Académique Documents
Professionnel Documents
Culture Documents
Igra Factsheet Oct2011 PDF
Transféré par
AuliaRahmanTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Igra Factsheet Oct2011 PDF
Transféré par
AuliaRahmanDroits d'auteur :
Formats disponibles
TUBERCULOSIS
www.who.int/tb
IGRA TB TESTS
Policy Statement 2011
The use of TB Interferon-Gamma Release Assays
(IGRAs) in Low- and Middle-income Countries
CONCLUSION
This policy applies to the use of
There is insufficient data and low quality
evidence on the performance of IGRAs in
low- and middle-income countries, typically
those with a high TB and/or HIV burden
IGRAs and the tuberculin skin test (TST)
cannot accurately predict the risk of infected
individuals developing active TB disease
Neither IGRAs nor the TST should be used
for the diagnosis of active TB disease
IGRAs are more costly and technically
complex to do than the TST. Given
comparable performance but increased cost,
replacing TST by IGRAs as a public health
intervention in resource-constrained settings
is not recommended
commercial IGRAs* in low- and
middle-income countries only
Commercial IGRAs are FDAapproved as indirect and adjunct
tests for TB infection, in conjunction
with risk assessment, radiography
and other medical and diagnostic
evaluations. Several international
guidelines on their use in highincome countries are available
This policy statement is not
intended to apply to high-income
countries or to supersede their
national guidelines
* QuantiFERON-TB Gold (QFT-G) and QuantiFERON-TB Gold InTube (QFT-GIT), (Cellestis, Australia); T-SPOT.TB (Immunotec, UK)
Exposure to Mycobacterium tuberculosis may result in latent TB infection. A person with latent
TB infection usually leads a healthy life without developing active TB disease. 2 billion people
have latent TB infection but only a fraction (<10 million a year) fall sick with active TB disease.
Testing for TB Infection and Disease
WHICH TEST AND WHEN?
IGRAs and the TST are designed to detect latent
TB infection. They are 'indirect tests' - they do not
detect the actual TB bacilli but instead an immune
response that suggests past or present exposure to
TB bacilli
Microscopy, growth on culture, and molecular tests
are designed to detect active TB disease. They are
'direct tests' that show the presence of the actual TB
bacilli or their DNA
IGRA and the TST tests cannot distinguish
between latent TB infection and active TB disease.
They are therefore expected to have poor specificity
for active TB in high-burden settings due to a high
background prevalence of latent TB infection
IGRAs vs TUBERCULIN SKIN TEST
IGRAs require a single patient visit, results are
available in 24-48hrs, and prior BCG
vaccination does not cause false-positive
results
IGRAs are expensive, require blood to be
drawn, special laboratory infrastructure and
supplies, and adequately trained staff
TST requires two patient visits, results are
available in 48-72hrs, and BCG vaccination
may cause false-positive results in younger
persons
TST is not expensive, requires an injection
into the skin, adequately trained staff, and no
special laboratory infrastructure or supplies
This policy was developed in compliance with the GRADE process for evidence synthesis and formulation of recommendations and
approved by the WHO Guidelines Review Committee, having satisfied the requirements for guideline development.
WHO Sept 2011
For more information: http://www.who.int/tb/laboratory/policy_statements/en
Turning Evidence into Policy and Practice
in Low- and Middle-Income Countries
IGRAs in DIAGNOSING active TB disease
IGRAs in PREDICTING active TB disease
There was no consistent evidence that IGRAs were
more sensitive than TST for diagnosis of active TB
disease. Two studies that evaluated the
incremental value of IGRAs to conventional
microbiological tests found no meaningful
contribution of IGRAs to the diagnosis of active TB.
IGRAs were considered inadequate as rule-out or
rule-in tests for active TB, especially in the context
of HIV infection.
IGRAs and the TST appeared to have only modest predictive
value and did not help identify those who were at highest risk
of progression to disease.
19 studies simultaneously estimating sensitivity and specificity
among 2,067 TB suspects showed a pooled sensitivity of 83%
(95% CI 70% - 91%) and pooled specificity of 58% (95% CI
42% - 73%) for T-SPOT (8 studies), and a pooled sensitivity of
73% (95% CI 61% -82%) and pooled specificity of 49% (95%
CI 40% - 58%) for QFT-GIT (11 studies). Among HIV-infected
patients, pooled sensitivity was between 60% (QFT-GIT) and
76% (T-SPOT). Pooled specificity was low for both IGRA
platforms (T-SPOT, 61%; QFT-GIT, 52%) and among HIVinfected persons (T-SPOT 61%; QFT-GIT 50%).
IGRAs in CHILDREN
IGRAs and the TST showed similar sensitivity in
detecting TB infection or disease, with reduced
sensitivity in young or HIV-infected children.
Collecting blood for IGRA testing in young children
was a specific challenge.
Two small studies prospectively measured incident TB in
children tested with IGRAs (QFT) and reported conflicting
results. Association of test response with exposure
(categorised dichotomously or as a gradient) was similar for
TST, QFT and T-SPOT, although differences in study
methodology limited the comparability of results.
IGRAs in
HEALTH CARE WORKER SCREENING
Data on serial testing and reproducibility of IGRAs,
as well as evidence on the predictive value of
IGRAs in health care workers (HCWs), are still
absent for high-incidence settings. There is no data
to suggest that IGRAs are better or worse than the
TST for identifying new TB infections after
exposure in HCWs, but serial IGRA testing is
compounded by a lack of optimum cut-offs and
unclear interpretation and prognosis of IGRA
conversions and reversions.
Two cross-sectional studies compared IGRA and TST
performance in HCWs. IGRA and TST positivity rates were high
in HCWs, ranging from 40% to 66%. IGRA positivity was
slightly lower than TST positivity but no consistent difference in
the prevalence of positive tests was evident.
Large prospective cohort studies have shown that persons with a positive
TST have a 1.4 to 1.7-fold higher rate of active TB within one year
compared to persons with a negative TST result. Three studies provided
incidence rate ratios (IRR) of TB stratified by IGRA as well as TST status at
baseline. The association with subsequent incident TB in test-positive
individuals compared to test-negatives was higher but not statistically
significant for IGRA compared to TST (IGRA: IRR=3.24; 95CI 0.62-5.85;
TST: IRR=2.28; 95CI 0.83-3.73: p=0.90). Both IGRAs and TST seemed to
show positive associations with exposure but the strength of the
association varied across populations, irrespective of BCG vaccination.
Both IGRAs and TST appeared to have only modest predictive value , suboptimal sensitivity, and did not help identify those who were at highest risk
of progression to disease.
IGRAs in PEOPLE LIVING WITH HIV
IGRAs seemed to perform similarly to the TST in identifying
HIV-infected individuals with latent TB infection and both
tests were adversely affected by low CD4+ count. The
benefit of isoniazid preventive therapy is greatest in
individuals with a positive TST although routine TST
screening is not considered mandatory in HIV-infected
persons. There is currently no evidence that people with
TST-negative/IGRA-positive results do better on isoniazid
preventive therapy than those with negative IGRA results.
37 studies involving 5,736 HIV-infected individuals were evaluated. 5
studies compared head-to-head sensitivity of IGRAs and TST for active TB:
T-SPOT was more sensitive than TST in one study (absolute difference
50%; 95CI 29%-71% ), less sensitive in one study (absolute difference
18%; 95CI 2%-34%), and as sensitive in one study (absolute difference 3%; 95CI -17% to11%). Similarly, QFT-GIT was more sensitive than TST in
one study (absolute difference 41%; 95CI 22%-60%) and less sensitive
than TST in one study (absolute difference 33%; 95CI 16%-51%). In three
longitudinal studies, the risk of active TB was higher in HIV-infected
individuals with positive versus negative IGRA results; however, the
difference was not significant in the two studies that reported IGRA results
according to manufacturer-recommended criteria.
IGRAs in CONTACT SCREENING
and OUTBREAK INVESTIGATIONS
The majority of studies showed comparable latent TB
infection prevalence by TST or IGRA and variable
associations with levels of exposure. Wide discordance
between TST and IGRA results was evident, mostly of the
TST-positive/IGRA-negative type.
16 studies evaluated IGRAs in contact screening and outbreak
investigations. Data could not be pooled due to significant heterogeneity in
study design and outcomes assessed. Most studies showed comparable
infection prevalence by TST or IGRA in contacts.
Vous aimerez peut-être aussi
- Post-Cardiac Arrest SyndromeDocument30 pagesPost-Cardiac Arrest SyndromeAuliaRahmanPas encore d'évaluation
- 10 1 1 563 4316 PDFDocument5 pages10 1 1 563 4316 PDFAuliaRahmanPas encore d'évaluation
- Centor ScoreDocument8 pagesCentor ScoreLoo DonPas encore d'évaluation
- Jurnal OkeDocument8 pagesJurnal OkeAuliaRahmanPas encore d'évaluation
- VACTERL-association EN PDFDocument12 pagesVACTERL-association EN PDFAuliaRahmanPas encore d'évaluation
- Chicken Pox Guidelines PDFDocument1 pageChicken Pox Guidelines PDFAuliaRahmanPas encore d'évaluation
- Anamnesis:: BB KG TB CM No - RM TGL - Masuk TGL - Lahir DPJPDocument4 pagesAnamnesis:: BB KG TB CM No - RM TGL - Masuk TGL - Lahir DPJPAuliaRahmanPas encore d'évaluation
- 2006 118 1774 Subcommittee On Diagnosis and Management of BronchiolitisDocument22 pages2006 118 1774 Subcommittee On Diagnosis and Management of BronchiolitisAuliaRahmanPas encore d'évaluation
- Centor ScoreDocument8 pagesCentor ScoreLoo DonPas encore d'évaluation
- Anamnesis:: BB KG TB CM No - RM TGL - Masuk TGL - Lahir DPJPDocument4 pagesAnamnesis:: BB KG TB CM No - RM TGL - Masuk TGL - Lahir DPJPAuliaRahmanPas encore d'évaluation
- RHDDocument130 pagesRHDDeepu RajendranPas encore d'évaluation
- Who TRS 923 PDFDocument130 pagesWho TRS 923 PDFAuliaRahmanPas encore d'évaluation
- Incase Qobam Lab 17 MaretDocument6 pagesIncase Qobam Lab 17 MaretAuliaRahmanPas encore d'évaluation
- Igra Factsheet Oct2011Document2 pagesIgra Factsheet Oct2011AuliaRahmanPas encore d'évaluation
- Chicken Pox Guidelines PDFDocument1 pageChicken Pox Guidelines PDFAuliaRahmanPas encore d'évaluation
- Varicella Vaccination AlgorithmDocument1 pageVaricella Vaccination AlgorithmAuliaRahmanPas encore d'évaluation
- Syarah Hikam 1Document108 pagesSyarah Hikam 1AuliaRahmanPas encore d'évaluation
- NEWSDocument183 pagesNEWSSebastian BaqueroPas encore d'évaluation
- Diagnosis of Childhood Acute Lymphoblastic Leukemia and Optimization of Risk-Benefit Ratio of TherapyDocument24 pagesDiagnosis of Childhood Acute Lymphoblastic Leukemia and Optimization of Risk-Benefit Ratio of TherapyAuliaRahmanPas encore d'évaluation
- Interesting Case March, 15 2016: Sri Yati, Charles, Aulia, Fanny, SasaDocument31 pagesInteresting Case March, 15 2016: Sri Yati, Charles, Aulia, Fanny, SasaAuliaRahmanPas encore d'évaluation
- Makalah Brain GYM International, BDocument17 pagesMakalah Brain GYM International, BAuliaRahmanPas encore d'évaluation
- Interesting Case March, 15 2016: Sri Yati, Charles, Aulia, Fanny, SasaDocument31 pagesInteresting Case March, 15 2016: Sri Yati, Charles, Aulia, Fanny, SasaAuliaRahmanPas encore d'évaluation
- bRAIN gYMDocument11 pagesbRAIN gYMshannay201050% (2)
- Wilayah 3'-DiterjemahkanDocument1 pageWilayah 3'-DiterjemahkanAuliaRahmanPas encore d'évaluation
- Breastfeeding: Best For Baby and MotherDocument12 pagesBreastfeeding: Best For Baby and MotherSari Whardani Mahligai PateryPas encore d'évaluation
- Interesting Case 27.03.2013Document10 pagesInteresting Case 27.03.2013AuliaRahmanPas encore d'évaluation
- Diagnosis of Childhood Acute Lymphoblastic Leukemia and Optimization of Risk-Benefit Ratio of TherapyDocument24 pagesDiagnosis of Childhood Acute Lymphoblastic Leukemia and Optimization of Risk-Benefit Ratio of TherapyAuliaRahmanPas encore d'évaluation
- Pediatric Dental CareDocument27 pagesPediatric Dental CareAuliaRahmanPas encore d'évaluation
- Interesting Case: Masruri, Esha, Alex, Milza, Wicak, Gita, Zaki, Arin, Eni, FiaDocument10 pagesInteresting Case: Masruri, Esha, Alex, Milza, Wicak, Gita, Zaki, Arin, Eni, FiaAuliaRahmanPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Total Selection Leftover Seats Morning PDFDocument12 pagesTotal Selection Leftover Seats Morning PDFSoniyaKanwalGPas encore d'évaluation
- Pandi An 2009Document4 pagesPandi An 2009Arkoprovo HalderPas encore d'évaluation
- Intermittent Asthma Case ReportDocument91 pagesIntermittent Asthma Case ReportCindy PrayogoPas encore d'évaluation
- Acute Renal Failure Nursing Care PlanDocument15 pagesAcute Renal Failure Nursing Care PlanRanusha AnushaPas encore d'évaluation
- Overcoming Shyness and InhibitionDocument3 pagesOvercoming Shyness and InhibitionralucaPas encore d'évaluation
- Gingival EnlargementCORRECTEDDocument7 pagesGingival EnlargementCORRECTEDLita DamafitraPas encore d'évaluation
- Mortality Toolkit PDFDocument41 pagesMortality Toolkit PDFAhmedPas encore d'évaluation
- Abnormal Psychology TestDocument7 pagesAbnormal Psychology TestCamae Snyder GangcuangcoPas encore d'évaluation
- Basic Information About Newborn ScreeningDocument5 pagesBasic Information About Newborn ScreeningJohn Ray AnderPas encore d'évaluation
- Internship 3Document4 pagesInternship 3Hirschmann Andro BoquilaPas encore d'évaluation
- Nursing Home Lesson PlanDocument3 pagesNursing Home Lesson Planapi-353697276100% (2)
- Published United States Court of Appeals For The Fourth CircuitDocument14 pagesPublished United States Court of Appeals For The Fourth CircuitScribd Government DocsPas encore d'évaluation
- TeratologyDocument36 pagesTeratologySafera RezaPas encore d'évaluation
- The Daily GrindDocument2 pagesThe Daily GrindRodrigo CarbajalPas encore d'évaluation
- Telephone DirectoryDocument9 pagesTelephone DirectoryRexelle RamosPas encore d'évaluation
- Novel Antiangiogenic Agents: Current Clinical Development: George W. Sledge, Jr. MD Indiana University Cancer CenterDocument27 pagesNovel Antiangiogenic Agents: Current Clinical Development: George W. Sledge, Jr. MD Indiana University Cancer CenterHaidir MuhammadPas encore d'évaluation
- Assignment 1 Evaluation and ManagementDocument5 pagesAssignment 1 Evaluation and ManagementHugsPas encore d'évaluation
- Letter For Participation in Internship Manila CampusDocument4 pagesLetter For Participation in Internship Manila CampusSEAN MELNOR LOSBAÑESPas encore d'évaluation
- GPP Conference Yields Strategies and Declaration for SE AsiaDocument83 pagesGPP Conference Yields Strategies and Declaration for SE AsiaMaria Wisnu DonowatiPas encore d'évaluation
- Bala MedicinalDocument23 pagesBala MedicinalJayesh BorolePas encore d'évaluation
- Request for Religious Exemption from COVID VaccineDocument20 pagesRequest for Religious Exemption from COVID VaccineSara BPas encore d'évaluation
- 105 Brucellosis: Etiology/Pathophysiology EpidemiologyDocument3 pages105 Brucellosis: Etiology/Pathophysiology EpidemiologyDamián ContrerasPas encore d'évaluation
- On Cardio Respiratory ExerciseDocument9 pagesOn Cardio Respiratory ExercisegomPas encore d'évaluation
- Congenital-Abnormalities-and-Preterm-Birth-Related-to-Maternal-Illnesses-During-Pregnancy (2010) PDFDocument542 pagesCongenital-Abnormalities-and-Preterm-Birth-Related-to-Maternal-Illnesses-During-Pregnancy (2010) PDFPuspa Sekar MentariPas encore d'évaluation
- Heart Defects and Vascular Anomalies: Causes, Types and TreatmentDocument17 pagesHeart Defects and Vascular Anomalies: Causes, Types and TreatmentA.V.M.Pas encore d'évaluation
- Clinical Parasitology: 1. Direct Fecal Smear (DFS)Document3 pagesClinical Parasitology: 1. Direct Fecal Smear (DFS)Monique Eloise GualizaPas encore d'évaluation
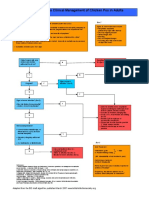
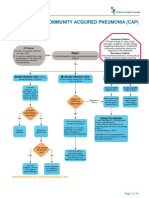
- Complicated Community Acquired Pneumonia Clinical PathwayDocument14 pagesComplicated Community Acquired Pneumonia Clinical PathwayFaisalMuhamadPas encore d'évaluation
- 7690 - Intermediate - Care Service Model Flow ChartDocument2 pages7690 - Intermediate - Care Service Model Flow ChartRizqon Sya'baniPas encore d'évaluation
- Nicu Case StudyDocument4 pagesNicu Case Studyapi-508102663Pas encore d'évaluation
- 10-Gram Monofilament TestDocument2 pages10-Gram Monofilament TestAlimyon Abilar MontoloPas encore d'évaluation