Académique Documents
Professionnel Documents
Culture Documents
Assessment and Approach of Patients With Severe Dementia: by Bernard Groulx, MD, FRCPC
Transféré par
sonoiochecomandoDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Assessment and Approach of Patients With Severe Dementia: by Bernard Groulx, MD, FRCPC
Transféré par
sonoiochecomandoDroits d'auteur :
Formats disponibles
Assessment and Approach of
Patients with Severe Dementia
In the past five years, a number of instruments have been made available for the treatment of
moderate to advanced Alzheimers disease (AD). The second installment of this two-part
article focuses on 12 principles for treating advanced AD.
by Bernard Groulx, MD, FRCPC
he first part of this article,1
expertly written by Dr. Serge
Gauthier, updated us on new instruments and evaluation scales that
allow us to better study the advanced
stages of Alzheimers disease (AD),
as well as the clinical benefits of
cholinergic agents and memantine.
For the second part of this article,
I could have written about the benefits of neurotropics (antidepressants,
neuroleptics, etc.), especially for
behavioral problems commonly
associated with the advanced stages,
but I chose not to. First of all, several articles on the subject have
already been published in past
issues of the Review.2,3 Second, as
the disease progresses, behavioral
problems that do not respondor
respond poorlyto neurotropics
also increase. Such is the case, for
example, observed in disinhibition,
and screaming and wailing.4,5
What can we do when our routine toolsmedicationsgive us
disappointing results? We need to
get back to basics, back to square
one, to a better understanding of the
very nature of this terrible disease.
Retrogenesis
Dr. Groulx is Chief Psychiatrist,
Ste-Anne-de-Bellevue Hospital
and Associate Professor, McGill
University, Montreal, Quebec.
No one understood the nature of AD
better nor described it as well as
Reisberg when he introduced the
concept
of
retrogenesis.6-8
Retrogenesis, already described in
the Review,9,10 demonstrates that
people suffering from AD lose their
cognitive skills and abilities virtually
in the reverse order in which they
learned them. This explains the fact
that, in the early stages of the dis-
10 The Canadian Review of Alzheimers Disease and Other Dementias
ease, patients lose skills acquired
during adolescence (planning,
judgment, social skills, etc.) at the
same time or perhaps even before
their cognitive skills deteriorate.
In the later stages of this disease,
patients regress, feeling and
behaving like two- to five-year-old
children (stage 6) and zero- to
two-year-olds (stage 7), with emotional needs, fears and anxieties.
Stage 6
During this stage, which lasts
approximately two and a half years
and is typically characterized by
behavioral disorders, patients
quickly go from an MMSE score of
10 to a score of zero. When we try
to classify them, we quickly find
evidence to this effect.11 Some of the
dysfunctional behavior is the result
of psychiatric problems that have a
good chance of responding to a pharmacologic approach (Table 1).
Many more behavioral disorders,
however, will not respond or will
respond poorly because they are the
result of retrogenesis. In many cases,
behavioral disorders are reactions to
this regressive or even normal state,
given the context (Table 2). If we
think of an agitated two- or threeyear-old child in an unfamiliar environment with strangers taking care
of them, some of this behavior
(intrusive behavior, disinhibition,
obstinacy, hoarding items, getting
dressed or undressed inappropriately, asking repetitive questions, hiding objects, trying to remove any
restraints, etc.) is certainly not atypical or incomprehensible.
Stage 7
Many patients, I would almost say
happily, do not make it to stage 7.
Many die at the end of stage 6,
often due to pneumonia, a disease
Mark Twain referred to as the
elderlys best friend. Patients
who progress until the final stage of
AD will regress to a mental age of
two to zero years. At the beginning
of this stage, they are able to walk,
but they will eventually lose that
ability. They will only be able to sit
down and will become bedridden,
lying in increasingly fetal positions
due to muscle contraction.
Assessment
In stages 6 and 7, understanding
what the patient is experiencing,
making astute observations and having a good imagination will help
alleviate patients mental pain and
resolve their behavioral problems. Is
there an internal cause for their agitation? Is the patient hungry or
thirsty and unable to express his or
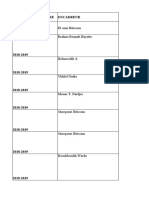
Table 1
Dysfunctional Behaviors in the Elderly with Dementia which
may be Amenable to Pharmacotherapeutic Management
1. Anxiousness: restlessness (hand-wringing, pressured pacing, etc.), fidgeting,
agitation, sometimes self-mutilation
2. Sadness: crying, anorexia, insomnia (particulaly terminal awakening),
nihilism, guilty/paranoid thinking, morbid preoccupation with death
3. Withdrawn: apathy, quiet negativity, anorexia, sullenness, uncooperation,
frequent mutedness, stuporous
4. Markedly bizarre or regressed behavior from previous standards (including
personal appearance and lifetime moral standards)
5. Over-elation: insomnia, psychomotor hyperactivity, rapid/pressured speech,
often disorganized thinking
6. Overly boisterous: verbal hostility, aggressiveness, argumentativeness,
belligerence, physically assaultive
7. Delusions: ideas of influence and reference, jealousy, paranoia, fear,
persecution, grandiosity, and/or tactile (formication)
8. Hallucinations: primarily auditory, visual, and/or tactile (formication)
her needs because he or she has lost
the ability to speak? Is the patient
constipated? Is he or she suffering
from a urinary infection or any other
hidden medical problem? Above all,
is the patient in pain and, again, incapable of expressing himself or herself verbally?
Does the patient respond to an
external cause, meaning the
patients setting or environment? Is
the environment too complex? Does
the patient have too many elements
to cope with? Do the physical, psychological, architectural or other
(environmental) demands exceed
their abilities? Is the environment
overstimulating? Understimulating?
More important, is the environment
hostile? Are the interventions or
interactions from caregivers not
consistent enough, given that
patients see three different groups of
caregivers on the same day?
It is clear that, in the advanced
stages of AD, the most therapeutic
approach is based on understanding retrogenesis: constantly
adjusting to patients (and not the
other way around), understanding
what they are feeling as they are
undergoing this inevitable regression. This approach will result in
interventions that meet the real
needs of patients, delivered in a
professional and, it must be stated,
compassionate manner.
Therapeutic Approach
Allow me to refer to some principles9 that are useful in providing
healthcare interventions to patients
in the advanced stages of AD who
are agitated or in mental pain.
Determine who is agitated.
Ask yourself who is really agitated in a specific situation. Is it the
patient, a member of the family or
The Canadian Review of Alzheimers Disease and Other Dementias 11
Table 2
Dysfunctional Behaviors in the Elderly with Dementia
Usually Not Amenable to Pharmacotherapeutic Management
1. Wandering without aim, pacing
11.Spitting
2. Inappropriate ambulation into
others rooms, toilets, beds
12. Inappropriate undressing/dressing
3. Inappropriate, insulting, hostile or
obnoxious verbalizing (including
perseveration, echolalia,
incoherence, calling out, cursing,
strange noises, yelling or screaming)
13.Constant requests, comments, or
questions
14.Prolonged, frequent repetition of
words/sentences
15. Hiding things
4. Annoying activities (touching, hugging,
unreasonable requests, invading
personal space, banging a walker,
repetitive tapping, rocking, etc.)
16.Pushing a wheelchair-bound
patient
5. Hypersexuality (verbal or physical)
18.Inadvertently putting oneself or
someone else in a hazardous
situation/place
6. Innappropriate sexual activities
(including public masturbation,
exposing oneself)
7. Willfulness or other difficult
personality traits (including refusing
treatments, medications, care or food)
17.Tearing things; flushing items
down the toilet
19.Eating inedible objects (including
feces)
20.Bumping into objects, tripping
over someone or something
8. Hoarding materials (pencils,
straws, cups, toiletries, clothes,
etc. from other patients, nursing
stations, med carts, etc.)
21. Tugging at/removal of restraints
9. Appropriating (stealing) items
from other patients and staff
(glasses, teeth, etc.)
23.Inappropriate isolation (e.g.,
refusal to leave room or socialize)
22.Physical self-abuse (e.g.,
scratching or picking at oneself,
banging head, removing catheter)
10.Inappropriate urination/defecation
(including smearing feces)
24. Physically disruptive (dumping or
throwing food trays, eating from
anothers tray, lying on the floor)
a healthcare provider who is concerned with the patients behavior?
Ensure that the physical environment meets the patients
needs. Organizing the patients
environment should be the first
therapeutic measure taken. The
patients room should be well lit
and adapted to the elderly (calendars, schedules, a clock and familiar objects from the patients
home should also be placed within view). The patient must be able
to have contact with family mem-
bers and have enough room to
move around.
Particular attention should
be paid to the attitude of caregivers. They must reassure
patients, treat them with respect,
help them become aware of their
environment and orient them
every time they interact with
them. The patients functional
capacity must be re-assessed on a
regular basis so caregivers can
modify their interactions accordingly. Personality conflicts
12 The Canadian Review of Alzheimers Disease and Other Dementias
between patients and healthcare
providers must be resolved quickly.
Speak to your patients. It is
easy for us to forget to speak to
patients with advanced AD, especially if they are aphasic and unresponsive. There is nothing better
to reassure AD patients and calm
them than speaking to them in a
natural manner. Telling them what
is going on in the care unit, speaking to them about their past interests or giving them news about
their family creates a normal environment, not to mention that talking to them has therapeutic value
and helps to strengthen the bond
between healthcare professionals
and patients.
Resist the natural temptation to
probe AD patients for information.
It may be difficult for them to answer
simple questions, such as What is
wrong? or Why are you angry?
which will only make them more
confused. Connect with them instead
by saying, for example, I know that
you are angry or You are not feeling well, but I will help youmessages that are much more positive.
Develop efficient communication strategies. In Table 3, you will
find the acronym FOCUSED
which reminds us of the major principles of efficient communication
with patients with advanced AD.12
Avoid construing a patients
agitation, aggressiveness or violence as a personal attack.
Caregivers should never think that
such behavior is directed at them
personally or that their patient is
angry with them.
Never underestimate the benefits of physical activity. Regular
physical activity channels patients
energy, helps them sleep better, and
increases their general well-being.
Never underestimate the benefits of distracting patients during
a crisis. Bring the patient into
another room or suggest another
activity, such as eating, which may
help diffuse aggressive outbursts.
Provide consistent interventions. Regardless of the type of care
plan or strategies that have been
adopted for the patient, make sure
the plan is applied on a regular basis
by the staff of all three work shifts.
The patients family members
are the professional caregivers
best allies. When patients are agitated, the presence of their loved
ones reassures them.
Finally, if the patient is agitated, determine the cause. If the
behavioral problem is a new one,
assess the patients gestures and
try to find out what causes it. If
the disruptive behavior is something the patient has done before,
References:
1. Gauthier S. Treatment of Advanced
Alzheimers Disease (Part I). The Canadian
Alzheimer Disease Review 2005; 8(1):4-6.
2. Van Reekum R. Disinhibitions in
Alzheimers disease: Assessment, prevalence and management. The Canadian
Alzheimer Disease Review 2002; 5(1):4-9.
3. Herrmann N. Pharmacotherapy of
Behavioral Disturbances in Dementia.
The Canadian Alzheimer Disease
Review 1998; 1(2):6-8.
4. Groulx B. Screaming and Wailing in
Dementia patients (Part I). The Canadian
Alzheimer Disease Review 2004; 6(2):11-14.
Table 3
FOCUSED Communication Strategies in Dementia
Face to face:
- face the patient directly
- attract the patients attention
- maintain eye contact
Orientation:
- orient the patient by repeating key words several times
- repeat sentences exactly
- give the patient time to comprehend
Continuity:
- continue the same topic of conversation for as long as possible
- prepare the patient if a new topic must be introduced
Unsticking:
- help the patient become unstuck if he uses a word
incorrectly by suggesting the word hes looking for
- repeat the patients sentence using the correct word
Structure:
- structure your questions to give the patient a simple choice to
respond with
- provide only two options at a time
- provide options the patient would like
Exchange:
- keep up normal exchange of ideas found in conversation
- begin conversations with pleasant, normal topics
- ask easy questions the patient can answer
- give the patient clues as to how to answer
Direct:
- keep sentences short, simple and direct
- use and repeat nouns rather than pronouns
- use hand signals, pictures and facial expressions
find out what caused it in the past
and, more important, find out
what helped resolve the problem.
AD, especially in the advanced
stages, seems to be the most horrible disease. Nonetheless, when we
think of the last 15 years and the
next 25, hope reigns. With two dif-
ferent classes pf medication now
available, there is every reason to
hope for major therapeutic breakthroughs with pharmacologic
research and, perhaps, source cells.
With a better understanding of the
real needs of AD patients, clinicians
and caregivers will be able to provide
a level of healthcare that is increasingly human and compassionate.
5. Groulx B. Screaming and Wailing in
Dementia patients (Part II). The Canadian
Alzheimer Disease Review 2005; 8(1):7-11.
6. Eastwood R, Reisberg B. Mood and behavior, in: Gauthier S (ed): Clinical Diagnosis
and Management of Alzheimer's Disease,
Martin Dunitz, London, 1996, pp. 175-89.
7. Reisberg B, Ferris SH, DeLeon MJ. The
global deterioration scale for assessment
of primary degenerative dementia. Am. J
Psychiatry 1982; 139(9):1136-9.
8. Reisberg B. Functional assessment staging (FAST). Psychopharmacological
Bulletin 1988; 24:653-9.
9. Groulx B. Nonpharmacologic Treatment
of Behavioral Disorders in Dementia.
The Canadian Alzheimer Disease
Review 1998; 2(1):6-8.
10. Tanguay A. The progressive course of
AD: A training tool for caregivers. The
Canadian Alzheimer Disease Review
2002; 5(1):10-2.
11. Maletta GJ. Treatment of behavioral symptomatology of AD, with emphasis on
aggression: Current clinical approaches. Int
Psychogeriatr 1992; 4(Suppl 1):117-30.
12. Ripich DN. Functional communication
with AD patients: A caregiver training
program. Alzheimer Dis Assoc Disord
1994; 8(3):95-109.
Conclusion
The Canadian Review of Alzheimers Disease and Other Dementias 13
Vous aimerez peut-être aussi
- The Mental Status ExamDocument3 pagesThe Mental Status ExamShrests SinhaPas encore d'évaluation
- The Mental Status Exam (MSE)Document5 pagesThe Mental Status Exam (MSE)Huma IshtiaqPas encore d'évaluation
- A Simple Guide to Dementia and Alzheimer's DiseasesD'EverandA Simple Guide to Dementia and Alzheimer's DiseasesÉvaluation : 5 sur 5 étoiles5/5 (1)
- PsychopathologyDocument6 pagesPsychopathologybrookegzi88Pas encore d'évaluation
- Clinical Case Scenarios PDF 136292509 PDFDocument23 pagesClinical Case Scenarios PDF 136292509 PDFRheeza Elhaq100% (2)
- Global Mental Health Around The World: A Global Look At Depression: An Introductory Series, #9D'EverandGlobal Mental Health Around The World: A Global Look At Depression: An Introductory Series, #9Pas encore d'évaluation
- Azheimer Disease III How is it treated? What is its evolution? How do you prevent it?D'EverandAzheimer Disease III How is it treated? What is its evolution? How do you prevent it?Pas encore d'évaluation
- Behavioral and Psychological Disturbances in Alzheimer Disease: Assessment and TreatmentDocument11 pagesBehavioral and Psychological Disturbances in Alzheimer Disease: Assessment and Treatmenttiara perdana pPas encore d'évaluation
- Tugas Skill - UnlockedDocument9 pagesTugas Skill - Unlockednamasaya1Pas encore d'évaluation
- Autism Spectrum Disorder: A guide with 10 key points to design the most suitable strategy for your childD'EverandAutism Spectrum Disorder: A guide with 10 key points to design the most suitable strategy for your childPas encore d'évaluation
- Assessment of The Older Adults (Geriatrics)Document14 pagesAssessment of The Older Adults (Geriatrics)Yna Joy B. LigatPas encore d'évaluation
- Summary of The Man Who Mistook His Wife for a Hat: by Oliver Sacks | Includes AnalysisD'EverandSummary of The Man Who Mistook His Wife for a Hat: by Oliver Sacks | Includes AnalysisPas encore d'évaluation
- Final Capstone PaperDocument15 pagesFinal Capstone Paperapi-478784238Pas encore d'évaluation
- Psych p3Document8 pagesPsych p3Fatima MajidPas encore d'évaluation
- Alzheimer's Disease Student's Name Student's ID Course NameDocument7 pagesAlzheimer's Disease Student's Name Student's ID Course NameandrewPas encore d'évaluation
- Research ProposalDocument17 pagesResearch Proposalmullamuskaan95Pas encore d'évaluation
- Complex Cases and Comorbidity in Eating Disorders: Assessment and ManagementD'EverandComplex Cases and Comorbidity in Eating Disorders: Assessment and ManagementPas encore d'évaluation
- CBT Manual OcdDocument19 pagesCBT Manual OcdRedefining Self with MeghaPas encore d'évaluation
- Understanding The Individual With Alzheimer's Disease: Can Socioemotional Selectivity Theory Guide Us?Document10 pagesUnderstanding The Individual With Alzheimer's Disease: Can Socioemotional Selectivity Theory Guide Us?Andre ZulkhasogiPas encore d'évaluation
- Mental Health Case StudyDocument15 pagesMental Health Case Studyapi-508142358Pas encore d'évaluation
- Dealing with Depression: A commonsense guide to mood disordersD'EverandDealing with Depression: A commonsense guide to mood disordersÉvaluation : 2 sur 5 étoiles2/5 (1)
- CognitiveDocument19 pagesCognitiveLaila MajenumPas encore d'évaluation
- The Dysregulated Adult: Integrated Treatment ApproachesD'EverandThe Dysregulated Adult: Integrated Treatment ApproachesPas encore d'évaluation
- Older People - Patterns of Illness, Physiological Changes and Multiple PathologyDocument4 pagesOlder People - Patterns of Illness, Physiological Changes and Multiple PathologyTweenie DalumpinesPas encore d'évaluation
- Group 6 Revised Final Research With AppendicesDocument71 pagesGroup 6 Revised Final Research With AppendicesAbby GutierrezPas encore d'évaluation
- Hysteria: Personal PracticeDocument2 pagesHysteria: Personal PracticeNando AswinPas encore d'évaluation
- Weathering the Storm: A Guide to Understanding and Overcoming Mood DisordersD'EverandWeathering the Storm: A Guide to Understanding and Overcoming Mood DisordersPas encore d'évaluation
- Abnormal Psychology IntroductionDocument11 pagesAbnormal Psychology IntroductionAyesha FayyazPas encore d'évaluation
- Ocd-Treatment Publishing NardoneDocument62 pagesOcd-Treatment Publishing Nardoneneri100% (2)
- When Traditional CareDocument23 pagesWhen Traditional CareEvaPas encore d'évaluation
- Alzheimer's Disease: The Complete IntroductionD'EverandAlzheimer's Disease: The Complete IntroductionÉvaluation : 3 sur 5 étoiles3/5 (3)
- Study Notes PsychiatryDocument50 pagesStudy Notes PsychiatryMedShare90% (10)
- Mood DisordersDocument14 pagesMood DisordersHayat AL AKOUMPas encore d'évaluation
- Obsessive-Compulsive Disorder: Clinical Picture and Cognitive-Behavioral Treatment ImplicationsDocument45 pagesObsessive-Compulsive Disorder: Clinical Picture and Cognitive-Behavioral Treatment Implicationstennisnavis4Pas encore d'évaluation
- Alzheimer's Disease MemorDocument11 pagesAlzheimer's Disease MemorPatrick OrtizPas encore d'évaluation
- Overcoming Bipolar Disorder - 17 Ways To Manage Depression And Multiple Moods Without Going CrazyD'EverandOvercoming Bipolar Disorder - 17 Ways To Manage Depression And Multiple Moods Without Going CrazyPas encore d'évaluation
- Examen Final de Idioma II InglesDocument5 pagesExamen Final de Idioma II InglesLa Spera OttavaPas encore d'évaluation
- Body Dysmorphic DisorderDocument6 pagesBody Dysmorphic DisorderAllan DiasPas encore d'évaluation
- Final PaperDocument7 pagesFinal Paperapi-339682129Pas encore d'évaluation
- Davys Ongwae Assignment 2Document5 pagesDavys Ongwae Assignment 2Isaac MwangiPas encore d'évaluation
- Literature ReviewDocument7 pagesLiterature ReviewResianaPutriPas encore d'évaluation
- Depression and The Elderly - FinalDocument8 pagesDepression and The Elderly - Finalapi-577539297Pas encore d'évaluation
- Psychopathology PDFDocument26 pagesPsychopathology PDFBenedicte NtumbaPas encore d'évaluation
- Abnormal PsychologyDocument70 pagesAbnormal PsychologyHec ChavezPas encore d'évaluation
- Chap12 Abnormal PsychDocument34 pagesChap12 Abnormal PsychshaigestPas encore d'évaluation
- FRAILTY - Someone Who Is Skinny, Weak and Vulnerable (Cannot Be Diagnosed Based On Appearance)Document14 pagesFRAILTY - Someone Who Is Skinny, Weak and Vulnerable (Cannot Be Diagnosed Based On Appearance)Jhon Mark Miranda Santos100% (1)
- Analyse The Biological and Diathesis-Stress Paradigms To Psychopathology and Comment About Their Strengths and Weaknesses.Document5 pagesAnalyse The Biological and Diathesis-Stress Paradigms To Psychopathology and Comment About Their Strengths and Weaknesses.Paridhi JalanPas encore d'évaluation
- 20 Questions Psychiatric Emergencies PDFDocument4 pages20 Questions Psychiatric Emergencies PDFakelog getahunPas encore d'évaluation
- Patoloji Notlarım: Abnormal Psychology Family AggregationDocument5 pagesPatoloji Notlarım: Abnormal Psychology Family AggregationMelike ÖnolPas encore d'évaluation
- Mental RetardationDocument10 pagesMental RetardationYAMINIPRIYANPas encore d'évaluation
- The Man Who Mistook His Wife for a Hat: by Oliver Sacks | Key Takeaways, Analysis & Review: And Other Clinical TalesD'EverandThe Man Who Mistook His Wife for a Hat: by Oliver Sacks | Key Takeaways, Analysis & Review: And Other Clinical TalesPas encore d'évaluation
- Review of Related LiteratureDocument15 pagesReview of Related Literaturemarielle rumusudPas encore d'évaluation
- 16 Schragand Edwards Psychogenic Movement Disorders 2012Document10 pages16 Schragand Edwards Psychogenic Movement Disorders 2012آسيل محمدPas encore d'évaluation
- UnconsciousnessDocument6 pagesUnconsciousnessSeema RahulPas encore d'évaluation
- Calmer: Medical Events with Cognitively Impaired ChildrenD'EverandCalmer: Medical Events with Cognitively Impaired ChildrenPas encore d'évaluation
- Autism Revealed: All you Need to Know about Autism, Autistic Children and Adults, How to Manage Autism, and More!D'EverandAutism Revealed: All you Need to Know about Autism, Autistic Children and Adults, How to Manage Autism, and More!Pas encore d'évaluation
- Harciareketal 2011Document17 pagesHarciareketal 2011sonoiochecomandoPas encore d'évaluation
- Psychological Correlates of Sleep ApneaDocument14 pagesPsychological Correlates of Sleep ApneasonoiochecomandoPas encore d'évaluation
- Applying Skinner's Analysis of Verbal Behavior To Persons With DementiaDocument21 pagesApplying Skinner's Analysis of Verbal Behavior To Persons With DementiasonoiochecomandoPas encore d'évaluation
- Alzheimer in Down SyndromeDocument12 pagesAlzheimer in Down SyndromesonoiochecomandoPas encore d'évaluation
- Two Dimensions of Anosognosia in Patients With Alzheimer's Disease. Reliability and Validity of The Japanese Version of The Anosognosia Questionnaire For Dementia (AQ-D)Document7 pagesTwo Dimensions of Anosognosia in Patients With Alzheimer's Disease. Reliability and Validity of The Japanese Version of The Anosognosia Questionnaire For Dementia (AQ-D)sonoiochecomandoPas encore d'évaluation
- Sumerians Elamites Egyptians: AmoritesDocument5 pagesSumerians Elamites Egyptians: AmoritessonoiochecomandoPas encore d'évaluation
- Abdominsl Surgery MergedDocument141 pagesAbdominsl Surgery MergedTemitope AdeosunPas encore d'évaluation
- Paeds EMQDocument8 pagesPaeds EMQfasdPas encore d'évaluation
- Donanemab in Early Alzheimer's Disease: Original ArticleDocument14 pagesDonanemab in Early Alzheimer's Disease: Original ArticleBalla ElkhiderPas encore d'évaluation
- Computed Tomography & Magnetic Resonance Imaging: Neurological Disorder Diagnostic TestsDocument20 pagesComputed Tomography & Magnetic Resonance Imaging: Neurological Disorder Diagnostic TestsissaiahnicollePas encore d'évaluation
- Pneumonia in ChildrenDocument22 pagesPneumonia in ChildrenHarsha HinklesPas encore d'évaluation
- PESCI Recalls PDFDocument9 pagesPESCI Recalls PDFDanishPas encore d'évaluation
- PTSD and Autoimmune DiseasesDocument24 pagesPTSD and Autoimmune DiseasesEnida XhaferiPas encore d'évaluation
- Occt651 - Occupational Profile Paper - FinalDocument20 pagesOcct651 - Occupational Profile Paper - Finalapi-293182319Pas encore d'évaluation
- The Head and Neck Lectures: Anas Ibrahim YahayaDocument242 pagesThe Head and Neck Lectures: Anas Ibrahim YahayaBilkisu badamasiPas encore d'évaluation
- UNIVERSITY of SAN AGUSTIN - Capillary Electrophoresis Lecture 2023Document231 pagesUNIVERSITY of SAN AGUSTIN - Capillary Electrophoresis Lecture 2023alyssa apudPas encore d'évaluation
- Activity # 7 Fluid and Electrolyte Balance (WITH NCP)Document15 pagesActivity # 7 Fluid and Electrolyte Balance (WITH NCP)Louise OpinaPas encore d'évaluation
- Vitreomacular Traction: I Wayan Ardy Paribrajaka Vitreoretina Division of Bali Mandara Eye HospitalDocument29 pagesVitreomacular Traction: I Wayan Ardy Paribrajaka Vitreoretina Division of Bali Mandara Eye HospitalArdyPas encore d'évaluation
- CH 001Document6 pagesCH 001Maaz KhajaPas encore d'évaluation
- A Case of Alport Syndrome Presented With Bilateral Anterior LenticonusDocument3 pagesA Case of Alport Syndrome Presented With Bilateral Anterior LenticonusBOHR International Journal of Current Research in Optometry and Ophthalmology (BIJCROO)Pas encore d'évaluation
- Icmr Specimen Referral Form For Covid-19 (Sars-Cov2) : (If Yes, Attach Prescription If No, Test Cannot Be Conducted)Document2 pagesIcmr Specimen Referral Form For Covid-19 (Sars-Cov2) : (If Yes, Attach Prescription If No, Test Cannot Be Conducted)ShakirShafiPas encore d'évaluation
- Complications of DialysisDocument7 pagesComplications of DialysisDilessandro PieroPas encore d'évaluation
- Major Intra and Extracellular ElectrolytesDocument9 pagesMajor Intra and Extracellular ElectrolytesJana BluePas encore d'évaluation
- Biological Factors Responsible For Failure of Osseointegration in OralimplantsDocument7 pagesBiological Factors Responsible For Failure of Osseointegration in OralimplantsKarim MohamedPas encore d'évaluation
- Neuropsychiatry and Behavioral NeurologyDocument302 pagesNeuropsychiatry and Behavioral NeurologyTomas Holguin70% (10)
- Mehlmanmedical Hy Neuro Part IDocument18 pagesMehlmanmedical Hy Neuro Part IAzlan OmarPas encore d'évaluation
- Cutaneous Reactions To Chemo and RadiotherapyDocument37 pagesCutaneous Reactions To Chemo and Radiotherapyimdad khanPas encore d'évaluation
- RBCs Abnormal Morphology FinalDocument33 pagesRBCs Abnormal Morphology FinalInahkoni Alpheus Sky OiragasPas encore d'évaluation
- How To Write Killer AdsDocument15 pagesHow To Write Killer Adshfi11939100% (9)
- Gambar Rajah Menunjukkan Satu Neuron.: The Diagram Shows A NeuronDocument3 pagesGambar Rajah Menunjukkan Satu Neuron.: The Diagram Shows A Neuronkikio123Pas encore d'évaluation
- 1 thePoisonedNeedle PDFDocument432 pages1 thePoisonedNeedle PDFcas100% (4)
- Fats and OilsDocument36 pagesFats and Oilstafer692002100% (1)
- Biomechanical Basis of Foot Orthotic PrescriptionDocument6 pagesBiomechanical Basis of Foot Orthotic PrescriptionDusan OrescaninPas encore d'évaluation
- Catalogue Master 2019-2021Document309 pagesCatalogue Master 2019-2021ChaoukiMatimaticPas encore d'évaluation
- 6 - Neurodiagnostics II - Essentials of Neuroradiology LectureDocument44 pages6 - Neurodiagnostics II - Essentials of Neuroradiology LectureShailendra Pratap SinghPas encore d'évaluation
- Uploaded Activity 3 - Alyssa Angelaccio 1Document3 pagesUploaded Activity 3 - Alyssa Angelaccio 1api-544674720Pas encore d'évaluation