Académique Documents
Professionnel Documents
Culture Documents
Week 3 Caiata-Zufferey
Transféré par
coffeedanceCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Week 3 Caiata-Zufferey
Transféré par
coffeedanceDroits d'auteur :
Formats disponibles
This article was downloaded by: [NUS National University of Singapore]
On: 03 November 2012, At: 19:35
Publisher: Routledge
Informa Ltd Registered in England and Wales Registered Number: 1072954 Registered office: Mortimer House,
37-41 Mortimer Street, London W1T 3JH, UK
Health Communication
Publication details, including instructions for authors and subscription information:
http://www.tandfonline.com/loi/hhth20
Physicians' Communicative Strategies in Interacting
With Internet-Informed Patients: Results From a
Qualitative Study
a
Maria Caiata-Zufferey & Peter J. Schulz
a
Department of Sociology, University of Geneva
Institute of Communication and Health, University of Lugano
Version of record first published: 19 Jan 2012.
To cite this article: Maria Caiata-Zufferey & Peter J. Schulz (2012): Physicians' Communicative Strategies in Interacting With
Internet-Informed Patients: Results From a Qualitative Study, Health Communication, 27:8, 738-749
To link to this article: http://dx.doi.org/10.1080/10410236.2011.636478
PLEASE SCROLL DOWN FOR ARTICLE
Full terms and conditions of use: http://www.tandfonline.com/page/terms-and-conditions
This article may be used for research, teaching, and private study purposes. Any substantial or systematic
reproduction, redistribution, reselling, loan, sub-licensing, systematic supply, or distribution in any form to
anyone is expressly forbidden.
The publisher does not give any warranty express or implied or make any representation that the contents
will be complete or accurate or up to date. The accuracy of any instructions, formulae, and drug doses should
be independently verified with primary sources. The publisher shall not be liable for any loss, actions, claims,
proceedings, demand, or costs or damages whatsoever or howsoever caused arising directly or indirectly in
connection with or arising out of the use of this material.
Health Communication, 27: 738749, 2012
Copyright Taylor & Francis Group, LLC
ISSN: 1041-0236 print / 1532-7027 online
DOI: 10.1080/10410236.2011.636478
Physicians Communicative Strategies in Interacting With
Internet-Informed Patients: Results From a Qualitative Study
Downloaded by [NUS National University of Singapore] at 19:35 03 November 2012
Maria Caiata-Zufferey and Peter J. Schulz
Department of Sociology, University of Geneva
and Institute of Communication and Health, University of Lugano
This article describes the strategies used by physicians to interact with Internet-informed
patients, alongside illustrating the motives underlying such strategies. Semistructured interviews were conducted with a sample of 17 physicians from primary care and medical specialist
practices in the Italian part of Switzerland. The sample was diversified in terms of specialty,
age, and gender. Data collection and analysis were driven by grounded theory and supported
by a computer-assisted qualitative analysis program. A typology of four communicative strategies has been outlined. The adoption of these strategies is shaped by physicians general
attitude toward Internet-informed patients, based on their conception of medical information
for lay people through the Internet. However, this general attitude is mediated by doctors
interpretation of the specific communicative context, that is, their appraisal of three aspects:
the patients health literacy, the relevance of the online information to be discussed, and their
own communicative efficacy. At the end, the process of interpretation underlying the strategies
is discussed to expand on it and to identify implications for practice and research.
Nothing has recently changed clinical practice more fundamentally than a communication innovation: the Internet.
This statement reflects the position of a number of scholars and health practitioners concerning the impact of the
Internet on patients, doctors, and their relationship with one
another. In general, the Internet has been seen as having
remarkable potential for improving the physicianpatient
relationship by increasingly sharing the responsibility for
knowledge, by offering the possibility of more collaborative
models of physicianpatient interaction, and by fostering
greater patient involvement in health maintenance and care
(Wald, Dube, & Anthony, 2007). As a matter of fact, numerous studies have shown that the role of the Web in regard to
health care delivery and the physicianpatient relationship
is actually more complex than these positive expectations
suggest.
It is well established that patients increasingly use the
Internet for health information in all western societies (Fox,
2006; Spadaro, 2003). Despite its potential to challenge the
position of the health care provider, patients appear to see the
Correspondence should be addressed to Maria Caiata-Zufferey,
University of Lugano, Institute of Communication and Health, Via G. Buffi
13, 6900 Lugano, Switzerland. E-mail: caiatazm@usi.ch
Internet as an additional resource to support existing and valued relationships with their doctors (Caiata Zufferey et al.,
2010). Moreover, Internet-informed patients (IIPs) usually
report the improvement of their understanding and their ability to manage their health conditions (Akesson, Saveman,
& Nilsson, 2007). But if the lay public generally thinks
positively about health information on the Internet, physicians perceptions are more ambivalent. According to some
authors, health care professionals hold that the popularization of information alerts patients to important symptoms
at an earlier stage (Laing, Hogg, & Winkelman, 2004) and
helps them in the decision-making process (Giveon et al.,
2009). Consultations with IIPs can thus involve a more
patient-centered interaction (Wald, Dube, & Anthony, 2007).
Yet many studies also report negative reactions from physicians. Some doctors believe that Internet information can
generate patient misinformation, leading to distress, or an
inclination toward wrong self-diagnosis and/or detrimental
self-treatment (Ahmad et al., 2006). The consequence is an
increase in the number of patients questions and in requests
for inappropriate or unavailable testing or treatment, which
complicates the medical consultation (Dilliway & Maudsley,
2008) and adds a new interpretive role to the doctors clinical responsibilities (Sommerhalder et al., 2009). In addition,
Downloaded by [NUS National University of Singapore] at 19:35 03 November 2012
PHYSICIANS COMMUNICATIVE STRATEGIES
several authors observed that providerpatient discussions
about Internet health information can be difficult, as the former may feel that patients will be unwilling to accept treatments offered to them or that patients are challenging their
authority (Ziebland et al., 2004). In her review article on
how patients online information-seeking behavior affects
their relationship with health providers, McMullan (2006)
synthesizes physicians reactions to IIPs by identifying
three outcomes: The health professional feels threatened by
patients bringing information into consultation, and reacts
defensively by asserting an expert opinion (professionalcentered relationship); the health professional and patient
work together to find and analyze the information (patientcentered relationship); the health professional guides
patients to reliable health websites (Internet prescription).
If attitudes and behaviors of physicians who are confronted with IIPs are ambivalent, understanding the motives
and the mechanisms underlying these attitudes and behaviors is crucial. Indeed, several studies indicate that physicians validation of patients efforts in health information
seeking on the Internet is essential to patient satisfaction and the reduction of worries (Bylund et al., 2007).
In addition, consultations can be disempowering if physicians refuse to discuss health-related Internet information
with patients (Sommerhalder et al., 2009). Therefore, the
question emerges of how to explain the differential responses
of physicians to IIPs.
A review of the literature provides some insight into
this issue. A first factor that influences the way doctors
respond to IIPs concerns physicians personal characteristics. On this point, Hardey (1999) considers that physicians
who are more accustomed to an authoritarian or paternal
role may have difficulty adjusting to a more collaborative role. Another important factor is the interrelatedness
between physicians and patients attitudes and behaviors.
The literature on doctorpatient interaction states that the
way doctors behave with patients strongly depends on the
way they perceive them and on the inferences they make
from various information cues. For example, Willems and
colleagues (2005) show that doctors are more likely to adopt
a participative style of communication with high-educated
patients than with low-educated patients. Concerning the
specific interaction between doctors and IIPs, Malone et al.
(2004) note that patients who use online information for
self-diagnosis and self-treatment (thus before the consultation) are likely to make doctors feel disempowered; on
the other hand, patients who search for online health information in order to better understand their diagnosis (thus
after the consultation) evoke a more positive attitude from
physicians.
These results show that investigating reciprocity and
mutual influence is a promising direction for the understanding of the interaction between doctors and IIPs. However,
although some hints are provided concerning physicians
differential responses to IIPs, the mechanisms underlying
739
these responses still need to be the focus of a systematic and
deep investigation (Ahmad et al., 2006).
This article reports the results of a qualitative study conducted among a heterogeneous group of Swiss Italian physicians, whose common characteristic was having ever treated
IIPs. The Italian part of Switzerland is a particularly interesting field for this study. The number of regular Internet
users has grown remarkably in recent years in Switzerland:
They were 60% in 2004 (Froidevaux & Tube, 2006) and
75% in 2010 (Froidevaux, 2011). Among Internet users, the
number of those who searched for health information on
the Web has grown from 20% (Froidevaux & Tube, 2006)
to 55% (Froidevaux, 2011) in the same period. The situation is slightly different in the Italian part of Switzerland;
in this region, only 64% of Swiss residents were found to
use the Internet regularly in 2010 (Froidevaux, 2011). While
no prior data exist, we can infer that the percentage was
even lower in the years before. The number of Internet users
for health information is not known, but we can conclude
that using the Internet for health information in the Italian
part of Switzerland is not yet an ordinary behavior, even
though it is certainly becoming more and more frequent.
Swiss Italians physicians are thus good informants of physicians responses to IIPs: The increasing frequency and the
novelty of patients information seeking on the Internet in
their region make them especially able to report what they
do and why.
From a more theoretical point of view, investigating
physicians communicative strategies with IIPs in the Italian
part of Switzerland allows exploration of medical interactions in a context of uncertainty. For Swiss Italian physicians, indeed, patients use of the Internet for health information is a relatively new pattern of behavior that could
undermine the professional monopoly of medical knowledge. When they face IIPs, these physicians have to ask
themselves what the expectations and the preferences of
these patients are. At the same time, they have to reconsider their role as information providers and more generally
as doctors. An increasing level of uncertainty then characterizes this kind of interaction, in the sense that subjects cannot
ascribe a predetermined meaning to a given behavior and
cannot anticipate the outcome of the interaction.
To explore how physicians manage IIPs, a set of sensitizing concepts was used (Strauss & Corbin, 1990). The
concept of reflexivity of Anthony Giddens (1990) appeared
to be appropriate for this study. Reflexivity refers to the fact
that human beings constantly have to monitor their social
practices and to adapt them in the light of incoming information. Reflexivity has always formed an integral part of
the self and of the social relations. However, Giddens argues
that it becomes particularly pertinent in circumstances of
increasing uncertainty: When social practices are no longer
structured by established ways of doing things, the reflexive
monitoring of behavior becomes central and constant. This
study was also informed by the concept of good reasons
Downloaded by [NUS National University of Singapore] at 19:35 03 November 2012
740 CAIATA-ZUFFEREY AND SCHULZ
of French sociologist Raymond Boudon. According to
Boudon (1989), peoples actions are determined by motives
that, despite not always being objectively rational, are
subjectively valid given the situation in which people are.
Subjectively good reasons are seen as valid because they are
founded on theories or conjectures that have been proven
valid in many cases. Therefore, subjectively good reasons
are not arbitrary, but tend to be general in the sense that
most individuals who are placed in the same situation will
tend to perceive the same reasons as good.
This conceptual framework is in line with the interpretative sociology of Max Weber (1968), which is focused on
understanding agency and motives of individuals. On the
basis of it, explaining the differential responses of physicians
to IIPs requires describing physicians actions (strategies)
in this situation and illustrating the good reasons behind
these actions. Illustrating the good reasons of physicians
strategies, then, requires, on one side, depiction of the theories, and, on the other side, highlighting the conjectures that
legitimate these strategies.
Consistently with this framework, three research questions oriented this study:
RQ1: What are the communicative strategies used by physicians when facing IIPs?
RQ2: What are physicians general representations (theories) behind their communicative strategies?
RQ3: What are physicians specific interpretations (conjectures) that influence, in turn, their communicative
strategies?
METHODS
This article forms part of a larger Swiss study that was
designed to explore the impact of popularization of health
information on the Internet on doctorpatient relationships. We adopted a qualitative methodology using a general grounded theory approach (Strauss & Corbin, 1990).
Approval for the whole study was obtained from the governing ethical committee, and informed consent was obtained
from each participant before data were collected.
Semistructured interviews were completed between
2006 and 2008 with a sample of physicians from primary
care and medical specialist practices. We decided to recruit
physicians in one city of the Italian part of Switzerland and
to exclude psychiatrists and paediatricians because of the
specificity of their relationship with their patients. Based on
these criteria, a prominent physician helped us to identify
a set of medical practices that would allow us to explore
physicians communicative strategies with IIPs. Sixty-nine
medical practices were identified, contacted first by letter
and then by telephone. Ten never answered. Twenty-eight
answered that they did not have time. Nine felt that they were
not able to participate because their caseload was old and not
used to the Internet; at our insistence, four of them agreed
to participate only in case we did not find enough participants, but then were unreachable when we tried to recontact
them some weeks later. Twenty-two agreed to participate
straightaway.
In line with the grounded theory approach, data collection and analysis were performed simultaneously until data
saturation was achieved. At the beginning, we interviewed
physicians chosen among those who were more willing to
participate. Then we selected physicians according to the
ongoing analysis: First, we tried to diversify the sample in
terms of physicians age; then, we tried to diversify the sample in terms of their specialty. This procedure allowed us to
maximize the variability of physicians experiences. At the
end, the sample size of 17 participants was judged large
enough to provide a variety of experiences and to allow
sufficient depth in the analysis. Participants were 3 women
and 14 men aged between 40 and 64 years (mean age 52).
They had between 15 and 39 years of practice (mean years
25). They were general practitioners (n = 5), gynecologists
(n = 3), orthopedic surgeons (n = 2), urologists (n = 2),
oncologists (n = 2), and one each were allergist (n = 1),
endocrinologist (n = 1), and rheumatologist (n = 1).
Interviews were conducted in physicians medical practices and lasted about 45 minutes. Participants were asked to
describe their experience with IIPs in the order and manner
desired. However, to make sure all the points were covered, we prepared a flexible interview grid with the main
topics to be treated. Sixteen interviews were recorded and
transcribed to improve data management and content examination. One physician refused to be recorded. In this case,
detailed notes were taken during and immediately after the
interview. The collected data did not allow for a systematic
and refined analysis, as was the case with the other interviews. However, they were used to test the emerging model
and to expand on it. The interview was thus included in the
final sample, even though the lack of verbatim transcription
precludes quotations from it in this article.
During the transcription process, participants personal
data were removed. Data analysis was inspired by the constant comparative method (Strauss & Corbin, 1990). A general inductive approach was used to code every interview, to
link and group the identified codes into larger categories, and
to define more abstract concepts. These operations, which
had to be creative and rigorous at the same time, allowed
for reduction and interpretation of the large amount of data
and were realized with the support of the software for qualitative analysis Atlas.ti (Muhr, 2004). Literature was used
throughout the process of analysis as a means of questioning
and interpreting the retrieved categories. For example, after
we noticed that physicians appraised several characteristics
of the patient in order to decide how to behave, the article
of Willems et al. (2005) helped us to interpret these data by
suggesting the importance of patients education and, finally,
Downloaded by [NUS National University of Singapore] at 19:35 03 November 2012
PHYSICIANS COMMUNICATIVE STRATEGIES
by suggesting the category of patients health literacy. We
sought then evidence for this category by returning to the
data.
The results proposed in this article are the outcome of this
continual to-and-fro movement between empirical data and
developing theory, and provide a general model of physicians communicative strategies with IIPs. The first author
performed the interviews and the analysis. However, the
analysis was regularly discussed by both authors. Some quotations have been chosen from the qualitative data for their
illustrative power. They have been translated word-for-word
from Italian to English. When the extracts were not understandable with a literal translation, we preserved the cultural
meanings and nuances.
RESULTS
According to the participants, patients who search information on the Internet before their medical consultation are still
a minority, although their number has increased in recent
years. However, physicians recognize that probably some
IIPs do not explicitly say that they have been on the Internet
for fear of offending the physician.
When online information is brought to consultationon
the initiative of the patient or at the doctors invitation
doctors state that patients requests are threefold. Patients
may ask for clarification in order to better understand what
they have found. This request is usually followed by one
for contextualization: Patients may ask whether the retrieved
information can be applied to their case. Lastly, patients may
make suggestions on diagnosis and treatment, based on what
they found online.
For all the doctors, patients online information seeking constitutes a potential nuisance for their professional practice, as it disturbs the traditional course of
the consultation. Participants consider that the popularization of health information through the Internet has made
their role more complex, has broken routines and modified standard procedures. The following physician clearly
expresses this feeling, which was actually shared by all the
participants:
You are required to do more. More. You are required to
go beyond a known way of doing things, a usual way of
doing things. And this is not only due to the form of the
information or to the electronic tool. This has really to do
with the content of what you have to say. (endocrinologist,
man, 42)
The key word of the preceding excerpt is more:
Physicians have the feeling that they have to do more, in
terms of the content and of the form of their professional
practice, when they face IIPs. The analysis of the interviews
allows exploring what is behind the word more.
741
Managing the Internet-Informed Patient: A Fourfold
Typology of Communicative Strategies
We can identify four strategies doctors use to deal with IIPs.
These strategies are presented as Weberian ideal types, that
is, as conceptual abstractions from reality described in their
extreme pure form (Weber, 1968).
Resistance to online information. The purpose of
this strategy is to neutralize the IIP. The physicians
communication aims at avoiding the confrontation with
Internet-derived material the patient tries to enter into the
consultation.
Physicians use several techniques to reach this purpose.
Usually they start with ignoring the Internet-derived information offered by the patient, as far as this is possible.
Indeed, some patients do not explicitly say that they have
been on the Internet. Although the content of their speech
and the words they use suggest that this was the case, physicians pretend not to notice it. When doctors cannot avoid
acknowledging the patients information seeking behavior,
they tend to discredit the Internet in a strong and peremptory
way. No dialogue is encouraged on the topic:
When patients tell me, yes, but on the Internet . . . , I
always cut short: On the Web you find everything and its
opposite, so forget it all and listen to what Im saying, which
is the standard. (gynecologist, man, 63)
Another technique to resist consists in devaluing the
online information brought by the patient into the consultation: Physicians show that they knew the information
perfectly and that they have already considered it, even if
they have not discussed it with the patient.
As a last technique, physicians often enjoin IIPs to
choose between the doctor and the Internet. Basically, the
message sent is that going on the Internet was not a good
idea at all, as this 60-year-old surgeon expresses it:
Patients who begin to talk about the Internet, I dont make a
long speech. I mean, if I see that they think they know more
than me, I let them understand that they can go and be treated
by Mister Web. (surgeon, man, 60)
Repairing online information. The purpose of this
strategy is to correct IIPs and relate to them the point of view
of the doctor. The communication process is thus characterized by the transmission of selected medical information
chosen by the doctor according to their representation of
what the patient should know.
Usually physicians start with identifying IIPs, if these do
not mention that they have been on the Internet. For example,
this gynecologist says that he is able to identify IIPs based
on the terms used during the consultation:
Sometimes patients tell me; some others I gather it from
the way they speak. In the sense that sometimes they come
out saying Ah, but dysplasia and I think that they do
not even know if this is ham or cheese! And thus I say:
742 CAIATA-ZUFFEREY AND SCHULZ
Downloaded by [NUS National University of Singapore] at 19:35 03 November 2012
Excuse me, but where did you read that? And then I have
it. (gynecologist, man, 52)
Once the IIP has been identified, the repairing strategy
requires that the physician warns the patient and argues the
limits of the Internet. Attempts at persuasion take place and
several arguments are used: The quality of online information is bad, patients do not have enough experience to
identify relevant information, etc.
Physicians continue with evaluating the information
brought up by the IIP according to what they think the
patient should know. It is possible that the physician takes
time to understand the information brought to the consultation and suggests discussing it in a further consultation.
Regardless, when the discussion takes place, the physician
determines the value of the information. Once the doctor has
appraised it, the communication process is understood to be
a one-way flow: The doctor clarifies and contextualizes the
information following evidence-based criteria, and usually
no place is left for a dialogue around it. Doctors consider
this process of evaluation a necessary work in order to set
the record straight:
For us, the doctors, the problem is that before starting you
have to destroy. Patients come already with their theory and
you have to dismantle it. It takes some care, and then you
need to start anew. (allergist, man, 52)
Doctors who adopt the repairing strategy usually finish
by dissuading the patient from turning to the Internet again.
The dissuasion is often an implicit message of the warning process, but sometimes physicians also suggest explicitly abandoning the Internet information-seeking behavior.
Basically, the ultimate message is that going online to find
health information is not a good idea, but as it was done, it
is now necessary to make good on this mistake.
Coconstruction around online information. The purpose of this strategy is to build a shared reality with the
patient using the online information brought to the consultation as a springboard for the discussion. Doctors aim to
create a consensus concerning the diagnosis and the treatment, and they use the online information as a starting point
to understand the patients point of view and to explain their
own.
As in the reparation strategy, physicians who adopt
coconstruction often start with identifying the IIP. Different
from the repairing strategy, however, a dialogue is conducted
once the discussion takes place. The communication process is understood to be a two-way flow: Physicians ask IIPs
questions in order to understand their motivations for searching for information, their views on their situation, eventually
their fears and preferences concerning the treatment; at the
same time, they clearly propose their own evaluation of the
information, based on their scientific knowledge but also
taking into account the point of view of the patient. Risks
implied in relying on the Internet are not stressed, as the
online information is not the main focus of the discussion
but only the starting point to build a shared reality. A patientcentered evaluation of the online information brought to the
consultation is thus realized. On this point, a male urologist
stresses the importance of working together to decide a
diagnosis and a therapy:
I simply say: Explain to me your problem. I try to focus
on their problem. Then we examine, we evaluate, we reject
hypotheses and we make the diagnosis. . . . We do not
discuss the validity of the Internet. In the end, retrieved information is marginal. I try to give patients a hand, I try to better
understand them, we make the diagnosis together, and we
decide the therapy together. (urologist, man, 44)
Evidence-based medicine guidelines are used as an indispensable resource in order to evaluate the information.
However, doctors accept going beyond these guidelines in
order to integrate the patients perspective. As an illustration, another urologist justifies the importance of integrating
the patients perspective by claiming that each patient is
unique, while the doctor is not necessarily in possession of
the absolute truth:
We take care of patients, we do not treat prostates. Thus,
guidelines are suitable as they show a direction, but one must
be able to go beyond standard indications. Because, after all,
who needs guidelines? Those who are not good, those who
are not able to take responsibility for their patient. . . . I have
learnt to take responsibility for my patients. I do things, I
observe, I look, but I know that I am not the truth holder just
because I am the physician. Thats why I always take into
account the point of view of the patient. (urologist, man, 53)
Coconstructive doctors usually end by encouraging the
patient to come back with other information and to discuss
it. The message sent, thus, is that going on the Internet is a
good idea, as it is gives patients a chance for discussing their
health problem more deeply with the physician.
Enhancement of online information. The purpose of
this strategy is to empower IIPs, that is, to make them proactive and provide them with the instruments to obtain other
good quality information.
In this case also, physicians often start with identifying
IIPs. They tend then to ask them about their information
searching process, that is, about how they performed it and
what they found. In this way, they evaluate patients competences in searching for health information online, and they
explore what kind of information patients have found, and
what kind of information they still need or want in order to
have a clear picture of the situation.
Regarding the specific online information brought to the
consultation, physicians conduct a neutral evaluation of it:
They complete it by adding other details, they mention
costs and benefits of the therapies, and they clearly talk
about possible risks. This evaluation is supplied in a very
objective way, and is usually devoid of value judgments
Downloaded by [NUS National University of Singapore] at 19:35 03 November 2012
PHYSICIANS COMMUNICATIVE STRATEGIES
743
or personal suggestions. This excerpt from a 60-year-old
surgeon provides a good example:
than curing, one has to discuss. Yet discussing is by far not
considered the most important part of the job of physicians:
When patients come in my medical practice, they often get
scared [laughing]. Maybe then they regret that they have
asked me . . . [laughing]. Even though it is simply a gall
bladder or an inguinal hernia, I explain to them everything, I
explain also that they can die. Yes, I prefer doing it that way.
(surgeon, man, 60)
That kind of patient puts you on the spot, because you always
have to justify yourself, and the discussion takes long time.
. . . You fail to do your job, you cannot stop explaining.
(general practitioner, woman, 46)
Physicians usually finish by suggesting new valuable
information sources and by instructing patients about how to
recognize high-quality websites. The message sent by doctors who adopt the enhancement strategy is therefore that
going on the Internet is an excellent idea, as long as one is
able to select high-quality information sources.
The Good Reasons Behind the Strategies: General
Representations
How can we explain the adoption of the strategies just
described? The analysis of the interviews shows that a first
factor to be taken into account is the doctors representation of the IIP in general. In other words, physicians are
strongly influenced by their idea of health information for
patients and, consequently, by their idea of the Internet as
a tool for health information. Based on these conceptions,
doctors can be categorized as having a primarily resistant,
repairing, coconstructive, or enhancing attitude.
There is a clear difference between resistant physicians
and the three other categories concerning the conception of
health information patients hold. Resistant physicians tend
to consider patients information harmful. They consider
that the role of the doctor is curing the patient, and that the
role of the patient is complying with the doctor in order to
recover as soon as possible. Information is not taken into
consideration, as the two partners are considered too different to communicate on medical questions. A 59-year-old
surgeon exemplifies this point of view:
Doctors and patients . . . speak two completely different languages. As if I said my motor car has 120 horsepower and
one thinks that in my car there are 120 horses riding! The
problem is that the patient does not understand the problem
of the motorcar; they have a different idea of horses. This is
why you need to put things in order. Computer, informatics,
I do not understand anything about that, and I do not debate
with experts. (surgeon, man, 59)
Information is seen as harmful because it prevents the
doctor and the patient from doing their real jobs, which are
curing people (the doctor) and being committed to recovering (the patient). Consistent with this conception of patients
information, the Internet, as any other media source, is
considered a danger to the patients health and to the doctor successfully doing his work. A 46-year-old participant,
for example, emphasizes that patients who are too wellinformed make physicians unable to do their job: More
In contrast to resistant physicians, doctors belonging to
the three other categories agree in considering information
a necessary and positive aspect of the patients health care
and the doctorpatient relationship. All suggest that it is
the patients right to be informed and that well-informed
patients will be more compliant and satisfied. However,
physicians differ with regard to who should inform the
patient.
Repairing physicians think that health information should
be delivered exclusively by health professionals in the context of the medical consultation. They think that the popularization of health information generates confusion and
misunderstanding. Information should thus be selectively
provided by doctors, based on their experience and on their
knowledge of the patient. The underlying conception of the
doctors and the patients roles implies that the former is to
cure patients and transmit to them some information to make
them understand what is happening; the latter is to try to
understand the medical intervention and to comply with it.
As a 57-year-old general practitioner says:
Information is not necessarily good for everybody. It can
generate useless worries, lead people to imagine wrong
diagnoses, lead people to imagine side effects, etc.
Therefore, information is okay, but only if it is a well-judged
information, if it is adjusted to single patients and to their
capacity to integrate it. This is why informing is a doctors
task: because the doctor knows their patients. (general
practitioner, man, 57)
As a consequence, repairing doctors consider the Internet
a risk that they have to defuse. This risk is all the more acute
because of the characteristics of the tool: The Internet is
considered easily accessible, yet greatly unreliable.
Coconstructing physicians do not discriminate against
primary sources of health information. On one side, they
conceive that their role is to build an agreement on the diagnosis and the treatment, taking into account both patients
point of view and objective biological facts. On the other
side, they define the patients role as participating in
healthcare, providing information, suggesting preferences,
and negotiating decisions. Thus, coconstructing physicians
consider any health information the patient can find as valuable, provided that this information is discussed with a
health professional in the context of the medical consultation. This point of view is observable in the next excerpt:
In my opinion, people have to be informed, people have to
know what they have to face. In my opinion, this is right.
However, it is not right to think that if one is informed,
744 CAIATA-ZUFFEREY AND SCHULZ
Downloaded by [NUS National University of Singapore] at 19:35 03 November 2012
then they will be free to decide. This is not right, because
those who face a health problem, they are not free. It is up
to the doctor to propose a treatment, and to persuade them,
as well. Because one needs to be convinced. (gynecologist,
woman, 53)
This type of physician considers the Internet, as well
as any other source of health information, a powerful tool.
Certainly, the Internet can eventually involve some risk.
Starting from the online information, nonetheless, doctors
can better understand their patients, they can propose a
diagnosis and a treatment that takes into account patients
psychosocial characteristics, and they can obtain patients
trust and adherence. As this 44-year-old urologist says, then,
in the end the Internet constitutes an opportunity for the
doctor:
I see a lot of advantages for the doctor. I mean, the patients
have got information, they have seen with their own eyes,
they have dealt with the topic. Therefore it is possible to
talk . . . extensively. Because they are prepared, they already
know something, and then it is easier to explain and to
discuss. (urologist, man, 44)
Similar to coconstructive physicians, enhancing doctors
do not discriminate against primary sources of health information. They consider that any medium is a legitimate
provider of health information, as long as high quality is
guaranteed. Implicitly, these doctors consider that patients
have the responsibility for decisions in their health care,
and that they are able to make the best decision, provided
that they base their decision on high-quality information.
For example, this 44-year-old doctor argues that high-quality
information helps patients in recognizing symptoms:
I think it is a good thing for patients to have access to medical
information. . . . But this only applies to high-quality information. Because it makes people proactive. For instance, it
makes people aware of insidious health problems that are
often discovered too late. (urologist, man, 44)
In this conception, the Internet is considered an opportunity for the patient. However, the condition to exploit it at
its best is that patients acquire a high competence in searching and evaluating information. It is part of the doctors role,
then, to instruct the patient in properly using this medium.
The Good Reasons Behind the Strategies: Specific
Interpretations
The doctors general representation of the IIP as already
discussed is important to understand the adoption of
the communicative strategies. Resistant, repairing,
coconstructive, and enhancing doctors, indeed, differ
in their level of openness toward online health information
for patients: Resistant physicians are the least open, while
enhancing doctors are best disposed toward it. Based on
their level of openness, physicians tend to adopt different
behaviors.
However, the interviews show that things are more complicated than it might appear. When asked to describe specific examples of interactions with IIPs, it clearly appears
that participants vary their strategies between and within
consultations. The majority of the participants are thus
not bound to a particular position: Although they claim
a basic general attitude toward IIPs, their actual way of
managing them, in the end, depends. A 53-year-old urologist provides the best illustration of this phenomenon.
He describes his communicative strategies as being often
between reparation and coconstruction. Asked about this
apparent contradiction, he answers:
You need to do the right thing with the right person. With
some people you take the time to look at the information
together, to evaluate it together. But there are also situations
where you say no, I dont want to go into it. You have to
consider, evaluate and grade, you need to weed some things
out and to keep others. (urologist, man, 53)
A closer examination of the physicians accounts shows
that the level of openness toward health information held by
patients can be increased or decreased based on a second
factor, that is, the physicians interpretation of the specific
communicative context with the IIP. In particular, doctors
act relying on their assessment of three aspects: the patients
health literacy, the relevance of the online information, and
their own communicative efficacy.
Patients health literacy. A perceived low level of
patients health literacy encourages physicians to adopt
a closed-minded position toward Internet information,
whereas a perceived high level pushes them to be more welldisposed. Health literacy is usually judged on the basis of
the patients cognitive and social skills. Regarding cognitive
skills, a highly educated patient is considered better able to
manage health information than someone with only a basic
education. Nonetheless, sometimes physicians are open to
IIPs with a lower level of education if these can count on the
assistance of highly educated family members. Additionally,
patients cognitive skills are evaluated also based on the
quality of the information brought into the consultation.
A 42-year-old physician emphasizes this point:
On electronic media, patients find information that is quite
crazy, and it puts me off beginning to have a closer look at it.
Yes, I say, My goodness, from where do we begin? Dont
you want to listen to me and thats enough? (endocrinologist, man, 42)
As for social skills, they refer to the patients ability to
behave properly with the doctor, that is, to respect the roles
by recognizing the doctors expertise and by remaining open
to their suggestions and remarks. If doctors think that IIPs
behave properly, it is likely that they will treat them with
PHYSICIANS COMMUNICATIVE STRATEGIES
more benevolence than someone with a self-important attitude. A 53-year-old urologist provides a clear example of
this:
Downloaded by [NUS National University of Singapore] at 19:35 03 November 2012
A few times, when I was really exasperated, I have said:
Time is up! Those people were arrogant, and I have said
Time is up! Two of them then left really pissed, but after
the third repetition of the same thing . . . Some patients do
not want to understand: They have their idea and they want
me to agree with it. (urologist, man, 53)
Relevance of the online information to be discussed.
A perceived low level of relevance encourages physicians to
adopt a closed-minded position toward the Internet-retrieved
information held by a patient, whereas a high level pushes
them to be more well-disposed. Relevance is primarily
defined in terms of its direct influence on the patients health
and general well-being. Usually, the information is considered relevant if it refers to rare or chronic diseases. In these
cases the information-seeking behavior is considered perfectly legitimate, as it helps patients to better understand
their health problem and to manage it in their daily life.
The physicians position toward information seeking in
case of serious disease is more ambiguous. Some doctors
think that in case of serious disease the patient has neither the
skills nor the tranquility to search and evaluate health information on the Internet. In contrast, other physicians consider
it perfectly legitimate that patients search for health information in the case of life-threatening diseases, because of the
issues involved in their situation. Some physicians also evaluate the relevance of the information based on the interest
the patient shows toward it and on their preferences.
Physicians communicative efficacy. When they
have to decide how to respond to IIPs, physicians also estimate their own capacity or possibility of discussing the
online information in a satisfactory way. If they estimate that
their communicative efficacy in a specific situation is low,
physicians tend to adopt a closed-minded position toward
IIPs. On the other hand, if they think that the level of
their communicative efficacy is high, they tend to be more
well-disposed.
Physicians primarily assess their communicative efficacy
on the basis of their medical knowledge around the information brought into the consultation. The next account is particularly illustrative on this point. The participant explains
that he tends to adopt a resistant attitude with IIPs when he
feels uncertain on the topic to be discussed.
The problem is that today it is not easy to make things
understandable, because often even us, the doctors, we do
not understand what we are saying. . . . I give an example:
breastfeeding and allergy. I have heard everything and its
opposite: Avoid everything, otherwise the baby will become
allergic; eat everything to diminish intolerance; eat everything, except this and this. Every three years there is a new
theory. . . . A woman comes and tells me that she has heard
this and that. As a doctor, I tell her the current theory and
745
meanwhile I think: What a fib am I telling? In three years,
this will be worthless. . . . This is our problem: we are
not sure anymore. We, the doctors, we are more and more
unsure, and we are not able to give good reasons. You can
imagine that I didnt feel very comfortable with this woman.
(allergist, man, 52)
Sometimes, it also happens that physicians evaluate their
communicative efficacy based on the time they have for discussing with patients. On this point, the experience of this
57-year-old GP is illustrative:
It depends how the day is going on, too: A few days ago,
there was a medical emergency and afterward the waiting
room was crowded. A patient came with some printed sheets
and I passed him by in a flash. Of course, I am not proud of it,
but one has to come to terms with the reality. And to discuss
takes time. (general practitioner, man, 57)
To summarize, doctors communicative strategies are
influenced by their appraisal of the communicative context
in which they are involved. As three aspects are taken into
consideration, the chosen communicative strategy is usually
a kind of compromise. The following physician is clear
about this point:
You know, apparently physicians behave having in their head
an idea of what the doctorpatient relationship should be, but
actually I can assure you that for every act I commit, I have a
lot of things in my head. Every act is ... how to say ... a reasonable compromise between several alternatives. (general
practitioner, man, 49)
DISCUSSION AND CONCLUSION
In this article, we have outlined a general model of the
strategies used by physicians in interacting with IIPs, starting from the point of view of the physicians themselves.
In general, the analysis confirms that patients online information seeking is not yet the norm in the Italian part of
Switzerland. According to the participants, only a minority
of patients searched for health information in the Internet
prior to their appointment. This perception may be explained
by the fact that the number of IIPs is still moderate in this
region (Froidevaux, 2011). It is also possible that IIPs did
not tell the doctor that they had surfed the Internet, as this
behavior may be seen as improper. This is all the more likely,
as physicians still represent the most legitimate source of
information for health topics among the Swiss population
(Seematter-Bagnoud & Santos-Eggimann, 2007). Thus, it
is no accident that the interviewed physicians consider the
course of the medical consultation as being disturbed by
patients who introduce the Internet in it.
In this context, four physicians responses to IIPs emerge:
resistance, repairing, coconstruction, and enhancement. The
former two can be considered physician-centered strategies, the latter two patient-centered strategies. Physicians
Downloaded by [NUS National University of Singapore] at 19:35 03 November 2012
746 CAIATA-ZUFFEREY AND SCHULZ
opt for a particular communicative strategy on the basis
of their conception of the medical information available to lay people on the Internet. This general attitude toward IIPs is then mediated by physicians interpretation of the specific communicative context, that is,
their appraisal of the patients health literacy, the relevance of the online information to be discussed, and their
own communicative efficacy. These results are summarized in Table 1. Based on these considerations, we can
argue that physicians communicative strategies are partly
personality-dependent, that is, resulting from a stable
system of beliefs, and partly context-dependent, that is,
depending on circumstances, time and place, thus subject to
vary across situations.
The variety of physicians responses to IIPs is consistent with the consulted literature. Several studies have
observed the same diversity in physicians attitudes toward
IIPs. The Internet has been found to be seen both as a
source of opportunity and a source of trouble (Ahmad
et al., 2006; Sommerhalder et al., 2009). Similar to our
study, furthermore, the literature shows that physicians
may react to IIPs in different ways. For example, the
three responses identified by McMullan (2006) can be
related to the four communicative strategies described
in this article (defensive reaction parallels resistance and reparation, collaborative reaction parallels
coconstruction, Internet prescription reaction parallels
enhancement).
If we consider how the Internet influences the doctor
patient relationships in general, we can see that it does not
necessarily shift consultations toward patient-centeredness,
as it could be expected (Wald, Dube, & Anthony, 2007).
With reference to Roters (2000) prototypes of doctor
patient relationship, we can assume that the physicians
strategies of resistance and repairing will generate a paternalistic relationship, provided that the patient accepts the
doctors dominance in agenda setting, goals, and decision
making. In contrast, a default relationship will develop if
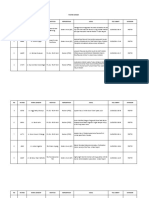
TABLE 1
Physicians Communicative Strategies in Interacting With Internet-Informed Patients
Resistance
Characteristics of the
communication
strategies
General
representations
behind the
strategies
Specific
interpretations
behind the
strategies
Repairing
Coconstruction
Enhancement
Purpose
Neutralize the
patient
Correct the patient
Build a shared reality
with the patient
Empower the patient
Techniques
Ignore the patient
Discredit the Internet
Devalue the online
information
Enjoin to avoid other
online information
Identify the patient
Argue the limits of the
Internet
Evaluate the online
information in a
physician-centered
way
Dissuade from
looking for other
online information
Identify the patient
Ask about motives of
online health
information
Evaluate the online
information in a
patient-centered
way
Encourage to come
back with other
online information
Identify the patient
Ask about modalities
and results of
online health
information
Evaluate the online
information
neutrally
Suggest new
high-quality online
information
Ultimate message
Its bad that you
were on the
Internet.
Its bad that you
were on the
Internet, but lets
consider what you
have found.
Its great that you
were on the
Internet. Lets
consider what you
have found.
Its great that you
were on the
Internet. Here are
some other good
websites.
Conception of health
information for
patients
Information is useless
or harmful
Information is fine
only if it comes
from the
consultation
Information is fine
only if it is brought
to the consultation
Information is fine
only if it is of good
quality
Conception of the
Internet as provider
of health information
Internet as a damage
Internet as a risk
Internet as an
opportunity for the
doctor
Internet as an
opportunity for the
patient
Patients health literacy
Low health literacy- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -High health literacy
Information relevance
Low relevance- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -High relevance
Physicians
communicative
efficacy
Low efficacy- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - High efficacy
Downloaded by [NUS National University of Singapore] at 19:35 03 November 2012
PHYSICIANS COMMUNICATIVE STRATEGIES
the patient contests it. Coconstruction is likely to produce
mutuality, that is, the doctor and the patient are both experts
in their fieldsmedical discipline for the doctor; values,
needs, and experience of the body for the patientand
become partners in negotiating goals, agenda, and decisions.
Yet the relationship may come to a kind of default if the
patient refuses to go along with the physicians expectations.
Lastly, enhancement will generate a consumerist relationship if the patient accepts being an autonomous decision
maker, or a default relationship if the patient refuses to
assume this role. In brief, the Internet may affect the doctor
patient relationship differently, depending on physicians
responses and on patients expectations. The default relationship may be frequent, since it is not rare that physicians
and patients perspectives differ in terms of the way of treating the online information during the medical consultation
(Imes et al., 2008).
Beyond confirming the ambivalence of the Internet in
shaping the doctorpatient consultation, the main contribution of this study is the illustration of the mechanisms
underlying the physicians communicative strategies. In particular, this article highlights the process of interpretation of the communicative context that physicians perform during the medical consultation and that ultimately
informs their responses to IIPs. This finding is consistent
with the literature that claims the importance of interrelatedness of patients and physicians in the understanding
of the medical interaction (Ahmad et al., 2006; Bylund
et al., 2007; Malone et al., 2004; Willems et al., 2005).
However, our study goes beyond that, in the sense that it
describes how in fact physicians interpret the communicative
context.
The process of interpretation is necessary as the interaction with an IIP patient involves a dimension of uncertainty
for the physician: When confronted with IIPs, physicians
have to wonder about the patients capacity to understand,
the patients expectations and preferences in terms of information, and their own capacity to explain. Consultations
with IIPs, indeed, present some risks for the physicians,
such as the risks of misleading the patient, of displeasing the
patient by refusing to join a discussion of online information,
or of losing face. To manage these risks, physicians have to
increase their level of reflexivity, with reflexivity referring
to the constant revision of social activity in light of incoming information (Giddens, 1990). Physicians cannot simply,
as in the golden age of doctoring, serenely dispense
both medication and authoritative judgment (McKinlay &
Marceau, 2002); they are involved in a continuous process of
recognition of self and of other, that is, they have to reflect
actively on their own and others actions in order to make
sense of the best way to act and thus to orient their behaviors. Certainly this is valid for any medical consultation
these days, but it is particularly true for consultations including IIPs, because of the specific dimension of uncertainty
involved in them.
747
What is important to underline is that this process of
interpretation is complex, delicate, and crucial. First, it is
complex because physicians have to take into account three
different factors simultaneously: the patients health literacy, the relevance of the online information to be discussed,
and their own communicative efficacy. These three factors
might suggest contradictory paths of action. For instance, a
health-literate patient would encourage an enhancing strategy, but if this literate patient wants to discuss irrelevant
information in depth, this would rather suggest a resistant strategy. This shows that the process of interpretation
also requires a work of arbitrage in order to decide what
aspect to favor. Second, it is delicate because the risk of
mistakes is always present and cannot be ignored. Indeed,
as doctors adopt their communicative strategies based on
their appraisal of different aspects that might contradict one
another, the adopted strategy might be a compromise that
does not perfectly fit the patient. Additionally, the literature has shown that physicians inferences about patients
are often incorrect (Charles, Gafni, & Whelan, 1997). Third,
the process of interpretation is crucial because wrong inferences can create misunderstandings and decrease the quality
of health care (van Ryn et al., 2006) and, consequently,
impact patients health outcomes (Travaline, Ruchinskas, &
DAlonzo, 2005).
Beyond illustrating the interpretation process that underlies the way physicians adopt their communicative strategies
when facing IIPs, this study provides an example of reflexivity in action. This example confirms Giddenss idea (1990)
that reflexivity is a central issue in uncertain interactions, and
that it has a double-edged nature, meaning that it leads to
greater flexibility of action, but at the same time it requires a
continuous and demanding work to adjust ones behavior
to others. Despite the effort made to monitor their own conduct and that of others and to revise their social activities in
light of incoming information, however, no certainty exists
about the success of the behavioral adjustment and about the
outcome of the interaction.
These findings should be considered in light of the
studys limitations. Physicians strategies were explored
through semistructured interviews. This method was appropriate to understand the logic behind physicians behaviors,
but it did not allow examining the strategies in situ. Data
collected thus rely on physicians reconstruction. Besides,
the sample might be biased toward those doctors who were
willing to tell their experience. We also could not reach a
balance between men and women. Finally, because of the
limited number of the interviews, we could not examine the
role of specific variables, such as physicians age, familiarity
with the Internet, or specialty.
Despite these limitations, this study allows a better understanding of physicians behaviors with IIPs and of the
process by which these behaviors occur. Some practical
implications result from it. From the point of view of the
doctor, all the communicative strategies are legitimate ways
Downloaded by [NUS National University of Singapore] at 19:35 03 November 2012
748 CAIATA-ZUFFEREY AND SCHULZ
of interacting with IIPs. However, coconstruction can be
considered the best approach, as the Internet is used in this
situation as a means of strengthening rather than weakening
the physicianpatient bond. Two main implications for the
encouragement of coconstruction emerge from this study,
one that is physician oriented and the other that is patient
oriented. First, it would be important to develop health
communication training programs for doctors that take into
account the characteristics of the process of interpretation.
For example, it could be useful to increase physicians
awareness of their communicative strategies and of the
motives underlying their strategies. It may also be important to encourage physicians to avoid implicit inferences,
because these could be erroneous. For example, it is possible that information considered irrelevant by the physician
is important for the patient. Finally, techniques could be
suggested to physicians to face IIPs when they feel unsure
about the online information. For example, the physician
could suggest a follow-up consultation, in order to have
time to examine the online information prior to discussing
it. Second, this study has also shown that patients attitudes and behaviors contribute to shaping the way physicians
think and communicate about the illness that patients suffer
from. Patients could therefore be sensitized to their power in
medical consultation. This could be achieved, for example,
through patients association, through flyers from medical insurances, or through specific educational programs.
Websites monitored by health professionals could furthermore be offered to patients in order to help them retrieve
high-quality health information to be discussed with their
physician.
This study also suggests directions for future investigations. First, a validation study of the process of interpretation
would be useful. In this work, we have identified three
factors that physicians consider simultaneously when they
decide how to manage IIPs. Focus groups with different
kinds of physicians could help to complete these factors
and to deepen our understanding of their role in the choice
of communicative strategies. Second, quantitative designs
could be utilized to investigate the variables associated with
the resistant, repairing, coconstructive, and enhancing strategies. For example, it would be worthwhile to examine the
effects of physicians age, familiarity with the Internet,
and specialty on their choice of communicative strategies.
Old age and low familiarity with the Internet are likely
to be correlated with physician-centered communicative
strategies (Hardey, 1999). The role of medical specialty,
however, seems to be more complex. Our hypothesis is
that the medical specialty may influence the feeling of
self-confidence that physicians have in their medical knowledge. In our study, indeed, physicians with clear expertise
(for example, surgeons) seemed to be more confident in
their communicative efficacy than primary care physicians,
who have to face a large variety of health problems without being a specialist in any of them. Furthermore, some
studies argue that the way patients and doctors communicate influences patients behavior, quality of life, understanding of medical information, and even health outcomes
(Travaline, Ruchinskas, & DAlonzo, 2005). Thus, it would
be important to examine the outcomes of the different communication strategies. Third, experimental studies could
be conducted to investigate the work of arbitrage that
physicians do when their interpretation suggests contradictory communicative strategies. A standardized patient
design, for example, could be implemented to manipulate
the patients health literacy, the information relevance, and
the physicians communicative efficacy, in order to determine which of them has the largest effect on physicians
choice of communication strategies. These are all studies
that could help understand what really happens between
physicians and IIPs, why this happens, and what its consequences are, and that could contribute to making these
interactions as efficacious as possible.
REFERENCES
Ahmad, F., Hudak, P. L., Bercovith, K., Hollenberg, E., & Levinson, W.
(2006). Are physicians ready for patients with Internet-based health
information? Journal of Medical Internet Research, 8, e22.
Akesson, K., Saveman, B. I., & Nilsson, G. (2007). Health care consumers
experiences of information communication technologya summary of
literature. International Journal of Medical Informatics, 76, 633645.
Boudon, R. (1989). Subjective rationality and the explanation of social
behavior. Rationality and Society, 1, 173196.
Bylund, C. L., Gueguen, J. A., Sabee, C. M., Imes, R. S., Li, Y., &
Sanford, A. A. (2007). Providerpatient dialogue about Internet health
information: An exploration of strategies to improve the providerpatient
relationship. Patient Education and Counseling, 66, 346352.
Caiata Zufferey, M., Abraham, A., Sommerhalder, K., & Schulz, P.
J. (2010). Online health information seeking in the context of the
medical consultation in Switzerland. Qualitative Health Research, 20,
10501061.
Charles, C., Gafni, A., & Whelan, T. (1997). Shared decision making in the
medical encounter: What does it mean? Social Science & Medicine, 44,
681692.
Dilliway, G., & Maudsley, G. (2008). Patients bringing information to
primary care consultations: A cross-sectional (questionnaire) study of
doctors and nurses views of its impact. Journal of Evaluation in
Clinical Practice, 14, 545547.
Fox, S. (2006). Online health search 2006. Washington, DC: Pew Internet
& American Life Project.
Froidevaux, Y. (2011). Internet dans les mnages en Suisse [Internet in
Swiss households]. Neuchtel: OFS.
Froidevaux, Y., & Tube, V. G. (2006). Utilisation dInternet dans les
mnages en Suisse. Rsultats de lenqute 2004 et indicateurs [Internet
use in Swiss households. Results of the 2004 survey and indicators].
Neuchtel: OFS.
Giddens, A. (1990). The consequences of modernity. Stanford, CA:
Stanford University Press.
Giveon, S., Yaphe, J., Hekselman, I., Mahamid, S., & Hermoni, D. (2009).
The e-patient: A survey of Israeli primary care physicians responses
to patients use of online information during the consultation. Israel
Medical Association Journal, 11, 537541.
Hardey, M. (1999). Doctor in the house: The Internet as a source of lay
health knowledge and the challenge to expertise. Sociology of Health and
Illness, 21, 820835.
Downloaded by [NUS National University of Singapore] at 19:35 03 November 2012
PHYSICIANS COMMUNICATIVE STRATEGIES
Imes, R. S., Bylund, C. L., Sabee, C. M., Routsong, T. R., & Sanford, A. A.
(2008). Patients reasons for refraining from discussing Internet health
information with their healthcare providers. Health Communication, 23,
538547.
Laing, A., Hogg, G., & Winkelman, D. (2004). Healthcare and the information revolution: Re-configuring the healthcare service encounter. Health
Services Management Research, 17, 188199.
Malone, M., Harris, R., Hooker, R., Tucker, T., Tanna, N., & Honnor, S.
(2004). Health and the Internet-changing boundaries in primary care.
Family Practice, 21, 189191.
McKinlay, J. B., & Marceau, L. D. (2002). The end of the golden
age of doctoring. International Journal of Health Services, 32,
379416.
McMullan, M. (2006). Patients using the Internet to obtain health information: How this affects the patient-health professional relationship. Patient
Education and Counseling, 63, 2428.
Muhr, T. (2004). ATLAS.ti (Version 5) [Computer software]. Berlin,
Germany: Scientific Software Development.
Roter, D. (2000). The enduring and evolving nature of the patientphysician
relationship. Patient Education and Counseling, 39, 515.
Seematter-Bagnoud, L., & Santos-Eggimann, B. (2007). Sources and level
of information about health issues and preventive services among youngold persons in Switzerland. International Journal of Public Health, 52,
313316.
Sommerhalder, K., Abraham, A., Caiata Zufferey, M., Barth, J., & Abel, T.
(2009). Internet information and medical consultations: Experiences
749
from patients and physicians perspectives. Patient Education and
Counseling, 77, 266271.
Spadaro, R. (2003). European Union citizens and sources of information about health (Eurobarometer 58.0). Brussels: European Opinion
Research Group (EORG).
Strauss, A., & Corbin, J. (1990). Basics of qualitative research: Grounded
theory procedures and techniques. Newbury Park, CA: Sage.
Travaline, J. M., Ruchinskas, R., & DAlonzo, G. E. (2005). Patient
physician communication: Why and how. Journal of the American
Osteopath Association, 105, 1318.
van Ryn, M., Burgess, D., Malat, J., & Griffin, J. (2006). Physicians
perceptions of patients social and behavioral characteristics and race
disparities in treatment recommendations for men with coronary artery
disease. American Journal of Public Health, 96, 351357.
Wald, H. S., Dube, C. E., & Anthony, D. C. (2007). Untangling the Web
The impact of Internet use on health care and the physicianpatient
relationship. Patient Education and Counseling, 68, 218224.
Weber, M. (1968). Economy and society: An outline of interpretive sociology. New York: Bedminster Press.
Willems, S., De Maesschalck, S., Deveugele, M., Derese, A., & De
Maeseneer, J. (2005). Socio-economic status of the patient and doctor
patient communication: Does it make a difference? Patient Education
and Counseling, 56, 139146.
Ziebland, S., Chapple, A., Dumelow, C., Evans, J., Prinjha, S., &
Rozmovits, L. (2004). How the Internet affects patients experiences of
cancer: A qualitative study. British Medical Journal, 328, 564570.
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Textbook Solution Ch8Document10 pagesTextbook Solution Ch8coffeedancePas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Questions For DSCDocument62 pagesQuestions For DSCcoffeedance0% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Week 3 Health Communication - RuttenDocument4 pagesWeek 3 Health Communication - RuttencoffeedancePas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- FIN3102 Fall14 Investments SyllabusDocument5 pagesFIN3102 Fall14 Investments SyllabuscoffeedancePas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- DSC 1Document7 pagesDSC 1coffeedancePas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Practice MCQ Set 1Document3 pagesPractice MCQ Set 1coffeedance100% (1)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- FIN3102 01 IntroductionDocument88 pagesFIN3102 01 IntroductioncoffeedancePas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Fabozzi Chapter09Document21 pagesFabozzi Chapter09coffeedancePas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Chapter 1: IntroductionDocument13 pagesChapter 1: IntroductioncoffeedancePas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Fabozzi ETF SolutionsDocument10 pagesFabozzi ETF SolutionscoffeedancePas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Corporate Finance Workshop 1Document24 pagesCorporate Finance Workshop 1coffeedancePas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- CH 13 Ans 4 eDocument33 pagesCH 13 Ans 4 ecoffeedancePas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Chapter 15 Questions V1Document6 pagesChapter 15 Questions V1coffeedancePas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Fabozzi ETF SolutionsDocument10 pagesFabozzi ETF SolutionscoffeedancePas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- RWJ CHPT 17Document23 pagesRWJ CHPT 17coffeedancePas encore d'évaluation
- Ross. Westerfield. Jaffe. Jordan Chapter 22 Test PDFDocument26 pagesRoss. Westerfield. Jaffe. Jordan Chapter 22 Test PDFSitti NajwaPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Ross. Westerfield. Jaffe. Jordan Chapter 22 Test PDFDocument26 pagesRoss. Westerfield. Jaffe. Jordan Chapter 22 Test PDFSitti NajwaPas encore d'évaluation
- International FinanceDocument20 pagesInternational FinancecoffeedancePas encore d'évaluation
- Chapter 1 - HandoutDocument21 pagesChapter 1 - Handoutcoffeedance100% (1)
- Wall Color of Patients RoomDocument80 pagesWall Color of Patients RoomHadži Olivera NikolićPas encore d'évaluation
- TSRQ CompleteDocument10 pagesTSRQ CompletedrsheapherdPas encore d'évaluation
- Teresa Iacono 2014 What It Means To Have Complex Communication NeedsDocument6 pagesTeresa Iacono 2014 What It Means To Have Complex Communication Needsapi-260603230Pas encore d'évaluation
- Part B-13-Night Shift SleepDocument4 pagesPart B-13-Night Shift Sleepfernanda1rondelliPas encore d'évaluation
- A Comparative Study of The Clinical Efficiency of Chemomechanical Caries Removal Using Carisolv® and Papacarie® - A Papain GelDocument8 pagesA Comparative Study of The Clinical Efficiency of Chemomechanical Caries Removal Using Carisolv® and Papacarie® - A Papain GelA Aran PrastyoPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- VaccinationDocument22 pagesVaccinationFareed KhanPas encore d'évaluation
- Konker AbstractDocument39 pagesKonker AbstractWigunaPas encore d'évaluation
- Food Affects Mood and EmotionsDocument90 pagesFood Affects Mood and Emotionsarbeta100% (3)
- Summer Internship ReportDocument103 pagesSummer Internship ReportChandan Srivastava100% (4)
- Approach Considerations: Nita V Bhatt, MD, MPH Clinical Instructor, Resident Physician, Department ofDocument7 pagesApproach Considerations: Nita V Bhatt, MD, MPH Clinical Instructor, Resident Physician, Department ofHiLmy ZakiyahPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Manual Service CavitadorDocument29 pagesManual Service CavitadorErik Sanchez HernandezPas encore d'évaluation
- Hypothesis ProblemsDocument7 pagesHypothesis Problemsrj0% (1)
- Introduction Cysts of JawsDocument62 pagesIntroduction Cysts of JawsEnass Alhadi50% (2)
- Mnemonic DeviceDocument12 pagesMnemonic DeviceJonathan ObañaPas encore d'évaluation
- Enoxaparin FDADocument40 pagesEnoxaparin FDAImam Nur Alif Khusnudin100% (2)
- CholesterolDocument76 pagesCholesterolmartyn_brannan100% (1)
- Supervision Professional Disclosure Statement Updated August 2017Document4 pagesSupervision Professional Disclosure Statement Updated August 2017api-337285911Pas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Antihypertensive DrugsDocument64 pagesAntihypertensive DrugsPSC100% (1)
- Powerpoint On Henna LeavesDocument10 pagesPowerpoint On Henna LeavesloloayungPas encore d'évaluation
- Types and Complication of C-SectionDocument13 pagesTypes and Complication of C-SectionMeghaUnniPas encore d'évaluation
- StrategicDocument79 pagesStrategicpradnya7289Pas encore d'évaluation
- Monoclonal AntibodiesDocument35 pagesMonoclonal Antibodiespreetylyall100% (5)
- NewDocument58 pagesNewAkhil SoodPas encore d'évaluation
- Uses of TanninsDocument1 pageUses of TanninsMike SalcedoPas encore d'évaluation
- 2005 - Stavridakis - Immediate Dentin Sealing of Onlay Preparations - Thickness of Pre-Cured Dentin Bonding Agent and Effect of Surface CleaningDocument11 pages2005 - Stavridakis - Immediate Dentin Sealing of Onlay Preparations - Thickness of Pre-Cured Dentin Bonding Agent and Effect of Surface CleaningAndreea BorislavschiPas encore d'évaluation
- Katalog Pavna ANG Siebec-03-WEBDocument24 pagesKatalog Pavna ANG Siebec-03-WEBzanjan98Pas encore d'évaluation
- Compartment ModelsDocument67 pagesCompartment ModelsGhadeer M HassanPas encore d'évaluation
- UK Info & LabelDocument28 pagesUK Info & LabelJenn LamPas encore d'évaluation
- Thyroid TumorsDocument43 pagesThyroid Tumorspleasediscount pleasePas encore d'évaluation
- The Dangers of CrammingDocument2 pagesThe Dangers of CrammingIntan Shafira RachmadhiniPas encore d'évaluation
- The Compound Effect by Darren Hardy - Book Summary: Jumpstart Your Income, Your Life, Your SuccessD'EverandThe Compound Effect by Darren Hardy - Book Summary: Jumpstart Your Income, Your Life, Your SuccessÉvaluation : 5 sur 5 étoiles5/5 (456)
- No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems ModelD'EverandNo Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems ModelÉvaluation : 4.5 sur 5 étoiles4.5/5 (5)
- The 7 Habits of Highly Effective People: The Infographics EditionD'EverandThe 7 Habits of Highly Effective People: The Infographics EditionÉvaluation : 4 sur 5 étoiles4/5 (2475)