Académique Documents
Professionnel Documents
Culture Documents
Vacations Health
Transféré par
IfáláwoniléAgboléObemoTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Vacations Health
Transféré par
IfáláwoniléAgboléObemoDroits d'auteur :
Formats disponibles
Are Vacations Good for Your Health?
The 9-Year Mortality Experience After the
Multiple Risk Factor Intervention Trial
BROOKS B. GUMP, PHD, MPH,
AND
KAREN A. MATTHEWS, PHD
Objective: The objective of this study was to determine the risk for various causes of posttrial death associated with
vacation frequency during the Multiple Risk Factor Intervention Trial (MRFIT). Methods: Middle-aged men at high
risk for coronary heart disease (CHD) were recruited for the MRFIT. As part of the questionnaires administered
during the first five annual visits, men were asked whether they had had a vacation during the past year. For trial
survivors (N 12,338), the frequency of these annual vacations during the trial were used in a prospective analysis
of posttrial all-cause and cause-specific mortality during the 9-year follow-up period. Results: The relative risk (RR)
associated with more annual vacations during the trial was 0.83 (95% confidence interval [CI], 0.71 0.97) for
all-cause mortality during the 9-year follow-up period. For cause of death, the RRs were 0.71 (95% CI, 0.58 0.89)
and 0.98 (95% CI, 0.78 1.23) for cardiovascular and noncardiovascular causes, respectively. The RR was 0.68 (95%
CI, 0.53 0.88) for CHD (including acute myocardial infarction). These associations remained when statistical
adjustments were made for possible confounding variables, including baseline characteristics (eg, income), MRFIT
group assignment, and occurrence of a nonfatal cardiovascular event during the trial. Conclusions: The frequency
of annual vacations by middle-aged men at high risk for CHD is associated with a reduced risk of all-cause mortality
and, more specifically, mortality attributed to CHD. Vacationing may be good for your health. Key words: coronary
heart disease, vacations, respite, restorative behaviors, Multiple Risk Factor Intervention Trial.
CHD coronary heart disease; CI confidence interval; DBP diastolic blood pressure; ICD-9 International Classification of Diseases, ninth revision; MI
myocardial infarction; MRFIT Multiple Risk Factor
Intervention Trial; RR relative risk; SES socioeconomic status; SI special intervention; UC usual
care.
Psychological stress is positively associated with
morbidity and mortality for a variety of diseases, including atherosclerosis (1), MI (2, 3), metabolic syndrome (4, 5), infectious disease (6, 7), and AIDS (8, 9).
Stress is thought to influence disease risk through a
number of pathways, including alterations in health
behaviors such as smoking (10), alcohol consumption
(11), compliance with medications (12), and emotional
states (13). More recently, it has been recognized that
normal restorative activities, such as sleep (14), exercise (15), and other leisure time activities, might influence disease risk. The present study examined
whether frequent annual vacations, a common form of
respite, serves a health protective function.
The Framingham Heart Study found an association
between infrequent vacationing and increased inci-
From the Department of Psychology (B.B.G.), State University of
New York, Oswego, NY; and the Department of Psychiatry (K.A.M.),
University of Pittsburgh, Pittsburgh, PA.
Address reprint requests to: Karen Matthews, Department of Psychiatry, University of Pittsburgh, 3811 OHara Street, Pittsburgh, PA
15213. Address correspondence to: Brooks B. Gump, PhD, MPH,
Department of Psychology, State University of New York, Oswego,
NY 13126. Email: gump@oswego.edu
Received December 27, 1999; revision received March 15, 2000.
608
0033-3174/00/6205-0608
Copyright 2000 by the American Psychosomatic Society
dence of MI or death due to coronary causes during a
20-year follow-up of women participants (16). Because
coronary death was not analyzed separately in this
study (there were only 10 coronary deaths), this increased risk associated with infrequent vacationing
does not necessarily represent an increased risk of
mortality. In another study, men who developed psychosomatic illnesses were less likely to take vacations
than men who never developed such illnesses (17).
Although taking regular annual vacations may serve
a protective function, it is important to consider alternative explanations. For example, higher SES may produce both lower morbidity and mortality (18) and
more frequent annual vacations, thereby producing a
spurious association between frequent annual vacations and physical health. Along similar lines, poor
health (eg, nonfatal MIs) may produce both higher
rates of subsequent mortality (19) and prevent annual
vacations. It is important to consider these alternative
explanations when analyzing the effects of vacationing
annually on mortality.
The purpose of this study was to evaluate 9-year
posttrial mortality and cause of death among MRFIT
participants as a function of the number of annual
vacations assessed during 5 years of the trial. This
study includes statistical controls for nonfatal healthrelated events and SES.
METHODS
Design of the MRFIT
A total of 361,662 men aged 35 to 57 years were initially screened
at 22 clinical centers in 18 US cities for MRFIT. A total of 12,866 of
these men were enrolled in the trial. At the time of study entry, these
men were in the upper 10% to 15% of the risk score distribution,
which was derived from the Framingham Heart Study data. Exclusion criteria included clinical evidence of CHD, based on history,
Psychosomatic Medicine 62:608 612 (2000)
VACATIONS AND HEALTH
physical examination, or electrocardiography (at rest); a serum cholesterol level 9.05 mmol/liter (350 mg/dl); DBP readings 115
mm Hg; or a body weight at least 50% greater than the standard
weight for height (20 22). After exclusion, the remaining participants were randomly assigned to an SI (N 6428) or UC (N 6438)
group. Participants in the SI group received dietary instructions
designed to alter eating patterns to reduce the intake of saturated fats
and to reduce blood cholesterol levels, a smoking cessation program,
and stepped-care drug therapy for hypertension. Details of the multifactor intervention program are described elsewhere (23, 24). In
our analyses, we included survivors of the trial (N 12,338).
Measurement of Annual Vacations
Vacationing was assessed by an item on a checklist of life events
(Within the last 12 months, have you experienced a vacation?).
The vacation item was not included on the checklist used at baseline
but was included on the checklist used at the first, second, third,
fourth, and fifth annual examinations. This checklist did not include
an option for indicating that an event had not occurred; as a result,
a missing response on items on this questionnaire did not enable
differentiation of missing data from intentional indications that an
event had not occurred. However, the life events checklist was
administered along with a number of other questionnaires; therefore, we treated data as missing for participants with known missing
data for five forced-choice questions that either directly preceded or
followed (depending on year) the life events questionnaire. Missing
data increased steadily from year 1 (N 695, 5.4%) to year 5 (N
1550, 12.0%) because of participant death or attrition. Mean vacationing was computed for all valid responses and reflects the proportion of years the participant reported vacationing for those years
with valid data.
Risk Factor Assessment
The following risk factors were considered: age at study entry;
MRFIT group assignment (SI or UC); education, measured on a scale
from 1 (eighth grade or less) to 9 (graduate or professional degree);
total family income, measured on a scale from 1 ($4200) to 9
($35,000); DBP, defined as the average of two random-zero manometer readings; serum cholesterol concentration; and cigarette
smoking, determined by self-report. To index cumulative risk factor
burden, we computed trial means for blood pressure, serum cholesterol, and smoking. For smoking, the average corresponds to the
proportion of assessments when smoking was reported. Additional
details about these assessments are published elsewhere (25, 26).
Morbidity and Mortality Ascertainment
A nonfatal cardiovascular event during the trial was defined as
angina (Rose questionnaire), intermittent claudication (Rose questionnaire), congestive heart failure, peripheral arterial occlusive disease, stroke, left ventricular hypertrophy (electrocardiography), impaired renal function, accelerated hypertension, coronary artery
bypass surgery, serial electrocardiographic evidence of MI, or definite clinical MI (determined by coding criteria of electrocardiographic tracings and/or physician inspection of hospital records)
(27).
Since February 1982, vital status has been ascertained by matching identifying information reported by participants at the time of
enrollment with the National Death Index. The latest search of the
National Death Index was for all deaths through December 1990 and
is considered to be essentially 100% complete (28). To determine
Psychosomatic Medicine 62:608 612 (2000)
cause of death, death certificates were collected and coded independently by two nosologists using ICD-9 codes (29). Disagreements
between the two nosologists were adjudicated by a third nosologist.
Cause-specific mortality categories (and corresponding ICD-9 codes)
considered in the present study were selected by the MRFIT Mortality and Morbidity Committee and are reported elsewhere (27).
Statistical Analyses
All analyses included trial survivors and considered mortality
during the 9-year follow-up period. Posttrial mortality was analyzed
using Cox proportional hazard regression equations and 95% CIs for
the RRs associated with mean vacationing during the trial. In these
analyses, proportion of years with report of vacation was treated as
a continuous variable (ranging from 0 to 1.00). To control for possible confounding variables, additional analyses included age, MRFIT
group assignment, DBP, serum cholesterol, education, family income, and cigarette smoking as covariates. Because the occurrence
of nonfatal cardiovascular events (ie, morbidity) might both interfere
with vacationing and predict future cardiovascular mortality, the
occurrence of a nonfatal cardiovascular event during the trial was
included as an additional covariate.
For analysis of differences in participants trial characteristics as
a function of annual vacationing, vacationing frequency was dichotomized into those reporting vacationing 60% of the years surveyed
(low-frequency group, N 6745) and those reporting vacationing for
60% of the years surveyed (high-frequency group, N 5822) in
these analyses. This dichotomous variable (low vs. high vacationing
frequency) was used in analyses of variance for tests of continuous
variables (blood pressure, age, educational attainment, smoking, and
cholesterol) and a 2 2 2 analyses of group proportions for tests of
categorical variables (ie, study group and occurrence of nonfatal
cardiovascular events during the trial).
RESULTS
Characteristics of Participants Taking Frequent
and Infrequent Vacations
For the five assessments of vacationing in the past
year, 12.8% of participants in MRFIT reported never
taking an annual vacation, 10.1% reported 1 annual
vacation, 11.4% reported 2 annual vacations, 14.4%
reported 3 annual vacations, 18.2% reported 4 annual
vacations, and 25.6% reported 5 annual vacations. The
remaining 7.6% had missing data; therefore, frequency
of annual vacations for these participants was the proportion of years in which the participant took a vacation for those years with valid data. The differences in
characteristics of participants taking frequent and infrequent annual vacations are shown in Table 1. The
large sample in MRFIT provides power to detect rather
small effects. Those taking frequent annual vacations
during the trial were significantly younger at study
entry, were less likely to be in the SI group, were less
likely to report cigarette smoking, were more educated,
had a higher family income, were less likely to experience a nonfatal cardiovascular event during the trial,
and had a higher serum cholesterol level during the
trial.
609
B. B. GUMP AND K. A. MATTHEWS
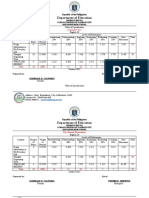
TABLE 1. Characteristics of Participants in MRFIT Taking
Infrequent and Frequent Annual Vacations During the Trial
TABLE 2. Cause of Death, Number of Deaths, and RR (with 95%
CI) for Deaths Through 9 Years of Post-trial Follow-Up
Associated With Frequency of Annual Vacations During the Trial
Annual Vacationing
Participant Characteristics
Age at entry into study, years
Study group, % in SI group
Smoking, %
DBP, mm Hga
Serum cholesterol, mg/dla
Educationb
Total family incomec
Nonfatal cardiovascular event
during trial, %
Infrequent
(N 6745)
Frequent
(N 5822)
46.57
51.49
48.66
86.36
239.16
5.14
6.21
24.02
46.21
48.29
43.45
86.21
241.48
5.70
6.85
19.34
.001
.001
.001
.189
.001
.001
.001
.001
Values are trial means.
Education was measured using a nine-point scale (1 eighth grade
or less, 9 graduate or professional degree).
c
Total family income was measured using a nine-point scale (1
$4200, 9 $35,000).
b
Frequency of Annual Vacations During the Trial
and Posttrial Mortality
The median length of follow-up for survivors of the
trial through December 1990 was approximately 9
years (8.8 years; range 7.8 to 10.1 years). During this
time, 770 cardiovascular and 743 noncardiovascular
deaths occurred. The RRs associated with more frequent annual vacations were 0.68 (95% CI, 0.59 0.79)
for all-cause mortality, 0.61 (95% CI, 0.50 0.75) for
cardiovascular mortality, and 0.77 (95% CI, 0.62 0.96)
for noncardiovascular mortality. As shown in Table 2,
after the addition of covariates to control for potential
confounding factors, the RRs associated with more
frequent annual vacations were 0.83 (95% CI, 0.71
0.97) for all-cause mortality, 0.71 (95% CI, 0.58 0.89)
for cardiovascular mortality, and 0.98 (95% CI, 0.78
1.23) for noncardiovascular mortality.
In addition to analyses of all cardiovascular and all
noncardiovascular deaths, specific causes of death
within each category were considered. For cardiovascular mortality, the frequency of annual vacations was
associated with a significant RR, 0.68 (95% CI, 0.53
0.88), for CHD. Within the CHD category, cause of
death was further categorized into acute MI (ICD-9
code 410) and other ischemic (coronary) heart disease
(ICD-9 codes 411 414 and 429.2). The RRs associated
with more frequent annual vacations were marginally
significant for acute MI (RR 0.70, 95% CI, 0.49 1.01)
and significant for other ischemic (coronary) heart disease (RR 0.66, 95% CI, 0.46 0.94). The frequency of
annual vacations was not associated with significant
RRs for any other specific cause of cardiovascular mortality or noncardiovascular mortality.
610
Cause of Death
Deaths
(N)
RR (95% CI)a
All causes
1443 0.83 (0.710.97) .018
All cardiovascular causes
745 0.71 (0.580.89) .002
CHD
540 0.68 (0.530.88) .003
Acute MI
262 0.70 (0.491.01) .058
Other ischemic CHD
278 0.66 (0.460.94) .020
Cardiac dysrhythmias
27 0.72 (0.232.23) .571
b
Hypertensive heart disease
14
b
Other hypertensive
7
Cerebrovascular
61 0.86 (0.411.82) .699
Other cardiovascular disease
97 0.76 (0.421.38) .361
All noncardiovascular causes
696 0.98 (0.781.23) .868
Neoplastic
464 1.16 (0.881.53) .294
b
Lip, oral cavity, and pharynx
10
Digestive organs and peritoneum 120 1.25 (0.722.18) .415
Colorectal
47 1.00 (0.422.40) .996
Other gastrointestinal
73 1.45 (0.712.95) .305
Respiratory and intrathoracic
187 1.15 (0.741.77) .541
organs
Lung
178 1.07 (0.691.68) .751
Other neoplasms
147 1.12 (0.681.82) .663
Respiratory
41 1.16 (0.452.95) .760
Digestive system
48 0.54 (0.231.25) .152
Accidents
57 0.65 (0.301.42) .282
Other noncardiovascular disease
86 0.71 (0.381.34) .292
a
In all Cox proportional hazard models, the following characteristics were included as covariates: age, study group (SI vs. UC), educational attainment, income, occurrence of a nonfatal cardiovascular
event during the trial, smoking, DBP, and serum cholesterol (the
later three values were trial averages). Missing covariate values
resulted in a subject being dropped from the analysis.
b
Insufficient number of events for calculation of RR.
The effect of morbidity on both vacationing frequency and subsequent mortality is a particular concern when considering the effects of the frequency of
annual vacations on subsequent mortality. Therefore,
we conducted additional analyses using only the frequency of annual vacations assessed at the first, second, and third annual examinations to predict mortality in survivors of the trial. Using this approach, a
4-year gap is placed between the assessment of the
frequency of annual vacations and the assessment of
mortality, making it unlikely that any observed association between vacationing frequency and mortality
would be a spurious association created by their common association with morbidity. In these analyses and
with the addition of covariates to control for potential
confounding factors, the RRs associated with more
frequent annual vacations were 0.86 (95% CI, 0.76
1.01, p .079) for all-cause mortality and 0.76 (95%
CI, 0.60 0.95, p .018) for CHD mortality.
Psychosomatic Medicine 62:608 612 (2000)
VACATIONS AND HEALTH
DISCUSSION
More frequent annual vacations during the MRFIT
was associated with a significant reduction in the risk
of death during the 9-year posttrial period. The specific cause of death most strongly associated with vacationing frequency was CHD. This association persisted with the addition of statistical controls for
baseline characteristics.
Although frequent vacationing may have a direct
protective effect on health, it is important to consider
alternative explanations for the observed associations.
First, it is possible that morbidity produces both less
frequent vacationing and an increased risk of death,
thereby producing a spurious association between the
frequency of annual vacations and mortality. In other
words, those who are ill are both unable to take a
vacation and more likely to die. The continued association of annual vacation frequency and CHD mortality in the context of statistical controls for nonfatal
cardiovascular events and when using the frequency of
annual vacations assessed during the first 3 years of
the trial to predict mortality 4 years latter (during the
posttrial period) does not support this alternative
explanation.
The positive association between SES and health is
well documented (18), and in the current sample,
lower SES was associated with less frequent vacationing. Therefore, another possibility is that those of
lower SES are both unable to take a vacation and more
likely to die. A continued significant association between vacationing frequency and CHD mortality in the
context of a statistical control for participants educational attainment and income does not support this
alternative explanation.
There are a few possible mechanisms through
which vacationing might have direct protective effects
on health. First, vacations may reduce stress by removing ongoing stressors (eg, avoidance). The health benefits of stress reduction are well documented (30, 31).
Furthermore, the current pattern of findings (ie, stronger effects with CHD relative to other causes of death,
eg, cancer) is consistent with research demonstrating
stronger stress and disease associations for CHD relative to cancer (32). Second, vacations may reduce
stress by removing potential stressors and anticipated
threats, providing a period of signaled safety (33).
Anticipated threats are known to have adverse effects
as great as (34), if not greater than (35), the threat itself.
Finally, annual vacations may provide a unique opportunity for behaviors having restorative effects on anabolic physiological processes, such as social contact
with family and friends (36 38) and physical activity
Psychosomatic Medicine 62:608 612 (2000)
(15), in the context of reduction of stress-initiated catabolic effects.
Some limitations of the current study should be
noted. First, vacationing frequency was assessed using
a single question about a vacation within the past
year. Therefore, we have no information about the
quantity or length of vacations within each year nor
information about the quality of these vacations. Such
information might enable a description of the type and
pattern of vacationing that have health-protective effects. Second, the MRFIT included the question about
annual vacations as a measure of attention to the questionnaires. Therefore, it is possible that the generally
hasty or less than fully compliant participants were
both at greater risk of CHD death and reported few
annual vacations as a consequence of low adherence.
Finally, vacationing frequency may serve as a marker
of other activities or personality characteristics that
are, in turn, associated with the reduced risk of mortality. For example, those taking annual vacations may
also engage in more health-promoting leisure-time activities. Leisure-time physical activity was measured
in MRFIT using a questionnaire assessment of various
physical activities. This questionnaire has been validated against treadmill exercise performance in MRFIT (39). Furthermore, leisure-time physical activity
measured with this questionnaire had a modest inverse relationship with CHD and overall mortality during MRFIT (15). However, the inclusion of leisure-time
physical activity as a covariate in the current analyses
did not alter the significant risk reduction in CHD
mortality associated with vacationing (RR 0.69, p
.006 with all covariates, including leisure-time physical activity).
In conclusion, more frequent annual vacations during the MRFIT seemed to exert a direct positive effect
on mortality during the 9-year posttrial period. Although the specific mechanism of this association remains unknown, these findings suggest the importance of considering the health benefits of restorative
behaviors, such as vacationing. Vacations may not
only be enjoyable but also health promoting.
This work was supported by Grant HL58867 from
the National Institutes of Health. We thank James Neaton, Ronald Prineas, Lewis Kuller, Greg Grandits, and
Yue-fang Chang for their consultation on analytic
strategy and manuscript preparation.
REFERENCES
1. Rozanksi A, Blumenthal JA, Kaplan J. Impact of psychological
factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation 1999;99:2192217.
611
B. B. GUMP AND K. A. MATTHEWS
2. Kamarck T, Jennings JR. Biobehavioral factors in sudden death.
Psychol Bull 1991;109:4275.
3. Karasek RA, Theorell T, Schwartz JE, Schnall PL, Pieper CF,
Michela JL. Job characteristics in relation to the prevalence of
myocardial infarction in the US Health Examination Survey
(HES) and the Health and Nutrition Examination Survey
(HANES). Am J Public Health 1988;78:910 8.
4. Rikknen K, Keltikangas-Jrvinen L, Hautanen A, Adlercreutz
H. Neuroendocrine mechanisms in chronic perceived stress:
associations with the metabolic syndrome. Endocrinol Metab
1997;4:24754.
5. Rikknen K, Keltikangas-Jrvinen L, Adlercreutz H, Hautanen
A. Psychosocial stress and the insulin resistance syndrome.
Metabolism 1996;45:1533 8.
6. Cohen S, Williamson GM. Stress and infectious disease in humans. Psychol Bull 1991;109:524.
7. Cohen S, Tyrrell DAJ, Smith AP. Psychological stress and susceptibility to the common cold. N Engl J Med 1991;325:606 12.
8. Leserman J, Jackson ED, Petitto JM, Golden RN, Silva SG, Perkins DO, Cai J, Folds JD, Evans DL. Progression to AIDS: the
effects of stress, depressive symptoms, and social support. Psychosom Med 1999;61:397 406.
9. Evans DL, Leserman J, Perkins DO, Stern RA, Murphy C, Zheng
B, Gettes D, Longmate JA, Silva SG, van der Horst CM, Hall CD,
Folds JD. Severe life stress as a predictor of early disease progression in HIV infection. Am J Psychiatry 1997;154:630 4.
10. Cohen S, Lichenstein E. Perceived stress, quitting smoking, and
smoking relapse. Health Psychol 1990;9:466 78.
11. Jennison KM. The impact of stressful life events and social
support on drinking among older adults: a general population
survey. Int J Aging Hum Dev 1992;35:99 123.
12. Coons SJ, Sheahan SL, Martin SS, Hendricks J, Robbins CA,
Johnson JA. Predictors of medication noncompliance in a sample of older adults. Clin Ther 1994;16:110 7.
13. Eckenrode J. Impact of chronic and acute stressors on daily
reports of mood. J Pers Soc Psychol 1984;46:90718.
14. Kripke DF, Ancoli-Israel S, Mason W, Messin S. Sleep related
mortality and morbidity in the aged. In: Chase M, Weitzman E,
editors. Sleep disorders: basic and clinical research. New York:
SP Medical & Scientific Books; 1983. p. 41529.
15. Leon AS, Connett J, Jacobs DR Jr, Rauramaa R. Leisure-time
physical activity levels and risk of coronary heart disease and
death: the Multiple Risk Factor Intervention Trial. JAMA 1987;
258:2388 95.
16. Eaker ED, Pinsky J, Castelli WP. Myocardial infarction and coronary death among women: psychosocial predictors from a 20year follow-up of women in the Framingham Study. Am J Epidemiol 1992;135:854 64.
17. Vaillant GE. Natural history of male psychological health. IV.
What kinds of men do not get psychosomatic illness? Psychosom Med 1978;40:420 31.
18. Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL,
Syme SL. Socioeconomic status and health: the challenge of the
gradient. Am Psychol 1994;49:1524.
19. The Multiple Risk Factor Intervention Trial Research Group.
Mortality after 16 years for participants randomized to the Multiple Risk Factor Intervention Trial. Circulation 1996;94:
946 51.
20. Multiple Risk Factor Intervention Trial Research Group. Statistical design considerations in the NHLI Multiple Risk Factor
Intervention Trial. J Chronic Dis 1977;30:26175.
612
21. Sherwin R, Kaelber CT, Kezdi P, Kjelsberg MO, Thomas HE Jr.
The Multiple Risk Factor Intervention Trial (MRFIT). II. The
development of the protocol. Prev Med 1981;10:40225.
22. Neaton JD, Grimm RH Jr, Cutler JA. Recruitment of participants
for the Multiple Risk Factor Intervention Trial (MRFIT). Controlled Clin Trials 1987;8:41S53S.
23. Benfari RC. Multiple Risk Factor Intervention Trial (MRFIT). III.
The model for intervention. Prev Med 1981;10:426 42.
24. Caggiula AW, Christakis G, Farrand M, Hulley SB, Johnson R,
Lasser NL, Stamler J, Widdowson G. Multiple Risk Factor Intervention Trial (MRFIT). IV. Intervention on blood lipids. Prev
Med 1981;10:44375.
25. Multiple Risk Factor Intervention Trial Research Group. Multiple Risk Factor Intervention Trial: risk factor changes and mortality results. JAMA 1982:248,146577.
26. Multiple Risk Factor Intervention Trial Research Group. Baseline rest electrocardiographic abnormalities, antihypertensive
treatment, and mortality in the Multiple Risk Factor Intervention Trial. Am J Cardiol 1985;55:115.
27. Multiple Risk Factor Intervention Trial Research Group. Mortality after 16 years for participants randomized to the Multiple
Risk Factor Intervention Trial. Circulation 1996;94:946 51.
28. Wentworth D, Neaton J, Rasmussen W. An evaluation of the
Social Security Administration master beneficiary record file
and the National Death Index in the ascertainment of vital
status. Am J Public Health 1983;73:1270-4.
29. Anonymous. International Classification of Diseases, North
American Clinical Modification. Ann Arbor (MI): Edwards;
1981;1.
30. McCubbin JA, Wilson JF, Bruehl S, Ibarra P, Carlson CR, Norton
JA, Colclough GW. Relaxation training and opioid inhibition of
blood pressure response to stress. J Consult Clin Psychol 1996;
64:593 601.
31. Dusseldorp E, van-Elderen T, Maes S, Meulman J, Kraaij V. A
meta-analysis of psychoeducational programs for coronary heart
disease patients. Health Psychol 1999;18:506 19.
32. Rosengren A, Tibblin G, Wilhelmsen L. Self-perceived psychological stress and incidence of coronary artery disease in middle-aged men. Am J Cardiol 1991;68:11715.
33. Weinberg J, Levine S. Psychobiology of coping in animals: the
effects of predictability. In: Levine S, Ursin H, editors. Coping
and health. NATO conference series III: human factors. New
York: Plenum; 1980. p. 39 60.
34. Spacapan S, Cohen S. Effects and aftereffects of stressor expectations. J Pers Soc Psychol 1983;45:124354.
35. Nomikos MS, Opton EM, Averill JR, Lazarus RS. Surprise versus
suspense in the production of stress reaction. J Pers Soc Psychol
1968;8:204 8.
36. House JS, Landis KR, Umberson D. Social relationships and
health. Science 1988;241:540 4.
37. Kaplan GA, Cohn BA, Cohen RD, Guralnik J. The decline in
ischemic heart disease mortality: prospective evidence from the
Alameda County study. Am J Epidemiol 1988;127:1131 42.
38. Orth-Gomer K, Johnson JV. Social network interaction and
mortality: a six year follow-up study of a random sample of the
Swedish population. J Chronic Dis 1987;40:949 57.
39. Leon AS, Jacobs DR Jr, DeBacker G, Taylor HL. Relationship of
physical characteristics and life habits to treadmill exercise
capacity. Am J Epidemiol 1981;113:653 60.
Psychosomatic Medicine 62:608 612 (2000)
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Ethanol Production From Waste Materials: June 2013Document5 pagesEthanol Production From Waste Materials: June 2013deepu kumarPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- 19 SkyBusDocument5 pages19 SkyBusIfáláwoniléAgboléObemoPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Energy Ethatol Wilson 2009Document48 pagesEnergy Ethatol Wilson 2009IfáláwoniléAgboléObemoPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Ethanol Production From Waste Materials: June 2013Document5 pagesEthanol Production From Waste Materials: June 2013deepu kumarPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Is Iso 21951 2001Document11 pagesIs Iso 21951 2001yesvvnPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Agama Di Kota MalangDocument13 pagesAgama Di Kota MalangIfáláwoniléAgboléObemoPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Amssm Position Statement Concussion in SportDocument13 pagesAmssm Position Statement Concussion in SportIfáláwoniléAgboléObemoPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Alex Barrows Training PDFDocument12 pagesAlex Barrows Training PDFIfáláwoniléAgboléObemo100% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Strategic AlliancesDocument22 pagesStrategic AlliancesAngel Anita100% (2)
- Calculator EngenhariaDocument77 pagesCalculator EngenhariaIfáláwoniléAgboléObemoPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- 2-09 A Graff UsaDocument11 pages2-09 A Graff UsaIfáláwoniléAgboléObemoPas encore d'évaluation
- Vivelle - DOT InglexDocument30 pagesVivelle - DOT InglexIfáláwoniléAgboléObemoPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Supported ID docs for PoI, PoA, PoR, DoBDocument1 pageSupported ID docs for PoI, PoA, PoR, DoBVinit JhingronPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Hurley2001 - Disc AbrasiveDocument7 pagesHurley2001 - Disc AbrasiveIfáláwoniléAgboléObemoPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Estimated Testing TimesDocument1 pageEstimated Testing TimesIfáláwoniléAgboléObemoPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Mef Country CodesDocument6 pagesMef Country CodesIfáláwoniléAgboléObemoPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Enclothed Cognition ArticleDocument8 pagesEnclothed Cognition ArticlelloydmofPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- Shows Mac LarDocument9 pagesShows Mac LarIfáláwoniléAgboléObemoPas encore d'évaluation
- Fast Fact Bullying in SchoolsDocument9 pagesFast Fact Bullying in SchoolsNix DarvishPas encore d'évaluation
- FBI's Evolving Role in Terrorism Investigations Since 9/11Document30 pagesFBI's Evolving Role in Terrorism Investigations Since 9/11IfáláwoniléAgboléObemoPas encore d'évaluation
- Skredderberget - Heaven of Pain - Author's PresentationDocument2 pagesSkredderberget - Heaven of Pain - Author's PresentationIfáláwoniléAgboléObemoPas encore d'évaluation
- CpE194 Lab Experiment # 1 - MTS-88 FamiliarizationDocument4 pagesCpE194 Lab Experiment # 1 - MTS-88 FamiliarizationLouieMurioPas encore d'évaluation
- 7 JitDocument36 pages7 JitFatima AsadPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Tamil Literary Garden 2010 Lifetime Achievement Award CeremonyDocument20 pagesTamil Literary Garden 2010 Lifetime Achievement Award CeremonyAnthony VimalPas encore d'évaluation
- حقيبة تعليمية لمادة التحليلات الهندسية والعدديةDocument28 pagesحقيبة تعليمية لمادة التحليلات الهندسية والعدديةAnjam RasulPas encore d'évaluation
- Liberal Theory: Key Aspects of Idealism in International RelationsDocument11 pagesLiberal Theory: Key Aspects of Idealism in International RelationsArpit JainPas encore d'évaluation
- Finance Process Optimization - Mapping The Journey To High PerformanceDocument3 pagesFinance Process Optimization - Mapping The Journey To High PerformanceStephen G. LynchPas encore d'évaluation
- PLC 2 Ladder DiagramDocument53 pagesPLC 2 Ladder DiagramAnkur GuptaPas encore d'évaluation
- Shailesh Sharma HoroscopeDocument46 pagesShailesh Sharma Horoscopeapi-3818255Pas encore d'évaluation
- Develop Your Kuji In Ability in Body and MindDocument7 pagesDevelop Your Kuji In Ability in Body and MindLenjivac100% (3)
- S32 Design Studio 3.1: NXP SemiconductorsDocument9 pagesS32 Design Studio 3.1: NXP SemiconductorsThành Chu BáPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Math Curriculum Overview Grades 1 8Document1 pageMath Curriculum Overview Grades 1 8GuisellePas encore d'évaluation
- Table of Specification ENGLISHDocument2 pagesTable of Specification ENGLISHDonn Abel Aguilar IsturisPas encore d'évaluation
- 1 PDFDocument14 pages1 PDFPM JFPas encore d'évaluation
- NIT JRF OpportunityDocument4 pagesNIT JRF Opportunitybalaguru78Pas encore d'évaluation
- Two Monuments by C Mann 1493 Copy - PDF - OcredDocument23 pagesTwo Monuments by C Mann 1493 Copy - PDF - OcredStephania FrancoPas encore d'évaluation
- GR 5 Unit Plan 18-19 Art Warli ArtDocument4 pagesGR 5 Unit Plan 18-19 Art Warli ArtSanjay RautPas encore d'évaluation
- Roadmap For SSC CGLDocument11 pagesRoadmap For SSC CGLibt seoPas encore d'évaluation
- 10 1016@j Ultras 2016 09 002Document11 pages10 1016@j Ultras 2016 09 002Ismahene SmahenoPas encore d'évaluation
- Policarpio 3 - Refresher GEODocument2 pagesPolicarpio 3 - Refresher GEOJohn RoaPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Decision MatrixDocument12 pagesDecision Matrixrdos14Pas encore d'évaluation
- DPCA OHE Notice of Appeal 4-11-2018 FinalDocument22 pagesDPCA OHE Notice of Appeal 4-11-2018 Finalbranax2000Pas encore d'évaluation
- Instruction Manual For National Security Threat Map UsersDocument16 pagesInstruction Manual For National Security Threat Map UsersJan KastorPas encore d'évaluation
- What Is Science Cornell Notes ExampleDocument3 pagesWhat Is Science Cornell Notes Exampleapi-240096234Pas encore d'évaluation
- Activity Emcee Mid-Year INSET 2021Document3 pagesActivity Emcee Mid-Year INSET 2021Abegail A. Alangue-Calimag67% (6)
- Engineering Mathematics I - Class Test December 2015Document6 pagesEngineering Mathematics I - Class Test December 2015Kunal RamnatsingPas encore d'évaluation
- Indian Oil Corporation- Leading Indian State-Owned Oil and Gas CompanyDocument10 pagesIndian Oil Corporation- Leading Indian State-Owned Oil and Gas CompanyPrakhar ShuklaPas encore d'évaluation
- 5.mpob - LeadershipDocument21 pages5.mpob - LeadershipChaitanya PillalaPas encore d'évaluation
- Humanities Unit Plan Plus Lesson PlansDocument12 pagesHumanities Unit Plan Plus Lesson Plansapi-298200210Pas encore d'évaluation
- Companies DatabaseDocument2 pagesCompanies DatabaseNIRAJ KUMARPas encore d'évaluation
- Bluehill BrochureDocument24 pagesBluehill BrochureGeorge SingerPas encore d'évaluation
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeD'EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BePas encore d'évaluation
- The Motive: Why So Many Leaders Abdicate Their Most Important ResponsibilitiesD'EverandThe Motive: Why So Many Leaders Abdicate Their Most Important ResponsibilitiesÉvaluation : 5 sur 5 étoiles5/5 (219)
- The 7 Habits of Highly Effective People: The Infographics EditionD'EverandThe 7 Habits of Highly Effective People: The Infographics EditionÉvaluation : 4 sur 5 étoiles4/5 (2475)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionD'EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionÉvaluation : 4 sur 5 étoiles4/5 (402)
- Indistractable: How to Control Your Attention and Choose Your LifeD'EverandIndistractable: How to Control Your Attention and Choose Your LifeÉvaluation : 3.5 sur 5 étoiles3.5/5 (4)