Académique Documents
Professionnel Documents
Culture Documents
Roberts 2009
Transféré par
RosarioBengocheaSecoCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Roberts 2009
Transféré par
RosarioBengocheaSecoDroits d'auteur :
Formats disponibles
Available online at www.sciencedirect.
com
Psychiatry Research 166 (2009) 141 147
www.elsevier.com/locate/psychres
Social cognition and interaction training (SCIT) for outpatients with
schizophrenia: A preliminary study
David L. Roberts, David L. Penn
Department of Psychology, University of North Carolina, Chapel Hill, NC, USA
Received 22 September 2007; received in revised form 10 February 2008; accepted 20 February 2008
Abstract
Social functioning deficits (e.g., social skill, community functioning) are a core feature of schizophrenia. These deficits are only
minimally improved via the frontline treatments for schizophrenia (e.g. medication, social skills training, cognitive-behavioral
therapy). Social cognition is a promising treatment target in this regard as it may be more strongly related to social functioning
outcomes than traditional neurocognitive domains [Couture, S., Penn, D.L., Roberts, D.L., 2006. The functional significance of
social cognition in schizophrenia: a review. Schizophrenia Bulletin (Suppl. 1), S-4463]. Social cognition and interaction training
(SCIT) is a 20-week, manualized, group treatment designed to improve social functioning in schizophrenia by way of improved
social cognition. This article reports preliminary data from a quasi-experimental study comparing SCIT + treatment as usual (TAU;
n = 20) to TAU alone (n = 11) among outpatients. Results using analysis of variance (ANOVA) suggest SCIT-related improvements
in emotion perception and social skill.
2008 Elsevier Ireland Ltd. All rights reserved.
Keywords: Psychosis; Emotion perception; Theory of Mind; Attributional style; Social functioning
1. Introduction
Social cognition is impaired in schizophrenia (Penn
et al., 2006), is relatively independent of traditional
neurocognitive domains (e.g. attention, memory,
executive functioning), and may be the strongest
predictor of functional outcome in this illness (Couture
et al., 2006; Brne et al., 2007). For these reasons,
there has been recent interest in social cognitive treat Corresponding author. University of North Carolina, Chapel Hill,
Department of Psychology, CB: #3270, Davie Hall, Chapel Hill, NC,
27599, USA. Tel.: +1 919 843 7514; fax: +1 919 962 2537.
E-mail address: dpenn@email.unc.edu (D.L. Penn).
ment interventions. Most of these interventions can be
conceptualized as either targeted (e.g. Silver et al.,
2004) or broad-based (e.g. Hogarty et al., 2004)
approaches. Targeted interventions focus on a single
social cognitive ability (e.g. emotion perception),
whereas broad-based interventions typically comprise
a variety of psychosocial strategies, including techniques for improving social cognitive skills. Both of
these approaches have shown promise, but both have
important limitations. Notably, both conceptualize
social cognitive dysfunction as a deficit state despite
evidence that social cognitive biases play an important
role in this population (Rosse et al., 1994; Bentall
et al., 2001; Allen et al., 2004). Similarly, intervention
0165-1781/$ - see front matter 2008 Elsevier Ireland Ltd. All rights reserved.
doi:10.1016/j.psychres.2008.02.007
142
D.L. Roberts, D.L. Penn / Psychiatry Research 166 (2009) 141147
techniques are adapted from information processing
models that do not account for the qualitatively
different characteristics of social cognitive stimuli
(Penn et al., 1997) or brain functions (Frith and
Wolpert, 2003).
We developed a treatment model and intervention
package aimed at addressing these limitations. Social
cognition and interaction training (SCIT; Roberts
et al., 2006) is a 20-week, manualized group
intervention that targets dysfunctional social cognitive processes which have been observed in schizophrenia, including problems with emotion perception
and Theory of Mind (ToM), hasty judgment making,
and biased social attributions. The treatment comprises the following three phases: (1) Emotions,
which addresses emotion perception dysfunction;
(2) Figuring out situations, which addresses attributional biases and ToM dysfunction; and (3) Integration, in which participants practice applying
learned skills to interpersonal problems in their
own lives.
Preliminary studies suggest that SCIT is feasable, and
may improve social cognition and social functioning in
inpatient populations (Penn et al., 2005; Combs et al.,
2007a). The current study was a quasi-experimental trial
comparing SCIT plus treatment-as-usual (TAU) to TAU
among individuals with schizophrenia-spectrum disorders. Consistent with the inpatient findings, we
predicted that SCIT would be associated with improved
emotion perception, Theory of Mind, and social skill, as
well as reduced attributional bias, relative to the TAU
condition.
2. Methods
2.1. Participant recruitment and sample characteristics
Thirty-one adults with schizophrenia-spectrum
diagnoses and without current substance use problems were recruited from an outpatient psychiatry
clinic. All participants were receiving regular outpatient psychiatric treatment, including antipsychotic
medication, throughout the study. Participants were
assigned to the TAU group who either (1) declined
to participate in the SCIT group (n = 4), (2) were
unable to attend SCIT due to a scheduling conflict
(n = 1), or (3) had participated in previous research
with our laboratory, had agreed to be contacted for
future research participation, and met study criteria
(n = 6). Three SCIT treatment groups were conducted, each with 4 to 11 participants and two cofacilitators.
2.2. Measures
Diagnosis was obtained from participants' medical
charts, and confirmed with items from the psychotic
disorders section of the Structured Clinical Interview for
DSM-IV Patient Edition (SCID-P; First et al., 2001).
Symptomatology was assessed with the Positive and
Negative Syndrome Scale (PANSS) (Kay et al., 1987).
2.2.1. Social cognitive measures
Emotion perception was assessed with two measures:
The Face Emotion Identification Task (FEIT; Kerr and
Neale, 1993) and the Bell-Lysaker Emotion Recognition
Task (BLERT; Bell et al., 1997). Performance on the
FEIT is indexed as the total number of correctly
identified emotions out of nineteen pictured faces.
Reliability (Cronbach's alpha) for the FEIT was 0.51.
Although low, this is consistent with previous research
that has used this measure (Kerr and Neale, 1993;
Mueser et al., 1996; Penn et al., 2000). The BLERT
consists of 21 brief video scenes in which an actor utters
phrases using emotionally salient facial expressions and
vocal prosody. Performance is indexed as the total
number of correctly identified emotions (021). Reliability (Cronbach's alpha) of the BLERT was 0.77.
Theory of Mind was also assessed with two
measures. The Hinting task (Corcoran et al., 1995)
consists of ten brief, written vignettes including social
hints that the respondent must interpret. Total scores
range from 0 to 20, with higher scores indicating better
performance. Reliability (Cronbach's alpha) for the
Hinting task was 0.65. The Awareness of Social
Inference Test (TASIT; McDonald et al., 2003) was
abbreviated due to time constraints (from 16 to 10
items). The abbreviated TASIT requires participants to
view and answer four Yes/No questions about each of
ten brief video-taped social vignettes depicting examples of sarcasm and white lies." Performance is indexed
as the total number of correct responses, ranging from 0
to 40. Reliability (Cronbach's alpha) for the abbreviated
TASIT was 0.81.
Attributional style was measured with the Ambiguous Intentions Hostility Questionnaire-Ambiguous
items (AIHQ-A; Combs et al., 2007b). The AIHQ-A
comprises five short, written, second-person vignettes
describing negative interpersonal events with ambiguous causality. Each of the five vignettes is followed by
a Hostility question (e.g. Why did the other person do
what s/he did?), an Aggression question (e.g. How
would you respond?), and a Blame question (e.g. How
much would you blame the person?). Scores on each
range from 0 to 5; higher scores indicate greater bias.
D.L. Roberts, D.L. Penn / Psychiatry Research 166 (2009) 141147
Hostility and Aggression scores are derived from
response ratings made by two independent, blinded
coders, while Blame scores are derived from subject
responses on Likert-type (0 to 5) scales. Agreement
between raters (Intraclass Correlation Coefficient, ICC)
was 0.85. The reliability (Cronbach's alpha) of the
Likert-rated Blame scores was 0.92.
2.2.2. Social skill
The Social Skills Performance Assessment (SSPA;
Patterson et al., 2001) consists of two 3-min role-play
conversations with a confederate on pre-determined
topics (e.g. Your landlord has not fixed a leak that you
told him about last week, and now you are calling him
on the phone to follow-up.). SSPA performance was
tape-recorded and scored by two coders, trained to
reliability (ICC N 0.70), and blind to treatment condition
and pre/post status. Ratings were made of the following
domains: interest/disinterest, speech fluency, clarity,
focus, affect, social appropriateness, submissivenessversus-persistence, negotiation ability, and overall
conversational effectiveness. Domains were summed
to yield a total score. Ratings from two scenes were
collapsed into an overall composite social skill scale
(overall ICC = 0.79), with a range from 16 to 80, with
higher scores signifying greater skill.
The BLERT, TASIT, and SSPA were added to the
study protocol after completion of the first cohort, and
therefore were considered secondary outcome variables.
All assessments were conducted by trained assessors
who were not blind to treatment condition or pre/post
status.
2.3. Treatment conditions
Treatment as usual (TAU) comprised a suite of
available services, including medication management, individual and group psychotherapy, case
management, family education and support, and
occupational therapy. Use of TAU services differed
across participants based on collaborative planning
between clients and their clinicians. This was not
influenced by study procedures. No TAU participants received social-cognitively oriented treatment
during the study period; several received individual,
symptom-focused cognitive-behavioral treatment as
part of TAU.
All SCIT sessions followed a similar format,
beginning with structured check-ins in which participants made increasingly fine-grained observations about
their current emotional state and its relationship to their
behavior, thoughts, and social interactions. Next, home-
143
work was reviewed to bridge content from the previous
week to the current session. Early sessions in Phases 1
and 2 focused on psychoeducation and discussion of
social cognitive principles. The bulk of most core
sessions was spent learning specific social cognitive
strategies, and then utilizing these strategies to analyze
social cognitive stimuli (photographs, specialized
videos, or incidents from group members' lives).
Strategy practice was structured in the form of games
(including feedback about right and wrong answers) or
as collaborative data-gathering exercises or problemsolving sessions. All sessions ended with assignment of
homework.
3. Results
3.1. Data sample
All 31 study participants completed baseline and
post-test assessments. Study hypotheses were evaluated
using two experimental samples: the full intent-to-treat
(ITT) sample and a Completer sample (n = 14 or 70%
of the full SCIT group sample); completion was defined
as attendance to at least 50% of the therapy sessions
with at least two sessions in each of SCIT's three phases.
We required attendance at sessions in all three phases
because the skills taught in SCIT are cumulative, with
higher-level skills and real-world application not being
addressed until the second half of the intervention. Of
the six non-completers, three dropped out during phase
1, and three attended inconsistently throughout the
treatment. The attendance rates for the ITT and
Completer samples were 64% and 82%, respectively.
Chi-square and t-tests revealed that the full and
completer samples did not differ significantly on any
demographic or baseline clinical measures.
3.2. Demographic and baseline clinical analyses
Table 1 summarizes the characteristics of the SCIT
and TAU groups. SCIT participants were significantly
more symptomatic and were more likely to be diagnosed with schizoaffective disorder. However these
differences were unrelated to social cognitive outcome
variables, and therefore were not entered in the primary
analyses. Comparisons revealed no baseline differences
on any of the social cognitive or social skill measures.
At baseline, the PANSS total symptoms score was
significantly correlated with social skill performance
(r = 0.678, P = 0.003). Therefore, symptom change was
entered as a covariate in analyses of the social skill
data only.
144
D.L. Roberts, D.L. Penn / Psychiatry Research 166 (2009) 141147
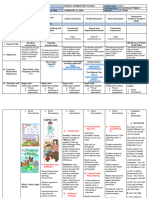
Table 1
Demographic and clinical information.
SCIT + TAU
(n = 20)
Age
Female (%)
Ethnicity (%)
African Am.
Caucasian
Other
Diagnosis (%)
Schizophrenia
Schizoaffective
Yrs education
WRAT Reading
Living status (%)
Independent
Family home
MH supported
Group home
PANSS symptoms
Positive
Negative
General
TAU (n = 11)
Mean/%
S.D.
Mean/%
S.D.
36.8
45.0
12.3
41.4
36.0
12.3
25.0
75.0
0.0
18.2
72.7
9.1
35.0
65.0
13.9
44.4
3.6
8.3
81.8
18.2
14.0
47.7
1.8
6.0
11.7
4.5
5.9
7.2
54.5
9.1
18.2
18.2
51.3
13.1
11.6
26.5
10.0
3.1
4.7
5.6
35.0
15.0
30.0
20.0
67.9
16.3
17.7
34.0
MH supported = Apartment with functional supports from a mental
health provider.
Diagnosis: 2 = 6.23; P = 0.013.
Symptoms: t = 3.97; P b 0.001; NB: All PANSS subscales also
P b 0.05.
3.3. Treatment findings1
In the Completer sample, the effect of SCIT on social
cognition was examined with an omnibus 2 (time: pretest versus post-test) 2 (group: TAU versus SCIT +
TAU) mixed model multivariate analysis of variance
(MANOVA) conducted on the primary social cognitive
measures (FEIT, AIHQ hostility bias, and Hinting task).
The time group interaction was statistically significant
(Wilk's = 0.592, F = 4.82, P = 0.010). To probe this
interaction, follow-up 2 (time) 2 (group) ANOVAs
were conducted on each of the three dependent
variables, and the two additional AIHQ variables
(summarized in Table 2). For the FEIT (emotion
perception task), neither of the main effects for time
1
The FEIT and Hinting task variable distributions were found to
violate parametric statistics assumptions of normality. Therefore, the
statistical tests in this section were replicated using non-parametric
MannWhitney and Wilcoxon change-score tests. Non-parametric
findings mirrored parametric results to an acceptable degree for both
the FEIT (MannWhitney U = 24.00; Wilcoxon W = 90.00; P = 0.003)
and the Hinting task (MannWhitney U = 74.50; Wilcoxon
W = 140.50; P = 0.887). Thus, it was determined that assumption
violations did not distort findings on these measures.
nor treatment group was statistically significant. However, there was a significant time group interaction
(F = 13.27, P = 0.001); SCIT + TAU completers
improved significantly from pre- to post-test (F = 9.52,
P = 0.009), whereas TAU participants' performance
declined at a trend level of statistical significance
(F = 4.57, P = 0.06). The improved performance in the
SCIT + TAU group corresponded to a medium withingroup effect size.2
Neither the main effects nor the interactions for the
Hinting (ToM) or AIHQ (attributional) tasks were
statistically significant.
Results from a series of 2 2 ANOVAs on the
secondary outcome variables are summarized in the
lower portion of Table 2. On the BLERT (emotion
perception task), neither of the main effects for time nor
group was statistically significant. However, the time
group interaction approached a trend level of statistical
significance (F = 3.27, P = 0.092). Probing revealed that
participants who received SCIT + TAU had a trend toward
higher performance on the BLERT at post-test relative to
participants in the TAU group (t = 1.69, P = 0.11).
On the TASIT (ToM task), the time group
interaction approached statistical significance (F =2.58,
P = 0.128). Probing of this interaction revealed trendlevel improvement in the SCIT + TAU group (F = 4.24,
P = 0.070), and no improvement in the TAU group. The
SCIT + TAU group's improvement corresponded to a
moderate effect size.
A 2 (time) 2 (group) analysis of covariance
(ANCOVA) was conducted on the SSPA (social skill
test) with PANSS symptom change score ([pre-test
PANSS total post-test PANSS total]/ pre-test PANSS
total) entered as a covariate. This yielded a statistically
significant time group interaction (F = 6.49, P =
0.024). Follow-up analyses revealed that participants
who received SCIT + TAU improved significantly in
social skill from pre- to post-test (F = 30.13, P = 0.001)
whereas individuals who received TAU did not. The
SCIT + TAU group's improvement corresponded to a
large effect size.
Results from the ITT sample were similar to
Completer results, although slightly attenuated.
Among primary variables, the FEIT yielded a significant
time group interaction (F = 7.04, P = 0.013), driven by
improvement from pre- to post-test in the SCIT group
2
Within-group effect sizes were calculated to estimate the
magnitude of change from pre- to post-test within the treatment
condition. Cohen's d (Cohen, 1988) was calculated using Dunlap
et al.'s (1996) conservative calculation, which corrects for effect size
inflation due to within-variable correlation in paired samples.
D.L. Roberts, D.L. Penn / Psychiatry Research 166 (2009) 141147
145
Table 2
Completer sample outcomes.
SCIT + TAU
FEIT
Hinting task
AIHQ Hostility
AIHQ Aggression
AIHQ Blame
BLERT
TASIT
SSPA
Pre-test M (S.D.)
Post-test M (S.D.)
12.21 (2.39)
16.14 (2.66)
1.97 (0.61)
1.79 (0.33)
2.90 (1.04)
15.57 (3.26)
26.30 (6.90)
55.33 (5.17)
13.57 (2.82)
15.92 (2.59)
2.11 (0.70)
1.89 (0.27)
2.93 (0.95)
16.50 (2.22)
29.50 (5.72)
62.61 (6.56)
14
14
14
14
14
10
10
9
Within
SCIT
effect
size
(d)
0.50
0.08
0.22
0.31
0.03
0.29
0.50
1.17
TAU
Pre-test M (S.D.)
Post-test M (S.D.)
13.73 (2.05)
15.45 (2.94)
1.70 (0.48)
1.95 (0.33)
2.50 (1.01)
14.12 (5.52)
27.38 (5.42)
58.64 (4.10)
12.54 (2.21)
15.27 (3.38)
1.51 (0.60)
1.98 (0.52)
2.26 (0.73)
13.00 (5.93)
27.50 (5.73)
59.00 (6.46)
Within
TAU
effect
size
(d)
11
11
11
11
11
7
8
7
0.55
0.06
0.35
0.05
0.22
0.19
0.02
0.06
SCIT = Social Cognition and Interaction Training; TAU = Treatment as usual; FEIT = Face Emotion Identification Task; AIHQ = Ambiguous
Intentions Hostility Questionnaire; BLERT = Bell & Lysaker Emotion Recognition Task; TASIT = The Awareness of Social Inference Test; SSPA =
Social Skill Performance Assessment.
Significant time group interaction (P = 0.001).
Significant time group interaction (P = 0.024).
that reached a trend level of statistical significance
(F = 3.00, P = 0.10). No other main effects or interactions
were found. Among secondary variables, the BLERT
yielded a time-by-group interaction that reached a trend
level of statistical significance (F = 3.91, P = 0.067), also
driven by pre- to post-test improvement in the SCIT
group (F = 3.37, P = 0.096). The SSPA yielded a time
group interaction that approached statistical significance
(F = 2.71, P = 0.121). This was driven by significant
improvement in the SCIT group (F = 11.86, P = 0.006)
which approached a large effect size (d = 0.79). TASIT
results were not statistically significant.
4. Discussion
This study provides preliminary evidence that SCIT
is feasible among outpatients, and may yield improvements in social cognition and social skill. Specific
findings are discussed below.
Individuals who received SCIT + TAU showed
significant improvement in emotion perception relative
to TAU. This finding generally replicates the recent
inpatient study of SCIT (Combs et al., 2007a) and is
consistent with previous research demonstrating that it
is possible to modify performance in this domain among
outpatients (reviewed in Couture et al., 2006). SCIT
differs from previous, targeted interventions, however, in that it addresses emotion perception as the first
of three treatment phases (instead of as a stand-alone
treatment). Therefore, post-treatment assessment does
not occur until approximately four months after
completion of targeted emotion perception training.
Thus, the positive results in the current study suggest
that emotion training effects in SCIT may be fairly
durable. Alternatively, participants may have utilized
the second and third phases of SCIT to rehearse and
consolidate emotion perception gains, as these skills
remain applicable in the exercises conducted during
these latter phases.
The impact of SCIT on ToM varied across outcome
measures. SCIT was not associated with improvement
on the primary ToM measure, the Hinting task. This is a
notable deviation from previous research with inpatient
samples, which showed large improvement on this
measure following SCIT (Penn et al., 2005; Combs
et al., 2007a). Examination of frequency distributions on
this measure revealed that most (57%) SCIT treatment
completers performed in the normative range at pre-test
(i.e. 17 or above, out of 20; Corcoran et al., 1995;
Pinkham and Penn, 2006). Thus, the limited impact of
SCIT on Hinting task performance may be due to a
ceiling effect. In contrast, SCIT was associated with
improvements in ToM that approached a trend level on
the TASIT. These results are consistent with previous
research showing that social cognitive training programs
can improve ToM among individuals with schizophrenia (Roncone et al., 2004). It is also encouraging in that
SCIT does not specifically target the ability to identify
white lies and sarcasm, abilities assessed by the TASIT.
Thus, SCIT may have promise in improving realworld ToM, although this conclusion is tempered by
the small sample in this analysis.
SCIT did not reduce hostile and aggressive attributional biases, a finding which differs from our previous
work with inpatients (Combs et al., 2007a). Examination of descriptive data revealed that means at both pre-
146
D.L. Roberts, D.L. Penn / Psychiatry Research 166 (2009) 141147
and post-test for all participants on all three attribution
scales were lower than means produced by a normative
sample of college students (Combs et al., 2007b). In the
face of negative interpersonal events, participants
reported inferring very low hostile intent, feeling very
low aggressive response tendency, and having a very
low tendency to blame others. This suggests a floor
effect such that SCIT participants had little room for
treatment-related improvement. Several factors may
explain this floor effect. Participants may have faked
good, which is possible because the AIHQ is face valid.
Alternatively, participants may actually have low bias,
which is consistent with the low observed levels of
paranoia in this sample.
The results showed that SCIT was associated with
improvements in social skill. This finding is quite
encouraging given that the primary goal of SCIT is to
improve social functioning by way of improved social
cognition. This provides preliminary support both for
the theoretical model underlying SCIT and for SCIT's
ability to generalize from cognition to social behavior.
Not surprisingly, SCIT-related effects were attenuated in the ITT sample relative to the Completer
sample, suggesting a doseresponse effect. To probe
this effect, post-hoc bivariate correlations were computed between attendance and change scores on
outcome variables in the full ITT sample. All correlations were non-significant, suggesting that more
research is needed to elucidate the relationship between
the dose of SCIT treatment components and social
cognitive change.
The current project had several methodological
limitations. First, although the raters of social cognitive
bias and social skill measures were blind to treatment
condition and pre/post status, the assessors were not.
This is an important limitation, as Tarrier and Wykes
(2004) have identified non-blinded assessment as a key
source of treatment-effect inflation among studies of
CBT for psychosis. Second, the use of a quasiexperimental design prevents full confidence in attributing the observed effects solely to SCIT. Third, small
sample size limited power to detect all but moderate and
large effect sizes, especially in the secondary variables.
And last, floor and ceiling effects on two assessment
measures may have prevented sensitive evaluation of
change. These limitations are being addressed in a
randomized, controlled trial that is currently underway.
In closing, this study provides preliminary evidence
that SCIT is a feasible and promising method for
improving social cognition and social skill among
outpatients, although more controlled research is needed
before the efficacy of SCIT is established.
Acknowledgments
This work was supported by a grant from the
Foundation of Hope for Research and Treatment of
Mental Illness. The authors thank Dr. Piper Meyer,
Sarah Uzenoff, and David Johnson for their help in this
research.
References
Allen, P.P., Johns, L.C., Fu, C.H.Y., Broome, M.R., Vythelingum, G.N.,
McGuire, P.K., 2004. Misattribution of external speech in patients
with hallucinations and delusions. Schizophrenia Research 69,
277287.
Bell, M., Bryson, G., Lysaker, P., 1997. Positive and negative affect
recognition in schizophrenia: a comparison with substance abuse
and normal control subjects. Psychiatry Research 73 (12), 7382.
Bentall, R.P., Corcoran, R., Howard, R., Blackwood, N., Kinderman,
P., 2001. Persecutory delusions: a review and theoretical interpretation. Clinical Psychological Review 21, 11431192.
Brne, M., Abdel-Hamid, M., Lehmkamper, C., Sonntag, C., 2007.
Mental state attribution, neurocognitive functioning, and psychopathology: what predicts poor social competence in schizophrenia
best? Schizophrenia Research 92, 151159.
Cohen, J., 1988. Statistical Power Analysis for the Behavioral
Sciences. Lawrence Erlbaum, Hillsdale, NJ.
Combs, D.R., Adams, S.D., Penn, D.L., Roberts, D.L., Tiegreen, J.,
Stem, P., 2007a. Social Cognition and Interaction Training (SCIT)
for inpatients with schizophrenia spectrum disorders: preliminary
findings. Schizophrenia Research 91, 112116.
Combs, D.R., Penn, D.L., Wicher, M., Waldheter, E., 2007b. The
Ambiguous Intentions Hostility Questionnaire (AIHQ): a new
measure for evaluating attributional biases in paranoia. Cognitive
Neuropsychiatry 12, 128143.
Corcoran, R., Mercer, G., Frith, C., 1995. Schizophrenia, symptomatology and social inference: investigating theory of mind in
people with schizophrenia. Schizophrenia Research 17, 513.
Couture, S., Penn, D.L., Roberts, D.L., 2006. The functional
significance of social cognition in schizophrenia: a review.
Schizophrenia Bulletin Suppl. 1, S-44S-63.
Dunlap, W.P., Cortina, J.M., Vaslow, J.B., Burke, M.J., 1996. Metaanalysis of experiments with matched groups or repeated measures
designs. Psychological Methods 1, 170177.
First, M.B., Spitzer, R.L., Gibbon, M., Williams, J.B.W., 2001.
Structured Clinical Interview for DSM-IVAxis I Disorders, Patient
Edition. Biometrics Research Department, New York State
Psychiatric Institute, New York.
Frith, C., Wolpert, D.M., 2003. The Neuroscience of Social
Interaction: Decoding, Imitating and Influencing the Actions of
Others. Oxford University Press, New York.
Hogarty, G.E., Flesher, S., Urlich, R., Carter, M., Greenwald, D., PogueGeile, M., Kechavan, M., Cooley, S., DiBarry, A.L., Garrett, A.,
Parepally, H., Zoretich, R., 2004. Cognitive enhancement therapy in
schizophrenia. Archives of General Psychiatry 61, 866876.
Kay, S., Fiszbein, A., Opler, L., 1987. The Positive and Negative
Syndrome Scale (PANSS) for schizophrenia. Schizophrenia
Bulletin 13, 261274.
Kerr, S.L., Neale, J.M., 1993. Emotion perception in schizophrenia:
specific deficit or further evidence of generalized poor performance? Journal of Abnormal Psychology 102, 312318.
D.L. Roberts, D.L. Penn / Psychiatry Research 166 (2009) 141147
McDonald, S., Flanagan, S., Rollins, J., Kinch, J., 2003. TASIT: a new
clinical tool for assessing social perception after traumatic brain
injury. Journal of Head Trauma Rehabilitation 18, 219238.
Mueser, K.T., Doonan, R., Penn, D.L., Blanchard, J.J., Bellack, A.S.,
Nishith, P., 1996. Emotion recognition and social competence in
chronic schizophrenia. Journal of Abnormal Psychology 105,
271275.
Patterson, T.L., Moscona, S., McKibbin, C.L., Davidson, K., Jeste, D.V.,
2001. Social skills performance assessment among older patients
with schizophrenia. Schizophrenia Research 48, 351360.
Penn, D.L., Corrigan, P.W., Bentall, R., Racenstein, J.M., Newman, L.,
1997. Social cognition in schizophrenia. Psychological Bulletin
121, 114132.
Penn, D.L., Combs, D.R., Ritchie, M., Francis, J., Cassissi, J., Morris,
S., Townsend, M., 2000. Emotion recognition in schizophrenia:
further investigation of generalized versus specific deficit models.
Journal of Abnormal Psychology 109, 512516.
Penn, D.L., Roberts, D., Munt, E.D., Silverstein, E., Jones, N.,
Sheitman, B., 2005. A pilot study of Social Cognition and
Interaction Training (SCIT) for schizophrenia. Schizophrenia
Research 80, 357359.
Penn, D.L., Addington, J., Pinkham, A., 2006. Social cognitive
impairments. In: Lieberman, J.A., Stroup, T.S., Perkins, D.O.
147
(Eds.), American Psychiatric Association Textbook of Schizophrenia. American Psychiatric Publishing Press, Arlington, VA,
pp. 261274.
Pinkham, A.E., Penn, D.L., 2006. Neurocognitive and social cognitive
predictors of social skill in schizophrenia. Psychiatry Research
143, 167178.
Roberts, D. L., Penn, D. L., Combs, D., 2006. Social Cognition and
Interaction Training. Unpublished treatment manual, University of
North Carolina, Chapel Hill, NC.
Roncone, R., Mazza, M., Frangou, I., DeRisio, A., Ussorio, D.,
Tozzini, C., Casacchia, M., 2004. Rehabilitation of theory of mind
deficit in schizophrenia: a pilot study of metacognitive strategies.
Neuropsychological Rehabilitation 14, 421435.
Rosse, R.B., Kendrick, K., Wyatt, R.J., Isaac, A., Deutsch, S.I., 1994.
Gaze discrimination in patients with schizophrenia: preliminary
report. American Journal of Psychiatry 151, 919921.
Silver, H., Goodman, C., Knoll, G., Isakov, V., 2004. Brief emotion
training improves recognition of facial emotions in chronic
schizophrenia: a pilot study. Psychiatry Research 128, 147154.
Tarrier, N., Wykes, T., 2004. Is there evidence that cognitive behaviour
therapy is an effective treatmetn for schizophrenia? A cautious or
cautionary tale? Behaviour Research and Therapy 42, 13771401.
Vous aimerez peut-être aussi
- Guide to Psychological Assessment with HispanicsD'EverandGuide to Psychological Assessment with HispanicsLorraine T. BenutoPas encore d'évaluation
- Social Perception in Schizophrenia - The Role of ContextDocument11 pagesSocial Perception in Schizophrenia - The Role of ContextFlávia AndradePas encore d'évaluation
- ED602396Document34 pagesED602396Mekhla PandeyPas encore d'évaluation
- Ansiedad Cognitivo ConductualDocument6 pagesAnsiedad Cognitivo ConductualCarlos ContrerasPas encore d'évaluation
- Social Perception in Schizophrenia - The Role of ContextDocument11 pagesSocial Perception in Schizophrenia - The Role of ContextDaniela SalazarPas encore d'évaluation
- Morgan 2011Document6 pagesMorgan 2011TabindaLodhiPas encore d'évaluation
- Vaskin 2009Document3 pagesVaskin 2009RosarioBengocheaSecoPas encore d'évaluation
- Psychiatry ResearchDocument7 pagesPsychiatry ResearchLetyAlarcónPas encore d'évaluation
- Emotional Intelligence and Personality in Major Depression: Trait Versus State EffectsDocument6 pagesEmotional Intelligence and Personality in Major Depression: Trait Versus State EffectsLaura AlfaroPas encore d'évaluation
- A Case Study of Person With Depression: A Cognitive Behavioural Case Work ApproachDocument11 pagesA Case Study of Person With Depression: A Cognitive Behavioural Case Work Approachmitesh vermaPas encore d'évaluation
- NIH Public Access: Author ManuscriptDocument20 pagesNIH Public Access: Author ManuscriptRamona FodorPas encore d'évaluation
- Promoting Homework Adherence in Cognitive-Behavioral Therapy For Adolescent DepressionDocument10 pagesPromoting Homework Adherence in Cognitive-Behavioral Therapy For Adolescent DepressionKevin CaperaPas encore d'évaluation
- Anderson 2014Document16 pagesAnderson 2014Bárbara FernandesPas encore d'évaluation
- Bell 2010Document8 pagesBell 2010RosarioBengocheaSecoPas encore d'évaluation
- Trauma-Focused Cognitive-Behavioral Therapy For CHDocument13 pagesTrauma-Focused Cognitive-Behavioral Therapy For CHLuis BernardoPas encore d'évaluation
- Bora2009 Theory of Mind Impairment in Schizophrenia Meta-AnalysisDocument9 pagesBora2009 Theory of Mind Impairment in Schizophrenia Meta-AnalysisPaula TerPas encore d'évaluation
- 50 Years of RationalDocument15 pages50 Years of RationalLynda HernandezPas encore d'évaluation
- The Moral Injury and Distress Scale: Psychometric Evaluation and Initial Validation in Three High-Risk PopulationsDocument12 pagesThe Moral Injury and Distress Scale: Psychometric Evaluation and Initial Validation in Three High-Risk PopulationsJonathan MacFarlanePas encore d'évaluation
- Comparison of MMPI - 2 Measures of PsychopathicDocument7 pagesComparison of MMPI - 2 Measures of PsychopathicMaría SanchezPas encore d'évaluation
- NIH Public AccessDocument31 pagesNIH Public AccessLuciana MarinPas encore d'évaluation
- Depression and Social Anxiety in ChildrenDocument15 pagesDepression and Social Anxiety in ChildrenMichaela CoravuPas encore d'évaluation
- 1 S2.0S0165178111008079 Main - 2Document1 page1 S2.0S0165178111008079 Main - 2George MartinezPas encore d'évaluation
- Journal of Behavior Therapy and Experimental Psychiatry: Kristine Kahr NilssonDocument5 pagesJournal of Behavior Therapy and Experimental Psychiatry: Kristine Kahr NilssonlucianaeuPas encore d'évaluation
- 2007 CESItem Level PsychometricsDocument15 pages2007 CESItem Level PsychometricsCamila Andrea Barrera BlancoPas encore d'évaluation
- Social Cognition in Schizophrenia, Part 2: 12-Month Stability and Prediction of Functional Outcome in First-Episode PatientsDocument8 pagesSocial Cognition in Schizophrenia, Part 2: 12-Month Stability and Prediction of Functional Outcome in First-Episode PatientsRosarioBengocheaSecoPas encore d'évaluation
- Journal of Contextual Behavioral Science: Marge A. Sierra, Eliana OrtizDocument12 pagesJournal of Contextual Behavioral Science: Marge A. Sierra, Eliana OrtizEliana Ortiz GarzonPas encore d'évaluation
- Subcomponents of Psychopathy Have Opposing Correlations With Punishment JudgmentsDocument22 pagesSubcomponents of Psychopathy Have Opposing Correlations With Punishment JudgmentsnimadupaPas encore d'évaluation
- The Liebowitz Social Anxiety Scale: A Comparison of The Psychometric Properties of Self-Report and Clinician-Administered FormatsDocument11 pagesThe Liebowitz Social Anxiety Scale: A Comparison of The Psychometric Properties of Self-Report and Clinician-Administered FormatsAndreea OniceanuPas encore d'évaluation
- This Content Downloaded From 111.68.96.36 On Thu, 22 Oct 2020 05:33:31 UTCDocument6 pagesThis Content Downloaded From 111.68.96.36 On Thu, 22 Oct 2020 05:33:31 UTCMuhammad MaazPas encore d'évaluation
- Ciarrochi Scott PID Relations Between Social Emotional Competence Mental Health 2003 PDFDocument17 pagesCiarrochi Scott PID Relations Between Social Emotional Competence Mental Health 2003 PDF5l7n5Pas encore d'évaluation
- Effect of Psychosocial Interventions On Social Functioning in Depression and Schizophrenia: Meta-AnalysisDocument37 pagesEffect of Psychosocial Interventions On Social Functioning in Depression and Schizophrenia: Meta-AnalysiswardahPas encore d'évaluation
- Research Article: Social Anxiety, Tremor Severity, and Tremor Disability: A Search For Clinically Relevant MeasuresDocument7 pagesResearch Article: Social Anxiety, Tremor Severity, and Tremor Disability: A Search For Clinically Relevant MeasuresazzzzzzzzzzzacPas encore d'évaluation
- MascDocument14 pagesMascIsaac EliasPas encore d'évaluation
- A Pilot Study of Emotion Regulation Therapy For GeneralizedDocument16 pagesA Pilot Study of Emotion Regulation Therapy For GeneralizedMaria GabrielaPas encore d'évaluation
- Practical 2 UdpdDocument11 pagesPractical 2 Udpdidonttttknowww1234567890Pas encore d'évaluation
- Social Skill InterventionDocument11 pagesSocial Skill Interventionsyariah hairudinPas encore d'évaluation
- Thibaudeau Achim 2018 PRDocument7 pagesThibaudeau Achim 2018 PRrichard LemieuxPas encore d'évaluation
- Transference Focused Psychotherapy For Borderline Personality Disorder Change in Reflective FunctionDocument2 pagesTransference Focused Psychotherapy For Borderline Personality Disorder Change in Reflective FunctionDaniela Saralegui FPas encore d'évaluation
- 2012 - Patients With Bipolar Disorder Show Impaired Performance On Complex Tests of Social CognitionDocument7 pages2012 - Patients With Bipolar Disorder Show Impaired Performance On Complex Tests of Social CognitionRaúl VerdugoPas encore d'évaluation
- J Jcbs 2019 02 005Document36 pagesJ Jcbs 2019 02 005kenth yuPas encore d'évaluation
- Children and Youth Services Review: Nilüfer Özabac IDocument5 pagesChildren and Youth Services Review: Nilüfer Özabac IFrancisco Matías Ponce MirandaPas encore d'évaluation
- Rorschach Revised DEPI and CDI With Inpatient Major Depressives and Borderline Personality Disorder With Major Depression: Validity IssuesDocument8 pagesRorschach Revised DEPI and CDI With Inpatient Major Depressives and Borderline Personality Disorder With Major Depression: Validity IssuesMichelle SchultzPas encore d'évaluation
- Radloff 1977Document17 pagesRadloff 1977Fitrisia AgustinaPas encore d'évaluation
- Jurnal BipolarDocument8 pagesJurnal BipolarArif NurohmanPas encore d'évaluation
- Dissociation of Cognitive and Emotional Empathy in Adults With Asperger Syndrome Using The Multifaceted Empathy Test (MET)Document10 pagesDissociation of Cognitive and Emotional Empathy in Adults With Asperger Syndrome Using The Multifaceted Empathy Test (MET)pipejaramilloPas encore d'évaluation
- Validity of The Sluggish Cognitive Tempo, Inattention, and Hyperactivity Symptom Dimensions: Neuropsychological and Psychosocial CorrelatesDocument15 pagesValidity of The Sluggish Cognitive Tempo, Inattention, and Hyperactivity Symptom Dimensions: Neuropsychological and Psychosocial Correlatescinfer75Pas encore d'évaluation
- A Synopsis of Rational-Emotive Behavior Therapy (Rebt), David, Szentagotai, Kallay, MacaveiDocument47 pagesA Synopsis of Rational-Emotive Behavior Therapy (Rebt), David, Szentagotai, Kallay, MacaveiRildoPas encore d'évaluation
- Organizacion de Las Estrategias de Afrontaiento Segun Centradas en La Emocion, Problema y DisfuncionalesDocument6 pagesOrganizacion de Las Estrategias de Afrontaiento Segun Centradas en La Emocion, Problema y DisfuncionalesRuddy marcella Sanchez GuarnizoPas encore d'évaluation
- Thompson Et Al. (2021) - Internet-Based Acceptance and Commitment TherapyDocument16 pagesThompson Et Al. (2021) - Internet-Based Acceptance and Commitment TherapyDaniel Garvi de Castro100% (1)
- Cusi 2010Document5 pagesCusi 2010Πέγκυ ΠρεσβέλουPas encore d'évaluation
- Seidel 2012 - Patients - RelativesDocument7 pagesSeidel 2012 - Patients - RelativesΠέγκυ ΠρεσβέλουPas encore d'évaluation
- (2007) - A Psychometric Investigation of Two Self-Report Measures of Emotional ExpressivityDocument10 pages(2007) - A Psychometric Investigation of Two Self-Report Measures of Emotional ExpressivityBruno SallesPas encore d'évaluation
- Dbasse 170048Document71 pagesDbasse 170048Esha ShafiqPas encore d'évaluation
- Collins 2005Document15 pagesCollins 2005selamet apriyantoPas encore d'évaluation
- CBT EssayDocument16 pagesCBT EssayCristín Ní LiatháinPas encore d'évaluation
- Achim 2012 PR (MTZ-FEP)Document7 pagesAchim 2012 PR (MTZ-FEP)richard LemieuxPas encore d'évaluation
- Exploring Risk Factors For Depression Among Older Men Residing in MacauDocument11 pagesExploring Risk Factors For Depression Among Older Men Residing in MacauaryaPas encore d'évaluation
- Assessing Emotion Regulation in Social Anxiety DisDocument10 pagesAssessing Emotion Regulation in Social Anxiety DisalejandroPas encore d'évaluation
- Distinct Neuronal Patterns of Positive and Negative MoralDocument24 pagesDistinct Neuronal Patterns of Positive and Negative MoralFabián Eraso MuñozPas encore d'évaluation
- Exploring Hubris in Physicians (1) - 221202 - 211145Document4 pagesExploring Hubris in Physicians (1) - 221202 - 211145Mustafa AkviranlıPas encore d'évaluation
- Working With The Suicidal PatientDocument4 pagesWorking With The Suicidal PatientRosarioBengocheaSeco100% (1)
- Coat of ArmsDocument1 pageCoat of ArmsRosarioBengocheaSecoPas encore d'évaluation
- Suicide in SchizophreniaDocument12 pagesSuicide in SchizophreniaRosarioBengocheaSecoPas encore d'évaluation
- Hor. Suicide and SchizophreniaDocument11 pagesHor. Suicide and SchizophreniaRosarioBengocheaSecoPas encore d'évaluation
- Assesing RecoveryDocument6 pagesAssesing RecoveryRosarioBengocheaSecoPas encore d'évaluation
- Mosolov. Remission in Schizophrenia 6 MesesDocument26 pagesMosolov. Remission in Schizophrenia 6 MesesRosarioBengocheaSecoPas encore d'évaluation
- IPT, Vallina, Lemos, RoderDocument3 pagesIPT, Vallina, Lemos, RoderRosarioBengocheaSecoPas encore d'évaluation
- Maintenance Guide PDFDocument2 pagesMaintenance Guide PDFRosarioBengocheaSecoPas encore d'évaluation
- Coat of ArmsDocument1 pageCoat of ArmsRosarioBengocheaSecoPas encore d'évaluation
- Developing A Model of Recovery in Mental HealthDocument12 pagesDeveloping A Model of Recovery in Mental HealthRosarioBengocheaSecoPas encore d'évaluation
- A Structured Risk Approach To Risk Decision MakingDocument1 pageA Structured Risk Approach To Risk Decision MakingRosarioBengocheaSecoPas encore d'évaluation
- What Does Recovery Mean in PracticeDocument7 pagesWhat Does Recovery Mean in PracticeRosarioBengocheaSecoPas encore d'évaluation
- ConnectednessDocument13 pagesConnectednessRosarioBengocheaSeco100% (1)
- Person-Centred Strengths AssessmentDocument10 pagesPerson-Centred Strengths AssessmentRosarioBengocheaSecoPas encore d'évaluation
- Kelly. Exploring The Concept of Recovery in SchizophreniaDocument7 pagesKelly. Exploring The Concept of Recovery in SchizophreniaRosarioBengocheaSecoPas encore d'évaluation
- Davidson. Remission and Recovery in SchizophreniaDocument4 pagesDavidson. Remission and Recovery in SchizophreniaRosarioBengocheaSecoPas encore d'évaluation
- What Professionals Need To Know About FamiliesDocument3 pagesWhat Professionals Need To Know About FamiliesRosarioBengocheaSecoPas encore d'évaluation
- Early Warning SignsDocument1 pageEarly Warning SignsRosarioBengocheaSecoPas encore d'évaluation
- ConnectednessDocument13 pagesConnectednessRosarioBengocheaSeco100% (1)
- Activities For Assessing and Developing ReadinessDocument17 pagesActivities For Assessing and Developing ReadinessRosarioBengocheaSecoPas encore d'évaluation
- Eack 2009Document5 pagesEack 2009RosarioBengocheaSecoPas encore d'évaluation
- A Structured Risk Approach To Risk Decision MakingDocument1 pageA Structured Risk Approach To Risk Decision MakingRosarioBengocheaSecoPas encore d'évaluation
- Vaskin 2009Document3 pagesVaskin 2009RosarioBengocheaSecoPas encore d'évaluation
- Psychiatry Research: Philip Brittain, Dominic H. Ffytche, Allison Mckendrick, Simon SurguladzeDocument6 pagesPsychiatry Research: Philip Brittain, Dominic H. Ffytche, Allison Mckendrick, Simon SurguladzeRosarioBengocheaSecoPas encore d'évaluation
- Bell 2010Document8 pagesBell 2010RosarioBengocheaSecoPas encore d'évaluation
- Esquizos y Teoria de La Mente 1Document9 pagesEsquizos y Teoria de La Mente 1stromero100% (1)
- Social Perception and Social Skill in SchizophreniaDocument12 pagesSocial Perception and Social Skill in SchizophreniaRosarioBengocheaSecoPas encore d'évaluation
- Fett 2011Document16 pagesFett 2011Achmad Ageng SeloPas encore d'évaluation
- Ziv 2011Document2 pagesZiv 2011RosarioBengocheaSecoPas encore d'évaluation
- What Are The Main Differences Between The Orientation Design School and Planning School Guidance On Formalizing The StrategyDocument3 pagesWhat Are The Main Differences Between The Orientation Design School and Planning School Guidance On Formalizing The StrategykarimaelPas encore d'évaluation
- Leading Teams and Group DynamicsDocument13 pagesLeading Teams and Group DynamicsPanda BeruPas encore d'évaluation
- Week 3 DLL Catch Up Friday Grade 5Document8 pagesWeek 3 DLL Catch Up Friday Grade 5May JerezoPas encore d'évaluation
- Breakdowns in Intercultural Communication Create Serious Problems For Multicultural SocietiesDocument3 pagesBreakdowns in Intercultural Communication Create Serious Problems For Multicultural SocietiesMadhu AgarwalPas encore d'évaluation
- Do Younger Employees Really Have Less of A Work Ethic?Document14 pagesDo Younger Employees Really Have Less of A Work Ethic?Reginald VelanoPas encore d'évaluation
- Ivey's PptRead Only)Document34 pagesIvey's PptRead Only)MAHIMA DASPas encore d'évaluation
- HEM 53 Timetable 2012 Ver 3Document8 pagesHEM 53 Timetable 2012 Ver 3Chema SaizPas encore d'évaluation
- Characteristics InnovationDocument26 pagesCharacteristics InnovationTan 程惠萍Pas encore d'évaluation
- Trial and Error Learning PDFDocument3 pagesTrial and Error Learning PDFTanishqa RawlaniPas encore d'évaluation
- Pull Your Ex BackDocument93 pagesPull Your Ex BackDitend TeshPas encore d'évaluation
- Theories and ApproachesDocument13 pagesTheories and ApproachesPrince Rupee GonzalesPas encore d'évaluation
- Maslow: Holistic Dynamic TheoryDocument1 pageMaslow: Holistic Dynamic TheoryAnjanette DoradoPas encore d'évaluation
- Mental Health of GNMDocument133 pagesMental Health of GNMGuruKPO100% (9)
- ReflectionDocument4 pagesReflectionJuan Pablo Aidom NemidPas encore d'évaluation
- ALDRIDGE, NEUGEBAUER AND GUSTORFF - A Preliminary Study of Creative Music Therapy in The Treatment of Children With Developmental DelayDocument17 pagesALDRIDGE, NEUGEBAUER AND GUSTORFF - A Preliminary Study of Creative Music Therapy in The Treatment of Children With Developmental DelayCamila Rocha FerrariPas encore d'évaluation
- B.Ed SNDT Semester 1 - Course 1 Notes-1 PDFDocument66 pagesB.Ed SNDT Semester 1 - Course 1 Notes-1 PDFmini favourite song's rai100% (2)
- Rubric For ManifestoDocument3 pagesRubric For Manifestoapi-316144468Pas encore d'évaluation
- 5.2 - Information Processing: Assessment Statement Notes 5.2.1Document10 pages5.2 - Information Processing: Assessment Statement Notes 5.2.1Alamedin SabitPas encore d'évaluation
- PErsonal GrowthDocument4 pagesPErsonal GrowthNishantha FernandoPas encore d'évaluation
- Assignment 1. What Is Management?Document2 pagesAssignment 1. What Is Management?Jeffrey De BelenPas encore d'évaluation
- Adverse Effects of Gadgets On KidsDocument1 pageAdverse Effects of Gadgets On Kidsnicole bejasaPas encore d'évaluation
- Counseling For StudentsDocument9 pagesCounseling For StudentsMark Ruzzel MarañaPas encore d'évaluation
- Self PerceptionDocument6 pagesSelf PerceptionBhuvanaPas encore d'évaluation
- Character Formation With Leadership Decision MakingDocument13 pagesCharacter Formation With Leadership Decision MakingShaine Frugalidad II100% (4)
- Peplau's TheoryDocument25 pagesPeplau's Theoryshoba0880Pas encore d'évaluation
- Test Bank For Foundations of Addictions Counseling 4th Edition David Capuzzi Mark D StaufferDocument8 pagesTest Bank For Foundations of Addictions Counseling 4th Edition David Capuzzi Mark D Stauffermarisgemma0j3vPas encore d'évaluation
- I. Overview of Abnormal PsychologyDocument55 pagesI. Overview of Abnormal PsychologyTori YamaPas encore d'évaluation
- Kumpulan InstrumenDocument10 pagesKumpulan Instrumenreni50% (2)
- 214 ArticleText 1307 1 10 20200401Document8 pages214 ArticleText 1307 1 10 20200401ankitakomath0805Pas encore d'évaluation
- Week Class Topic / Theme Skill Focus Unit 1: Introduction To Study SkillsDocument1 pageWeek Class Topic / Theme Skill Focus Unit 1: Introduction To Study SkillsNguyễn Thế HảiPas encore d'évaluation
- The Age of Magical Overthinking: Notes on Modern IrrationalityD'EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityÉvaluation : 4 sur 5 étoiles4/5 (28)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionD'EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionÉvaluation : 4 sur 5 étoiles4/5 (404)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsD'EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsÉvaluation : 5 sur 5 étoiles5/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsD'EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsPas encore d'évaluation
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 5 sur 5 étoiles5/5 (81)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDD'EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDÉvaluation : 5 sur 5 étoiles5/5 (2)
- Why We Die: The New Science of Aging and the Quest for ImmortalityD'EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityÉvaluation : 4 sur 5 étoiles4/5 (3)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaD'EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeD'EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeÉvaluation : 2 sur 5 étoiles2/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsD'EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsÉvaluation : 3.5 sur 5 étoiles3.5/5 (3)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)D'EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Pas encore d'évaluation
- The Marshmallow Test: Mastering Self-ControlD'EverandThe Marshmallow Test: Mastering Self-ControlÉvaluation : 4.5 sur 5 étoiles4.5/5 (58)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsD'EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsÉvaluation : 4.5 sur 5 étoiles4.5/5 (170)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningD'EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningÉvaluation : 4 sur 5 étoiles4/5 (3)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisD'EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisÉvaluation : 3.5 sur 5 étoiles3.5/5 (2)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisD'EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisÉvaluation : 4 sur 5 étoiles4/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.D'EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Évaluation : 4.5 sur 5 étoiles4.5/5 (110)
- Self-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!D'EverandSelf-Care for Autistic People: 100+ Ways to Recharge, De-Stress, and Unmask!Évaluation : 5 sur 5 étoiles5/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessD'EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessÉvaluation : 4.5 sur 5 étoiles4.5/5 (328)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingD'EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingÉvaluation : 4 sur 5 étoiles4/5 (1138)
- The Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceD'EverandThe Molecule of More: How a Single Chemical in Your Brain Drives Love, Sex, and Creativity--and Will Determine the Fate of the Human RaceÉvaluation : 4.5 sur 5 étoiles4.5/5 (517)
- Summary: Hidden Potential: The Science of Achieving Greater Things By Adam Grant: Key Takeaways, Summary and AnalysisD'EverandSummary: Hidden Potential: The Science of Achieving Greater Things By Adam Grant: Key Takeaways, Summary and AnalysisÉvaluation : 4.5 sur 5 étoiles4.5/5 (15)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryD'EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryÉvaluation : 4 sur 5 étoiles4/5 (44)
- Troubled: A Memoir of Foster Care, Family, and Social ClassD'EverandTroubled: A Memoir of Foster Care, Family, and Social ClassÉvaluation : 4.5 sur 5 étoiles4.5/5 (27)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeD'EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeÉvaluation : 4.5 sur 5 étoiles4.5/5 (253)
- The Secret of the Golden Flower: A Chinese Book Of LifeD'EverandThe Secret of the Golden Flower: A Chinese Book Of LifeÉvaluation : 5 sur 5 étoiles5/5 (4)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedÉvaluation : 4 sur 5 étoiles4/5 (61)