Académique Documents
Professionnel Documents
Culture Documents
3
Transféré par
SDCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
3
Transféré par
SDDroits d'auteur :
Formats disponibles
Behavioural Brain Research 225 (2011) 498504
Contents lists available at ScienceDirect
Behavioural Brain Research
journal homepage: www.elsevier.com/locate/bbr
Research report
Electrical stimulation over the left inferior frontal gyrus (IFG) determines
long-term effects in the recovery of speech apraxia in three chronic aphasics
P. Marangolo a,c, , C.V. Marinelli b,c , S. Bonifazi a , V. Fiori a,c , M.G. Ceravolo a , L. Provinciali a ,
F. Tomaiuolo d,1
a
Department of Neuroscience, Faculty of Medicine, University of Ancona, Ancona, Italy
Faculty of Psychology, University of Rome, Rome, Italy
c
IRCCS Fondazione Santa Lucia, Rome, Italy
d
Unit Cerebrolesioni Acquisite Auxilium Vitae Volterra, Pisa, Italy
b
a r t i c l e
i n f o
Article history:
Received 3 May 2011
Received in revised form 31 July 2011
Accepted 5 August 2011
Available online 12 August 2011
Keywords:
tDCS
Apraxia of speech
Verbal apraxia
Brain stimulation
Language rehabilitation
Aphasia
a b s t r a c t
A number of studies have shown that modulating cortical activity by means of transcranial direct current
stimulation (tDCS) affects the performance of both healthy and brain-damaged subjects. In this study, we
investigated the potential of tDCS for the recovery of apraxia of speech in 3 patients with stroke-induced
aphasia. Over 2 weeks, three aphasic subjects participated in a randomized double-blinded experiment
involving intensive language training for their articulatory difculties in two tDCS conditions. Each subject
participated in ve consecutive daily sessions of anodic tDCS (20 min, 1 mA) and sham stimulation over
the left inferior frontal gyrus (referred to as Brocas area) while they performed a repetition task. By the
end of each week, a signicant improvement was found in both conditions. However, all three subjects
showed greater response accuracy in the anodic than in the sham condition. Moreover, results for transfer
of treatment effects, although different across subjects, indicate a generalization of the recovery at the
language test. Subjects 2 and 3 showed a signicant improvement in oral production tasks, such as
word repetition and reading, while Subjects 1 and 2 had an unexpected signicant recovery in written
naming and word writing under dictation tasks. At three follow-ups (1 week, 1 and 2 months after the
end of treatment), response accuracy was still signicantly better in the anodic than in sham condition,
suggesting a long-term effect on the recovery of their articulatory gestures.
2011 Elsevier B.V. All rights reserved.
1. Introduction
Apraxia of speech (AOS), also known as verbal apraxia, is an
acquired motor speech disorder characterized by an impaired ability to coordinate the sequential, articulatory movements necessary
to produce speech sounds [1,2].
Though there may be some disagreement as to its precise location, there is a general consensus that the disorder results from
brain injury in the language-dominant (usually left) hemisphere
due to a damage either to the inferior frontal gyrus [3], in the left
anterior insula [4] and/or in the subcortical structures, particularly
in the basal ganglia [5,6].
The severity of AOS varies from person to person. The disorder
can be so mild to give the patient troubles with very few speech
sounds or only occasional problems pronouncing words with
Corresponding author at: Department of Neuroscience, Faculty of Medicine,
Ancona, Italy. Tel.: +39 0712206093/3477548995;
fax: +39 071887262/0712206214.
E-mail addresses: p.marangolo@univpm.it
(P. Marangolo), f.tomaiuolo@riabilitazione-volterra.it (F. Tomaiuolo).
1
Dr. F.Tomaiuolo should be referred for neuroanatomical analysis.
0166-4328/$ see front matter 2011 Elsevier B.V. All rights reserved.
doi:10.1016/j.bbr.2011.08.008
many syllables. In the most severe cases, a patient may not be able
to communicate effectively with speech, and may need the help of
alternative or additional communication methods. One of the most
notable symptoms is the tendency of the patient to make groping
oral movements to locate the correct articulatory position, and the
presence of increasing articulatory errors with increasing word
and phrase length [7, for a review]. Another common characteristic
is the incorrect use of prosody, that is, the varying rhythms,
stresses, and inections of speech that are used to express ones
emotional state.
Although AOS is not due to weakness or paralysis of the speech
muscles (the muscles of the face, tongue and lips), it may occur
together with muscle impairments or concomitant acquired language difculties, such as Brocas aphasia.
There is no single factor or test that can be used to diagnose
verbal apraxia. The person making the diagnosis generally looks for
the presence of some of the symptoms described above in verbal
production tasks such as naming, repetition and reading stimuli of
increasing length and articulatory complexity [2].
Numerous treatment approaches have been developed to remediate the apraxia motor speech disorder. However, no single
approach has been proven to be the most effective [e.g. 710].
P. Marangolo et al. / Behavioural Brain Research 225 (2011) 498504
Typically, the therapy is concentrated on the disordered articulation. It emphasizes the relearning of adequate points of articulation
and the sequencing of articulatory gestures in order to provide conditions such that the patient can advance from limited,
automatic-reactive speech to appropriate, volitional-purposive
communication. Apraxic patients, in general, may achieve greater
phonemic accuracy if they are allowed to monitor their own speech
in a mirror and if they can watch the articulatory movements of the
clinician as he/she speaks [11]. In some cases, people with apraxia
of speech recover some or all of their speech abilities. However,
in the most severe conditions, persistent difculties in articulating
speech sounds may be observed also after an intensive language
treatment period [12].
In recent years, new approaches for the treatment of motor
and language impairments, such as non-invasive neurostimulation
techniques, have emerged. Transcranial direct current stimulation
(tDCS) makes use of a weak polarizing direct current delivered
to the cortex via two electrodes placed on the scalp. The nature
of the effect depends on the polarity of the current. Generally,
the anode increases cortical excitability when applied over the
region of interest with the cathode above the contralateral orbit
or above the shoulder (as the reference electrode), whereas the
cathode decreases it, limiting the resting membrane potential. In
particular, during anodic stimulation in healthy subjects enhanced
visuomotor performance [13], motor learning [14], verbal uency
[15] and working memory [16] have been observed. Recent studies of chronic neurological subjects have further demonstrated
how increased cortical excitability inuences the recovery of motor
[17,18], neurological and psychiatric symptoms [1921].
With regard to the language domain, few studies have already
shown that tDCS may be effective in enhancing verbal learning in
normal subjects [22,23] and in the recovery of oral word production
in aphasic patients [2427].
However, there have been no reports to date that have explored
its inuence for the improvement of articulatory disturbances
in the aphasic population. Recent studies suggest that long-term
effects might be more easily obtained with repeated tDCS applications. It has been proposed that the greatest improvement is
obtained when the damaged areas are stimulated during simultaneous specic language training [2527].
The main purpose of the present study was to investigate in
three chronic nonuent aphasic patients whether the application
of anodic tDCS over the left inferior frontal gyrus (referred to as
Brocas area) during concomitant language training would lead to
an improvement of their articulatory disturbances. The choice to
stimulate this area was based on the results of previous research
which demonstrates the importance of this region for articulating
speech sounds [3].
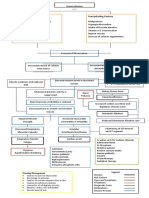
Since all patients had damage to cerebral structures functionally connected to Brocas area (see Fig. 1), we wondered whether
stimulation of this region would ameliorate their articulatory difculties.
In order to measure the potential, long-term benecial effects
in the aphasic subjects, three follow-up sessions were carried out
1 week, 1 month and 2 months after the end of each treatment
condition.
2. Experiment
2.1. Materials and methods
2.1.1. Subjects
Three subjects (2 males and 1 female) who had suffered a single
left hemispheric stroke were included in the study. Inclusion criteria during this study were subjects with native Italian prociency,
499
pre-morbid right-handedness, a single left hemispheric stroke at
least 6 months prior to investigation and no acute or chronic neurological symptoms requiring medication. The data analyzed in the
current study were collected in accordance with the Helsinki Declaration and the Institutional Review Board of the Ospedale Riuniti
Torrette in Ancona, Italy. Prior to participation, all patients signed
informed consent forms.
2.1.2. Clinical data
Subjects 1 and 3 suffered from an ischemic lesion involving the
left hemisphere (see Fig. 1). In Subject 2, MRI revealed a hemorrhagic lesion involving the same hemisphere. As shown in Fig. 1,
none of the patients had damage to the inferior frontal gyrus where
the tDCS anode was positioned.
Formal testing was conducted within 1 week prior to stimulation. Aphasic disorders were assessed using standardized language
tests (i.e. Esame del Linguaggio II [28]; Token test [29]).
The three subjects were classied as nonuent aphasics because
of their severely compromised oral production due to AOS. Two
subjects (1 and 2) were not able to produce any sounds in
spontaneous speech with severe articulatory groping in naming,
repetition and reading tasks. Subject 3 exhibited marked difculties
in initiating speech and presented with distortions of phonemes
and articulatory groping with bisyllabic words for naming, repetition and reading tasks. Written naming and writing under dictation
tasks were markedly compromised in Subjects 2 and 3, while Subject 1 showed a partial recovery in the word writing task (see
Table 1).
For all cases, auditory comprehension abilities were functionally
adequate in the Esame del Linguaggio II and in the Token test in
which two patients obtained scores of medium severity (Subjects
2 and 3) and one patient (Subject 1) showed complete recovery
(the cut-off score which discriminates between pathological and
normal performance is 29/36) (see Table 1).
To evaluate nonverbal oral motor skills, the Oral Apraxia test
[30] was administered. None of the patients showed apraxic disturbances.
2.2. Materials
A list of 60 syllables (e.g. PA, MO, CA, FU) and a list of 50 CVCV
(CV consonantvowel, e.g. luna [moon], pipa [pipe], dito [nger],
vino [wine]) and 40 CVCCV (e.g. palla [ball], nonno [grandfather],
panna [cream], letto [bed]) very simple bisyllabic words were used
[Fanzago test, 31].
According to the International Phonetic Alphabet (IPA, [32]), syllables included different places (e.g. plosive, nasal, fricative) and
manners of articulation (e.g. bilabial, dental, velar).
2.3. Procedure
One week before the language training, different stimulus sets
were developed for each participant, based on their prole of
decits and stimulability for speech behaviours. First, all the 150
stimuli (syllables and words) were auditorily presented, one at a
time, through an audiotape for 3 consecutive days. The participants
had to repeat each stimulus within 15 s. We identied the stimuli
the patients could not correctly produce or always omitted.
Since Subject 1 had severe difculties in producing syllables and
words, a list of 56 CV syllables (i.e. /pa/, /me/) and a list of 14 CVCV
and 10 CVCCV bisyllabic words were considered. For Subjects 2 and
3, stimuli included a list of 44 CVCV (CV consonantvowel) and 36
CVCCV bisyllabic words.
For each subject, the selected stimuli were subdivided into two
groups of 40 stimuli each with bisyllabic words matched for frequency and length. Two stimulation conditions were carried out,
500
P. Marangolo et al. / Behavioural Brain Research 225 (2011) 498504
Fig. 1. Analysis of the patients brain lesions. Numbers refer to Broadmanns areas. The yellow arrows indicate the vertical ramus of the Sylvian ssure. The orange arrows
indicate the Heschel gyrus. CC: corpus callosum; Th: thalamus; Pu: putamen; and nc: caudate nucleus. Volume of the individual brain lesion was obtained after transforming
of each brain image into a standardized proportional stereotaxic space of [44] to correct for any inter-individual differences in gross brain size by means of an automatic
registration program which uses a 3-D cross-correlation approach to match the single CT volume with the intensity average of 305 MRI brain volumes previously aligned
into the standardized stereotaxic space [45,46].
From left to right: Subject 1: Lesion is mainly localized in the white matter pathways supplied by the left middle cerebral artery including the superior longitudinal fasciculus,
the arcuate fasciculus, part of the internal external and extreme capsule and part of the inferior third of the central gyrus. The claustrum, the putamen, part of the supramarginal
and the angular gyri are also damaged. The inferior frontal gyrus does not show any damage. The overall brain lesion is about 310 cmq. Subject 2: Lesion mainly involves
the frontal and the parietal cortex. Posteriorly, the lesion includes the intraparietal sulcus sparing the upper part of the superior parietal lobe, the posterior segment of the
superior temporal gyrus up to the level of the sulcus acusticus. Anteriorly, most of the superior frontal gyrus, the precentral gyrus up to the level of the middle frontal gyrus
and the frontal pole are damaged. The insula cortex, the claustrum and the capsula extrema are also compromised. Although partially atrophized, the inferior frontal gyrus
does not show any damage. The overall brain lesion is about 26 cmq. Subject 3: Lesion mainly involves the brain regions supplied by the left middle and caudal part of the
anterior cerebral arteries: from the internal part of the operculum, the lesion includes the mesial superior temporal gyrus and the insular cortex. The Rolandic and the parietal
operculi, the supramarginal and angular gyri, the post-central gyrus and the posterior parietal cortex are also compromised. In addition, the white matter lesion affects the
superior longitudinal fasciculus, the arcuate fasciculus, part of the internal external and extreme capsule and the lateral part of the body of the corpus callosum. A lesion is
also present in the middle portion of the cingulate gyrus (gyrus limbicus) and the caudal/middle portion of the superior frontal gyrus, and in the precentral gyrus up to the
level of the middle frontal gyrus. The inferior frontal gyrus does not show any damage. The overall brain lesion is about 172 cmq. (For interpretation of the references to color
in this gure legend, the reader is referred to the web version of the article.)
P. Marangolo et al. / Behavioural Brain Research 225 (2011) 498504
501
Table 1
Sociodemographic and clinical data of the three aphasic subjects.
Participants
Sex
Age
Educational
level
Type of
aphasia
Time
post-onset
Oral naming
noun
Written
Naming noun
Word
repetition
Word
reading
Word writing
under dictation
Token
test
Subject 1
Subject 2
Subject 3
F
M
M
68
63
67
13
13
17
Nonuent
Nonuent
Nonuent
1 years
4 year
7 months
0/20
1/20
7/20
13/20
0/20
0/20
0/20
0/20
7/20
0/20
0/20
5/20
3/20
0/20
0/20
30/36
18/36
11/36
Fig. 2. Overview of study design. All patients underwent daily language treatment for 5 consecutive days. During the language training, tDCS was delivered over the left
inferior frontal gyrus (IFG, BA 44/45). Two stimulation conditions were performed: anodic and sham stimulations, each stimulation was carried out a different weak period
with a 6-day inter-session interval. At the beginning of each week (to measure baseline performance) and after 1 week, 1 month and 2 months from the end of the training
(rst, second and third follow-up) for each stimulation condition subjects were shown the list of stimuli and asked to repeat them without help.
one group of stimuli was used for the anodic and the other one for
the sham stimulation.
All patients underwent daily language treatment for the two
groups of stimuli for 5 consecutive days. Each stimulation condition
was carried out a different weak period with a 6-day inter-session
interval. In order to measure baseline performance at the beginning of each week for each stimulation condition, the three subjects
were shown the corresponding list of stimuli and asked to repeat
them without help. The same was done in the follow-up sessions at
1 week, 1 month and 2 months after the training (see Fig. 2). Each
participants responses to all stimuli were transcribed and recorded
on audiotape for reliability purposes. Responses were scored as correct if all sounds in the syllable or in the word were perceived as
accurate by the examiner.
2.3.1. Treatment
The therapy method was similar for all patients. The clinician
and the patient were seated face to face so that the patient could
watch the articulatory movements of the clinician as she spoke. The
treatment involved the use of 5 different steps (see below) which
would progressively induce the patient to correctly reproduce the
whole stimulus. If the patient was not able to articulate the stimulus
in the rst step, the clinician would move on to the next step and so
on up to the last step. Anytime, the patient was able to reproduce
the articulatory gestures facilitated by the clinician, he/she would
be asked to repeat the whole stimulus without the clinicians help
and only if he/she succeeded in doing so again, the response was
considered as correct. If the patient was not able to articulate the
stimulus in the last step, the response was considered as an error.
Step 1: The clinician auditorily presented the whole stimulus and
asked the patient to repeat it. If the patient correctly repeated the
stimulus, the clinician would present another stimulus, if he/she
made errors the clinician would move on the next step.
Step 2: The clinician auditorily presented the stimulus with a pause
between each syllable, prolonged the vowel sound, exaggerated
the articulatory gestures and asked the patient to do the same.
Step 3: As in step 2, the clinician auditorily presented the stimulus
again with a pause between each syllable, prolonged the vowel
sound, exaggerated the articulatory gestures and asked the patient
to do the same.
Step 4: The clinician auditorily presented one syllable at a time,
prolonged the vowel sound, exaggerated the articulatory gestures
and asked the patient to do the same.
Step 5: As in step 4, the clinician auditorily presented one syllable at a time again, prolonged the vowel sound, exaggerated the
articulatory gestures and asked the patient to do the same.
2.3.2. Transcranial direct current stimulation (tDCS)
tDCS was applied using a battery-driven, Eldith (neuroConn
GmbH) Programmable Direct Current Stimulator with a pair of
surface-soaked sponge electrodes (5 cm 7 cm). Two different
electrode montages were used: the stimulating electrode (to which
the term anodic stimulation refers) was centered over the left inferior frontal gyrus (IFG, BA 44/45, position dened according to
the extended International 10-20 System; using the Munster T2Tconverter to determine the position on the EEG system). The second
electrode was positioned over the contralateral supraorbital region
[33].
During the training task, anodic tDCS (current of 1 mA) was
delivered for 20 min. If applied according to safety guidelines, tDCs
is considered to be a safe brain stimulation technique with minor
adverse effects [14]. Sham stimulation was performed exactly like
anodic stimulation on the left IFG, but the stimulator was turned off
after 30 s. It has been shown that this procedure makes it possible to
blind subjects as to the respective stimulation condition [34]. Furthermore, to ensure the double-blind procedure, the examiner was
not told which stimulation was being applied, and the stimulator
was turned on by another person. The order of item presentation
was randomized across trials.
Fig. 3. Mean percentage of correct responses for aphasic subjects at the pre- and
post-treatment evaluation for the anodic and sham conditions, respectively.
502
P. Marangolo et al. / Behavioural Brain Research 225 (2011) 498504
Table 2
Number of correct responses on the pre-anodic, post-anodic, pre-sham and post-sham administration of the language test (Esame del Linguaggio II, Ciurli et al. [28]). Subjects
1 and 3 were administered before the anodic and after the sham condition, while Subject 2 was administered before the sham and after the anodic condition.
Participants
Oral naming noun
Written naming noun
Word repetition
Word reading
Word writing under
dictation
I (pre)
II (post)
I (pre)
II (post)
I (pre)
II (post)
I (pre)
II (post)
I (pre)
II (post)
0/20
0/20
13/20
16/20
0/20
2/20
0/20
0/20
3/20
0/20
0/20
15/20
15/20
1/20
1/20
0/20
0/20
20/20
20/20*
p < .0001
20/20
1/20
1/20
1/20
2/20
0/20
0/20
0/20
7/20*
p < .008
0/20
0/20
0/20
5/20*
p < .047
0/20
0/20
0/20
7/20*
p < .008
0/20
0/20
0/20
8/20*
p < .003
Subject 3
Pre/post-anodic
7/20
10/20
0/20
0/20
7/20
5/20
0/20
9/20
9/20
0/20
0/20
20/20
17/20*
p < .0003
17/20
0/20
Pre/post-sham
20/20*
p < .0001
20/20
0/20
0/20
Subject 1
Pre/post-anodic
Pre/post-sham
Subject 2
Pre/post-sham
Pre/post-anodic
16/20
chi square test.
2.3.3. Data analysis
Accuracy data of the whole group of patients were analyzed with
Mixed Effect Model [35,36], which allows controlling for item and
subject variability. Two xed factors were included, that is, Training
(two levels, pre- vs. post-training) and Condition (two levels, anodic
vs. sham); participant and item were inserted in the analysis as random factors. Interaction was explored using Bonferronis post-hoc
test.
2.3.4. Results
The analysis showed a signicant effect of Training (two levels, pre- vs. post-treatment, F(1,238) = 55.47, p < .0001) indicating
higher accuracy in the post-training compared to the pre-training
evaluation (mean percentage in response accuracy was 26.3%
vs.7.1%, respectively) and Condition (two levels, anodic vs. sham,
F(1,236) = 4.74, p < .05). The mean number of correct responses was
signicantly greater in the anodic than in the sham condition (mean
percentage in response accuracy was 20.8% vs.12.5%, respectively).
The participant random effect was not signicant (Wald Z < 1),
while the item factor showed a signicant effect (Wald Z = 5.42,
p < .0001).
The analysis also showed a signicant Training Condition interaction (F(1,238) = 8.49, p < .001). As shown in Fig. 3, although the
effect of Training was signicant in both conditions (differences
in the mean percentage of response accuracy between pre- and
post-training = 26.7% vs. 11.7%, p < .0001, for the anodic and sham
condition, respectively), in the post-training test, response accuracy was greater for the anodic than for the sham condition (mean
percentage of response accuracy was 34.2% vs.18.3%, p < .01, respectively).
2.3.5. Follow-up
2.3.5.1. Data analysis. Data were analyzed using Mixed Effect
Model, which allows controlling for item and subject variability. Two within-subject factors were included: Time (four levels,
post-treatment vs. rst follow-up vs. second follow-up vs. third
follow-up) and Condition (two levels, anodic vs. sham); participant
and item were included in the analysis as random factors. Interaction was explored using the Bonferronis post-hoc test.
2.3.5.2. Results. The analysis showed a signicant Condition effect
(F(1,238) = 18.03, p < .0001) indicating greater response accuracy in
the anodic than in the sham condition (mean percentage was 34.8%
vs.13.5%, respectively). The effect of Time was not signicant (F
about 1). The participant random effect was not signicant (Wald
Z < 1), while there was a signicant effect of the item factor (Wald
Z = 10.36, p < .0001).
The analysis also showed a signicant Condition Time interaction (F(3,714) = 3.45, p < .01). As shown in Fig. 4, while in the anodic
condition there were no signicant differences in response accuracy between the post-treatment and each follow-up evaluation
(about 35% of response accuracy in all evaluations) indicating a
persistence of the achieved recovery, in the sham condition there
was a signicant decrease in response accuracy when comparing
each follow-up to the post-training evaluation (at least p < .0001).
In this last condition, no further decrease in response accuracy
was observed in each successive follow-up. Moreover, for each
follow-up evaluation, response accuracy was always greater in the
anodic than in the sham condition (mean differences anodic vs.
sham = 22.5%, 20.8% and 25.8% at least p < .01 on the rst, second
and third follow-up, respectively).
Since the number of patients (N = 3) did not allow us to counterbalance the order of conditions across subjects (Subjects 1 and 3
went through the anodic condition rst and then through the sham
condition, while Subject 2 went through the sham condition rst
and then through the anodic condition), we ran further analysis
by adding the order of condition (anodic vs. sham) as xed factor.
Neither in the pre-post-training comparison nor in the follow-up
analysis the order of condition was signicant (F(1,236) = 1.55, ns; and
F(1,944) = .08, ns; respectively).
3. Discussion
Fig. 4. Mean percentage of correct responses for aphasic subjects at the posttreatment evaluation and at the rst (1 week), second (1 month) and third (2
months) follow-ups for the anodic and sham conditions, respectively.
The aim of this study was to determine whether anodic tDCS
over left inferior frontal gyrus together with concomitant lan-
P. Marangolo et al. / Behavioural Brain Research 225 (2011) 498504
guage training would bring about any signicant improvement in
relearning the sequencing of articulatory gestures for the correct
production of syllables and words in three chronic nonuent aphasics with severe AOS. In all subjects, the analysis showed that anodic
stimulation had a benecial effect on the recovery of the aphasic
subjects articulatory disturbances. With regard to response accuracy, the patients performance signicantly improved in both the
anodic and the sham conditions. This was because all the three
subjects underwent intensive language training in both conditions.
However, the benecial effect of anodic stimulation was evident
because response accuracy was greater in this condition than in
the sham condition.
Moreover, the follow-up testing revealed retention of the
achieved improvement only for the anodic condition which did not
show any decrement in response accuracy suggesting long-term
recovery of the subjects articulatory disturbances.
Although to date the mechanisms underlying the benecial
effects of tDCS are largely unknown, some authors have hypothesized that anodic stimulation elicits a prolonged increment in
cortical plasticity, probably due to the depolarization of the neuronal membrane and the changes in the synaptic connections of
the N-methyl-d-aspartate (NMDA) receptors involved in long-term
potentiation [37,38]. It could be that in our subjects in which
tDCS was directly delivered over the left IFG, anodic stimulation
had in some way enhanced the capacity for spared left hemispheric regions to make compensatory plastic changes promoting
an improvement in the patients articulatory speech gestures.
In a recent review, Bolognini et al. suggested that non-invasive
brain stimulation might enhance the positive effect of motor training by inducing modications in cerebral plasticity. Given that
these strategies have some similar mechanisms of action, that
is, both induce similar changes in the neural excitability of the
lesioned area, they might be more benecial when used together.
In fact, brain stimulation can prime cortical excitability, optimizing
the learning processes involved in standard rehabilitation therapies which can lead to more pronounced and long-term functional
gains [17].
In line with Bologninis proposal, Fridriksson et al. [27] recently
showed in a group of eight uent chronic aphasics that anodic tDCS
administered for 5 consecutive days with concomitant language
treatment decreased processing time during a picture naming task.
Similar results were found by Baker et al. [25] in a group of ten
aphasics who received 5 days of anodic tDCS over the left frontal
cortex while performing a computerized anomia treatment.
Thus, the above mentioned studies conrm the importance of
associating stimulation with specic training.
Although we are unable to draw any denitive conclusions from
our results because of the small size of our patient group, data suggest that in aphasic patients anodic tDCS applied over the left IFG
together with simultaneous language training leads to signicantly
improved performance on an articulatory task which continued to
persist even 2 months after the end of treatment. Very recently,
Kim et al. [39] reported two cases of chronic stroke patients whose
neurological functions were improved by continuous, unipolar cortical stimulation combined with rehabilitation. Patient 1 presented
with motor and language decits, while patient 2 only had motor
disturbances. Follow-up evaluation after 4 months of stimulation
and concurrent rehabilitation showed improvement in neurological symptoms in both patients and in speech and articulation in
patient 1 whose electrode covered the IFG. Therefore, although
preliminary, in line with our results, these data suggest a plausible
relationship between stimulation over the left IFG and the recovery
of articulation.
Results for transfer of treatment effects, although different
across subjects, indicate a generalization of the recovery in the language test only after performing the anodic stimulation condition
503
(see Table 2). Subjects 2 and 3 showed signicant improvement in
oral production tasks, such as word repetition and reading, while
Subjects 1 and 2 had an unexpected signicant recovery in written
naming and word writing under dictation tasks.
It has recently been hypothesized that the premotor cortices
(such as area 6, Exners area) play some role in implementing the
motor and sensory activity patterns involved in writing materials.
Lubrano et al. [40] used direct stimulation in patients with brain
tumors and reported that stimulation of Exners area caused difculty in reading and writing [see also 41]. Anderson et al. [42]
reported the case of a patient who could not read or write letters
and words following a surgical lesion in area 6 at the foot of the
left second frontal circonvolution, immediately above Brocas area.
In our patients (Subjects 1 and 2), the hypothesis that could be
advanced is that the stimulation of Brocas area coactivated the surrounding premotor regions (including Exners area) which lead to
an improvement in their writing abilities. Although Subjects 2 and 3
had very similar lesions, the same improvement was not observed
in Subject 3. Probably, the fact that Subject 2 had a hemorrhagic
lesion might have encouraged better functional reorganization and
greater responsiveness to stimulation by the perilesional regions
[43].
Although the small number of subjects studied here precludes
any denite statements about the effects of tDCS stimulation on the
treatment of AOS, we believe that they might be useful for planning
new therapeutic interventions in aphasia rehabilitation and for the
development of future studies.
Competing interests
None declared.
References
[1] Darley FL. Aphasia. Philadelphia: W.B. Saunders; 1982.
[2] Wertz RT, Lapointe LL, Rosenbek JC. Apraxia of speech in adults: the disorders
and its management. Orlando: Grune and Stratton, Inc.; 1984.
[3] Hillis AE, Work M, Barker PB, Jacobs PB, Breese EL, Maurer K. Reexamining the brain regions crucial for orchestrating speech articulation. Brain
2004;127:147987.
[4] Dronkers N. A new brain region for coordinating speech articulation. Nature
1996;384:15961.
[5] Square PA, Martin RE, Bose A. Nature and treatment of neuromotor speech
disorders in aphasia. In: Chapey R, editor. Language intervention strategies in
aphasia and related neurogenic communication disorders. 4th ed. Philadelphia:
Lippincott Williams & Wilkins; 2001. p. 84782.
[6] Peach R, Tonkovich J. Phonemic characteristics of apraxia of speech resulting
from subcortical hemorrhage. J Commun Disord 2004;37:7790.
[7] McNeil MR, Robin DA, Schmidt RA. Apraxia of speech: denition, differentiation and treatment. In: McNeil MR, editor. Clinical management of
sensorimotor speech disorders. New York: Thieme Medical Publishers; 1997.
p. 31144.
[8] Knock TR, Ballard KJ, Robin DA, Smith RA. Inuence of order of stimulus presentation on speech motor learning: a principled approach to treatment for
apraxia of speech. Aphasiology 2000;14:65368.
[9] Wambaugh JL. A summary of treatments for apraxia of speech and review of
replicated approaches. In: Seminars in speech and language: apraxia of speech:
from concept to clinic, vol. 23. 2002. p. 293308.
[10] Wambaugh JL, Doyle PJ. Treatment for acquired apraxia of speech: a review of
efcacy reports. Clin Aphasiology 1995;22:23143.
[11] Rosenbek JC, Lemme ML, Ahern MB, Harris EH, Wertz RT. A treatment for
apraxia of speech in adults. J Speech Hear Disord 1973;38:46272.
[12] Basso A, Corno M, Marangolo P. Evolution of oral and written confrontation
naming errors in aphasia. A retrospective study on vascular patients. J Clin Exp
Neuropsychol 1996;18:7787.
[13] Antal A, Nitsche MA, Kincses TZ, Kruse W, Hoffmann KP, Paulus W. Facilitation of visuo-motor learning by transcranial direct current stimulation of
the motor and extrastriate visual areas in humans. Eur J Neurosci 2004;19:
288892.
[14] Nitsche MA, Schauenburg A, Lang N, Liebetanz D, Exner C, Paulus W, et al.
Facilitation of implicit motor learning by weak transcranial direct current
stimulation of the primary motor cortex in the human. J Cogn Neurosci
2003;15:61926.
[15] Iyer MB, Mattu U, Grafman J, Lomarev M, Sato S, Wassermann EM. Safety
and cognitive effects of frontal DC brain polarization in healthy individuals.
Neurology 2005;64:8725.
504
P. Marangolo et al. / Behavioural Brain Research 225 (2011) 498504
[16] Fregni F, Boggio PS, Nitsche MA, Bermpohl F, Antal A, Feredoes E, et al. Anodal
transcranial current stimulation of prefrontal cortex enhances working memory. Exp Brain Res 2008;166:2330.
[17] Bolognini N, Pascual-Leone A, Fregni F. Using non-invasive brain stimulation to
augment motor training-induced plasticity. J NeuroEng Rehabil 2009;6:123.
[18] Hummel F, Celnik P, Giraux P, Floel A, Wu WH, Gerloff C, et al. Effects of noninvasive cortical stimulation on skilled motor function in chronic stroke. Brain
2005;128:4909.
[19] Boggio PS, Rigonatti SP, Ribeiro RB, Myczkowski ML, Nitsche MA, Pascual-Leone
A, et al. A randomized double-blind clinical trial on the efcacy of cortical
direct current stimulation for the treatment of major depression. Int J Neuropsychopharmacol 2007;11:16.
[20] Ferrucci R, Mameli F, Guidi L, Mrakic-Sposta S, Vergari M, Marceglia S,
et al. Transcranial direct current stimulation improves recognition memory
in Alzheimer Disease. Neurology 2008;71:4938.
[21] Mrakic-Sposta S, Marceglia S, Mameli F, Dilena R, Tadini L, Priori A. Transcranial
direct current stimulation in two patients with Tourette Syndrome. Mov Disord
2008;15:225961.
[22] Floel A, Rosser N, Michka O, Knecht S, Breitenstein C. Non invasive brain stimulation improves language learning. J Cogn Neurosci 2008;8:141522.
[23] Sparing R, Dafotakis M, Meister IG, Thirugnanasambandam N, Fink GR.
Enhancing language performance with non-invasive brain stimulationa transcranial direct current stimulation study in healthy humans. Neuropsychologia
2008;46:2618.
[24] Monti A, Cogiamanian F, Marceglia S, Ferrucci F, Mameli F, Mrakic-Sposta S,
et al. Improved naming after transcranial direct current stimulation in aphasia.
J Neurol Neurosurg Psychiatry 2008;79:4513.
[25] Baker JM, Roden C, Fridriksson J. Using transcranial direct-current stimulation
to treat stroke patients with aphasia. Stroke 2010;41:122936.
[26] Fiori V, Coccia M, Marinelli CV, Vecchi V, Bonifazi S, Ceravolo MG, et al.
Transcranial direct current stimulation (tDCS) improves word retrieval in
healthy and nonuent aphasic subjects. J Cogn Neurosci 2011;23:230923,
doi:10.1162/jocn.2010.21579.
[27] Fridriksson J, Richardson JD, Baker JM, Rorden C. Transcranial direct current
stimulation improves naming reaction time in uent aphasia: a double-blind,
sham-controlled study. Stroke 2011;42:81921.
[28] Ciurli P, Marangolo P, Basso A. Esame del Linguaggio (II versione). Organizzazioni Speciali Firenze; 1996.
[29] De Renzi E, Faglioni P. Normative data and the screening power of a shortened
version of the token test. Cortex 1978;14:419.
[30] De Renzi E, Pieczuro A, Vignolo LA. Oral apraxia and aphasia. Cortex
1966;2:573.
[31] Fanzago F. Test di valutazione dellarticolazione. In Trattamento Logopedico
delle dislalie e delle insufcienze velo-faringee. Quaderni Acta Phoniatrica
Latina; 1983.
[32] Handbook of the international phonetic association: a guide to the use of the
International Phonetic Alphabet. Cambridge University Press; 1999.
[33] Nitsche MA, Doemkes S, Karakose T, Antal A, Liebetanz D, Lang N, et al. Shaping
the effects of transcranial direct current stimulation of the human motor cortex.
J Neurophysiol 2007;97:310917.
[34] Gandiga PC, Hummel FC, Cohen LG. Transcranial DC stimulation (tDCS): a tool
for double-blind sham-controlled clinical studies in brain stimulation. Clin
Neurophysiol 2006;117:84550.
[35] Baayen RH, Tweedie FJ, Schreuder R. The subjects as a simple random effect fallacy: subject variability and morphological family effects in the mental lexicon.
Brain Lang 2002;81:5565.
[36] Brysbaert M. The language-as-xed-effect fallacy: some simple SPSS solutions to a complex problem (version 2.0). Royal Holloway: University of
London; 2007.
[37] Nitsche MA, Paulus W. Sustained excitability elevations induced by transcranial DC motor cortex stimulation in humans. Neurology 2001;57:
1899901.
[38] Nitsche MA, Paulus W. Excitability changes induced in the human motor
cortex by weak transcranial direct current stimulation. J Physiol 2000;527:
6339.
[39] Kim HI, Shin YIL, Moon SK, Chung GH, Lee MC, Kim HG. Unipolar and continuous
cortical stimulation to enhance motor and language decit in patients with
chronic stroke: report of 2 cases. Surg Neurol 2008;69:7780.
[40] Lubrano V, Roux FE, Dmonet JF. Writing-specic sites in frontal areas: a cortical
stimulation study. J Neurosurg 2004;101:78798.
[41] Lesser RP, Lueders H, Dinner DS, Hahn J, Cohen L. The location of speech
and writing functions in the frontal language areas. Brain 1984;107:
27591.
[42] Anderson SW, Damasio AR, Damasio H. Troubled letters but not numbers
domain specic cognitive impairments following focal damage in frontal cortex. Brain 1990;113:74966.
[43] Paolucci S, Antonucci G, Grasso MG, Bragoni M, Coiro P, De Angelis D, et al. Functional outcome of ischemic and hemorrhagic stroke patients after inpatient
rehabilitation: a matched comparison. Stroke 2003;34:28615.
[44] Talairach J, Tournoux P. Co-Planar Stereotaxic Atlas of the Human Brain: 3dimensional Proportional System: An approach to Cerebral Imaging. Thieme
Publishers; 1988.
[45] Collins DL, Neelin P, Peters TM, Evans AC. Automatic 3D intersubject registration of MR volumetric data in standardized Talairach space. J Comput Assist
Tomogr 1994;18:192205.
[46] Tomaiuolo F, MacDonald JD, Caramanos Z, Posner G, Chiavaras M, Evans AC,
et al. Morphology, morphometry and probability mapping of the pars opercularis of the inferior frontal gyrus: an in vivo MRI analysis. Eur J Neurosci
1999;11:303346.
Vous aimerez peut-être aussi
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Immune System Lecture NotesDocument2 pagesImmune System Lecture NotesPrabin KumarPas encore d'évaluation
- Anatomy of The Central Nervous SystemDocument7 pagesAnatomy of The Central Nervous SystemKristine AlejandroPas encore d'évaluation
- Meridian Dentistry EmotionsDocument1 pageMeridian Dentistry EmotionsMaurizio Maurizio KartPas encore d'évaluation
- Overt Agitation Severity ScaleDocument8 pagesOvert Agitation Severity ScaleSD100% (1)
- Homeopathy Narayani FinderDocument50 pagesHomeopathy Narayani FinderNicky Chhajwani100% (1)
- Basavaraj-Colour Therapy PDFDocument144 pagesBasavaraj-Colour Therapy PDFTanuku Net86% (14)
- Phenol For SpasticityDocument3 pagesPhenol For SpasticitySDPas encore d'évaluation
- Breast Engrogement FinalDocument41 pagesBreast Engrogement FinalSharmistha DebnathPas encore d'évaluation
- A Case Study On Graves DiseaseDocument46 pagesA Case Study On Graves DiseaseRenie SerranoPas encore d'évaluation
- Hypercalcemia Concept MapDocument3 pagesHypercalcemia Concept MapAlvin Dagumbal100% (1)
- Methods in Comparative Effectiveness ResearchDocument575 pagesMethods in Comparative Effectiveness ResearchSDPas encore d'évaluation
- SCIM QI Project: Assessing Cognitive Function in The SCI PopulationDocument7 pagesSCIM QI Project: Assessing Cognitive Function in The SCI PopulationSDPas encore d'évaluation
- 10 Sexuality After SCI 0516Document6 pages10 Sexuality After SCI 0516SDPas encore d'évaluation
- Clinical Practice Guideline: Bladder Management After SCIDocument10 pagesClinical Practice Guideline: Bladder Management After SCISDPas encore d'évaluation
- Instructions For Employee Child Abuse Clearances 9-2018Document2 pagesInstructions For Employee Child Abuse Clearances 9-2018SDPas encore d'évaluation
- 11 Neurogenic Obesity in SCIDocument16 pages11 Neurogenic Obesity in SCISDPas encore d'évaluation
- 01 Acute Spinal Cord InjuryDocument17 pages01 Acute Spinal Cord InjurySDPas encore d'évaluation
- Pha ProfilesDocument5 178 pagesPha ProfilesSDPas encore d'évaluation
- Orders B1weDocument5 pagesOrders B1weSDPas encore d'évaluation
- Pha ProfilesDocument5 178 pagesPha ProfilesSDPas encore d'évaluation
- 2016 FacultySurveyDocument1 page2016 FacultySurveySDPas encore d'évaluation
- Dis RegisterDocument1 pageDis RegisterSDPas encore d'évaluation
- Inpatient CensusDocument5 pagesInpatient CensusSDPas encore d'évaluation
- Rancho Los Amigos Scale of ConsciousnessDocument1 pageRancho Los Amigos Scale of ConsciousnessCedricFernandezPas encore d'évaluation
- Adm RegisterDocument1 pageAdm RegisterSDPas encore d'évaluation
- Code B1weDocument41 pagesCode B1weSDPas encore d'évaluation
- Anticipated DischgDocument1 pageAnticipated DischgSDPas encore d'évaluation
- Inpatient CensusDocument5 pagesInpatient CensusSDPas encore d'évaluation
- Brain Injury Medicine MilestonesDocument19 pagesBrain Injury Medicine MilestonesSDPas encore d'évaluation
- Fneur 04 00018Document18 pagesFneur 04 00018SDPas encore d'évaluation
- Ni Hms 809839Document15 pagesNi Hms 809839SDPas encore d'évaluation
- Spinal Cord Injury Medicine MilestonesDocument21 pagesSpinal Cord Injury Medicine MilestonesSDPas encore d'évaluation
- Speech Facilitation by Left Inferior Frontal Cortex StimulationDocument5 pagesSpeech Facilitation by Left Inferior Frontal Cortex StimulationSDPas encore d'évaluation
- Multiscale Control and Sense of AgencyDocument14 pagesMultiscale Control and Sense of AgencySDPas encore d'évaluation
- Pain Medicine MilestonesDocument30 pagesPain Medicine MilestonesSDPas encore d'évaluation
- Great CEOs See The Importance of Being UnderstoodDocument5 pagesGreat CEOs See The Importance of Being UnderstoodSDPas encore d'évaluation
- Brain & Language: Dae Sang You, Dae-Yul Kim, Min Ho Chun, Seung Eun Jung, Sung Jong ParkDocument5 pagesBrain & Language: Dae Sang You, Dae-Yul Kim, Min Ho Chun, Seung Eun Jung, Sung Jong ParkSDPas encore d'évaluation
- The Rehabilitative Effects On Written Language of A Combined Language and Parietal dual-tDCS Treatment in A Stroke CaseDocument16 pagesThe Rehabilitative Effects On Written Language of A Combined Language and Parietal dual-tDCS Treatment in A Stroke CaseSDPas encore d'évaluation
- Gustatory SystemDocument32 pagesGustatory SystemGalih Wahyu SaputraPas encore d'évaluation
- Introducting The Antibody-42914Document1 pageIntroducting The Antibody-42914Liudmila RusuPas encore d'évaluation
- 9 SkinDocument2 pages9 SkinDr.inerdevPas encore d'évaluation
- Comparative Renal Function in Reptiles, Birds, and MammalsDocument10 pagesComparative Renal Function in Reptiles, Birds, and MammalsAnais FaveroPas encore d'évaluation
- Subject: Biology Student Name: Grade: 7 Date: Revision Worksheet Topic2 Lesson 5 Controlling ProcessesDocument4 pagesSubject: Biology Student Name: Grade: 7 Date: Revision Worksheet Topic2 Lesson 5 Controlling Processessaeeda shoaib100% (1)
- NEMA. 301: Morphology of Nematodes: "Digestive, Reproductive, Nervous and Excretory System"Document24 pagesNEMA. 301: Morphology of Nematodes: "Digestive, Reproductive, Nervous and Excretory System"Soni AggarwalPas encore d'évaluation
- Pylorus Preserving PancreaticoduodenectomyDocument22 pagesPylorus Preserving PancreaticoduodenectomypaingmyintPas encore d'évaluation
- هستو نظري 1Document15 pagesهستو نظري 1مصطفى حاتم العبيلةPas encore d'évaluation
- Chennai ThesisDocument22 pagesChennai ThesisShradhanjali PandaPas encore d'évaluation
- 5 BubbleheDocument1 page5 BubbleheErick SumicadPas encore d'évaluation
- Chapter 1 - The Nervous SystemDocument8 pagesChapter 1 - The Nervous SystemRadha RamineniPas encore d'évaluation
- Blood Supply of BrainDocument2 pagesBlood Supply of BrainvmagtotoPas encore d'évaluation
- Excretory System For StudentsDocument2 pagesExcretory System For StudentsmargemunozPas encore d'évaluation
- PosnerPetersen - 1990 - The Attention System of The Human Brain PDFDocument18 pagesPosnerPetersen - 1990 - The Attention System of The Human Brain PDFLizel Clases ParticularesPas encore d'évaluation
- How Does The Brain Distinguish Between Good and Bad SmellsDocument1 pageHow Does The Brain Distinguish Between Good and Bad SmellsCarlos BacajolPas encore d'évaluation
- Session #17 SAS - AnaPhy (Lab)Document4 pagesSession #17 SAS - AnaPhy (Lab)Nicole Ken AgdanaPas encore d'évaluation
- Lesson Plan For Control GroupDocument7 pagesLesson Plan For Control Grouppete pansPas encore d'évaluation
- Reviste Medicale Internationale Cotate IsiDocument28 pagesReviste Medicale Internationale Cotate IsidoruPas encore d'évaluation
- The Gut-Liver Axis in Liver Disease: Pathophysiological Basis For TherapyDocument20 pagesThe Gut-Liver Axis in Liver Disease: Pathophysiological Basis For TherapyDayane RomanPas encore d'évaluation
- Organ Systems of The Body: - Integumentary SystemDocument12 pagesOrgan Systems of The Body: - Integumentary SystemKevin TariganPas encore d'évaluation
- Psych c61 Midterm2 ReviewDocument26 pagesPsych c61 Midterm2 ReviewKate SongPas encore d'évaluation
- Lecture 3 - Sept 14 - CH 2 Part 2 - Neuronal Basis For Cognition - REVISED POSTED SLIDESDocument29 pagesLecture 3 - Sept 14 - CH 2 Part 2 - Neuronal Basis For Cognition - REVISED POSTED SLIDESnathanagbeyi772000Pas encore d'évaluation