Académique Documents
Professionnel Documents
Culture Documents
Psychological Problems and Quality of Life in Beta Thalassemia
Transféré par
Ho Yong WaiCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Psychological Problems and Quality of Life in Beta Thalassemia
Transféré par
Ho Yong WaiDroits d'auteur :
Formats disponibles
See
discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/6054414
Pychological problems and quality of life in
Children with thalassemia
Article in The Indian Journal of Pediatrics September 2007
Impact Factor: 0.87 DOI: 10.1007/s12098-007-0127-6 Source: PubMed
CITATIONS
READS
70
824
3 authors, including:
Satish C Girimaji
Santosh K Chaturvedi
National Institute of Mental Health and Neur
National Institute of Mental Health and Neur
64 PUBLICATIONS 1,178 CITATIONS
289 PUBLICATIONS 2,466 CITATIONS
SEE PROFILE
All in-text references underlined in blue are linked to publications on ResearchGate,
letting you access and read them immediately.
SEE PROFILE
Available from: Santosh K Chaturvedi
Retrieved on: 22 May 2016
27
Original Article
Psychological Problems and Quality of Life in Children
with Thalassemia
D. Shaligram, S.C. Girimaji and S.K. Chaturvedi
Department of Psychiatry1, National Institute of Mental Health and Neurosciences, Bangalore.
ABSTRACT
Objective. The study is aimed to assess psychological problems and quality of life (QOL) in children with thalassemia.
Methods. Thirty-nine children (8-16 yr) with transfusion dependent thalassemia attending day care services for blood transfusion
were assessed for psychological problems using the Childhood Psychopathology Measurement Schedule and QOL was
assessed using the EQ-5D.
Results. Forty-four percent of the children had psychological problems and 74% had a poor QOL. Anxiety-related symptoms
(67%), emotional problems, particularly depression (62%), and conduct problems (49%) were the main findings. The children
were most likely to report impaired QOL due to severe difficulties in pain/discomfort (64%) dimension, followed by depression
and mobility problems of equal severity (33%). The side effects of chelation were an independent predictor of psychological
problems and impaired QOL. Also psychological problems were a significant predictor of impaired QOL.
Conclusion. The recognition and management of the psychological problems that accompany chronic physical illnesses
including thalassemia would optimize treatment outcomes and QOL. [Indian J Pediatr 2007; 74 (8) : 727-730] E-mail :
dpka.sha@ gmail.com
Key words : Thalassemia; Chronic illness; Psychological problems; Quality of Life
Children with chronic physical illnesses exemplified by
thalassemia are vulnerable to emotional and behavioral
problems.1 Each yr 8000 children with thalassemia are
born in India, accounting for 10% of the annual world
incidence. 2 The onset of symptoms, the rigors of
treatment, and frequent absence from school make huge
demands on the emotional and interpersonal resources of
the children and their families. The emotional and
cognitive needs of a child with thalassemia are patently
different from those of the adolescent striving for
independence and identity. Adults with thalassemia face
problems related to career, finding partners, establishing
a family (due to infertility) and waning social support as
parents age. Thus each age group has problems unique to
that stage of development. In India, medical management
of thalassemia takes precedence over the integrated
(biopsychosocial) model that is the norm in the West.
However, the increasing longevity of children with
Correspondence and Reprint requests : Dr. Deepika Shaligram, 11,
New Beach Road, Thiruvanmiyur, Chennai 600 041, India.
Telephone : 044-42158519
[Received February 2, 2006; Accepted March 28, 2007]
Indian Journal of Pediatrics, Volume 74August, 2007
thalassemia has brought psychological problems to the
fore.
Various authors have reported that up to 80% of
children with thalassemia are likely to have psychological
problems e.g. oppositional defiant disorder, anxiety
disorders and depression. 3-5 Although children with all
types of blood disorders are exposed to similar stressors,
those with thalassemia are unique in that they have to
attend hospital regularly for blood transfusions.
Sadowski et al., 2002, concluded that specific blood
disorders have differential impact on affected children,
resulting in higher rates of psychological disturbances in
children with thalassemia. A Quality of Life (QOL) study
in adolescents with thalassemia indicates that those with
psychiatric problems had poorer QOL. 6 There is a dearth
of studies that address QOL across different age groups in
children with thalassemia. The present study aimed to
assess psychological problems and QOL in Indian
children with thalassemia.
MATERIALS AND METHODS
This study was conducted by the Department of
Psychiatry, National Institute of Mental Health and
727
28
D. Shaligram et al
Neurosciences, Bangalore. The sample consisted of
children of either sex (aged 8-16 years) with confirmed
diagnosis of transfusion dependent thalassemia attending
the day care facility at 2 general hospitals Bangalore.
Those with mental retardation and other chronic illnesses
including seizures were excluded from the study.
Demographic and clinical details of the children were
collected using a semi-structured proforma that was
developed for study. Psychological problems of the
children
were
assessed
using
Childhood
Psychopathology Measurement Schedule (CPMS), an 8
factor, 75 item parent administered instrument adapted
from the Child Behavior Checklist and standardized for
use in India.7 The factors assessed are (1) Low intelligence
with behavior problems (2) Conduct disorder (3) Anxiety
(4) Depression (5) Psychotic symptoms (7) Physical illness
with emotional problems (8) Somatization. Total and
specific factor scores were used to quantify and
categorize psychopathology. A cut-off score of 10 is
significant. It has been used in childhood chronic physical
illness including thalassemia in other Indian centres.8
The QOL was assessed using the EQ-5D, an
instrument that describes QOL in 5 dimensions- mobility,
self-care, usual activities, pain/discomfort and anxiety/
depression. 9 QOL is measured as a sub-score in each
domain and as a composite score. QOL was also proxy
rated by the caregiver. The EQ-5D has been used in
children (>11 years of age) with chronic physical
illnesses.10,11
months). Most were pursuing primary education (n = 24,
62%). Two (5%) had discontinued schooling and 1 was
not sent to school because of the illness. Eighteen families
(46%) spent > Rs. 7200 per annum for the treatment of
thalassemia but none received blood transfusions/
chelation as frequently as needed (to maintain
recommended levels of blood hemoglobin and serum
ferritin) because of economic problems.
The mean age of the father was 40 5.6 yr and that of
the mother 32.6 5.1 yr. Fathers were predominantly
semi-skilled workers (34, 77%) and 25 (64%) had
completed primary school. Mothers were predominantly
homemakers 25 (64%) and 24 (62%) had completed
primary school. Most (36, 92%) of the children had
thalassemia major, 2 had thalassemia intermedia and 1
had sickle thalassemia. The mean pre-transfusion
hemoglobin was 6.73 1.23 g/dl. The children received
approximately 7 blood transfusions (mean = 6.92 2.07)
in 6 months. The side-effects of blood transfusion were
febrile reaction in 25 (64%), allergic reaction in 1(2.5%),
none in 13 (33%) children. The side-effects of chelation as
assessed using a semi structured proforma (and cross
checked with medical records) were musculoskeletal pain
15 (38.5%) and gastro-intestinal side-effects in 9 (23%)
children. Past history of complications (e.g. congestive
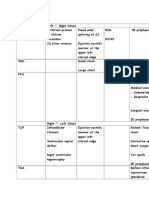
TABLE 1. Demographic Details (n=39)
Variable
Age
8-12 yr
12 yr
Male
Female
Urban
Rural
primary
> primary
Rs. 30,000
> Rs. 30,000
Nuclear
Joint
Rs. 7200
> Rs. 7200
Frequency
Percentage
21
18
23
16
17
22
24*
14
19
20
23
16
21
18
54
46
59
41
44
56
62
38
49
51
59
41
54
46
Children with transfusion dependent thalassemia
were taken up for the study by convenience sampling
method. The family caregivers were informed about the
nature of the study and written consent was sought. The
instruments were administered in a single session by the
same investigator. Amongst the 40 children fulfilling
criteria, one refused consent. A list of side-effects of
chelating agents drawn from standard literature was
included in the semistructured proforma and these
problems were assessed by interview with family
caregivers and cross-checked with medical records.
Gender
Data was analyzed using the Statistical Package for the
Social Sciences - version 10. The Chi square test was
applied to find significant associations between the
demographic and clinical data and the outcome
measures. Bivariate correlational analysis and multiple
linear regression (step-wise) were also used to
characterize the relationship between childrens
demographic and clinical details with the outcome
measures.
* 1 child was not sent to school because of the severity of illness
RESULTS
The sample consisted of 23 boys (59%) and 16 girls (41%)
with the mean age of approximately 11 yr (131.12 29.6
728
Background
Education
Income per
annum
Type of
family
Medical
expenses
per annum
TABLE 2. Children Scoring above Cut Off on CPMS2
Factor
Lower intelligence
Conduct problems
Anxiety
Depression
Psychotic symptoms
Special symptoms
Physical illness
Somatization
Total
n=39
9
19
16
24
3
14
26
22
17
23
49
41
62
8
6
67
56
44
High scores were obtained on more than 1 factor by many children
2
CPMS - Childhood Psychopathology Measurement schedule
Indian Journal of Pediatrics, Volume 74August, 2007
29
Psychological Problems and Quality of Life in Children with Thalassemia
cardiac failure, hepatitis) due to thalassemia and its
treatment were present in 14 (35.8%) children. One child
was HBV positive but none were HIV positive.
Thalassemic facies was present in 35 (89.7%) children.
Regarding the psychological problems in the children,
the special symptoms and the physical illness with
emotional problems factors in the CPMS incorporate
elements relating to anxiety symptoms which along with
emotional problems, particularly depression (62%), and
conduct problems (49%) were the main findings as
represented in Table 2. High scores were obtained on
more than 1 factor by many children. The QOL of the
children was affected in 29 (74%) on self-rating and 32
(82%) on proxy rating. The dimensions affected were
Pain/discomfort (64%) followed by Anxiety/depression
and Mobility (33% each), Usual activities (23%) and Self
care (8%) as represented in table 3. Self care was good in
92%, Usual activities in 77%, Mobility in 66% while 66%
did not have Anxiety/depression and 36% denied Pain/
discomfort. Concordance statistics showed excellent
agreement between self and proxy ratings on the
Mobility, Self- care, Usual activities, Anxiety/depression
and total scores (kappa = 0.642, 0.845, 0.574, 0.530, 0.539
respectively, p= 0.000) and very good agreement on the
Pain/discomfort scores (kappa = 0.394, p=0.001). On
applying quartiles, a composite score of 1 emerged in the
> 75th percentile (n = 10, 26%) i.e. 26% had a good HRQOL
despite thalassemia.
The relationship between the outcome measures
(CPMS, EQ5D) of the children and the demographic,
clinical details were computed using the Chi square test.
In order to perform the Chi square test continuous data
was divided into 2 groups (i.e. CPMS scores above and
below cut off). Seventeen children (17/39) had CPMS
scores above the cut-off value. The mean CPMS scores for
boys were 7.69 2.85, and that amongst the girls was
10.35 5.52. The CPMS total scores were significantly
associated with the sex of the children i.e. the majority of
girls (n = 11/17, 69%) had psychological problems (2=
6.985, df= 1, p= 0.008). Interestingly, CPMS scores were
not significantly associated with any other demographic
or clinical details. There was a strong positive correlation
between higher CPMS depression factor scores (r = 0.71,
p = 0.0001), CPMS total scores (r= 0.57, p = 0.0001) and
poorer HRQOL. There was a positive correlation between
a somatization scores (r = 0.32, p = 0.04), anxiety scores (r
= 0.31, p = 0.04) on the CPMS and poorer HRQOL.
Multiple linear regression (step-wise) was performed for
each of the outcome measures (CPMS, EQ5D). The total
score on the CPMS and presence of side effects of
chelation were significant predictors of the HRQOL,
accounting for 57.2% of the variation in the EQ5D score
(R= 0.327). The EQ5D score (HRQOL) and presence of
side effects of chelation per year were significant
predictors of the psychological problems, accounting for
63.7% of the variation in the CPMS total score (R = -0.631).
DISCUSSION
In this study, a cross-sectional rather than prospective
design was preferred due to logistic constraints i.e. the
children visited once in 4-6 weeks from distant homes
and stayed only for the duration of the blood transfusion.
Assessment performed during a blood transfusion has
drawbacks in terms of pain and side-effects versus
beneficial effect of transfusion influencing responses;
however it was the only feasible method. The prevalence
of psychological problems was 44% (17/39) similar to a
Greek study 12 that reported psychological problems in
42.9%. A subsequent multi-center European study 5
reported psychological problems in 47%. In keeping with
other studies, anxiety and related problems (67%),
emotional problems, particularly depression (62%),
somatization (56%) and conduct problems (49%) were the
main findings. 5, 8, 13-17 Our study found higher rates of
conduct problems and somatization than previous
studies. Differences in socio-cultural factors may account
for these findings. Also, the current study included young
children (unlike previous studies) who may express
psychological distress in the form of conduct problems
and somatization while older children have a growing
insight into the nature of the illness which might account
for the increase in depressive symptoms with increase in
age. Psychological distress might form a common base,
which evolves into depression, anxiety and somatization
in vulnerable individuals. There was no correlation
between the psychological problems in the children and
the demographic (except for sex of the child) and clinical
variables. It is a worrisome that 69% of the girls had
psychological problems. The girl child in India receives
less medical attention and care at home due to sociocultural factors: whether this has a direct role to play in
the greater prevalence of psychological problems in girls
is worthy of exploration. The QOL of the children was
affected in 74%. The impairments in the pain/discomfort,
Anxiety/depression and mobility dimensions of QOL
TABLE 3. Quality of Life (EQ - 5D rated by the child)
Grade of
Problem
No
Some
Severe
Mobility
Self-care
Usual
activities
Pain/
discomfort
26 (67)
11 (28)
2 (5)
36 (92)
3 (8)
-
30 (77)
9 (23)
-
14 (36)
21 (54)
4 (10)
Indian Journal of Pediatrics, Volume 74August, 2007
Anxiety/
depression
26 (67)
11 (28)
2 (5)
729
30
D. Shaligram et al
may be explained on the basis of complications of
thalassemia and side-effects of treatmet. Chelation is
known to produce arthritis, abdominal pain, diarrhea
and vomiting which may have a bearing on the high
scores on the pain, mobility and anxiety/depression
dimensions.
Interestingly, 67% of children had anxiety and 62%
had depression on CPMS while on EQ5D 66% had
neither anxiety/ depression. It should be noted that the
CPMS has several specific probes to assess Anxiety and
Depression individually and in detail, while EQ5D asks a
yes/no question about perceived Anxiety/depression as
a single dimension. This highlights how a child or
caregiver may fail to recognize symptoms because of the
inherent differences in childhood Anxiety and
Depression from their adult counterpart.
The current study found a strong positive correlation
between psychological problems, specifically depression
and poorer HRQOL confirming previous findings in
Greece.6 Anxiety and somatization symptoms may have
similarly contributed to poorer QOL. Understandably,
psychological problems and impaired QOL serve as
predictors for one another with side effects of chelation
being a common predictor for both psychological
problems and QOL for reasons already discussed.
Conclusions and Implications
Forty four percent of the children had psychological
problems and 74% had poor QOL. These psychological
problems were similar to that seen in other chronic
physical illnesses but had not been recognized nor
treated. The study also demonstrated an association
between untreated psychological problems and poor
HRQOL. It is well known that psychological disturbances
adversely affect compliance to treatment in thalassemia18
as in other chronic illnesses. 19 We suggest that due
importance to the recognition and management
(medication, psychosocial interventions e.g. individual
therapy, family intervention packages, self-help groups)
of psychological problems would improve treatment
outcomes including the HRQOL.
Future directions
As the current sample is largely from the lower socioeconomic group, future studies should draw on a sample
representative of all socio-economic strata to enhance the
generalizability of results. Also deprivation of basic needs
(lower socio-economic group), major life events e.g. death
of parents and stressors at school may produce
psychological problems. These variables have to be
controlled in future studies. A prospective study with a
control group powered by a large sample size and
multiple assessments of QOL to gauge changing needs
through the life-cycle would be ideal. Further exploration
of the predictors of psychological problems and QOL
730
might improve the quality of interventions and thus
better address the needs of these children and their
families.
REFERENCES
1. Eiser C. Psychological effects of chronic disease. J Child Psychol
Psychiatry 1990; 31(1): 85-98.
2. Madan N, Sharma S, Rusia U, Sen S, Sood SK. Betathalassemia mutations in northern India (Delhi). Indian J Med
Res 1998; 107 : 134-141.
3. Beratis S. Psychosocial status in pre-adolescent children with
beta-thalassemia. J Psychosom Res 1993; 37(3): 271-279.
4. Tsiantis J, Dragonas Th, Richardson C, Anastasopoulos D,
Masera G, Spinetta J. Psychosocial problems and adjustment
of children with beta-thalassemia and their families. Eur Child
Adolesc Psychiatry 1996; 5(4): 193-203.
5. Sadowski H, Kolvin I, Clemente C, Tsiantis J, Baharaki S, Ba G.
Psychopathology in children from families with blood
disorders: a cross national study. Eur Child Adolesc Psychiatry
2002; 11: 151-161.
6. Mikelli A, Tsiantis J. Brief report: Depressive symptoms and
quality of life in adolescents with beta-thalassemia. J Adolesc
2004; 27 : 213-216.
7. Malhotra S, Varma VK, Verma SK, Malhotra A. Childhood
Psychopathology Measurement Schedule: Development and
Standardization. Indian J Psychiatry 1988; 30(4) : 325-331.
8. Pradhan PV, Shah H, Rao P, Ashturkar D, Ghaisas P.
Psychopathology and Self-esteem in Chronic Illness. Indian J
Pediatrics 2003; 70(2) : 135-138.
9. EuroQOL Group. EuroQOL a new facility for the
measurement of Health-related Quality of Life. Health Policy
1990; 16 : 199-203.
10. Patel AB, Pathan HG. Quality of life in children with sickle cell
hemoglobinopathy. Indian J Pediatr 2005; 72 : 567-571.
11. Stolk EA, Busschbach JJ, Vogels T. Performance of the
EuroQol in children with imperforate anus. Qual Life Res 2000;
9(1) : 29-38.
12. Tsiantis J, Xypolita-Tsantili D, Papadakou-Lagoyianni S.
Family reactions and their management in a parents group
with beta-thalassemia. Arch Dis Child 1982; 57 : 860-863.
13. Logothetis J, Haritos-Fatouros M, Constantoulakis M,
Economidou J, Augoustaki O, Loewenson RB. Intelligence and
behavioral patterns in patients with Cooleys anemia
(homozygous beta-thalassemia); A study based on 138
consecutive cases. Pediatrics 1971; 48(5) : 740-744.
14. Woo R, Giardina PJ, Hilgartner MW. A psychosocial needs
assessment of patients with homozygous beta thalassemia.
Ann NY Acad Sci 1985; 445 : 316-322.
15. Massaglia P, Pozzan M. T, Piga A, Davico S, Luzatto L,
Carpignano M. Psychological aspects of Thalassemia. Pediatr
Med Chir 1986; 8(1) : 27-31.
16. Tsiantis J. Family reactions and relationships in thalassemia.
Sixth Cooleys Anemia Symposium. Ann NY Acad Sci 1990;
612 : 451-461.
17. Canatan D, Ratip S, Kaptan S, Cosan R. Psychosocial burden
of beta-thalassemia major in Antalya, south Turkey. Soc Sci
Med 2003; 56: 815-819.
18. Beratis S. Noncompliance with Iron Chelation Therapy in
patients with beta- thalassemia. J Psychosom Res 1989; 33(6):
739-745.
19. Stuber ML. Psychiatric Sequelae in seriously ill children and
their families. Psychiatr Clin North Am 1996; 19(3) : 481-493.
Indian Journal of Pediatrics, Volume 74August, 2007
Vous aimerez peut-être aussi
- Obs History MandarinDocument1 pageObs History MandarinHo Yong WaiPas encore d'évaluation
- Approach To The Patient With Dysphagia PDFDocument7 pagesApproach To The Patient With Dysphagia PDFHo Yong Wai100% (1)
- Approach To The Patient With Dysphagia PDFDocument7 pagesApproach To The Patient With Dysphagia PDFHo Yong Wai100% (1)
- Dengue CaseDocument4 pagesDengue CaseHo Yong WaiPas encore d'évaluation
- Dengue CaseDocument4 pagesDengue CaseHo Yong WaiPas encore d'évaluation
- Cerebellar SyndromeDocument2 pagesCerebellar SyndromeHo Yong WaiPas encore d'évaluation
- Dengue CaseDocument4 pagesDengue CaseHo Yong WaiPas encore d'évaluation
- Part 1Document18 pagesPart 1Ho Yong WaiPas encore d'évaluation
- Taking A Gynaecological HistoryDocument21 pagesTaking A Gynaecological Historyasif_siddiqui_2100% (1)
- Department Coordinator BioDocument1 pageDepartment Coordinator BioHo Yong WaiPas encore d'évaluation
- HivDocument1 pageHivHo Yong WaiPas encore d'évaluation
- Bipolar DisorderDocument1 pageBipolar DisorderHo Yong WaiPas encore d'évaluation
- Paediatrics at A GlanceDocument2 pagesPaediatrics at A GlanceHo Yong WaiPas encore d'évaluation
- Ob-Gyn Clinical Cases (From Apgo Site)Document221 pagesOb-Gyn Clinical Cases (From Apgo Site)jamiePas encore d'évaluation
- BVMDocument3 pagesBVMHo Yong WaiPas encore d'évaluation
- Internal Medicine Venepuncture IM & SC Injection Cannulation ABGDocument1 pageInternal Medicine Venepuncture IM & SC Injection Cannulation ABGHo Yong WaiPas encore d'évaluation
- Common ENT ComplaintsDocument9 pagesCommon ENT ComplaintsHo Yong WaiPas encore d'évaluation
- HomeworkDocument12 pagesHomeworkHo Yong WaiPas encore d'évaluation
- CPG Management of Dengue Infection in Adults (Revised 2nd Edition)Document68 pagesCPG Management of Dengue Infection in Adults (Revised 2nd Edition)umiraihana1Pas encore d'évaluation
- Test Yourself AnaesthesiologyDocument4 pagesTest Yourself AnaesthesiologyHo Yong WaiPas encore d'évaluation
- Common Long Cases IM Sem 7Document3 pagesCommon Long Cases IM Sem 7Ho Yong WaiPas encore d'évaluation
- Reflective ReportDocument2 pagesReflective ReportHo Yong WaiPas encore d'évaluation
- Lesson 9 ReviewDocument2 pagesLesson 9 ReviewHo Yong WaiPas encore d'évaluation
- Lesson 6 ReviewDocument2 pagesLesson 6 ReviewHo Yong WaiPas encore d'évaluation
- Lesson 3 ReviewDocument4 pagesLesson 3 ReviewHo Yong WaiPas encore d'évaluation
- Lesson 8 ReviewDocument3 pagesLesson 8 ReviewHo Yong WaiPas encore d'évaluation
- TBL PaedsDocument10 pagesTBL PaedsHo Yong WaiPas encore d'évaluation
- TBL RheumatologyDocument16 pagesTBL RheumatologyHo Yong WaiPas encore d'évaluation
- Lesson 5 ReviewDocument4 pagesLesson 5 ReviewHo Yong WaiPas encore d'évaluation
- Psy Case DiscussionDocument16 pagesPsy Case DiscussionHo Yong WaiPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Model of Creative Ability PDFDocument8 pagesThe Model of Creative Ability PDFOvidiu MunteanPas encore d'évaluation
- Javon Floyd Questions Proposal Template 3Document4 pagesJavon Floyd Questions Proposal Template 3api-583347132Pas encore d'évaluation
- Hypnotic Script-Writing Secrets and Other Hypnosis Tips The Masters UseDocument111 pagesHypnotic Script-Writing Secrets and Other Hypnosis Tips The Masters UseShakeel100% (1)
- HyteriaDocument4 pagesHyteriaHarinderPas encore d'évaluation
- Counseling and Its Work SettingsDocument16 pagesCounseling and Its Work SettingsMaryJoyceRamosPas encore d'évaluation
- Module 6 AbstractionDocument3 pagesModule 6 AbstractionCherry Rose J. DeniegaPas encore d'évaluation
- Purposive Behaviorism by Edward Chance TolmanDocument3 pagesPurposive Behaviorism by Edward Chance TolmanAris Watty100% (1)
- Approaches To Music TherapyDocument31 pagesApproaches To Music TherapyLuis AlbertoPas encore d'évaluation
- Exploring Art Therapy Group Practice in Early Intervention PsychosisDocument13 pagesExploring Art Therapy Group Practice in Early Intervention PsychosisDiana TimeaPas encore d'évaluation
- Process Recording Psychiatric NursingDocument17 pagesProcess Recording Psychiatric NursingAaLona Robinson100% (4)
- CBT JealousyDocument15 pagesCBT Jealousydtsimona100% (4)
- How To Manage Trauma: Trauma Can Stem FromDocument1 pageHow To Manage Trauma: Trauma Can Stem FromSparking The Genius0% (1)
- Gepsych: Gepsych Productive Work OutputDocument1 pageGepsych: Gepsych Productive Work OutputCarlos ReyesPas encore d'évaluation
- The Problem and Its BackgroundDocument7 pagesThe Problem and Its BackgroundFrizie Jane Sacasac MagbualPas encore d'évaluation
- 5 Reasons People Have Low Self-Confidence - Psychology TodayDocument5 pages5 Reasons People Have Low Self-Confidence - Psychology TodaycreativePas encore d'évaluation
- Behavior Management (Notes)Document3 pagesBehavior Management (Notes)alvinlinlPas encore d'évaluation
- Together TheScienceofSocialPsyDocument506 pagesTogether TheScienceofSocialPsyMarch EllenePas encore d'évaluation
- Why Some Psychopaths Make Great CEOsDocument4 pagesWhy Some Psychopaths Make Great CEOsalexandru_gheoPas encore d'évaluation
- Skin ShamingDocument4 pagesSkin Shamingcedrick abalosPas encore d'évaluation
- Empathy Map Canvas 006 PDFDocument1 pageEmpathy Map Canvas 006 PDFAdam LenaartsPas encore d'évaluation
- The Body, The Play and The DramaDocument4 pagesThe Body, The Play and The DramaEzequiel Martins100% (1)
- Introduction To PsychologyDocument9 pagesIntroduction To PsychologymeenalairanPas encore d'évaluation
- Historical Survey of Mental HygieneDocument22 pagesHistorical Survey of Mental Hygieneyno kho100% (1)
- Psychopathology WorksheetDocument9 pagesPsychopathology Worksheetapi-308625760Pas encore d'évaluation
- The Impact of Social Media On Depression in 18-34-Year-Olds in The United StatesDocument66 pagesThe Impact of Social Media On Depression in 18-34-Year-Olds in The United StatesjoyPas encore d'évaluation
- GOALS PARTNERSHIP - Occupational Therapist and Other Health ProfessionalsDocument4 pagesGOALS PARTNERSHIP - Occupational Therapist and Other Health ProfessionalsarvinPas encore d'évaluation
- Argumentative Essay - Nanda NoveriaDocument2 pagesArgumentative Essay - Nanda NoveriaNo VenaPas encore d'évaluation
- Comprehensive Study Guide For NCEDocument73 pagesComprehensive Study Guide For NCEoscarcortina100% (6)
- Nursing Care Plans SchizDocument27 pagesNursing Care Plans SchizClariza Castro76% (17)
- 10 Things You Need To Know About PsychologyDocument6 pages10 Things You Need To Know About PsychologyhuvanrajPas encore d'évaluation