Académique Documents
Professionnel Documents
Culture Documents
Pulmonary Physiology Handout One Slide 10-13-16
Transféré par
Anonymous 7WWMwAhH8Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Pulmonary Physiology Handout One Slide 10-13-16
Transféré par
Anonymous 7WWMwAhH8Droits d'auteur :
Formats disponibles
10/13/2016
Pulmonary Physiology
Respiration
Chris L. Wells, PhD, PT, CCS, ATC
BSII: 2015
10/13/2016
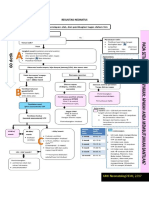
Three Phases of Respiration
Ventilation
Diffusion
Perfusion
Wells,CL 2016
10/13/2016
Movement System
Mitochondria
CO2
Muscle
Mitochondria
O2
Aerobic or
Anaerobic
Metabolism
Veins
S
y
s
t
e
m
I
c
Arteries
Right Heart
Veins
Heart
P
u
l
m
o
n
a
r
y
Left Heart Arteries
Heart Pump
Cardiac Output
CO = HR x SV
Expired Air
CO2
Production
VCO2
Lungs
VO2
Inspired Air
O2
Consumption
Lung Pump
Minute Ventilation
VE = RR x TV
Wells,CL 2016
Adapted from: Wasserman, Lea & Febriger, 1987: S Tepper 2013
10/13/2016
Functions of Ventilation
Exchange O2 and CO2
pH balance
Hormone function
Temperature regulation
Pressure regulation: thoracic / abdominal
Association with
Balance
Airway clearance
Incontinence
Wells,CL 2016
10/13/2016
Chest Wall
Pediatric:
Adults
Smaller ratio of trunk
Horizontal rib cage
Unstable chest wall
Ineffective accessory muscles
2/3 of trunk
Cone shape
Closed Osseous ring
Normal length tension for
accessory muscles
Response to stress?
Response to stress?
Wells,CL 2016
10/13/2016
Age Difference of Lungs
Pediatrics: varies upon age
Infant:
Smaller airways
Higher airway pressure
Less cartilaginous support
Early airway closure
Less alveoli
Surface area for diffusion
Glands
Secretions
Type I fibers of Diaphragm
More susceptible to respiratory insufficiency / failure
Wells,CL 2016
10/13/2016
Chest Wall
Purpose:
Protect vital organs
Mobility
Sufficient ventilation
UE function
Wells,CL 2016
10/13/2016
Chest Wall Mobility: Breathing
Mechanics
Rib 1:
elevation during inspiration
Joint: inferior
Ribs 2-6 (pump handle)
Anterior and superior direction during inspiration
Joints: downward, anterior and posterior rotation
Ribs 7-10 (bucket handle)
Lateral and superior direction during inspiration
Joints: posterior and lateral, slight downward and posterior rotation
Ribs 11-12
Caliper movement
Little effect on chest wall expansion
10/13/2016
Muscles of Ventilation
Diaphragm
Fiber type
55% slow oxidative type
21% fast oxidative type
24% fast glycolytic type
75% of thoracic volume at rest
Intercostals
?? function
Stabilize rib cage
Wells,CL 2016
10/13/2016
Muscles of Ventilation
Accessory Inspiratory
Accessory Expiratory
What muscles could be
recruited by a patient with SCI
above C6?
What would change if injury
level was T8
How would breathing by altered if the patient
had suffered a significant stroke?
Wells,CL 2016
10
10/13/2016
Nervous System
Voluntary sensation / motor
Central Nervous system
Medulla
Ventral: regulates rhythm, voluntary forced exhalation and acts to increase force of
inspiration
Dorsal: controls inspiration and timing
Pons
Pneumotaxic center: controls speed, fine tuning rate
Apneustic center: coordinates speed, activities and prolongs inhalation, overrides
pneumotaxic center to end inspiration
Wells,CL 2016
11
10/13/2016
Nervous System: ANS
Efferent
PNS: via vagus nerve (X)
Medulla to run // with airway
Secrete acetylcholine
Airway muscle contraction (bronchoconstriction)
Vascular dilation (pulmonary vasodilatation)
Glandular secretion
Wells,CL 2016
12
10/13/2016
Nervous System: ANS
Efferent
SNS: spinal cord to thoracic sympathetic ganglia
Also runs // with airways
Primary secrete norepinephrine to bind with
Alpha-adrenergic receptors pulmonary vasoconstriction
Beta-adrenergic receptors bronchodilation
Beta-adrenergic receptors bronchovascular dilation
Wells,CL 2016
13
10/13/2016
Nervous System: non-ANS
Efferent
Along pathway of vagus nerve
Promote nitric oxide production
Airway dilation
May also cause local bronchoconstriction through release of
Substance P and neurokinin A
Wells,CL 2016
14
10/13/2016
Chemoreceptors
Central
Peripheral
Carotid bodies
Upper Medulla
Common carotid bifurcation
Aortic arch
Responsive to CO 2
PaCO2 activates
chemoreceptors
Depth of breathing
Respiratory rate
Hypoxemia ( PaO2)
Ventilation
Hypoxic Drive
COPD
Wells,CL 2016
15
10/13/2016
Reflexes
Hering-Breuer Reflex:
Cough Reflex:
Trachea to bronchioles (smooth
muscle)
Over inflation (800ml > FRC
Larynx to lower bronchi
Chemical / Mechanical stimulation
Respiratory rate
Expiratory time
Rapid inspiration
Epiglottis closes
Abdominals contract
Airway pressure
Vocal cords and epiglottis open
Expectoration
Wells,CL 2016
16
10/13/2016
Reflexes
Stretch reflexes:
ICS and diaphragm Spinal cord
Muscle recruitment Ventilation
Joint / Muscle Receptors
Limb movement ventilation in preparation
Mechanoreceptors arterial circulation
BP hyperventilation
BP hypoventilation
Wells,CL 2016
17
10/13/2016
Nervous System: Afferent
Via Vagus Nerve
Slow adapting receptors (SAR) inflation stretch
Rapid adapting receptors (RAR) changes to
Tidal volume
Respiratory rate
Lung compliance
Responses to mechanical and chemical irritants
Other receptors
Chest wall, muscles, O2, CO2, H+
Wells,CL 2016
18
10/13/2016
Nervous System: Afferent
Juxtacapillary receptors (J receptors ): ?? Function but appears to
Alveoli and capillary beds
Pulmonary edema, PE, CHF, barotrauma
Pulmonary nociceptors / C fibers
Response:
Rapid shallow breathing
Dyspnea
Stimuli
Bradycardia
Hypotension
Bronchoconstriction
Mucus production
Apnea
Wells,CL 2016
19
10/13/2016
Parietal
Sensory nerves
Pleural Space
Visceral
Stomata
Openings into lymphatic drainage
Pleural space / fluid
.26 ml/kg fluid
friction
Airtight seals
Lung expansion
Costophrenic angle
30-45 degree angle
Wells,CL 2016
20
10/13/2016
Clinical Significance
Rib Fracture
Open heart surgery
Disruption of both pleura
Pleural effusion
Loss of costophrenic angel
Clinical results:
Air / blood leak into space
Inspiration
Chest wall
Lung
Compression from Fluid
Atelectasis
Clinical results:
Loss of intrapleural pressure
Lung collapse (PTX)
Compression from fluid:
Atelectasis
Wells,CL 2016
21
10/13/2016
Clinical Significance
Chest tube:
Wells,CL 2016
22
10/13/2016
Review Anatomy of Airway
23
10/13/2016
Airways
Conducting airways
Upper:
Lower
Respiratory
airways
Wells,CL 2016
24
10/13/2016
Lower Respiratory Tract
Conducting
1-15 generation
Bronchial division
cross sectional area airway
velocity
Larynx
Laminar flow
Cricoid cartilage CPR
airway resistance
work of breathing
Complete ring
Trachea
Allows for gas exchange
Creates normal breath sounds
C shaped rings
Carina : Sternal angle
Airway Management
Main Bronchi
Difference in angles
RLL clinical risk
Wells,CL 2016
25
10/13/2016
Conducting System: Histology
Layers:
Mucosa
Epithelia
Submucosa
Connective tissue, glands
Smooth fibers
Adventitia
Cartilaginous rings
Wells,CL 2016
26
10/13/2016
Conducting System: Histology
Mucosa:
Pseudostratified, ciliated, columnar epithelia
Maintenance of fluid and electrolytes
Key for proper mucus function and transport
Serous cells: secrete Cl- and HCO3 Secretion consistency and pH
Goblet cells: mucous (mucin)
Basement membrane
Key for repair of mucous membrane
Wells,CL 2016
27
10/13/2016
Conducting System: Histology
Mucosa
Mucus Blanket
Gel Layer
Sol Layer
Ciliated Cells
Mucus
Primarily water (97%)
Solute: protein, lipids, minerals
Function:
Protection from toxins and organisms
Fluid balance
Attracts air participles
Wells,CL 2016
28
10/13/2016
Conductive System: Histology
Submucosa
Bronchial glands: role in inflammation, mucin (solute portion of mucus)
Mast cells histamine
Vasodilation
Bronchoconstriction
Smooth muscle
Cartilage
Wells,CL 2016
29
10/13/2016
Conductive System: Histology
Adventitia
Connective tissue
Vascular
Lymph vessels
Adipose tissue
Wells,CL 2016
30
10/13/2016
Conducting System
Dead space
Physiologic dead space is part of TV that does not participate in gas exchange
Anatomical: air from the conducting system
With a TV of 500 ml
150 ml in conducting airway
350 ml in respiratory airways gas exchange
Alveolar: air in alveoli that is not exposed to blood for gas exchange
Wells,CL 2016
31
10/13/2016
Dead Space
Alveolar dead space:
Air in alveoli that is not
exposed to blood flow
Pathological Dead Space
Atelectasis
COPD
Dead Space
Wells,CL 2016
32
10/13/2016
Lower Respiratory Tract:
Respiratory System
12 (15) 23 generation
Function
Conducting air
Gas exchange
Acinus (primary lobule)
Respiratory bronchioles
Alveolar ducts
Alveolar sac (alveolar duct and alveoli)
Alveoli
Wells,CL 2016
33
10/13/2016
Respiratory System: Alveoli
Septa (alveolar walls)
Type I pneumocytes
Cover 93% of surface area
Gas exchange
Type II pneumocytes
7% of surface area
Produce surfactant
Stem cell like Differentiate into type I cells
Repair
Release cytokinnes inflammation
Wells,CL 2016
34
10/13/2016
Surfactant
Composed of phospholipids & proteins
Purpose
Surface tension of alveoli
Shed water from alveoli surface
Function
Work of breathing
Improves compliance
Prevents collapse
Protects alveolar surface
Wells,CL 2016
35
10/13/2016
Respiratory System
Alveolar-capillary membrane
= Respiratory membrane
Type 1 endothelial to erythrocytes
Diffusion: difference in partial pressure
Gas Exchange
Wells,CL 2016
36
10/13/2016
Respiratory System
Macrophages / lymphocytes
Key defense for respiratory system
Interstitial space
Elastin and collagen fibers
Supports alveolar shape
Pores of Kohn (b/w alveoli)
Channels of Lambert (b/w respiratory bronchioles)
Wells,CL 2016
37
10/13/2016
Cleaning Mechanisms of the Lungs
Large Airways
Small Airways
Alveoli
Wells,CL 2016
38
10/13/2016
Bronchial Circulation
Metabolic needs of lung and pleura
Low demand: 1-2% of cardiac output
Compensatory
pulmonary circulation bronchial circulation
risk of pulmonary infarction
Wells,CL 2016
39
10/13/2016
Lymphatic System
Function
Fluid balance
Clears fluid from interstitial and pleural space
Immune defense via
Drainage through lymph fluid
Phagocytosis (macrophages)
Produces lymphocytes and plasma cells
Wells,CL 2016
40
10/13/2016
Ventilation
41
10/13/2016
Ventilation
Process of moving air in and out of lung
Tidal volume: resting volume inspired or expired
Sufficient to meet metabolic needs
Factors
Pressure: force generated by respiratory muscles
Compliance: ease of air acceptance (chest wall & lung)
Resistance: air flow and tissue resistance against ventilation
Resistance muscles work against to ventilate lungs
Flow: volume changes / time
Wells,CL 2016
42
10/13/2016
Ventilation
Ventilation goes to dependent lungs
Gravity /weight of lungs (upright lung)
More negative pressure upper airways
Leads to larger resting volume in apices
Less negative pressure lower airways
Leads to higher compliance and smaller resting volume
RESULTS
Greater change in volume in lower lung fields
What happens when the patient is supine? Sidelying?
Wells,CL 2016
43
10/13/2016
Ventilation
Ventilation occurs because of transpulmonary pressure
Ptp =
Ppl - Pa
Pressure gradient between
Pleural pressure created by muscles
Inspiration: -7 cm/ H2O pressure
Airway pressure created by lungs
Inspiration: -1 cm/H2O pressure
Leads to a tidal volume ~ .5 L
-5cm. H2O to prevent airway closure (atelectasis)
Wells,CL 2016
44
10/13/2016
Forces Opposing Inhalation
Compliance
Lung parenchyma
Elastin and Collagen
Elasticity = tendency to return to resting state
Frictional forces
Gas flow through airways
Airway resistance
Tissue movement
Lungs, abdomen, diaphragm, rib cage
Ascites, obesity, fibrosis
Wells,CL 2016
45
10/13/2016
Compliance
Resting
Lung Chest Wall = FRC
Functional Residual Capacity
RV+ ERV
Resting balance of
elastic forces
Resting volume
Wells,CL 2016
46
10/13/2016
Functional Residual Capacity
Function
Work of breathing
Gas exchange
Decrease with
Atelectasis
Positioning : standing to supine
Pulmonary fibrosis
Wells,CL 2016
47
10/13/2016
FRC: Clinical Significant
Posture:
Upright: greatest FRC
Reduces airway closure
Maximizes gas exchange
Supine: reduces FRC by 50%
atelectasis
Hospitalization: anesthesia / surgery
Alteration in ventilation mechanics
Alteration in diaphragm position / function
Further reduces FRC
Airway closure
Work of breathing
Wells,CL 2016
48
10/13/2016
FRC: Pathology
Auto Peep:
Is gas trapped in alveoli at end expiration, due to inadequate time for
expiration,
Causes:
Mechanical ventilation:
Decrease expiratory time
Increase expiratory pressure
Airway obstructions (mucous plugs)
Exercise with COPD
Air hunger
Wells,CL 2016
49
10/13/2016
Forces Opposing Inhalation
Airway Resistance: Tracheobronchial flow
Laminar flow
Gas moves in discrete layers
Center flow is faster than air near airway
20% of airway resistance in small airways from laminar
Turbulent flow
Irregular currents
Smaller airways flow
80% of total resistance at upper airway from turbulent
It is the turbulence of air
flow that leads to normal
breath sounds
Wells,CL 2016
50
10/13/2016
Work of Breathing (WOB)
Inhalation:
Compliance: work to expand lungs against elastic forces
Tissue Resistance: work to overcome viscosity of lung and chest wall
Airway Resistance: work to overcome airway resistance
Clinical relevance: What is my
patients problem? Can I, as a Pt,
do something about it?
Wells,CL 2016
51
10/13/2016
Ventilation Activities
Involuntary
Sighing
Laughing
Yawning
Hiccoughing
Vomiting
Sneezing
Exhalation
Signing
Talking
Blowing
Coughing
Breath hold
Inhalation
Sniffing
sucking
Valsalva
Defecation
Heavy exertion
Wells,CL 2016
52
10/13/2016
Diffusion
Crossing the alveoli capillary membranes
53
10/13/2016
Diffusion
O2
O2
Alveoli
O2
O2
Surfactant
alveolar epithelial
capillary endothelial
plasma
erthyrocyte membrane
intracellular fluid
Hemoglobin
CO2
CO2
CO2
CO2
CO2
Wells,CL 2016
54
10/13/2016
Diffusion
O2
Alveoli
O2
O2
O2
Surfactant
alveolar epithelial
Edema
capillary endothelial
Exudate
Fluid
Fibrosis
CO2
CO2
plasma
erthyrocyte membrane
intracellular fluid
Hemoglobin
CO2
CO2
CO2
Wells,CL 2016
55
10/13/2016
Sarcoidosis, scleroderma,
pulmonary edema, PF
Diffusion
PaCO2
Alveoli
Surfactant
CO2
O2
CO2
CO2
alveolar epithelial
capillary endothelial
CO2
CO2
O2
Hypoxemia
O2
plasma
erthyrocyte membrane
O2
intracellular fluid
Hemoglobin
PaO2
Wells,CL 2016
56
10/13/2016
Air Pressure: = 760 mmHg
Atmospheric Air: Inhale
O2: 159 mmHg (20.84%)
CO2: 0.3 mmHg (0.04%)
Atmospheric Air: Exhale
O2: 120 mmHg (15.7%)
CO2: 27 mmHg (3.6%)
Alveolar Air:
O2 = 104 mmHg (13.6%)
CO2 = 40 mmHg (6.2%)
Pulmonary Capillary
Arterial
PO2 = 40 mmHg
PCO2 = 45 mmHg
Venous
PO2 = 104 mmHg
PCO2 = 40 mmHg
Wells,CL 2016
57
10/13/2016
Gas Pressure Differences
Constant diffusion of gases
Humidification of alveolar air
Only partial exchange of alveolar air
Allows for stable concentrations stable pH
Wells,CL 2016
58
10/13/2016
Diffusion Rate Factors
Thickness of respiratory membrane
Alveoli capillary fused walls
Pathologies
PF
ARDS
Surface area
Clinically significant when reduced to 1/3 to
Pathology
COPD
Pressure gradient
Wells,CL 2016
59
10/13/2016
Diffusion Capacity
Measures diffusion across respiratory membrane
Volume of gas per minute for 1 mmHg pressure difference
O2: 21 ml/min/mmHg at rest
O2: 65 ml/min/mmHg at peak exercise
REMEMBER: What is happening to the
airways and vasculature at times of
exercise (SNS and catecholamine
activation?
Wells,CL 2016
60
10/13/2016
Diffusion Capacity
Possible by opening dominant capillaries and alveoli = O2
saturation
surface area (3 times the active respiratory membrane)
Diffusion occurs in first 1/3 of capillary exposure
2/3 more available time for diffusion to occur
Wells,CL 2016
61
10/13/2016
Perfusion
Pulmonary Circulation available for gas exchange
62
10/13/2016
Vascular: Pulmonary
Pulmonary
Pulmonary Function
Veins: oxygenated blood
Arteries: deoxygenated
Capillaries within alveolar walls
Covers 90% of alveolar surface
Capillaries more sheet like
coverage over alveoli
Gas exchange
Fluid barrier
Blood reservoir
Filter for blood clots
Clearance
Adenosine, NE, prostaglandins
Conversion of angiotension I to II
Release cytokines
Inflammatory response
Wells,CL 2016
63
10/13/2016
Hemoglobin
97% of O2 is carried by Hemoglobin
3% is dissolved
Normal references:
Male: 14 18 g/dL
Female: 12- 16 g/dL
Wells,CL 2016
64
10/13/2016
Hemoglobin
Low: 8-10 g/dl
High (polycythemia)
exercise tolerance
fatigue
Tachycardia
>20 g/dl
Capillary clotting
< 8 g/dl
High risk of falls in elderly
Wells,CL 2016
65
10/13/2016
Hematocrit
Percentage of packed red cells in volume of
whole blood
Norms:
Males: 42 52%
Females: 37 - 47%
<25% no exercise
YES to FUNCTION
<20% heart failure
Stable?
> 60% spontaneous clotting
Wells,CL 2016
66
10/13/2016
Perfusion
Gravity
Hydrostatic Pressure (weight of blood itself)
15 mmHg less in UL compared to PAP
8 mmHg greater in LL compared to PAP
Perfusion of lower lobes
Exercise: pressure difference is less
Wells,CL 2016
67
10/13/2016
Perfusion
Key Factors
Driving pressure
Vascular resistance
Gravity
Pulmonary arterial pressure increase
Superior to inferior hydrostatic pressure
Less driving pressure in apices than bases
Zones of lungs
Perfusion greatest in dependent position
Wells,CL 2016
68
10/13/2016
Zones of Perfusion
Wells,CL 2016
69
10/13/2016
Shunting
Areas were there is blood flowing by non-aerated alveoli
Shunt
Dead Space
Wells,CL 2016
70
10/13/2016
Oxygenation
Thickness & surface area
Ventilation
Alveolar condition
Oxyhemoglobin dissociation
Wells,CL 2016
71
10/13/2016
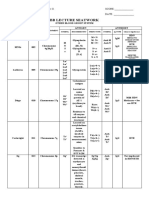
Arterial Blood Gases
pH
7.35-7.45
pCO2
35-45 mmHg
pO2
80-100 mmHg
HCO-3
22-26
O2 saturation
95-99% arterial
70-85% venous
SvO2
60-70%
Wells,CL 2016
72
10/13/2016
Pulse Oximeter
Oxygen Carrying Capability
CaO2 = (SpO2 x Hbg x 1.34) + (.003 x PaO2)
Normal 16-20 ml/O2/dL blood
Determine the accuracy
Sensing
Wave form
Heart rate
Wells,CL 2016
73
10/13/2016
Pulse Oximeter
Factors that influence accuracy
Proper sensor / fit
Cool temperature
Tremors
Finger nail polish
Artificial nails
Fungal infections
Peripheral ischemia
Hypotension
Shock
Exercise / weight bearing
Fluorescent lights
Wells,CL 2016
74
10/13/2016
Oxyhemoglobin Dissociation Curve
**
Alkalosis
Acidosis
Wells,CL 2016
75
10/13/2016
Oxyhemoglobin
Dissociation Curve
Shift to the left
Increase in hemoglobin / oxygen affinity
Hemoglobin resistant to give up the oxygen
pH: > 7.4
Causes: alkalosis
Respiratory
Metabolic
Wells,CL 2016
76
10/13/2016
Respiratory Alkalosis
Cause:
Hypoxemia
CNS stimulation
Sepsis, ASA overdose
TBI, tumor
Excessive stress
Hyperventilation
Hepatic encephalopathy
IPF
S/O:
Hypocapnia
Tachypnea
Lightheadedness
Peripheral tingling / tetany
Convulsions
Diaphoresis
Tachy-arrhythmias
Wells,CL 2016
77
10/13/2016
Metabolic Alkalosis
Cause:
Hydochloric acid
Potassium
Diarrhea
Steroids
Diuresis
NG suction
PUD
Massive blood transfusion
S/O:
Hypoventilation
MS
Agitation
Dizziness
Peripheral numbness
Muscle twitching / tetany
Convulsions
Tachy-arrhythmias
Wells,CL 2016
78
10/13/2016
Oxyhemoglobin
Dissociation Curve
Shift to the right
Decrease in hemoglobin / oxygen affinity Hemoglobin gives up oxygen more
readily
pH < 7.4
Causes: acidosis
Respiratory
Metabolic
Wells,CL 2016
79
10/13/2016
Respiratory Acidosis
Cause:
CNS injury to respiratory
center
TBI , tumor, CVA
COPD
Respiratory ms. Weakness
Flail chest
CNS depressant drugs
S/O:
Hypoventilation
Hypercapnia
Headache
Visual disturbance
Confusion, anxiety
MS, Coma
Brady-arrhythmias
VF arrest
Wells,CL 2016
80
10/13/2016
Metabolic Acidosis
Cause:
Uncontrolled DM
Starvation
Renal failure
ASA overdose
Prolonged stress
Hypoxia
Severe diarrhea
ETOH
Lactic acidosis
S/O:
Headache
MS / stupor / coma
Hyperventilation
Deep respiration
Brady-arrhythmias
Muscle twitching
N/V/D
Malaise
Wells,CL 2016
81
10/13/2016
Acid Base Balance
Normal
Range
pH
7.35-3.45
Acid
7.40 Alkaline
PaCO2 35-45
Alkaline 40
Acid
HCO-3
Acid
Alkaline
22-26
24
Wells,CL 2016
82
10/13/2016
Determining Acid Base Balance
Determine which side of the acid base balance is each value
pH 7.21
PaCO2: 67
HCO-3: 28
acid
acid
alkaline
Circle the two that are similar:
Ex:
acid
Wells,CL 2016
83
10/13/2016
Determining Acid Base Balance
To determine if the disorder is respiratory or metabolic:
Acidosis:
Respiratory: if CO2 is circled
Metabolic: if HCO-3 is circled
Alkalosis:
Respiratory: if CO2 is circled
Metabolic: if HCO-3 is circled
Ex: Respiratory
Wells,CL 2016
84
10/13/2016
Determining Acid Base Balance
To determine the extent of compensation:
Absent:
pH is OUTSIDE of normal range
One value (PaCO2 or HCO-3) is WITHIN normal range
One value (PaCO2 or HCO-3) is OUTSIDE normal range
Wells,CL 2016
85
10/13/2016
Determining Acid Base Balance
To determine the extent of compensation:
Partial:
pH is OUTSIDE normal range
PaCO2 and HCO-3 are outside normal range
Wells,CL 2016
86
10/13/2016
Determining Acid Base Balance
Complete:
pH is WITHIN normal range
One value (PaCO2 or HCO-3) is OUTSIDE normal
Second value has changed sufficiently to place pH WITHIN range
Ex: Partial Respiratory Acidosis
pH 7.21
acid
PaCO2: 67
acid
HCO-3: 28 alkaline
Wells,CL 2016
87
10/13/2016
Acid Base Balance
1. Age 57, IPF
PaO2 :
70
pH
7.47
PaCO2
25
-3
HCO
14
2. Age 15, asthma
PaO2 :
70
pH
7.50
PaCO2
28
-3
HCO
24
3. Age 71, lasix
PaO2
77
pH
7.50
PaCO2
48
-3
HCO
37
4. Age 67, COPD
PaO2 :
62
pH
7.38
PaCO2
46
-3
HCO
28
Wells,CL 2016
88
Vous aimerez peut-être aussi
- Respiratory System: The Second HalfDocument35 pagesRespiratory System: The Second HalfnicopiiPas encore d'évaluation
- Stressors That Affect Oxygen NeedsDocument40 pagesStressors That Affect Oxygen NeedsChucky VergaraPas encore d'évaluation
- Respiratory System - Tini ST 2Document67 pagesRespiratory System - Tini ST 2adlyfarisPas encore d'évaluation
- Respiratory Physiology IDocument33 pagesRespiratory Physiology IThayalan AllanPas encore d'évaluation
- Respiratory System: Azis Beru Gani 2007Document49 pagesRespiratory System: Azis Beru Gani 2007Risal MujahidinPas encore d'évaluation
- Stressors That Affect Oxygen Needs: NUR101 FALL 2008 K. Burger, Msed, MSN, RN, Cne Lecture #19Document39 pagesStressors That Affect Oxygen Needs: NUR101 FALL 2008 K. Burger, Msed, MSN, RN, Cne Lecture #19TobiDaPas encore d'évaluation
- Breathing & CirculationDocument40 pagesBreathing & CirculationRia UtamiPas encore d'évaluation
- Assessment of Respi FXDocument133 pagesAssessment of Respi FXIrish Jane GalloPas encore d'évaluation
- Sistem RespirasiDocument154 pagesSistem RespirasiStephanie Ming FunPas encore d'évaluation
- 06 Respiratory System PhysiologyDocument43 pages06 Respiratory System PhysiologyKaye Alyssa EnriquezPas encore d'évaluation
- Airway, Breathing & Circulation in Ews: Dr. Rumaisah Satyawati SP - An, KICDocument71 pagesAirway, Breathing & Circulation in Ews: Dr. Rumaisah Satyawati SP - An, KICNda ErdisPas encore d'évaluation
- CHPT 70 Respiratory Part 2Document56 pagesCHPT 70 Respiratory Part 2helen brockPas encore d'évaluation
- Ventilasi PerfusiDocument44 pagesVentilasi PerfusiIdahrachman515100% (1)
- Chapter 13 Student Version The Respiratory System 2020.ppt (1186)Document18 pagesChapter 13 Student Version The Respiratory System 2020.ppt (1186)S. MartinezPas encore d'évaluation
- Diving PhysiologyDocument334 pagesDiving PhysiologyemilidiverPas encore d'évaluation
- 1 - Respiratory Idone.Document24 pages1 - Respiratory Idone.Hinna SinghPas encore d'évaluation
- Functional Anatomy of The Respiratory SystemDocument9 pagesFunctional Anatomy of The Respiratory SystemKat ArriolaPas encore d'évaluation
- Overview Cardio-Respiratory SystemDocument20 pagesOverview Cardio-Respiratory Systemdhea wirantiPas encore d'évaluation
- Physiology of The Lungs: Ucscimed21 Fall 2016 Daria AndreevaDocument17 pagesPhysiology of The Lungs: Ucscimed21 Fall 2016 Daria Andreevajgeorge095Pas encore d'évaluation
- Critical Care Alterations in RespiratoryDocument96 pagesCritical Care Alterations in RespiratoryNatukunda DianahPas encore d'évaluation
- Respiration SystemDocument49 pagesRespiration Systemfebe_aldellaPas encore d'évaluation
- The Respiratory System 2019 dk-20191118110326Document26 pagesThe Respiratory System 2019 dk-20191118110326Jackson JastariPas encore d'évaluation
- 8respiratory SystemDocument49 pages8respiratory SystemJack OnePas encore d'évaluation
- Respiratory System & Related Disorders: by Grace Ann P. Mosqueda, RNDocument151 pagesRespiratory System & Related Disorders: by Grace Ann P. Mosqueda, RNfatevzPas encore d'évaluation
- Anatomy of Respiratory SystemDocument61 pagesAnatomy of Respiratory SystemLalu Fatria ZulhadiPas encore d'évaluation
- OXYGENATIONDocument69 pagesOXYGENATIONTina Talmadge100% (4)
- OxygenationDocument50 pagesOxygenationLulu MushiPas encore d'évaluation
- The Respiratory SystemDocument53 pagesThe Respiratory SystemShaila AliPas encore d'évaluation
- Anatomy of Respiratory SystemDocument61 pagesAnatomy of Respiratory SystemjihanPas encore d'évaluation
- PP Part 1 Respiratory AssessmentDocument14 pagesPP Part 1 Respiratory AssessmentAngela LumPas encore d'évaluation
- Pengantar Sistem RespirasiDocument23 pagesPengantar Sistem RespirasiJAQUELINEPas encore d'évaluation
- UNIT 7 RespirationDocument95 pagesUNIT 7 Respirationkrystal1994Pas encore d'évaluation
- MonitoringDocument45 pagesMonitoringضبيان فرحانPas encore d'évaluation
- DT Ventilasi MekanikDocument53 pagesDT Ventilasi MekanikRadinal MauludiPas encore d'évaluation
- Respiratory Lecture1Document43 pagesRespiratory Lecture1Angel CepedaPas encore d'évaluation
- Physiology of The Pleural SpaceDocument78 pagesPhysiology of The Pleural SpaceAhmad RafiqiPas encore d'évaluation
- Med Surg Respiratory SystemDocument173 pagesMed Surg Respiratory Systembamfalcon100% (4)
- Respiratory Physiology Summary NotesDocument63 pagesRespiratory Physiology Summary NotesAlfredII100% (1)
- Cardiovascular and Respiratory System-1Document24 pagesCardiovascular and Respiratory System-1Yujie dela cruzPas encore d'évaluation
- NCM 118Responses-to-Altered-Ventilatory-FunctionDocument169 pagesNCM 118Responses-to-Altered-Ventilatory-FunctionAddah, Dhenaraiza H.Pas encore d'évaluation
- Perubahan Fisiologik BBLDocument56 pagesPerubahan Fisiologik BBLAndi AmeliapppPas encore d'évaluation
- Respiratory FailureDocument15 pagesRespiratory FailureKennedy Ng'andwePas encore d'évaluation
- Anatomy of The Heart: Epicardium Myocardium EndocardiumDocument8 pagesAnatomy of The Heart: Epicardium Myocardium EndocardiumTrishna ShahPas encore d'évaluation
- Respiration: 1. The Respiratory Tract A. The Upper Respiratory TractDocument28 pagesRespiration: 1. The Respiratory Tract A. The Upper Respiratory TractMsKizzyPas encore d'évaluation
- A. Fisiologi RespirasiDocument48 pagesA. Fisiologi RespirasiDyandraFAPas encore d'évaluation
- Oxygen Therapy, Trach Care and SuctioningDocument44 pagesOxygen Therapy, Trach Care and SuctioningEmily Boehmer100% (1)
- Acute Respiratory Fauilr - PDF CVS PART 4Document61 pagesAcute Respiratory Fauilr - PDF CVS PART 4LexPas encore d'évaluation
- Physiology of Respiratory System-1Document29 pagesPhysiology of Respiratory System-1AYSHA ANWARPas encore d'évaluation
- Module 3 Biology NotesDocument12 pagesModule 3 Biology NotesKnock KnockPas encore d'évaluation
- Respiratory AssessmentDocument25 pagesRespiratory AssessmentLIBIN PALLUPPETTAYIL JOSE100% (2)
- CCPACatheter Basics 07 MedicineDocument44 pagesCCPACatheter Basics 07 MedicinerinbijoyPas encore d'évaluation
- Functional Human Physiology: The Respiratory SystemDocument64 pagesFunctional Human Physiology: The Respiratory SystemnashqonashPas encore d'évaluation
- Anatomy and PhysiologyDocument5 pagesAnatomy and PhysiologyKenPas encore d'évaluation
- All Lessons NotesDocument34 pagesAll Lessons NotesKiem Ashley DeluvioPas encore d'évaluation
- Respiratory System: Assessment & Disorders Dr. Mohamed IdrissDocument41 pagesRespiratory System: Assessment & Disorders Dr. Mohamed IdrissBsoom .iPas encore d'évaluation
- Pulmonary Function Tests-Nursing MasenoDocument43 pagesPulmonary Function Tests-Nursing Masenoakoeljames8543Pas encore d'évaluation
- Respiratorysystem 101228012430 Phpapp01Document69 pagesRespiratorysystem 101228012430 Phpapp01Val Angelo BugayPas encore d'évaluation
- FON oxygenationPPTDocument58 pagesFON oxygenationPPTSaeed khanPas encore d'évaluation
- Digestive SystemDocument4 pagesDigestive SystemVictoria VictoriaPas encore d'évaluation
- NCM 112 LEC Topic 2 Oxygenation Current Health History Physical Examination Normal Abnormal Breath Sounds Breathing PatternsDocument7 pagesNCM 112 LEC Topic 2 Oxygenation Current Health History Physical Examination Normal Abnormal Breath Sounds Breathing PatternsViviene Faye FombuenaPas encore d'évaluation
- Science Form 3 Collections.Document335 pagesScience Form 3 Collections.Fazil JayPas encore d'évaluation
- Digestion and Absorption Study GuideDocument6 pagesDigestion and Absorption Study GuideBritanny NelsonPas encore d'évaluation
- Resusitasi NeonatusDocument7 pagesResusitasi NeonatusIqbal Miftahul HudaPas encore d'évaluation
- Parts of The Male Reproductive SystemDocument2 pagesParts of The Male Reproductive SystemEris MolenoPas encore d'évaluation
- Blood Bank Notes Unit - 1Document4 pagesBlood Bank Notes Unit - 1princy paulPas encore d'évaluation
- Other Blood Group System AssignmentDocument5 pagesOther Blood Group System AssignmentMary ChristellePas encore d'évaluation
- MGW 5 PDFDocument26 pagesMGW 5 PDFSuhana SinghPas encore d'évaluation
- Respiratory SystemDocument18 pagesRespiratory SystemMonica NainPas encore d'évaluation
- A Clinical Guide To Pediatric SleepDocument304 pagesA Clinical Guide To Pediatric Sleepchucrallah1968Pas encore d'évaluation
- Skills LabDocument2 pagesSkills LabJessa Mae BarquillaPas encore d'évaluation
- BIO 235 Human Physiology SyllabusDocument5 pagesBIO 235 Human Physiology SyllabusKevin PhanPas encore d'évaluation
- Duke University - Medical Neuroscience - by Leonard E. White, Ph.D.Document16 pagesDuke University - Medical Neuroscience - by Leonard E. White, Ph.D.Ejogheneta OnojakePas encore d'évaluation
- Dolor Postoperatorio y Efectos Secundarios de La Uvulo Palstia Con Radiofrecuencia en Roncopatia Primaria.Document5 pagesDolor Postoperatorio y Efectos Secundarios de La Uvulo Palstia Con Radiofrecuencia en Roncopatia Primaria.Alejandro RuizPas encore d'évaluation
- Toksikologi LainDocument26 pagesToksikologi LainGigih Kenanga SariPas encore d'évaluation
- Health Effects of Sleep DeprivationDocument7 pagesHealth Effects of Sleep DeprivationEmily KajlaPas encore d'évaluation
- Modelo: Instrucciones Generales Y Calificación QuestionsDocument1 pageModelo: Instrucciones Generales Y Calificación QuestionsDA MAPas encore d'évaluation
- Lab 8Document6 pagesLab 8Naz PulatPas encore d'évaluation
- Blood Groups PPT by TKR&SRDocument24 pagesBlood Groups PPT by TKR&SRseshagiriPas encore d'évaluation
- Maharlika Highway, Brgy. Magsaysay, Lopez, Quezon: Lopez National Comprehensive High SchoolDocument5 pagesMaharlika Highway, Brgy. Magsaysay, Lopez, Quezon: Lopez National Comprehensive High SchoolJoenell CabungcalPas encore d'évaluation
- Northwestern Agusan Colleges Bayview Hill, Nasipit, Agusan Del NorteDocument2 pagesNorthwestern Agusan Colleges Bayview Hill, Nasipit, Agusan Del NortejoyPas encore d'évaluation
- An Assignment On Respiratory System and Sound SystemDocument17 pagesAn Assignment On Respiratory System and Sound SystemMD Taufique HussainPas encore d'évaluation
- An Scie Report Final1Document5 pagesAn Scie Report Final1Abas S. AcmadPas encore d'évaluation
- NormaltestreportDocument1 pageNormaltestreportTayyeb KhanPas encore d'évaluation
- Digestive and Respiratory System ExamDocument3 pagesDigestive and Respiratory System ExamAnonymous zGjXogXPas encore d'évaluation
- A-P - Ch01 - Organ Systems Overview HandoutDocument3 pagesA-P - Ch01 - Organ Systems Overview HandoutMaggie GonzalesPas encore d'évaluation
- Hemodynamic Disorders, Thrombosis, and Shock GWAIDocument102 pagesHemodynamic Disorders, Thrombosis, and Shock GWAIkavindukarunarathnaPas encore d'évaluation
- 2012 Digestive System in ManDocument52 pages2012 Digestive System in ManhueymeyPas encore d'évaluation
- Blood Transfusion SLPDocument10 pagesBlood Transfusion SLPLovesehun OhPas encore d'évaluation