Académique Documents
Professionnel Documents
Culture Documents
Williams 24th Ed Chap 40 Hypertension
Transféré par
Rem AlfelorCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Williams 24th Ed Chap 40 Hypertension
Transféré par
Rem AlfelorDroits d'auteur :
Formats disponibles
Williams 24th Ed Includes
CHAPTER 40: Hypertensive Disorders findings
such as
Complicate 5-10% of all pregnancies
One member of the deadly triad that contributes greatly to maternal morbidity
and mortality
Along with hemorrhage and infection
Preeclampsia Syndrome, either alone or superimposed on Chronic
Hypertension, is the most dangerous.
Gestational Hypertension
New-onset hypertension during pregnancy
headaches/epigastric pain, proteinuria, and thrombocytopenia.
Followed by signs and symptoms of preeclampsia almost half the time
Transient Hypertension
Preeclampsia is identified in 3.9% of all pregnancies
If evidence for preeclampsia does not develop and the blood pressure
WHO (2006): 16% of maternal deaths were reported to be due to hypertensive
returns to normal by 12 weeks postpartum.
disorders (Khan, 2006).
This proportion is greater than three other leading causes that include:
a) Hemorrhage (13%) Preeclampsia Syndrome
b) Abortion (8%) Pregnancy-specific syndrome that can affect virtually every organ system.
c) Sepsis (2% ) More than simply gestational hypertension with proteinuria, appearance of
proteinuria remains an important diagnostic criterion. Proteinuria is an objective
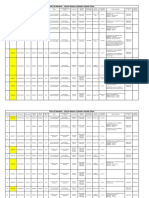
Diagnostic Criteria for Pregnancy-associated Hypertension (Table 40.1) marker and reflects the system-wide endothelial leak, which characterizes the
preeclampsia syndrome.
Abnormal Protein Excretion
24-hour urinary excretion exceeding 300 mg
Urine Protein: Creatinine Ratio 0.3
Persistent 30 mg/dL (1+ dipstick) protein in random urine samples
Determination of a spot Urine: Creatinine Ratio is a suitable replacement
for a 24- hour urine measurement
Evidence of multi-organ involvement may include:
Thrombocytopenia
Renal Dysfunction
Hepatocellular Necrosis (Liver Dysfunction)
Central Nervous System Perturbations
Pulmonary Edema
Indicators of Preeclampsia Severity
Default classification is either implied or specifically termed as
TERMINOLOGY AND DIAGNOSIS
a) MILD
ACOG (2013b): Four types of hypertensive disease: b) LESS SEVERE
1) Gestational Hypertension c) NONSEVERE
Evidence for the preeclampsia syndrome does not develop and
hypertension resolves by 12 weeks postpartum
2) Preeclampsia and Eclampsia Syndrome
3) Chronic Hypertension of any etiology
4) Preeclampsia Superimposed on Chronic Hypertension.
Diagnosis of Hypertensive Disorders
Hypertension is diagnosed empirically when appropriately taken blood pressure
140 mm Hg systolic or 90 mm Hg diastolic.
Korotkoff Phase V is used to define diastolic pressure.
Women who have a rise in pressure of 30 mm Hg systolic or 15 mm Hg diastolic
should be observed more closely because Eclamptic Seizures develop in some
of these women whose blood pressures have stayed < 140/90 mm Hg
Sudden rise in Mean Arterial Pressure later in pregnancy (Delta Hypertension)
may also signify Preeclampsia even if blood pressure is < 140/90 mm Hg
FIGURE 40-1 Schematic shows normal reference ranges for blood pressure changes across
pregnancy. Patient A (blue) has blood pressures near the 20th percentile throughout pregnancy.
Patient B (red) has a similar pattern with pressures at about the 25th percentile until about 36
weeks when blood pressure begins to increase. By term, it is substantively higher and in the 75th
percentile, but she is still considered Normotensive.
Gestational Hypertension
Women whose blood pressures reach 140/90 mm Hg for the first time after
midpregnancy, but in whom proteinuria is not identified
Almost half of these women subsequently develop Preeclampsia Syndrome
Rem Alfelor 2015
OBSTETRICS MODULE: Hypertension Page 1 of 12
Multiparas: Variable but is less than that for nulliparas.
Population studies from Australia, Canada, Denmark, Norway, Scotland,
Sweden, and Massachusetts: Incidence of 1.4 -4%
Figure 40.2 Other risk factors associated with preeclampsia:
a) Obesity
Headaches or visual disturbances such as scotomata can be premonitory The relationship between maternal weight and risk of preeclampsia
symptoms of eclampsia. is progressive.
Epigastric or right upper quadrant pain BMI < 20 kg/m2: 4.3%
Frequently accompanies hepatocellular necrosis, ischemia, and edema BMI > 35 kg/m2: 13.3%
that ostensibly stretches Glisson capsule. b) Multifetal Gestation
This characteristic pain is frequently accompanied by elevated Serum Gestational Hypertension: Twin gestation (13%), Singletons (6%)
Hepatic Transaminase levels. Preeclampsia: Twin gestation (13%), Singletons (5%)
Thrombocytopenia Incidence is unrelated to zygosity
Characteristic of worsening preeclampsia c) Maternal Age
Signifies platelet activation and aggregation as well as Microangiopathic d) Hyperhomocysteinemia
Hemolysis. e) Metabolic Syndrome
Other factors indicative of Severe Preeclampsia include: Although smoking during pregnancy has consistently been associated with a
Renal or cardiac involvement reduced risk for hypertension during pregnancy
Obvious fetal-growth restriction which also attests to its duration Smoking upregulates placental Adrenomedullin expression, which
The more profound these signs and symptoms, the less likely they can be regulates volume homeostasis.
temporized, and the more likely delivery will be required. Women with preeclampsia in the first pregnancy are at greater risk in a second
pregnancy compared with women normotensive during their first pregnancy
Woman who was normotensive during her first pregnancy, the incidence of
preeclampsia in a subsequent pregnancy is much lower than for a first
Eclampsia pregnancy
In a woman with preeclampsia, a convulsion that cannot be attributed to another
cause Eclampsia
Seizures are generalized Somewhat preventable by adequate prenatal care, the incidence has decreased
May appear before, during, or after labor over the years in areas where health care is more readily available.
Approximately, 10% do not develop seizures until after 48 hours postpartum In countries with adequate resources, incidence averages 1 in 2000 deliveries
Up to a fourth of Eclamptic Seizures develop beyond 48 hours postpartum
Parkland hospital: delayed postpartum eclampsia continues to occur in about ETIOPATHOGENESIS
10% of cases Gestational hypertensive disorders are more likely to develop in women with the
following characteristics:
Preeclampsia Superimposed on Chronic Hypertension Are exposed to chorionic villi for the first time
Are exposed to a superabundance of chorionic villi, as with twins or
Regardless of its cause, any chronic hypertensive disorder predisposes a
hydatidiform mole
woman to develop Superimposed Preeclampsia Syndrome.
Have preexisting conditions of endothelial cell activation or inflammation
Chronic Hypertension
such as diabetes or renal or cardiovascular disease
Women with documented blood pressures 140/90 mm Hg before
Are genetically predisposed to hypertension developing during pregnancy.
pregnancy or before 20 weeks gestation, or both.
A fetus is not a requisite for preeclampsia to develop.
Woman with previously undiagnosed chronic vascular disease who is seen
Although chorionic villi are essential, they need not be intrauterine
before 20 weeks frequently has blood pressures within the normal range.
Preeclampsia syndrome is characterized by abnormalities that result in vascular
Third trimester: As blood pressures return to their originally hypertensive levels,
endothelial damage with resultant vasospasm, transudation of plasma, and
it may be difficult to determine whether hypertension is chronic or induced by
ischemic and thrombotic sequelae.
pregnancy
At least two major subtypes differentiated by whether or not remodeling of
Women with chronic hypertension, their blood pressure increases to obviously
uterine spiral arterioles by endovascular trophoblastic invasion is defective.
abnormal levels typically after 24 weeks.
Two-stage disorder theory of preeclampsia etiopathogenesis.
Superimposed Preeclampsia
Two stage disorder includes maternal and placental preeclampsia.
If new-onset or worsening baseline hypertension is accompanied by new-
onset proteinuria or other findings listed in Table 40-1 Stage 1 is caused by faulty endovascular trophoblastic remodeling
Commonly develops earlier in pregnancy that downstream causes the stage 2 clinical syndrome
Tends to be more severe Stage 2 is susceptible to modification by preexisting maternal
Often is accompanied by fetal-growth restriction conditions that are manifest by endothelial cell activation or
inflammation.
Same criteria shown in Table 40-2 are also used to further characterize
Such conditions include cardiovascular or renal disease,
severity
diabetes, obesity, immunological disorders, or hereditary
influences.
INCIDENCE AND RISK FACTORS Etiology
Preeclampsia Syndrome Currently considered important include:
Preeclampsia: Young and nulliparous women 1. Placental implantation with abnormal trophoblastic invasion of uterine vessels
Chronic Hypertension with Superimposed Preeclampsia: Older women 2. Immunological maladaptive tolerance between maternal, paternal (placental),
Incidence is markedly influenced by race and ethnicity, thus genetic and fetal tissues
predisposition 3. Maternal maladaptation to cardiovascular or inflammatory changes of normal
Incidence of preeclampsia: White (5%), Hispanic (9%), and African-American pregnancy
(11%) 4. Genetic factors including inherited predisposing genes and epigenetic
Other factors include environmental, socioeconomic, and even seasonal influences.
influences
Incidence of Preeclampsia Abnormal Trophoblastic Invasion
Nulliparous: 3-10%
Rem Alfelor 2015
OBSTETRICS MODULE: Hypertension Page 2 of 12
Normal implantation is characterized by extensive remodeling of the spiral Diminished perfusion and a hypoxic environment eventually lead to release of
arterioles within the decidua basalis. placental debris or microparticles that incite a systemic inflammatory response
Endovascular trophoblasts replace the vascular endothelial and muscular Defective placentation is posited to further cause the susceptible (pregnant)
linings to enlarge the vessel diameter. woman to develop gestational hypertension, the preeclampsia syndrome,
The veins are invaded only superficially. preterm delivery, a growth-restricted fetus, and/or placental abruption
In some cases of preeclampsia, however, there may be incomplete trophoblastic Acute atherosis identifies a group of women at increased risk for later
invasion. atherosclerosis and cardiovascular disease.
Decidual vessels, but not myometrial vessels, become lined with
endovascular trophoblasts. Immunological Factors
The deeper myometrial arterioles do not lose their endothelial lining and
Maternal immune tolerance to paternally derived placental and fetal antigens
musculoelastic tissue, and their mean external diameter is only half that of
Loss of this tolerance is another theory cited to account for preeclampsia
corresponding vessels in normal placentas
syndrome
In general, the magnitude of defective trophoblastic invasion is thought to
Histological changes at the maternal placental interface are suggestive of acute
correlate with severity of the hypertensive disorder
graft rejection.
Early preeclamptic changes included endothelial damage, insudation of plasma
Some of the factors possibly associated with dysregulation include
constituents into vessel walls, proliferation of myointimal cells, and medial
immunization from a previous pregnancy, some inherited human leukocyte
necrosis.
antigen (HLA) and natural killer (NK)-cell receptor haplotypes, and shared
Lipid accumulated first in myointimal cells and then within macrophages. These
susceptibility genes with diabetes and hypertension
lipid-laden cell changes, were referred to as atherosis
Suggest preeclampsia to be an immune-mediated disorder.
Vascular lesions including spiral arteriole narrowing, atherosis, and infarcts were
The risk of preeclampsia is appreciably enhanced in circumstances in which
more common in placentas from women diagnosed with preeclampsia before 34
formation of blocking antibodies to placental antigenic sites might be impaired.
weeks.
First pregnancy would carry a higher risk.
Tolerance dysregulation might also explain an increased risk when the paternal
antigenic load is increased with two sets of paternal chromosome, a double
dose.
Women with molar pregnancies have a high incidence of early-onset
preeclampsia.
Women with a trisomy 13 fetus also have a 30-40% incidence of
preeclampsia.
These women have elevated serum levels of antiangiogenic factors and
the gene for one of these factors, sflt-1, is on chromosome 13
Women previously exposed to paternal antigens, such as a prior pregnancy with
the same partner, are immunized against preeclampsia.
This phenomenon is not as apparent in women with a prior abortion.
In women destined to be preeclamptic, extravillous trophoblasts early in
pregnancy express reduced amounts of immunosuppressive non-classic HLA G.
During normal pregnancy, T-helper (Th) lymphocytes are produced so that type
2 activity is increased in relation to type 1 (type 2 bias)
Th2 cells promote humoral immunity, whereas Th1 cells stimulate
inflammatory cytokine secretion.
Beginning in the early second trimester in women who develop
FIGURE 40-2 Schematic representation of normal placental implantation shows proliferation of preeclampsia, Th1 action is increased and the Th1/Th2 ratio changes.
extravillous trophoblasts from an anchoring villus. These trophoblasts invade the decidua and Contributors to an enhanced immunologically mediated inflammatory reaction
extend into the walls of the spiral arteriole to replace the endothelium and muscular wall to create a are stimulated by placental microparticles and by adipocytes
dilated low-resistance vessel. With preeclampsia, there is defective implantation characterized by
incomplete invasion of the spiral arteriolar wall by extravillous trophoblasts. This results in a small
caliber vessel with high resistance to flow. Endothelial Cell Activation
Inflammatory changes are believed to be a continuation of the stage 1 changes
caused by defective placentation
In response to placental factors released by ischemic changes or by any other
inciting cause, a cascade of events begins
Antiangiogenic and metabolic factors and other inflammatory mediators
are thought to provoke endothelial cell injury.
Endothelial cell dysfunction may result from an extreme activated state of
leukocytes
In the maternal circulation, cytokines such as tumor necrosis factor- (TNF-)
and the interleukins (IL) may contribute to the oxidative stress associated with
preeclampsia.
This is characterized by reactive oxygen species and free radicals that
lead to formation of self-propagating lipid peroxides
These in turn generate highly toxic radicals that injure endothelial cells,
modify their nitric oxide production, and interfere with prostaglandin
FIGURE 40-3 Atherosis in a blood vessel from a placental bed. A. Photomicrograph shows balance.
disruption of the endothelium that result in a narrowed lumen because of subendothelial Other consequences of oxidative stress include production of the lipid-laden
accumulation of plasma proteins and foamy macrophages. Some of the foamy macrophages are macrophage foam cells seen in atherosis; activation of microvascular
shown by curved arrows, and straight arrows highlight areas of endothelial disruption. B. coagulation manifest by thrombocytopenia; and increased capillary permeability
Schematic diagram of the photomicrograph. manifest by edema and proteinuria.
Abnormally narrow spiral arteriolar lumen likely impairs placental blood flow. Nutritional Factors
Decreased soluble antiangiogenic growth factors may be involved in faulty
endovascular remodeling.
Rem Alfelor 2015
OBSTETRICS MODULE: Hypertension Page 3 of 12
In the general population, a diet high in fruits and vegetables with antioxidant Damaged or activated endothelial cells may produce less nitric oxide and
activity is associated with decreased blood pressure. secrete substances that promote coagulation and increase sensitivity to
Incidence of preeclampsia was doubled in women whose daily intake of ascorbic vasopressors
acid as less than 85 mg. Evidence of endothelial activation includes the characteristic changes in
Calcium supplementation in populations with a low dietary calcium intake had a glomerular capillary endothelial morphology, increased capillary permeability,
small effect to lower perinatal mortality rates but no effect on preeclampsia and elevated blood concentrations of substances associated with endothelial
incidence activation.
These latter substances are transferable, and serum from women with
preeclampsia stimulates some of these substances in greater amounts.
Genetic factors
Preeclampsia is a multifactorial, polygenic disorder
Incident risk for preeclampsia of 20-40% for daughters of preeclamptic mothers; Increased Pressor Responses
11-37% for sisters of preeclamptic women; 22-47% for twins there was a genetic As discussed in Chapter 4 (p. 61), pregnant women normally develop refractoriness to
component for gestational hypertension and for preeclampsia., 60% infused
concordance in monozygotic female twin pairs. vasopressors (Abdul-Karim, 1961). Women with early preeclampsia, however, have
Plasma-derived factors may induce some of genes in preeclampsia increased
Polymorphisms of the genes for Fas receptor, hypoxia-inducible factor-1 vascular reactivity to infused norepinephrine and angiotensin II (Raab, 1956; Talledo,
protein (hif-1), il-1, lymphotoxin-, transforming growth factor beta 3 (TGF- 1968).
3), apolipoprotein E (apo E), and TNF- have also been studied with varying Moreover, increased sensitivity to angiotensin II clearly precedes the onset of
results gestational
Because of the heterogeneity of the preeclampsia syndrome and other genetic
hypertension (Gant, 1974).
and environmental factors that interact with its complex phenotypic expression, it
is doubtful that any one candidate gene will be found responsible. Prostaglandins
Linked preeclampsia predisposition to fetal genes on chromosome 18. Several prostanoids are thought to be central to preeclampsia syndrome
pathophysiology.
Specifically, the blunted pressor response seen in normal pregnancy is at least
partially due to
decreased vascular responsiveness mediated by endothelial prostaglandin synthesis.
For example,
compared with normal pregnancy, endothelial prostacyclin (PGI2) production is
decreased in
preeclampsia. This action appears to be mediated by phospholipase A2 (Davidge,
2014). At the same
time, thromboxane A2 secretion by platelets is increased, and the
prostacyclin:thromboxane A2 ratio
decreases. The net result favors increased sensitivity to infused angiotensin II and,
ultimately,
vasoconstriction (Spitz, 1988). These changes are apparent as early as 22 weeks in
Other Genetic Variables women who later
Ethnoracial factors are important as discussed regarding the high incidence of develop preeclampsia (Chavarria, 2003).
preeclampsia in African-American women.
Nitric Oxide
Latina women have a lower prevalence because of interactions of American
Indian and white race genes This potent vasodilator is synthesized from L-arginine by endothelial cells. Withdrawal
of nitric
oxide results in a clinical picture similar to preeclampsia in a pregnant animal model
Pathogenesis
(Conrad, 1989).
Vasospasm
Inhibition of nitric oxide synthesis increases mean arterial pressure, decreases heart
Endothelial activation causes vascular constriction with increased resistance rate, and
and subsequent hypertension. reverses the pregnancy-induced refractoriness to vasopressors. In humans, nitric
At the same time, endothelial cell damage causes interstitial leakage through oxide likely is the
which blood constituents, including platelets and fibrinogen, are deposited
compound that maintains the normal low-pressure vasodilated state characteristic of
subendothelial.
fetoplacental
disruption of endothelial junctional proteins
The much larger venous circuit is similarly involved, and with diminished blood perfusion (Myatt, 1992; Weiner, 1992). It also is produced by fetal endothelium, and
here it is
flow because of maldistribution, ischemia of the surrounding tissues can lead to
necrosis, hemorrhage, and other end-organ disturbances characteristic of the increased in response to preeclampsia, diabetes, and sepsis (Parra, 2001; von
syndrome. Mandach, 2003).
One important clinical correlate is the markedly attenuated blood volume seen in The effects of nitric oxide production in preeclampsia are unclear (Davidge, 2014). It
women with severe preeclampsia appears that
the syndrome is associated with decreased endothelial nitric oxide synthase
Endothelial Cell Injury expression, thus
Protein factor likely placental are secreted into the maternal circulation and increasing nitric oxide inactivation. These responses may be race related, with African-
provoke activation and dysfunction of the vascular endothelium. American
Circulating endothelial cell (CEC) levels are elevated fourfold in the peripheral women producing more nitric oxide (Wallace, 2009).
blood of preeclamptic women Endothelins
Increased levels of circulating endothelial microparticles (EMPS) in preeclamptic These 21-amino acid peptides are potent vasoconstrictors, and endothelin-1 (ET-1) is
women. the primary
Intact endothelium has anticoagulant properties, and endothelial cells blunt the isoform produced by human endothelium (George, 2011). Plasma ET-1 levels are
response of vascular smooth muscle to agonists by releasing nitric oxide. increased in
Rem Alfelor 2015
OBSTETRICS MODULE: Hypertension Page 4 of 12
normotensive pregnant women, but women with preeclampsia have even higher levels Although the cause of preeclampsia remains unknown, evidence for its manifestation
(Ajne, 2003; begins early in
Clark, 1992). According to Taylor and Roberts (1999), the placenta is not the source of pregnancy with covert pathophysiological changes that gain momentum across
increased gestation and
ET-1 concentrations, and they likely arise from systemic endothelial activation. eventually become clinically apparent. Unless delivery supervenes, these changes
Interestingly, ultimately result in
treatment of preeclamptic women with magnesium sulfate lowers ET-1 concentrations multiorgan involvement with a clinical spectrum ranging from an attenuated
(Sagsoz, manifestation to one of
2003). cataclysmic deterioration that is life threatening for both mother and fetus. As
Angiogenic and Antiangiogenic Proteins discussed, these are
Placental vasculogenesis is evident by 21 days after conception. There is an ever- thought to be a consequence of endothelial dysfunction, vasospasm, and ischemia.
expanding list of Although the many
pro- and antiangiogenic substances involved in placental vascular development. The maternal consequences of the preeclampsia syndrome are usually described in terms
families of of individual
vascular endothelial growth factor (VEGF) and angiopoietin (Ang) are most extensively organ systems, they frequently are multiple, and they overlap clinically.
studied. Cardiovascular System
Angiogenic imbalance is used to describe excessive amounts of antiangiogenic factors Severe disturbances of normal cardiovascular function are common with preeclampsia
that are syndrome.
hypothesized to be stimulated by worsening hypoxia at the uteroplacental interface. These are related to: (1) increased cardiac afterload caused by hypertension; (2)
Trophoblast of cardiac preload,
women destined to develop preeclampsia overproduces at least two antiangiogenic which is affected negatively by pathologically diminished hypervolemia of pregnancy
peptides that and is
enter the maternal circulation (Karumanchi, 2014): increased by intravenous crystalloid or oncotic solutions; and (3) endothelial activation
1. Soluble Fms-like tyrosine kinase 1 (sFlt-1) is a variant of the Flt-1 receptor for with
placental growth interendothelial extravasation of intravascular fluid into the extracellular space and
factor (PlGF) and for VEGF. Increased maternal sFlt-1 levels inactivate and decrease importantly, into
circulating the lungs.
free PlGF and VEGF concentrations, leading to endothelial dysfunction (Maynard, Hemodynamic Changes and Cardiac Function
2003). As shown in Figure 40-4, sFlt-1 levels begin to increase in maternal serum The cardiovascular aberrations of pregnancy-related hypertensive disorders vary
months before depending on
preeclampsia is evident. Haggerty and colleagues (2012) observed that these high several modifiers. These factors include hypertension severity, underlying chronic
levels in the disease,
second trimester were associated with a doubling of the risk for preeclampsia. This preeclampsia severity, and in which part of the clinical spectrum these are studied. In
divergence some women,
from normal levels appears to occur even sooner with early-onset preeclampsia these cardiovascular changes may precede hypertension onset (De Paco, 2008;
(Vatten, 2012). Easterling, 1990;
2. Soluble endoglin (sEng) is a placenta-derived 65-kDa molecule that blocks Khalil, 2012; Melchiorre, 2013). Nevertheless, with the clinical onset of preeclampsia,
endoglin, which is a cardiac
surface coreceptor for the TGF family. Also called CD105, this soluble form of output declines, due at least in part to increased peripheral resistance. When
endoglin inhibits assessing cardiac
various TGF isoforms from binding to endothelial receptors and results in decreased function in preeclampsia, consideration is given to echocardiographic measures of
endothelial myocardial
nitric oxide-dependent vasodilatation (Levine, 2006; Venkatesha, 2006). Serum levels function and to clinically relevant ventricular function.
of sEng also Myocardial Function. Serial echocardiographic studies have documented in
begin to increase months before clinical preeclampsia develops (Haggerty, 2012). preeclampsia evidence
for ventricular remodeling that is accompanied by diastolic dysfunction in 40 percent of
The cause of placental overproduction of antiangiogenic proteins remains an enigma. women
Concentrations of the soluble forms are not increased in the fetal circulation or (Melchiorre, 2012). In some of these women, functional differences persisted up to 16
amnionic fluid, and months after
their levels in maternal blood dissipate after delivery (Staff, 2007). Research currently delivery (Evans, 2011). Ventricular remodeling was judged to be an adaptive response
is focused on to maintain
immunological mechanisms, oxidative stress, mitochondrial pathology, and hypoxia normal contractility with the increased afterload of preeclampsia. In the otherwise
genes healthy pregnant
(Karumanchi, 2014). Clinical research is directed at use of antiangiogenic proteins in woman, these changes are usually clinically inconsequential. But when combined with
the prediction underlying
ventricular dysfunctionfor example, concentric ventricular hypertrophy from chronic
and diagnosis of preeclampsia. In a systematic review, Widmer and associates (2007) hypertension
concluded that
third-trimester elevation of sFlt-1 levels and decreased PlGF concentrations correlate further diastolic dysfunction may cause cardiogenic pulmonary edema as discussed
with in Chapters 47
preeclampsia development after 25 weeks. These results require verification in (p. 943) and 49 (p. 990).
prospective studies. Ventricular Function. Despite the relatively high frequency of diastolic dysfunction with
Subsequently, Haggerty and coworkers (2012) reported that doubling of expressions of preeclampsia, in most women clinical cardiac function is appropriate. This has been
sFlt-1 and shown by
sEng increased the preeclampsia risk 39 and 74 percent, respectively. several studies in which ventricular function was assessed using invasive
PATHOPHYSIOLOGY hemodynamic methods
Rem Alfelor 2015
OBSTETRICS MODULE: Hypertension Page 5 of 12
(Hibbard, 2014). Importantly, both normally pregnant women and those with consequence of blood loss at delivery (Chap. 41, p. 783). It may also partially result
preeclampsia syndrome from increased
can have normal or slightly hyperdynamic ventricular function (Fig. 40-5). Thus, both erythrocyte destruction as subsequently described. Vasospasm and endothelial
have a cardiac leakage of plasma may
output that is appropriate for left-sided filling pressures. Data from preeclamptic persist for a variable time after delivery as the endothelium is restored to normalcy. As
women obtained by this takes
invasive hemodynamic studies are confounded because of the heterogeneity of place, vasoconstriction reverses, and as the blood volume increases, the hematocrit
populations and usually falls.
interventions that also may significantly alter these measurements. Some of these are Thus, women with eclampsia:
crystalloid Are unduly sensitive to vigorous fluid therapy administered in an attempt to expand
infusions, antihypertensive agents, and magnesium sulfate. Ventricular function the contracted
studies of preeclamptic women from several investigations are shown in blood volume to normal pregnancy levels
Figure 40-6. Although cardiac function was hyperdynamic in all women, filling Are sensitive to amounts of blood loss at delivery that are considered normal for a
pressures were normotensive
dependent on the volume of intravenous fluids. Specifically, aggressive hydration woman.
resulted in overtly hyperdynamic ventricular function in most women. However, this Hematological Changes
was accompanied by elevated
Several hematological abnormalities are associated with the preeclampsia syndrome.
pulmonary capillary wedge pressures. In some of these women, pulmonary edema Among those
may develop
commonly identified is thrombocytopenia, which at times may become severe enough
despite normal ventricular function because of an alveolar endothelial-epithelial leak. to be life
This is
threatening. Occasionally, the levels of some plasma clotting factors may be
compounded by decreased oncotic pressure from a low serum albumin concentration decreased, and
(American
erythrocytes display abnormal morphology and undergo rapid hemolysis.
College of Obstetricians and Gynecologists, 2012b). Thus, increased cardiac output
and hyperdynamic ventricular function is largely a result of low Thrombocytopenia
wedge pressures and not a result of augmented myocardial contractility. By Decreased platelet concentrations with eclampsia were described as early as 1922 by
comparison, women Stancke. The
given appreciably larger volumes of fluid commonly had filling pressures that platelet count is routinely measured in women with any form of gestational
exceeded normal, but hypertension. The
their ventricular function remained hyperdynamic because of concomitantly increased frequency and intensity of thrombocytopenia vary and are dependent on the severity
cardiac output. and duration of
From these studies, it is reasonable to conclude that aggressive fluid administration to the preeclampsia syndrome and the frequency with which platelet counts are
otherwise normal women with severe preeclampsia substantially elevates normal left- performed (Heilmann,
sided filling pressures 2007; Hupuczi, 2007). Overt thrombocytopeniadefined by a platelet count <
and increases a physiologically normal cardiac output to hyperdynamic levels. 100,000/L
Blood Volume indicates severe disease (see Table 40-2). In general, the lower the platelet count, the
higher the rates
For nearly 100 years, hemoconcentration has been a hallmark of eclampsia. This was
not precisely of maternal and fetal morbidity and mortality (Leduc, 1992). In most cases, delivery is
advisable
quantified until Zeeman and colleagues (2009) expanded the previous observations of
Pritchard and because thrombocytopenia usually continues to worsen. After delivery, the platelet
count may
associates (1984) and showed in eclamptic women that the normally expected
hypervolemia is continue to decline for the first day or so. It then usually increases progressively to
reach a normal
severely curtailed (Fig. 40-7). Women of average size should have a blood volume of
nearly 4500 level within 3 to 5 days. As discussed on page 768, in some instances with HELLP
syndrome, the
mL during the last several weeks of a normal pregnancy. In nonpregnant women, this
volume platelet count continues to fall after delivery. If these do not reach a nadir until 48 to 72
hours, then
approximates only 3000 mL. With eclampsia, however, much or all of the anticipated
normal excess preeclampsia syndrome may be incorrectly attributed to one of the thrombotic
microangiopathies
1500 mL is lost. Such hemoconcentration results from generalized vasoconstriction
that follows (George, 2013). These syndromes are discussed in Chapter 56 (p. 1116).
endothelial activation and leakage of plasma into the interstitial space because of Other Platelet Abnormalities
increased In addition to thrombocytopenia, there are myriad other platelet alterations described
permeability. In women with preeclampsia, and depending on its severity, with the
hemoconcentration is preeclampsia syndrome. These were reviewed by Kenny and coworkers (2014) and
usually not as marked. Women with gestational hypertension, but without include platelet
preeclampsia, usually have activation with increased -degranulation producing -thromboglobulin, factor 4, and
a normal blood volume (Silver, 1998). increased
clearance. Paradoxically, in most studies, in vitro platelet aggregation is decreased
compared with
For women with severe hemoconcentration, it was once taught that an acute fall in
hematocrit the normal increase characteristic of pregnancy. This likely is due to platelet
exhaustion following
suggested resolution of preeclampsia. In this scenario, hemodilution follows
endothelial healing with in vivo activation. Although the cause is unknown, immunological processes or simply
plateletdeposition at sites of endothelial damage may be implicated. Platelet-bound
return of interstitial fluid into the intravascular space. Although this is somewhat and circulating plateletbindable
correct, it is
immunoglobulins are increased, which suggest platelet surface alterations.
important to recognize that a substantive cause of this fall in hematocrit is usually the
Neonatal Thrombocytopenia
Rem Alfelor 2015
OBSTETRICS MODULE: Hypertension Page 6 of 12
Severe thrombocytopenia does not develop in the fetus or infant born to preeclamptic The normal pregnancy-induced extra- and intracellular volume increases that are
women despite accompanied by
severe maternal thrombocytopenia (Kenny, 2014; Pritchard, 1987). Importantly, vasodilatation undergo further complex shifts with the preeclampsia syndrome. In
maternal addition to blood
thrombocytopenia in hypertensive women is not a fetal indication for cesarean delivery. volume changes shown in Figure 40-7, there are many hormonal, fluid, and electrolyte
Hemolysis aberrations.
Severe preeclampsia is frequently accompanied by evidence of hemolysis as manifest Endocrine Changes
by elevated Plasma levels of renin, angiotensin II, angiotensin 17, aldosterone, and atrial
serum lactate dehydrogenase levels and decreased haptoglobin levels. Other natriuretic peptide
evidence comes from are substantively increased during normal pregnancy. Deoxycorticosterone (DOC) is a
schizocytosis, spherocytosis, and reticulocytosis in peripheral blood (Cunningham, potent
1985; Pritchard, mineralocorticoid that is also increased remarkably in normal pregnancy (Chap. 4, p.
1954, 1976). These derangements result in part from microangiopathic hemolysis 71). This
caused by compound results from conversion of plasma progesterone to DOC rather than
endothelial disruption with platelet adherence and fibrin deposition. Sanchez-Ramos increased maternal
and colleagues adrenal secretion. Because of this, DOC secretion is not reduced by sodium retention
(1994) described increased erythrocyte membrane fluidity with HELLP syndrome. or hypertension.
Cunningham and This may explain why women with preeclampsia retain sodium (Winkel, 1980). In
coworkers (1995) postulated that these changes were due to serum lipid alterations, pregnancy, the
and Mackay and mineralocorticoid receptor becomes less sensitive to aldosterone (Armanini, 2012).
associates (2012) found substantively decreased long-chain fatty acid content in Vasopressin levels are similar in nonpregnant, normally pregnant, and preeclamptic
erythrocytes of women even
preeclamptic women. Erythrocytic membrane changes, increased adhesiveness, and though the metabolic clearance is increased in the latter two (Drr, 1999).
aggregation may Atrial natriuretic peptide is released during atrial wall stretching from blood volume
also promote a hypercoagulable state (Gamzu, 2001). expansion,
HELLP Syndrome. Subsequent to reports of hemolysis and thrombocytopenia with and it responds to cardiac contractility (Chap. 4, p. 61). Serum levels rise in pregnancy,
severe and its
preeclampsia, descriptions followed that abnormally elevated serum liver secretion is further increased in women with preeclampsia (Borghi, 2000; Luft, 2009).
transaminase levels were Levels of its
commonly found and were indicative of hepatocellular necrosis (Chesley, 1978). precursorproatrial natriuretic peptideare also increased in preeclampsia (Sugulle,
Weinstein (1982) 2012).
referred to this combination of events as the HELLP syndromeand this moniker now Fluid and Electrolyte Changes
is used In women with severe preeclampsia, the volume of extracellular fluid, manifest as
worldwide. Also, and as shown in Table 40-2, facets of the HELLP syndrome are edema, is usually
included in criteria much greater than that in normal pregnant women. The mechanism responsible for
that differentiate severe from nonsevere preeclampsia. The HELLP syndrome is pathological fluid
discussed in further retention is thought to be endothelial injury (Davidge, 2014). In addition to generalized
detail on page 742. edema and
Coagulation Changes proteinuria, these women have reduced plasma oncotic pressure. This reduction
Subtle changes consistent with intravascular coagulation, and less often erythrocyte creates a filtration
destruction, imbalance and further displaces intravascular fluid into the surrounding interstitium.
commonly are found with preeclampsia and especially eclampsia (Kenny, 2014). Some Electrolyte concentrations do not differ appreciably in women with preeclampsia
of these compared with
changes include increased factor VIII consumption, increased levels of fibrinopeptides those of normal pregnant women. This may not be the case if there has been vigorous
A and B and diuretic therapy,
o f D-dimers, and decreased levels of regulatory proteinsantithrombin III and protein sodium restriction, or administration of free water with sufficient oxytocin to produce
C and S. antidiuresis.
Except for thrombocytopenia discussed above, coagulation aberrations generally are Following an eclamptic convulsion, the serum pH and bicarbonate concentration are
mild and are lowered due
seldom clinically significant (Kenny, 2014; Pritchard, 1984). Unless there is associated to lactic acidosis and compensatory respiratory loss of carbon dioxide. The intensity of
placental acidosis
abruption, plasma fibrinogen levels do not differ remarkably from levels found in relates to the amount of lactic acid producedmetabolic acidosisand the rate at
normal pregnancy. which carbon
Fibrin degradation products such as d-dimers are elevated only occasionally. dioxide is exhaledrespiratory acidosis.
Fibronectin, a Kidney
glycoprotein associated with vascular endothelial cell basement membrane, is During normal pregnancy, renal blood flow and glomerular filtration rate are increased
elevated in women appreciably
with preeclampsia (Brubaker, 1992). As preeclampsia worsens, so do abnormal (Chap. 4, p. 63). With development of preeclampsia, there may be a number of
findings with reversible anatomical
thromboelastography (Pisani-Conway, 2013). Despite these changes, routine and pathophysiological changes. Of clinical importance, renal perfusion and
laboratory assessments glomerular filtration are
of coagulation, including prothrombin time, activated partial thromboplastin time, and reduced. Levels that are much less than normal nonpregnant values are infrequent
plasma and are the
fibrinogen level, were found to be unnecessary in the management of pregnancy- consequence of severe disease.
associated
hypertensive disorders (Barron, 1999). Volume Homeostasis
Rem Alfelor 2015
OBSTETRICS MODULE: Hypertension Page 7 of 12
A small degree of decreased glomerular filtration may result from reduced plasma mg/g, that is, 0.13 to 0.15, indicate a low likelihood of proteinuria exceeding 300
volume. Mostof the decrement, however, is from increased renal afferent arteriolar mg/day. Midrange
resistance that may be elevated ratios, that is, 300 mg/g or 0.3 have poor sensitivity and specificity. Stout and
up to fivefold (Conrad, 2014; Cornelis, 2011). There are also morphological changes colleagues (2013)
characterized found that values < 0.08 or > 1.19 had negative- or positive-predictive values of 86 and
by glomerular endotheliosis blocking the filtration barrier. This is discussed further 96 percent,
subsequently. respectively. At this time, most recommend that with midrange ratio values, 24-hour
Diminished filtration causes serum creatinine levels to rise to values seen in protein excretion
nonpregnant individuals, should be quantified.
that is, 1 mg/mL, and sometimes even higher (Lindheimer, 2008a). Abnormal values There are several methods used to measure proteinuria, and none detect all of the
usually begin to various proteins
normalize 10 days or later after delivery (Spaan, 2012a). normally excreted (Nayeri, 2013). A more accurate method involves measurement of
In most preeclamptic women, urine sodium concentration is elevated. Urine osmolality, albumin
urine:plasma creatinine ratio, and fractional excretion of sodium also indicate that a excretion. Albumin filtration exceeds that of larger globulins, and with glomerular
prerenal disease such as
mechanism is involved. Kirshon and coworkers (1988) infused dopamine intravenously preeclampsia, most of the protein in urine is albumin. There are test kits that permit
into oliguric rapid
women with preeclampsia, and this renal vasodilator stimulated increased urine measurement of urinary albumin:creatinine ratios in an outpatient setting (Kyle, 2008).
output, fractional Although worsening or nephrotic-range proteinuria has been considered by most to be
sodium excretion, and free water clearance. As was shown in Figure 40-6, sodium- a sign of
containing severe disease, this does not appear to be the case (Airoldi, 2007). Certainly, this
crystalloid infusion increases left ventricular filling pressure, and although oliguria concept was not
temporarily accepted by the 2013 Task Force. Finally, increasing proteinuria is more common in
improves, rapid infusions may cause clinically apparent pulmonary edema. Intensive multifetal
intravenous pregnancy complicated by preeclampsia (Zilberberg, 2013).
fluid therapy is not indicated as treatment for preeclamptic women with oliguria. Anatomical Changes
Exceptions Sheehan and Lynch (1973) commonly found changes identifiable at autopsy by light
are diminished urine output from hemorrhage or fluid loss from vomiting or fever. and electron
Plasma uric acid concentration is typically elevated in preeclampsia. The elevation microscopy in the kidneys of eclamptic women. Glomeruli are enlarged by
exceeds the approximately 20 percent,
reduction in glomerular filtration rate and likely is also due to enhanced tubular they are bloodless, and capillary loops variably are dilated and contracted.
reabsorption Endothelial cells are
(Chesley, 1945). At the same time, preeclampsia is associated with diminished urinary swollentermed glomerular capillary endotheliosis by Spargo and associates (1959).
excretion of Endothelial
calcium, perhaps because of increased tubular reabsorption (Taufield, 1987). Another cells are often so swollen that they block or partially block the capillary lumens (Fig.
possibility is 40-8).
from increased placental urate production compensatory to increased oxidative stress. Homogeneous subendothelial deposits of proteins and fibrin-like material are seen.
Proteinuria
As shown in Table 40-1, some degree of proteinuria will establish the diagnosis of
preeclampsia
syndrome. Proteinuria may develop late, and some women may already be delivered
or have had an
eclamptic convulsion before it appears. For example, 10 to 15 percent of women with
HELLP
syndrome did not have proteinuria at presentation (Sibai, 2004). In another report, 17
percent of
eclamptic women did not have proteinuria by the time of seizures (Zwart, 2008).
Problematically, the optimal method of establishing abnormal levels of either urine
protein or
albumin remains to be defined. Chen and associates (2008) have shown that clean-
catch and FIGURE 40-8 Schematic showing glomerular capillary endotheliosis. The capillary of
the normal
catheterized urine specimens correlate well. But dipstick qualitative determinations
depend on glomerulus shown on the left has wide endothelial fenestrations, and the pedicels
emanating from the
urinary concentration and are notorious for false-positive and -negative results. For a
24-hour podocytes are widely spaced (arrow). The illustration on the right is of a glomerulus
with changes
quantitative specimen, the consensus threshold value used is > 300 mg/24 h (Task
Force, 2013). induced by the preeclampsia syndrome. The endothelial cells are swollen and their
fenestrae
Tun and colleagues (2012) have shown equivalent efficacy using protein excretion of
165 mg in a 12- narrowed, as are the pedicels that now abut each other.
hour sample. Importantly, these values have not been irrefutably established.
Determination of urinary protein:creatinine ratio may supplant the cumbersome 24- Endothelial swelling may result from angiogenic factor withdrawal caused by free
hour angiogenic
quantification (Ethridge, 2013; Kyle, 2008; Morris, 2012). In a systematic review, proteins complexing with the circulating antiangiogenic protein receptor discussed on
Papanna and page 735
associates (2008) concluded that random urine protein:creatinine ratios that are below (Conrad, 2014; Eremina, 2007; Karumanchi, 2009). The angiogenic proteins are
130 to 150 crucial for podocyte
Rem Alfelor 2015
OBSTETRICS MODULE: Hypertension Page 8 of 12
health, and their inactivation leads to podocyte dysfunction and endothelial swelling. Second, asymptomatic elevations of serum hepatic transaminase levelsAST and
One marker of ALTare also
this is excretion of podocyte proteins such as nephrin, podocalyxin, and ig-h3 considered markers for severe preeclampsia. Values seldom exceed 500 U/L, but
(transforming growth have been reported
factor, -induced) (Wang, 2012b). Also, eclampsia is characterized by increased to be greater than 2000 U/L in some women (Chap. 55, p. 1085). In general, serum
excretion of urinary levels inversely
podocytes, a phenomenon shared by other proteinuric disorders (Garrett, 2013; follow platelet levels, and they both usually normalize within 3 days following delivery
Wagner, 2012). Of as previously
interest, podocytes are epithelia, and thus renal pathology involves both endothelial discussed on page 738.
and epithelial In a third example of liver involvement, hemorrhagic infarction may extend to form a
cells (see Fig. 40-8). hepatic
Acute Kidney Injury hematoma. These in turn may extend to form a subcapsular hematoma that may
Rarely is acute tubular necrosis caused by preeclampsia alone. Although mild degrees rupture. They can be
are identified using computed tomography (CT) scanning or magnetic resonance (MR)
encountered in neglected cases, clinically apparent renal failure is invariably induced imaging as shown
by coexistent in Figure 40-10. Unruptured hematomas are probably more common than clinically
hemorrhage with hypovolemia and hypotension (Chap. 41, p. 814). This is usually suspected and are
caused by severe more likely to be found with HELLP syndrome (Carlson, 2004; Vigil-De Gracia, 2012).
obstetrical hemorrhage for which adequate blood replacement is not given. Drakeley Although
and coworkers once considered a surgical condition, contemporaneous management usually consists
(2002) described 72 women with preeclampsia and renal failure. Half had HELLP of observation
syndrome, and a and conservative treatment of hematomas unless hemorrhage is ongoing. In some
third had placental abruption. As discussed on page 742, Haddad and colleagues cases, however,
(2000) reported that prompt surgical intervention may be lifesaving. Vigil-De Gracia and coworkers (2012)
5 percent of 183 women with HELLP syndrome had kidney injury. Half of these, reviewed 180
however, also had a cases of hepatic hematoma or rupture. More than 90 percent had HELLP syndrome,
placental abruption, and most had postpartum hemorrhage. Rarely, irreversible renal and in 90 percent,
cortical the capsule had ruptured. The maternal mortality rate was 22 percent, and the
necrosis develops (Chap. 53, p. 1064). perinatal mortality rate
Liver was 31 percent. In rare cases, liver transplant is necessary (Hunter, 1995; Wicke,
2004).
Hepatic changes in women with fatal eclampsia were described in 1856 by Virchow.
The
characteristic lesions were regions of periportal hemorrhage in the liver periphery. In Last, acute fatty liver of pregnancy is sometimes confused with preeclampsia (Nelson,
their elegant 2013;
autopsy studies, Sheehan and Lynch (1973) described that some degree of hepatic Sibai, 2007a). It too has an onset in late pregnancy, and often there is accompanying
infarction hypertension,
accompanied hemorrhage in almost half of women who died with eclampsia. These elevated serum transaminase and creatinine levels, and thrombocytopenia (Chap. 55,
corresponded p. 1086).
with reports that had appeared during the 1960s describing elevated serum hepatic HELLP Syndrome
transaminase There is no universally accepted strict definition of this syndrome, and thus its
levels. Along with the earlier observations by Pritchard and associates (1954), who incidence varies by
described investigator. When it is identified, the likelihood of hepatic hematoma and rupture is
hemolysis and thrombocytopenia with eclampsia, this constellation of hemolysis, substantially
hepatocellular increased. In a multicenter study, Haddad and colleagues (2000) described 183
necrosis, and thrombocytopenia was later termed HELLP syndrome by Weinstein women with HELLP
(1985) to call syndrome of whom 40 percent had adverse outcomes including two maternal deaths.
attention to its seriousness (p. 742). The incidence of
Lesions as extensive as those shown in Figure 40-9 are unusual, even in the autopsy subcapsular liver hematoma was 1.6 percent. Other complications included eclampsia
series by 6 percent,
Sheehan and Lynch (1973). From a pragmatic point, liver involvement with placental abruption10 percent, acute kidney injury5 percent, and pulmonary
preeclampsia may be edema10 percent.
clinically significant in several circumstances. Other serious complications included stroke, coagulopathy, acute respiratory distress
syndrome, and
sepsis.
First, symptomatic involvement is considered a sign of severe disease. It typically
manifests by Women with preeclampsia complicated by the HELLP syndrome typically have worse
outcomes
moderate to severe right-upper quadrant or midepigastric pain and tenderness. In
many cases, such than those without these findings (Kozic, 2011; Martin, 2012, 2013). In their review of
693 women
women also have elevated levels of serum aminotransferase, namely, aspartate
aminotransferase with HELLP syndrome, Keiser and coworkers (2009) reported that 10 percent had
concurrent
(AST) or alanine aminotransferase (ALT). In some cases, however, the amount of
hepatic tissue eclampsia. Sep and associates (2009) also described a significantly increased risk for
complications
involved with infarction may be surprisingly extensive yet still clinically insignificant. In
our in women with HELLP syndrome compared with those with isolated preeclampsia.
These included
experiences, infarction may be worsened by hypotension from obstetrical hemorrhage,
and it eclampsia15 versus 4 percent; preterm birth93 versus 78 percent; and perinatal
mortality rate
occasionally causes hepatic failureso-called shock liver (Alexander, 2009).
Rem Alfelor 2015
OBSTETRICS MODULE: Hypertension Page 9 of 12
hypothesized to result in ischemia, cytotoxic edema, and eventually tissue infarction.
9 versus 4 percent, respectively. Because of these marked clinical differences, these Although this
investigators theory was widely embraced for many years, there is little objective evidence to
postulate that HELLP syndrome has a distinct pathogenesis. Others have shown a support it.
difference in the The second theory is that sudden elevations in systemic blood pressure exceed the
ratio of antiangiogenic and inflammatory acute-phase proteins in these two conditions normal
and have cerebrovascular autoregulatory capacity (Hauser, 1988; Schwartz, 2000). Regions of
reached similar conclusions (Reimer, 2013). Given all of the variables contributing to forced
the incidence vasodilation and vasoconstriction develop, especially in arterial boundary zones. At the
and pathophysiology of preeclampsia as discussed on page 736, this is a reasonable capillary
conclusion. Sibai level, disruption of end-capillary pressure causes increased hydrostatic pressure,
and Stella (2009) have discussed some of these aspects under the rubric of atypical hyperperfusion, and
preeclampsiaeclampsia. extravasation of plasma and red cells through endothelial tight-junction openings. This
Pancreas leads to
According to Sheehan and Lynch (1973), there are no convincing data that the vasogenic edema. This theory is incomplete because very few eclamptic women have
pancreas has special mean arterial
involvement with preeclampsia syndrome. If so, the occasional case reports of pressures that exceed limits of autoregulationapproximately 160 mm Hg.
concurrent
hemorrhagic pancreatitis are likely unrelated (Swank, 2012). That said, severe It seems reasonable to conclude that the most likely mechanism is a combination of
hemoconcentration the two. Thus,
may predispose to pancreatic inflammation. a preeclampsia-associated interendothelial cell leak develops at blood pressure
Brain (hydraulic) levels
Headaches and visual symptoms are common with severe preeclampsia, and much lower than those usually causing vasogenic edema and is coupled with a loss of
associated convulsions upper-limit
define eclampsia. The earliest anatomical descriptions of brain involvement came from autoregulation (Zeeman, 2009). With imaging studies, these changes manifest as
autopsy facets of the
specimens, but CT- and MR-imaging and Doppler studies have added many important reversible posterior leukoencephalopathy syndrome (Hinchey, 1996). This
insights into subsequently became
cerebrovascular involvement. referred to as the posterior reversible encephalopathy syndromePRES. This term is
misleading
Neuroanatomical Lesions
because although PRES lesions principally involve the posterior brainthe occipital
Most gross anatomical descriptions of the brain in eclamptic women are taken from
and parietal
eras when
corticesin at least a third of cases, they also involve other brain areas (Edlow, 2013;
mortality rates were high. One consistent finding was that brain pathology accounted
Zeeman,
for only about a
2004a). The most frequently affected region is the parietooccipital cortexthe
third of fatal cases such as the one shown in Figure 40-11. In fact, most deaths were
boundary zone of the
from pulmonary
anterior, middle, and posterior cerebral arteries. Also, in most cases, these lesions are
edema, and brain lesions were coincidental. Thus, although gross intracerebral
reversible
hemorrhage was seen
(Cipolla, 2014).
in up to 60 percent of eclamptic women, it was fatal in only half of these (Melrose,
1984; Richards, Cerebral Blood Flow
1988; Sheehan, 1973). As shown in Figure 40-12, other principal lesions found at Autoregulation is the mechanism by which cerebral blood flow remains relatively
autopsy of constant despite
eclamptic women were cortical and subcortical petechial hemorrhages. The classic alterations in cerebral perfusion pressure. In nonpregnant individuals, this mechanism
microscopic protects the
vascular lesions consist of fibrinoid necrosis of the arterial wall and perivascular brain from hyperperfusion when mean arterial pressures increase to as high as 160
microinfarcts and mm Hg. These are
hemorrhages. Other frequently described major lesions include subcortical edema, pressures far greater than those seen in all but a very few women with eclampsia.
multiple Thus, to explain
nonhemorrhagic areas of softening throughout the brain, and hemorrhagic areas in eclamptic seizures, it was theorized that autoregulation must be altered by pregnancy.
the white matter. Although
There also may be hemorrhage in the basal ganglia or pons, often with rupture into the species differences must be considered, studies by Cipolla and colleagues (2007,
ventricles. 2009, 2014) have
convincingly shown that autoregulation is unchanged across pregnancy in rodents.
That said, some,
Cerebrovascular Pathophysiology
but not others, have provided evidence of impaired autoregulation in women with
Clinical, pathological, and neuroimaging findings have led to two general theories to
preeclampsia
explain cerebral
(Janzarik, 2014; van Veen, 2013).
abnormalities with eclampsia. Importantly, endothelial cell dysfunction that
characterizes the Zeeman and associates (2003) showed that cerebral blood flow during the first two
trimesters of
preeclampsia syndrome likely plays a key role in both. The first theory suggests that in
response to normal pregnancy is similar to nonpregnant values, but thereafter, it significantly
decreases by 20
acute and severe hypertension, cerebrovascular overregulation leads to vasospasm
(Trommer, 1988). percent during the last trimester. These investigators also documented significantly
increased cerebral
This presumption is based on the angiographic appearance of diffuse or multifocal
segmental blood flow in women with severe preeclampsia compared with that of normotensive
pregnant women
narrowings suggestive of vasospasm (Ito, 1995). In this scheme, diminished cerebral
blood flow is
Rem Alfelor 2015
OBSTETRICS MODULE: Hypertension Page 10 of 12
(Zeeman, 2004b). Taken together, these findings suggest that eclampsia occurs when and cortical regions of the parietal and occipital lobes (Fig. 40-13). There is also
cerebral relatively common
hyperperfusion forces capillary fluid interstitially because of endothelial damage, which involvement of the basal ganglia, brainstem, and cerebellum (Brewer, 2013; Zeeman,
leads to 2004a).
perivascular edema characteristic of the preeclampsia syndrome. In this regard, Although these PRES lesions are almost universal in women with eclampsia, their
eclampsia is an incidence in
example of the posterior reversible encephalopathy syndrome as previously women with preeclampsia is less frequent. They are more likely to be found in women
discussed. who have
Neurological Manifestations severe disease and who have neurological symptoms (Schwartz, 2000). And although
There are several neurological manifestations of the preeclampsia syndrome. Each usually
signifies severe reversible, a fourth of these hyperintense lesions represent cerebral infarctions that
involvement and requires immediate attention. First, headache and scotomata are have persistent
thought to arise findings (Loureiro, 2003; Zeeman, 2004a).
from cerebrovascular hyperperfusion that has a predilection for the occipital lobes.
According to Visual Changes and Blindness
Sibai (2005) and Zwart and coworkers (2008), 50 to 75 percent of women have Scotomata, blurred vision, or diplopia are common with severe preeclampsia and
headaches and 20 to eclampsia. These
30 percent have visual changes preceding eclamptic convulsions. The headaches may usually improve with magnesium sulfate therapy and/or lowered blood pressure.
be mild to Blindness is less
severe and intermittent to constant. In our experiences, they are unique in that they do common, is usually reversible, and may arise from three potential areas. These are the
not usually visual cortex
respond to traditional analgesia, but they do improve after magnesium sulfate infusion of the occipital lobe, the lateral geniculate nuclei, and the retina. In the retina,
is initiated. pathological lesions
Convulsions are a second potential manifestation and are diagnostic for eclampsia. may be ischemia, infarction, or detachment (Roos, 2012).
These are Occipital blindness is also called amaurosisfrom the Greek dimming. Affected
caused by excessive release of excitatory neurotransmittersespecially glutamate; women usually
massive have evidence of extensive occipital lobe vasogenic edema on imaging studies. Of 15
depolarization of network neurons; and bursts of action potentials (Meldrum, 2002). women cared
Clinical and for at Parkland Hospital, occipital blindness lasted from 4 hours to 8 days, but it
experimental evidence suggest that extended seizures can cause significant brain resolved completely
injury and later brain in all cases (Cunningham, 1995). Rarely, extensive cerebral infarctions may result in
dysfunction. total or partial
visual defects (Fig. 40-14).
As a third manifestation, blindness is rare with preeclampsia alone, but it complicates
eclamptic Blindness from retinal lesions is caused either by serous retinal detachment or rarely
convulsions in up to 15 percent of women (Cunningham, 1995). Blindness has been by retinal
reported to infarction, which is termed Purtscher retinopathy (Fig. 40-15). Serous retinal
develop up to a week or more following delivery (Chambers, 2004). There are at least detachment is usually
two types of unilateral and seldom causes total visual loss. In fact, asymptomatic serous retinal
blindness as discussed subsequently. detachment is
Last, generalized cerebral edema may develop and is usually manifest by mental relatively common (Saito, 1998). In most cases of eclampsia-associated blindness,
status changes visual acuity
that vary from confusion to coma. This situation is particularly dangerous because fatal subsequently improves, but if caused by retinal artery occlusion, vision may be
transtentorial permanently impaired
herniation may result. (Lara-Torre, 2002; Roos, 2012). In some women, these findings are additive.
Neuroimaging Studies Moseman and Shelton
With CT imaging, localized hypodense lesions at the gray- and white-matter junction, (2002) described a woman with permanent blindness due to a combination of retinal
primarily in the infarctions and
parietooccipital lobes, are typically found in eclampsia. Such lesions may also be seen bilateral lesions in the lateral geniculate nuclei
in the frontal
and inferior temporal lobes, the basal ganglia, and thalamus (Brown, 1988). The Cerebral Edema
spectrum of brain Clinical manifestations suggesting widespread cerebral edema are worrisome. During
involvement is wide, and increasing involvement can be identified with CT imaging. 13 years at
Edema of the Parkland Hospital, 10 of 175 women with eclampsia were diagnosed with symptomatic
occipital lobes or diffuse cerebral edema may cause symptoms such as blindness, cerebral
lethargy, and edema (Cunningham, 2000). Symptoms ranged from lethargy, confusion, and blurred
confusion (Cunningham, 2000). In the latter cases, widespread edema shows as a vision to
marked obtundation and coma. In most cases, symptoms waxed and waned. Mental status
compression or even obliteration of the cerebral ventricles. Such women may develop changes generally
signs of correlated with the degree of involvement seen with CT and MR imaging studies.
impending life-threatening transtentorial herniation. These women are
Several MR imaging acquisitions are used to study eclamptic women. Common very susceptible to sudden and severe blood pressure elevations, which can acutely
findings are worsen the
hyperintense T2 lesionsposterior reversible encephalopathy syndrome (PRES)in already widespread vasogenic edema. Thus, careful blood pressure control is
the subcortical essential. In the 10
Rem Alfelor 2015
OBSTETRICS MODULE: Hypertension Page 11 of 12
women with generalized edema, three became comatose and had imaging findings of vasodilatory response. Moreover, other pregnancy conditions are also associated with
impending increased
transtentorial herniation. One of these three died from herniation. Consideration is resistance (Urban, 2007). One major adverse effect, fetal-growth restriction, is
given for treatment discussed in Chapter
with mannitol or dexamethasone. 44 (p. 874).
Long-Term Neurocognitive Sequelae Pimenta and colleagues (2013) assessed placental vascularity using a three-
Women with eclampsia have been shown to have some cognitive decline when dimensional power
studied 5 to 10 years Doppler histogram. These researchers described the placental vascularity index, which
following an eclamptic pregnancy. This is discussed further on page 770. was
Uteroplacental Perfusion decreased in women with any pregnancy-associated hypertensive disorders11.1
percent compared
with 15.2 percent in normal controls.
Defects in endovascular trophoblastic invasion and placentation germane to
development of the Despite these findings, evidence for compromised uteroplacental circulation is found in
only a few
preeclampsia syndrome and fetal-growth restriction were discussed on page 732. Of
immense women who go on to develop preeclampsia. Indeed, when preeclampsia develops
during the third
clinical importance, compromised uteroplacental perfusion is almost certainly a major
culprit in the trimester, only a third of women with severe disease have abnormal uterine artery
velocimetry (Li,
increased perinatal morbidity and mortality rates. Thus, measurement of uterine,
intervillous, and 2005). In a study of 50 women with HELLP syndrome, only a third had abnormal
uterine artery
placental blood flow would likely be informative. Attempts to assess these in humans
have been waveforms (Bush, 2001). In general, the extent of abnormal waveforms correlates with
severity of
hampered by several obstacles that include inaccessibility of the placenta, the
complexity of its fetal involvement (Ghidini, 2008; Groom, 2009).
venous effluent, and the need for radioisotopes or invasive techniques. PREDICTION AND PREVENTION
Measurement of uterine artery blood flow velocity has been used to estimate Prediction
resistance to
uteroplacental blood flow (Chap. 17, p. 345). Vascular resistance is estimated by Measurement during early pregnancyor across pregnancyof various biological,
comparing arterial biochemical, and
systolic and diastolic velocity waveforms. By the completion of placentation, biophysical markers implicated in preeclampsia syndrome pathophysiology has been
impedance to uterine proposed to
artery blood flow is markedly decreased, but with abnormal placentation, abnormally predict its development. Attempts have been made to identify early markers of faulty
high resistance placentation,
persists (Everett, 2012; Ghidini, 2008; Napolitano, 2012). Earlier studies were done to impaired placental perfusion, endothelial cell activation and dysfunction, and activation
assess this by of
measuring peak systolic:diastolic velocity ratios from uterine and umbilical arteries in coagulation. For the most, these have resulted in testing strategies with poor
preeclamptic sensitivity and with poor
pregnancies. The results were interpreted as showing that in some cases, but certainly positive-predictive value for preeclampsia (Conde-Agudelo, 2014; Lindheimer, 2008b;
not all, there Odibo,
was increased resistance (Fleischer, 1986; Trudinger, 1990). 2013). Currently, no screening tests are predictably reliable, valid, and economical
Another Doppler waveformuterine artery notchinghas been reported to be (Kleinrouweler,
associated with 2012). There are, however, combinations of tests, some yet to be adequately
increased risks for preeclampsia or fetal-growth restriction (Groom, 2009). In the evaluated, that may be
MFMU Network promising (Dugoff, 2013; Kuc, 2011; Navaratnam, 2013; Olsen, 2012).
study reported by Myatt and colleagues (2012a), however, notching had a low The list of predictive factors evaluated during the past three decades is legion.
predictive value Although most have
except for early-onset severe disease. been evaluated in the first half of pregnancy, some have been tested as predictors of
Matijevic and Johnson (1999) measured resistance in uterine spiral arteries. severity in the
Impedance was third trimester (Chaiworapongsa, 2013; Mosimann, 2013; Rana, 2012). Others have
higher in peripheral than in central vesselsa so-called ring-like distribution. Mean been used to
resistance was forecast recurrent preeclampsia (Demers, 2014). Some of these tests are listed in
higher in all women with preeclampsia compared with that in normotensive controls. Table 40-4, which
Ong and is by no means all inclusive. Conde-Agudelo and coworkers (2014) have recently
associates (2003) used MR imaging and other techniques to assess placental provided a
perfusion ex vivo in the thorough review of many of these testing strategies.
myometrial arteries removed from women with preeclampsia or fetal-growth restriction.
These
investigators confirmed that in both conditions myometrial arteries exhibited
endothelium-dependent
Rem Alfelor 2015
OBSTETRICS MODULE: Hypertension Page 12 of 12
Vous aimerez peut-être aussi
- OB Williams Chap 2 Maternal AnatomyDocument7 pagesOB Williams Chap 2 Maternal AnatomyRem Alfelor0% (1)
- Reviewer - LE4Document3 pagesReviewer - LE4Rem AlfelorPas encore d'évaluation
- Chap 8 Prenatal CareDocument9 pagesChap 8 Prenatal CareRem AlfelorPas encore d'évaluation
- POST-TEST Mock Written Diplomate ExaminationDocument62 pagesPOST-TEST Mock Written Diplomate ExaminationRem AlfelorPas encore d'évaluation
- Maternal Physiology Changes in PregnancyDocument5 pagesMaternal Physiology Changes in PregnancyRem AlfelorPas encore d'évaluation
- Gyne Prelims 2009Document10 pagesGyne Prelims 2009Rem AlfelorPas encore d'évaluation
- Chapter 2 Maternal AnatomyDocument9 pagesChapter 2 Maternal AnatomyRem Alfelor100% (2)
- OB Williams Chap 2 Maternal PhysiologyDocument9 pagesOB Williams Chap 2 Maternal PhysiologyRem Alfelor100% (2)
- Chapter 4 Maternal PhysiologyDocument12 pagesChapter 4 Maternal PhysiologyRem AlfelorPas encore d'évaluation
- Gyne 1st Long Exam 2009 ANSDocument3 pagesGyne 1st Long Exam 2009 ANSRem AlfelorPas encore d'évaluation
- Gyne 6th Long Exam ANSDocument4 pagesGyne 6th Long Exam ANSRem AlfelorPas encore d'évaluation
- Im Nephro ExamDocument4 pagesIm Nephro ExamRem AlfelorPas encore d'évaluation
- Chapter 3 Congenital Genitourinary AbnormalitiesDocument4 pagesChapter 3 Congenital Genitourinary AbnormalitiesRem AlfelorPas encore d'évaluation
- Gyne 5 Long ExamDocument3 pagesGyne 5 Long ExamRem Alfelor100% (1)
- Surgery 6th TCVSDocument3 pagesSurgery 6th TCVSRem AlfelorPas encore d'évaluation
- Gyne 3rd LEDocument4 pagesGyne 3rd LERem AlfelorPas encore d'évaluation
- Pedia MidtermDocument6 pagesPedia MidtermRem AlfelorPas encore d'évaluation
- Signs of Possible Eye Tumors in ChildrenDocument1 pageSigns of Possible Eye Tumors in ChildrenRem AlfelorPas encore d'évaluation
- Pedia QuizthyroidDocument2 pagesPedia QuizthyroidRem AlfelorPas encore d'évaluation
- Psychiatric History and Mental Status ExaminationDocument6 pagesPsychiatric History and Mental Status ExaminationRem AlfelorPas encore d'évaluation
- Case 04 - Prenatal CareDocument3 pagesCase 04 - Prenatal CareRem AlfelorPas encore d'évaluation
- PEDIA Nephroquiz2015Document4 pagesPEDIA Nephroquiz2015Rem AlfelorPas encore d'évaluation
- Alcohol Induced SchizophreniaDocument3 pagesAlcohol Induced SchizophreniaRem AlfelorPas encore d'évaluation
- HP CardDocument3 pagesHP CardRem AlfelorPas encore d'évaluation
- Pcap 2012Document1 pagePcap 2012Rem AlfelorPas encore d'évaluation
- Floors Census PDFDocument2 pagesFloors Census PDFRem AlfelorPas encore d'évaluation
- Pediatric Sarcoma Case PresentationDocument36 pagesPediatric Sarcoma Case PresentationRem AlfelorPas encore d'évaluation
- Community Medicine Cavite ReportDocument46 pagesCommunity Medicine Cavite ReportRem AlfelorPas encore d'évaluation
- Clinicopathological Conference 2Document23 pagesClinicopathological Conference 2Rem AlfelorPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Last Clean ExceptionDocument24 pagesLast Clean Exceptionbeom choiPas encore d'évaluation
- Olympics Notes by Yousuf Jalal - PDF Version 1Document13 pagesOlympics Notes by Yousuf Jalal - PDF Version 1saad jahangirPas encore d'évaluation
- Inventory Control Review of LiteratureDocument8 pagesInventory Control Review of Literatureaehupavkg100% (1)
- The European Journal of Applied Economics - Vol. 16 #2Document180 pagesThe European Journal of Applied Economics - Vol. 16 #2Aleksandar MihajlovićPas encore d'évaluation
- Data Sheet: Experiment 5: Factors Affecting Reaction RateDocument4 pagesData Sheet: Experiment 5: Factors Affecting Reaction Ratesmuyet lêPas encore d'évaluation
- Decision Maths 1 AlgorithmsDocument7 pagesDecision Maths 1 AlgorithmsNurul HafiqahPas encore d'évaluation
- Antenna VisualizationDocument4 pagesAntenna Visualizationashok_patil_1Pas encore d'évaluation
- DMDW Mod3@AzDOCUMENTS - inDocument56 pagesDMDW Mod3@AzDOCUMENTS - inRakesh JainPas encore d'évaluation
- IGCSE Chemistry Section 5 Lesson 3Document43 pagesIGCSE Chemistry Section 5 Lesson 3Bhawana SinghPas encore d'évaluation
- HCW22 PDFDocument4 pagesHCW22 PDFJerryPPas encore d'évaluation
- CMC Ready ReckonerxlsxDocument3 pagesCMC Ready ReckonerxlsxShalaniPas encore d'évaluation
- Account Statement From 30 Jul 2018 To 30 Jan 2019Document8 pagesAccount Statement From 30 Jul 2018 To 30 Jan 2019Bojpuri OfficialPas encore d'évaluation
- 17BCE0552 Java DA1 PDFDocument10 pages17BCE0552 Java DA1 PDFABHIMAYU JENAPas encore d'évaluation
- Biagioli Did Galileo Copy The TelescopeDocument28 pagesBiagioli Did Galileo Copy The TelescopeGregory HooPas encore d'évaluation
- Sysmex Xs-800i1000i Instructions For Use User's ManualDocument210 pagesSysmex Xs-800i1000i Instructions For Use User's ManualSean Chen67% (6)
- Evaluating Sources IB Style: Social 20ib Opvl NotesDocument7 pagesEvaluating Sources IB Style: Social 20ib Opvl NotesRobert ZhangPas encore d'évaluation
- Propiedades Grado 50 A572Document2 pagesPropiedades Grado 50 A572daniel moreno jassoPas encore d'évaluation
- Moor, The - Nature - Importance - and - Difficulty - of - Machine - EthicsDocument4 pagesMoor, The - Nature - Importance - and - Difficulty - of - Machine - EthicsIrene IturraldePas encore d'évaluation
- 8dd8 P2 Program Food MFG Final PublicDocument19 pages8dd8 P2 Program Food MFG Final PublicNemanja RadonjicPas encore d'évaluation
- Conv VersationDocument4 pagesConv VersationCharmane Barte-MatalaPas encore d'évaluation
- Yellowstone Food WebDocument4 pagesYellowstone Food WebAmsyidi AsmidaPas encore d'évaluation
- How Psychology Has Changed Over TimeDocument2 pagesHow Psychology Has Changed Over TimeMaedot HaddisPas encore d'évaluation
- Modified Syllabus of Control SystemDocument2 pagesModified Syllabus of Control SystemDigambar PatilPas encore d'évaluation
- Liebert PSP: Quick-Start Guide - 500VA/650VA, 230VDocument2 pagesLiebert PSP: Quick-Start Guide - 500VA/650VA, 230VsinoPas encore d'évaluation
- Music 7: Music of Lowlands of LuzonDocument14 pagesMusic 7: Music of Lowlands of LuzonGhia Cressida HernandezPas encore d'évaluation
- SD8B 3 Part3Document159 pagesSD8B 3 Part3dan1_sbPas encore d'évaluation
- Current Diagnosis and Therapy For Head and Neck MalignanciesDocument249 pagesCurrent Diagnosis and Therapy For Head and Neck MalignanciesMara TomaPas encore d'évaluation
- Archlinux 之 之 之 之 Lmap 攻 略 ( 攻 略 ( 攻 略 ( 攻 略 ( 1 、 环 境 准 备 ) 、 环 境 准 备 ) 、 环 境 准 备 ) 、 环 境 准 备 )Document16 pagesArchlinux 之 之 之 之 Lmap 攻 略 ( 攻 略 ( 攻 略 ( 攻 略 ( 1 、 环 境 准 备 ) 、 环 境 准 备 ) 、 环 境 准 备 ) 、 环 境 准 备 )Goh Ka WeePas encore d'évaluation
- Unit-1: Introduction: Question BankDocument12 pagesUnit-1: Introduction: Question BankAmit BharadwajPas encore d'évaluation