Académique Documents
Professionnel Documents
Culture Documents
HRT 09000977
Transféré par
Cory Monica MarpaungTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
HRT 09000977
Transféré par
Cory Monica MarpaungDroits d'auteur :
Formats disponibles
977
EDITORIAL
Anaemia and heart failure
A J S Coats
...............................................................................................................................
Heart 2004;90:977979. doi: 10.1136/hrt.2003.012997
Anaemia has been found to be a common complication of
chronic heart failure, reducing oxygen delivery to the
periphery. Erythropoietin to correct anaemia has a long
history in the management of renal failure with
complicating anaemia, and the first reports of the use or
erythropoietin in heart failure are coming through.
...........................................................................
hronic heart failure (CHF) is frequently
associated with poor exercise tolerance and
debilitating symptoms despite optimal
modern treatment. In the past we expected that
this was due to the direct consequences of poor
cardiac output and congested lungs. Other
important pathophysiological disturbances in
CHF occur as both short and long term consequences of the initial cardiac dysfunction.
These include neurohormonal activation, cytokine release and trophic changes in skeletal
muscle and the peripheral vasculature, and
disturbances in reflex control systems.
The severity of symptomatic exercise limitation
varies between patients, and bears little relation
to the extent of the left ventricular systolic
dysfunction measured at rest, or to markers of
central haemodynamic disturbance.1 Although
there are several reasons for this, much recent
research has suggested that changes which occur
in the periphery as a consequence of the systemic effects of heart failure, may have become
the principal factors limiting exercise.2 Many
changes have been described in skeletal muscle,
peripheral arterial and endothelial function, and
in reflex cardiopulmonary control systems. These
have all been implicated in being limiting
features to exercise tolerance in CHF patients.
In its most severe form this can lead to cardiac
cachexia.3 Major abnormalities in anabolic and
catabolic hormones4 and in immune activation5
have been proposed to explain these developments in CHF. Therapeutic advances in
managing heart failure have followed these
pathophysiological studies, as neurohormonal
blockade rather than positive inotropic treatment
is now the mainstay of CHF therapy.
HEART FAILURE SYNDROME
.......................
Correspondence to:
Professor Andrew J S Coats,
Faculty of Medicine,
University of Sydney,
Sydney, NSW 2006,
Australia; ajscoats@med.
usyd.edu.au
.......................
One manifestation of the heart failure syndrome is the frequent finding of a form of noniron deficient mild to moderate anaemia. This
anaemia has much in common with the better
recognised anaemia of chronic disorders which
appears to be a defect in iron utilisation and
which is a well known complication of chronic
inflammatory conditions. Anaemia is more common in heart failure than could be accounted for
by age or the degree of renal dysfunction. It has
also been realised that this anaemia could
contribute importantly to exercise intolerance
and is associated with a more advanced clinical
severity, a more rapid deterioration in heart
failure, and an increased mortality.
In normal subjects exercise is usually possible
until maximal cardiac output is achieved, at
which time a further increase in workload will
produce extra carbon dioxide (CO2) but with no
commensurate increase in oxygen (O2) uptake.6
This is termed maximal oxygen uptake
O2max). At between 8595% of V
O2max a
(V
point in exercise is reached where there is an
excessive release of CO2 for the rate of O2 uptake
due to a limitation in the rate of delivery of O2
leading to the onset of anaerobic muscular
metabolism with lactate production. This produces arterial acidosis and directly stimulates the
chemoreceptors to produce relative hyperventilation. This point is called the anaerobic threshold.
In most normal subjects exercise is limited by
cardiac reserve, with lung function rarely being
the limiting factor. Training status and genetic
factors determine the overall fitness to exercise.
A reduced oxygen carrying capacity, as caused by
a reduction in haemoglobin concentration,
reduces the effective maximal oxygen carrying
capacity; this effect may be even more pronounced when the cardiopulmonary reserve is
limited, such as it is in chronic heart failure.7
Increasing the haemoglobin concentration will
inevitably increase maximum potential oxygen
delivery, but at the cost of increased blood
viscosity. Thus there is for each individual an
optimal haemoglobin value that is a trade off
between oxygen carrying capacity while avoiding
excess viscous drag to blood flow. In heart failure
this is probably above 12.5 g/dl in most patients.
In confirmation of this theoretical effect we
have recently described a significant association
between haemoglobin concentration and peak
O2 consumption in 113 male patients with
chronic heart failure.8 We found haemoglobin
to be the single most powerful predictor of peak
O2 consumption in this cohort.
The frequency of anaemia in stable treated
chronic heart failure has only recently received
detailed study. An early report from Israel
suggested the prevalence of anaemia (defined
as a haemoglobin concentration , 12.0 g/dl)
varied from 9.1% of patients in New York Heart
Association (NYHA) class I to 79.1% of patients
Abbreviations: ACE, angiotensin converting enzyme;
CHF, chronic heart failure; CRF, chronic renal failure;
EPO, erythropoietin; GFR, glomerular filtration rate;
O2, peak oxygen consumption; SOLVD, studies of left
PKV
ventricular dysfunction; TNFa, tumour necrosis factor a
www.heartjnl.com
978
Editorial
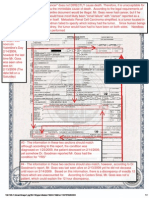
Table 1 Clinical outcomes by heamatocrit (Hct) quartile
Patients hospitalised
Total per patient hospital days
Cardiac per patient hospital days
Mortality
Quartile 1
(n = 66)
Quartile 2
(n = 54)
Quartile 3
(n = 63)
Quartile 4
(n = 56)
p Value
53.0%
7.84
2.77
15.1%
38.9%
7.22
5.53
18.5%
38.1%
2.00
1.55
12.7%
21.4%
1.48
1.05
3.6%
0.005
0.0008
0.03
0.09
Quartile 1: Hct ,35%; Quartile 2: Hct = 3538%; Quartile 3: Hct = 3942%; Quartile 4: Hct .42%.
Reproduced from McClellan et al.18
with NYHA class IV symptoms.9 These estimates are higher
than those seen in subsequent reports, although no true
population report of chronic heart failure has been published
to date. Wisniacki and colleagues found prevalences going
from 0.0% in class I, 36.4% in class II, 52.0% in class III, and
65.9% in class IV.10 In contrast, Tanner and colleagues found
much lower estimates in 193 patients from a tertiary heart
failure outpatient clinic (mean age 54 years) in Switzerland:
7% in class I, 9% in class II, 17% in class III, and 26% in class
IV.11 The frequency is of course dependent on the precise
definition of anaemia. Although less than 12 g/dl is the most
commonly used cut off this is of course arbitrary, and
whether we should use different ranges for women (where
the majority of heart failure patients are post-menopausal) is
also not clear. The estimates of frequency nearly double in the
lower symptomatic classes if a cut off of 12.5 g/dl is used.
CAUSE OF ANAEMIA IN CHF
The cause of anaemia in heart failure is not known. There are
many recognised causes of anaemia such as iron, folate, or
B12 deficiency, which should be looked for and, if found,
treated. One report from Dundee of new heart failure cases
with anaemia found that simple causes of anaemia such as
iron B12 or folate deficiency were rare in heart failure, and
that in most cases of anaemia in heart failure no specific
aetiology could be found.12 There may of course be other
causative or contributory factors operative in heart failure
that can cause anaemia by other routes. These include
dysfunction of the bone marrow caused by low output
failure13 as a result of the effects of cytokine activation. For
example, tumour necrosis factor a (TNFa) can cause anaemia
via known effects, including direct bone marrow depression,
the induction of erythropoietin (EPO) insensitivity, and
interference with the release and utilisation of iron.9 The
TNFa/Fas pathway in lymphocytes has been shown to be
activated in the bone marrow of a heart failure model in
mice, suggesting one possible mode of effect.14 Within a
severe heart failure population Bolger and colleagues recently
showed that circulating concentrations of TNF, soluble TNF
receptor-1, soluble TNF receptor-2, and soluble CD14all
cytokine activation markersall relate strongly to haemoglobin, suggesting that anaemia is related to inflammatory
immune activation in severe CHF.15
Other factors include the known down regulation of EPO
by angiotensin converting enzyme (ACE) inhibitors.16 Heart
failure is frequently associated with a degree of functional
chronic renal failure (CRF) with a relative deficiency of EPO
production. It is not clear how much of the anaemia of heart
failure can be explained by this mechanism, although if
anaemia correction by EPO administration proves to be
worthwhile this might remain a distinction of less practical
importance. Although in heart failure EPO values are raised,
they are still below what they should be, taking into account
the level of anaemia, thus indicating a relative EPO
deficiency.17
In addition to having an impact on exercise capacity,
anaemia complicating heart failure has been shown in several
reports to be associated, possibly causatively, with a worse
outcome. In one retrospective survey of community hospital
admissions for heart failure (665 eligible patients, mean (SD)
age 75.7 (10.9) years), both haematocrit and serum creatinine were independently associated with an increased risk of
death during follow up, after controlling for other patient risk
factors (table 1).18 In one of the largest single centre reports
the heart transplant assessment population of the University
of Californa, Los Angeles (UCLA) was investigated. In a
cohort of 1061 patients with advanced heart failure (NYHA
functional class III or IV) with haemoglobin assessed at the
time of initial evaluation, lower haemoglobin was associated
with an impaired haemodynamic profile, higher blood urea
nitrogen and creatinine, and also with the higher NYHA
functional class (p , 0.0001), and a lower peak oxygen
O2) (p , 0.0001). Survival at one year was
consumption (PKV
higher with increased haemoglobin quartile (55.6%, 63.9%,
71.4%, and 74.4% for quartiles 1, 2, 3, and 4, respectively). On
multivariate analysis adjusting for known heart failure
prognostic factors, low haemoglobin proved to be an
independent predictor of mortality (relative risk 1.131, 95%
confidence interval (CI) 1.045 to 1.224 for each decrease of
1 g/dl).19 In a confirmatory report on a larger multi-centre
Table 2 Interaction between chronic kidney disease, chronic heart failure anaemia and
subsequent mortality
Patient group
Number of patients
2 year death rate (%)
RR (95% CI)
CHF(2)CKD(2)Anaemia(2)
CHF(2)CKD(2)Anaemia(+)
CHF(2)CKD(+)Anaemia(2)
CHF(+)CKD(2)Anaemia(2)
CHF(2)CKD(+)Anaemia(+)
CHF(+)CKD(2)Anaemia(+)
CHF(+)CKD(+)Anaemia(2)
CHF(+)CKD(+)Anaemia(+)
848182
108926
12031
90886
7381
40364
7131
9404
7.7
16.6
16.4
26.1
27.3
34.6
38.4
45.6
1.00
1.90
2.05
2.86
3.37
3.78
4.86
6.07
(reference)
(1.87 to 1.94)
(1.96 to 2.15)
(2.82 to 2.91)
(3.23 to 3.53)
(3.71 to 3.85)
(4.67 to 5.05)
(5.89 to 6.27)
CHF, chronic heart failure; CKD, chronic kidney disease; CI, confidence interval; RR, relative risk
22
Reproduced from Herzog et al.
www.heartjnl.com
Editorial
trial the database of the SOLVD database was studied. Using
a calculated glomerular filtration rate (GFR) the authors
found both lower predicted GFR and lower hematocrit were
risk factors for all cause mortality (p , 0.001 for both). After
adjustment for other factors significant in univariate analysis,
a 10 ml/min/1.73 m2 lower GFR and a 1% lower haematocrit
were associated with a 1.064 (95% CI 1.033 to 1.096) and 1.027
(95% CI 1.015 to 1.038) higher risk for mortality, respectively.
At lower GFR and lower haematocrit, the risk was higher
(p = 0.022 for the interaction) than that predicted by both
factors independently, indicating a possible interaction
between these two risk markers for heart failure mortality.20
A similar effect of low haemoglobin being associated with
increased mortality independent of conventional severity
markers for heart failure was also seen in an analysis of the
ELITE-II trial in moderate heart failure, although in this case
a strong U shaped curve was seen with increased mortality in
patients with haemoglobin concentrations above 15.4 g/dl,
suggesting an optimal haemoglobin value of between 14.5
15.4 g/dl.21 In the largest report to date the claims records of
1 124 302 patients in the US General Medicare database (end
stage renal disease excluded) were identified in a two year
(199697) entry cohort. Chronic renal disease and anaemia
were found independently to confer a twofold increased risk
of death risk, and CHF a nearly threefold increased risk. The
authors summarised that these data suggest a role for
aggressive CHF treatment and anaemia correction in the
elderly (table 2).22
TREATMENT OF ANAEMIA IN HEART FAILURE
There have been only a very small number of reports on the
treatment of anaemia in heart failure patients. In an early
uncontrolled report 26 patients with heart failure and
anaemia treated for an average of 7.2 months with EPO
and intravenous iron were reported to show an increase in
haemoglobin. from 10 to 12 g/dl, an increase in left
ventricular ejection fraction from 27% to 35%, a decrease in
hospitalisations for heart failure by 91%, an improvement
in mean NYHA class from 3.6 to 2.6, and a reduction in
the use of diuretics.9 Although these would be important
benefits, limitations in trial design made them unreliable.
Clearly further evidence from properly controlled trials was
necessary.
In a second report with a control group (although not with
a randomised double blind allocation) 16 patients with
moderate to severe CHF and haemoglobin values persistently
between 10.011.5 g/dl received subcutaneous EPO and
intravenous iron to increase the concentration of haemoglobin to at least 12.5 g/dl. Over a mean (SD) period of 8.2 (2.6)
months, the mean NYHA class improved by 42.1%, the left
ventricular ejection fraction increased by 5.5%, and the need
for oral and intravenous furosemide (frusemide) decreased
by 51.3% and 91.3%, respectively. In addition the number of
days spent in hospital compared with the same period of time
before entering the study decreased by 79.0%.23 A previous
larger randomised controlled trial of recombinant human
erythropoietin (epoetin) in 1233 dialysis patients, many with
symptoms of heart failure, failed to show a benefit of aiming
for higher rather than lower haematocrit values. Surprisingly
the higher haematocrit group showed increased cardiovascular mortality and morbidity despite the fact that within
each randomised group a higher haematocrit was associated
with a lower cardiovascular event rate.24 The explanation for
this apparent conundrum remains unclear despite much
analysis and discussion. What does remain attractive is that
correcting anaemia with EPO or an erythropoietic agent could
not only increase exercise tolerance but possibly also reverse
the excess risk associated with the presence of anaemia in
CHF.
979
CONCLUSION
Our increased understanding of the complex pathophysiology
of heart failure has introduced a new era in the treatment of
heart failure in which anti-neurohormonal and metabolic25
treatments are tested for their ability to improve both
functional capacity and survival of CHF patients. The era of
trials on EPO in this effort looks imminent. Even if the
strategy is successful its role in practice, given the high cost,
may prove difficult to determine.26
REFERENCES
1 Franciosa JA, Baker BJ, Seth L. Pulmonary versus systemic hemodynamics in
determining exercise capacity of patients with chronic left ventricular failure.
Am Heart J 1985;110:80713.
2 Clark AL, Poole-Wilson PA, Coats AJ. Exercise limitation in chronic heart
failure: central role of the periphery. J Am Coll Cardiol 1996;28:1092102.
3 Anker SD, Sharma R. The syndrome of cardiac cachexia. Int J Cardiol
2002;85:5166.
4 Brink M, Anwar A, Delafontaine P. Neurohormonal factors in the development
of catabolic/anabolic imbalance and cachexia. Int J Cardiol
2002;85:11121.
5 Conraads VM, Bosmans JM, Vrints CJ. Chronic heart failure: an example of a
systemic chronic inflammatory disease resulting in cachexia. Int J Cardiol
2002;85:3349.
6 Clausen JP. Circulatory adjustments to dynamic exercise and effect of physical
training in normal subjects and in patients with coronary artery disease.
Progress in Cardiovascular Diseases 1976;18:45995.
7 Tanabe Y, Nakagawa I, Ito E, et al. Hemodynamic basis of the reduced
oxygen uptake relative to work rate during incremental exercise in patients
with chronic heart failure. Int J Cardiol 2002;83:5762.
8 Kalra PR, Bolger AP, Sharma R, et al. The relationship between hemoglobin
and exercise capacity in patients with stable chronic heart failure (CHF).
Circulation 2002;106(suppl):II570.
9 Silverberg DS, Wexler D, Blum M, et al. The use of subcutaneous
erythropoietin and intravenous iron for the treatment of the anemia of severe,
resistant congestive heart failure improves cardiac and renal function and
functional cardiac class, and markedly reduces hospitalizations. J Am Coll
Cardiol 2000;35:173744.
10 Wisniacki N. Is anaemia a cause or a consequence of heart failure in the
elderly? [abstract] Heart 2001;85(suppl I):P4.
11 Tanner H, Moschovitis G, Kuster GM, et al. The prevalence of anemia in
chronic heart failure. Int J Cardiol 2002;86:11521.
12 Cromie N, Lee C, Struthers AD. Anaemia in chronic heart failure: what is its
frequency in the UK and its underlying causes? Heart 2002;87:3778.
13 Chatterjee B, Nydegger UE, Mohacsi P. Serum erythropoietin in heart failure
patients treated with ACE-inhibitors or AT(1) antagonists. Eur J Heart Fail
2000;2:3938.
14 Iversen PO, Woldbaek PR, Tonnessen T, et al. Decreased hematopoiesis in
bone marrow of mice with congestive heart failure. Am J Physiol Regul Integr
Comp Physiol 2002;282:R16672.
15 Bolger AP, Doehner W, Sharma R, et al. Anaemia in chronic heart failure: the
relationship to inflammatory cytokine expression and prognostic importance.
Circulation 2002;106(suppl):5701.
16 Volpe M, Tritto C, Testa U, et al. Blood levels of erythropoietin in congestive
heart failure and correlation with clinical, hemodynamic, and hormonal
profiles. Am J Cardiol 1994;74:46873.
17 Jensen J, Eiskjaer H, Bagger JP, et al. Elevated level of erythropoietin in
congestive heart failure: relationship to renal perfusion and plasma renin.
J Intern Med 1993;233:12530.
18 McClellan WM, Flanders WD, Langston RD, et al. Anemia and renal
insufficiency are independent risk factors for death among patients with
congestive heart failure admitted to community hospitals: a population-based
study. J Am Soc Nephrol 2002;13:192836.
19 Horwich TB, Fonarow GC, Hamilton MA, et al. Anemia is associated with
worse symptoms, greater impairment in functional capacity and a significant
increase in mortality in patients with advanced heart failure. J Am Coll Cardiol
2002;39:17806.
20 Al-Ahmad A, Rand WM, Manjunath G, et al. Reduced kidney function and
anemia as risk factors for mortality in patients with left ventricular dysfunction.
J Am Coll Cardiol 2001;38:95562.
21 Anker SD, Sharma R, Francis D, et al. Anemia and survival in 3044 patients
with chronic heart failure (CHF) in the ELITE II trial. Circulation
2002;106(suppl):472.
22 Herzog CA, Li S, Collins AJ. The impact of congestive heart failure (CHF),
chronic kidney disease (CKD), and anemia on survival in the Medicare
population. Circulation 2002;106(suppl):4712.
23 Silverberg DS, Wexler D, Sheps D, et al. The effect of correction of mild
anemia in severe, resistant congestive heart failure using subcutaneous
erythropoietin and intravenous iron: a randomized controlled study. J Am Coll
Cardiol 2001;37:177580.
24 Besarab A, Bolton WK, Browne JK, et al. The effects of normal as compared
with low hematocrit values in patients with cardiac disease who are receiving
hemodialysis and epoetin. N Engl J Med 1998;339:58490.
25 Harrington D, Chua TP, Coats AJ. The effect of salbutamol on skeletal muscle
in chronic heart failure. Int J Cardiol 2000;73:25765.
26 Coats AJ. Making choices in cardiology: difficulties of rationing and equality
of access. Int J Cardiol 2001;78:20912.
www.heartjnl.com
Vous aimerez peut-être aussi
- What Are Fractures?Document51 pagesWhat Are Fractures?Cory Monica MarpaungPas encore d'évaluation
- Kuliah Hipertensi KrisisDocument31 pagesKuliah Hipertensi KrisisZulfa N. FathPas encore d'évaluation
- Presentation 1Document2 pagesPresentation 1Cory Monica MarpaungPas encore d'évaluation
- Shock Kardiogenik Disebabkan Kegagalan Fungsi Pompa JantungDocument11 pagesShock Kardiogenik Disebabkan Kegagalan Fungsi Pompa JantungCory Monica MarpaungPas encore d'évaluation
- Presentation 1Document2 pagesPresentation 1Cory Monica MarpaungPas encore d'évaluation
- Laporan Ok Prof Budhi Jaya - Cory RettaDocument3 pagesLaporan Ok Prof Budhi Jaya - Cory RettaCory Monica MarpaungPas encore d'évaluation
- Factors Associated with Severe Postpartum HemorrhageDocument27 pagesFactors Associated with Severe Postpartum HemorrhageCory Monica MarpaungPas encore d'évaluation
- Postpartum Hemorrhage Resulting From Uterine Atony.5Document11 pagesPostpartum Hemorrhage Resulting From Uterine Atony.5Cory Monica MarpaungPas encore d'évaluation
- All About The IVP: April 1 2004 Andrea WilsonDocument30 pagesAll About The IVP: April 1 2004 Andrea WilsonCory Monica MarpaungPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Efsa PDFDocument277 pagesEfsa PDFDany DidiPas encore d'évaluation
- History of shingles rehabilitationDocument1 pageHistory of shingles rehabilitationTrixter GarciaPas encore d'évaluation
- Cga - 1Document19 pagesCga - 1Kenji Tolero100% (1)
- Oncology: Nursing Management in Cancer CareDocument27 pagesOncology: Nursing Management in Cancer CareAmy50% (2)
- Oiling The NavelDocument4 pagesOiling The NavelHazel100% (3)
- PCR Test Certificate SampleDocument1 pagePCR Test Certificate SamplegheparduPas encore d'évaluation
- Gastrointestinal Health Problems Test DrillDocument9 pagesGastrointestinal Health Problems Test DrillChristian Angel PoncianoPas encore d'évaluation
- Rotator Cuff Injuries: Symptoms, Causes and TreatmentDocument2 pagesRotator Cuff Injuries: Symptoms, Causes and TreatmentMinnie Hubalde-LoprettiPas encore d'évaluation
- Management of The Infant With Atypical Genitalia (Disorder of Sex Development) - UpToDateDocument31 pagesManagement of The Infant With Atypical Genitalia (Disorder of Sex Development) - UpToDateNicolle SchioPas encore d'évaluation
- Nines P Bautista, MD, MSDocument12 pagesNines P Bautista, MD, MSadnep1991Pas encore d'évaluation
- Powerful Natural Remedies for COVID-19 and Variant StrainsDocument24 pagesPowerful Natural Remedies for COVID-19 and Variant StrainsTracyPas encore d'évaluation
- CongenitalcholesteatomaDocument20 pagesCongenitalcholesteatomaMeilina Elin WardhaniPas encore d'évaluation
- Michael Goss - Death CertificateDocument1 pageMichael Goss - Death CertificateAlex EstradaPas encore d'évaluation
- Hypercalcemia in Dogs Emergent Care Diagnostics and TreatmentsDocument8 pagesHypercalcemia in Dogs Emergent Care Diagnostics and Treatmentstarilubis277Pas encore d'évaluation
- Variability and Accuracy of Sahlis Method InEstimation of Haemoglobin ConcentrationDocument8 pagesVariability and Accuracy of Sahlis Method InEstimation of Haemoglobin Concentrationastrii 08Pas encore d'évaluation
- Pharmacology of GIT: Drugs Used in Peptic Ulcer TreatmentDocument29 pagesPharmacology of GIT: Drugs Used in Peptic Ulcer TreatmentMohammed Bahnasy100% (1)
- Pelvic Traction SlingDocument3 pagesPelvic Traction SlingArturo Jr Garces RNPas encore d'évaluation
- MS Set 1Document6 pagesMS Set 1Julienne ManabatPas encore d'évaluation
- DKD and Sglt2iDocument61 pagesDKD and Sglt2iماكريلا المصريPas encore d'évaluation
- Nutrition Care ProcessDocument22 pagesNutrition Care ProcessIrhamna Fauziah100% (1)
- Integumentary SystemDocument22 pagesIntegumentary SystemEunice Angela FulguerasPas encore d'évaluation
- Common Peroneal Nerve: AnatomyDocument13 pagesCommon Peroneal Nerve: AnatomySitti Maryam AmiliPas encore d'évaluation
- Comparison Between Proprioceptive Neuromuscular Facilitation and Neuromuscular Reeducation For Reducing Facial Disability and Synkinesis in Patients W PDFDocument8 pagesComparison Between Proprioceptive Neuromuscular Facilitation and Neuromuscular Reeducation For Reducing Facial Disability and Synkinesis in Patients W PDFbenjiPas encore d'évaluation
- Pharmacovigilance 1Document28 pagesPharmacovigilance 1Gideon AdurojaPas encore d'évaluation
- Medical-Surgical Nursing 75 Items TestDocument13 pagesMedical-Surgical Nursing 75 Items Testwiffato25% (4)
- EAU Guidelines On Urolithiasis 2022Document114 pagesEAU Guidelines On Urolithiasis 2022Waleed MalikPas encore d'évaluation
- BIOL 0211 - Lab Report 4 - Blood PressureDocument7 pagesBIOL 0211 - Lab Report 4 - Blood PressureFIYINPas encore d'évaluation
- NRes1 AssignmentDocument2 pagesNRes1 AssignmentAinee MeuvinPas encore d'évaluation
- Cetirizine drug study summaryDocument1 pageCetirizine drug study summaryArthur Christopher Corpuz100% (1)
- NUR 102 - Chapter 14 Fluid and ElectrolytesDocument32 pagesNUR 102 - Chapter 14 Fluid and ElectrolytesIanna J. L. Pedrosa100% (1)