Académique Documents
Professionnel Documents
Culture Documents
Disturbed Sensory Perception
Transféré par
Calimlim Kim100%(1)100% ont trouvé ce document utile (1 vote)
4K vues3 pagesDisturbed Sensory Perception
Copyright
© © All Rights Reserved
Formats disponibles
DOCX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDisturbed Sensory Perception
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
100%(1)100% ont trouvé ce document utile (1 vote)
4K vues3 pagesDisturbed Sensory Perception
Transféré par
Calimlim KimDisturbed Sensory Perception
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 3
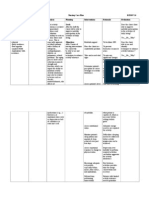
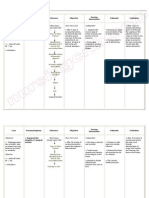
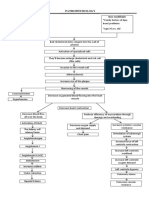
Disturbed Sensory Perception
Disturbed Sensory Perception: Change in the amount or patterning of incoming stimuli
accompanied by a diminished, exaggerated, distorted, or impaired response to such stimuli.
Nursing Diagnosis
Disturbed Sensory Perception
May be related to
Altered sensory reception, transmission, integration (neurological trauma or
deficit)
Psychological stress (narrowed perceptual fields caused by anxiety)
Possibly evidenced by
Disorientation to time, place, person
Change in behavior pattern/usual response to stimuli; exaggerated emotional
responses
Poor concentration, altered thought processes/bizarre thinking
Reported/measured change in sensory acuity: hypoparesthesia; altered sense of
taste/smell
Inability to tell position of body parts (proprioception)
Inability to recognize/attach meaning to objects (visual agnosia)
Altered communication patterns
Motor incoordination
Desired Outcomes
Regain/maintain usual level of consciousness and perceptual functioning.
Acknowledge changes in ability and presence of residual involvement.
Demonstrate behaviors to compensate for/overcome deficits.
Nursing Interventions
Review pathology of individual condition.
Rationale
Awareness on the type and areas of
involvement aid in assessing specific deficit
and planning of care.
Nursing Interventions
Rationale
Observe behavioral responses: crying,
inappropriate affect, agitation, hostility,
agitation, hallucination.
Individual responses are variable, but
commonalities such as emotional lability,
lowered frustration threshold, apathy, and
impulsiveness may complicate care.
Establish and maintain communication with
the patient. Set up a simple method of
communicating basic needs. Remember to
phrase your questions so hell be able to
answer using this system. Repeat yourself
quietly and calmly and use gestures when
necessary to help in understanding.
Note: even an unresponsive patient may be
able to hear, so dont say anything in his
presence you wouldnt want him to hear and
remember.
Eliminate extraneous noise and stimuli as
necessary.
Speak in calm, comforting, quiet voice, using
short sentences. Maintain eye contact.
Ascertain patients perceptions. Reorient
patient frequently to environment, staff,
procedures.
Evaluate for visual deficits. Note loss of visual
field, changes in depth perception (horizontal
and/or vertical planes), presence of diplopia
(double vision).
Approach patient from visually intact side.
Leave light on; position objects to take
advantage of intact visual fields. Patch affected
eye if indicated.
Assess sensory awareness: dull from sharp, hot
from cold, position of body parts, joint sense.
Stimulate sense of touch. Give patient objects
to touch, and hold. Have patient practice
touching walls boundaries.
Protect from temperature extremes; assess
environment for hazards. Recommend testing
warm water with unaffected hand.
Reduces anxiety and exaggerated emotional
responses and confusion associated with
sensory overload.
Patient may have limited attention span or
problems with comprehension. These measures
can help patient attend to communication.
Assists patient to identify inconsistencies in
reception and integration of stimuli and may
reduce perceptual distortion of reality.
Presence of visual disorders can negatively
affect patients ability to perceive environment
and relearn motor skills and increases risk of
accident and injury.
Helps the patient to recognize the presence of
persons or objects and may help with depth
perception problems. This also prevents patient
from being startled. Patching the eye may
decrease sensory confusion of double vision.
Diminished sensory awareness and impairment
of kinesthetic sense negatively affects
balance and positioning and appropriateness of
movement, which interferes with ambulation,
increasing risk of trauma.
Aids in retraining sensory pathways to
integrate reception and interpretation of
stimuli. Helps patient orient self spatially and
strengthens use of affected side.
Promotes patient safety, reducing risk of injury.
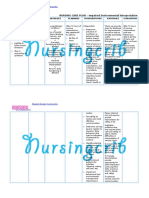
Nursing Interventions
Rationale
Note inattention to body parts, segments of
environment, lack of recognition of familiar
objects/persons.
Agnosia, the loss of comprehension of
auditory, visual, or other sensations, may lead
result to unilateral neglect, inability to
recognize environmental cues, considerable
self-care deficits, and disorientation or bizarre
behavior.
Encourage patient to watch feet when
appropriate and consciously position body
parts. Make patient aware of all neglected body
parts: sensory stimulation to affected side,
exercises that bring affected side across
midline, reminding person to dress/care for
affected (blind) side.
Use of visual and tactile stimuli assists in
reintegration of affected side and allows
patient to experience forgotten sensations of
normal movement patterns.
Vous aimerez peut-être aussi
- NCP-Disturbed Sensory PerceptionDocument3 pagesNCP-Disturbed Sensory PerceptionAlexis Abigail de Leon29% (7)
- Nursing Care PlanDocument5 pagesNursing Care PlanJohn Paul Delos Santos100% (1)
- NCP Visual SensoryDocument2 pagesNCP Visual SensoryEugene UCPas encore d'évaluation
- NCP - GlaucomaDocument1 pageNCP - GlaucomaKath CuevasPas encore d'évaluation
- Disturbed Sensory PerceptionDocument3 pagesDisturbed Sensory PerceptionJames Lozano83% (6)
- Self Care DeficitDocument3 pagesSelf Care DeficitAlexa Roque100% (2)
- NCPDocument8 pagesNCPJayrald RosalesPas encore d'évaluation
- NCP DisturbedThoughtProcessesDocument1 pageNCP DisturbedThoughtProcessesJoan KarlaPas encore d'évaluation
- NCP Cataract SurgeryDocument5 pagesNCP Cataract SurgeryKristaJaneCelmarBagcatPas encore d'évaluation
- Disturbed Sensory PerceptionDocument3 pagesDisturbed Sensory PerceptionJoenna GaloloPas encore d'évaluation
- NCP For Disturbed Sensory PerceptionDocument9 pagesNCP For Disturbed Sensory PerceptionRYAN SAPLADPas encore d'évaluation
- HoplessnessDocument16 pagesHoplessnessHamza IshtiaqPas encore d'évaluation
- NXCP Disturbed Sensory Perception3Document2 pagesNXCP Disturbed Sensory Perception3marielle_dellaPas encore d'évaluation
- NCP Icu-CcuDocument6 pagesNCP Icu-CcuJohn CenasPas encore d'évaluation
- Impaired Verbal CommunicationDocument6 pagesImpaired Verbal CommunicationLaura Sansonetti100% (1)
- NCP Chronic ConfusionDocument4 pagesNCP Chronic ConfusionLyka DianaPas encore d'évaluation
- Nursing Care PlanDocument2 pagesNursing Care PlanJewelyn Bronda100% (2)
- NCPDocument3 pagesNCPeun kyung shinPas encore d'évaluation
- NCP Disturbed Sensory PerceptionDocument3 pagesNCP Disturbed Sensory PerceptionEdmarkmoises ValdezPas encore d'évaluation
- Disturbed Sensory PerceptionDocument2 pagesDisturbed Sensory Perceptionsuper ahga-once0% (1)
- Assessment Diagnosis Planning Implementation Rationale EvaluationDocument3 pagesAssessment Diagnosis Planning Implementation Rationale Evaluationria_soriano_2Pas encore d'évaluation
- As Needed.: Environmental Stimuli 6Document4 pagesAs Needed.: Environmental Stimuli 6Nicole GumolonPas encore d'évaluation
- Disturbed Thought ProcessDocument3 pagesDisturbed Thought ProcessAira AlaroPas encore d'évaluation
- AudiDocument3 pagesAudiFlorygene Kris Disagon0% (1)
- Word Ncp.......... TetanusDocument6 pagesWord Ncp.......... TetanusaianrPas encore d'évaluation
- Nursing Care Plan: Cues Nursing Diagnosis Definitio N Goal and Objectives Nursing Interventions Rationale Evaluati ONDocument5 pagesNursing Care Plan: Cues Nursing Diagnosis Definitio N Goal and Objectives Nursing Interventions Rationale Evaluati ONOphelia Ross Omaña TutanesPas encore d'évaluation
- Nursing Diagnosis: AdvertisementsDocument7 pagesNursing Diagnosis: AdvertisementsJamea TumbagaPas encore d'évaluation
- Orientation PhaseDocument3 pagesOrientation Phasekimchi girlPas encore d'évaluation
- Activity Intolerance CholecystectomyDocument2 pagesActivity Intolerance CholecystectomyPrincess Danica Purcia100% (3)
- NCP IntraDocument1 pageNCP IntraCharlene Valerie Alviola0% (1)
- NCP CamsDocument3 pagesNCP CamsNica Cielo B. LibunaoPas encore d'évaluation
- NCPDocument4 pagesNCPaviesoreal100% (1)
- Nursing Care Plan: General: Goals Met GenreralDocument3 pagesNursing Care Plan: General: Goals Met GenreralRomzy BasañesPas encore d'évaluation
- NCP Disturbed Visual Sensory Perception Related To Chemotherapy Evidenced by Visual DistortionDocument2 pagesNCP Disturbed Visual Sensory Perception Related To Chemotherapy Evidenced by Visual DistortionCamille Grace100% (2)
- Ncp-Impaired S.i.-NavidasDocument4 pagesNcp-Impaired S.i.-NavidasFran LanPas encore d'évaluation
- Nursing Care Plan: Phinma University of IloiloDocument4 pagesNursing Care Plan: Phinma University of IloiloLestly Mae Tedios MongayaPas encore d'évaluation
- Clinical Example:: What Additional Assessments Would The Nurse Want To Make To Plan Care For This Client?Document2 pagesClinical Example:: What Additional Assessments Would The Nurse Want To Make To Plan Care For This Client?Kim Kristine D. GuillenPas encore d'évaluation
- Hopelessness NCPDocument5 pagesHopelessness NCPMatty JolbitadoPas encore d'évaluation
- Disturbed Sensory Perception (Hearing)Document2 pagesDisturbed Sensory Perception (Hearing)Diane Rey60% (5)
- Nursing Care Plan For Impaired Environmental Interpretaion NCPDocument4 pagesNursing Care Plan For Impaired Environmental Interpretaion NCPderic100% (2)
- Risk For InjuryDocument4 pagesRisk For InjuryJanina Patricia BuddlePas encore d'évaluation
- Nursing Diagnosis 3Document2 pagesNursing Diagnosis 3Mark Cau Meran100% (2)
- NCP-Impaired Physical Mobility - E+ ImbalanceDocument3 pagesNCP-Impaired Physical Mobility - E+ ImbalanceRene John FranciscoPas encore d'évaluation
- NCP Violence - OtherDocument2 pagesNCP Violence - OtherRosean Venus SilangPas encore d'évaluation
- NURSING CARE PLAN Eyes&earsDocument4 pagesNURSING CARE PLAN Eyes&earsWiljohn de la Cruz100% (3)
- Assessment Nursing Diagnosis Planning Implemantation Rationale EvaluationDocument2 pagesAssessment Nursing Diagnosis Planning Implemantation Rationale EvaluationChloie Marie Rosalejos100% (1)
- NCPDocument7 pagesNCPChris Denver BancalePas encore d'évaluation
- Psychiatric Reflection JournalDocument2 pagesPsychiatric Reflection JournalKatherine TanPas encore d'évaluation
- Schizophrenia Nursing ManagementDocument56 pagesSchizophrenia Nursing ManagementHumphreyPas encore d'évaluation
- Nursing Care Plan Impaire Physical MobilityDocument2 pagesNursing Care Plan Impaire Physical Mobilityderic90% (10)
- Compartment Syndrome NCP (PAIN)Document2 pagesCompartment Syndrome NCP (PAIN)eunica16Pas encore d'évaluation
- NCP Impaired Physical MobilityDocument1 pageNCP Impaired Physical MobilityCharmaine SolimanPas encore d'évaluation
- Nursing Care Plan For CamoxDocument1 pageNursing Care Plan For CamoxRolena Johnette B. PiñeroPas encore d'évaluation
- NCP Epidural HemDocument32 pagesNCP Epidural HemKatrina PoncePas encore d'évaluation
- Nursing Care PlanDocument6 pagesNursing Care PlanNeza AgdalesPas encore d'évaluation
- Sensory DeprivationDocument25 pagesSensory DeprivationPrabhjot Singh67% (3)
- Advance Nursing Practice Presentation On Sensory DeprivationDocument22 pagesAdvance Nursing Practice Presentation On Sensory DeprivationLaveena Aswale67% (3)
- Nursing Care Plans of A Patient With StrokeDocument15 pagesNursing Care Plans of A Patient With StrokeJoy JarinPas encore d'évaluation
- Mental Status ExamDocument44 pagesMental Status ExamHershey Cordero Briones100% (1)
- Nursing Care PlanDocument25 pagesNursing Care PlanIndah MardianiPas encore d'évaluation
- Why Study A Masters in Surgical Nursing?Document5 pagesWhy Study A Masters in Surgical Nursing?Calimlim KimPas encore d'évaluation
- Path o Physiology GastrroDocument1 pagePath o Physiology GastrroCalimlim KimPas encore d'évaluation
- Introduction Brain Abcess Nursing ManagementDocument2 pagesIntroduction Brain Abcess Nursing ManagementCalimlim KimPas encore d'évaluation
- Sal But AmolDocument2 pagesSal But AmolCalimlim KimPas encore d'évaluation
- NCM 106Document13 pagesNCM 106Calimlim KimPas encore d'évaluation
- Pathophysiology CHF MineDocument2 pagesPathophysiology CHF MineCalimlim KimPas encore d'évaluation
- Prelim Bioethics Handouts.Document13 pagesPrelim Bioethics Handouts.Calimlim KimPas encore d'évaluation
- Nursing Care Plan: Cues Nursing Diagnosis Analysis Goal and Objectives Interventions Rationale EvaluationDocument3 pagesNursing Care Plan: Cues Nursing Diagnosis Analysis Goal and Objectives Interventions Rationale EvaluationCalimlim KimPas encore d'évaluation
- Philippine Anti CyberbullyingDocument4 pagesPhilippine Anti CyberbullyingCalimlim Kim100% (2)
- Red Cross 143 Program 3Document23 pagesRed Cross 143 Program 3Calimlim KimPas encore d'évaluation
- Working Phase (Psych Nursing) Progress Report Process ReportingDocument5 pagesWorking Phase (Psych Nursing) Progress Report Process ReportingCalimlim KimPas encore d'évaluation
- Think Before You Click. The Effects of Social Media in The Nursing WorkplaceDocument42 pagesThink Before You Click. The Effects of Social Media in The Nursing WorkplaceCalimlim Kim100% (1)
- TracheostomyDocument17 pagesTracheostomyCalimlim KimPas encore d'évaluation
- Impaired Verbal CommunicationDocument3 pagesImpaired Verbal CommunicationCalimlim KimPas encore d'évaluation
- FINAL Discharge-PlanningDocument3 pagesFINAL Discharge-PlanningCalimlim KimPas encore d'évaluation
- Case Slip DRDocument4 pagesCase Slip DRCalimlim KimPas encore d'évaluation
- Dumping Syndrome 508Document8 pagesDumping Syndrome 508Calimlim KimPas encore d'évaluation
- Self Care DeficitDocument2 pagesSelf Care DeficitCalimlim KimPas encore d'évaluation
- Deficient KnowledgeDocument3 pagesDeficient KnowledgeCalimlim KimPas encore d'évaluation
- Risk For Impaired SwallowingDocument3 pagesRisk For Impaired SwallowingCalimlim Kim100% (1)
- Ineffective CopingDocument3 pagesIneffective CopingCalimlim Kim100% (2)
- Impaired Physical MobilityDocument3 pagesImpaired Physical MobilityCalimlim Kim100% (1)
- Discharge PlanningfinalDocument2 pagesDischarge PlanningfinalCalimlim KimPas encore d'évaluation
- Surgeons Perform WorldDocument4 pagesSurgeons Perform WorldCalimlim KimPas encore d'évaluation
- Drug StudyDocument19 pagesDrug StudyCalimlim KimPas encore d'évaluation
- Nutrition For Late Preterm Babies What Should We Know.Document25 pagesNutrition For Late Preterm Babies What Should We Know.IKA UNAIRPas encore d'évaluation
- LESSON 10. Identifying Different Random Sampling 1Document20 pagesLESSON 10. Identifying Different Random Sampling 1Ian Lorenzo ReyesPas encore d'évaluation
- Journal of Management Science & Engineering Research - Vol.4, Iss.1 March 2021Document45 pagesJournal of Management Science & Engineering Research - Vol.4, Iss.1 March 2021Bilingual PublishingPas encore d'évaluation
- New Mexico MPJE Study Guide (Master Exam)Document30 pagesNew Mexico MPJE Study Guide (Master Exam)Chinhui Dang100% (12)
- NCP Rheumatoid ArthritisDocument3 pagesNCP Rheumatoid ArthritisJanieross Lamboso100% (1)
- Unit 7 Activity 2Document2 pagesUnit 7 Activity 2Jeremiah Paul UretaPas encore d'évaluation
- QVASDocument1 pageQVASAnjaswati Farida AdyanaPas encore d'évaluation
- Total Lead Content in Synthetic Turf Fibers: Standard Specification ForDocument2 pagesTotal Lead Content in Synthetic Turf Fibers: Standard Specification ForAhmad Zubair RasulyPas encore d'évaluation
- Personal Development Unit 1: Self-Development Self-ConceptDocument3 pagesPersonal Development Unit 1: Self-Development Self-ConceptEL FuentesPas encore d'évaluation
- Republic of The Philippines Department of Education: Annual Accomplishment Report Calendar Year 2019Document4 pagesRepublic of The Philippines Department of Education: Annual Accomplishment Report Calendar Year 2019sheareign dainchylles gamayanPas encore d'évaluation
- Heart Shape GuideDocument50 pagesHeart Shape GuideMaya JacksonPas encore d'évaluation
- Ball Mastery ProgramDocument13 pagesBall Mastery Programhz4s8g26trPas encore d'évaluation
- Human Papillomavirus InfectionDocument78 pagesHuman Papillomavirus InfectionJoaquín PeñaPas encore d'évaluation
- Yanamoffbeat - SalherDocument16 pagesYanamoffbeat - SalherAnaghaPas encore d'évaluation
- Jebsen Application FormDocument3 pagesJebsen Application FormCharlemaigne Josef DolorielPas encore d'évaluation
- Test Bank For Microbiology With Diseases by Body System 5th Edition by BaumanDocument36 pagesTest Bank For Microbiology With Diseases by Body System 5th Edition by Baumanquinazolmadraguevlvvsh100% (39)
- Journal ReflectionDocument2 pagesJournal ReflectionRuthchell CiriacoPas encore d'évaluation
- التاريخ المرضي PDFDocument2 pagesالتاريخ المرضي PDFاللهم أصلح أمريPas encore d'évaluation
- WFP Shelf Life Study Protocol - Processed Food Products: Food Safety and Quality Assurance UnitDocument3 pagesWFP Shelf Life Study Protocol - Processed Food Products: Food Safety and Quality Assurance UnitĐăng LưuPas encore d'évaluation
- Let'S Do This!: Activity 1 Lifestyle EvaluationDocument2 pagesLet'S Do This!: Activity 1 Lifestyle EvaluationracmaPas encore d'évaluation
- Consenso Hepato Prof Helma CotrimDocument5 pagesConsenso Hepato Prof Helma CotrimrapphamouraPas encore d'évaluation
- LGBTQIA+ Rights Are Human RightsDocument13 pagesLGBTQIA+ Rights Are Human RightsI'm World Wide Handsome u know??Pas encore d'évaluation
- Tonic-Clonic Seizure?: SymptomsDocument3 pagesTonic-Clonic Seizure?: SymptomsMaria Jessica DumdumPas encore d'évaluation
- Crafting A SeasoningDocument14 pagesCrafting A SeasoningWulan LeePas encore d'évaluation
- University of Central Punjab: Course Title: Performance StrategyDocument4 pagesUniversity of Central Punjab: Course Title: Performance StrategyAyesha HamidPas encore d'évaluation
- MILLER - ProHeat35 - Induction CoolerDocument32 pagesMILLER - ProHeat35 - Induction CoolerHien NguyenPas encore d'évaluation
- 1 SMDocument6 pages1 SMRinaldi AdhytiaPas encore d'évaluation
- Go For No! 52 Personal Development Books in 52 WeeksDocument10 pagesGo For No! 52 Personal Development Books in 52 WeeksWalter YujraPas encore d'évaluation
- Accuracy and Validity of HbA1c POCT Report - August 2020Document86 pagesAccuracy and Validity of HbA1c POCT Report - August 2020Iura FlorinPas encore d'évaluation
- City Bantay Asin TaskDocument1 pageCity Bantay Asin TaskBob JoePas encore d'évaluation
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)D'EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Évaluation : 3 sur 5 étoiles3/5 (1)
- The Age of Magical Overthinking: Notes on Modern IrrationalityD'EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityÉvaluation : 4 sur 5 étoiles4/5 (30)
- Summary of Atomic Habits: An Easy and Proven Way to Build Good Habits and Break Bad Ones by James ClearD'EverandSummary of Atomic Habits: An Easy and Proven Way to Build Good Habits and Break Bad Ones by James ClearÉvaluation : 4.5 sur 5 étoiles4.5/5 (560)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionD'EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionÉvaluation : 4 sur 5 étoiles4/5 (404)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 5 sur 5 étoiles5/5 (81)
- No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems ModelD'EverandNo Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems ModelÉvaluation : 4.5 sur 5 étoiles4.5/5 (5)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDD'EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDÉvaluation : 5 sur 5 étoiles5/5 (3)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsD'EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsPas encore d'évaluation
- The Millionaire Fastlane: Crack the Code to Wealth and Live Rich for a LifetimeD'EverandThe Millionaire Fastlane: Crack the Code to Wealth and Live Rich for a LifetimeÉvaluation : 4.5 sur 5 étoiles4.5/5 (2)
- Eat That Frog!: 21 Great Ways to Stop Procrastinating and Get More Done in Less TimeD'EverandEat That Frog!: 21 Great Ways to Stop Procrastinating and Get More Done in Less TimeÉvaluation : 4.5 sur 5 étoiles4.5/5 (3227)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeD'EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeÉvaluation : 2 sur 5 étoiles2/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisD'EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisÉvaluation : 4.5 sur 5 étoiles4.5/5 (42)
- Indistractable: How to Control Your Attention and Choose Your LifeD'EverandIndistractable: How to Control Your Attention and Choose Your LifeÉvaluation : 3 sur 5 étoiles3/5 (5)
- The 5 Second Rule: Transform your Life, Work, and Confidence with Everyday CourageD'EverandThe 5 Second Rule: Transform your Life, Work, and Confidence with Everyday CourageÉvaluation : 5 sur 5 étoiles5/5 (12)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsD'EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsÉvaluation : 5 sur 5 étoiles5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsD'EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsÉvaluation : 4 sur 5 étoiles4/5 (4)
- The Obesity Code: Unlocking the Secrets of Weight LossD'EverandThe Obesity Code: Unlocking the Secrets of Weight LossÉvaluation : 4 sur 5 étoiles4/5 (6)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessD'EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessÉvaluation : 4.5 sur 5 étoiles4.5/5 (328)
- Why We Die: The New Science of Aging and the Quest for ImmortalityD'EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityÉvaluation : 4 sur 5 étoiles4/5 (5)
- The One Thing: The Surprisingly Simple Truth Behind Extraordinary ResultsD'EverandThe One Thing: The Surprisingly Simple Truth Behind Extraordinary ResultsÉvaluation : 4.5 sur 5 étoiles4.5/5 (709)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryD'EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryÉvaluation : 4 sur 5 étoiles4/5 (46)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.D'EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Évaluation : 4.5 sur 5 étoiles4.5/5 (110)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaD'EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)