Académique Documents
Professionnel Documents
Culture Documents
Document
Transféré par
retCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Document
Transféré par
retDroits d'auteur :
Formats disponibles
Original Paper
Med Princ Pract 2008;17:290295
DOI: 10.1159/000129608
Received: July 10, 2007
Revised: October 7, 2007
Psychiatric Disorders in Tsunami-Affected
Children in Ranong Province, Thailand
Nawanant Piyavhatkul a Srivieng Pairojkul b Chanyut Suphakunpinyo b
Departments of a Psychiatry and b Pediatrics, Faculty of Medicine, Khon Kaen University, Khon Kaen, Thailand
Abstract
Objective: To study the prevalence of psychiatric disorders
in children affected by the Asian tsunami in Ranong province, Southern Thailand 10 months after the disaster. Subjects and Methods: The subjects were 47 boys and 47 girls,
age 118 years, who were affected by the tsunami. They
were participants in the Psychosocial Care and Protection
System for Tsunami-Affected Children in Ranong Province
project. The subjects were interviewed by a psychiatrist and
diagnoses were made according to DSM IV criteria. Results:
Of the 94 children, 47 (50%) had at least one psychiatric diagnosis: posttraumatic stress disorder (PTSD): n = 31 (33%);
major depression: n = 9 (9.6%); adjustment disorder: n = 9
(9.6%), and separation anxiety disorder: n = 3 (3.2%). The psychiatric diagnoses, specifically PTSD, were significantly associated with the childs age and exposure to the traumatic
events. Conclusion: Ten months after the tsunami disaster,
there is a high prevalence of psychiatric disorders in children, suggesting the importance of early identification, intervention and follow-up.
Copyright 2008 S. Karger AG, Basel
2008 S. Karger AG, Basel
10117571/08/01740290$24.50/0
Fax +41 61 306 12 34
E-Mail karger@karger.ch
www.karger.com
Accessible online at:
www.karger.com/mpp
Introduction
The Asian tsunami on the morning of December 26,
2004, as a result of an earthquake centered in the Indian
Ocean, measuring 9.09.3 on the Richter scale [1], devastated coastal areas of Indonesia, Thailand, Burma, Sri
Lanka, India and the Maldives. In Thailand, the area
along its Andaman Sea coastline of Krabi, Phang Nga,
Phuket, Ranong, Satun and Trang provinces were affected: 5,395 people died, 8,457 were injured and 2,817 were
missing [2], and 1,215 Thai children became orphans [3].
The tsunami destroyed 4,806 houses, 315 hotels and resorts, 4,365 fishing boats, 5,977 fish traps, and thousands
of acres of agricultural land, beach and coral reefs [24].
The disaster has had a major impact on the fishing and
coastal communities as well as the tourism industry.
Children experienced physical trauma from exposure
to the wave and psychological trauma from being in the
disaster. In addition they experienced the loss of significant persons, home, familiar community, school, teachers, property and lifestyle. The effect on livelihoods of
parents, resulting in economic and occupational disruption, also had an impact on the children. The Mental
Health Center for Thai Tsunami Disaster reported regressive symptoms in children, including enuresis, fear of
stranger, sleeping and eating problems, school and night
phobia, attention seeking, poor concentration, social isolation, poor school performance, depression, separation
Associate Prof. Nawanant Piyavhatkul
Department of Psychiatry, Faculty of Medicine
Khon Kaen University
Khon Kaen 40002 (Thailand)
Tel./Fax +66 43 348 384, E-Mail nawanant@kku.ac.th
Downloaded by:
139.195.64.201 - 7/2/2014 4:26:17 PM
Key Words
Psychiatric disorders Disaster Tsunami Posttraumatic
stress disorder Children
Background of the Study
In Ranong province, 156 Thai died, 215 were injured,
9 were missing, and 103 children lost their parents [3].
Three districts, 47 villages, 1,509 households and 5,942
individuals were affected by the tsunami. Two local health
centers were severely damaged and one school was totally destroyed [3]. One dyke, 27 piers, 10 bridges and 21
streets were destroyed [4]. The majority of the affected
people were Muslim.
Most of the affected children in Ranong had a disadvantaged background before the disaster. Many were
from the lower socioeconomic class, had poor housing or
grew up in a dysfunctional family with domestic violence, stepfamilies and single-parent homes with poor
child protection. These children were prone to chronic
developmental trauma associated with trauma spectrum
Post-Tsunami Psychiatric Disorders in
Children
disorders and other emotional and behavioral disturbance [16]. Trauma exposure affects what children anticipate and focus on and how they organize the way they
appraise and process information. Trauma-induced alterations in threat perception are expressed in how they
think, feel, behave, and regulate their biologic systems
[17]. And, trauma early in the life cycle has long-term effects on the neurochemical response to stress [18]. Therefore, some of the children may have already been vulnerable to psychological problems, which affected the incidence of psychiatric illnesses, when the natural disaster
occurred.
Longitudinal studies on the long-term effect of natural
disaster on children found that symptoms decreased with
time, but continue to have effects on the children. Shaw
et al. [19] evaluated the 21-month follow-up in schoolchildren exposed to Hurricane Andrew. There were a continuing high level of posttraumatic stress symptoms and
evidence of increasing emotional and behavioral problems. The result of the study of Karakaya et al. [20] on
secondary school students 3.5 years after the Marmara
earthquake showed that 22.2% of them had probable
PTSD and 30.8% had probable depression diagnoses.
Their anxiety levels were also higher than in the normal
population. Green et al. [21] did a 17-year follow-up of
child survivors of the Buffalo Creek dam collapse. The
rate of PTSD at the time of follow-up was 7% compared
to a postflood rate of 32%. This suggests that children
seem to continue to suffer from psychiatric disorders and
psychopathologies for many years after the disaster and
therefore, it is important to screen tsunami-affected children for the treatment and follow-up continuously. A
screening instrument is also needed to identify the severely affected population as the target group for intervention.
The objective of this research was to study the prevalence of psychiatric disorders in children affected by the
tsunami and investigate the association of the psychiatric
morbidity and the nature of the traumatic experience in
the 10 months following the tsunami.
Subjects and Methods
Two hundred and six children who lived in difficult situations
such as poverty, parental death or divorce after the tsunami were
enrolled in this project. However, only 94 who were directly affected by the tsunami were assessed; 89 were not directly affected
and the parents of the remaining 23 did not allow them to participate in the study. The 94 children were 47 boys and 47 girls,
ages 118 years. They were participants in the Psychosocial Care
Med Princ Pract 2008;17:290295
291
Downloaded by:
139.195.64.201 - 7/2/2014 4:26:17 PM
anxiety and somatic symptoms in 148 children up to 18
years old who were evaluated a few weeks after the disaster [5].
Exposure to the trauma, age, gender, social support,
difficulties at home and loss of significant others are variables that have been reported to be associated with psychiatric disorders or psychiatric symptoms in the children who have experienced natural disasters [613].
There are data available about psychiatric disorders in
children affected by the tsunami. For example, Neuner et
al. [14] studied 264 Sri Lankan children who lived in
coastal communities in severely affected areas and found
the prevalence rate of tsunami-related posttraumatic
stress disorder (PTSD) ranged between 14 and 39%. Five
hundred and twenty-three juvenile survivors of the tsunami in Tamil Nadu were studied using instruments validated in Tamil Nadu and found that the prevalence of
acute PTSD was as high as 70.7% and that there was delayed-onset PTSD in 10.9% [7]. Thienkrua et al. [15] studied children affected by the tsunami in Phang Nga,
Phuket, and Krabi provinces, Thailand, using a modified
version of the PsySTART Rapid Triage System, the UCLA
PTSD Reaction Index, and the Birleson Depression SelfRating Scale 2 months after tsunami. They found the
prevalence of PTSD symptoms were 13% among children
living in camps, 11% among children in affected villages
contrasted with 6% among children from unaffected villages. For depressive symptoms, the prevalence rates were
11, 5 and 8%, respectively. There was no epidemiological
data available on psychiatric disorders in tsunami-affected children in other areas of Thailand.
Results
There were 24 Buddhists and 70 Muslims. Most of
their parents were blue-collar workers and fishermen. At
the time of the evaluation, 57 (60.6%) children were living
with their parent(s) and the others were living with other
relatives. Sixty-five (69.1%) of them lost an important figure in their lives from the tsunami, 52 (55.3%) lost their
parent(s), and 31 (33.0%) lost other close relatives. Seventeen (18.1%) children lost the familys property. Sociodemographic data are shown in table 1. Sixty-five (69.1%)
children were exposed to the traumatic events caused by
the tsunami, 40 (42.6%) of them were directly exposed to
the tsunami and 42 (44.7%) were exposed to the traumatic events subsequent to the tsunami such as seeing dead
bodies or hearing about a horrible death of their loved
ones (table 2).
Psychiatric Disorders
Half of the children (n = 47) had at least one psychiatric diagnosis: PTSD: n = 31 (33%); major depressive episodes: n = 9 (9.6%); chronic adjustment disorder (unresolved grief): n = 9 (9.6%), and separation anxiety disorder: n = 3 (3.2%). One young girl had developmental
trauma. There were 4 (4.3%) children with mental retardation and 4 (4.3%) with attention deficit hyperactivity
disorder, 4 (4.3%) children had developmental disorders
unrelated to the tsunami. There were 8 (8.5%) children
with more than one diagnosis.
292
Med Princ Pract 2008;17:290295
Table 1. Sociodemographic data of the 94 children
Sociodemographic factors
Gender
Male
Female
Age, years
05
610
1115
1618
Religion
Buddhism
Islam
Educational status
Underage and kindergarten
Primary school
Secondary school
Parents occupation
Fisherman
Agricultural
Blue-collar worker
Merchant
Government service
Unemployed
Living status
With parent(s)
Other relative
Family background
Death of parent(s) from other causes
Parental divorce
47
47
50.0
50.0
18
36
37
3
19.1
38.3
39.4
3.2
24
70
25.5
74.5
26
44
24
27.4
46.8
25.5
34
5
34
18
2
1
36.2
5.3
36.2
19.1
2.1
1.1
57
37
60.6
39.4
19
31
20.2
33.0
Younger children had a higher prevalence of psychiatric diagnoses than the older children. The highest prevalence of PTSD and unresolved grief was among those 6
10 years of age. Boys had a higher prevalence of depression but lower unresolved grief than girls. There was a
higher prevalence of psychiatric disorder in the children
who were exposed to the event and the group that lost
a significant figure in their lives. Forty of 65 children
(61.5%) who were exposed to the traumatic events caused
by the tsunami had some psychiatric diagnosis. The children who were directly exposed to the tsunami had a
higher prevalence of PTSD but lower prevalence of depression and unresolved grief than the group that was
exposed to the traumatic events subsequent to the tsunami (seeing dead bodies or hearing about the horrible
death of their loved ones, table 2).
Factors Associated with Psychiatric Disorders
There was no association between psychiatric disorders and religion, parents occupation, parental divorce,
Piyavhatkul /Pairojkul /Suphakunpinyo
Downloaded by:
139.195.64.201 - 7/2/2014 4:26:17 PM
and Protection System for Tsunami-Affected Children in Ranong
Province project funded by Enfant Development, in the areas of
Kaper district and Sooksamran subdistrict. The information
leading to the inclusion of these children in the program was derived from information provided by the school and local citizens.
The study authors received permission from caretakers for the
children to participate in the research in October 2005, 10 months
after the tsunami.
Demographic data on age, gender, religion, parents occupations and education, current caretaker data and the nature of the
trauma from the tsunami were collected by research assistants at
the same time the assessment was being carried out by a psychiatrist doing the semistructured psychiatric interview protocol as
part of a broader psychosocial evaluation of the children in the
project. With younger children, the accompanied caretakers were
also interviewed. If a child had any psychiatric symptoms, additional probes were asked to determine a diagnosis. A checklist for
PTSD criteria and diagnoses was used to determine if a child met
DSM IV criteria. The data was analyzed using descriptive statistics, univariate analysis and bivariate logistic regression analysis
with a SPSS 11.5 program.
Table 2. Trauma, demographic data and psychiatric disorders
Gender
Male
Female
Age, years
05
610
1118
Trauma
Any loss
Loss of parent(s)
Loss of close relative(s)
Any exposure
Exposure to tsunami
Exposed to traumatic
events related to tsunami
Children
Any diagnosis
PTSD
Depression
SAD
47
47
50.0
50.0
24
23
51.1
48.9
18
36
40
19.1
38.3
42.6
10
25
12
65
52
31
65
40
69.1
55.3
33.0
69.1
42.6
42
44.7
Unresolved grief
15
16
31.9
34.0
7
2
14.9
4.3
0
3
0
6.4
3
6
6.4
12.8
55.6
69.4
30.0
3
18
10
16.7
50.0
25.0
3
2
4
16.7
5.6
10.0
1
1
1
5.6
2.8
2.5
2
6
1
11.1
16.7
2.5
37
29
18
40
24
56.9
55.8
56.3
61.5
60.0
22
14
11
31
21
33.8
26.9
34.4
47.7
52.5
8
7
4
7
3
12.3
13.5
12.5
10.8
7.5
3
2
1
2
1
4.6
3.8
3.1
3.1
2.5
9
9
4
6
1
13.8
17.3
12.5
9.2
2.5
26
61.9
18
42.9
11.9
2.4
16.7
SAD = Separation anxiety disorder.
Table 3. The positive results of binary backward stepwise logistic regression
Diagnosis
p value
Odds ratio
95% confidence interval
lower
upper
Any diagnosis
age 610 years
exposed to tsunami
exposed to event related to tsunami
0.000
0.012
0.031
7.631
3.961
2.929
2.483
1.361
1.103
23.452
11.525
7.781
PTSD
age 610 years
exposed to tsunami
exposed to event related to tsunami
0.017
0.000
0.019
3.894
7.635
3.655
1.279
2.514
1.240
11.854
23.194
10.770
Grief
age 610 years
exposed to event related to tsunami
0.015
0.042
24.987
7.810
1.879
1.078
332.368
56.577
Post-Tsunami Psychiatric Disorders in
Children
Discussion
In this study, psychiatric morbidity, especially PTSD,
was significantly associated with the childs age and exposure to the traumatic event, supportive of previous
findings [6, 11, 13, 1518]. Gender was not significantly
associated with PTSD, similar to the finding of McDermott et al. [10], which contrasted with the findings of
John et al. [6], Pynoos et al. [7] and Roussos et al. [9].
Our finding of a high prevalence of psychiatric morbidity in this sample fits with the concept of complex
trauma in children [22]. Our sample was from the popuMed Princ Pract 2008;17:290295
293
Downloaded by:
139.195.64.201 - 7/2/2014 4:26:17 PM
parental death from other causes, and the current caretaker when analyzed by univariate analysis. The results
of binary logistic stepwise backward regression analysis
showed that the psychiatric diagnosis and PTSD were significantly associated with the childs age and exposure to
the traumatic event caused by the tsunami (direct exposure to the tsunami or traumatic events related to tsunami). Major depressive episodes, separation anxiety disorder and comorbidity were not significantly associated
with any variables. Chronic adjustment disorder (unresolved grief reaction) was evidenced in the 6- to 10-year
age group who were exposed to the event (table 3).
294
Med Princ Pract 2008;17:290295
assessment or, most significant for this study, the time of
assessment after the disaster.
Our study demonstrates that chronic adjustment disorder (unresolved grief) was seen in children aged 610
years and was associated with exposure to dead bodies of
their loved ones or associated with hearing about horrible
deaths of their loved ones. There are no other studies that
mention this diagnosis and this association. Major depressive episodes, separation anxiety disorders and comorbidity were not significantly associated with any
variables.
We plan to follow up our sample for another 2.5 years
to see the long-term effect of tsunami on our children.
Limitation
A limitation of the study was the fact that the subjects
were selected from the Psychosocial Care and Protection
System for Tsunami-Affected Children in Ranong Province. Children were included who lost their parents in the
tsunami or were affected by the tsunami in other ways,
who were previously living in difficult situations, such as
divorce, death of the parents, or living with relatives.
Thus, they may not represent the general population of
the children who experienced the disaster.
Conclusion
Ten months after the Asian tsunami, there was a high
percentage of psychiatric disorders in tsunami-affected
children. The overall psychiatric morbidity and PTSD
were significantly associated with the childs age and exposure to the traumatic event. These results suggest the
importance of screening, follow-up and intervention for
these children.
Acknowledgment
We would like to thank Enfant Development for funding support for the Psychosocial Care and Protection System for Tsunami-Affected Children in Ranong Province project during
20052006.
Piyavhatkul /Pairojkul /Suphakunpinyo
Downloaded by:
139.195.64.201 - 7/2/2014 4:26:17 PM
lation who had a disadvantaged background prior to the
disaster, and who might have been exposed to repeated
trauma, which has been found to impact on the childs
affect regulation, attachment, behavioral regulation, integration of information and experience, cognition, selfconcept and regulation of the biologic systems [12]. Furthermore, kindling phenomena might occur when people
are repeatedly traumatized, which may lead to lasting
neurobiological and behavioral (characterological)
changes mediated by alterations in the temporal lobe [11].
Therefore, exposure to the developmental trauma before
the disaster might make some children more susceptible
to traumatization by the tsunami and the suffering of
loss.
Other researchers have studied the psychological impact of children affected by the tsunami and also found
a high prevalence of PTSD [6, 14]. On the other hand,
research on Thai children who lived in Phang Nga, Phuket, and Krabi provinces showed lower prevalence of
PTSD symptoms (613%) in tsunami-affected children
2 months after the tsunami [15] compared to 33% of
PTSD in our sample. They found the prevalence of depressive symptoms to be 511%, which is lower than the
prevalence in our study. Furthermore, when we combined major depressive disorder and chronic adjustment
disorder (unresolved grief), the prevalence of children
with significant depressive symptoms reached 19.2%.
The difference might be explained by the screening instruments that were utilized, since the cutoff points in
the Thai version [15] had not been validated for sensitivity and specificity in Thai children, and this study utilized a clinical diagnostic interview performed by a native Thai psychiatrist. There may also have been differences in the demographics of the study samples. For
example, there are more Muslim children and more
children with lower socioeconomic status and difficult
backgrounds in the affected communities in our study
that could have caused vulnerability as discussed
above.
As compared with other types of natural disaster, our
researchers found a high prevalence of PTSD and a moderate prevalence of depression in children. Other studies
reported PTSD in the range of 4.595% and a 776%
prevalence of depression in children exposed to earthquakes, super-cyclone and wildfire disasters. Separation
anxiety disorder and conversion disorder were also reported to be found in these children [20, 23, 24]. The different rates observed in our study as contrasted with other studies may be explained by differences in culture, severity of the trauma, nature of the disaster, method of
References
Post-Tsunami Psychiatric Disorders in
Children
8 Goenjian AK, Pynoos RS, Steinberg AM, Najarian LM, Asarnow JR, Karayan I, Ghurabi
M, Fairbanks LA: Psychiatric comorbidity in
children after the 1988 earthquake in Armenia. J Am Acad Child Adolesc Psychiatry
1995;34:11741184.
9 Roussos A, Goenjian AK, Steinberg AM,
Sotiropoulou C, Kakaki M, Kabakos C,
Karagianni S, Manouras V: Posttraumatic
stress and depressive reactions among children and adolescents after the 1999 earthquake in Ano Liosia, Greece. Am J Psychiatry 2005;162:530537.
10 McDermott BM, Lee EM, Judd M, Gibbon P:
Posttraumatic stress disorder and general
psychopathology in children and adolescents following a wildfire disaster. Can J Psychiatry 2005;50:137143.
11 Kolaitis G, Kotsopoulos J, Tsiantis J, Haritaki S, Rigizou F, Zacharaki L, Riga E, Augoustatou A, Bimbou A, Kanari N, Liakopoulou M, Katerelos P: Posttraumatic stress
reactions among children following the Athens earthquake of September 1999. Eur Child
Adolesc Psychiatry 2003; 12:273280.
12 Vijayakumar L, Kannan GK, Daniel SJ: Mental health status in children exposed to tsunami. Int Rev Psychiatry 2006;18:507513.
13 La Greca A, Silverman WK, Vernberg EM,
Prinstein MJ: Symptoms of posttraumatic
stress in children after Hurricane Andrew: a
prospective study. J Consult Clin Psychol
1996;64:712723.
14 Neuner F, Schauer E, Catani C, Ruf M, Elbert
T: Post-tsunami stress: a study of posttraumatic stress disorder in children living in
three severely affected regions in Sri Lanka.
J Trauma Stress 2006;19:339347.
15 Thienkrua W, Cardozo BL, Chakkaraband
ML, Guadamuz TE, Pengjuntr W, Tantipiwatanaskul P, Sakornsatian S, Ekassawin S,
Panyayong B, Varangrat A, Tappero JW,
Schreiber M, van Griensven F: Symptoms of
post traumatic stress disorder and depression among children in tsunami-affected areas in southern Thailand. JAMA 2006; 296:
576578.
16 van der Kolk BA: The body keeps the score:
memory and the evolving psychobiology of
posttraumatic stress. Harv Rev Psychiatry
1994;1:253265.
17 van der Kolk BA: The neurobiology of childhood trauma and abuse. Child Adolesc Psychiatr Clin N Am 2003;12:293317.
18 van der Kolk BA, Saporta J: The biological
mechanisms and treatment of intrusion and
numbing. Anxiety Res 1991;4:199212.
19 Shaw JA, Applegate B, Schorr C: Twentyone-month follow-up study of school-age
children exposed to Hurricane Andrew. J
Am Acad Child Adolesc Psychiatry 1996;35:
359364.
20 Karakaya I, Agaoglu B, Coskun A, Sismanlar
SG, Yildiz Oc O: The symptoms of PTSD, depression and anxiety in adolescent students
three and a half years after the Marmara
earthquake. Turk Psikiyatri Derg 2004; 15:
257263.
21 Green BL, Grace MC, Vary MG, Kramer TL,
Gleser GC, Leonard AC: Children of disaster
in the second decade: a 17-year follow-up of
Buffalo Creek survivors. J Am Acad Child
Adolesc Psychiatry 1994;33:7179.
22 Cook A, Spinazzola J, Ford J, Lanktree C,
Blaustein M, Cloitre M, DeRosa R, Hubbard
R, Kagan R, Mallah K, Olafson E, van der
Kolk BA: Complex trauma in children and
adolescents. Psychiatr Ann 2005;35:390
398.
23 Grigorian HM: The Armenian earthquake;
in Linda SA (ed): Responding to Disaster.
Washington, American Psychiatric Press,
1992, pp 157167.
24 Kar N, Mohapatra PK, Nayak KC, Pattanaik
P, Swain SP, Kar HC: Post-traumatic stress
disorder in children and adolescents one
year after a super-cyclone in Orissa, India:
exploring cross-cultural validity and vulnerability factors. BMC Psychiatry 2007;7:8.
Med Princ Pract 2008;17:290295
295
Downloaded by:
139.195.64.201 - 7/2/2014 4:26:17 PM
1 Wikipedia contributors: 2004 Indian Ocean
earthquake [homepage on the Internet].
Wikipedia, The Free Encyclopedia [updated
2006 May 22; cited 2006 May 23]. Available from: http://en.wikipedia.org/w/index.
php?title=2004_Indian_Ocean_earthquake
&oldid=54573150.
2 Tsunami Memorial Project [homepage on
the Internet]. Ministry of Natural Resources
and Environment Thailand: Information on
the disaster [updated 2006 May 17; cited
2006 May 23]; Available from: http://www.
tsunamimemorial.or.th/information.htm
3 Department of Disaster Prevention and Mitigation, Ministry of the interior of Thailand:
2006 Disaster report [homepage on the Internet]. Ministry of the interior of Thailand
[updated 18 May 2006; cited 2006 May 22].
Available from: www.disaster.go.th/disaster01/page/report_2547_2548/p210228.
4 Department of Disaster Prevention and Mitigation, Ministry of the interior of Thailand:
Earthquake/Tsunami Victims Relief Effort
[homepage on the Internet]. Ministry of the
interior of Thailand [updated 18 May
2006;cited 2006 May 22]. Available from:
http://www.disaster.go.th/html/english/
general/ddpm_tsunami.pdf
5 The Mental Health Center (MHC) for Thai
Tsunami Disaster: Symptoms Report of
Mental Health Services for Tsunami Victims
[homepage on the Internet]. Department of
Mental Health, Ministry of Public Health of
Thailand. c2005 [cited 2005 Feb 2]. Available
from: http://www.mis12.moe.go.th/tsunami/index.asp
6 John PB, Russell S, Russell PS: The prevalence of posttraumatic stress disorder among
children and adolescents affected by tsunami disaster in Tamil Nadu. Disaster Manag
Response 2007;5:37.
7 Pynoos RS, Goenjian A, Tashjian M, Karakashian M, Manjikian R, Manoukian G,
Steinberg AM, Fairbanks LA: Post-traumatic stress reactions in children after the 1988
Armenian earthquake. Br J Psychiatry 1993;
163:239247.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Jadwal Jaga IGD 1Document25 pagesJadwal Jaga IGD 1retPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Itinerary BALIDocument7 pagesItinerary BALIretPas encore d'évaluation
- Daftar Kelulusan Osce November 2018 PDFDocument73 pagesDaftar Kelulusan Osce November 2018 PDFAisyah Althafunnisa Bayu PutriPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- EaasmcDocument27 pagesEaasmcretPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Ante Natal CareDocument82 pagesAnte Natal CareretPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Group Moderators' Manual BookDocument37 pagesGroup Moderators' Manual BookretPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- New Text DocumentDocument1 pageNew Text DocumentretPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Soy Milk Consumption and Blood Pressure Among Type 2 Diabetic Patients With NephropathyDocument7 pagesSoy Milk Consumption and Blood Pressure Among Type 2 Diabetic Patients With NephropathyretPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- A B C D E: Senin Selasa Rabu Kamis Jumat SabtuDocument11 pagesA B C D E: Senin Selasa Rabu Kamis Jumat SabturetPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- New Text DocumentDocument1 pageNew Text DocumentretPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grafik GDS Ny. I: Tanggal PemeriksaanDocument7 pagesGrafik GDS Ny. I: Tanggal PemeriksaanretPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- 4-Planning Tools & TechniquesDocument17 pages4-Planning Tools & TechniquesretPas encore d'évaluation
- Bali Corat CoretDocument1 pageBali Corat CoretretPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Meeting 3Document28 pagesMeeting 3retPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Countries' Etiquette ARGENTINADocument3 pagesCountries' Etiquette ARGENTINAretPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Optimiz Ing The Membe R'S: Pation in SDC (Art Div Ision)Document7 pagesOptimiz Ing The Membe R'S: Pation in SDC (Art Div Ision)retPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Etipro Kelompok 4 (Kelas G)Document12 pagesEtipro Kelompok 4 (Kelas G)retPas encore d'évaluation
- Cleaning AgentSuppliesDocument5 pagesCleaning AgentSuppliesretPas encore d'évaluation
- Equipment HKDocument43 pagesEquipment HKretPas encore d'évaluation
- Organization ChartDocument29 pagesOrganization Chartret100% (1)
- Countries' Etiquette AFGHANISTANDocument4 pagesCountries' Etiquette AFGHANISTANretPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- 1-Introduction To Management & OrganizationDocument22 pages1-Introduction To Management & OrganizationretPas encore d'évaluation
- 3 Strategic ManagementDocument13 pages3 Strategic ManagementretPas encore d'évaluation
- FlooringDocument20 pagesFlooringretPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Tata Boga (India)Document5 pagesTata Boga (India)retPas encore d'évaluation
- 5-Organization Structure & DesignDocument19 pages5-Organization Structure & DesignretPas encore d'évaluation
- 9-Foundations of ControlDocument13 pages9-Foundations of ControlretPas encore d'évaluation
- 447Document10 pages447retPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- 5-Organization Structure & DesignDocument19 pages5-Organization Structure & DesignretPas encore d'évaluation
- Meeting 3Document33 pagesMeeting 3retPas encore d'évaluation
- Trail Mix Cookies IKDocument24 pagesTrail Mix Cookies IKDwi Intan WPas encore d'évaluation
- Mental Health Issues - ADHD Among ChildrenDocument9 pagesMental Health Issues - ADHD Among ChildrenFelixPas encore d'évaluation
- Notice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsDocument2 pagesNotice: Agency Information Collection Activities Proposals, Submissions, and ApprovalsJustia.comPas encore d'évaluation
- N4H InvitationLetter - FinalDocument2 pagesN4H InvitationLetter - Finalluis DiazPas encore d'évaluation
- 2018 MUSE Inspire Conference - Show and Tell SessionsDocument13 pages2018 MUSE Inspire Conference - Show and Tell SessionsMichele LambertPas encore d'évaluation
- Drug Study 1Document2 pagesDrug Study 1Hafza MacabatoPas encore d'évaluation
- Disaster Preparedness IntroDocument10 pagesDisaster Preparedness IntroBernadette-Mkandawire MandolomaPas encore d'évaluation
- Typology of Nursing Problems in Family Nursing PracticeDocument4 pagesTypology of Nursing Problems in Family Nursing PracticeLeah Abdul KabibPas encore d'évaluation
- NCLEX RN Practice Questions Set 1Document6 pagesNCLEX RN Practice Questions Set 1Jack SheperdPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Assoc Between Poor Sleep Quality - Depression Symptoms Among ElderlyDocument8 pagesAssoc Between Poor Sleep Quality - Depression Symptoms Among ElderlyWindyanissa RecitaPas encore d'évaluation
- Lab Report 15438869 20231127064225Document1 pageLab Report 15438869 20231127064225carilloabhe21Pas encore d'évaluation
- Tea and Industrial RevolutionDocument4 pagesTea and Industrial RevolutionPhuong NguyenPas encore d'évaluation
- Nursing - Burn InjuryDocument39 pagesNursing - Burn Injuryamaracha2003Pas encore d'évaluation
- Mini Clinical Examination (Mini-CEX)Document21 pagesMini Clinical Examination (Mini-CEX)Jeffrey Dyer100% (1)
- PNA 2012 National Convention LectureDocument60 pagesPNA 2012 National Convention LectureHarby Ongbay AbellanosaPas encore d'évaluation
- Peran Perawat KomDocument27 pagesPeran Perawat Komwahyu febriantoPas encore d'évaluation
- Health Declaration FormDocument1 pageHealth Declaration FormUzair KhalidPas encore d'évaluation
- Adani Targets Debt Cuts, Income Boost Coastal Shipping To Get Infra Status, Says SonowalDocument20 pagesAdani Targets Debt Cuts, Income Boost Coastal Shipping To Get Infra Status, Says SonowalboxorPas encore d'évaluation
- Disaster Nursing SAS Session 14Document6 pagesDisaster Nursing SAS Session 14Niceniadas CaraballePas encore d'évaluation
- Letters of Intent (Cover Letters)Document6 pagesLetters of Intent (Cover Letters)anca_ramona_s0% (1)
- Care ReportDocument23 pagesCare ReportSindi Muthiah UtamiPas encore d'évaluation
- Pattern Before Hospitalization During HospitalizationDocument2 pagesPattern Before Hospitalization During HospitalizationJean WinPas encore d'évaluation
- Gear Oil 85W-140: Safety Data SheetDocument7 pagesGear Oil 85W-140: Safety Data SheetsaadPas encore d'évaluation
- Fatal Airway Obstruction Due To Ludwig'sDocument6 pagesFatal Airway Obstruction Due To Ludwig'sRegina MugopalPas encore d'évaluation
- Physiological Changes Postpartum PeriodDocument2 pagesPhysiological Changes Postpartum PeriodEurielle MiolePas encore d'évaluation
- Nejmra 2023911Document8 pagesNejmra 2023911Merry LeePas encore d'évaluation
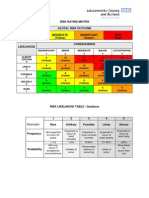
- Example of A NHS Risk Rating MatrixDocument2 pagesExample of A NHS Risk Rating MatrixRochady SetiantoPas encore d'évaluation
- Test Bank For Occupational Therapy in Mental Health A Vision For Participation 2nd Edition Catana Brown Virginia C Stoffel Jaime MunozDocument3 pagesTest Bank For Occupational Therapy in Mental Health A Vision For Participation 2nd Edition Catana Brown Virginia C Stoffel Jaime MunozDavid Ortiz97% (36)
- ResumeDocument4 pagesResumeAaRomalyn F. ValeraPas encore d'évaluation
- The Influence of Music in Horror Games (Final Draft)Document7 pagesThe Influence of Music in Horror Games (Final Draft)Panther LenoXPas encore d'évaluation