Académique Documents
Professionnel Documents
Culture Documents
BrazJOralSci 2009 Vol8 Issue4 p201 5
Transféré par
hardinaCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
BrazJOralSci 2009 Vol8 Issue4 p201 5
Transféré par
hardinaDroits d'auteur :
Formats disponibles
Original Article
Braz J Oral Sci.
October/December 2009 - Volume 8, Number 4
Chlorhexidine chip and tetracycline fibers
as adjunct to scaling and root planing
A clinical study
Ruchi Srivastava1; Pushpendra Kumar Verma2; Pradeep Tandon3;
Ramesh Kumar M4 ; Krishna Kumar Gupta5 ; Amitabh Srivastava6
1
BDS, Postgraduate student, Department of Periodontology & Implantology, Sardar Patel Postgraduate Institute of Dental & Medical Sciences, Lucknow, Uttar Pradesh, India
2
BDS, Postgraduate student, Department of Conservative Dentistry and Endodontics, Government Dental College, Calicut, Kerala- 673008, India
3
MDS, Professor and Head of the Department, Department of Periodontology & Implantology, Sardar Patel Postgraduate Institute of Dental & Medical Sciences, Lucknow, Uttar Pradesh, India
4
MDS, Professor and Head of the department, Department of Conservative Dentistry and Endodontics, Government Dental College, Calicut, Kerala- 673008, India
5
MDS, Professor, Department of Periodontology & Implantology, Sardar Patel Postgraduate Institute of Dental & Medical Sciences, Lucknow, Uttar Pradesh, India
6
MDS, Reader,Department of Periodontology & Implantology, Sardar Patel Postgraduate Institute of Dental & Medical Sciences, Lucknow, Uttar Pradesh, India
Abstract
Aim: Prevention of periodontal disease progression is the primary goal of periodontal therapy. When
conventional therapy is found inadequate to attain periodontal health in chronic periodontitis, local
antimicrobial agents have been used as adjunct to scaling and root planing, producing encouraging
results. Hence, a study was undertaken to evaluate clinically, the newly released sustained drugs, PerioColTMCG (Chlorhexidine - CHX- chip) with Periodontal Plus ABTM (Tetracycline fibers). Methods: Patients were
allocated in 3 experimental treatment groups, Group A- SRP + CHX Chip, Group B- SRP + Tetracycline
fibers, and Group C- SRP alone (control group). Forty-five sites in 14 patients (9 females and 5 males) with
chronic periodontitis (5-8mm probing depth), were evaluated clinically for probing depth (PD) and relative
attachment level (RAL). Results: All the treatment groups were found to be efficacious in the treatment
of periodontal disease as demonstrated by improvement in PD and RAL. Conclusion: Combination of
SRP + CHX chip (Group A) resulted in added benefits compared to the other two treatment groups.
Keywords: Chlorhexidine chip, chronic periodontitis, tetracycline fibers.
Introduction
Received for publication: November 2, 2009
Accepted: January 15, 2010
Correspondence to:
Ruchi Srivastava
Postgraduate student, Department of
Periodontology & Implantology,Sardar Patel
Postgraduate Institute of Dental &
Medical Sciences,
Lucknow, Uttar Pradesh, India
E-mail: lichi_ruchi@yahoo.com
Chronic periodontitis results in a progressive loss of attachment and formation of periodontal
pocket. The process of periodontal pocket formation represents the pathologic sequela of
microbial and inflammatory mediated degradation of collagenous connective tissue and alveolar
bone1.
Mechanical therapy may however fail to eliminate the pathogenic bacteria because of
their location within gingival tissues or in other areas inaccessible to periodontal instruments2.
Hence the use of several antimicrobial agents started gaining prominence as chemical aids
would compensate for technical limitations and prevent early microbial recolonization, to
ultimately ensure, the best chance for clinical improvements. These chemical agents may gain
access into the periodontal pocket through both a systemic and local route of delivery. Since
systemic use of antibiotics may cause several side effects (sensitivity, resistant strains and
superinfections), contemporary research is now focused on the role of topical antimicrobial
agents in the treatment of periodontitis.
Various agents have been used to prevent further progression of periodontal disease
Braz J Oral Sci. 8(4):201-205
202
Chlorhexidine chip and tetracycline fibers as adjunct to scaling and root planing A clinical study
either as monotherapy or as an adjunct to scaling and root planing
(SRP) procedure. These include tetracycline, doxycycline, minocycline,
chlorhexidine3, metronidazole4, enzymes and quaternary ammonium
compounds, which have been administered topically in pure forms by
their incorporation in chewing gums, dentifrices, acrylic strips, hollow
fibers, films, ointments, gels etc. It is clear that for local antimicrobial
therapy to be clinically effective, successful mechanisms to deliver
sustained and adequate concentration of the active agent to the
periodontal pocket are required5.
Topical antiseptics have been successfully used for treating
plaque-related gingivitis, among which chlorhexidine (CHX) remains
one of the most effective antimicrobials reported till now and is not
known for any appreciable resistance to oral microorganisms. However,
subgingival irrigation using CHX solution or CHX gels turned out to be
poorly effective in the treatment of periodontitis, due to the inability
to retain biologically significant concentrations of the drug for sufficient
lengths of time within the confines of the periodontal pocket. However,
it is difficult to maintain the effective antibacterial concentrations, for
a sufficient period in periodontal pockets for a variety of reasons like
poor penetration by mouth rinses, rapid dissipation of irrigation
solutions, relatively low localized concentrations achievable with high
systemic dose of antibiotics.
Hence, slow-release devices have been developed. There are two
subtypes: sustained release devices, delivering the drug for less than
24 h, and controlled delivery devices (CDDs), releasing the agent over
an extended period of time.
Goodson (1989) 6 pointed out that; successful control of
periodontal microflora requires a delivery of an intrinsically effective
antimicrobial agent, according to the fundamental pharmacokinetic
principles. These agents reach the site of action, i.e. the periodontal
pocket, and maintain minimum effective concentration for a sufficient
duration to produce the desired specific therapeutic effect.
Among the tested antibiotics, tetracyclines were the first and
had their efficacy evaluated in a number of periodontal clinical studies.
Tetracyclines have been incorporated into a variety of delivery systems
for insertion into periodontal pockets. These include hollow fibers7,
ethylene vinyl acetate copolymer fibers8, ethyl cellulose fibers9, acrylic
strips5, collagen preparations10.
Recently, a new local drug delivery system, PerioColTM-CG, which
contains fibrilar collagen of fish origin with 2.5 mg (approximately) of
CHX (Eucare Pharmaceuticals, Chennai, India), and another local
drug, Periodontal Plus ABTM, which contains 25 mg pure fibrilar collagen
with approximately 2 mg of evenly impregnated tetracycline
hydrochloride (Advanced Biotech Products, Chennai, India) have been
introduced.
Since research with drug delivery systems is limited, the present
clinical study evaluated comparatively the efficacy of two commercially
available new controlled-release drugs - CHX chip (PerioColTM -CG)
and Tetracycline fibers (Periodontal Plus AB)TM - as adjunct to SRP in
the treatment of chronic periodontitis.
Material and methods
Forty-five bleeding sites, with a probing depth 5-8mm, were
selected in 14 patients of both genders (9 females and 5 males) aged
between 20 to 50 years from the Outpatient Department of
Periodontics at Sardar Patel Postgraduate Institute of Dental and
Medical Sciences, Lucknow, Uttar Pradesh, India.
The Ethical committee of Sardar Patel Postgraduate Institute of
Braz J Oral Sci. 8(4):201-205
Dental and Medical Sciences, Lucknow, Uttar Pradesh, India, approved
the study and written informed consent was obtained from all patients.
Patients with good systemic health, patients who had not received any
surgical or non-surgical periodontal therapy in the past 6 months,
who had not received antibiotic therapy in the past 6 months, who
were diagnosed as suffering from chronic generalized periodontitis,
and patients who had periodontal pocket measuring 5-8mm in
different quadrants were enrolled. Individuals with history of using
anti-microbial mouthrinses within 2 months of the baseline visit or
on routine basis or patients having a history of allergy to tetracycline;
CHX or lidocaine, were excluded from the study.
The selected sites were randomly divided into 3 groups: Test
Group A (SRP + CHX Chip) Included 15 sites treated by SRP with
chlorhexidine chip. Test Group B (SRP + Tetracycline Fibers) - Included
15 sites treated by SRP with tetracycline fibers. Test Group C (SRP
alone) - Included 15 sites treated with SRP alone.
The clinical parameters recorded are the probing depth (PD)
using UNC-15 periodontal probe and relative attachment level (RAL)
using customized acrylic stent (Figure 1). After recording clinical
parameters from each site at baseline, a thorough SRP was done, in all
the 3 groups. The clinical parameters were assessed at baseline, after
1 month and 3 months after receiving all the 3 treatments in a same
patient; as it is a split-mouth study.
Fig.1. Measurement of probing depth and relative attachment level.
Chlorhexidine chip (PerioColTM- CG) (Figure 2)
PerioCol CG is a small, orange-brown in a rectangular chip form
(rounded at one end) for easy insertion into periodontal pockets. Size
of the chip is 4 x 5mm and thickness is 0.25-0.32mm and 10 mg
weight. Each chip contains approximately 2.5 mg of CHX in a
biodegradable matrix of fibrilar collagen of fish origin (Eucare
Pharmaceuticals, Chennai, India).
Tetracycline fibers (Periodontal Plus ABTM) (Figure 3)
The product contains 25 mg pure fibrilar collagen, containing
approximately 2 mg of evenly impregnated tetracycline HCl.
Periodontal Plus AB Fibers are available in strips containing four
individually packed and separable sterile product packs.
Chlorhexidine chip and tetracycline fibers as adjunct to scaling and root planing A clinical study
203
<0.05 was considered as significant. Paired t-test and Students t-test
were used to evaluate and establish differences between baseline, 1
month and 3 months values.
Fig. 2. Chlorhexidine chip (PerioColTM- CG).
Fig. 4. Placement of chlorhexidine chip
Fig. 3. Tetracycline fibers (Periodontal AB PlusTM).
Administration (Figures 4 and 5)
Subgingival administration of chlorhexidine chip was accomplished
by inserting the round end of the chip directly into the base of the
pocket. Chip was pressed apically so that it rest subgingivally at the
base of the pocket. Whereas, soaked Tetracycline fibers were inserted
into the base of the periodontal pocket. Gentle force was used with
straight probe, so that the material fills the depths and curves of the
pocket.
The gingiva was subsequently and carefully adapted to close the
entrance of the gingival margin and hand pressure was applied for
just a few minutes to encourage hemostasis and initial setting of the
material inside the pocket. The gingival margin was sealed with Coepak to prevent the dislodgement of the drug and to prevent the ingress
of oral fluids.
Both these drugs degrade within 7-10 days after insertion.
Patients were recalled after 7 days for Coe-pak removal and were
evaluated for any inflammatory response.
Patients were instructed not to chew any hard, crunchy or sticky
food for at least 1 week, postpone brushing and flossing on the treated
site for 1weeek, not to disturb the area with tongue, finger or tooth
pick, and to report immediately if the material is dislodged before the
scheduled recall visit or if pain, swelling or any other problem occurs.
The results were averaged out for each parameter. Values are
depicted as mean SD. For comparisons between different time
intervals paired t-test were used. T test for independent samples were
used for intergroup comparisons at the different time intervals, The
confidence level of the study was kept at 95% and hence a p value
Fig. 5. Placement of tetracycline fibers
Results
Results are presented in Tables 1 to 3. The recording of all the clinical
parameters was done at baseline and after 1 month and 3 months.
Finally, the complete data were statistically analyzed.
None of the subjects reported any oral symptoms at any time
during the trial such as toothache (including dental or gingival), painful
symptomatology (including oral pain, tenderness, soreness, discomfort
or sensitivity), inflammation, allergy, abscess, altered taste or increased
salivation, etc.
Probing Depth
From baseline to 3 months, Group A (SRP +CHX Chip) had significantly
higher mean percentage reduction as compared to Group B (p=0.007)
as well as Group C (p<0.001). These findings were similar to that of
previous studies11-15.
Relative Attachment Level
From baseline to 3 months Group A (SRP +CHX chip) had significantly
higher mean percentage gain as compared to Group B (p=0.046) as
well as Group C (p=0.001). These findings were similar to that of
other authors16-20, who studied the changes in probing depth following
2 years of periodontal maintenance therapy including adjunctive
controlled release of biodegradable CHX chip.
Braz J Oral Sci. 8(4):201-205
204
Chlorhexidine chip and tetracycline fibers as adjunct to scaling and root planing A clinical study
Table 1. Probing depth values (in mm).
Group A (CHX Chip + SRP)
Baseline
8.00
7.00
7.00
6.00
6.00
7.00
8.00
8.00
8.00
6.00
8.00
5.00
6.00
8.00
8.00
1 month
6.00
5.00
6.00
6.00
4.00
4.00
5.00
5.00
6.00
4.00
6.00
4.00
4.00
6.00
5.00
Group B (TTC Fibers + SRP)
3 months
3.00
3.00
4.00
5.00
3.00
3.00
3.00
4.00
5.00
3.00
4.00
3.00
3.00
5.00
4.00
Baseline
7.00
8.00
7.00
8.00
8.00
7.00
8.00
8.00
6.00
7.00
5.00
6.00
7.00
8.00
7.00
1 month
5.00
6.00
6.00
7.00
5.00
4.00
6.00
5.00
5.00
5.00
4.00
5.00
6.00
6.00
5.00
3 months
4.00
4.00
6.00
5.00
4.00
3.00
4.00
4.00
4.00
5.00
4.00
5.00
6.00
4.00
3.00
Group C (SRP alone)
Baseline
7.00
6.00
5.00
6.00
6.00
7.00
7.00
7.00
5.00
5.00
6.00
6.00
5.00
6.00
6.00
1 month
6.00
5.00
4.00
5.00
4.00
6.00
5.00
5.00
4.00
4.00
4.00
5.00
4.00
5.00
4.00
3 months
5.00
5.00
4.00
5.00
4.00
5.00
5.00
4.00
4.00
5.00
5.00
5.00
3.00
5.00
5.00
Table 2. Relative attachment level values (in mmm).
Group A (CHX Chip + SRP)
Baseline
12.00
11.00
11.00
10.00
10.00
11.00
11.00
11.00
12.00
10.00
12.00
9.00
10.00
11.00
11.00
1 month
8.00
7.00
7.00
7.00
9.00
8.00
6.00
7.00
7.00
8.00
9.00
7.00
8.00
8.00
8.00
Group B (TTC Fibers +SRP)
3 months
6.00
6.00
7.00
5.00
8.00
8.00
6.00
6.00
7.00
7.00
8.00
6.00
6.00
7.00
6.00
Baseline
11.00
12.00
10.00
11.00
11.00
12.00
11.00
11.00
8.00
9.00
9.00
10.00
10.00
11.00
11.00
1 month
8.00
8.00
8.00
8.00
9.00
9.00
7.00
7.00
6.00
7.00
7.00
7.00
8.00
7.00
8.00
3 months
8.00
7.00
7.00
8.00
8.00
8.00
7.00
6.00
6.00
7.00
6.00
7.00
8.00
7.00
7.00
Group C (SRP alone)
Baseline
10.00
9.00
8.00
9.00
10.00
11.00
10.00
9.00
7.00
8.00
8.00
9.00
8.00
9.00
10.00
1 month
7.00
7.00
6.00
7.00
8.00
9.00
7.00
6.00
6.00
6.00
6.00
8.00
7.00
7.00
8.00
3 months
7.00
6.00
7.00
6.00
8.00
9.00
7.00
6.00
5.00
6.00
6.00
8.00
7.00
6.00
6.00
Table 3. Post treatment clinical changes and comparison between the 3 groups
Measurement
Groups
0-1 month
0-3 months
Probing depth(in mm)
Group A
Group B
Group C
2.0000.795
1.8030.716
1.3400.489
p < 0.01 Sig.
3.2001.099
2.8660.788
2.0000.605
p < 0.01 Sig.
3.4000.995
2.8031.231
1.4000.754
p < 0.01 Sig.
4.2001.214
3.3330.821
2.3341.000
p < 0.01 Sig.
Significance
Relative attachmentlevel
(Gain) (in mm)
Group A
Group B
Group C
Significance
Discussion
A periodontal disease essentially comprises of a group of oral
infections, whose primary etiological factor is dental plaque, which
results in an inflammatory lesion in the supporting tissues. Removal
of the cause (and its effects) is the primary aim of both non-surgical
and surgical treatment regimens. The major non-surgical therapeutic
approach involves mechanical SRP. The infective nature of the disease
has lead to the widespread use of antimicrobials, as an adjunct to
SRP.
Local delivery of controlled release antimicrobials has some
advantages over the systemic route, including the high local drug
levels in the periodontal pockets and avoidance of drug compliance
Braz J Oral Sci. 8(4):201-205
issues. In the present study, an attempt was made to evaluate
effectiveness of CHX chip (PerioColTM- CG) and tetracycline fibers
(Periodontal AB PlusTM), in the treatment of chronic periodontitis, as
an adjunct to SRP. CHX and tetracycline were chosen in the present
study, because of their proven efficacy in the management of periodontal
diseases. Tetracycline is known for its antibacterial actions and also
due to number of additional properties that have been recently
identified. These include colagenase inhibition, anti-inflammatory
actions and inhibition of bone resorption.
CHX is a widely used broad-spectrum antimicrobial agent,
encompassing gram-positive and gram-negative bacteria, yeasts,
Chlorhexidine chip and tetracycline fibers as adjunct to scaling and root planing A clinical study
dermatophytes and some lipophilic viruses. The antibacterial mode
of action is explained by the fact that the cationic CHX molecule is
rapidly attracted by the negatively charged bacterial cell surface. After
adsorption, the integrity of the bacterial cell membrane is altered,
which results in a reversible leakage of bacterial low molecular-weight
components at low dosage or more severe membrane damage at
higher doses (bactericidal). Tetracycline-HCl is a bacteriostatic agent
that inhibits bacterial protein synthesis and, as such, requires a
significantly longer exposure time for bacterial damage than, for
example, metronidazole or CHX. It however, has the ability to bind to
the hard tissue walls of pockets to establish a drug reservoir.
The crux of the present study clearly shows that, the locally
delivered CHX chip (PerioColTM-CG) along with mechanical debridement
resulted in a clinically meaningful improvement of all clinical parameters,
which was maintained significant throughout the study duration.
In order to be effective, a pharmaceutical agent should reach the
entire periodontal pocket up to the bottom and should be maintained
long enough at a sufficient concentration for the intended
pharmaceutical effect to occur. Periodontal pockets, however, possess
complicating anatomic characteristics. Furthermore, periodontal
pathogens in the subgingival environment reside in a biofilm adhering
to the exposed root cementum or to the soft tissue, or even invading
the pocket epithelium, the underlying connective tissue or the root
dentin. The aggregation of bacteria in a biofilm impairs the diffusion
or may even inactivate antimicrobial agents. Thus, high concentrations
of antimicrobial agents are needed before a beneficial effect can be
expected. Various biofilm experiments indicate that the necessary
minimum inhibitory concentrations (MIC) of antimicrobial agents,
are at least 50 times higher (or even 210,000 times), than for bacteria
growing under planktonic conditions21-23.
Moreover, the minimum contact time for an antimicrobial agent
to be active depends on the mechanism by which the agent inhibits or
destroys target bacteria. CHX (which kills microorganisms by
compromising the integrity of the cell membrane) and povidone-iodine
(which kills bacteria on contact) require a shorter exposure time than,
for example, a bacteriostatic agent, such as tetracycline, which inhibits
protein synthesis23.
However, the substantivity of a topically applied agent is increased
spontaneously, if it binds to the soft and/or hard tissue surfaces within
the pocket. CHX has the advantage of prolonged supragingival
substantivity, because it can bind to the intraoral soft and hard tissues24.
Ciancio et al.25, reported that tetracycline applied via TTC-fibers does
not penetrate into the gingiva a significant distance to kill or suppress
tissue invasive organisms, such as A. actinomycetemcomitans.
Besides the pharmacokinetics, the patients comfort, ease of
placement of the drug into the periodontal pocket and the costbenefit ratio are key elements for determining the selection and
efficacy of a product.
The results from the present study suggest that the application of
CHX chip combined with SRP is beneficial in the treatment of chronic
periodontitis and improving periodontal parameters for 3 months
duration. In spite of the proven additive benefits, the availability and
costs associated with controlled delivery devices have so far limited
their application. However, as this material i.e. PerioColTM- CG (CHX
chip) is of Indian origin, easy to place in periodontal pocket, less time
consuming and is relatively cost effective, its use can be expanded easily
in Indian population.
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
205
Drisko CL, Cobb CM, Killoy WJ, Michalowicz BS, Pihlstrom BL, Lowenguth RA et
al. Evaluation of periodontal treatment using controlled release tetracycline
fibers: clinical response. J Periodontol. 1995; 66: 692-9.
Slots J, Rams TE. Antibiotics in periodontal therapy: Advantages and
disadvantages. J Clin Periodontol. 1990; 17: 479-95
Cetin EO, Buduneli N, Atlihan E, Kirilmaz L. In vitro studies on controlled-release
cellulose acetate films for local delivery of chlorhexidine, indomethacin, and
meloxicam. J Clin Periodontol. 2004; 31: 1117-21.
Kaner D, Bernimoulin J-P, Hopfenmuller W, Kleber B-M, Friedmann A.
Controlled-delivery chlorhexidine chip versus amoxicillin/ metronidazole as
adjunctive antimicrobial therapy for generalized aggressive periodontitis: a
randomized controlled clinical trial. J Clin Periodontol. 2007; 34: 880-91.
Addy M, Rawle L, Handley R, Newman HN, Coventry JF. The development and
in-vitro evaluation of acrylic strips and dialysis tubing for local drug delivery.
J Periodontol. 1982; 53: 693-9.
Goodson JM. Pharmacokinetic principles controlling efficacy of oral therapy. J
Dent Res.. 1989; 68: 1625-32.
Goodson JM, Haffajee A, Socransky SS. Periodontal therapy by local delivery of
tetracycline. J Clin Periodontol. 1979; 6: 83-92.
Goodson JM, Holborow D, Dunn RL, Hogan P, Dunham S. Monolithic tetracycline
containing fibers for controlled delivery to periodontal pockets. J Periodontol.
1983; 54: 575-9.
Friedman M, Golomb G. New sustained release dosage form of chlorhexidine
for dental use. 1. Development and kinetics of release. J Periodont Res. 1982;
17: 323-8.
Minabe M, Takeuchi K, Tamura T, Hori T, Umemoto T. Subgingival administration
of tetracycline on a collagen film. J Periodontol. 1989; 60: 552-6.
Jeffcoat MK, Bray KS, Ciancio SG, Dentino AR, Fine DH, Gordon JM et al.
Adjunctive use of a subgingival controlled-release chlorhexidine chip reduces
probing depth and improves attachment level compared with scaling and
root planing alone. J Periodontol. 1998; 69: 989-97.
Killoy WJ. Assessing the effectiveness of locally delivered chlorhexidine in the
treatment of periodontits. J Am Dent Assoc. 1999; 130: 567-90.
Heasman PA, Heasman L, Stacey F, McCracken GI. Local delivery of chlorhexidine
gluconate (PerioChipTM) in periodontal maintenance patients. J Clini
Periodontol. 2001; 28: 90-5.
R. Mythili, T. Ramakrishnan, Biju Mammen. Effect of controlled-release device
containing chlorhexidine gluconate in the treatment of adult periodontitis A
clinical and microbiological study. J Ind Soc Periodontol. 2006; 10: 321-4.
Ronald HW Cheng, W. Keung Leung, Esmonde F. Corbet. Non-surgical
periodontal therapy with adjunctive chlorhexidine use in adults with Down
Syndrome. A prospective case series. J Periodontol. 2008; 79: 379-85.
Soskolne WA, Proskin HM, Stabholz A. Probing depth changes following 2 years
of periodontal maintenance therapy including adjunctive controlled release of
chlorhexidine. J Periodontol. 2003; 74: 420-7.
Chen YT, Hung SL, Lin LW, Chi LY, Ling LJ. Attachment of periodontal ligament
cells to Chlorhexidine loaded guided tissue regeneration membranes. J
Periodontol. 2003; 74: 1652-59.
Juliana Carvalho, M. John Novak, LF Mota. Evaluation of the effect of subgingival
placement of chlorhexidine chips as an adjunct to scaling and root planing. J
Periodontol. 2007; 78: 997-1001.
Paolantonio M, DAngelo M, Grassi RF, Perinetti G, Piccolomini R, Pizzo G et al.
Clinical and microbiologic effects of subgingival controlled release delivery of
chlorhexidine chip in the treatment of periodontitis : a multicenter study. J
Periodontol. 2008; 79: 271-82.
Mizrak T, Guncu GN, Caglayan F, Balci TA, Aktar GS, Ipek F. Effect of a controlled
release chlorhexidine chip on clinical and microbiological parameters and
prostaglandin E2 levels in gingival crevicular fluid. J Periodontol. 2006; 77: 437-43.
Rodrigues IF, Machion L, Casati MZ, Nociti FH Jr, de Toledo S, Sallum AW, Sallum
EA. Clinical evaluation of the use of locally delivered chlorhexidine in periodontal
maintenance therapy. J Periodontol. 2007; 78: 624-8.
Iyad Hussein, Meena Ranka, Angela Gilbert and Kevin Davey. Locally delivered
antimicrobials in the management of periodontitis: a critical review of the
evidence for their use in practice. Dent Update. 2007; 34: 494-506.
Quirynen M, Teughels W, De Soete M, van Steenberghe D. Topical antiseptics
and antibiotics in the initial therapy of chronic adult periodontitis: microbiological
aspects. Periodontol 2000. 2002; 28: 72-90.
Bonesvoll P, Gjermo P. A comparison between chlorhexidine & some quaternary
ammonium compounds with regard to retention, salivary concentration &
plaque inhibiting effect in human mouth after mouth rinses. Arch Oral Biol.
1978; 23: 289-94.
Ciancio SG, Cobb CM, Leung M. Tissue concentration and localization of
tetracycline following site specific tetracycline fiber therapy. J Periodontol.
1992; 63: 849-53.
References
Braz J Oral Sci. 8(4):201-205
Vous aimerez peut-être aussi
- Tonsil PictureDocument10 pagesTonsil PicturehardinaPas encore d'évaluation
- 13 38 1 PBDocument5 pages13 38 1 PBhardinaPas encore d'évaluation
- AbsenteeismDocument6 pagesAbsenteeismArga KafiPas encore d'évaluation
- University of Michigan Normalizes 3D Printing of TrachealDocument3 pagesUniversity of Michigan Normalizes 3D Printing of TrachealhardinaPas encore d'évaluation
- Tracheal Collapse-ToRing or ToStent PDFDocument3 pagesTracheal Collapse-ToRing or ToStent PDFhardinaPas encore d'évaluation
- RespimatDocument8 pagesRespimathardinaPas encore d'évaluation
- Electric NebuDocument5 pagesElectric NebuhardinaPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Waleed Hassan, 00551188, Vivid Institute of Occupational Safety & Health-940Document19 pagesWaleed Hassan, 00551188, Vivid Institute of Occupational Safety & Health-940qadeesbhatti09511Pas encore d'évaluation
- Pat An AnewDocument126 pagesPat An AnewgshchurovskiyPas encore d'évaluation
- American Family PhysicianDocument4 pagesAmerican Family PhysicianGoddess Nth The Artemis EffectPas encore d'évaluation
- Bronchopneumonia Care PlanDocument6 pagesBronchopneumonia Care PlanAbhijit Soundade0% (1)
- Vital Signs NotesDocument3 pagesVital Signs NotesJoelyn Noble CabalatunganPas encore d'évaluation
- Challenges Faced by Families of Autistic Children-153Document5 pagesChallenges Faced by Families of Autistic Children-153Zahoor Ahmad100% (1)
- Heart Reviewer 1Document6 pagesHeart Reviewer 1tokzzPas encore d'évaluation
- CellCommunication Assessment3Document6 pagesCellCommunication Assessment3Michaela Maria GarciaPas encore d'évaluation
- 4th HEALTH SUMMATIVE TEST Grade 8Document2 pages4th HEALTH SUMMATIVE TEST Grade 8Albert Ian Casuga90% (10)
- 299.08 - Renal Pathology) Chronic Kideny Disease (CKD)Document15 pages299.08 - Renal Pathology) Chronic Kideny Disease (CKD)AnishilPas encore d'évaluation
- Summary Notes - Topic 9 Transport in Animals - CIE Biology IGCSEDocument5 pagesSummary Notes - Topic 9 Transport in Animals - CIE Biology IGCSEMadhan Reddy SuddalaPas encore d'évaluation
- Digestive System Charts 1Document14 pagesDigestive System Charts 1api-306762527Pas encore d'évaluation
- ControlDocument10 pagesControlAhmed FathiPas encore d'évaluation
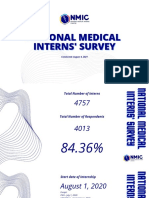
- National Medical National Medical Interns' Survey Interns' SurveyDocument20 pagesNational Medical National Medical Interns' Survey Interns' SurveyKaren Jodes CapananPas encore d'évaluation
- The Role of Chronic PainDocument23 pagesThe Role of Chronic PainNovia RambakPas encore d'évaluation
- Revalida 1Document3 pagesRevalida 1herrabiel solisPas encore d'évaluation
- HypothesisDocument4 pagesHypothesisSunny Boy Ng SinadjanPas encore d'évaluation
- Vestibular SchwannomaDocument12 pagesVestibular SchwannomaEustakia Rini Kartika DewiPas encore d'évaluation
- Origin and Importance of GeneticsDocument12 pagesOrigin and Importance of Geneticshuyenthanh1807100% (1)
- Crozer Manual - Second Edition PDFDocument219 pagesCrozer Manual - Second Edition PDFTyler Lawrence CoyePas encore d'évaluation
- Glossary of Commonly Used Dental Terms: 14212 Ambaum Boulevard Southwest Suite #101, Burien, WA 98166Document10 pagesGlossary of Commonly Used Dental Terms: 14212 Ambaum Boulevard Southwest Suite #101, Burien, WA 98166Mayra RojasPas encore d'évaluation
- Newborn Screening of Neuromuscular Diseases - 2021 - Neuromuscular DisordersDocument11 pagesNewborn Screening of Neuromuscular Diseases - 2021 - Neuromuscular DisordersSuzie Simone Mardones SilvaPas encore d'évaluation
- SunCoBe ShampooDocument24 pagesSunCoBe ShampooDong YulPas encore d'évaluation
- Medical Revision PaperDocument106 pagesMedical Revision PaperDavin SugumarPas encore d'évaluation
- WSN 78 (2017) 193-198Document6 pagesWSN 78 (2017) 193-198Santiago López BuitragoPas encore d'évaluation
- Anatomy and Physiology of EyelidDocument34 pagesAnatomy and Physiology of Eyelidsushma shrestha100% (1)
- MCN ReviewerDocument5 pagesMCN ReviewerJunghoon YangParkPas encore d'évaluation
- Persuasive LetterDocument2 pagesPersuasive Letterapi-341527188Pas encore d'évaluation
- Strategies For Feeding The Preterm Infant: ReviewDocument10 pagesStrategies For Feeding The Preterm Infant: ReviewSanjuy GzzPas encore d'évaluation