscle contraction is
initiated by action potentials
that normally originate from
a pacemaker site (SA Node)
in the right atrium.
Action Potentials depolarize
cells, causing contraction.
Sequence of contraction
DIASTOLE
Systole
Begins with ventricular contraction.
Ends when ejection ceases.
Diastole
Begins when ejection ceases as ventricles relax
Ventricular filling begins after sufficient relaxation occurs.
Filled volume is the End
Diastolic Volume
Initiated by ventricular
depolarization (QRS of ECG
LVP increases
AV Valve Closes
LV contraction is initially
isovolumetric
Ejection
Outflow valves open
Repolarization (T wave of
ECG) initiates relaxation
causing ejection rate to
rapidly decline.
Residual volume after ejection
is End Systolic Volume
19
9/18/2014
Atrial Systole
Ventricular Diastole
(Contraction & Ejection)
Relaxation
Initiated by repolarization (T
wave of ECG)
LVP decreases
Outflow valves close (begins
diastole)
Initially Isovolumetric
Ejection
AV valves open when LV
pressure < atrial pressure.
Most ventricular filling occurs
before atrial contraction.
Maximal filled volume is enddiastolic volume.
Initiated by
depolarization (P wave
of ECG)
Occurs near end of
diastole
Atrial pressure
transiently increases (a
wave), forcing
additional blood into the
ventricles.
Accounts for 10% of
ventricular filling at
resting (up to 40%
during exercise)
Cardiac Cycle and its
Relationship to the ECG
Atrial Diastole
(Relaxation & Filling)
Blood continously
enters the atria, except
when transiently
impeded during atrial
systole.
Occurs throughout
ventricular systole and
diastole (until P wave of
ECG).
AV valves suddenly
open when LV pressure
< atrial pressure
(creating the v wave).
Average, Normal Intracardiac
and Vascular Pressures (mmHg)
20
9/18/2014
Stroke Volume
Ventricular Stroke volume is the difference
between ventricular end-diastolic volume
(EDV) and end-systolic volume (ESV).
SV = EDV - ESV
In a normal heart, EDV-ESV is the same
volume of blood as ejected into the aorta
during each systole.
Stroke Volume
3 Factors Determine Stroke Volume
1. PRELOAD the vol of
blood in the ventricles at
the end of diastole,
before the next
contraction. (Lewis, et al 2008)
proportional to the
end-diastolic volume
(EDV).
Q: Factors AFFECTING
Preload
b. Ventricular compliance
the elasticity when blood enters
ventricle.
Conditions that elasticity:
When muscle thickens =Hypertrophy
increased fibrotic tissue within the
ventricle = after MI
cardiac tamponade
Stroke Volume
3 Factors Determine Stroke Volume
1. PRELOAD
the distending force
that stretches the
ventricular muscle during
ventricular relaxation
(Woods, 2010).
Can be compared to
the stretching of a rubber
band.
Q: Factors AFFECTING
Preload
a. Venous return
the vol of blood that enters
the ventricle during diastole.
Conditions venous return:
Fluid overload
Frank Starlings Law of
the Heart
The > the volume,
the > the stretch of the
cardiac muscle,
the > the force of
contraction to accomplish
emptying.
21
9/18/2014
Frank Starlings Law of the
Heart
Has physiologic limit
Overstretching of the
cardiac muscle fibers
eventually results in
ineffective contraction.
Conditions that Decreases
Preload
Hemorrhage
Fluid shifting to 3rd space
vasodilation
Conditions that Increases
Preload
Stroke Volume
CHF
Renal disease
Vasoconstriction
Hypervolemia
Regurgitation of cardiac valves
2. CONTRACTILITY
Q: Why do you think blockage of coronary
arteries affect the hearts contractility?
Q: What are the substances
that increases contractility?
3 Factors Determine Stroke Volume
the forcefulness of
contraction of ventricular
muscle fibers.
Q: WHAT will happen if
contractility is poor?
Poor contractility =
reduction of CO
positive inotropic agents.
1. Dopamine
2. Dobutamine
3. Dopexamine
4. Epinephrine (adrenaline)
5. Isoprenaline (isoproterenol)
6. Norepinephrine
7. Digoxin
8. Digitalis
9. Insulin
22
9/18/2014
Q: What are the substances
that decreases contractility?
negative inotropic agents.
1. Beta blockers
2. Calcium channel blockers
a) Diltiazem
b) Verapamil
c) Clevidipine
3. Class IA antiarrhythmics such as
a) Quinidine
b) Procainamide
c) disopyramide
4. Class IC antiarrhythmics such as
a) Flecainide
Stroke Volume
3 Factors Determine Stroke Volume
Stroke Volume
3 Factors Determine Stroke Volume
3. AFTERLOAD
the force that the
ventricles must generate
to eject blood.
Amount of pressure left
ventricle must work
against to eject blood
during systole.
Determinants of LV AFTERLOAD
Resistance
3. AFTERLOAD
Factors Affecting Afterload
1. Diameter of the aorta &
pulmonary artery.
Systemic Vascular
Resistance (SVR)
2. Opening and competence of
the pulmonary & aortic valves.
HPN
Aortic Valve
Stenosis
The FORCE
Determinants of RV AFTERLOAD
Resistance
The FORCE
Pulmonary vascular
resistance (PVR
CONGESTED
LUNGS
Pulmonic Valve
Stenosis
Ejection Fraction
Ejection Fraction (EF) is the fraction of
blood ejected by the ventricle relative to its
filled volume (end-diastolic volume).
EF is a measure of the ability of the heart
to eject blood.
EF is normally about 0.55-0.65 (55%-65%)
PULMONARY
EMBOLISM
23
9/18/2014
Cardiac Output
Cardiac Output is the amount of blood the
left ventricle pumps into the aorta per
minute.
=
Normal cardiac output is 4-8L per
minute, depending on body size.
Sample Computation
(Compute the SV, EF & CO)
HR = 70/min
End diastolic volume
End systolic volume
= 120 ml
= 50 ml
Ejection volume (stroke volume) =
Ejection fraction = 70ml/120ml =
70 ml
58%
(normally 60%)
If heart rate (HR) is 70 beats/minute, what
is cardiac output?
Cardiac output
= HR x SV
= 70/min * 70 ml
= 4900ml/min
24
Vous aimerez peut-être aussi
- Human Anatomy and Physiology MCQ With Answers PDFDocument4 pagesHuman Anatomy and Physiology MCQ With Answers PDFPrince Maurya88% (8)
- A DETAILED LESSON PLAN IN SCIENCE IV ArjayDocument6 pagesA DETAILED LESSON PLAN IN SCIENCE IV ArjayArlea TrinidadPas encore d'évaluation
- The Heart: Anatomy, Chambers, Circulation & ValvesDocument14 pagesThe Heart: Anatomy, Chambers, Circulation & ValvesGary Bowen100% (1)
- NAGA COLLEGE FOUNDATION ANATOMY & PHYSIOLOGY LABORATORYDocument4 pagesNAGA COLLEGE FOUNDATION ANATOMY & PHYSIOLOGY LABORATORYPado100% (1)
- Lecture 6 Cardiovascular: Vascular System - The HemodynamicsDocument70 pagesLecture 6 Cardiovascular: Vascular System - The HemodynamicsAndreea ŞtefănescuPas encore d'évaluation
- ANPH-M2-CU8. The HeartDocument20 pagesANPH-M2-CU8. The HeartMary Grace MapulaPas encore d'évaluation
- The Cardiac Cycle: Chapter 19Document62 pagesThe Cardiac Cycle: Chapter 19BishwambherPas encore d'évaluation
- Chapter 15 - Cardiovascular SystemDocument89 pagesChapter 15 - Cardiovascular SystemOliver Namyalo100% (1)
- Blood CirculationDocument1 pageBlood Circulationjuliana sachicaPas encore d'évaluation
- Chapter 11-The Normal ElectrocardiogramDocument18 pagesChapter 11-The Normal Electrocardiogrammuna s100% (1)
- Circulatory System - Part 2 4-8-14 For BBDocument23 pagesCirculatory System - Part 2 4-8-14 For BBroman7dbPas encore d'évaluation
- Anatomy and Physiology II Course OutcomesDocument50 pagesAnatomy and Physiology II Course OutcomesShirley LourdesPas encore d'évaluation
- A&P 302 - Respiratory NotesDocument31 pagesA&P 302 - Respiratory NotesBethanyPas encore d'évaluation
- P6 English Term II 2020 WorkDocument144 pagesP6 English Term II 2020 WorkAlex SsembalirwaPas encore d'évaluation
- Heart, Circulation, and Blood Unit Test: Biology 11 April 3, 2014Document8 pagesHeart, Circulation, and Blood Unit Test: Biology 11 April 3, 2014api-279500653Pas encore d'évaluation
- 1st Lec On Heart Physiology by Dr. RoomiDocument21 pages1st Lec On Heart Physiology by Dr. RoomiMudassar RoomiPas encore d'évaluation
- CV SYSTEM ANATOMYDocument42 pagesCV SYSTEM ANATOMYJerilee SoCute WattsPas encore d'évaluation
- Anatomy of Cardiovascular SystemDocument23 pagesAnatomy of Cardiovascular SystemElvira Wisakhadewi100% (1)
- Hemodynamics: DR Axelle Saverettiar Mbbs Physiology Department SSR Medical CollegeDocument31 pagesHemodynamics: DR Axelle Saverettiar Mbbs Physiology Department SSR Medical CollegeÑäd ÉèmPas encore d'évaluation
- Anatomy Heart and Great VesselsDocument54 pagesAnatomy Heart and Great VesselsRaviPas encore d'évaluation
- Introduction To Cell PhysiologyDocument149 pagesIntroduction To Cell PhysiologyAlysaPas encore d'évaluation
- Anatomy of Larynx Lecture 7Document21 pagesAnatomy of Larynx Lecture 7sallykamareddine100% (1)
- AP Chapter 16BDocument35 pagesAP Chapter 16BJay Patel100% (1)
- Coronary Circulation: Dr. Syma RizwanDocument34 pagesCoronary Circulation: Dr. Syma RizwanAttiqaQureshiPas encore d'évaluation
- AsdaDocument42 pagesAsdaratchagarajaPas encore d'évaluation
- Physiology of The Cardiovascular System-CVSDocument56 pagesPhysiology of The Cardiovascular System-CVSAmanuel MaruPas encore d'évaluation
- Cardiovascular Blood VesselsDocument12 pagesCardiovascular Blood VesselswatuwaitingforPas encore d'évaluation
- Introduction To The CvsDocument43 pagesIntroduction To The CvsParmesh PandeyPas encore d'évaluation
- Important SEQs Heart Physiology by Dr. RoomiDocument3 pagesImportant SEQs Heart Physiology by Dr. RoomiMudassar Roomi100% (2)
- Kidney Anatomy and Histology ExplainedDocument7 pagesKidney Anatomy and Histology ExplainedLaura TorpeyPas encore d'évaluation
- Bped 65 Urinary SystemDocument26 pagesBped 65 Urinary SystemDollie May Maestre-TejidorPas encore d'évaluation
- Embryo Exam 2: Respiratory System: Download The Android App!Document4 pagesEmbryo Exam 2: Respiratory System: Download The Android App!AzizPas encore d'évaluation
- Thoracic CageDocument30 pagesThoracic CageLizz MariePas encore d'évaluation
- (PHY) 3.03 Mechanical Properties of The Heart - Dr. JerezDocument12 pages(PHY) 3.03 Mechanical Properties of The Heart - Dr. JerezKate Lynne CamonayanPas encore d'évaluation
- Functional Human Physiology: For The Exercise and Sport Sciences The Cardiovascular System: Cardiac FunctionDocument186 pagesFunctional Human Physiology: For The Exercise and Sport Sciences The Cardiovascular System: Cardiac FunctionBery Agana F. PurbaPas encore d'évaluation
- Embryology Session 6 Development of The Kidneys and Urinary TractDocument6 pagesEmbryology Session 6 Development of The Kidneys and Urinary TractMuhammadBasimPas encore d'évaluation
- Composition and Function of Blood ComponentsDocument17 pagesComposition and Function of Blood ComponentsPrakash Kumar Nayak100% (1)
- Rhythmical Excitation of The HeartDocument6 pagesRhythmical Excitation of The HeartTONY GO AWAYPas encore d'évaluation
- CVS Lect 6 Blood Pressure, PathophysiologyDocument13 pagesCVS Lect 6 Blood Pressure, PathophysiologySherwan R Shal100% (5)
- Cardiovascular Physiology: Cardiac Output, Blood Flow ControlsDocument33 pagesCardiovascular Physiology: Cardiac Output, Blood Flow ControlsLuiz Jorge MendonçaPas encore d'évaluation
- Transport of Respiratory GasesDocument47 pagesTransport of Respiratory Gasessib786123Pas encore d'évaluation
- SPIROMETRYDocument5 pagesSPIROMETRYJayarubini JeyapalPas encore d'évaluation
- Circulatory SystemDocument304 pagesCirculatory Systemyapyihao2100% (1)
- Cardiac CycleDocument31 pagesCardiac CycleAdwaitha KrPas encore d'évaluation
- Dr. Aaijaz Ahmed Khan Sr. Lecturer in Anatomy PPSP, UsmDocument38 pagesDr. Aaijaz Ahmed Khan Sr. Lecturer in Anatomy PPSP, UsmeliseudesafatePas encore d'évaluation
- CardiovascularDocument92 pagesCardiovascularRolinette DanePas encore d'évaluation
- Regulation of Heart Rate, Stroke Volume, Cardiac Output, Blood FlowDocument20 pagesRegulation of Heart Rate, Stroke Volume, Cardiac Output, Blood FlowShveta MahajanPas encore d'évaluation
- 3 MAJOR OPENINGS /right Atirum: Cardiovascular System Serious PericardiumDocument3 pages3 MAJOR OPENINGS /right Atirum: Cardiovascular System Serious PericardiumAebee Alcaraz100% (1)
- IMD - Step-Up To USMLE Step 3 - Chapter 1 - CardiologyDocument124 pagesIMD - Step-Up To USMLE Step 3 - Chapter 1 - CardiologyAly SherifPas encore d'évaluation
- 1st Lec On Heart Physiology by Dr. RoomiDocument13 pages1st Lec On Heart Physiology by Dr. RoomiMudassar Roomi100% (1)
- Cardiac Cycle: Prepared By: Mineshkumar Prajapati Roll No: 05 Biomedical Science (2021-22)Document21 pagesCardiac Cycle: Prepared By: Mineshkumar Prajapati Roll No: 05 Biomedical Science (2021-22)minesh prajapatiPas encore d'évaluation
- Cardiac Output: Dr. AthulyaDocument29 pagesCardiac Output: Dr. AthulyaamrendraPas encore d'évaluation
- Structure and Functions of The Major Types of Blood VesselsDocument6 pagesStructure and Functions of The Major Types of Blood VesselsCharls DeimoyPas encore d'évaluation
- Anatomy Lecture Notes Unit 7 Circulatory System - The Blood VesselsDocument10 pagesAnatomy Lecture Notes Unit 7 Circulatory System - The Blood VesselsIssac LauPas encore d'évaluation
- Bundle Branch BlockDocument37 pagesBundle Branch BlocksyukronchalimPas encore d'évaluation
- Cardiac Cycle: Mechanical Event and Their Electrical and Clinical CorrelationDocument28 pagesCardiac Cycle: Mechanical Event and Their Electrical and Clinical Correlationhawas muhammed100% (1)
- A&P - 1. Heart Anatomy (9p)Document9 pagesA&P - 1. Heart Anatomy (9p)mr. fakePas encore d'évaluation
- Gross Anatomy of Posterior Thigh CompartmentDocument20 pagesGross Anatomy of Posterior Thigh CompartmentOnah ArinzePas encore d'évaluation
- Test ReviewDocument7 pagesTest ReviewOliver NamyaloPas encore d'évaluation
- Alwadi International School Grade 9 Biology 9. Transport in Animals NotesDocument62 pagesAlwadi International School Grade 9 Biology 9. Transport in Animals NotesMohammed HelmyPas encore d'évaluation
- Blood Vessels and Circulation 1Document36 pagesBlood Vessels and Circulation 1Kuya RnJPas encore d'évaluation
- Chp 05 (Blood and Circulation) DrRiyadAhmed PC 3Document69 pagesChp 05 (Blood and Circulation) DrRiyadAhmed PC 3Kamrun NaherPas encore d'évaluation
- Management of Clients With Lower Urinary Tract Disorders - Cys$$s - Urethri$s - UrosepsisDocument26 pagesManagement of Clients With Lower Urinary Tract Disorders - Cys$$s - Urethri$s - UrosepsisLouise Anne Agnazata GayoPas encore d'évaluation
- Uri Sys HO1Document25 pagesUri Sys HO1Louise Anne Agnazata GayoPas encore d'évaluation
- Anatomy & Physiology Myelodysplastic Syndrome: PathophysiologyDocument8 pagesAnatomy & Physiology Myelodysplastic Syndrome: PathophysiologyLouise Anne Agnazata GayoPas encore d'évaluation
- Heart FailureDocument42 pagesHeart FailureLouise Anne Agnazata GayoPas encore d'évaluation
- Valvular DiseasesDocument46 pagesValvular DiseasesLouise Anne Agnazata GayoPas encore d'évaluation
- Cardio AssessmentDocument19 pagesCardio AssessmentLouise Anne Agnazata GayoPas encore d'évaluation
- Inflammatory Heart DiseaseDocument69 pagesInflammatory Heart DiseaseLouise Anne Agnazata GayoPas encore d'évaluation
- Hemato LymphaticsCY14 15Document16 pagesHemato LymphaticsCY14 15Louise Anne Agnazata GayoPas encore d'évaluation
- Diseases of Myocardial PerfusionDocument84 pagesDiseases of Myocardial PerfusionLouise Anne Agnazata GayoPas encore d'évaluation
- AneurysmDocument18 pagesAneurysmLouise Anne Agnazata GayoPas encore d'évaluation
- Fluids and Electrolytes: Homeostasis and DisturbancesDocument48 pagesFluids and Electrolytes: Homeostasis and DisturbancesLouise Anne Agnazata GayoPas encore d'évaluation
- Fluids and Electrolytes: Homeostasis and DisturbancesDocument48 pagesFluids and Electrolytes: Homeostasis and DisturbancesLouise Anne Agnazata GayoPas encore d'évaluation
- Pulmonary ContusionDocument83 pagesPulmonary ContusionLouise Anne Agnazata GayoPas encore d'évaluation
- Journal 1Document2 pagesJournal 1Louise Anne Agnazata GayoPas encore d'évaluation
- Ethnographic Investigation of Oral Care in The Intensive Care UnitDocument2 pagesEthnographic Investigation of Oral Care in The Intensive Care UnitLouise Anne Agnazata GayoPas encore d'évaluation
- TPN Journal 1Document2 pagesTPN Journal 1Louise Anne Agnazata GayoPas encore d'évaluation
- Cardiac Monitoring ChecklistDocument6 pagesCardiac Monitoring Checklistdigdag100% (1)
- Science (Mains MCQ Part-2)Document24 pagesScience (Mains MCQ Part-2)Rajat KumarPas encore d'évaluation
- Kasus Acute Alcohol Poisoning ForensikDocument8 pagesKasus Acute Alcohol Poisoning ForensikSheila Sesary JPas encore d'évaluation
- Assessment of The Heart and Neck VesselsDocument10 pagesAssessment of The Heart and Neck VesselsJasmin MolanoPas encore d'évaluation
- Pharmacotherapy Update in Heart Failure: Siti Elkana Nauli Tangerang District HospitalDocument45 pagesPharmacotherapy Update in Heart Failure: Siti Elkana Nauli Tangerang District HospitalFadly AminPas encore d'évaluation
- Lutembacher SyndromeDocument12 pagesLutembacher SyndromeDiany LarasatiPas encore d'évaluation
- Department of Education: in Science 4 On Classroom Observation ToolDocument3 pagesDepartment of Education: in Science 4 On Classroom Observation ToolArlyne Mantillas100% (2)
- BiomdcDocument11 pagesBiomdcNurSyafiqahAbdulHalimPas encore d'évaluation
- Spooky 2 Rife Frequency ListDocument17 pagesSpooky 2 Rife Frequency ListSara100% (2)
- General Biology Q4 M3Document16 pagesGeneral Biology Q4 M3Delfin LeePas encore d'évaluation
- CHFbooklet WebDocument20 pagesCHFbooklet WebjyothiPas encore d'évaluation
- P5 Science SA2 2019 ACS Exam PapersDocument42 pagesP5 Science SA2 2019 ACS Exam PapersAsvinnaah kumarPas encore d'évaluation
- MedicineDocument48 pagesMedicineKasun Perera0% (1)
- Patent Ductus Arteriosus (PDA) Diagnosis and TreatmentDocument19 pagesPatent Ductus Arteriosus (PDA) Diagnosis and Treatmentputri avriantiPas encore d'évaluation
- European Heart Journal (2003) 24, 787-788Document2 pagesEuropean Heart Journal (2003) 24, 787-788api-26263700Pas encore d'évaluation
- Medical Surgical NursingDocument16 pagesMedical Surgical NursingMelvin TarkporPas encore d'évaluation
- Inhouse Cardiac Surgery Team LaunchDocument2 pagesInhouse Cardiac Surgery Team LaunchUmeshPas encore d'évaluation
- Smoking and HypertensionDocument7 pagesSmoking and HypertensionFian Al GhifariPas encore d'évaluation
- 5 Cardiac Cycle & Heart SoundsDocument32 pages5 Cardiac Cycle & Heart SoundsDisha SuvarnaPas encore d'évaluation
- Drugs ORDocument17 pagesDrugs ORCatherine ZamoraPas encore d'évaluation
- Chapter 8 Transport in Mammals - Lecture NotesDocument10 pagesChapter 8 Transport in Mammals - Lecture Notesapi-3728508100% (2)
- Preparing For Post Offer Evaluation & Health History Form 4.26.22Document13 pagesPreparing For Post Offer Evaluation & Health History Form 4.26.22Antonella VitalePas encore d'évaluation
- Syllabus For MD PhysiologyDocument20 pagesSyllabus For MD PhysiologyPhysiology by Dr RaghuveerPas encore d'évaluation
- Proper Vital Signs MonitoringDocument7 pagesProper Vital Signs MonitoringCristoper BodionganPas encore d'évaluation
- Electric Alex 519171918 GernDocument950 pagesElectric Alex 519171918 GernShyamSoniPas encore d'évaluation
- FHS Laying The Foundation From NIHDocument4 pagesFHS Laying The Foundation From NIHantoniocoreo65Pas encore d'évaluation
- Biology: Paper 5090/01 Multiple ChoiceDocument10 pagesBiology: Paper 5090/01 Multiple Choicemstudy123456Pas encore d'évaluation
- Fitness, Sports and Recreation Leadership: Quarter 3 - Module 2Document26 pagesFitness, Sports and Recreation Leadership: Quarter 3 - Module 2Regie Carino100% (2)