Académique Documents
Professionnel Documents
Culture Documents
Antibacterial Properties of Tualang Honey and Its Effect in Burn Wound Management - A Comparative Study PDF
Transféré par
Anonymous sllHltTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Antibacterial Properties of Tualang Honey and Its Effect in Burn Wound Management - A Comparative Study PDF
Transféré par
Anonymous sllHltDroits d'auteur :
Formats disponibles
Nasir et al.
BMC Complementary and Alternative Medicine 2010, 10:31
http://www.biomedcentral.com/1472-6882/10/31
RESEARCH ARTICLE
Open Access
Antibacterial properties of tualang honey and its
effect in burn wound management: a comparative
study
Research article
Nur-Azida Mohd Nasir1, Ahmad Sukari Halim*1, Kirnpal-Kaur Banga Singh2, Ananda Aravazhi Dorai1 and MehruNisha Muhammad Haneef2
Abstract
Background: The use of honey as a natural product of Apis spp. for burn treatment has been widely applied for
centuries. Tualang honey has been reported to have antibacterial properties against various microorganisms, including
those from burn-related diagnoses, and is cheaper and easier to be absorbed by Aquacel dressing. The aim of this
study is to evaluate the potential antibacterial properties of tualang honey dressing and to determine its effectiveness
as a partial thickness burn wound dressing.
Methods: In order to quantitate the bioburden of the swabs, pour plates were performed to obtain the colony count
(CFU/ml). Swabs obtained from burn wounds were streaked on blood agar and MacConkey agar for bacterial isolation
and identification. Later, antibacterial activity of Aquacel-tualang honey, Aquacel-Manuka honey, Aquacel-Ag and
Aquacel- plain dressings against bacteria isolated from patients were tested (in-vitro) to see the effectiveness of those
dressings by zone of inhibition assays.
Results: Seven organisms were isolated. Four types of Gram-negative bacteria, namely Enterobacter cloacae, Klebsiella
pneumoniae, Pseudomonas spp. and Acinetobacter spp., and three Gram-positive bacteria, namely Staphylococcus
aureus, coagulase-negative Staphylococcus aureus (CONS) and Streptococcus spp., were isolated. Total bacterial count
decreased on day 6 and onwards. In the in-vitro antibacterial study, Aquacel-Ag and Aquacel-Manuka honey dressings
gave better zone of inhibition for Gram positive bacteria compared to Aquacel-Tualang honey dressing. However,
comparable results were obtained against Gram negative bacteria tested with Aquacel-Manuka honey and AquacelTualang honey dressing.
Conclusions: Tualang honey has a bactericidal as well as bacteriostatic effect. It is useful as a dressing, as it is easier to
apply and is less sticky compared to Manuka honey. However, for Gram positive bacteria, tualang honey is not as
effective as usual care products such as silver-based dressing or medical grade honey dressing.
Background
The uses of honey as a burn injury treatment were first
documented by the Egyptians in 2000 BC [1]. It is well
documented that honey inhibits a broad spectrum of bacterial species [2-4]. Also letter to editor from Majtan and
Majtan 2009 (personal communication) support this
finding.
* Correspondence: ashalim@kb.usm.my
1 Reconstructive Sciences Unit, School of Medical Sciences, Universiti Sains
Malaysia, Health Campus 16150 Kubang Kerian, Kelantan, Malaysia
Contributed equally
Honey, which is high in carbohydrates, is produced
from bee floral nectar, with fructose and glucose as major
components and other honeybee derived chemical compounds or phytochemicals present in small quantities.
These combinations and a number of other factors, such
as low water activity, hydrogen peroxide, low pH, and
other partially characterized or uncharacterized compounds, produce a high antimicrobial action [5-9].
The increasing rate of multi-resistant to parenteral
antibiotic and ineffectiveness of antibacterial topical
dressings such as Silver sulfadiazine (SSD) which is
Full list of author information is available at the end of the article
2010 Nasir et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons
Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in
any medium, provided the original work is properly cited.
Nasir et al. BMC Complementary and Alternative Medicine 2010, 10:31
http://www.biomedcentral.com/1472-6882/10/31
widely used to represent a major challenge in burn care.
This problem required alternative treatment option.
Conventional dressings such as gauze, Tulle gras and
hydrofibre based do not address the issues of infection
effectively. Therefore new generation of silver based
dressing such as Aquacel-Ag and Acticoat has been
developed to reduce local infection and is related morbidity. At the same time other non conventional treatment
approach such as the use of honey has become an attractive alternative[10-12]. Manuka honey is not widely used
for the management of burn compared to silver based
dressings. The silver based dressing is presently used in
most clinical settings with good scientific evidence. Tualang honey has been reported to have antibacterial properties against various microorganisms, including those
from burn-related diagnoses such as Pseudomonas spp.
and MRSA [2,9,13-15], and it is cheaper and easier to be
absorbed by Aquacel dressing. Tualang honey was
obtained from the tualang tree (Koompassia excelsa) and
used as a partial thickness burn treatment.
This partial thickness burn usually extends through the
epidermis downward into the papillary, or superficial,
layer of the dermis or it can be extended downward into
the reticular, or deeper, layer or the dermis [16].
This study evaluated the potential antibacterial properties of tualang honey dressing and its effectiveness compared to Aquacel-Ag dressing to treat partial thickness
burn wounds patient. Tualang honey was chosen as it is a
Malaysian honey used to treat local people. It has been
reported from various parts of the world that various
types of honey differ substantially in their activity,
depending on the nectar source [6]. Later, in this study,
Aquacel-Ag dressings, Aquacel-Tualang, Aquacel-plain
(as a control) were used in in-vitro antibacterial studies to
make it comparable to our clinical treatment. Bacteria
isolated from patients with partial thickness burn wounds
were treated with all of the above dressings to assess the
dressing's antibacterial effect.
Methods
Dressing samples
Tualang honey was supplied by the Federal Agriculture
Marketing Authority (FAMA) office in Kedah, Malaysia.
The tualang honey was sterilized by gamma radiation (25
kGy) for clinical use, and commercial manuka honey
(Kordel's UMF10+) was used for laboratory use. Aquacel
(plain dressing) and Aquacel Ag were purchased from
ConvaTec, E.R. Squibb & Sons, L.L.C, US. for clinical and
laboratory use. The study aim was to compare Aquaceltualang honey (Aquacel plain soaked with tualang honey)
with Aquacel Ag (as it was known as a standard dressing
in clinical practice) to see its potential antibacterial effect.
Whereas, manuka honey was well known having antibacterial effect and used as a dressing. Tualang honey is eas-
Page 2 of 7
ier to be absorbed by Aquacel plain compared to Manuka
honey. Furthermore tualang honey is easy to access as it is
Malaysian honey and cheaper compare to manuka or
Aquacel-Ag dressing.
Selection of Patients and Treatment Procedure
This study has been approved by Universiti Sains Malaysia Human Ethical Committee. A total of 10 patients, ages
2 - 60 years old, with partial thickness burns (< 30%) and
requiring tangential excision were included in this study
after consent. Subjects were expected to survive and were
kept in a hospital environment. Selected patients were
screened on day 0 to day 2. Dressings were applied on day
3 (randomly treated with either Aquacel-Tualang honey
dressing or Aquacel-Ag dressings). Dressing was on day 6
and day 9 (only if patient delayed for surgery). Swabs were
taken at every dressing change.
Surface Swabs
Two surface swabs from 2-5 cm2 of burn wound were collected from each patient on day 0 before applying any
dressing material. One swab was put in normal saline and
the other one was kept in a container without normal
saline. The collected samples were immediately processed for bacteriological analysis. Later, swabs were collected on day 3, day 6, day 6+ or on the day of surgery.
Bacteria identification
Swabs collected were streaked on blood agar and MacConkey agar plates for bacterial identification. The plates
were incubated at 35 2C for 24 hours. Further identification on the microorganisms' growth on the plates (if
any) was done using the conventional method or using
the RapID STR or RapID SS/u System (Remel Inc.
USA).
Total bacterial count determination
The other swab obtained from the same patient was
immersed in 2 ml of normal saline and 10 fold serial dilutions were performed. Then, 1 ml of each dilution was
pipetted onto petri dishes in triplicate. All the plates were
incubated at 35 2C for 24 hours. Colony counts were
performed on each plate and were recorded as CFU/ml.
Measurement of zone of inhibition
Bactericidal activity was tested against each bacteria
identified from the burn wound. This was done to compare the zone of inhibition obtained when the bacteria
were treated with Aquacel-Tualang honey dressing,
Aquacel-Manuka honey dressing Aquacel-Ag dressing
and Aquacel-plain dressing (as a control) by zone of inhibition assay [17]. The Aquacel plain dressings were cut
into 1 cm 1 cm squares each and were soaked with 200
l of pure Tualang honey or 200 l of pure Manuka
honey. Inocula of 0.5 MacFarland (1 108 CFU/ml)
Nasir et al. BMC Complementary and Alternative Medicine 2010, 10:31
http://www.biomedcentral.com/1472-6882/10/31
microorganisms were prepared and inoculated onto a
Mueller-Hinton agar (MHA) plate. Inoculation was done
within 15 minutes of preparation time. Then, the four different dressings were placed onto the MHA plate. The
test was done in triplicate. All plates were incubated overnight at 35 2C, and the zone of inhibition was measured after 24 hours of incubation.
Page 3 of 7
yielded growth of bacteria. On day 3, 70% of the samples
showed growth of microorganisms, in which only 10% of
samples gave 104 CFU/ml. On day 6, 40% of swabs
showed growth of bacteria, in which 20% were 104, and
no growth was observed in 10% of the samples tested. On
day 6, 50% of the swab samples could not be collected.
Only 2 swab samples were obtained after day 6, which
resulted in < 104 CFU/ml and 104 CFU/ml, respectively.
Results
Identification
Zone of inhibition
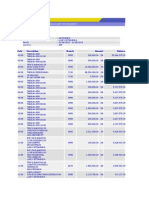
Table 1 shows the 7 different bacteria that were isolated
and identified from 10 patients. Four types of Gram-negative bacteria, namely Enterobacter cloacae, Klebsiella
pneumoniae, Pseudomonas spp. and Acinetobacter spp.,
and three Gram-positive bacteria, namely Staphylococcus
aureus, coagulase-negative Staphylococcus aureus
(CONS) and Streptococcus spp., were isolated. S. aureus
was isolated in most of the swab samples having mixed
growth.
On day 0 (admission day), swabs were taken on the partial thickness burn wound patients. Days 0 - 2 were a
screening period which is only Aquacel plain was given to
the patients. Only sample 6 yielded a positive culture,
with mixed growth of CONS and S. aureus; the other
nine yielded no bacterial growth.
On day 3, 2 single cultures from samples 1 (E. cloacae)
and 5 (CONS) were obtained, and 6 yielded mixed bacterial growth. Those mixed growths contained two microorganisms.
Day 6 showed microorganisms isolated from 5 samples
of burn wounds 3 days after treatment. Samples 1, 2 and 5
yielded single growth of E. cloacae, Streptococcus spp.
and K. pneumoniae, respectively, while sample 10 yielded
mixed growth of Pseudomonas spp. and Acinetobacter
spp. Sample 6 yielded no growth.
Sampling after day 6 was less, as patients went for early
surgery as soon as their wound was stabilized. Mixed bacterial growth was observed in both samples collected
after day 6 when treated with honey. Two bacteria were
isolated from sample 2 (S. aureus and Streptococcus spp.),
whereas three types of bacteria were isolated from sample
5 (CONS, K. pneumoniae and Pseudomonas spp.)
Table 3 shows that all dressings had antibacterial effects
against all the microorganisms isolated from burn
wounds by an in-vitro assay. The silver-based dressing
(Aquacel-Ag) showed better antibacterial effects than
other dressings. Aquacel-Ag dressing was the most effective antimicrobial agent against Gram-negative bacteria,
and it was most effective against Pseudomonas spp., with
a zone of inhibition 18 mm. However, Aquacel-Ag and
Aquacel-Manuka honey dressings gave better zone of
inhibition for Gram positive bacteria compared to Aquacel-Tualang honey dressing. The highest zone of inhibition was obtained for streptococci treated with AquacelManuka honey dressings. The zone of inhibition obtained
for Gram negative bacteria were comparable when
treated with Aquacel-Manuka honey and Aquacel-Tualang honey dressing.
Total bacterial count
Table 2 shows that burn wounds treated with the silverbased dressing yielded less than 104 CFU/ml for sample 6,
while sample 7 showed no microorganisms isolated.
Burn wounds treated with tualang honey showed an
increase in CFU/ml for sample 3 on day 3. The CFU/ml
was 104 on day 6 for samples 5 and 10, and on day 6
onward, sample 2 showed a CFU/ml 104.
In this study, bioburdens of the swab were determined
in each patient on days 0, 3, 6 and > 6. On day 0, no bacteria was isolated from 90% of the samples, and only 10%
Discussion
This study used Aquacel-tualang honey dressing and
Aquacel-Ag dressing to treat partial thickness burn
patients clinically and to determine their antimicrobial
effects in vitro. Aquacel plain was soaked with tualang
honey and used as a dressing instead of being taken orally
(systemic agent) [18]. The superficial swab was chosen to
collect samples, in order to identify the commonly isolated microorganisms from the burn wound. This
method was simple, inexpensive and less painful [19]. A
previous study had shown no significant differences in
bacterial counts between full thickness and partial thickness burns, whether by surface swab or by biopsy [20].
No infection or bacteria were isolated on day 0 (first
day of injuries), as the burn wound surface is sterile
immediately following thermal injury, as reported by
Church and colleagues [21]. Gosh and colleagues [22]
reported that re-epithelialization of the wound begins
within hours after injury by the movement of epithelial
cells from the surrounding epidermis over the denuded
surface. Rapid reestablishment of the epidermal surface
and its permeability barrier prevents excessive water loss
and time of exposure to bacterial infections, which
decreases the morbidity and mortality of patients who
have lost a substantial amount of skin surface. Unfortunately, as thermal injuries impair the skin and its normal
barrier function, contamination and infection is almost
Nasir et al. BMC Complementary and Alternative Medicine 2010, 10:31
http://www.biomedcentral.com/1472-6882/10/31
Page 4 of 7
Table 1: Bacteria isolated and colony count from burn wounds treated with tualang honey and silver-based dressing
Sample
Treatment
Days
Aquacel plain
NG
E. cloacae
E. cloacae
Aquacel-tualang honey
Microorganisms
CFU/ml
0.97101
6+
NS
Aquacel plain
NG
Aquacel-tualang honey
S. aureus &Streptococcus spp.
3.3 103
Streptococcus spp.
3.3 103
6+
S. aureus &
Streptococcus spp.
2.4 105
Aquacel plain
NG
Aquacel-tualang honey
K. pneumoniae &
S. aureus
NS
6+
NS
Aquacel plain
NG
Aquacel-tualang honey
S. aureus &
CONS
NS
5.3104
2.0 101
6+
5
Aquacel plain
NG
Aquacel-tualang honey
CONS
1.6102
K. pneumoniae
5.9105
CONS, K. pneumoniae &
Pseudomonas spp.
9.3103
CONS &S. aureus
5.9101
2.3102
6+
6
0
Silver
7
Silver
10
CONS &S. aureus
NG
6+
NS
NG
NG
NS
6+
NS
Aquacel plain
NG
Aquacel-tualang honey
NG
NS
6+
NS
Aquacel plain
NG
Aquacel-tualang honey
CONS &
Acinetobacter spp.
2.0 103
NS
6+
NS
Aquacel plain
NG
Aquacel-tualang honey
Pseudomonas spp.
Acinetobacter spp.
3.8 102
Pseudomonas spp.
Acinetobacter spp.
6.8 105
6+
CONS - coagulase-negative S. aureus, NG - no growth, NS - no sample
NS
Nasir et al. BMC Complementary and Alternative Medicine 2010, 10:31
http://www.biomedcentral.com/1472-6882/10/31
unavoidable, even with the use of topical antimicrobial
agents [23]. In this study, bacteria were isolated on day 3,
as the colonization and infection began [14,21]. Infection
of the burn wound is indicated if the number of bacteria
is 104 CFU/ml or mg [21,24]. The infection rate
increased until day 6 and more (> day 6) if the patient was
delayed for surgery. Otherwise, no swabs or tissues were
obtained after day 6, as surgery was done as soon as the
patient was hemodynamically stabilized [13,21]. The
early burn wound excision that now occurs within the
first few days after burn injury has resulted in improved
survival rates. The primary aims of early excision are
removal of the dead tissue that stimulates an overwhelming systemic inflammatory response syndrome and prevention of infection by temporary or permanent closure
of burn wound [21].
The most common microorganism identified in this
study was S. aureus followed by CONS, K. pneumoniae,
Streptococcus spp., E. cloacae, Pseudomonas spp. and
Acinetobacter spp. These microorganisms were commonly isolated from partial thickness burn wounds. Similar results were reported by Dastouri and colleagues [25],
Basualdo and colleagues [14] and Pieper [9]. These
microorganisms showed differences in zones of inhibition when treated with Aquacel plain dressing soaked
with pure tualang honey, Aquacel plain dressing soaked
with pure manuka honey and Aquacel-Ag dressing, with
Aquacel plain as the control.
The disc diffusion assay showed that Aquacel-manuka
honey dressing had almost the same antibacterial effect
as Aquacel-Ag dressing and was more effective than
Aquacel-tualang honey dressing against Gram-positive
bacteria, such as S. aureus, CONS and Streptococcus spp.
Page 5 of 7
The Aquacel-Ag dressing was the most effective dressing against the four Gram-negative bacteria isolated from
burn wounds [10] Aquacel-manuka honey dressing gave
slightly higher MIC values compared to Aquacel-tualang
honey dressing for all the bacteria tested. Plain Aquacel
dressing was used as the control in this study, and it had
no antibacterial effect against any of the microorganisms
tested.
Aquacel-tualang honey worked more effectively if the
dressing was applied and covered the wound area properly. Gentle pressure applied to the dressing covering the
wound area would be very helpful, as reported by Jones
and colleagues [26].
Visual inspection of the disc diffusion assay also
showed that tualang honey had more partial inhibition
(PI)/a lower concentration that retarded growth [15] than
manuka honey. This is because tualang honey is more liquid than manuka honey and can be easily absorbed by
MHA and other substances, such as human skin. It was
observed in this study that tualang honey took less than
one minute to be absorbed through the dressing, whereas
manuka honey took almost one hour to be absorbed in
the dressing.
Conclusions
In this study, tualang honey demonstrated to poses substantial bactericidal as well as bacteriostatic effect. The
Aquacel dressing soaked with pure tualang honey without any dilution was less sticky than manuka honey and
was easier to apply as a dressing. However, for Gram positive bacteria, tualang honey is not as effective as usual
care products such as silver-based dressing or medical
grade honey dressing.
Table 2: Total bacterial count of swab samples treated with Aquacel-tualang honey dressing and Aquacel-Ag
Sample
Treatment
CFU/ml
Day 0
Day 3
Day 6
> Day 6
NG
< 104
NS
Aquacel-tualang honey
NG
Aquacel-tualang honey
NG
<
Aquacel-tualang honey
NG
104
Aquacel-tualang honey
NG
<
104
NS
NS
Aquacel-tualang honey
NG
< 104
104
< 104
Aquacel-Ag
< 104
< 104
NG
NS
Aquacel-Ag
NG
NG
NS
NS
Aquacel-tualang honey
NG
NG
NS
NS
Aquacel-tualang honey
NG
<
NS
NS
10
Aquacel-tualang honey
NG
< 104
104
NS
NG - No growth, NS - No sample
104
104
<
104
NS
104
NS
Nasir et al. BMC Complementary and Alternative Medicine 2010, 10:31
http://www.biomedcentral.com/1472-6882/10/31
Page 6 of 7
Table 3: Antibacterial effect of selected dressings on isolated bacteria from burn wounds
Bacteria strains
Average zone of inhibition (mm)
Aquacel- Tualang honey (100%)
Aquacel-Manuka honey
(100%)
Aquacel-Ag
Aquacel (Plain)
Staphylococcus aureus
11
15.3
13.2
Coagulase-negative Staphylococcus aureus
11
14.7
14.3
Streptococcus spp.
12.8
16.8
13.7
Enterobacter cloacae
10.5
11.2
12.3
Klebsiella pneumoniae
10.5
11.2
12.3
Pseudomonas spp.
11
11.8
18
Acinetobacter spp.
11
12.3
13.5
Competing interests
The authors declare that they have no competing interests.
8.
Authors' contributions
NAMN carried out the microbiological analysis and prepared the manuscript,
HAS designed the study and drafted manuscript, KKBS involved in microbiological analysis, design of the study and manuscript correction, DAA participated in design of the study and manuscript correction and MNMH involved in
microbiological analysis. All authors have read and approved the final manuscript.
9.
Acknowledgements
We would like to thank to Universiti Sains Malaysia RU Grant 1001/PPSP/
8120215 for providing the financial support and Agromas, Federal Agriculture
and Marketing (FAMA), Kedah, Malaysia for supplying the tualang honey for
this study.
Author Details
1Reconstructive Sciences Unit, School of Medical Sciences, Universiti Sains
Malaysia, Health Campus 16150 Kubang Kerian, Kelantan, Malaysia and
2Department of Medical Microbiology & Parasitology, School of Medical
Sciences, Universiti Sains Malaysia, Health Campus 16150 Kubang Kerian,
Kelantan, Malaysia
Received: 31 January 2010 Accepted: 24 June 2010
Published: 24 June 2010
This
BMC
2010
is
article
Complementary
an
Nasir
Open
is et
available
Access
al; licensee
and
from:
article
Alternative
BioMed
http://www.biomedcentral.com/1472-6882/10/31
distributed
Central
Medicine
under
Ltd.
2010,
the terms
10:31 of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
References
1. Dunford CCR, Molan P, White R: The use of honey in wound
management. Nursing Standard 2000, 15:63-68.
2. Tan HT, Abdul Rahman R, Gan SH, Halim AS, Hassan SA, Sulaiman SA,
Kirnpal-Kaur BS: The antibacterial properties of Malaysian Tualang
honey against wound and enteric microorganisms in comparison to
Manuka honey. BMC Complementary and Alternative Medicine 2009,
9(34):1-8.
3. Cooper RA, Molan PC, Harding KG: Antibacterial activity of honey
against strains of Staphylococcus aureus from infected wound. Journal
of Society of Medicine 1999, 92:283-285.
4. Cooper RA, Molan PC: The use of honey as an antiseptic in the
managing pseudomonas infection. Journal of Wound Care 1999,
8(6):161-164.
5. Molan P: A brief review of the use of honey as a clinical dressing.
Australian J of Management 1998, 6:148-158.
6. Aljady AMKMY, Jamal AM, Mohd Yassim MY: Biochemical Study on the
Efficacy of Malaysian Honey on Inflicted Wounds: An Animal Model.
Medical Journal of Islamic Academy of Sciences 2000, 13(3):125-132.
7. Jeffrey AE, Echazarreta CM: Medical uses of honey. Rev Biomed 1996,
7:43-49.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
Lusby P, Coombes AL, Wilkinson JM: Bactericidal activity of different
honeys against pathogenic bacteria. Archives of Medical Reaseach 2005,
36:464-467.
Pieper B: Honey-Based Dressings and Wound Care. An Option for care
in the Uniter States. Journal Wound Ostomy Continence Nursing 2009,
36(1):60-66.
Atiyeh BSCM, Hayek SN, Dibo SA: Effect of silver on burn wound
infection control and healing: Review of the literature. Burns 2007,
33:139-148.
Wright JBLK, Hansen D, Burrel RE: Efficacy of topical silver against fungal
burn wound pathogens. American Journal of Infection Control 1999,
27:344-350.
Wright JBLK, Burrel RE: Wound management in an era of increasing
bacterial antibiotic resistance: A role for topical silver treatment.
American Journal of Infection Control 1998, 26:572-577.
Molan P: The Evidence Supporting the Use of Honey as a Wound
Dressing. Lower Extremity Wounds 2006, 5(1):40-54.
Basualdo C, Sgroy V, Finola MS, Marioli JM: Comparison of the
Antibacterial Activity of Honey from Different Provenance Against
Bacteria Usually Isolated from Skin Wound. Veterinary Microbiology
2007, 124:375-381.
Mulu A, Tessema B, Derbie F: In vitro assessment of the antimicrobial
potential of honey on common human pathogen. Ethiop J Health Dev
2004, 18(2):107-112.
Johnson RMR: R.M.S: Prtial Thickness Burns: Identification and
Maangemenat. Advances in Skin and Wound 2003, 16(4):178-187.
Shubangi Bhende: In-Vitro Assessment of Chlorhexidine GluconateImpregnated Polyurethane Foam Antimicrobial Dressing Using Zone
of Inhibition Assay. Infection Control and Hospital Epidemiology 2004,
25(8):664-667.
Molan P: Honey as an antimicrobial agent. New York: Plenum Press;
1997.
Danilla SAP, Gomez ME, Chamorro M, Leniz P, Pineros JL, Lianos S, Roco H,
Correa G, Pasten JA, Eulufi A, Roa R, Calderon W: Concordance between
qualitative and quantitative culture in burned patients analysis of 2008
cultures. Burns 2005, 31:967-971.
Steer JA, Papini R.P.G, Wilson A.P.R, McGrouther GA, Parkhouse N:
Quantitative microbiology in the management of burn patient. II.
Relationship between bacterial counts obtained by burn wound
biopsy culture and surface alginate swab culture, with clinical
outcome following burn surgery and change of dressings. Burns 1996,
22(3):177-181.
Church DES, Reid O, Winston B, Lindsay R: Burn Wound Infection. Clinical
Microbiology Review 2006, 19(2):403-434.
Gosh K, Clark R.A.F: Principle of tissue engineering. 3rd edition. Elsevier
B.V; 1997.
Nasser SMA, Maher A: Colonization of burn wounds in Ain Shams Burn
Unit. Burns 2003, 29:229-233.
Seal DV, Hay RJ, Middleton KR: Skin and wound infection investigation
and treatment in practice. United Kingdom: Martin Dunitz Ltd; 2000.
Nasir et al. BMC Complementary and Alternative Medicine 2010, 10:31
http://www.biomedcentral.com/1472-6882/10/31
25. Dastouri MR, Fakhimzadeh K, Shayeg J, Dolgari-Sharaf J, Valilou MR,
Maheri-Sis N: Evaluating antibacterial activity of the Iranian honey
through MIC method on some dermal and intestinal pathogenic
bacteria. J of Animal and Veterinary Advances 2008, 7(4):409-412.
26. Jones S, Bowler PG, Walker M: Antimicrobial activity of silver-containing
dressing in influenced by dressing conformability with a wound
surface. Wounds 2005, 17(9):263-270.
Pre-publication history
The pre-publication history for this paper can be accessed here:
http://www.biomedcentral.com/1472-6882/10/31/prepub
doi: 10.1186/1472-6882-10-31
Cite this article as: Nasir et al., Antibacterial properties of tualang honey and
its effect in burn wound management: a comparative study BMC Complementary and Alternative Medicine 2010, 10:31
Page 7 of 7
Vous aimerez peut-être aussi
- 05 N002 46800Document18 pages05 N002 46800Anonymous sllHltPas encore d'évaluation
- EJCP Jurnl JiwaDocument3 pagesEJCP Jurnl JiwaAnonymous sllHltPas encore d'évaluation
- A Review of Various Approaches To Face Hallucination: SciencedirectDocument9 pagesA Review of Various Approaches To Face Hallucination: SciencedirectAnonymous sllHltPas encore d'évaluation
- Gagal TumbuhDocument6 pagesGagal TumbuhTeofilus KristiantoPas encore d'évaluation
- DI Profile Kenya PDFDocument4 pagesDI Profile Kenya PDFAnonymous sllHltPas encore d'évaluation
- U0015 0000001 0000797Document99 pagesU0015 0000001 0000797Anonymous sllHltPas encore d'évaluation
- Factors Associated With Exclusive Breastfeeding Among Mothers Seen at The University of Nigeria Teaching HospitalDocument4 pagesFactors Associated With Exclusive Breastfeeding Among Mothers Seen at The University of Nigeria Teaching HospitalAnonymous sllHltPas encore d'évaluation
- Betamethasone Gel Reduces Postoperative Sore ThroatDocument6 pagesBetamethasone Gel Reduces Postoperative Sore ThroatriddickvbPas encore d'évaluation
- Jurnal Asli Kelompok 8Document5 pagesJurnal Asli Kelompok 8Anonymous sllHltPas encore d'évaluation
- EngDocument65 pagesEngWhinet Jojo TerunaPas encore d'évaluation
- Account Information - Account Statement: Date Description Branch Amount BalanceDocument7 pagesAccount Information - Account Statement: Date Description Branch Amount BalanceAnonymous sllHltPas encore d'évaluation
- OUTPUT STATISTIK PrinDocument16 pagesOUTPUT STATISTIK PrinAnonymous sllHltPas encore d'évaluation
- Sea Food Fried Rice RecipeDocument2 pagesSea Food Fried Rice RecipeAnonymous sllHltPas encore d'évaluation
- Explore the Mentawai Tribe and Rainforests of Siberut IslandDocument2 pagesExplore the Mentawai Tribe and Rainforests of Siberut IslandAnonymous sllHltPas encore d'évaluation
- No Sedan G 2 Sedan G 2: Juml Ah Kateg Ori Kod IngDocument4 pagesNo Sedan G 2 Sedan G 2: Juml Ah Kateg Ori Kod IngAnonymous sllHltPas encore d'évaluation
- Presentation: - Work in Group - Choose A Topic Related To The Issues of Health - Min.8 Slides Max.15 SlidesDocument5 pagesPresentation: - Work in Group - Choose A Topic Related To The Issues of Health - Min.8 Slides Max.15 SlidesAnonymous sllHltPas encore d'évaluation
- E-Journal Impaired Endothelium-Dependent Vasodilatation in PDFDocument7 pagesE-Journal Impaired Endothelium-Dependent Vasodilatation in PDFAnonymous sllHltPas encore d'évaluation
- On Saturday Morning at 9Document3 pagesOn Saturday Morning at 9Anonymous sllHltPas encore d'évaluation
- Arch Dis Child 1988 Cole 1007 9Document4 pagesArch Dis Child 1988 Cole 1007 9Anonymous sllHltPas encore d'évaluation
- Penatalaksanaan Hipertensi Pada Lanjut Us1a (DR Ra Tuty K)Document6 pagesPenatalaksanaan Hipertensi Pada Lanjut Us1a (DR Ra Tuty K)Ayu Isyana WardhaniPas encore d'évaluation
- Lyric of Pink - Just Give Me A ReasonDocument2 pagesLyric of Pink - Just Give Me A ReasonDwiyana DharmayasaPas encore d'évaluation
- Topic Presentation IsDocument18 pagesTopic Presentation IsAnonymous sllHltPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Guns, Germs, & SteelDocument20 pagesGuns, Germs, & Steelapi-25956160100% (1)
- Epidemiological TriadDocument14 pagesEpidemiological TriadmanjulaPas encore d'évaluation
- Diagnostics 13 00220Document20 pagesDiagnostics 13 00220msworkbbhPas encore d'évaluation
- Hepatitis Viruses Combination (Blood Borne Pathogens)Document51 pagesHepatitis Viruses Combination (Blood Borne Pathogens)Hosam GomaaPas encore d'évaluation
- Immunity To Parasitic Infections 3Document33 pagesImmunity To Parasitic Infections 3Fikadu AberaPas encore d'évaluation
- IM - Patient Esguera (Final)Document4 pagesIM - Patient Esguera (Final)k.n.e.d.Pas encore d'évaluation
- COCONUT OIL 101 Miraculous Coconut Oil Benefits Cures Uses and Remedies by Victoria Lane PDFDocument22 pagesCOCONUT OIL 101 Miraculous Coconut Oil Benefits Cures Uses and Remedies by Victoria Lane PDFedwinw18Pas encore d'évaluation
- Asuncion, Rachel Mae (Infectious Dse)Document3 pagesAsuncion, Rachel Mae (Infectious Dse)Rachel AsuncionPas encore d'évaluation
- Matary Differential Diagnosis 2013Document128 pagesMatary Differential Diagnosis 2013Raouf Ra'fat Soliman100% (9)
- Pancytopenia: Clinical Approach: Ajai Kumar Garg, AK Agarwal, GD SharmaDocument5 pagesPancytopenia: Clinical Approach: Ajai Kumar Garg, AK Agarwal, GD SharmaYudhistiraPas encore d'évaluation
- Treatment of Rheumatoid Arthritis in Patients With Concomitant Chronic Hepatitis C InfectionDocument24 pagesTreatment of Rheumatoid Arthritis in Patients With Concomitant Chronic Hepatitis C InfectionMuhammad Farras Razin PerdanaPas encore d'évaluation
- Prokaryotic Cell-1Document26 pagesProkaryotic Cell-1Sarah PavuPas encore d'évaluation
- The Philippines Recommends For Animal Health CareDocument7 pagesThe Philippines Recommends For Animal Health CarePaul ValcorzaPas encore d'évaluation
- Dermal Arteritis of The Nasal Philtrum in A Giant Schnauzer and Three Saint Bernard DogsDocument7 pagesDermal Arteritis of The Nasal Philtrum in A Giant Schnauzer and Three Saint Bernard DogsjenPas encore d'évaluation
- Module 3 BiocontainmentDocument7 pagesModule 3 BiocontainmentAzraPas encore d'évaluation
- Pathophysiology of Hansen's DiseaseDocument1 pagePathophysiology of Hansen's DiseaseGrace Lyn Borres ImpasPas encore d'évaluation
- Antimicrobial Susceptibility Testing - Primer For CliniciansDocument20 pagesAntimicrobial Susceptibility Testing - Primer For Cliniciansdipzhit100% (1)
- Health: Quarter 3 - Module 3A Disease Prevention and Control of Communicable DiseaseDocument15 pagesHealth: Quarter 3 - Module 3A Disease Prevention and Control of Communicable DiseaseJnJ AntonioPas encore d'évaluation
- Anatomi dan Patofisiologi Aneurisma Sinus ValsalvaDocument16 pagesAnatomi dan Patofisiologi Aneurisma Sinus ValsalvaKhandar YosuaPas encore d'évaluation
- Valadi - Guillain-Barré SyndromeDocument5 pagesValadi - Guillain-Barré SyndromeMarcelo BedoyaPas encore d'évaluation
- Sample Write UpDocument4 pagesSample Write UpMaha Mohamed100% (1)
- Genitourinary SystemDocument93 pagesGenitourinary Systemraene_bautistaPas encore d'évaluation
- Blueberry Ipm PosterDocument1 pageBlueberry Ipm PosterDejan PanticPas encore d'évaluation
- Loop Mediated Isothermal Amplification (LAMP) - An Alternative To Polymerase Chain Reaction (PCR)Document16 pagesLoop Mediated Isothermal Amplification (LAMP) - An Alternative To Polymerase Chain Reaction (PCR)amelia nurdiniPas encore d'évaluation
- Reverse Vaccinolgy - PresntationDocument20 pagesReverse Vaccinolgy - PresntationselnikrajPas encore d'évaluation
- CHN 1 Immunization ProgramDocument12 pagesCHN 1 Immunization ProgramKyle VargasPas encore d'évaluation
- Hepatitis E InfectionDocument27 pagesHepatitis E Infectiontummalapalli venkateswara raoPas encore d'évaluation
- Approach To The Patient With Diarrhea and MalabsorptionDocument19 pagesApproach To The Patient With Diarrhea and MalabsorptionFitriyana Winarno100% (1)
- Nervous System Disorders and MeningitisDocument42 pagesNervous System Disorders and MeningitisRifqi FuadiPas encore d'évaluation
- Index To Medicine and Colonialism PDFDocument6 pagesIndex To Medicine and Colonialism PDFPickering and ChattoPas encore d'évaluation