Académique Documents
Professionnel Documents
Culture Documents
Stout 2003
Transféré par
Gabriel Mercado InsignaresCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Stout 2003
Transféré par
Gabriel Mercado InsignaresDroits d'auteur :
Formats disponibles
Assessment
http://asm.sagepub.com/
Factor Analysis of the Frontal Systems Behavior Scale (FrSBe)
Julie C. Stout, Rebecca E. Ready, Janet Grace, Paul F. Malloy and Jane S. Paulsen
Assessment 2003 10: 79
DOI: 10.1177/1073191102250339
The online version of this article can be found at:
http://asm.sagepub.com/content/10/1/79
Published by:
http://www.sagepublications.com
Additional services and information for Assessment can be found at:
Email Alerts: http://asm.sagepub.com/cgi/alerts
Subscriptions: http://asm.sagepub.com/subscriptions
Reprints: http://www.sagepub.com/journalsReprints.nav
Permissions: http://www.sagepub.com/journalsPermissions.nav
Citations: http://asm.sagepub.com/content/10/1/79.refs.html
>> Version of Record - Mar 1, 2003
What is This?
Downloaded from asm.sagepub.com at Afyon Kocatepe Universitesi on May 12, 2014
ASSESSMENT Stout
ARTICLE
10.1177/1073191102250339
et al. / FrSBe FACTOR ANALYSIS
Factor Analysis of the Frontal
Systems Behavior Scale (FrSBe)
Julie C. Stout
Indiana University
Rebecca E. Ready
Janet Grace
Paul F. Malloy
Brown University
Jane S. Paulsen
University of Iowa
The Frontal Systems Behavior Scale (FrSBe), formerly called the Frontal Lobe Personality
Scale (FLOPS), is a brief behavior rating scale with demonstrated validity for the assess-
ment of behavior disturbances associated with damage to the frontal-subcortical brain cir-
cuits. The authors report an exploratory principal factor analysis of the FrSBeFamily
Version in a sample including 324 neurological patients and research participants, of which
about 63% were diagnosed with neurodegenerative diseases (Huntingtons, Parkinsons,
and Alzheimers diseases). The three-factor solution accounted for a modest level of vari-
ance (41%) and confirmed a factor structure consistent with the three subscales proposed on
the theoretical basis of the frontal systems. Most items (83%) from the FrSBe subscales of
Apathy, Disinhibition, and Executive Dysfunction loaded saliently on three corresponding
factors. The FrSBe factor structure supports its utility for assessing both the severity of the
three frontal syndromes in aggregate and separately.
Keywords: disinhibition; executive function; apathy; frontal
Damage to the prefrontal cortex is associated with a lies and on society at large. Neuropsychological methods
wide range of behavioral changes, including disinhibition, for assessing cognitive changes associated with frontal
irritability, apathy, decreased initiation, emotional lability, systems damage have been a focus of study for many
distractibility, irresponsibility, as well as problems with years, and neuropsychological tests are available that ef-
executive functions, working memory, attention, abstract fectively address many of these cognitive disturbances
thinking, mental flexibility, and recall (for a recent review, (Lezak, 1995; Spreen & Strauss, 1998). Fewer measures
see Lichter & Cummings, 2001b). These symptoms pose a are available to assess behavioral disturbances lying out-
threat to personal autonomy and increase burden on fami- side of the cognitive realm, although recent years have
Jessica Jones at Indiana University provided excellent assistance in preparation of this manuscript. We gratefully acknowledge the
contributions of Mary Wyman at Indiana University, who assisted in compiling data. We thank Drs. Guerry Peavy and David Salmon at
the University of California, San Diego Alzheimer Disease Research Center, for providing data from patients with Alzheimers disease.
Beth Turner and Laura Stierman provided assistance in data compilation at the University of Iowa. The project was supported by National
Institutes of HealthNational Institute of Aging AGO-5131 (UCSD-ADRC) and T32AG00214 (predoctoral fellowship to second au-
thor). Correspondence concerning this article should be addressed to Julie C. Stout, Department of Psychology, Indiana University, 1101
E. 10th St., Bloomington, IN 47405-7007; e-mail: jcstout@indiana.edu.
Assessment, Volume 10, No. 1, March 2003 79-85
DOI: 10.1177/1073191102250339
2003 Sage Publications
Downloaded from asm.sagepub.com at Afyon Kocatepe Universitesi on May 12, 2014
80 ASSESSMENT
seen an increase in the availability of such measures (the & Salloway, 2001; Paulsen et al., 1996, 2000; Zawacki
Neuropsychiatric Inventory, Cummings et al., 1994; the et al., 2002). The Family Version of the FrSBe has been
Frontal Systems Behavior Scale [FrSBe], formerly re- used in the majority of the reports, including the primary
ferred to as the Frontal Lobe Personality Scale [FLOPS], validity study of the FrSBe (Grace et al., 1999).
Grace, Stout, & Malloy, 1999; the Frontal Behavior In- The FrSBe has been shown to have high internal consis-
ventory, Kertesz, Davidson, & Fox, 1997; the Apathy tency reliability, and there is growing evidence for the
Evaluation Scale, Marin, Biedrzycki, & Firincioguliari, tests validity for assessing behavioral changes associated
1991). Accurate conceptualization and measurement of with frontal systems damage (Boyle, Grace, Zawacki, Ott,
frontal behavior disturbances are essential steps for de- & Stout, 2001; Grace et al., 1999). The clinical utility of
termining their prevalence and their impact on activities the instrument is indicated by the fact that it measures
of daily living. Furthermore, the precise measurement of characteristics that are at least partly independent of cog-
treatment efficacy depends on the availability of nitive dysfunction and thus is not redundant with cognitive
psychometrically sound scales for measuring specific be- measures (Paulsen et al., 1996; Stout, Wyman, Peavy, &
havioral disturbances. Salmon, 2001; Zawacki et al., 2002). Ratings on the FrSBe
Of the scales listed above, the FrSBe is of particular in- also are associated with important outcome criteria, such
terest for characterizing behavior disturbances related to as functional status (Norton et al., 2001; Stout et al., 2001;
frontal system dysfunction.1 The FrSBe is a behavior rat- Zawacki et al., 2002).
ing scale designed to provide a total frontal disturbance Evidence is beginning to accrue that the FrSBe
score and three subscale scores made up of items devel- subscales are differentially associated with clinical fea-
oped to assess particular behavioral disturbances. Apathy, tures. For example, the Apathy Subscale of the FrSBe was
disinhibition, and executive function were chosen by the more strongly related to activities of daily living in vascu-
scales authors following an extensive search of the clini- lar dementia (Zawacki et al., 2002) and mixed dementia
cal research literature that revealed these three categories groups (Norton et al., 2001). Furthermore, Ready,
of behavior as the most frequently cited behavioral distur- Stierman, and Paulsen (2001) reported evidence of eco-
bances associated with damage to the frontal lobes and logical validity for the various subscales in a healthy un-
frontal-subcortical brain circuitry. In fact, these three fron- dergraduate student sample; the Disinhibition Subscale
tal behavior syndromes have been linked to regional dis- showed differential relationship to engaging in risky and
turbances in frontal lobe function. Specifically, damage to aggressive behaviors (Ready et al., 2001). Sufficient data
the dorsolateral prefrontal cortex has been linked to prob- from neurological patients and research participants has
lems with executive function, the mesial frontal and ante- now accumulated so that it is possible to conduct a factor
rior cingulate cortex with apathy and akinesia, and the analysis of the scale items and to determine if the factor
orbitofrontal cortex with disinhibited behavior and emo- structure of the instrument corresponds to the hypothe-
tional outbursts. These behavioral disturbances are found sized three-subscale structure. This is an essential step for
in individuals who have frontal lobe damage and in indi- determining whether the psychometric features of the
viduals whose damage is at the subcortical levels in brain scale support the intended use of the measure for assessing
structures known to be linked in a regionally specific fash- overall frontal behavior disturbance, as well as differential
ion to frontal cortex (Levin, Eisenberg, & Benton, 1991; presentation of the three frontal syndromes of apathy,
Lhermitte, Pillon, & Serdaru, 1986; Lichter & Cummings, disinhibition, and executive dysfunction.
2001a; Mega & Cummings, 1994; Stuss & Benson, 1986). The goal of this study was to determine whether the fac-
The FrSBe is a 46-item behavior rating scale (Grace & tor structure of the FrSBe supports the subscale structure
Malloy, 2001). Parallel forms exist for use by a family of the scale. For this purpose, we evaluated data from a
member or close caregiver (Family Version), a staff mem- mixed group of neurological patients and research partici-
ber caring for a patient in a professional setting (Staff Ver- pants regarding the frequency ratings of recent behaviors
sion), and for self-ratings by the patient/subject (Self on the FrSBeFamily Version. The study sample was de-
Version). The FrSBe is designed to allow ratings to be signed to include a wide range of neurological disorders
made of recent behavior, and for comparison, an optional that is representative of those for whom the scale will be
retrospective rating of behavior prior to accident, injury, or used in clinical and research settings. Diagnostic heteroge-
treatment. The majority of the studies that have used the neity in the sample ensured that a wide and comprehensive
FrSBe have focused on ratings only of recent (post- range of FrSBe item scores would be represented in the
accident, postinjury, or posttreatment) behavior (Hulver- data, as is recommended for optimal factor analysis
shorn, Stout, Paulsen, & Siemers, 1999; Norton, Malloy, (Gorsuch, 1997; Reise, Waller, & Comrey, 2000).
Downloaded from asm.sagepub.com at Afyon Kocatepe Universitesi on May 12, 2014
Stout et al. / FrSBe FACTOR ANALYSIS 81
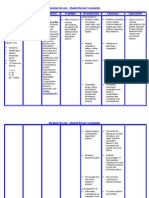
TABLE 1
Descriptive Statistics for Age, Education, and FrSBe Scales by Diagnosis (N = 324)
AD HD PD FLD Dem, NOS HI CVA
M SD M SD M SD M SD M SD M SD M SD
Age 75.4 7.8 46.5 12.2 68.2 7.8 69.9 8.8 70.7 11.8 41.8 17.5 60.0 19.2
Education 13.1 3.6 13.1 2.3 14.0 2.8 12.5 2.6 11.4 3.7 12.6 3.2
Apathy 41.6 10.7 39.0 11.8 34.8 10.7 48.6 7.9 35.6 12.2 32.3 10.3 36.0 11.5
Disinhibition 27.4 8.9 29.1 9.0 23.8 7.5 34.5 11.0 27.7 9.8 29.5 7.6 29.2 10.3
Executive dysfunction 55.9 12.9 46.1 14.3 40.0 11.1 57.8 13.5 48.8 16.3 41.3 10.4 44.3 15.6
Total 124.9 27.9 114.2 31.0 98.63 23.3 140.9 27.0 112.1 34.6 103.1 25.5 109.6 33.6
N 76 91 38 13 27 29 50
NOTE: AD = probable Alzheimers disease; HD = Huntingtons disease; PD = Parkinsons disease; FLD = frontal lobe dementia; Dem, NOS = dementia,
not otherwise specified, Lewy Body Variant, vascular dementia, traumatic dementia, dementia due to multiple sclerosis; HI = head injury; CVA = cerebral
vascular accident.
METHOD ticipants gave institutionally approved informed consent.
Some of these data have appeared in prior publications
Sample (Grace et al., 1999; Hulvershorn et al., 1999; Paulsen et al.,
1996; Stout et al., 2001).
The sample consisted of 324 neurological outpatients
and research participants from eight diagnostic categories Instrument
(Table 1). Alzheimers disease was diagnosed according to
The FrSBe is a 46-item behavior rating scale that mea-
National Institutes of Neurological and Communicative
sures behaviors that are clinically and theoretically linked
Disorders and Stroke criteria (McKhann et al., 1984). The
to frontal lobe damage. The items on the scale were devel-
diagnosis of Huntington Disease was made by a senior
oped from a list of descriptors used in the neuropsycho-
staff neurologist on the basis of chorea as screened on the
logical, neurological, and psychiatric literatures. Next, a
Unified Huntingtons Disease Rating Scale (Huntington
panel of experts reviewed the items, and a set of items
Study Group, 1996) and the presence of a confirmed fam-
judged to be redundant or poorly worded were eliminated.
ily history of Huntingtons disease. Parkinsons disease
Items were then assigned to three subscales. Q-sort of
was diagnosed using a clinical evaluation to document the
these items by an expert on frontal-subcortical circuits and
presence of symptoms (i.e., stooped posture, bradykinesia,
behavior revealed an acceptable level of agreement ( =
resting tremor, muscular rigidity) and to rule out other pos-
.77, p < .001). Items from the scale were worded to assess
sible diagnoses (Bannister, 1992). Hoehn and Yahr (1967)
the frequency of problems related to three behavioral do-
criteria were used to document the severity of the disorder.
mains: apathy/akinesia (Scale A, 14 items), disinhibition/
Dementia patients with prominent changes in behavior
emotional dysregulation (Scale D, 15 items), and execu-
and personality at the onset of dementia and with major
tive dysfunction (Scale E, 17 items). For all participants,
frontal lobe impairments on neuropsychological testing
ratings of recent behavior were obtained from an infor-
and single photon emission computed tomography
mant (i.e., close family member or caregiver) using the fol-
(SPECT) were diagnosed with frontotemporal dementia.
lowing instructions:
Dementia due to Lewy Bodies was diagnosed in dementia
patients with at least two of the following three character-
Below is a list of phrases used to describe someone.
istics: visual hallucinations, parkinsonian symptoms, or How well does each of these descriptions character-
fluctuating cognitive ability. Patients with dementia and an ize the person you were asked to evaluate? Please
Hachinski ischemia score greater than or equal to 7 rate these items according to the persons behavior
(Hachinski et al., 1975) were diagnosed with vascular de- in the past two weeks. Place a number in each box
mentia. These data were obtained in clinical research set- that corresponds to your rating.
tings at the Indiana University Department of Psychology,
the Brown University Department of Psychiatry and Hu- Below these instructions and reprinted at the top of each
man Behavior, the University of California San Diego Alz- page was a box containing the list of possible ratings with
heimer Disease Research Center and Genetically descriptors. For the first 35 items, informants were asked
Handicapped Persons Program, and the University of to rate each item according to the following 5-point scale:
Iowa Departments of Psychiatry and Neurology. All par- 1 = almost never, 2 = seldom, 3 = sometimes, 4 = frequently,
Downloaded from asm.sagepub.com at Afyon Kocatepe Universitesi on May 12, 2014
82 ASSESSMENT
and 5 = almost always. The 5-point scale on the last page TABLE 2
(containing the final 11 positively stated scale items) was Pattern Matrix From Principal
reversed so that 1 = almost always, 2 = frequently, 3 = Factor Analysis With Oblique Rotation
sometimes, 4 = seldom, and 5 = almost never, and a rating to Simple Structure (N = 324)
scheme was maintained such that higher ratings corre- A Priori Factor 1 Factor 2 Factor 3
sponded to relatively more abnormal behavior. Item Abbreviation (number) Scale E D A
Shows poor judgment (19) E .73 .04 .04
Data Analysis Repeats same mistakes (7) E .70 .00 .08
Mixes up a sequence (5) E .67 .00 .00
We conducted exploratory principal component factor Is disorganized (15) E .65 .01 .13
analysis with iterated communalities on the 46 FrSBe Forgets to do things (25) E .57 .02 .11
Does not finish things (23) A .57 .02 .21
items. A three-factor solution was specified based on the
Is inflexible (26) E .54 .02 .11
theoretical conceptualization of the scale. Because we ex- Unaware of problems (13) E .54 .03 .06
pected the three factors to be correlated, as typically oc- Repeats certain actions (3) E .54 .03 .06
curs when the factors are components of a more general Says one thing, does another (22) E .53 .24 .07
a
construct (e.g., frontal system dysfunction), we used an Thinks things through (35) E .53 .00 .17
a
Pays attention (34) E .52 .11 .16
oblique rotation to simple structure as recommended by a
Is able to plan ahead (37) E .47 .06 .39
Reise and colleagues (2000). In this rotation, equal weight Cannot do two things at once (17) E .47 .01 .27
was given to the two criteria that enter into the oblique ro- Laughs or cries too easily (6)
b
D .37 .21 .10
b
tation, namely, orthogonal and correlated factors. Makes up stories (20) E .36 .25 .05
The fit of the resulting factor structure was evaluated Does embarrassing things (10) D .20 .67 .05
Makes sexual comments (9) D .05 .64 .02
using the following criteria: eigenvalues greater than or
Swears (32) D .03 .51 .02
equal to 1, scree test, and the interpretability of the factors Does things impulsively (4) D .33 .49 .17
with respect to the specific subscales proposed by the au- Is overly silly (30) D .30 .49 .10
a
thors in developing the FrSBe. We used a value greater Acts appropriately (45) D .18 .48 .14
than .40 as a criterion to define a salient factor loading as Talks out of turn (18) D .39 .47 .22
Neglects personal hygiene (11) A .02 .45 .43
recommended by Gorsuch (1997). A sample size of at a
Gets along with others (44) D .06 .42 .14
least 300 is recommended to identify item loadings of this b
Does risky things (28) D .08 .37 .03
magnitude in item-level data (Gorsuch, 1997). This rela- b
Is easily angered (2) D .24 .34 .06
b
tively large sample size also is recommended to ensure that Is hyperactive (12) D .23 .34 .16
b
the factors will emerge from error variance associated Trouble with the law (27) D .02 .27 .07
b
Loss of taste or smell (31) D .10 .24 .13
item-level data, which are known (in comparison to scales)
Lacks energy (29) A .25 .11 .61
to have relatively low intercorrelations, low reliability, Lost interest in things (21) A .24 .02 .60
varying distributions, and noncontinuous response for- Does nothing (14) A .31 .07 .60
a
mats (Gorsuch, 1997). Gets involved spontaneously (41) A .23 .14 .59
a
Starts conversations (46) A .04 .06 .51
a
Does things without reminders (42) A .22 .03 .50
Unconcerned and unresponsive (24) A .18 .06 .48
RESULTS Lacks initiative, motivation (8) A .40 .05 .48
a
Cares about appearance (39) A .04 .29 .46
a
Results of the factor analytic study supported the ex- Is sensitive to others (43) D .07 .22 .42
a, b
traction of three factors, which were consistent with the Benefits from feedback (40) E .22 .20 .37
a, b
Is interested in sex (38) A .10 .14 .36
subscales designed by the authors of the FrSBe. Below we b
Incontinence (16) A .12 .32 .36
describe the primary factor analysis results, followed by Uses memory strategies (36)
a, b
E .22 .09 .35
item-loading characteristics. a, b
Apologizes for misbehavior (33) E .04 .15 .30
b
Speaks only when spoken to (1) A .10 .07 .30
Primary Factor Analysis NOTE: E = Executive Dysfunction; A = Apathy; D = Disinhibition. Fac-
tor loadings of .40 or greater are in italics.
The three-factor solution accounted for 40.7% of the a. Reverse-keyed item.
b. Items with no salient loading on any of the three factors.
common variance among the 46 items (see Table 2). Three
lines of evidence supported the extraction of the three fac-
tors. First, the eigenvalues for the factors were all greater extracting factors beyond three in regard to accounting for
than 1. Second, the factors were above the elbow on the additional variance. Third, items from each of the three
scree plot, indicating significantly diminishing returns for FrSBe subscales tended to have primary loadings on the
Downloaded from asm.sagepub.com at Afyon Kocatepe Universitesi on May 12, 2014
Stout et al. / FrSBe FACTOR ANALYSIS 83
same factor, and thus, it was possible to make substantive the subscale to which they were theoretically assigned
interpretations of the factors based on item loadings. were Neglects personal hygiene from the Apathy sub-
The first factor, which we labeled Executive Dysfunc- scale, which cross-loaded on the Apathy and Disinhibition
tion, accounted for 29.1% of the variance. Twelve of the factors, and Has difficulty starting an activity, lacks ini-
original 16 Executive Dysfunction subscale items as well tiative, motivation, which cross-loaded on the Apathy and
as 1 item developed for the Apathy subscale had salient Executive Dysfunction factors.
loadings on the Executive Dysfunction factor. The second
factor, which we labeled Disinhibition, accounted for
7.2% of the common variance. It included salient loadings DISCUSSION
by 8 of the original 15 items from the Disinhibition
subscale as well as 1 item from the Apathy subscale. The The exploratory principal factor analysis of the FrSBe
third factor, which we labeled Apathy, accounted for 4.4% confirmed a factor structure consistent with the three
of the common variance, and 9 of the 15 items proposed in subscales that were proposed on the basis of frontal sys-
the original Apathy subscale loaded saliently on this fac- tems behavioral theory. That is, items from the individual
tor, as did one item from the Disinhibition subscale. FrSBe subscales tended to load together on each of three
Consistent with the notion that the three factors were corresponding factors, Apathy, Disinhibition, and Execu-
related to a similar underlying construct (i.e., frontal sys- tive Dysfunction. The Executive Dysfunction factor ac-
tems abnormality), the three factors were significantly (p < counted for the largest portion of the variance, but the
.01) correlated (Executive Dysfunction with Disinhibition Apathy and Disinhibition factors also emerged as impor-
r = .43, Executive Dysfunction with Apathy r = .43, tant in accounting for the patterns of responses. Thus, the
Disinhibition with Apathy r = .22). Such correlations can factor structure, in conjunction with the previous studies
be troubling when they are a result of a high level of item that have indicated construct validity of the scale, suggests
cross-loadings, because this indicates that items in the that the FrSBe is useful for assessing the severity of the
scale have such a high degree of overlap as to be ineffective three frontal syndromes in aggregate, as well as for assess-
for distinguishing the constructs targeted by the factors. ing these syndromes separately. Additional evidence of
However, only 2 of the 46 items had salient cross-loadings subscale utility has been obtained in clinical and research
as defined by .40 or greater, so item cross-loadings do settings. For example, in several studies, FrSBe subscales
not account for a significant portion of the factor were related to measures of independence in activities of
intercorrelations. daily living (Norton et al., 2001; Stout et al., 2001;
Zawacki et al., 2002).
Item Loading Characteristics The FrSBe has significant intercorrelations between
the factors, ranging from r = .22 to r = .43, a finding that is
Using the criterion of > .40 to indicate salient loading, expected when the constructs underlying the subscales are
29 of the 46 FrSBe items performed as predicted, loading related to a broader construct such as behavioral character-
saliently and solely on the expected factor. An additional 9 istics of frontal system dysfunction. Despite the interrela-
items showed strongest loadings on the expected factor, tionships, a significant level of unshared variance remains
but at a value lower than the criterion of .40. Thus, 38 of the in the factors, supporting the use of FrSBe subscales for
original 46 items loaded on the expected factor in the fac- differentiating specific patterns of behavior disturbances
tor analysis. For the remaining 8 items, 6 had their highest in individuals with frontal systems damage. Also of note,
loading on a factor other than the one corresponding only about 41% of the variance was accounted for by the
subscale to which they were assigned, and 2 had salient factor structure of the FrSBe. Thus, there is a substantial
cross-loadings both on the factor corresponding to their amount of variance in FrSBe scores that is also independ-
subscale assignment and an additional subscale (see Ta- ent of the three factors. Further studies will be necessary to
ble 2). determine whether that variance contributes to the mea-
Of the six items that loaded most highly on factors other surement of more general frontal syndromes.
than the one expected, only two had salient loadings, in- Only two of the items in the FrSBe cross-loaded
cluding Starts things but fails to finish them, which was strongly on more than one factor. Although these items
assigned to the Apathy subscale but which loaded saliently were written to measure part of a single construct, it ap-
on the Executive Dysfunction factor, and Is sensitive to pears that more than one process underlies the behaviors
the needs of other people, which was assigned to the tapped by these two items. Relatively more of the items
Disinhibition subscale but instead loaded saliently on the performed below optimal levels in the factor analysis be-
Executive Dysfunction factor and the Apathy factor, re- cause they loaded less saliently (less than .40) on any of the
spectively. The two items that failed to show specificity to three factors (17 items) or loaded saliently only on a factor
Downloaded from asm.sagepub.com at Afyon Kocatepe Universitesi on May 12, 2014
84 ASSESSMENT
other than the one corresponding to the subscale for which points to the need for additional studies to determine the
they were proposed (2 items). There are several possible predictive validity of the subscales.
reasons for such findings. For example, a few items had
very low endorsement rates and restricted variance in our
sample (e.g., trouble with the law, does risky things, un- NOTE
concerned about incontinence), which may account for 1. Throughout the article, we refer to the scale as the Frontal Systems
their failure to covary with other items in a manner that Behavior Scale (FrSBe). In publications prior to this, the scale has been
would have resulted in a salient factor loading. Although consistently referred to as the Frontal Lobe Personality Scale (FLOPS).
their psychometric properties are not ideal, they may be
useful for clinical purposes. For example, trouble with
the law is infrequently endorsed and could alert a clini- REFERENCES
cian to the potential involvement of the legal process in the
patients outcome. Similarly, incontinence is a particularly Bannister, Sir Roger. (1992). Brain & Bannisters clinical neurology. Ox-
burdensome problem for caregivers and is associated with ford, UK: Oxford University Press.
higher rates of nursing home placement. Boyle, P. A., Grace, J., Zawacki, T. M., Ott, B. R., & Stout, J. C. (2001).
Frontal behavior change in neurodegenerative and acute neurologi-
Ratings may differ depending on features of the rater cal disorders. Manuscript submitted for publication.
and his or her relationship with the person being rated. In Cummings, J., Mega, M., Gray, K., Rosenberg-Thompson, S., Carusi, D.,
this sample, we did not systematically classify the type and & Gornbein, J. (1994). The Neuropsychiatric Inventory: Comprehen-
extent of the relationships between raters and the individu- sive assessment of psychopathology in dementia. Neurology, 44(12),
2308-2314.
als they rated. However, all raters considered themselves Finch, J. F., & West, F. G. (1997). The investigation of personality struc-
to be close family members or caregivers, and the majority ture: Statistical models. Journal of Research in Personality, 31(4),
were cohabiting with the person whom they rated. None- 439-485.
Gorsuch, R. L. (1997). Exploratory factor analysis: Its role in item analy-
theless, some items may be too difficult for the caregiver or sis. Journal of Personality Assessment, 68, 532-560.
family member to rate because the items require informa- Grace, J., & Malloy, P. F. (2001). Frontal Systems Behavior Scale: Pro-
tion about the patients experience that is typically avail- fessional manual. Lutz, FL: Psychological Assessment Resources,
able only on self-reflection rather than by observation by Inc.
Grace, J., Stout, J., & Malloy, P. (1999). Assessing frontal behavior syn-
another individual (i.e., interest in sex, food has no taste or dromes with the Frontal Lobe Personality Scale. Assessment, 6(3),
smell, uses memory strategies). Finally, some items may 269-284.
have been ambiguous or confusing (i.e., apologizes for Hachinski, V. C., Iliff, L. D., Zilhka, E., Du Boulay, G. H., McAllister,
misbehavior), leading respondents to interpret the items V. L., Marshall, J., et al. (1975). Cerebral blood flow in dementia. Ar-
chives of Neurology, 32(9), 632-637.
differently than intended by the authors of the FrSBe. In Hoehn, M. M., & Yahr, M. D. (1967). Parkinsonism: Onset, progression
fact, idiosyncratic interpretation of items has been identi- and mortality. Neurology, 17, 427-442.
fied as a major source of discrepancy between self and in- Hulvershorn, L. A., Stout, J. C., Paulsen, J. S., & Siemers, E. (1999).
formant personality ratings (McCrae, Stone, Fagan, & Frontal neuropsychiatric syndromes in Huntingtons disease and Par-
kinsons disease [Abstract]. Archives of Clinical Neuropsychology,
Costa, 1998). For several of the remaining items that did 14(1), 133.
not load highly on any of the factors, there does not appear Huntington Study Group. (1996). Unified Huntingtons Disease Rating
to be any systematic reason for their failure to load sa- Scale: Reliability and consistency. Movement Disorders, 11, 136-
142.
liently on their corresponding factor. These items simply Kertesz, A., Davidson, W., & Fox, H. (1997). Frontal Behavioral Inven-
may not have adequately captured the construct that they tory: Diagnostic criteria for frontal lobe dementia. Canadian Journal
were written to assess. of Neurological Sciences, 24, 29-36.
In summary, the results from the present study are con- Levin, J., Eisenberg, J., & Benton, A. (1991). Frontal lobe function and
dysfunction. New York: Oxford University Press.
sistent with the use of the FrSBe subscales in the assess- Lezak, M. D. (1995). Neuropsychological assessment (3rd ed.). New
ment of behavioral disturbances associated with York: Oxford University Press.
neurological dysfunction. In addition, the item character- Lhermitte, F., Pillon, B., & Serdaru, M. (1986). Human autonomy and the
istics revealed by the factor analysis provide initial indica- frontal lobes. Part I: Imitation and utilization behavior: A
neuropsychological study of 75 patients. Annals of Neurology, 19(4),
tions regarding which items perform best in terms of the 326-334.
goals of the FrSBe. This exploratory factor analysis re- Lichter, D. G., & Cummings, J. L. (Eds.). (2001a). Frontal-subcortical
quires replication with confirmatory factor analysis to circuits in psychiatric and neurological disorders. New York:
Guilford.
avoid capitalization on chance findings (Finch & West,
Lichter, D. G., & Cummings, J. L. (2001b). Introduction and overview. In
1997). Such further studies are essential prior to any modi- D. G. Lichter & J. L. Cummings (Eds.), Frontal-subcortical circuits
fications in the use of the FrSBe, such as eliminating items. in psychiatric and neurological disorders (pp. 1-43). New York:
The finding of the three factors provides psychometric Guilford.
support for the subscale structure of the FrSBe and also
Downloaded from asm.sagepub.com at Afyon Kocatepe Universitesi on May 12, 2014
Stout et al. / FrSBe FACTOR ANALYSIS 85
Marin, R. S., Biedrzycki, R. C., & Firincioguliari, S. (1991). Reliability Stout, J. C., Wyman, M. F., Peavy, G. M., & Salmon, D. P. (2001). Frontal
and validity of the Apathy Evaluation Scale. Psychiatry Res, 38, 143- neuropsychiatric symptoms in probable Alzheimers disease. Manu-
162. script submitted for publication.
McCrae, R. R., Stone, S. V., Fagan, P. J., & Costa, P. T., Jr. (1998). Iden- Stuss, D., & Benson, D. (1986). The frontal lobes. New York: Raven.
tifying causes of disagreement between self-reports and spouse rat- Zawacki, T. M., Grace, J., Paul, R. H., Moser, D. J., Ott, B. R., Gordon,
ings of personality. Journal of Personality, 66, 285-313. N., et al. (2002). Impact of apathy on the prediction of functional abil-
McKhann, G., Drachman, D., Folstein, M., Katzman, R., Price, D., & ities of vascular dementia patients. Journal of Neuropsychiatry and
Stadlan, E. M. (1984). Clinical diagnosis of Alzheimers disease: Re- Clinical Neuroscience, 14, 296-302.
port of the NINCDS-ADRDA work group under the auspices of De-
partment of Health and Human Services Task Force on Alzheimers.
Neurology, 34, 939-944. Julie C. Stout, Ph.D., is an assistant professor at Indiana Univer-
Mega, M., & Cummings, J. (1994). Frontal-subcortical circuits and neu- sity. Her research interests are in the area of basal ganglia and
ropsychiatric disorders. Journal of Neuropsychiatry and Clinical frontal diseases, especially Parkinsons and Huntingtons, and in
Neurosciences, 6(4), 38-70. drug abuse.
Norton, L., Malloy, P. F., & Salloway, S. (2001). The impact of behavioral
symptomology on activities of daily living in patients with dementia. Rebecca E. Ready, Ph.D., is a research fellow at Brown Univer-
American Journal of Geriatric Psychology, 9(1), 41-48.
sity. Her research focuses on neuropsychology and caregiving in
Paulsen, J. S., Ready, R. E., Stout, J. C., Salmon, D. P., Thal, L. J.,
Grant, I., & Jeste, D. V. (2000). Neurobehaviors and psychotic symp- dementia.
toms in Alzheimers disease. Journal of the International Neuro-
psychological Society, 6, 815-820. Janet Grace, Ph.D., is an associate professor at Brown Univer-
Paulsen, J. S., Stout, J. C., DeLaPena, J., Romero, R., Tawfik-Reedy, Z., sity. Her research interests include clinical neuropsychology, re-
Swenson, M. R., et al. (1996). Frontal behavioral syndromes in corti- habilitation, and frontal behavior disturbances.
cal and subcortical dementia. Assessment, 3(3), 327-337.
Ready, R. E., Stierman, L., & Paulsen, J. (2001). Ecological validity of Paul F. Malloy, Ph.D., is an associate professor at Brown Uni-
neuropsychological and personality measures of executive functions. versity. His research interests are in the field of frontal-
The Clinical Neuropsychologist, 15(3), 314-324.
subcortical brain systems, neuropsychology, and obsessive-
Reise, S., Waller, N., & Comrey, A. (2000). Factor analysis and scale re-
vision. Psychological Assessment, 12(3), 287-297. compulsive disorder.
Spreen, O., & Strauss, E. (1998). A compendium of neuropsychological
tests: Administration, norms, and commentary (2nd ed.). New York:
Jane S. Paulsen, Ph.D., is a professor at the University of Iowa.
Oxford University Press. Her research focuses on frontal-subcortical brain systems, Hun-
tingtons disease, and schizophrenia.
Downloaded from asm.sagepub.com at Afyon Kocatepe Universitesi on May 12, 2014
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Initial Clinical Assessment FormDocument10 pagesInitial Clinical Assessment FormOchee De Guzman CorpusPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- QBANKDocument38 pagesQBANKsbarolia2673% (11)
- Surgery QuestionsDocument312 pagesSurgery Questionsmonaliza7100% (9)
- Review Notes in Infection Control - NCLEXDocument1 pageReview Notes in Infection Control - NCLEXwyndz100% (10)
- NURSING CARE PLAN - Liver CirrhosisDocument2 pagesNURSING CARE PLAN - Liver Cirrhosisderic100% (27)
- Landau 1999Document10 pagesLandau 1999Gabriel Mercado InsignaresPas encore d'évaluation
- The Many Faces of Impulsivity PDFDocument8 pagesThe Many Faces of Impulsivity PDFGabriel Mercado InsignaresPas encore d'évaluation
- The Forms and Functions of Impulsive Actions: Implications For Behavioral Assessment and TherapyDocument19 pagesThe Forms and Functions of Impulsive Actions: Implications For Behavioral Assessment and TherapyGabriel Mercado InsignaresPas encore d'évaluation
- NIH Public Access: Behavioral Measures of Impulsivity and The LawDocument16 pagesNIH Public Access: Behavioral Measures of Impulsivity and The LawGabriel Mercado InsignaresPas encore d'évaluation
- 1088767908324430Document15 pages1088767908324430Gabriel Mercado InsignaresPas encore d'évaluation
- Watkins 1992Document53 pagesWatkins 1992Gabriel Mercado InsignaresPas encore d'évaluation
- Bartels 14 PHDDocument222 pagesBartels 14 PHDGabriel Mercado InsignaresPas encore d'évaluation
- Caluschi MarianaDocument5 pagesCaluschi MarianaGabriel Mercado InsignaresPas encore d'évaluation
- The Endocrinopathies of Anorexia NervosaDocument13 pagesThe Endocrinopathies of Anorexia NervosaCarla MesquitaPas encore d'évaluation
- 2004 4050B1 14 Fosinopril Label PedsDocument23 pages2004 4050B1 14 Fosinopril Label PedsМаргарет ВејдPas encore d'évaluation
- Common Causes of BlindnessDocument58 pagesCommon Causes of BlindnesskaunaPas encore d'évaluation
- Gestational Diabetes Mellitus: A Harbinger of The Vicious Cycle of DiabetesDocument21 pagesGestational Diabetes Mellitus: A Harbinger of The Vicious Cycle of DiabetesEmma Lyn SantosPas encore d'évaluation
- Unit 11 Role of Fungi in Human Welfare: ObjectivesDocument12 pagesUnit 11 Role of Fungi in Human Welfare: Objectivessivaram888Pas encore d'évaluation
- Common Pulmonary Diseases: Emmanuel R. Kasilag, MD, FPCP, FPCCPDocument74 pagesCommon Pulmonary Diseases: Emmanuel R. Kasilag, MD, FPCP, FPCCPDivine Grace FernandezPas encore d'évaluation
- Jurnal TinitusDocument14 pagesJurnal TinitusAndriyani YaniPas encore d'évaluation
- Castle Connolly Graduate Board Review SeriesDocument63 pagesCastle Connolly Graduate Board Review SeriesCCGMPPas encore d'évaluation
- Atkinson R L - Weight CyclingDocument7 pagesAtkinson R L - Weight CyclingmaddafackerPas encore d'évaluation
- DesenteryDocument3 pagesDesenteryAby Gift AnnPas encore d'évaluation
- The Mental and Sexual DisordersDocument5 pagesThe Mental and Sexual DisordersGrace BrionesPas encore d'évaluation
- Approach To The Infant or Child With Nausea and Vomiting - UpToDateDocument47 pagesApproach To The Infant or Child With Nausea and Vomiting - UpToDatemayteveronica1000Pas encore d'évaluation
- Lung FlukesDocument23 pagesLung FlukesGelli LebinPas encore d'évaluation
- Chronic Myelogenous Leukemia (CML) - Causes, Symptoms, TreatmentDocument10 pagesChronic Myelogenous Leukemia (CML) - Causes, Symptoms, Treatmentnurul auliaPas encore d'évaluation
- Diabetes Flow ChartDocument8 pagesDiabetes Flow ChartNicky ChhajwaniPas encore d'évaluation
- HistoryDocument3 pagesHistoryJennesse May Guiao IbayPas encore d'évaluation
- Racelis Vs United Philippine LinesDocument1 pageRacelis Vs United Philippine LinesEarvin Joseph BaracePas encore d'évaluation
- StomatitisDocument3 pagesStomatitiswidya RDPas encore d'évaluation
- Care For Your Heart While You SleepDocument6 pagesCare For Your Heart While You SleepkrishnaPas encore d'évaluation
- Radiology DVTDocument90 pagesRadiology DVTDhruv KushwahaPas encore d'évaluation
- Proceedings of BUU Conference 2012Document693 pagesProceedings of BUU Conference 2012Preecha SakarungPas encore d'évaluation
- Esmr 2Document1 pageEsmr 2Martina FitriaPas encore d'évaluation
- Appendicitis (History & Examination)Document6 pagesAppendicitis (History & Examination)Doctor Saleem Rehman75% (4)
- Undo It!: How Simple Lifestyle Changes Can Reverse Most Chronic Diseases - Dean Ornish M.D.Document5 pagesUndo It!: How Simple Lifestyle Changes Can Reverse Most Chronic Diseases - Dean Ornish M.D.besahahu7% (15)
- Onychauxis or HypertrophyDocument3 pagesOnychauxis or HypertrophyKathleen BazarPas encore d'évaluation
- Covered Diagnoses & Crosswalk of DSM-IV Codes To ICD-9-CM CodesDocument12 pagesCovered Diagnoses & Crosswalk of DSM-IV Codes To ICD-9-CM CodesAnonymous 1EQutBPas encore d'évaluation