Académique Documents
Professionnel Documents
Culture Documents
JR Induk 5
Transféré par
Nurul Falah KalokoTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
JR Induk 5
Transféré par
Nurul Falah KalokoDroits d'auteur :
Formats disponibles
Research
Original Investigation
Effects of Golden Hour Thrombolysis
A Prehospital Acute Neurological Treatment and Optimization
of Medical Care in Stroke (PHANTOM-S) Substudy
Martin Ebinger, MD; Alexander Kunz, MD; Matthias Wendt, MD; Michal Rozanski, MD; Benjamin Winter, MD;
Carolin Waldschmidt, MD; Joachim Weber, MD; Kersten Villringer, MD; Jochen B. Fiebach, MD;
Heinrich J. Audebert, MD
Editorial page 9
IMPORTANCE The effectiveness of intravenous thrombolysis in acute ischemic stroke is time
dependent. The effects are likely to be highest if the time from symptom onset to treatment
is within 60 minutes, termed the golden hour.
CME Quiz at
jamanetworkcme.com and
CME Questions page 135
OBJECTIVE To determine the achievable rate of golden hour thrombolysis in prehospital care
and its effect on outcome.
DESIGN, SETTING, AND PARTICIPANTS The prospective controlled Prehospital Acute
Neurological Treatment and Optimization of Medical Care in Stroke study was conducted in
Berlin, Germany, within an established infrastructure for stroke care. Weeks were randomized
according to the availability of a specialized ambulance (stroke emergency mobile unit
(STEMO) from May 1, 2011, through January 31, 2013. We included 6182 consecutive adult
patients for whom a stroke dispatch (44.1% male; mean [SD] age, 73.9 [15.0] years) or regular
care (45.0% male; mean [SD] age, 74.2 [14.9] years) were included.
INTERVENTIONS The STEMO was deployed when the dispatchers suspected an acute stroke
during emergency calls. If STEMO was not available (during control weeks, when the unit was
already in operation, or during maintenance), patients received conventional care. The
STEMO is equipped with a computed tomographic scanner plus a point-of-care laboratory
and telemedicine connection. The unit is staffed with a neurologist trained in emergency
medicine, a paramedic, and a technician. Thrombolysis was started in STEMO if a stroke was
confirmed and no contraindication was found.
MAIN OUTCOMES AND MEASURES Rates of golden hour thrombolysis, 7- and 90-day
mortality, secondary intracerebral hemorrhage, and discharge home.
RESULTS Thrombolysis rates in ischemic stroke were 200 of 614 patients (32.6%) when
STEMO was deployed and 330 of 1497 patients (22.0%) when conventional care was
administered (P < .001). Among all patients who received thrombolysis, the proportion of
golden hour thrombolysis was 6-fold higher after STEMO deployment (62 of 200 patients
[31.0%] vs 16 of 330 [4.9%]; P < .01). Compared with patients with a longer time from
symptom onset to treatment, patients who received golden hour thrombolysis had no higher
risks for 7- or 90-day mortality (adjusted odds ratios, 0.38 [95% CI, 0.09-1.70]; P = .21 and
0.69 [95% CI, 0.32-1.53]; P = .36) and were more likely to be discharged home (adjusted odds
ratio, 1.93 [95% CI, 1.09-3.41]; P = .02).
CONCLUSIONS AND RELEVANCE The use of STEMO increases the percentage of patients
receiving thrombolysis within the golden hour. Golden hour thrombolysis entails no risk to
the patients safety and is associated with better short-term outcomes.
TRIAL REGISTRATION clinicaltrials.gov Identifier: NCT01382862
JAMA Neurol. 2015;72(1):25-30. doi:10.1001/jamaneurol.2014.3188
Published online November 17, 2014.
Author Affiliations: Department
of Neurology,
CharitUniversittsmedizin Berlin,
Berlin, Germany (Ebinger, Kunz,
Wendt, Rozanski, Winter,
Waldschmidt, Weber, Villringer,
Fiebach, Audebert); Center for Stroke
Research Berlin,
CharitUniversittsmedizin Berlin,
Berlin, Germany (Ebinger, Kunz,
Rozanski, Villringer, Fiebach,
Audebert).
Corresponding Author: Martin
Ebinger, MD, Department of
Neurology,
CharitUniversittsmedizin Berlin,
Charitplatz 1, 10117 Berlin, Germany
(martin.ebinger@charite.de).
25
Copyright 2014 American Medical Association. All rights reserved.
Downloaded From: http://archneur.jamanetwork.com/ by elfrida meryance on 03/06/2016
Research Original Investigation
Golden Hour Thrombolysis
ime to treatment with tissue plasminogen activator (tPA)
is crucial to outcomes among patients with acute ischemic stroke.1,2 Numerous attempts have been made to
reduce the time from symptom onset to treatment (OTT).3,4
However, many centers struggle to keep the time from arrival
at the hospital to initiation of tPA (door-to-needle time) shorter
than 60 minutes.5,6 When prehospital times are added to inhospital delays, an OTT within the first 60 minutes of symptom onset, termed the golden hour, seems out of reach for most
patients. In fact, most patients undergoing routine care for
stroke receive treatment rather late. In the Safe Implementation of ThrombolysisStroke Monitoring Study (SITS-MOST)
registry,7 10.6% of 6483 patients were treated within 90 minutes and only 1.4% within 60 minutes. The median OTT in the
SITSInternational Stroke Thrombolysis Register8 was 145 (interquartile range [IQR], 115-170) minutes. Structured approaches have been successful in increasing thrombolysis rates
and shortening door-to-needle times.9-11 Centers with greater
numbers of tPA treatments per year tend to have shorter doorto-needle times compared with smaller centers.5 However,
some of the centers with shortened door-to-needle times still
have long prehospital times.9,12
A forceful approach to shorten the OTT is prehospital thrombolysis in emergency vehicles equipped with a computed tomographic scanner and a point-of-care laboratory.13-15 A reduced
time from the emergency call to treatment after deployment of
such an ambulance compared with regular care was observed
in the Prehospital Acute Neurological Treatment and Optimization of Medical Care in Stroke (PHANTOM-S) study.15 We used
data from the PHANTOM-S study to evaluate the rate and effectiveness of golden hour thrombolysis.
Methods
The study was approved by the Charit Ethics Committee and
conducted in accordance with published protocol. Written informed consent was obtained from patients able to communicate and waived for those unable to provide consent, as described in detail previously.15
Methodologic details of the PHANTOM-S study have been
described previously.16,17 In brief, an ambulance, the stroke
emergency mobile unit (STEMO), was equipped with a computed tomographic scanner and point-of-care laboratory. The
unit was staffed with a neurologist trained in emergency medicine (including M.E., A.K., M.W., M.R., B.W., C.W., and J.W.), a
paramedic, and a radiology technician. A neuroradiologist was
on call to evaluate images acquired on board the STEMO via a
teleradiology connection. We evaluated the effects of the
STEMO implementation prospectively by comparing weeks
with and without STEMO availability. The STEMO was deployed when the dispatchers suspected an acute stroke during emergency calls. If STEMO was not available (during control weeks, while the unit was in operation, or during
maintenance), patients received conventional care.
For this post hoc analysis based on data from the
PHANTOM-S study, we used the same consecutive patients
and baseline variables as in the original study. 15 Stroke
26
severity at baseline was assessed according to the National
Institutes of Health Stroke Scale (NIHSS).18 In addition, we
calculated the proportion of patients treated in 1-hour intervals. The OTT intervals were dichotomized as 60 minutes or
less (the golden hour) or longer than 60 minutes. Only 1
STEMO was available within a catchment area of more than
1 million inhabitants. Therefore, the STEMO could not be
deployed for all suspected strokes during STEMO weeks
when the STEMO was occupied with another emergency. In
contrast to the original study,15 we did not compare STEMO
weeks with control weeks in the data presented here.
Instead we compared tPA treatments occurring after STEMO
deployment with tPA treatments during conventional care.
Conventional care included tPA treatments during control
weeks and tPA treatments during STEMO weeks without
STEMO deployment (Figure 1). In a second step, we compared stroke patients who received golden hour thrombolysis with stroke patients who received tPA more than 60 minu te s a f te r s y m p to m o n s e t , i n d e p e n d e nt o f S T E M O
deployment or conventional care. Patients with stroke mimics who received tPA were not included in this evaluation of
treatment effects.
We calculated unadjusted outcomes for 7- and 90-day mortality, secondary intracerebral hemorrhage, and discharge
home among patients with an OTT within 60 minutes compared with those with an OTT longer than 60 minutes. We then
performed analyses to achieve the adjusted probability of each
outcome.
With relatively few patients who experienced a secondary hemorrhage (n = 29) or died within 7 days (n = 24), we had
to restrict the adjustment to 2 variables and adjusted for age
(in decades) and stroke severity (NIHSS score per point). For
the outcomes of death within 90 days (n = 75) and discharge
home (n = 239), we adjusted for age (in decades), sex, atrial fibrillation, and NIHSS score categories according to the Third
International Stroke Trial (NIHSS scores, 0-5, 6-10, 11-15, 1620, and 21).19 We considered P < .05 to be a statistically significant difference.
Results
STEMO Deployment vs Conventional Care
All data of this post hoc analysis presented herein were recalculated on the basis of the PHANTOM-S data set. During the
21 months from May 1, 2011, through January 31, 2013, there
were 3213 emergency calls for suspected stroke during STEMO
weeks and 2969 during control weeks (Figure 1). Of the 1804
patients with STEMO deployment (44.1% male; mean [SD] age,
73.9 [15.0] years), 200 received tPA treatment. Of those, tPA infusion was started in 17 patients after hospital arrival.15 Of 4378
patients in conventional care (45.0% male; mean [SD] age, 74.2
[14.9] years), 330 were treated with tPA (110 of those in STEMO
weeks and 220 in control weeks). Overall, 200 of 614 patients
with ischemic stroke (32.6%) received thrombolysis when the
STEMO was deployed and 330 of 1497 (22.0%) received thrombolysis in conventional care (P < .001). The mean NIHSS score
was higher among patients with STEMO deployment com-
JAMA Neurology January 2015 Volume 72, Number 1
Copyright 2014 American Medical Association. All rights reserved.
Downloaded From: http://archneur.jamanetwork.com/ by elfrida meryance on 03/06/2016
jamaneurology.com
Golden Hour Thrombolysis
Original Investigation Research
Figure 1. Study Flowchart
6182 Patients with stroke dispatch activation
and in-hospital documentation
3213 Patients during STEMO weeks
1804 Patients with STEMO
deployment
2969 Patients during control weeks
4378 Patients with conventional care
1409 Patients without STEMO
deployment
614 Patients with ischemic stroke
1497 Patients with ischemic stroke
414 Excluded
8 MRI-based thrombolysis
405 No thrombolysis
1 Enrolled in other trial
1167 Excluded
15 MRI-based thrombolysis
1152 No thrombolysis
200 Received tPA
330 Received tPA
138 >60 min
Irrespective of dispatch activation during weeks when the stroke emergency
mobile unit (STEMO) was deployed or during control weeks, 78 patients
received thrombolysis with tissue plasminogen activator (tPA) within 60
minutes of symptom onset (the golden hour), whereas 451 patients received
pared with patients receiving conventional care (10.5 vs 9.1
[P = .02]). Median OTT was 24.5 minutes shorter after STEMO
deployment compared with conventional care (80.5 [IQR, 54126] vs 105.0 [IQR, 82-146] minutes; P < .01). In all ischemic
strokes, the rate of golden hour thrombolysis increased from
16 of 1497 patients (1.1%) during conventional care to 62 of 614
(10.1%) after STEMO deployment (Figure 2). Among all patients who received thrombolysis, the proportion of golden
hour thrombolysis was 6-fold higher after STEMO deployment (62 patients [31.0%] vs 16 [4.9%]; P < .01). Of all patients
who received golden hour thrombolysis, 66 (84.6%) received
tPA during a STEMO week and 12 (15.4%) during a control week.
16 60 mina
One patient with unknown time of thrombolysis initiation was excluded.
Figure 2. Thrombolysis Rates in 60-Minute Intervals
16
STEMO care
14
Conventional care
12
10
8
6
4
2
Golden Hour Thrombolysis vs Later Thrombolysis
Median OTT was 50.0 (IQR, 43-55) minutes in golden hour
thrombolysis vs 105.0 (IQR, 85-155) minutes in all other thrombolysis (P < .001). In patients who received golden hour thrombolysis, median NIHSS score was higher than that in patients
who received tPA more than 60 minutes after symptom onset
(12 [IQR, 5-18] vs 7 [IQR, 4-13]; P = .006) (additional baseline
characteristics are given in Table 1). In unadjusted univariate
analysis of the outcomes mortality within 7 and 90 days, discharge home, and hemorrhagic complications, we detected no
significant differences between golden hour thrombolysis and
later thrombolysis (Table 2). In adjusted analysis, patients with
golden hour thrombolysis had no higher risks for 7- or 90-day
mortality (adjusted odds ratios, 0.38 [95% CI, 0.09-1.70]; P = .21
and 0.69 [95% CI, 0.32-1.53]; P = .36) compared with patients
with longer OTT and were more likely to be discharged home
(adjusted odds ratio, 1.93 [95% CI, 1.09-3.41]; P = .02) (Table 3).
313 >60 min
treatment more than 60 minutes after the onset of symptoms. MRI indicates
magnetic resonance imaging.
Patients, %
62 60 min
0
0-60
61-120
121-180
181-240
241-270
Time From Symptom Onset to Thrombolysis, min
The major difference in proportions between the group treated after
deployment of the stroke emergency mobile unit (STEMO) and the group
treated with conventional care can be observed within the first 60 minutes of
symptom onset.
Discussion
Prehospital stroke treatment within the STEMO concept increased the number of tPA treatments within the golden hour
almost 10-fold. Golden hour thrombolysis was associated with
improved patient outcomes regarding the discharge destination from acute in-hospital care. We observed no increased risk
jamaneurology.com
JAMA Neurology January 2015 Volume 72, Number 1
Copyright 2014 American Medical Association. All rights reserved.
Downloaded From: http://archneur.jamanetwork.com/ by elfrida meryance on 03/06/2016
27
Research Original Investigation
Golden Hour Thrombolysis
Table 1. Baseline Characteristics of Patients Who Received Golden Hour Thrombolysis
Compared With Later Thrombolysis
Patients With Thrombolysis
OTT >60 min
(n = 451)
Characteristic
OTT 60 min
(n = 78)
P Valuea
Age, mean (SD), y
75.5 (13.0)
75.5 (11.9)
.65
Male sex, No. (%)
226 (50.1)
34 (43.6)
.29
Comorbidities, No. (%)
Atrial fibrillation
151 (33.5)
35 (44.9)
.052
Diabetes mellitus
119 (26.4)
18 (23.1)
.54
Stroke severity
NIHSS score at treatmentb
Mean
9.3
11.7
Median (IQR)
7 (4-13)
12 (5-18)
0-5
160 (36.0)
21 (26.9)
6-10
133 (30.0)
13 (16.7)
11-15
62 (14.0)
16 (20.5)
16-20
59 (13.3)
18 (23.1)
21
30 (6.8)
10 (12.8)
.006
NIHSS score according to IST-3,19 No. (%)b
.004c
Abbreviations: IQR, interquartile
range; IST-3, Third International
Stroke Trial; NIHSS, National
Institutes of Health Stroke Scale; OTT,
time from symptom onset to
treatment.
a
Categorial variables were compared
with the 2 test and continuous
variables with the Mann-Whitney
test.
Seven patients were missing from
the analysis.
Calculated using the linear trend
test.
One patient was missing from the
analysis.
Process indicators
Length of stay, d
Mean
9.0
8.9
Median (IQR)
7 (5-11)
7 (5-11)
.80
OTT, mind
Mean
123.8
Median (IQR)
48.6
105.0 (85-155)
50.0 (43-55)
<.001
Table 2. Unadjusted Clinical Outcomes After Thrombolysis
Patients With Thrombolysis, No. (%)
OTT >60 min
(n = 451)
OTT 60 min
(n = 78)
P Value
23 (5.1)
6 (7.7)
.35
200 (44.3)
39 (50.0)
.35
24 (5.3)
2 (2.6)
.30
198 (43.9)
32 (41.0)
.64
In-hospital
29 (6.4)
5 (6.4)
.99
22 (4.9)
2 (2.6)
.36
64 (14.3)
11 (14.3)
>.99
Outcome
Hemorrhagic complications
Discharge
Home
Nursing home
Referral to other department/hospital/rehabilitation institution
Death
Within 7 d
Within 90 db
for hemorrhagic complications or mortality in patients undergoing golden hour thrombolysis. Deployment of STEMO led
to a significant proportion of patients with extremely early
treatment, even in a setting with already short median doorto-needle times and OTT in the control group (36.0 [IQR, 2851] and 105.0 [IQR, 81-145] minutes, respectively). Our results
regarding safety and discharge status after golden hour thrombolysis are in line with previous analyses of the association of
improved outcomes with shorter OTT.1,2,20
Thrombolytic treatment within the first 60 minutes has
rarely been reported. Only 4 of 3670 patients with time to treatment within 1 hour were included in the randomized stroke
thrombolysis trials according to the last pooled data set.21 Nevertheless, the term golden hour has become used frequently
28
Abbreviation: OTT, time from
symptom onset to treatment.
a
One patient was missing from the
analysis.
Four patients were missing from the
analysis.
in acute stroke management.3,4 The rapid death of brain cells
after blockage of cerebral blood supply makes immediate treatment to dissolve or remove clots indispensable.
Starting treatment at the scene has become a realistic scenario. The high percentage of early treatments also raises hopes
for other potentially effective treatments, such as neuroprotective substances.
This study has limitations. The significance and generalizability of the results presented here are limited owing to
the nature of a post hoc analysis. These explorative results
need to be confirmed using a prospective approach. The
PHANTOM-S study was originally designed to detect a
reduced time from the emergency call to treatment and was
not powered to detect functional outcome differences. The
JAMA Neurology January 2015 Volume 72, Number 1
Copyright 2014 American Medical Association. All rights reserved.
Downloaded From: http://archneur.jamanetwork.com/ by elfrida meryance on 03/06/2016
jamaneurology.com
Golden Hour Thrombolysis
Original Investigation Research
Table 3. Adjusted Analyses of Clinical Outcomes
Outcome (No. of Events/No. of Patients)
Secondary Intracerebral
Hemorrhage
(29/522)a
Characteristic
Age (in decades)
OR (95% CI)
1.35 (0.51-3.56)
Discharge to Home
(239/522)b
P Value
.54
Mortality Within 7 d
(24/521)a
Mortality Within 90 d
(75/518)b
OR (95% CI)
P Value
OR (95% CI)
P
Value
OR (95% CI)
P Value
0.59 (0.50-0.71)
<.001
1.51 (1.01-2.27)
.045
2.51 (1.79-3.51)
<.001
Male sex
NSc
1.32 (0.88-1.98)
.18
NSc
1.43 (0.78-2.63)
.25
Atrial fibrillation
NSc
0.77 (0.49-1.20)
.24
NSc
0.95 (0.53-1.70)
.95
NIHSS score
0-5
1 [Reference]
6-10
0.73 (0.23-2.28)
.58
0.34 (0.21-0.56)
<.001
3.47 (0.69-17.55)
.13
2.73 (0.99-7.46)
11-15
1.89 (0.65-5.48)
.24
0.23 (0.12-0.42)
<.001
3.32 (0.54-20.49)
.20
5.68 (2.02-16.02)
.001
16-20
0.47 (0.10-2.32)
.35
0.15 (0.08-0.29)
<.001
7.96 (1.58-40.18)
.01
9.09 (3.31-24.90)
<.001
21
3.78 (1.25-11.43)
.018
0.09 (0.03-0.24)
<.001
16.95 (3.12-92.11)
.002
25.80 (8.62-77.22)
<.001
1.35 (0.52-3.49)
.54
1.93 (1.09-3.41)
.02
0.38 (0.09-1.70)
.21
0.69 (0.32-1.53)
.36
OTT 60 min
1 [Reference]
Abbreviations: NIHSS, National Institutes of Health Stroke Scale; NS, not
significant; OR, odds ratio; OTT, time from symptom onset to treatment.
a
1 [Reference]
ARTICLE INFORMATION
Accepted for Publication: September 4, 2014.
Published Online: November 17, 2014.
doi:10.1001/jamaneurol.2014.3188.
Author Contributions: Drs Ebinger and Audebert
had full access to all the data in the study and take
responsibility for the integrity of the data and the
accuracy of the data analysis.
Study concept and design: Ebinger, Audebert.
Acquisition, analysis, or interpretation of data: All
authors.
Drafting of the manuscript: Ebinger, Audebert.
Critical revision of the manuscript for important
intellectual content: Kunz, Wendt, Rozanski, Winter,
Waldschmidt, Weber, Villringer, Fiebach, Audebert.
Statistical analysis: Audebert.
.053
Adjusted for age, sex, atrial fibrillation, and NIHSS categories.
Indicates not significant in univariable analysis, therefore not included in
multivariable logistic regression.
Adjusted for age and NIHSS categories.
use of discharge destination from acute in-hospital care can
only be interpreted as a surrogate variable. The higher frequency of patients discharged home was only shown for patients treated within the golden hour and not for the entire cohort of patients who received STEMO care. Randomization was
not performed at the patient level, but weeks were allocated
to usual stroke care or additional STEMO availability. Finally,
bias of spontaneous recovery remains a possibility when comparing extremely early vs late thrombolysis.
The question of generalizability of the prehospital thrombolysis concept warrants further studies. Not all countries are
accustomed to emergency physicians in the field, which may
be required for adaptation of the STEMO concept. The OTT
found in our study after STEMO deployment (median OTT, 80.5
minutes) and during conventional care (median OTT, 105.0
minutes) were much shorter than in published stroke thrombolysis registries (median OTTs, 144 minutes in Saver et al2 and
140 minutes in Wahlgren et al7) or even in best-practice hospital systems (median OTT, 119 minutes for Meretoja et al9).
Apart from a selection bias by restriction to patients with ambulance care, this difference may be explained at least in part
1 [Reference]
by a well-established metropolitan stroke care system with
trained dispatchers and paramedics, short distances to stroke
units, and rather optimized in-hospital procedures. During the
study period, the dispatchers identified patients with typical
stroke symptoms during the emergency call and notified the
emergency medical services, which may have raised awareness of the entire rescue chain.
Conclusions
The concept of prehospital thrombolysis is still relatively new,
and experience is limited to few groups. Further improvements in time reduction may be expected with growing
routine.
After analyzing data from the Get With the Guidelines
Stroke Program, Saver and colleagues2 concluded that every
effort should be made to accelerate thrombolytic treatment in
patients with stroke. Our post hoc analysis supports this timeis-brain concept. Golden hour thrombolysis was associated
with better short-term outcomes.
Obtained funding: Audebert.
Administrative, technical, or material support:
Ebinger, Kunz, Wendt, Waldschmidt, Weber,
Villringer.
Study supervision: Ebinger, Fiebach, Audebert.
Conflict of Interest Disclosures: Dr Audebert
received speaker honoraria from Boehringer
Ingelheim, the manufacturer of alteplase (not
involved in this trial), and speaker and consultancy
honoraria from Lundbeck A/S, which has conducted
a recent acute stroke thrombolysis trial. No other
disclosures were reported.
Funding/Support: The PHANTOM-S study was
supported by the Zukunftsfonds Berlin and the
Technology Foundation Berlin with cofinancing by
the European Regional Development Fund.
jamaneurology.com
Role of the Funder/Sponsor: The funding sources
had no role in the design and conduct of the study;
collection, management, analysis, and
interpretation of the data; preparation, review, or
approval of the manuscript; and decision to submit
the manuscript for publication.
Additional Contributions: Ulrike Grittner, PhD,
Center for Stroke Research Berlin,
CharitUniversittsmedizin Berlin, provided
statistical advice. He received no compensation for
this contribution.
REFERENCES
1. Lees KR, Bluhmki E, von Kummer R, et al; ECASS,
ATLANTIS, NINDS and EPITHET rt-PA Study Group.
Time to treatment with intravenous alteplase and
JAMA Neurology January 2015 Volume 72, Number 1
Copyright 2014 American Medical Association. All rights reserved.
Downloaded From: http://archneur.jamanetwork.com/ by elfrida meryance on 03/06/2016
29
Research Original Investigation
Golden Hour Thrombolysis
outcome in stroke: an updated pooled analysis of
ECASS, ATLANTIS, NINDS, and EPITHET trials. Lancet.
2010;375(9727):1695-1703.
2. Saver JL, Fonarow GC, Smith EE, et al. Time to
treatment with intravenous tissue plasminogen
activator and outcome from acute ischemic stroke.
JAMA. 2013;309(23):2480-2488.
3. Fassbender K, Balucani C, Walter S, Levine SR,
Haass A, Grotta J. Streamlining of prehospital
stroke management: the golden hour. Lancet Neurol.
2013;12(6):585-596.
4. Audebert HJ, Saver JL, Starkman S, Lees KR,
Endres M. Prehospital stroke care: new prospects
for treatment and clinical research. Neurology.
2013;81(5):501-508.
5. Fonarow GC, Smith EE, Saver JL, et al. Timeliness
of tissue-type plasminogen activator therapy in
acute ischemic stroke: patient characteristics,
hospital factors, and outcomes associated with
door-to-needle times within 60 minutes. Circulation.
2011;123(7):750-758.
6. Fonarow GC, Zhao X, Smith EE, et al.
Door-to-needle times for tissue plasminogen
activator administration and clinical outcomes in
acute ischemic stroke before and after a quality
improvement initiative. JAMA. 2014;311(16):16321640.
7. Wahlgren N, Ahmed N, Dvalos A, et al;
SITS-MOST investigators. Thrombolysis with
alteplase for acute ischaemic stroke in the Safe
Implementation of Thrombolysis in
StrokeMonitoring Study (SITS-MOST): an
observational study. Lancet. 2007;369(9558):275282.
30
8. Lorenzano S, Ahmed N, Tatlisumak T, et al; SITS
Investigators. Within-day and weekly variations of
thrombolysis in acute ischemic stroke: results from
Safe Implementation of Treatments in
StrokeInternational Stroke Thrombolysis Register.
Stroke. 2014;45(1):176-184.
9. Meretoja A, Strbian D, Mustanoja S, Tatlisumak
T, Lindsberg PJ, Kaste M. Reducing in-hospital delay
to 20 minutes in stroke thrombolysis. Neurology.
2012;79(4):306-313.
10. Khrmann M, Schellinger PD, Breuer L, et al.
Avoiding in hospital delays and eliminating the
three-hour effect in thrombolysis for stroke. Int J
Stroke. 2011;6(6):493-497.
11. Walter S, Kostopoulos P, Haass A, et al.
Point-of-care laboratory halves
door-to-therapy-decision time in acute stroke. Ann
Neurol. 2011;69(3):581-586.
12. Meretoja A, Weir L, Ugalde M, et al. Helsinki
model cut stroke thrombolysis delays to 25 minutes
in Melbourne in only 4 months. Neurology. 2013;81
(12):1071-1076.
13. Walter S, Kostopoulos P, Haass A, et al.
Diagnosis and treatment of patients with stroke in a
mobile stroke unit versus in hospital: a randomised
controlled trial. Lancet Neurol. 2012;11(5):397-404.
14. Weber JE, Ebinger M, Rozanski M, et al;
STEMO-Consortium. Prehospital thrombolysis in
acute stroke: results of the PHANTOM-S pilot study.
Neurology. 2013;80(2):163-168.
thrombolysis on time to thrombolysis in acute
ischemic stroke: a randomized clinical trial. JAMA.
2014;311(16):1622-1631.
16. Ebinger M, Rozanski M, Waldschmidt C, et al;
STEMO-Consortium. PHANTOM-S: the Prehospital
Acute Neurological Therapy and Optimization of
Medical Care in Stroke Patients study. Int J Stroke.
2012;7(4):348-353.
17. Ebinger M, Lindenlaub S, Kunz A, et al.
Prehospital thrombolysis: a manual from Berlin.
J Vis Exp. 2013;(81):e50534. doi:10.3791/50534.
18. Brott T, Adams HP Jr, Olinger CP, et al.
Measurements of acute cerebral infarction:
a clinical examination scale. Stroke. 1989;20(7):
864-870.
19. Sandercock P, Wardlaw JM, Lindley RI, et al;
IST-3 Collaborative Group. The benefits and harms
of intravenous thrombolysis with recombinant
tissue plasminogen activator within 6 h of acute
ischaemic stroke (the Third International Stroke
Trial [IST-3]): a randomised controlled trial
[published correction appears in Lancet.
2012;380(9843):730]. Lancet. 2012;379(9834):
2352-2363.
20. Meretoja A, Keshtkaran M, Saver JL, et al.
Stroke thrombolysis: save a minute, save a day.
Stroke. 2014;45(4):1053-1058.
21. Grotta JC. tPA for stroke: important progress in
achieving faster treatment. JAMA. 2014;311(16):
1615-1617.
15. Ebinger M, Winter B, Wendt M, et al; STEMO
Consortium. Effect of the use of ambulance-based
JAMA Neurology January 2015 Volume 72, Number 1
Copyright 2014 American Medical Association. All rights reserved.
Downloaded From: http://archneur.jamanetwork.com/ by elfrida meryance on 03/06/2016
jamaneurology.com
Vous aimerez peut-être aussi
- Nutricia Advertorial 3Document1 pageNutricia Advertorial 3Nurul Falah KalokoPas encore d'évaluation
- Pakistan Armed Forces Medical Journal: Comparison of Median and Paramedian Techniques of Spinal AnaesthesiaDocument5 pagesPakistan Armed Forces Medical Journal: Comparison of Median and Paramedian Techniques of Spinal AnaesthesiaNurul Falah KalokoPas encore d'évaluation
- MR Sunday MorningDocument10 pagesMR Sunday MorningNurul Falah KalokoPas encore d'évaluation
- Genetic Risk, Adherence To A Healthy Lifestyle, and Coronary DiseaseDocument10 pagesGenetic Risk, Adherence To A Healthy Lifestyle, and Coronary DiseaseNurul Falah KalokoPas encore d'évaluation
- Inverted Papilloma of Middle Ear and Mastoid: A Rare EntityDocument3 pagesInverted Papilloma of Middle Ear and Mastoid: A Rare EntityNurul Falah KalokoPas encore d'évaluation
- Relationship Between Surface Area and Volume of The Mastoid Air Cell System in Adult HumansDocument8 pagesRelationship Between Surface Area and Volume of The Mastoid Air Cell System in Adult HumansNurul Falah KalokoPas encore d'évaluation
- Eustachian Tube Diameter: Is It Associated With Chronic Otitis Media Development?Document7 pagesEustachian Tube Diameter: Is It Associated With Chronic Otitis Media Development?Nurul Falah KalokoPas encore d'évaluation
- Central Venous Lines (CVP) : Looking For More Health Information?Document6 pagesCentral Venous Lines (CVP) : Looking For More Health Information?Nurul Falah KalokoPas encore d'évaluation
- Complementary and Alternative Medicine Use in England: Results From A National SurveyDocument7 pagesComplementary and Alternative Medicine Use in England: Results From A National SurveyNurul Falah KalokoPas encore d'évaluation
- Fransiska Sihite - Entry Level Resume - 01Document1 pageFransiska Sihite - Entry Level Resume - 01Nurul Falah KalokoPas encore d'évaluation
- B 2 BDocument4 pagesB 2 BNurul Falah KalokoPas encore d'évaluation
- Critical Care in The Emergency Department: Monitoring The Critically Ill PatientDocument4 pagesCritical Care in The Emergency Department: Monitoring The Critically Ill PatientNurul Falah KalokoPas encore d'évaluation
- Cough: Presentator: Herbet Supervisor: Dr. Noni Soeroso, SP.P (K)Document31 pagesCough: Presentator: Herbet Supervisor: Dr. Noni Soeroso, SP.P (K)Nurul Falah KalokoPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Diazepam Drug StudyDocument1 pageDiazepam Drug StudyAndee Salegon100% (3)
- See - The.messages - Within.You.2013 - DR - Harvey.Bigelsen PDFDocument38 pagesSee - The.messages - Within.You.2013 - DR - Harvey.Bigelsen PDFSam100% (2)
- Brain Cancer ScriptDocument2 pagesBrain Cancer Scriptapi-251981413Pas encore d'évaluation
- US - Inggris 2017Document5 pagesUS - Inggris 2017SmabaitulhikmahPas encore d'évaluation
- Stress Management Strategies Adopted by Teachers in Public Primary Schools in Obio/Akpor Local Government Area of Rivers State, Nigeria.Document94 pagesStress Management Strategies Adopted by Teachers in Public Primary Schools in Obio/Akpor Local Government Area of Rivers State, Nigeria.sorbariPas encore d'évaluation
- Gen EdDocument14 pagesGen EdMark Julius G AlmadinPas encore d'évaluation
- Subcutaneous Mycoses: Presenter: DR Pranay Reddy Moderator: DR Tonita MNDocument81 pagesSubcutaneous Mycoses: Presenter: DR Pranay Reddy Moderator: DR Tonita MNSandipPas encore d'évaluation
- Deeper Trial - Asco 2021Document26 pagesDeeper Trial - Asco 2021Vuong Dinh Thy HaoPas encore d'évaluation
- 110 ch3Document3 pages110 ch3Hitesh KhuranaPas encore d'évaluation
- J Potratz ResumeDocument3 pagesJ Potratz Resumeapi-216040679Pas encore d'évaluation
- Covid-19 Expose (Unmask)Document2 pagesCovid-19 Expose (Unmask)Eduardo CasesPas encore d'évaluation
- Psychoeducation As Evidence-Based Practice - Considerations For Practice, Research, and Policy - Lukens & McFarlane (2003)Document21 pagesPsychoeducation As Evidence-Based Practice - Considerations For Practice, Research, and Policy - Lukens & McFarlane (2003)Eduardo Aguirre DávilaPas encore d'évaluation
- Documents 34-51Document3 pagesDocuments 34-51api-575141270Pas encore d'évaluation
- Cerebral PalsyDocument21 pagesCerebral PalsyEMily AbastaPas encore d'évaluation
- Agc332 Lecture 10-Wheat DiseasesDocument33 pagesAgc332 Lecture 10-Wheat DiseasesSolomon MbewePas encore d'évaluation
- Breast Cancer Staging SystemDocument4 pagesBreast Cancer Staging SystemGabriella PatriciaPas encore d'évaluation
- An Introduction To Volunteering at Camphill DevonDocument3 pagesAn Introduction To Volunteering at Camphill DevonjohnyPas encore d'évaluation
- Ivermectin CochraneDocument159 pagesIvermectin CochraneWan Razin Wan HassanPas encore d'évaluation
- Block 4Document106 pagesBlock 4Dr. Megha RichhariyaPas encore d'évaluation
- Devil You Know PDFDocument269 pagesDevil You Know PDFElissaPas encore d'évaluation
- Adhesive CapsulitisDocument6 pagesAdhesive CapsulitisEllan Giulianno FerreiraPas encore d'évaluation
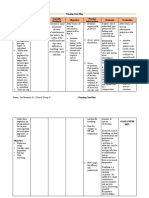
- Nursing Care PlanDocument13 pagesNursing Care PlanJan DamesPas encore d'évaluation
- Mental Disorder Due To AlcoholDocument18 pagesMental Disorder Due To AlcoholAnonymous Oj5JCpO5xPas encore d'évaluation
- Bad Romance A Crip Feminist Critique ofDocument17 pagesBad Romance A Crip Feminist Critique ofTylerescoPas encore d'évaluation
- Pereneal CareDocument2 pagesPereneal CareindumathiPas encore d'évaluation
- Dorothea Orem: Self-Care TheoryDocument16 pagesDorothea Orem: Self-Care TheoryHazel LezahPas encore d'évaluation
- Group Assignment Population EconomicsDocument7 pagesGroup Assignment Population EconomicsSayed Abdullah Shah SadaatPas encore d'évaluation
- Raw Milk FactsDocument9 pagesRaw Milk FactsRon Loewenstein100% (2)
- Annotated Bibliography - Research ProjectDocument3 pagesAnnotated Bibliography - Research Projectapi-237847760Pas encore d'évaluation
- Varicose Vein and Its Homeopathic Cure - DR Bashir Mahmud ElliasDocument8 pagesVaricose Vein and Its Homeopathic Cure - DR Bashir Mahmud ElliasBashir Mahmud Ellias100% (2)