Académique Documents
Professionnel Documents
Culture Documents
Management of Placenta Previa - UpToDate
Transféré par
JuanPulgarínTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Management of Placenta Previa - UpToDate
Transféré par
JuanPulgarínDroits d'auteur :
Formats disponibles
15/10/2016
ManagementofplacentapreviaUpToDate
OfficialreprintfromUpToDate
www.uptodate.com.scihub.cc2016UpToDate
Managementofplacentaprevia
Authors: CharlesJLockwood,MD,MHCM,KarenRussoStieglitz,MD
SectionEditors: DeborahLevine,MD,SusanMRamin,MD
DeputyEditor: VanessaABarss,MD,FACOG
Alltopicsareupdatedasnewevidencebecomesavailableandourpeerreviewprocessiscomplete.
Literaturereviewcurrentthrough:Sep2016.|Thistopiclastupdated:May09,2016.
INTRODUCTIONThemanagementofpregnanciescomplicatedbyplacentapreviaisbestaddressedintermsoftheclinical
setting:asymptomaticwomen,womenwhoareactivelybleeding,andwomenwhoarestableafteroneormoreepisodesofactive
bleeding.
ASYMPTOMATICPLACENTAPREVIAThemanagementgoalsinwomenwithasymptomaticplacentapreviaareto:
Determinewhetherthepreviaresolveswithincreasinggestationalage
Reducetheriskofbleeding
Reducetheriskofpretermbirth
FollowuptransvaginalultrasoundexaminationDevelopmentoftheloweruterinesegmentovertimeoftenrelocatesthe
loweredgeofamarginalorminimallyoverlyingpreviaawayfromtheinternalos.Themajorityofplacentapreviaidentifiedearlierin
pregnancywillresolvewithadvancinggestationalage.Weagreewiththeapproachofanexpertgroupformonitoringtheplacental
locationofthesepregnanciesacrossgestation[1]:
Forpregnancies>16weeks,
Iftheplacentaledgeis2cmfromtheinternalos,theplacentallocationisreportedasnormalandfollowupultrasoundfor
placentallocationisnotindicated.
Iftheplacentaledgeis<2cmfrom,butnotcovering,theinternalos,theplacentaislabeledaslowlying.Iftheplacental
edgecoverstheinternalos,theplacentaislabeledaprevia.Foreitherdiagnosis,followupultrasonographyforplacental
locationisperformedat32weeksofgestation.
Atthe32weekfollowupultrasound,
Iftheplacentaledgeis2cmfromtheinternalos,theplacentallocationisreportedasnormalandfollowupultrasoundfor
placentallocationisnotindicated.
Iftheplacentaledgeisstill<2cmfromtheinternalos(lowlying)orcoveringthecervicalos(previa),followuptransvaginal
ultrasoundisperformedat36weeks.
TransvaginalultrasonographywithcolorandpulsedDopplerisrecommendedtoruleoutplacentapreviaaswellasvasaprevia,as
resolutionofalowlyingplacentacanbeassociatedwithvasaprevia.(See"Clinicalfeatures,diagnosis,andcourseofplacenta
previa",sectionon'Ultrasoundpresentationandcourse'.)
Thesepregnanciesareatnoorminimallyincreasedriskofintrauterinegrowthrestriction.Thereisnoevidencethatspecifically
monitoringfetalgrowthwithserialultrasoundexaminationsisusefulhowever,thisinformationisgenerallyavailablesincefetal
growthisestimatedwheneverultrasoundexaminationisperformedforassessmentofplacentalposition.(See"Clinicalfeatures,
diagnosis,andcourseofplacentaprevia",sectionon'Associatedconditions'.)
PredictionofandreductionofriskofbleedingForanindividualpatient,itisnotpossibletoaccuratelypredictwhethera
bleedwilloccur,northegestationalage,volume,orfrequencyofbleeding.Sonographicfeaturesreportedtobeassociatedwitha
higherlikelihoodofbleedingincludeplacentacompletelycoveringtheos,placentawithathickedge(>1cm),placentawithanecho
freespaceintheedgeoverlappingtheos,andcervicallength3cm.(See"Clinicalfeatures,diagnosis,andcourseofplacenta
previa",sectionon'Bleeding'.)
SciHub
https://www.uptodate.com/contents/managementofplacentaprevia?source=search_result&search=placenta+previa&selected
URL,DOI,
http://www.uptodate.com.secure.scihub.cc/contents/managementofplacentaprevia/print?source=search_result&search=placenta%20previa&selectedTitle=
1/15
15/10/2016
ManagementofplacentapreviaUpToDate
Weadvisewomenwithplacentapreviatoavoidvaginalintercourseandexerciseafter20weeksofgestation(earlieriftheyhave
experiencedvaginalbleeding),andtodecreaseoverallphysicalactivityinthethirdtrimester.Therationaleisthattheseactivities
causeuterinecontractions,which,inturn,provokebleeding.Additionally,thereisconcernthatvaginalintercoursemightcause
directtraumatotheprevia,resultinginbleeding.Thereisnoevidencetoeithersupportorrefutetheserecommendations.However,
itisclearfromanecdotalexperiencethatpalpationofplacentapreviathroughapartiallydilatedcervixcanresultinsevere
hemorrhage.
Womenshouldalsobeadvisedtoseekimmediatemedicalattentionifcontractionsorvaginalbleedingoccur,giventhepotentialfor
severebleedingandneedforemergencycesareandelivery.
Itisunclearwhetherasymptomaticwomenbenefitfromhospitalizationpriortodelivery.Findingsfromobservationalstudiessuggest
thatwomenwithplacentapreviawhohavenotexperiencedanyantepartumbleedingareatlowriskofneedinganemergency
cesareandelivery[25].Thesewomencangenerallybemanagedonanoutpatientbasisuntilvaginalbleedingoccursoruntil
admissionforscheduledcesareanbirth.However,patientspecificriskfactors(eg,shortcervicallength,abilitytogettothehospital
promptlyinanemergency,homesupport)needtobetakenintoaccount.
DeliveryAworkshopheldbytheEuniceKennedyShriverNationalInstituteofChildHealthandHumanDevelopmentandthe
SocietyforMaternalFetalMedicinedevelopedconsensusrecommendationsregardingthegestationalagefordeliverytooptimize
maternal,fetalandneonataloutcomesinthesettingofvariouspregnancycomplications,includingplacentaprevia[6].They
stratifiedplacentapreviaascomplicatedoruncomplicated,whereuncomplicatedwasdefinedasnofetalgrowthrestriction,no
superimposedpreeclampsia,andnootherissuesthattakeprecedentfordeliverydecisionmaking.
Weagreewiththerecommendationsbythecommittee,whichwasbasedonavailabledataandexpertopinion,andtheAmerican
CollegeofObstetriciansandGynecologists(ACOG).Deliveryofpregnancieswithuncomplicatedplacentapreviashouldbe
accomplishedat360/7thsto376/7thsweeks,withoutdocumentationoffetallungmaturitybyamniocentesis[6,7].Therationalebehind
thisrecommendationisthattherisksassociatedwithcontinuingthepregnancy(severebleeding,emergencyunscheduleddelivery)
aregreaterthantherisksassociatedwithprematurityatthisgestationalage[6].(See"Latepreterminfants".)
Therouteofdeliveryandprocedurearedescribedbelow.(See'Route'belowand'Cesareanprocedure'below.)
ACUTECAREOFBLEEDINGPLACENTAPREVIAAnactivelybleedingplacentapreviaisapotentialobstetricalemergency.
ThesewomenshouldbeadmittedtotheLaborandDeliveryUnitformaternalandfetalmonitoring,andtheanesthesiateamshould
benotified.Themajorgoalsinmanagingthesepregnanciesareto:
Achieveand/ormaintainmaternalhemodynamicstability
Determineifcesareandeliveryisindicated
Ifthereisevidenceofpersistentseverevaginalbleeding(picture1),maternalhypotension,oranonreassuringfetalheartrate
pattern,deliveryisgenerallyexpeditedviacesareanregardlessofgestationalage.Ifbleedingisnotpersistentandsevere,the
motherishemodynamicallystableorquicklystabilized,andthefetalheartratepatternisnormal,expectantmanagementis
preferabletodeliverybefore34weeksofgestation.Tosomedegree,theseassessmentsaresubjectiveandmadeonacaseby
casebasiswhileobservingthepatientscourseonthelaborunit.Administrationofmagnesiumsulfatetopregnancies<32weeksof
gestationforneuroprotectionandacourseofantenatalcorticosteroidsmaysignificantlyimproveneonataloutcome.Thisbenefit
needstobecomparedwiththeestimatedmaternalriskfrompersistentorworseningbleeding.Theneonatalbenefitsofavoiding
expeditiousdeliverydecreasewithadvancinggestationalage,whilematernalrisksprobablyincrease.Duringtheperiodofdecision
making,everyattempttoensurematernalsafetyshouldbemade,asdescribedbelow.
Assessment
MaternalWeuseacardiacmonitorandautomatedbloodpressurecufftomonitormaternalheartrateandbloodpressure.
UrineoutputisevaluatedhourlywithaFoleycatheterattachedtoanurometer.
Accurateestimationofvaginalbloodlossisdifficulttodeterminevisually,particularlywhenbloodispartiallysaturatingorsoaking
towels,maternitypads,orgauzesponges,ordrippingontothefloor[8,9].Thefollowingtechniquesareusedforquantitatingblood
lossandcanbeusedincombination[9,10]:
Collectbloodingraduatedvolumetriccontainers.
SciHub
Useofvisualaidsthatcorrelatethesizeandappearanceofbloodonspecificsurfaces(eg,maternitypad,emesisbasin,bed
https://www.uptodate.com/contents/managementofplacentaprevia?source=search_result&search=placenta+previa&selected
sheet,lapsponge)withthevolumeofbloodabsorbedbythatsurface(picture1).Regularlyschedulingstandardizedtrainingin
URL,DOI,
theuseofthesechartscanbehelpfulforthisassessment.
http://www.uptodate.com.secure.scihub.cc/contents/managementofplacentaprevia/print?source=search_result&search=placenta%20previa&selectedTitle=
2/15
15/10/2016
ManagementofplacentapreviaUpToDate
Measurethetotalweightofbloodymaterialsandsubtracttheknownweightofthesamematerialswhendry.Thedifferencein
weightbetweenwetanddryingramsapproximatesthevolumeofbloodinmilliliters.
Forallofthesemethods,theclinicianshouldattempttoaccountforfluidsotherthanblood(eg,amnioticfluid,irrigationfluid,urine)
thatarecollectedorabsorbed.
FetalThefetalheartrateshouldbemonitored.Thepresenceoffetalhypoxiaoranemiamayresultincategory2or3fetal
heartratetracings.(See"Intrapartumfetalheartrateassessment".)
LaboratoryThereisnoconsensusaboutthecomponentsofroutinelaboratoryassessmentofpatientswithbleedingplacenta
previa[11,12].
Ataminimum,bloodshouldbesentforbaselinecompletebloodcountandtypeandantibodyscreen.Thebloodbankshould
benotifiedthatapatientwithplacentapreviahasbeenadmitted.
Whenbleedingisheavyorincreasing,deliveryislikely,ordifficultyinprocuringcompatiblebloodisanticipated,weadvise
crossmatchingtwotofourunitsofpackedredbloodcells.
Massivebloodlossorsuspicionofcoexistentabruptionshouldpromptevaluationforcoagulopathy:fibrinogenlevel,activated
partialthromboplastintime,prothrombintime.Acrudeclottingtestcanbeperformedatthebedsidebyplacing5mLofthe
patient'sbloodinatubewithnoanticoagulantfor10minutes[46].Failuretoclotwithinthistimeordissolutionofaninitialclot
impliesimpairmentofcoagulation,andissuggestiveofalowfibrinogenlevel.Prolongedoozingfromneedlepuncturesitesalso
suggestscoagulopathy.(See"Placentalabruption:Clinicalfeaturesanddiagnosis"and"Placentalabruption:Management".)
AKleihauerBetketestonaspecimenofvaginalbloodcandiagnosefetalbleedingfromdisruptionoffetalvesselsinplacentalvilli,
vasaprevia,oravelamentouscordhowever,thefetalbleedingtypicallyresultsinfetaldemiseoranonreassuringfetalheartrate
tracingnecessitatingemergencydelivery.(See"Velamentousumbilicalcordinsertionandvasaprevia".)
AntishockgarmentsAntishockgarmentshavebeenusedtorestoreadequatebloodpressureinpregnant/postpartumwomen
whoarehemodynamicallyunstableduetoseverebleedinginlowresourcesettings[1315].However,thesedeviceshavenotbeen
usedwhenthefetuswasviableandthereisnoinformationontheireffectonuteroplacentalbloodflowandthefetus.
IntravenousaccessandcrystalloidOneortwolargeboreintravenouslinesareinsertedandcrystalloid(Ringerslactateor
normalsaline)isinfusedtoachieve/maintainhemodynamicstabilityandadequateurineoutput(atleast30mL/hour).(See
"Treatmentofseverehypovolemiaorhypovolemicshockinadults".)
TransfusionTransfusionofbloodproductsinawomanwithanactivelybleedingplacentapreviashouldbeguidedbythe
volumeofbloodlossovertimeandchangesinhemodynamicparameters(eg,bloodpressure,maternalandfetalheartrates,
peripheralperfusion,andurineoutput),aswellasthehemoglobinlevel.Areasonableapproachistobeginredcelltransfusionsin
hypotensivepatientswhosebloodpressurefailstoimproveaftertwolitersofcrystalloidhavebeenrapidlyinfused.
Typesandactionsofbloodreplacementproductsareshowninthetable(table1).Thebloodbankshouldbenotifiedaboutthe
possibleneedformassivetransfusion(algorithm1).(See"Indicationsandhemoglobinthresholdsforredbloodcelltransfusionin
theadult"and"Massivebloodtransfusion".)
TocolysisTocolysisissometimesusedinpregnancieswithsymptomaticplacentapreviatoreduceoreliminateuterine
contractions,whichmaypromoteplacentalseparationandbleeding.Observationalstudiesinwomenwithsymptomaticplacenta
previasuggestthistherapymayprolongpregnancyandresultinanincreaseinbirthweight,withoutcausingadverseeffectsonthe
motherorfetus[16,17].However,itislikelythatunderlyingdifferencesinthetreatedanduntreated(control)patientsaccountedfor
thisbenefit.Furthermore,thesestudieshavegenerallynotshownadecreaseinthenumberofepisodesofhemorrhageafter
admission,thetotalamountofbloodloss,orthenumberofbloodtransfusions.Iftocolyticsareused,indomethacinhasaninhibitory
effectonplateletfunctionandthusshouldbeavoidedinwomenwithplacentapreviaduetotheriskofincreasedbloodloss.(See
"Inhibitionofacutepretermlabor".)
Wedonotadministertocolyticdrugstoactivelybleedingpatients.Wemayusetocolytics(otherthanindomethacin)tominimize
contractileactivitywhileadministeringacourseofbetamethasoneifbleedingisdiminishingorhasceasedanddeliveryisnot
otherwisemandatedbythematernalorfetalcondition.
MagnesiumsulfateWesuggestacourseofmagnesiumsulfatetherapyforneuroprotectioninpatientswithpreterm(24to32
https://www.uptodate.com/contents/managementofplacentaprevia?source=search_result&search=placenta+previa&selected
weeks)placentapreviainwhomadecisionhasbeenmadetodeliverwithin24hours,butnotemergently.Emergencydelivery
SciHub
URL,DOI,
http://www.uptodate.com.secure.scihub.cc/contents/managementofplacentaprevia/print?source=search_result&search=placenta%20previa&selectedTitle=
3/15
15/10/2016
ManagementofplacentapreviaUpToDate
becauseofmaternalorfetalstatusshouldnotbedelayedtoadministermagnesiumsulfate.(See"Neuroprotectiveeffectsofin
uteroexposuretomagnesiumsulfate".)
AntenatalcorticosteroidsAcourseofantenatalcorticosteroidtherapyshouldbeadministeredtosymptomaticwomenbetween
23and34weeksofgestationtoenhancefetalpulmonarymaturity.Wedonotadministersteroidstoasymptomaticwomen.We
wouldgiveafirstcourseofsteroidstowomenwhosefirstbleedisat>34and<37weeksofgestationandforasymptomaticwomen
whosecesareandeliveryisplannedbetween36and37completedweekswhohavenotreceivedpriorantenatalcorticosteroids.
(See"Antenatalcorticosteroidtherapyforreductionofneonatalmorbidityandmortalityfrompretermdelivery",sectionon'After34
weeks'.)
IndicationsfordeliveryCesareandeliveryisindicatedifanyofthefollowingoccur:
Anonreassuringfetalheartratetracingunresponsivetoresuscitativemeasures.(See"ManagementofintrapartumcategoryI,
II,andIIIfetalheartratetracings".)
Lifethreateningmaternalhemorrhagerefractorytostandardinterventions(transfusion,tocolysis,rest)
Significantvaginalbleedingafter34weeksofgestation
AnesthesiaGeneralanesthesiaistypicallyadministeredforemergencycesareandelivery,especiallyinhemodynamically
unstablewomenorifthefetalstatusisnonreassuring.However,regionalanesthesiaisanacceptablechoiceinhemodynamically
stablewomenwithreassuringfetalheartratetracings[1820].
Anepiduralanestheticmaybeplacedinahemodynamicallystablewoman,evenifthedecisiontodeliverisnotdefinite.The
advantageofthisapproachisthatitmayallowavoidanceofgeneralanesthesiafordelivery.Thedisadvantagesarethatthepatient
maynotbedeliveredandthecatheterwillhavetoberemoved,asubstantialhemorrhagemayinducehypotensionandthe
anestheticmayexacerbatehypotensiveendorganeffects,andgeneralanesthesiaispreferabletoepiduralanesthesiaif
hysterectomyisnecessaryatdeliverybecausetheplacentapreviaiscomplicatedbyaccretaoratonyunresponsivetoconservative
measures.
CONSERVATIVEMANAGEMENTAFTERANACUTEBLEEDMostwomenwhoinitiallypresentwithsymptomaticplacenta
previarespondtosupportivetherapyanddonotrequireimmediatedelivery[2125].Inobservationalseries,50percentofwomen
withasymptomaticprevia(anyamountofbleeding)werenotdeliveredforatleastfourweeks[22,24,25].Evenalargebleeddoes
notprecludeconservativemanagement.Inonelargeseries,50percentofwomenwhoseinitialhemorrhagicepisodeexceeded500
mLweresuccessfullymanagedwithaggressiveuseofantepartumtransfusionsandhadameanprolongationofpregnancyof17
days[21].
Managementofplacentapreviaafteracutebleedingisbaseduponfindingsfromobservationalstudiesandclinicalexperience.A
2003Cochranereviewthatattemptedtoassesstheimpactofclinicalinterventionsinthesepregnanciesconcludedtherewere
insufficientdatauponwhichtomakeevidencebasedrecommendationsforclinicalpracticeonlythreerandomizedtrialsinvolvinga
totalof114womenwereidentified[26].
Afterthepatienthasbeenstabilized,wetakethefollowingapproachwiththegoalofprolongingthepregnancy.
InpatientversusoutpatientmanagementSymptomaticwomenoftenremainhospitalizedfromtheirinitialorsecondsignificant
bleedingepisodeuntildelivery.Sincethefrequencyandseverityofrecurrentbleedingepisodesareunpredictable,maintaining
closeproximitytothelaboranddeliveryunitmayminimizetheriskofseriousmaternalorfetalcomplicationsbyenablingprompt
accesstotransfusiontherapyandemergencycesareandeliverywhenneeded.
Wedischargeselectedwomenwithplacentapreviawhosebleedinghasstoppedforaminimumof48hoursandwhohavenoother
pregnancycomplications,althoughthesafetyandefficacyofthisapproachhasnotbeenestablished[24,2729].Inouropinion,
candidatesforoutpatientcareshould:
Beabletoreturntothehospitalwithin20minutes[30].
Bereliableandabletomaintainbedrestathome.
Understandtherisksentailedbyoutpatientmanagement.
SciHub
Haveanadultcompanionavailable24hours/daywhocanimmediatelytransportthewomantothehospitalifthereislight
https://www.uptodate.com/contents/managementofplacentaprevia?source=search_result&search=placenta+previa&selected
bleedingorcallanambulanceforseverebleeding.
URL,DOI,
http://www.uptodate.com.secure.scihub.cc/contents/managementofplacentaprevia/print?source=search_result&search=placenta%20previa&selectedTitle=
4/15
15/10/2016
ManagementofplacentapreviaUpToDate
Theonlyrandomizedclinicaltrialofoutpatientversusinpatientmanagementofwomenwithplacentapreviaafterresolutionofthe
initialbleedingepisodereportedthatoutpatientcarewasnotassociatedwithgreatermorbiditythaninpatientmanagement[24].
Patientsrandomlyassignedtotheoutpatientarmwhohadarecurrentbleedweretreatedinitiallyasinpatients,andwereagain
dischargedhomeifstableafteraminimumof48to72hours.Ifthesepatientshadathirdepisodeofbleeding,theywere
hospitalizeduntildelivery.Significantdifferencesinoutcomemaynothavebeenappreciatedgiventhesmallnumberofwomen(n=
53)whoparticipatedinthistrial.
CorrectionofanemiaIronsupplementationmaybeneededforoptimalcorrectionofanemia.Stoolsoftenersandahighfiber
diethelptominimizeconstipationandavoidexcessstrainingthatmightprecipitatebleeding.(See"Treatmentofirondeficiency
anemiainadults".)
AutologousblooddonationSomewomenmayconsiderautologousblooddonation,giventhehighfrequencyofblood
transfusioninplacentaprevia.Aprogramofautologousbloodcollectionandtransfusioncandecreasetheneedforhomologous
bloodtransfusion[31].However,mostwomenwhohavebledfromaplacentaprevia,willnotmeetstandardcriteriaforautologous
donation[32,33].Autologousblooddonationissafeinstablewomenwhomeetusualcriteria(hemoglobin11.0g/dL)[31,34,35].
Somecentershaveloweredthehemoglobinthresholdto>10g/dLforpregnantwomenwithplacentapreviatoenableautologous
donationformoreofthesewomen[31].(See"Surgicalbloodconservation:Preoperativeautologousblooddonation".)
AntiDimmuneglobulinTheoretically,disruptionofthefetomaternalinterfacemayresultinfetomaternaltransfusion.Forthis
reason,preventionofRhalloimmunizationguidelinessuggestthatRh(D)negativewomenreceiveantiDimmuneglobulinfor
symptomaticplacentaprevia(ie,bleedingprevia)[36,37].ThepresenceofpositiveantiDantibodytitersonperiodicassessment
canhelpensurethatthepatientisprotectedfrompotentialalloimmunizationinthesettingofrecurrentbleeds.Readministrationis
notnecessaryifdeliveryorrebleedingoccurswithinthreeweeksofadministration,unlessalargefetomaternalhemorrhageis
detected.(See"PreventionofRh(D)alloimmunizationinpregnancy".)
FetalassessmentThereisnoprovenvalueofnonstresstestingorperformingabiophysicalprofileinpregnancieswith
asymptomaticplacentaandnoevidenceofuteroplacentalinsufficiency(eg,preeclampsia,fetalgrowthrestriction,oligohydramnios)
orotherindicationsforantepartumfetalassessment.Asdiscussedabove,activevaginalbleedingisanindicationforfetal
monitoring(see'Fetal'above).
CerclageCervicalcerclagehasbeenusedinanattempttominimizeearlydevelopmentoftheloweruterinesegment,whichis
thoughttopromoteplacentalseparation.However,theefficacyofthisapproachisunproven.Althoughametaanalysisoftwo,small
randomizedtrialsthatevaluatedcerclageforimprovingpregnancyoutcomeinplacentaprevia[38,39]reportedthatcervical
cerclagereducedtheriskofdeliverybefore34weeks(RR0.45,95%CI0.230.87)andthebirthofababyweighinglessthan2000
g(RR0.34,95%CI0.140.83),thelackofconsistencybetweentrialsandmethodologicalissuespreventmakingaclearconclusion
ofbenefit[26].Intheabsenceofhighqualityevidenceofefficacyandsafety,weadvisenotperformingprophylacticcerclageto
improvepregnancyoutcomeinplacentaprevia.However,thepresenceofastableplacentapreviaisnotacontraindicationto
cerclageplacementwhenindicatedforcervicalinsufficiency.(See"Cervicalinsufficiency".)
PretermprematureruptureofmembranesAntepartumdecidualhemorrhageisamajorriskfactorforpretermpremature
ruptureofmembranes(PPROM).PPROMcanoccurdespitethepresenceofacompleteplacentaprevia.Inthesecases,each
conditionismanagedindependently.(See"Pretermpremature(prelabor)ruptureofmembranes".)
Delivery
TimingTimingofdeliverydependsonthepatientsstatus.
Deliveryofpatientswithstable(nobleedingorminimalbleeding)placentapreviashouldbeaccomplishedat36to37weeks,without
documentationoffetallungmaturitybyamniocentesis(see'Delivery'above).
Deliveryisindicatedemergentlyifanyofthefollowingoccur(see'Indicationsfordelivery'above):
Anyvaginalbleedingwithanonreassuringfetalheartratetracingunresponsivetoresuscitativemeasures
Lifethreateningrefractorymaternalhemorrhage
Labor
Inwomenwithmoderatevaginalbleeding>34weeksorprogressivelyincreasingfrequencyorvolumeofbleedingaftercessationof
aninitialbleed,wedeliverthepatientifshehaspreviouslyreceivedacourseofbetamethasoneanytimeduringthepregnancy.If
https://www.uptodate.com/contents/managementofplacentaprevia?source=search_result&search=placenta+previa&selected
sheisclinicallystableandhasnotreceivedacourseofbetamethasonebecauseherfirstbleedingepisodeoccurredafter34weeks
andbefore37weeks,weadministeracourseofsteroidsandthenperformcesareandeliveryin48hours,basedonlimiteddatathat
URL,DOI,
SciHub
http://www.uptodate.com.secure.scihub.cc/contents/managementofplacentaprevia/print?source=search_result&search=placenta%20previa&selectedTitle=
5/15
15/10/2016
ManagementofplacentapreviaUpToDate
evenlateingestationneonatalrespiratoryproblemsmaybereducedwithsteroiduse.(See"Antenatalcorticosteroidtherapyfor
reductionofneonatalmorbidityandmortalityfrompretermdelivery".)
Route
PreviaAcesareandeliveryisalwaysindicatedwhenthereissonographicevidenceofacompleteplacentapreviaanda
viablefetus.Vaginaldeliverymaybeconsideredinrarecircumstances,suchasinthepresenceofafetaldemiseorapreviable
fetus,aslongasthemotherremainshemodynamicallystable.
Whentheplacentareachestheinternalosbutdoesnotcrossit,ithasbeenhypothesizedthatvaginaldeliverycanoccasionallybe
performedbecausethefetalheadtamponadestheadjacentplacenta,thuspreventinghemorrhage.Thesepregnanciesremainat
highriskofintrapartumhemorrhagetherefore,wesuggestscheduledcesareandeliverytominimizetheriskofemergentdelivery
andneedfortransfusion.
LowplacentaRatesofcesareandeliveryandantepartumbleedingdecreaseasthedistancebetweentheplacentaledge
andinternalosincreases.Thereisageneralconsensusofareasonablepossibilityofvaginaldeliverywithouthemorrhagewhenthe
placentaismorethan20mmfromtheinternalos,soatrialoflaborisappropriateiftherearenoothercontraindicationstovaginal
birth[4045].Whenthisdistanceisbetween1and20mm,therateofcesareandeliveryrangesfrom40to90percent,so
managementofthesepatientsismorecontroversial.Oneofthelargerretrospectivestudiesthatlookedattheoutcomeofthis
specificgroupofpregnanciesreportedvaginalbirthin6/24(25percent)womenwithacervixtoplacentadistanceof1to10mm
andin20/29(69percent)womenwithcervixtoplacentadistanceof11to20mm[46].Althoughavarietyoffactorsinfluencedthe
decisiontoperformcesareandelivery,thesedatasupportallowingatrialoflaborinpregnanciesinwhichtheplacentaismorethan
10mmfromtheinternalos.
CesareanprocedureTwotofourunitsofpackedredbloodcellsshouldbeavailableforthedelivery.Appropriatesurgical
instrumentsforperformanceofacesareanhysterectomyshouldalsobeavailablesincethesepatientsareatincreasedriskof
placentaaccreta,evenintheabsenceofapriorcesareandelivery.Evaluationforplacentapreviaaccretashouldhavebeen
performedantenatally,withappropriatepreparationsformanagement,ifpresent.(See"Clinicalfeatures,diagnosis,andcourseof
placentaprevia",sectionon'Associatedconditions'and"Clinicalfeaturesanddiagnosisofthemorbidlyadherentplacenta(placenta
accreta,increta,andpercreta)"and"Managementofthemorbidlyadherentplacenta(placentaaccreta,increta,andpercreta)"and
"Peripartumhysterectomyformanagementofhemorrhage".)
Thesurgeonshouldtrytoavoiddisruptingtheplacentawhenenteringtheuterus.Iftheplacentaisincised,hemorrhagefromfetal
vesselscanresultinsignificantneonatalanemia.Preoperativeorintraoperativesonographiclocalizationishelpfulindetermining
thepositionofthehysterotomyincision(forintraoperativeimaging,thetransducerisplacedinasterilebagandsleeve).Ifthe
placentaisinananterolaterallocation,averticalincisioncanbemadeintheloweruterinesegmentontheoppositesidefromthe
placenta.Iftheplacentawrapsaroundthecervixfromtheanteriortoposteriorloweruterinesegmentinthemidline,atransverseor
verticalincisionmaybepossibleaboveit[47,48],althoughthisoftenresultsinextensionintotheupperuterinesegment.When
incisionoftheplacentaisunavoidable,theinfantshouldbedeliveredrapidlyandthecordpromptlyclamped.
ManagementofhemorrhageAfterdeliveryoftheplacenta,severebleedingmayoccurfromtheplacentalbed.Standard
interventionsformanagementofpostpartumhemorrhageshouldbeperformed,andmayincludeplacementofendouterine
hemostaticsquaresutures,intrauterineballoontamponade,and/orplacementofuterinecompressionsutures[4951].(See
"Managementofpostpartumhemorrhageatcesareandelivery".)
Inaddition,vasopressininjectionattheplacentalsitemaybebeneficial[52,53].Inonereview,localinjectionof4unitsof
vasopressinin20mLofsalineintotheplacentalimplantationsitesignificantlyreducedbloodlosswithoutincreasingthemorbidity
[53].TheauthorsnotedthatthevasopressinV1receptorwashighlyexpressedinsmoothmusclecellsinthelowersegmentofthe
uterus.Inacasereport,5unitsofvasopressinin20mLsalineinjectedin1to2mLamountsintotheareaofplacentalimplantation
stoppedbleedingwithin90seconds[52].Useofthistechnique,whilebiologicallyplausibleandpotentiallyclinicallyrelevant,is
consideredanecdotal.
PREGNANCYTERMINATIONINWOMENWITHPLACENTAPREVIACliniciansshoulddiscusswithpatientsthevarious
optionsforpregnancyterminationinthesettingofplacentaprevia(eg,hysterotomy,dilationandevacuation,useofabortifacient)
anddocumentthediscussioninthemedicalrecord.Thepresenceofaplacentapreviadoesnotprecludesecondtrimester
pregnancyterminationbystandardtechniques,althoughdataarelimitedtoafewstudies[5457].
SciHub
Oneseriesof131consecutivewomenundergoingelectivepregnancyterminationbydilationandevacuation(D&E)after
https://www.uptodate.com/contents/managementofplacentaprevia?source=search_result&search=placenta+previa&selected
laminariaplacementat13to24weeksofgestationcomparedtheoutcomeofthosewith(n=23)andwithoutplacentaprevia
URL,DOI,
baseduponanultrasoundexaminationbeforetheprocedure[54].Womenwithaplacentapreviahadgreaterintraoperative
http://www.uptodate.com.secure.scihub.cc/contents/managementofplacentaprevia/print?source=search_result&search=placenta%20previa&selectedTitle=
6/15
15/10/2016
ManagementofplacentapreviaUpToDate
bloodloss(21mL),butnosignificantincreaseinoperativetime,timetodischarge,infection,hemorrhage,orother
complications.
Thesecondseriesconsistedof306consecutivewomenundergoingpregnancyterminationbyD&Eat19to24weeks[55].An
ultrasounddiagnosisofcompletepreviawasmadeineightpatients.Noneofthesewomenhadexcessivebleedingwith
laminariainsertionorrequiredbloodtransfusionduetoprocedurerelatedhemorrhage.Operativetimewascomparableto
womenwithoutcompleteprevia.
Thethirdseriesincluded15secondorthirdtrimesterterminationsofpregnancybyadministrationofsystemicabortifacientsin
womenwithcompleteprevia[56].Preinductionfeticidewasperformed2to14dayspriortotheprocedure.Fourofninewomen
whounderwentlaborinductionwithoutpreviousfeticiderequiredbloodtransfusionsandonerequiredhysterectomynoneof
thesixpatientswithpreinductionfeticiderequiredtransfusion.Theauthorsconcludedthatpreinductionfeticidemighthelpto
reducebloodlossinthesecases.
Thefourthseriesincluded158womenundergoingsecondtrimesterterminationinwhom11hadplacentaprevia,4underwentD&E
and7hadgemeprosttermination[57].Therewasnostatisticaldifferenceinmeanintraoperativebloodlossbetweenthesegroups
andcontrolswithoutprevia,butonewomanwithplacentapreviawhounderwentgemeprostterminationdevelopedseriousbleeding
requiringbloodtransfusion.
INFORMATIONFORPATIENTSUpToDateofferstwotypesofpatienteducationmaterials,"TheBasics"and"Beyondthe
Basics."TheBasicspatienteducationpiecesarewritteninplainlanguage,atthe5thto6thgradereadinglevel,andtheyanswerthe
fourorfivekeyquestionsapatientmighthaveaboutagivencondition.Thesearticlesarebestforpatientswhowantageneral
overviewandwhoprefershort,easytoreadmaterials.BeyondtheBasicspatienteducationpiecesarelonger,moresophisticated,
andmoredetailed.Thesearticlesarewrittenatthe10thto12thgradereadinglevelandarebestforpatientswhowantindepth
informationandarecomfortablewithsomemedicaljargon.
Herearethepatienteducationarticlesthatarerelevanttothistopic.Weencourageyoutoprintoremailthesetopicstoyour
patients.(Youcanalsolocatepatienteducationarticlesonavarietyofsubjectsbysearchingonpatientinfoandthekeyword(s)of
interest.)
Basicstopics(see"Patienteducation:Placentaprevia(TheBasics)")
SUMMARYANDRECOMMENDATIONS
Asymptomaticprevia
Inpregnancieswithasymptomaticplacentaprevia,wemonitorplacentalpositionwithultrasoundexaminationasanoutpatient
andcounselthesepatientstoavoidexcessphysicalactivityandtocalltheirproviderpromptlyifbleedingorlaboroccurs.We
performcesareandeliveryat36to37weeks.(See'Asymptomaticplacentaprevia'above.)
Acutemanagementofbleedingprevia
Anactivelybleedingplacentapreviaisapotentialobstetricalemergency.Womenwithactivebleedingarehospitalizedforclose
maternalandfetalmonitoringandsupportivecare.Indicationsforemergencycesareandeliveryincluderefractorylife
threateningmaternalhemorrhage,nonreassuringfetalstatus,andsignificantvaginalbleedingafter34weeksofgestation.(See
'Acutecareofbleedingplacentaprevia'above.)
Conservativemanagementafteranacutebleed
Afterableedingepisodehasresolved,outpatientmanagementofselectwomenisreasonable.Thesewomenshouldbeableto
returntothehospitalquicklyifrebleedingoccursandshouldnothaveadditionalpregnancycomplications.(See'Conservative
managementafteranacutebleed'above.)
Werecommendacourseofantenatalcorticosteroidtherapyforsymptomaticpatientsbetween23and34weeksofgestationto
enhancefetalpulmonarymaturity(Grade1A).Wewouldgiveafirstcourseofsteroids(butnotasecondcourse)towomen
whosefirstbleedisat>34weeksandtoasymptomaticwomen>34weeksinwhomcesareandeliveryisplannedbetween36
and37weeks.WealsorecommendantiDimmuneglobulinforsymptomaticRh(D)negativewomentopreventpossible
alloimmunization(Grade1B).ReadministrationofantiDimmuneglobulinisnotnecessaryifdeliveryorrebleedingoccurs
withinthreeweeks,unlessalargefetomaternalhemorrhageisdetected.(See'Antenatalcorticosteroids'aboveand'AntiD
immuneglobulin'above.) https://www.uptodate.com/contents/managementofplacentaprevia?source=search_result&search=placenta+previa&selected
SciHub
URL,DOI,
http://www.uptodate.com.secure.scihub.cc/contents/managementofplacentaprevia/print?source=search_result&search=placenta%20previa&selectedTitle=
7/15
15/10/2016
ManagementofplacentapreviaUpToDate
Weschedulecesareandeliveryat36to37weeks.(See'Timing'above.)Incisionoftheplacentashouldbeavoided,asthis
increasestheriskoffetalhemorrhage.(See'Cesareanprocedure'above.)
Vaginaldeliverymaybeattemptedwhentheplacentaledgeis>10mmfromtheinternalosbecausetheriskofhemorrhage
duringlaborismuchlower.(See'Lowplacenta'above.)
UseofUpToDateissubjecttotheSubscriptionandLicenseAgreement.
REFERENCES
1.ReddyUM,AbuhamadAZ,LevineD,etal.Fetalimaging:executivesummaryofajointEuniceKennedyShriverNational
InstituteofChildHealthandHumanDevelopment,SocietyforMaternalFetalMedicine,AmericanInstituteofUltrasoundin
Medicine,AmericanCollegeofObstetriciansandGynecologists,AmericanCollegeofRadiology,SocietyforPediatric
Radiology,andSocietyofRadiologistsinUltrasoundFetalImagingworkshop.ObstetGynecol2014123:1070.
2.LamCM,WongSF,ChowKM,HoLC.Womenwithplacentapraeviaandantepartumhaemorrhagehaveaworseoutcome
thanthosewhodonotbleedbeforedelivery.JObstetGynaecol200020:27.
3.LoveCD,FernandoKJ,SargentL,HughesRG.Majorplacentapraeviashouldnotprecludeoutpatientmanagement.EurJ
ObstetGynecolReprodBiol2004117:24.
4.RosenDM,PeekMJ.Dowomenwithplacentapraeviawithoutantepartumhaemorrhagerequirehospitalization?AustNZJ
ObstetGynaecol199434:130.
5.OnonezeBO,OnonezeVN,HolohanM.Managementofwomenwithmajorplacentapraeviawithouthaemorrhage:a
questionnairebasedsurveyofIrishobstetricians.JObstetGynaecol200626:620.
6.SpongCY,MercerBM,D'altonM,etal.Timingofindicatedlatepretermandearlytermbirth.ObstetGynecol2011118:323.
7.AmericanCollegeofObstetriciansandGynecologists.ACOGcommitteeopinionno.560:Medicallyindicatedlatepretermand
earlytermdeliveries.ObstetGynecol2013121:908.
8.YoongW,KaravolosS,DamodaramM,etal.Observeraccuracyandreproducibilityofvisualestimationofbloodlossin
obstetrics:howaccurateandconsistentarehealthcareprofessionals?ArchGynecolObstet2010281:207.
9.BoseP,ReganF,PatersonBrownS.Improvingtheaccuracyofestimatedbloodlossatobstetrichaemorrhageusingclinical
reconstructions.BJOG2006113:919.
10.LyndonA,MillerS,HuweV,RosenM,etal.Bloodloss:Clinicaltechniquesforongoingquantitativemeasurement.California
MaternalQualityCareCollaborative.CMQCCObstetricHemorrhageToolkit1/6/2010.
11.GoodnoughLT,DanielsK,WongAE,etal.Howwetreat:transfusionmedicinesupportofobstetricservices.Transfusion
201151:2540.
12.AmericanSocietyofAnesthesiologistsTaskForceonObstetricAnesthesia.Practiceguidelinesforobstetricanesthesia:an
updatedreportbytheAmericanSocietyofAnesthesiologistsTaskForceonObstetricAnesthesia.Anesthesiology2007
106:843.
13.MillerS,MartinHB,MorrisJL.Antishockgarmentinpostpartumhaemorrhage.BestPractResClinObstetGynaecol2008
22:1057.
14.MillerS,OjengbedeO,TuranJM,etal.Acomparativestudyofthenonpneumaticantishockgarmentforthetreatmentof
obstetrichemorrhageinNigeria.IntJGynaecolObstet2009107:121.
15.MillerS,FathallaMM,YoussifMM,etal.Acomparativestudyofthenonpneumaticantishockgarmentforthetreatmentof
obstetrichemorrhageinEgypt.IntJGynaecolObstet2010109:20.
16.BesingerRE,MoniakCW,PaskiewiczLS,etal.Theeffectoftocolyticuseinthemanagementofsymptomaticplacentaprevia.
AmJObstetGynecol1995172:1770.
17.SharmaA,SuriV,GuptaI.Tocolytictherapyinconservativemanagementofsymptomaticplacentaprevia.IntJGynaecol
Obstet200484:109.
18.FrederiksenMC,GlassenbergR,StikaCS.Placentaprevia:a22yearanalysis.AmJObstetGynecol1999180:1432.
19.HongJY,JeeYS,YoonHJ,KimSM.Comparisonofgeneralandepiduralanesthesiainelectivecesareansectionforplacenta
previatotalis:maternalhemodynamics,bloodlossandneonataloutcome.IntJObstetAnesth200312:12.
https://www.uptodate.com/contents/managementofplacentaprevia?source=search_result&search=placenta+previa&selected
SciHub
URL,DOI,
http://www.uptodate.com.secure.scihub.cc/contents/managementofplacentaprevia/print?source=search_result&search=placenta%20previa&selectedTitle=
8/15
15/10/2016
ManagementofplacentapreviaUpToDate
20.ParekhN,HusainiSW,RussellIF.Caesareansectionforplacentapraevia:aretrospectivestudyofanaestheticmanagement.
BrJAnaesth200084:725.
21.CottonDB,ReadJA,PaulRH,QuilliganEJ.Theconservativeaggressivemanagementofplacentaprevia.AmJObstet
Gynecol1980137:687.
22.SilverR,DeppR,SabbaghaRE,etal.Placentaprevia:aggressiveexpectantmanagement.AmJObstetGynecol1984
150:15.
23.FarineD,PeisnerDB,TimorTritschIE.Placentapreviaisthetraditionaldiagnosticapproachsatisfactory?JClinUltrasound
199018:328.
24.WingDA,PaulRH,MillarLK.Managementofthesymptomaticplacentaprevia:arandomized,controlledtrialofinpatient
versusoutpatientexpectantmanagement.AmJObstetGynecol1996175:806.
25.PlacentaAccreta,ACOGCommitteeOpinion2002266:169.
26.NeilsonJP.Interventionsforsuspectedplacentapraevia.CochraneDatabaseSystRev2003:CD001998.
27.MouerJR.Placentaprevia:antepartumconservativemanagement,inpatientversusoutpatient.AmJObstetGynecol1994
170:1683.
28.DrosteS,KeilK.Expectantmanagementofplacentaprevia:costbenefitanalysisofoutpatienttreatment.AmJObstet
Gynecol1994170:1254.
29.D'AngeloLJ,IrwinLF.Conservativemanagementofplacentaprevia:acostbenefitanalysis.AmJObstetGynecol1984
149:320.
30.RavelliAC,JagerKJ,deGrootMH,etal.Traveltimefromhometohospitalandadverseperinataloutcomesinwomenatterm
intheNetherlands.BJOG2011118:457.
31.YamadaT,MoriH,UekiM.Autologousbloodtransfusioninpatientswithplacentaprevia.ActaObstetGynecolScand2005
84:255.
32.DinsmoorMJ,HoggBB.Autologousblooddonationwithplacentaprevia:isitfeasible?AmJPerinatol199512:382.
33.ToedtME.Feasibilityofautologousblooddonationinpatientswithplacentaprevia.JFamPract199948:219.
34.WatanabeN,SuzukiT,OgawaK,etal.Fiveyearstudyassessingthefeasibilityandsafetyofautologousbloodtransfusionin
pregnantJapanesewomen.JObstetGynaecolRes201137:1773.
35.YamamotoY,YamashitaT,TsunoNH,etal.Safetyandefficacyofpreoperativeautologousblooddonationforhighrisk
pregnantwomen:experienceofalargeuniversityhospitalinJapan.JObstetGynaecolRes201440:1308.
36.FungKeeFungK,EasonE,CraneJ,etal.PreventionofRhalloimmunization.JObstetGynaecolCan200325:765.
37.ACOGpracticebulletin.PreventionofRhDalloimmunization.Number4,May1999(replaceseducationalbulletinNumber
147,October1990).Clinicalmanagementguidelinesforobstetriciangynecologists.AmericanCollegeofObstetricsand
Gynecology.IntJGynaecolObstet199966:63.Reaffirmed2016.
38.AriasF.Cervicalcerclageforthetemporarytreatmentofpatientswithplacentaprevia.ObstetGynecol198871:545.
39.CoboE,CondeAgudeloA,DelgadoJ,etal.Cervicalcerclage:analternativeforthemanagementofplacentaprevia?AmJ
ObstetGynecol1998179:122.
40.BhideA,PrefumoF,MooreJ,etal.Placentaledgetointernalosdistanceinthelatethirdtrimesterandmodeofdeliveryin
placentapraevia.BJOG2003110:860.
41.OppenheimerLW,FarineD,RitchieJW,etal.Whatisalowlyingplacenta?AmJObstetGynecol1991165:1036.
42.DawsonWB,DumasMD,RomanoWM,etal.Translabialultrasonographyandplacentaprevia:doesmeasurementoftheos
placentadistancepredictoutcome?JUltrasoundMed199615:441.
43.OyeleseY,SmulianJC.Placentaprevia,placentaaccreta,andvasaprevia.ObstetGynecol2006107:927.
44.PredanicM,PerniSC,BaergenRN,etal.Asonographicassessmentofdifferentpatternsofplacentaprevia"migration"inthe
thirdtrimesterofpregnancy.JUltrasoundMed200524:773.
45.BronsteenR,ValiceR,LeeW,etal.Effectofalowlyingplacentaondeliveryoutcome.UltrasoundObstetGynecol2009
33:204.
46.VerganiP,OrnaghiS,PozziI,etal.Placentaprevia:distancetointernalosandmodeofdelivery.AmJObstetGynecol2009
https://www.uptodate.com/contents/managementofplacentaprevia?source=search_result&search=placenta+previa&selected
201:266.e1.
SciHub
URL,DOI,
http://www.uptodate.com.secure.scihub.cc/contents/managementofplacentaprevia/print?source=search_result&search=placenta%20previa&selectedTitle=
9/15
15/10/2016
ManagementofplacentapreviaUpToDate
47.KayemG,DavyC,GoffinetF,etal.Conservativeversusextirpativemanagementincasesofplacentaaccreta.ObstetGynecol
2004104:531.
48.KotsujiF,NishijimaK,KurokawaT,etal.Transverseuterinefundalincisionforplacentapraeviawithaccreta,involvingthe
entireanterioruterinewall:acaseseries.BJOG2013120:1144.
49.YoongW,RidoutA,MemtsaM,etal.Applicationofuterinecompressionsutureinassociationwithintrauterineballoon
tamponade('uterinesandwich')forpostpartumhemorrhage.ActaObstetGynecolScand201291:147.
50.MatsubaraS,KuwataT,BabaY,etal.Anovel'uterinesandwich'forhaemorrhageatcaesareansectionforplacentapraevia.
AustNZJObstetGynaecol201454:283.
51.KavakSB,AtilganR,DemirelI,etal.Endouterinehemostaticsquaresuturevs.Bakriballoontamponadeforintractable
hemorrhageduetocompleteplacentaprevia.JPerinatMed201341:705.
52.ZakiZM,BaharAM.Massivehaemorrhageduetoplacentapraeviaaccreta:ausefulroleforvasopressin.JObstetGynaecol
199717:486.
53.KatoS,TanabeA,KankiK,etal.Localinjectionofvasopressinreducesthebloodlossduringcesareansectioninplacenta
previa.JObstetGynaecolRes2014.
54.ThomasAG,AlvarezM,FriedmanFJr,etal.Theeffectofplacentapreviaonbloodlossinsecondtrimesterpregnancy
termination.ObstetGynecol199484:58.
55.HalperinR,VakninZ,LangerR,etal.Latemidtrimesterpregnancyterminationinthepresenceofplacentaprevia.JReprod
Med200348:175.
56.RuanoR,DumezY,CabrolD,DommerguesM.Secondandthirdtrimestertherapeuticterminationsofpregnancyincases
withcompleteplacentapreviadoesfeticidedecreasepostdeliverymaternalhemorrhage?FetalDiagnTher200419:475.
57.NakayamaD,MasuzakiH,MiuraK,etal.Effectofplacentapreviaonbloodlossinsecondtrimesterabortionbylabor
inductionusinggemeprost.Contraception200775:238.
Topic6809Version22.0
SciHub
https://www.uptodate.com/contents/managementofplacentaprevia?source=search_result&search=placenta+previa&selected
URL,DOI,
http://www.uptodate.com.secure.scihub.cc/contents/managementofplacentaprevia/print?source=search_result&search=placenta%20previa&selectedTitle
10/15
15/10/2016
ManagementofplacentapreviaUpToDate
GRAPHICS
Visualaidforestimatingintrapartumbloodloss
Visualaid.Pocketcardwithimagesofmeasuredvolumesofartificialblood.
From:ZuckerwiseLC,PettkerCM,IlluzziJ,etal.Useofanovelvisualaidtoimproveestimationofobstetricbloodloss.ObstetGynecol2014
123:982.DOI:10.1097/AOG.0000000000000233.ReproducedwithpermissionfromLippincottWilliams&Wilkins.Copyright2014American
CollegeofObstetriciansandGynecologists.Unauthorizedreproductionofthismaterialisprohibited.
Graphic103418Version1.0
SciHub
https://www.uptodate.com/contents/managementofplacentaprevia?source=search_result&search=placenta+previa&selected
URL,DOI,
http://www.uptodate.com.secure.scihub.cc/contents/managementofplacentaprevia/print?source=search_result&search=placenta%20previa&selectedTitle
11/15
15/10/2016
ManagementofplacentapreviaUpToDate
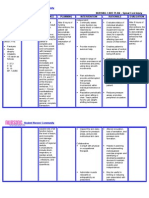
Bloodcomponents:Indicationsanddosinginadults
Component(volume)
Contents
Indicationsanddose
Wholeblood(1unit=500
mL)
RBCs,platelets,plasma
Rarelyrequired.Maybeappropriatewhenmassivebleedingrequirestransfusion
ofmorethan5to7unitsofRBCs.
Redbloodcells(RBCs)in
additivesolution,alsocalled
packedRBCs(1unit=350
mL)
RBCs
Anemia,bleeding.Oneunitincreasesthehemoglobinbyapproximately1g/dL
andthehematocritbyapproximately3percentagepoints.
FreshFrozenPlasma(FFP)*
(1unit=200to300mL)
Allsolubleplasma
proteinsandclotting
factors
Bleedingorexpectedbleeding(eg,emergencysurgery)inindividualswith
deficienciesofmultiplecoagulationfactors(eg,DIC,liverdisease,massive
transfusion,anticoagulationwithwarfarinorothervitaminKantagonist,warfarin
overdose)therapeuticplasmaexchangeinTTP.OneunitofFFPincreasesthe
plasmafibrinogenby7to10mg/dL.Ausualdoseis10to15mL/kg.Mayalsobe
usedinindividualswithisolatedfactordeficienciesifafactorconcentrateor
recombinantfactorisunavailable.
Cryoprecipitate,also
called"cryo"(1unit=10to
20mL)
FibrinogenfactorsVIII
andXIIIVWF
Bleedingorexpectedbleedingwithlowfibrinogen:oneunitofcryoprecipitateper
10kgbodyweightwillraisetheplasmafibrinogenbyapproximately50mg/dL.
BleedingorexpectedbleedinginindividualswithdeficienciesoffactorXIIIor
factorVIII(hemophiliaA)ifarecombinantproductorfactorconcentrateis
unavailable.
BleedingorexpectedbleedinginindividualswithVWDifDDAVPisineffectiveand
recombinantVWForaVWFconcentrateisunavailable.
Cryoprecipitateisgenerallyprovidedinpoolscontaining5unitsandmost
patientsreceivetwopools.
Platelets(derivedfrom
wholebloodorapheresis)
(1unit=200to300mL)
Platelets
Sixunitsofwholebloodderivedplateletsoroneunitofapheresisderived
plateletswillraisetheplateletcountbyapproximately30,000/microLinan
averagesizedadult.
RefertoUpToDatetopicsontheseproductsandonspecificconditionsfordetailsofuse.Frozenbloodproducts(FFP,Cryoprecipitate)take
10to30minutestothaw.Itmaytakethesameamountoftimetoperformanuncomplicatedcrossmatch.
*Otherplasmaproductsmaybesubstituted,includingPlasmaFrozenWithin24HoursAfterPhlebotomy(PF24)orThawedPlasma.
DIC:disseminatedintravascularcoagulationFFP:freshfrozenplasmakg:kilogramsTTP:thromboticthrombocytopenicpurpuraVWD:von
WillebranddiseaseVWF:vonWillebrandfactor.
Graphic53854Version11.0
SciHub
https://www.uptodate.com/contents/managementofplacentaprevia?source=search_result&search=placenta+previa&selected
URL,DOI,
http://www.uptodate.com.secure.scihub.cc/contents/managementofplacentaprevia/print?source=search_result&search=placenta%20previa&selectedTitle
12/15
15/10/2016
ManagementofplacentapreviaUpToDate
Samplemassivetransfusionalgorithm
TexasChildren'sPavilionforWomenmassivetransfusionprotocol.
MTP:massivetransfusionprotocolPRBC:packedredbloodcellsPCA:patientcontrolledanalgesia
RRT:rapidresponseteamBB:bloodbankHg:hemoglobinHct:hematocritDIC:disseminated
intravascularcoagulationPT:prothrombintimeINR:internationalnormalizedratioPTT:partial
thromboplastintimeABG:arterialbloodgasRBC:redbloodcellsFFP:freshfrozenplasmaOB:
ObstetricsAnes:AnesthesiaOR:operatingroomCRNA:certifiedregisterednurseanesthetistChrg:
chargeRN:registerednurseLab:laboratoryTech:technicianMD:medicaldoctorL&D:laborand
deliveryiCa:ionizedcalciumK:potassiumGlu:glucosePCA:patientcareassistant.
*Everytwopackagesorbasedonlabresults.
Reproducedwithpermission.AccessedonFebruary19,2013.CopyrightEvidenceBasedOutcomes
Center,2013.QualityandOutcomesCenter,TexasChildren'sHospital.Thisguidelinewaspreparedbythe
EvidenceBasedOutcomesCenter(EBOC)teamincollaborationwithcontentexpertsatTexasChildren's
HospitalPavilionforWomen.DevelopmentofthisguidelinesupportstheTCHQualityandPatientSafety
Programinitiativetopromoteclinicalguidelinesandoutcomesthatbuildacultureofqualityandsafety
withintheorganization.Guidelinerecommendationsaremadefromthebestevidence,clinicalexpertise
andconsensus,inadditiontothoughtfulconsiderationforthepatientsandfamiliescaredforwithinthe
https://www.uptodate.com/contents/managementofplacentaprevia?source=search_result&search=placenta+previa&selected
IntegratedDeliverySystem.Whenevidencewaslackingorinconclusive,contentexpertsmadeconsensus
recommendations.Expertconsensusisimpliedwhenareferenceisnototherwiseindicated.Theguideline
SciHub
URL,DOI,
http://www.uptodate.com.secure.scihub.cc/contents/managementofplacentaprevia/print?source=search_result&search=placenta%20previa&selectedTitle
13/15
15/10/2016
ManagementofplacentapreviaUpToDate
isnotintendedtoimposestandardsofcarepreventingselectivevariationinpracticethatisnecessaryto
meettheuniqueneedsofindividualpatients.Thephysicianmustconsidereachpatientandfamily's
circumstancetomaketheultimatejudgmentregardingbestcare.
Graphic91236Version4.0
SciHub
https://www.uptodate.com/contents/managementofplacentaprevia?source=search_result&search=placenta+previa&selected
URL,DOI,
http://www.uptodate.com.secure.scihub.cc/contents/managementofplacentaprevia/print?source=search_result&search=placenta%20previa&selectedTitle
14/15
15/10/2016
ManagementofplacentapreviaUpToDate
ContributorDisclosures
CharlesJLockwood,MD,MHCM Consultant/AdvisoryBoards:Celula[Aneuploidyscreening(Nocurrentproductsordrugsinthe
US)]. KarenRussoStieglitz,MD Nothingtodisclose DeborahLevine,MD Nothingtodisclose SusanMRamin,MD Nothingto
disclose VanessaABarss,MD,FACOG Nothingtodisclose
Contributordisclosuresarereviewedforconflictsofinterestbytheeditorialgroup.Whenfound,theseareaddressedbyvetting
throughamultilevelreviewprocess,andthroughrequirementsforreferencestobeprovidedtosupportthecontent.Appropriately
referencedcontentisrequiredofallauthorsandmustconformtoUpToDatestandardsofevidence.
Conflictofinterestpolicy
SciHub
https://www.uptodate.com/contents/managementofplacentaprevia?source=search_result&search=placenta+previa&selected
URL,DOI,
http://www.uptodate.com.secure.scihub.cc/contents/managementofplacentaprevia/print?source=search_result&search=placenta%20previa&selectedTitle
15/15
Vous aimerez peut-être aussi
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Gastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsD'EverandGastric Outlet Obstruction, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsPas encore d'évaluation
- Hydatidiform MoleDocument10 pagesHydatidiform MoleLisa TurnerPas encore d'évaluation
- Case StudyDocument48 pagesCase Studysimbarashe tangwadzanaPas encore d'évaluation
- Antenatal Obstetric ComplicationsDocument40 pagesAntenatal Obstetric ComplicationsArhum SiddiqiPas encore d'évaluation
- IUGRDocument22 pagesIUGRSairindri SahooPas encore d'évaluation
- Pregnancy Uterus Fetus Embryo: Morbidity Selectively Reduce Multiple PregnancyDocument4 pagesPregnancy Uterus Fetus Embryo: Morbidity Selectively Reduce Multiple Pregnancynyzgirl17Pas encore d'évaluation
- Hypertension in Pregnancy-LatestDocument32 pagesHypertension in Pregnancy-LatestshahiraazPas encore d'évaluation
- Placenta Previa Experience at Saudi HospitalDocument23 pagesPlacenta Previa Experience at Saudi HospitalGabbyPas encore d'évaluation
- Managing Multiple PregnanciesDocument33 pagesManaging Multiple PregnanciesAndi Farid APas encore d'évaluation
- Placenta PreviaDocument2 pagesPlacenta PreviaAnonymous 0C4OZmRPas encore d'évaluation
- Anaemia in PregnancyDocument41 pagesAnaemia in PregnancyWan Ahmad FaizFaizalPas encore d'évaluation
- Aklan State University Nursing Readings on Pyloric StenosisDocument5 pagesAklan State University Nursing Readings on Pyloric Stenosisensoooooooooo100% (1)
- Complications of The Third Stage of LabourDocument6 pagesComplications of The Third Stage of LabourSong QianPas encore d'évaluation
- Impey Obs and Gynae Revision Notes PDFDocument9 pagesImpey Obs and Gynae Revision Notes PDFRoisePas encore d'évaluation
- Case Study 1: Nicole: 1. Discuss The Significance of Nicole's Laboratory FindingsDocument12 pagesCase Study 1: Nicole: 1. Discuss The Significance of Nicole's Laboratory FindingsClint NavarroPas encore d'évaluation
- Lecture Notes On AphDocument41 pagesLecture Notes On AphEyob MizanPas encore d'évaluation
- Abruptio PlacentaDocument3 pagesAbruptio PlacentaNano KaPas encore d'évaluation
- PPH Introduction 1Document95 pagesPPH Introduction 1regine maePas encore d'évaluation
- Fetal Growth DisordersDocument26 pagesFetal Growth DisordersEdalyn CapiliPas encore d'évaluation
- PPROMDocument63 pagesPPROMSaraMohammedPas encore d'évaluation
- Myoma UteriDocument21 pagesMyoma UteriLangitBiruPas encore d'évaluation
- Threatened AbortionDocument1 pageThreatened AbortionKEn PilapilPas encore d'évaluation
- Antepartum Haemorrage (APH) : Dr. Mtumweni, MDDocument42 pagesAntepartum Haemorrage (APH) : Dr. Mtumweni, MDmarco luenaPas encore d'évaluation
- PROM SANJIDA FInal 2Document32 pagesPROM SANJIDA FInal 2Saiful islam RonyPas encore d'évaluation
- Ahmed Mohamed Abdel Rahim Rammah: Senior Registrar Obstetrics and Gynecology Department Al - Adan Hospital, KuwaitDocument32 pagesAhmed Mohamed Abdel Rahim Rammah: Senior Registrar Obstetrics and Gynecology Department Al - Adan Hospital, Kuwaithossam626Pas encore d'évaluation
- Abnormal Uterine BleedingDocument12 pagesAbnormal Uterine BleedingGilang DermawanPas encore d'évaluation
- Postpartum HemorrhageDocument8 pagesPostpartum HemorrhageMazlina MaidinPas encore d'évaluation
- Deep Vein Thrombosis and Pulmonary Embolism in Pregnancy - Prevention - UpToDateDocument11 pagesDeep Vein Thrombosis and Pulmonary Embolism in Pregnancy - Prevention - UpToDateGabyta007Pas encore d'évaluation
- Episiotomy Wound Haematoma: Recognition, Management and Healing Assessment by REEDA Scale in Postpartum PeriodDocument4 pagesEpisiotomy Wound Haematoma: Recognition, Management and Healing Assessment by REEDA Scale in Postpartum PeriodIOSRjournalPas encore d'évaluation
- Management of Pregnancy Related BleedingDocument75 pagesManagement of Pregnancy Related BleedingChuah Wei Hong100% (1)
- Endometrial HyperplasiaDocument12 pagesEndometrial HyperplasiaHenri KnafoPas encore d'évaluation
- Amniotic Fluid Embolism (AFE)Document26 pagesAmniotic Fluid Embolism (AFE)sanjivdas100% (1)
- Missed AbortionDocument5 pagesMissed AbortionDesta MarpaungPas encore d'évaluation
- Abruptio PlacentaDocument3 pagesAbruptio Placentachichilovesyou100% (1)
- The Pathophysiology of PPROMDocument2 pagesThe Pathophysiology of PPROMNano KaPas encore d'évaluation
- Pathophysiology of Abortion Case Study (Vizconde, Ehreiz Raiden C. BSN2-A)Document4 pagesPathophysiology of Abortion Case Study (Vizconde, Ehreiz Raiden C. BSN2-A)Raiden VizcondePas encore d'évaluation
- BENIGN OVARIAN DISEASES - Updated January 2018Document31 pagesBENIGN OVARIAN DISEASES - Updated January 2018daniel100% (1)
- A Nursing Case Study On EctopicPregnancy PDFDocument60 pagesA Nursing Case Study On EctopicPregnancy PDFSteffiPas encore d'évaluation
- Shoulder DystociaDocument39 pagesShoulder DystocianormaPas encore d'évaluation
- Mastitis Prevention and TreatmentDocument25 pagesMastitis Prevention and TreatmentGeetha SoundaryaPas encore d'évaluation
- Hypertension in PregnancyDocument45 pagesHypertension in PregnancyMary Anne Cabalza ApinardoPas encore d'évaluation
- Operative Delivery: Presenters: Yonas Gudeta (RMHS/402/09)Document71 pagesOperative Delivery: Presenters: Yonas Gudeta (RMHS/402/09)Jhon Negesse100% (1)
- Case Presentation: RH Negative PregnancyDocument19 pagesCase Presentation: RH Negative PregnancyNazee NazreenPas encore d'évaluation
- HypertensionDocument6 pagesHypertensionTj Kevin P-DoctorPas encore d'évaluation
- Pre and Post PregnancyDocument23 pagesPre and Post PregnancyJitendra ChaudharyPas encore d'évaluation
- Rupture of Tubal Pregnancy in The Vilnius Population: Pasquale Berlingieri, Grazina Bogdanskiene, Jurgis G. GrudzinskasDocument4 pagesRupture of Tubal Pregnancy in The Vilnius Population: Pasquale Berlingieri, Grazina Bogdanskiene, Jurgis G. Grudzinskaslilis lestariPas encore d'évaluation
- Fetal screening in the second trimesterDocument3 pagesFetal screening in the second trimesterYwagar Ywagar100% (1)
- Pregnancy Induced Hypertension PihDocument17 pagesPregnancy Induced Hypertension PihRose DeymPas encore d'évaluation
- Placenta PreviaDocument17 pagesPlacenta PreviaSundari AtmanegaraPas encore d'évaluation
- Abortion: Maxima Vera Pinalgan, MDDocument21 pagesAbortion: Maxima Vera Pinalgan, MDgayon09Pas encore d'évaluation
- Abortion ..Document53 pagesAbortion ..Karan SinghPas encore d'évaluation
- Evaluation of Fetal DeathDocument9 pagesEvaluation of Fetal DeathVinisia TakaraiPas encore d'évaluation
- Ectopic PregDocument6 pagesEctopic PregYwagar Ywagar0% (1)
- Ectopic PregnancyDocument5 pagesEctopic PregnancyFaith FuentevillaPas encore d'évaluation
- Live Preterm Baby Delivered NSDDocument13 pagesLive Preterm Baby Delivered NSDKristine Anne SorianoPas encore d'évaluation
- A Case Presentation On CholedocholithiasisDocument11 pagesA Case Presentation On CholedocholithiasisPaul Vincent EsperePas encore d'évaluation
- Obstetrics Case PresentationDocument27 pagesObstetrics Case PresentationMahaprasad sahoo 77Pas encore d'évaluation
- AbortionDocument62 pagesAbortionRaj KumarPas encore d'évaluation
- RH Disease and ABO IncompatibilityDocument21 pagesRH Disease and ABO Incompatibilityjeezislove617Pas encore d'évaluation
- Clinical ExemplarDocument5 pagesClinical Exemplarapi-302064530Pas encore d'évaluation
- Acute gastritis overviewDocument13 pagesAcute gastritis overviewFalaudin LaksanaPas encore d'évaluation
- MWU Chicago College of Pharmacy IPPE Case Presentation Evaluation FormDocument1 pageMWU Chicago College of Pharmacy IPPE Case Presentation Evaluation FormOmnia El HossienyPas encore d'évaluation
- Progyluton-26 1DDocument16 pagesProgyluton-26 1DUsma aliPas encore d'évaluation
- Medical skills checklist for nursesDocument5 pagesMedical skills checklist for nursesHussain R Al-MidaniPas encore d'évaluation
- Substance Abuse in Pregnancy Effects and ManagementDocument14 pagesSubstance Abuse in Pregnancy Effects and ManagementKhoirunnisa NovitasariPas encore d'évaluation
- Seminar 1 EXPANDED AND EXTENDED ROLE OF PEDIATRIC NURSEDocument15 pagesSeminar 1 EXPANDED AND EXTENDED ROLE OF PEDIATRIC NURSESuganthi Parthiban100% (7)
- 5 dfgs34 24dDocument2 pages5 dfgs34 24dKenneth SyPas encore d'évaluation
- Kanker PayudaraDocument60 pagesKanker PayudaranoviPas encore d'évaluation
- NCPDocument2 pagesNCPsphinx809100% (2)
- Physical Fitness TestDocument33 pagesPhysical Fitness Testdeepuphysio100% (1)
- Tolulope O Afolaranmi1, Zuwaira I Hassan1, Danjuma A Bello1, Yetunde O Tagurum1Document13 pagesTolulope O Afolaranmi1, Zuwaira I Hassan1, Danjuma A Bello1, Yetunde O Tagurum1Adolfina WamaerPas encore d'évaluation
- Nursing FoundationDocument48 pagesNursing Foundationgayathri rayapudiPas encore d'évaluation
- Guidance To The Internaitonal Medical Guide For Ships 3rd EdDocument14 pagesGuidance To The Internaitonal Medical Guide For Ships 3rd EdSaurabh YadavPas encore d'évaluation
- Zambia Country Profile: Health System Context and Innovation OpportunitiesDocument15 pagesZambia Country Profile: Health System Context and Innovation OpportunitiesBrianPas encore d'évaluation
- Curiculum VitaeDocument17 pagesCuriculum VitaedanicaPas encore d'évaluation
- 302 RUA - Interview WorksheetDocument4 pages302 RUA - Interview WorksheetChristy RobinettPas encore d'évaluation
- DEFTACDocument8 pagesDEFTACPendon Maria Mikhaela PPas encore d'évaluation
- Clinical Practice Guidelines On The Management of ChildrenDocument17 pagesClinical Practice Guidelines On The Management of ChildrenRajithaHirangaPas encore d'évaluation
- Introduction To Gerontology and Theories of AgingDocument106 pagesIntroduction To Gerontology and Theories of AgingCyden Shame delos Santos100% (1)
- 258 Viable and Non Viable Environmental MonitoringDocument2 pages258 Viable and Non Viable Environmental MonitoringOsama MahmoudPas encore d'évaluation
- Medication Competency Questions For NursesDocument13 pagesMedication Competency Questions For NursesAlex AndrewPas encore d'évaluation
- Asthma Word Fill KeyDocument2 pagesAsthma Word Fill KeyKaren brooksPas encore d'évaluation
- Resume William S Tokasz December 2015 For BuffstateDocument2 pagesResume William S Tokasz December 2015 For Buffstateapi-301347959Pas encore d'évaluation
- Advanced Wellbeing Offers Financial Therapy For Financial WellbeingDocument3 pagesAdvanced Wellbeing Offers Financial Therapy For Financial WellbeingPR.comPas encore d'évaluation
- Revised Hypergly NCPDocument15 pagesRevised Hypergly NCPDacillo GaillePas encore d'évaluation
- ValuCare University of Santo Tomas Hospital Plan Coordinators and SpecialistsDocument2 pagesValuCare University of Santo Tomas Hospital Plan Coordinators and SpecialistsAnonymous HH3c17osPas encore d'évaluation
- Flap Approaches in Plastic Periodontal and Implant Surgery: Critical Elements in Design and ExecutionDocument15 pagesFlap Approaches in Plastic Periodontal and Implant Surgery: Critical Elements in Design and Executionxiaoxin zhangPas encore d'évaluation
- Tepas 2010Document6 pagesTepas 2010Anonymous 44bTHDeHkbPas encore d'évaluation
- Fletcher 2016Document10 pagesFletcher 2016Christina Putri BongzuePas encore d'évaluation