Académique Documents
Professionnel Documents
Culture Documents
10 CNS Unlocked
Transféré par
Soodn Kang SoodnCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
10 CNS Unlocked
Transféré par
Soodn Kang SoodnDroits d'auteur :
Formats disponibles
Pharmacology of The C.N.S.
2011/2012
Pharmacology of C.N.S.
I-ANALGESICS
Definition: analgesics are drugs that relieve pain without loss of consciousness or loss of
other sensations (this is unlike general anaesthetics which relieve pain and other sensations
and cause loss of consciousness).
Classification: analgesics are classified into:
1. Central analgesics (proper analgesics):
They relieve pain by acting on CNS; and are further subdivided into:
a) Opioid analgesics (narcotic analgesics); e.g. morphine.
b) Antipyretic analgesics (Non-Steroidal Anti-inflammatory Drugs= NSAIDs); e.g. aspirin.
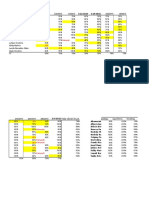
Morphine Aspirin
1. Potency Potent-relieves any type of pain Less potent-relieves mainly low
except itching. intensity pain.
2. Analgesic action Central on cortical and Central on subcortical level
subcortical levels. (thalamus) and peripheral (due
to anti-inflammatory action).
3. Other actions Narcosis-Drowsiness-Euphoria- Antipyretic-Antiinflammatory-
Tolerance-Dependence No narcosis, drowsiness,
(addiction) on prolonged use. euphoria, tolerance, or
dependence.
4. Analgesic in Deep visceral pain as cancer
pains-acute myocardial Superficial pain as headache-
infarction-Colics-Postoperative toothache-arthralgia-myalgia.
pain.
2. Peripheral analgesics (non-proper analgesics):
They relieve pain without acting on CNS; e.g.:
Local anaesthetics.
Counter-irritants.
Physical agents as astringents (they precipitate surface proteins) and demulcents
(form a protective layer).
Obtundants (they relieve pain of teeth, as oil of clover).
Drugs that relieve specific types of pain: nitrates in anginal pain, atropine in colics,
colchicine in acute gout.
1 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
A-Opioid (Narcotic) Analgesics
Classification:
1. Opioid Agonists: they act as agonists on opiate (opioid) receptors and are subdivided
into:
a) Phenanthrene opium alkaloids: morphine and codeine.
b) They are obtained from plant origin (unripe fruit of Papaver somniferum).
c) Semisynthetic derivatives: e.g. diacetyl morphine (heroin).
d) Synthetic substitutes: meperidine, fentanyl, methadone, dextropropoxyphene.
2. Mixed Agonist-Antagonists: they act as agonists on some opioid receptors and as
antagonists on other types of opioid receptors, e.g. pentazocine, nalbuphine,
buprenorphine, and butorphanol.
N.B.:
Opium is the dried extract obtained by scratching the unripe fruits of Papaver somniferum.
Opium alkaloids are classified into:
1. Phenanthrene alkaloids: morphine (main constituent), codeine and thebaine. They are
opioid analgesics and spasmogenic on smooth muscle fibres.
2. Benzylisoquinoline alkaloids: papaverine and narcotine. They are not analgesics (almost
no CNS actions).
Morphine
Source: plant origin (Papaver somniferum).
Chemistry: phenanthrene opium alkaloid (the chief cons tuent, 10% of opium).
Pharmacokinetics:
1. Absorption: morphine is well absorbed orally but it has low oral bioavailability (25%)
due to extensive 1st pass hepatic metabolism, so it is commonly given by injection
(S.C., I.M., and slowly diluted I.V.).
Give reason: in case of shock morphine is not given by S.C. injection.
2. Distribution:
Morphine passes BBB (but not as rapid as heroin).
Morphine passes the placental barrier and leads to fetal addiction (if given during
pregnancy) and neonatal asphyxia (if given during labor) which is treated by opioid
antagonists as naloxone (given I.M. to the mother before labor or intra-umbilical
to the fetus after labor).
3. Metabolism: conjugation with glucuronic acid by HME forming morphine -3-
glucuronide (inactive) and morphine -6- glucuronide (more active than morphine).
2 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
4. Excretion:
Mainly in urine (both conjugated and small amounts of unchanged morphine).
Small amounts of unchanged morphine are also excreted in:
1. Saliva (was used as a test for racing horses).
2. Stomach (that is why stomach wash should be performed in cases of acute
morphine toxicity although morphine is not orally administered in these cases).
3. Bile: entero-hepatic circulation of morphine prolongs the duration of action of
morphine compared to meperidine.
Breast milk: morphine may affect suckling infants and is therefore contraindicated
in lactating females.
Pharmacodynamics:
Mechanism of action: morphine acts as agonist on specific opiate (opioid) receptors in
brain and spinal cord inhibi on of release of substance P (and other
neurotransmitters)inhibi on of pain transmission.
Opiate receptors have the following characteristics:
1. They are present in CNS and in peripheral tissues as smooth muscle fibres especially
GIT- and adrenal medulla.
2. They are activated by endogenous opio-peptides as endorphins, enkephalins,
endomorphins and dynorphins (pleasure substances released in large amounts during
stress and pain).
3. They are G-protein coupled leading to: inhibition of adenylate cyclase and decrease c-
AMP- inhibition of Ca2+ influx by blocking voltage-gated channels-opening of K+
channels causing K+ efflux and hyperpolarization.
4. Types of opiate receptors include:
(Mu): induce analgesia both supraspinal and spinal- euphoria, miosis, R.C.
depression, drowsiness, and constipation (due to reduced GIT peristalsis).
(Kappa): induce analgesia-both spinal and supraspinal-less miosis, less
depression of R.C., and less drowsiness. Kappa receptors may induce dysphoria
and hallucinations (psychotomimetic action).
(delta): induce analgesia (mainly spinal) and constipation.
(sigma): induce dysphoria and hallucinations.
3 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Pharmacological actions:
Morphine has the following actions:
1. CNS actions: both depressant and stimulant actions, but it is considered a CNS
depressant drug.
2. A.N.S.: morphine stimulates parasympathetic nervous system (C.I.C. mainly) and
inhibits sympathetic nervous system (V.M.C. mainly).
3. Eye: morphine causes miosis by central not local- action.
4. Respiratory system actions.
5. CVS actions.
6. Actions on smooth muscle fibres: GIT-urinary system-Biliary tract-Bronchi.
7. Histamine release and action on skin: itching-sweating wheal formation.
8. Lowers basal metabolic rate (B.M.R.).
a) CNS Actions:
1. Analgesia:
Relieves any type of pain especially deep visceral pain (dull aching, high intensity
pain), but does not relieve itching because morphine is a potent histamine releaser.
Pain relief is due to supraspinal and spinal actions.
It also reduces psychological reaction to pain by reducing anxiety and fear.
Analgesia may be accompanied by drowsiness and stupor (mental clouding) and
narcosis.
2. Inhibition of repiratory centre (R.C.) and decreases the sensitivity of R.C. to CO2
CO2 in blood cerebral vasodilata on and increased CSF forma on eleva on of
intra-cranial pressure (ICP) more depression of R.C.
3. Inhibition of cough centre = central antitussive action.
4. Inhibition of V.M.C. occurs with large and toxic doses leading to vasodilatation and
hypotension.
5. Inhibition of heat regulating centre (H.R.C.) and lowering of basal metabolic rate
which may lead to hypothermia.
6. Euphoria (morphine may cause dysphoria if given in the absence of pain).
7. Miosis: morphine causes miosis by a central action (no miosis occurs if it is applied
locally to the eye) through stimulation of opiate receptors (mainly mu receptors) in
3rd nerve nucleus (Edinger-Westphal nucleus).
The miotic action of morphine can be antagonized by systemic antagonists as
naloxone or by local atropine.
In cases of acute morphine toxicity there is severe miosis referred to as "Pin-Point
Pupil = PPP" which is a very important diagnostic sign.
8. Excitation may occur in some human females and some animal species (as horses).
Morphine may cause seizures (convulsions) and trunkal rigidity which may be due to
inhibition of GABA release.
4 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
9. Stimulation of C.T.Z. causing nausea and vomiting.
10.Stimulation of C.I.C. causing bradycardia.
11.Hormonal actions: morphine inhibits the release of A.C.T.H. and gonadotrophins
(F.S.H. and L.H.) but stimulates the release of A.D.H. (may cause oligurea).
12.Spinal cord reflexes: morphine inhibits polysynaptic reflexes (withdrawal reflex) but
stimulates monosynaptic reflexes (stretch reflex).
Summary of C.N.S. actions of morphine:
Depressant actions Stimulant actions
1. Analgesia. 1. Euphoria.
2. Drowsiness, stupor, and narcosis. 2. Excitation, lowering of seizure threshold,
3. R.C. and trunkal rigidity.
4. cough center. 3. C.I.C.
5. V.M.C. 4. Edinger-Westphal nucleus.
6. A.C.T.H. and gonadotrophins (F.S.H. 5. C.T.Z.
and L.H.). 6. A.D.H.
7. polysynap c spinal reexes. 7. monosynap c spinal reexes.
b) Actions on Respiration:
1. Inhibition of R.C. and reduced sensitivity to CO2 (see before).
2. Bronchospasm (due to histamine release and spasmogenic action of morphine).
3. Inhibition of cough centre (see before).
Give reason: morphine is contraindicated in respiratory diseases as bronchial asthma
and chronic obstructive pulmonary disease (COPD).
c) Actions on CVS:
1. Small therapeutic doses cause only venodilatation which is beneficial in cases of
acute heart failure as it reduces preload but may lead to postural hypotension.
2. Large therapeutic doses (especially if given IV) and toxic doses cause hypotension due
to:
Arteriodilatation by histamine release and inhibition of VMC.
Bradycardia due to stimulation of CIC.
d) Action on Smooth Muscle Fibres:
Morphine is spasmogenic on smooth muscle fibres of GIT, urinary system, biliary system,
and bronchi but not spasmogenic on blood vessels or uterus.
1. GIT: morphine causes marked constipation due to:
Spasmogenic action on smooth muscles.
Inhibition of propulsive peristaltic movements.
Inhibition of defecation reflex.
5 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Spasm of internal sphincter.
Reduction of GIT secretions (except saliva)..
The spasmogenic action of morphine is partially antagonized by atropine and
completely antagonized by naloxone.
2. Biliary tract: morphine causes spasm of the wall of gall bladder, the biliary duct and
the sphincter of Oddi; leading to increased intra-biliary pressure.
Give reason:
Atropine is usually combined with morphine in treatment of biliary colic.
Morphine is not preferred to relieve post-cholecystectomy pain.
3. Urinary tract:
Spasm of the internal sphincter and inhibition of micturition reflex leading to
difficult micturition or urine retention.
Spasm of the ureteric smooth muscles which is partially antagonized by atropine.
Stimulation of ADH release leading to oligurea.
4. Uterus: no spasm on the uterus, but morphine causes fetal addiction and neonatal
asphyxia if given during pregnancy and labor; respectively (see before).
5. Bronchi: morphine causes bronchospasm which is also due to histamine release.
Tolerance:
Occurs a er 10:14 days of con nued administra on of morphine.
It may be due to inhibition of release of endogenous opio-peptides or due to
down-regulation of opiate receptors.
Tolerance occurs to analgesia, euphoria, and R.C. depression) and to euphoria; but
no tolerance occurs to miosis, constipation, and excitation (morphine addicts
always have miosis and constipation).
Tolerance is followed by physical and psychic dependence (addiction).
Cross tolerance and cross dependence occur between opioid analgesics and other
CNS depressants as barbiturates and alcohol.
Therapeutic uses:
1. Analgesic in cases of severe deep visceral pain as: acute myocardial infarction-Cancer
pain-Biliary and renal colic (combined with atropine)-Post-operative pain (except
after cholecystectomy and eye operations)-Bone fractures (except head injury).
N.B. morphine can be given intra-thecal or epidural to relieve chronic or post-
operative pain; this is known as "spinal analgesia".
2. Acute left ventricular failure (acute pulmonary edema): morphine is given IV, not as
analgesic (there is no pain in cases of acute left ventricular failure) but to reduce
anxiety and fear and to decrease sympathetic discharge leading to reduction of both
pre- and after-load (by vasodilatation).
6 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
3. Anaesthesia: morphine is given before general anaesthesia to reduce pain; this is
known as pre-anaesthetic medication.
Morphine has the following disadvantages: marked depression of R.C. nausea and
vomiting bronchospasm - post-operative constipation and urine retention-miosis
(which may interfere with stages of anesthesia).
That is why meperidine is preferred to morphine in pre-anaesthetic medication.
(Morphine may be used as IV anaesthetic).
4. Neurogenic shock (it is given diluted IV and not SC).
Adverse effects:
1. Nausea and vomiting (anti-emetics may be required).
2. Constipation and increased biliary pressure.
3. Urine retention.
4. Bronchospasm and depression of R.C.
5. Fetal addiction, delayed labor and neonatal asphyxia. It may affect suckling babies if
given to lactating women.
6. Bradycardia and hypotension in large doses.
7. Drowsiness and mental clouding and rarely dysphoria.
8. Itching (pruritus).
9. Tolerance and addiction = chronic toxicity.
10.Interferes with proper diagnosis of acute abdomen.
11.Acute morphine toxicity:
Manifestations: respiratory failure (central respiratory failure due to inhibition of R.C.)
Coma Hypotension and bradycardia Miosis in the form of pin-point pupil (PPP) which
is a diagnostic sign.
Treatment:
a) Gastric lavage by potassium permanganate, followed by purgative as MgSO4.
b) Arificial respiration.
c) Specific Antidote: opioid antagonists as naloxone IV.
Give reason: stomach wash should be performed in acute morphine poisoning
although it is mostly administered intravenously.
7 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Treatment of morphine addiction:
Avoid sudden withdrawal of morphine for fear of severe withdrawal symptoms as
insomnia, dysphoria, excitation, yawning, mydriasis, body aches, rhinorrhea, lacrimation,
and diarrhea. Treatment includes:
1. Hospitalization and psychotherapy.
2. Gradual withdrawal of morphine until a stabilizing dose is reached (the smallest dose
that prevents withdrawal symptoms).
3. Substitution: Administration of other opioid agonists as methadone which has the
following advantages:
Longer duration of action than morphine.
Same potency as morphine.
Less liable to tolerance and addiction.
Less severe withdrawal symptoms.
4. Complete withdrawal of morphine followed by withdrawal of methadone. This is
known as "detoxification".
5. Clonidine is given to control withdrawal symptoms.
6. Acupuncture to stimulate release of endorphins.
7. After detoxification; opioid antagonists as naltrexone are given orally to maintain the
opioid-free state.
Contraindications:
1. Head injury and other causes of increased intra-cranial pressure as brain tumours.
2. Hypothyroidism (myxedema).
3. Respiratory disease as bronchial asthma and COPD.
4. Pregnancy, labor and lactation.
5. Liver and kidney impairment.
6. Extremes of age (very young and very old patients due to deficient conjugation
leading to "supersensitivity").
7. Acute abdominal pain before diagnosis of the cause because morphine will mask pain
which is the diagnostic symptom.
8. After cholecystectomy.
9. Alone in renal and biliary colics (atropine is added).
10.Epilepsy and other convulsive states.
11.History of addiction to opiates.
12.Allergy to morphine.
8 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Codeine
Source: plant origin (from Papaver somniferum).
Chemistry: phenanthrene opium alkaloid (1% of opium) - codeine is "methyl
morphine".
Pharmacokinetics: given orally-metabolized by the liver-has higher oral bioavailability
than morphine-partially converted into morphine.
Pharmacodynamics:
Agonist on opiate receptors.
Actions are similar to morphine but less potent analgesic-less R.C. depression-less
tolerance and addiction-may cause excitation in large doses. It is as potent as
morphine as cough centre depressant.
Therapeutic uses:
1. Central antitussive in treatment of dry cough (non-addictive antitussives are now
preferred).
2. Analgesic: may be combined with aspirin and paracetamol (APC).
Semi-Synthetic Derivatives (substitutes):
They are derived from morphine and codeine, examples include:
1. Diacetyl morphine=Heroin:
Opioid agonist- More potent than morphine as analgesic but is highly addictive-
Deacetylated into morphine in C.N.S.
2. Apomorphine:
Opioid agonist and dopaminergic agonist-Causes severe nausea and vomiting by
stimulation of CTZ (central emetic) Given IV to induce vomiting in case of drug and food
poisoning (never used in comatose patients).
Synthetic Opioid Substitutes:
1-Meperidine (Pethidine):
Source: synthetic.
Chemistry: not a phenanthrene opium alkaloid.
Pharmacokinetics:
Absorbed orally, has higher bioavailability than morphine (50%). It is also given
parenterally. Meperidine has a rapid onset and short duration compared to
morphine.
Passes BBB and placental barrier but causes much less depression of fetal R.C.
Metabolized into normeperidine (active metabolite which may cause excitation and
convulsions) and meperidinic acid (inactive). Metabolites are excreted in urine.
9 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Pharmacodynamics:
Mechanism of action: Agonist on opiate receptors (mainly ).
Pharmacological actions:
1. Analgesic: less potent than morphine (1:10).
2. Less or no narcosis.
3. R.C. depression: less than morphine especially in newborn.
4. No depression of cough centre; i.e. meperidine is not antitussive.
5. Euphoria (less than morphine) and may cause excitation and seizures
(convulsions) if given in large and toxic doses or if given with MAO inhibitors.
6. No miosis; may even cause mydriasis due to atropine-like action.
7. Nausea and vomiting due to stimulation of CTZ: less than morphine.
8. Stimulates ADH release.
9. Less spasmogenic and less or no constipation due to atropine-like action.
10.Local anaesthetic action.
11.Tolerance and dependence: less than morphine.
Therapeutic uses:
1. Analgesic in deep visceral pain as acute myocardial infarction and cancer. It is
preferred to morphine in:
Renal and biliary colics (given alone because of atropine- like action)
Obstetric analgesia (less or no R.C. depression of newborn).
2. Pre-anaesthetic medication. It is preferred to morphine (less R.C. depression-less
emetic-less constipation).
Drug interactions:
With MAO inhibitors severe R.C. depression, excita on, delirium, convulsions, and
hyperpyrexia.
10 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Morphine Meperidine
1-Source: Natural from plant origin Synthetic.
(Papaver somniferum).
2-Chemistry: Phenanthrene opium alkaloid. Not an opium alkaloid.
3-Oral bioavailability: 25%. 50%.
4-Metabolism: Into morphine -6-glucuronide Into normeperidine (active)
(more active) and morphine - and meperidinic acid
3-glucuronide (inactive). (inactive).
5-Onset and duration: Delayed onset and longer Rapid onset and short
duration. duration.
6-Mechanism of action: Agonist on opiate receptors ( Agonist on opiate receptors
and ). (mainly ).
7-Actions:
Analgesic: Potent. Less potent (1/10).
Narcosis: Narcotic. Less or no narcosis.
R.C .depression: Potent. Less; especially in newborn.
An tussive: Potent. Not antitussive.
Euphoria: Potent. Less.
Excita on: In some human females and In large and toxic doses (due
some animals. to normeperidine).
Convulsions: In large and toxic doses due to In large and toxic doses or
inhibition of GABA release. with MAO inhibitors.
Atropine-like action: No atropine-like action. Has atropine-like action.
Pupil: Miosis (central). No miosis; may be mydriasis
(atropine-like)
Eme c ac on (nausea Potent due stimulation of CTZ. Less
and vomiting):
Spasmogenic ac on on Potent. Less or no action (atropine-
GIT and constipation: like).
Addic on: Highly addictive. Less addictive.
8-Uses: -Analgesic in deep visceral -Analgesic in deep visceral
pain. pain.
-Acute heart failure. -Pre-anaesthetic medication.
-Pre-anaesthetic medication. Better than morphine in:
-Neurogenic shock. Colics-Obstetric analgesia-
-Insomnia due to pain. Preanaesthetic medication.
11 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
2-Fentanyl:
Source: synthetic.
Chemistry: derivative of meperidine.
Pharmacokinetics: absorbed orally, given also by injection, transdermal patch and
intra-thecal.
Pharmacodynamics:
-Mechanism of action: Agonist mainly on receptors.
-Pharmacological actions: as morphine but much more potent analgesic; about 80
times.
Thearpeutic uses:
1. Analgesic in deep visceral pain.
2. Anaesthesia: combined with neuroleptics (major tranquilizer) as droperidol in short
painful operations. The emetic action of fentanyl (by stimulation of D2-receptors in
CTZ) is antagonized by the anti-emetic action of droperidol (blocks D2-receptors in
CTZ). This is known as "Neurolept-analgesia".
Adverse effects: nausea and vomiting-depression of R.C.-addiction-trunkal rigidity.
Alfentanil: similar to fentanyl but more potent.
Sufentanil: similar to fentanyl but shorter in duration.
N.B.
Loperamide and Diphenoxylate: are meperidine derivatives but are not analgesics as they
very poorly penetrate BBB. They stimulate opioid receptors in GIT and are used in
treatment of diarrhea. Diphenoxylate is usually combined with atropine.
3-Methadone:
Source: synthetic.
Pharmacokinetics: given orally and by injection-higher oral bioavailability and longer
duration than morphine.
Pharmacodynamics: agonist on opiate receptors, as potent as morphine but less liable
to tolerance and addiction and much less severe withdrawal symptoms.
Therapeutic uses: Analgesic in deep visceral pain-To substitute morphine and heroin in
treatment of addicts.
4-D-Propoxyphene:
Source: synthetic.
Chemistry: derivative of methadone.
Pharmacokinetics: given orally.
Pharmacodynamics: opioid agonist-less potent analgesic than codeine.
Therapeutic uses: analgesic in mild to moderate pain not relieved by aspirin.
Adverse effects: addiction-depression of R.C. and excitation in toxic doses.
12 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Mixed Agonist-Antagonists (Opioids with mixed action):
They include: Pentazocine Nalbuphine Butorphanol Buprenorphine.
They act as antagonists on -receptors and agonists on -receptors, except Buprenorphine
which is a partial agonist on -receptors and antagonist on -receptors.
Actions and uses:
1. Analgesics in deep visceral pain by stimulation of -receptors. They have the
following advantages:
a) Less liable to addiction.
b) "Ceiling effect" on R.C. depression; i.e. the dose can be increased to increase the
analgesic action without increase in R.C. depression because they act as -
antagonists.
2. Diagnosis of opioid addicts because they precipitate withdrawal symptoms by
blocking -receptors.
Pentazocine:
Antagonist on and agonist on -receptors.
Actions and uses: see before.
Given orally and parenterally.
Causes dyshoria and hallucination in large doses (due to stimulation of sigma receptors)
and increases blood pressure and heart rate (cardiac work).
Nalbuphine:
As pentazocine (antagonist on and agonist on ).
Actions and uses: see before.
Given parenterally.
No increase in cardiac work.
Butorphanol: as pentazocine.
Buprenorphine: partial agonist on and antagonist on -receptors.
Indicate" true or false" and explain why:
It is advisable to combine morphine and pentazocine in treatment of severe visceral pains.
N.B.:
Tramadol:
Central analgesic acting as a weak -agonist and by inhibi on of noradrenaline and 5-HT
uptake in CNS.
It is used in chronic pain, given orally and parenterally.
13 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Opioid Antagonists:
They are competitive antagonists that block opiate receptors.
They include:
a) Naloxone given IV and orally.
b) Naltrexone given orally.
c) Nalmefene given IV. Longer duration than naloxone.
Actions depend on the patient receiving these drugs:
1. In normal individuals (in the absence of opioids): no effect, i.e. they are not
analgesics.
2. In cases of acute opioid toxicity: they reverse the actions of opioids as morphine (R.C.
depression, constipation, miosis, vomiting).
3. In opioid addicts: they induce withdrawal symptoms.
Therapeutic uses:
1. Treatment of acute opioid toxicity (naloxone or nalmefene IV).
2. Treatment of neonatal asphyxia (naloxone IM to the mother before delivery or intra-
umbilical after delivery).
3. Diagnosis of morphine and heroin addicts.
4. Treatment of morphine-induced paralytic ileus.
5. To maintain opioid-free state after treatment of addicts, i.e.to prevent return to
opioids (naltrexone oral).
N.B. Nalorphine is similar to mixed agonist-antagonists but is not used as analgesic because
it causes anxiety and visual hallucinations.
Levallorphan is a partial agonist on opiate receptors and is not used clinically.
Classify drugs acting on opiate receptors with examples:
Drug Example Therapeutic uses
1-Opioid Agonists: -Morphine. Analgesics in deep visceral pain.
-Codeine.
-Meperidine.
-Methadone.
-Fentanyl.
2-Mixed Agonist- -Pentazocine. 1-Analgesics in deep visceral pain.
Antagonists: -Nalbuphine. 2-Diagnosis of opioid addicts.
-Butorphanol.
-Buprenorphine.
3-Opioid Antagonists: -Naloxone. 1-Treatment of acute opioid (morphine)
-Nalmefene. toxicity.
-Naltrexone. 2-Neonatal asphyxia.
3-Opioid-induced ileus.
4-To maintain opioid-free state.
5-Diagnosis of opioid addiction.
14 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
B-Antipyretic Analgesics
They are also known as "non-opioid analgesics" and more commonly as "Non-Steroidal
Anti-Inflammatory Drugs = NSAIDs".
They inhibit prostaglandin synthesis and accordingly their actions are summarized as
follows:
Actions of PGs Actions of NSAIDs
1. Pain. 1. Analgesics in superficial pains.
2. Fever. 2. Anti-pyretics (non-specific).
3. Inflammation. 3. Anti-inflammatory.
4. Protection of mucosa of stomach and 4. Peptic ulceration.
duodenum against HCl and pepsin
(Cytoprotective by HCl-mucus,
HCO3, and blood flow).
5. Increases renal blood flow (RBF). 5. Decreases RBF Na+ and water retention
and even nephropathy.
6. Uterine stimulation (Oxytocics). 6. Uterine relaxants (Tocolytics).
7. Maintain patency of ductus arteriosus. 7. Closure of patent ductus arteriosus (PDA).
They have the common characters:
a) Pharmacokinetic properties:
Well absorbed orally.
Highly bound to plasma proteins and displace other drugs from plasma protein
binding sites (as warfarin, oral hypoglycemics, digitoxin) leading to serious adverse
reactions by these drugs.
Pass BBB.
Pass placental barrier and may cause teratogenicity is given in early pregnancy
(aspirin is the safest anti-inflammatory during pregnancy) and premature closure
of DA if given in late pregnancy.
The main fate is commonly hepatic metabolism, some are partly excreted in urine
unchanged (as aspirin), some are partly excreted in bile and undergo entero-
hepatic recycle leading to long duration of action (as indomethacin and oxicams),
and some are prodrugs (as sulindac and nabumetone).
15 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
b) Pharmacodynamics:
1. Mechanism of action:
They inhibit synthesis of prostaglandins (PGs) by inhibition of cyclo-oxygenase
(COX) enzymes.
All are "reversible" COX inhibitors except aspirin (=acetyl salicylic acid) which is
"irreversible" COX inhibitor by acetylation.
2. Pharmacological actions: see previous table.
N.B.: paracetamol has analgesic and antipyretic actions only.
c) Adverse effects:
1. Allergy.
2. Bronchospasm and precipitation of attacks in asthmatic patients.
3. Peptic ulcer.
4. Teratogenicity.
5. Decrease renal blood flow, cause Na+ and water retention, and may lead to renal
impairment (analgesic nephropathy).
6. Premature closure of DA.
d) 4-Contraindications:
1. Allergic patients.
2. Bronchial asthma.
3. Peptic ulcer.
4. Pregnancy.
Important note:
There are 3 types of COX enzymes:
COX-1 (cons tu ve): present in the stomach where it stimulates synthesis of PGE2 and
PGI2 which are cytoprotective (HCl, mucus, bicarbonate, and blood ow), in the
kidney stimulating synthesis of vasodilator PGs as PGE and I thus increasing renal blood
flow, and in platelets where it induces TXA2 synthesis that activates platelet aggregation.
COX-2 (inducible): present in CNS and peripheral tissues inducing synthesis of PGs
causing pain, fever, and inflammation. It was recently found in the kidneys (as COX-1).
COX-3: found only in CNS and stimulates of PGs causing pain and fever. (COX-3 may be a
variant of COX-1).
16 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Classification of NSAIDs:
I-Non-selective COX inhibitors:
They act as analgesics, antipyretics, and anti-inflammatory drugs through inhibition of
COX-2 and COX-3.
Their main adverse effects are peptic ulcer and reduction of RBF due to inhibition of
COX-1 mainly.
They include:
1. Salicylic acid derivates=Salicylates: e.g. aspirin and sodium salicylate.
2. Pyrazolone derivatives: e.g. phenylbutazone.
3. Indole derivatives: e.g. indomethacin, sulindac (prodrug) and Tolmetin.
4. Propionic acid derivatives: e.g. ibuprofen, ketoprofen, and naproxen.
5. Phenyl acetic acid derivatives: e.g. diclofenac.
6. Oxicams: e.g. piroxicam, Tenoxicam, and Meloxicam (inhibits COX-2 more than COX-1).
7. Nabumetone (prodrug).
8. Anthranilic acid derivatives = Fenamates: e.g. mefenamic acid and flufenamic acid.
II-Selective COX-2 inhibitors:
Examples: meloxicam, celecoxib, rofecoxib, valdecoxib, eterocoxib.
They act as analgesics, antipyretics, and anti-inflammatory as non-selective COX
inhibitors.
The main advantage over non-selective drugs is much less incidence of peptic ulceration.
They may cause less reduction of RBF compared to non-selective COX inhibitors.
Some selective cox-2 inhibitors as rofecoxib (vioxx) were withdrawn from the market
because they caused cerebro-vascular strokes and cardiac toxicity (infarction and fatal
arrhythmias).
III-Selective COX-3 inhibitors:
Include Dipyrone (pyrazolone derivative) and Aniline derivatives e.g. paracetamol =
acetaminophen, and phenacetin (not commonly used). They are analgesics and antipyretics
but are not ant-inflammatory drugs (they act centrally and not peripherally).
17 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
SALICYLATES
Source: synthetic.
Chemistry: salicylates are derived from salicylic acid.
Derivatives: salicylates include the following derivatives:
a) Derivatives for local use: they are not used systemically because they are highly
irritant on GIT. They include:
1. Salicylic acid: used locally as antiseptic-fungistatic keratolytic.
2. Methylsalicylate: used locally as counter-irritant.
b) Derivatives for systemic use: they are used systemically as analgesics, antipyretics,
and anti-inflammatory drugs. They include:
1. Aspirin = Acetyl Salicylic Acid (ASA).
2. Sodium salicylate: given as "enteric-coated tablets".
3. Diflunisal: is a potent anti-inflammatory not it is not antipyretic or antiplatelet,
and has less adverse effects than aspirin.
Pharmacokinetics of systemically administered salicylates (aspirin and sodium
salicylate):
a) Absorption: they are partially absorbed from the stomach and completely absorbed
from the upper intestine (why?).
b) Distribution: highly bound to plasma proteins and displace other drugs (see drug
interactions) pass BBB pass placental barrier and is not preferred in early and in
late pregnancy before labor (see adverse effects).
c) Metabolism: most of the drug (about 75%) is conjugated with glucuronic acid and
glycine and only 1% is oxidized into gen sic acid.
d) Excretion: renal excre on of metabolites and partly (about 25%) excreted
unchanged. Renal excretion is enhanced by NaHCO3 and reduced by vitamin C and
NH4Cl (why?).
e) N.B.: the elimina on t1/2 is variable according to the dose of aspirin because aspirin
in small doses (<5g. /day) obeys rst-order kine cs; i.e. t1/2 is constant whereas
larger doses follow zero-order kine cs and t1/2 increases with increasing doses (due
to enzyme saturation).
Pharmacodynamics:
Mechanism of action: inhibition of PGs synthesis by non-selective COX inhibition.
Aspirin causes irreversible inhibition by acetylation but other salicylates as all
NSAIDs- cause reversible inhibition.
Remember that very small doses; known as "pediatric or infan le doses" =75-150 mg.
/day, cause selective irreversible inhibition of thromboxane A2 (TXA2) synthetase
(may be called platelet COX) leading to inhibition of platelet aggregation.
18 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Pharmacological actions:
a) Local actions:
1. Antiseptic-fungistatic- keratolytic actions by salicylic acid.
2. Counter-irritant action by methyl salicylate.
b) Systemic actions:
1. CNS actions: Analgesic action Antipyretic action.
2. Anti-inflammatory (anti-rheumatic) action.
3. Action on respiration and acid-base balance.
4. Actions on CVS.
5. Actions on blood.
6. Action on serum uric acid.
7. Action on GIT.
8. Action on the kidney.
9. Metabolic action.
10.Endocrine actions.
11.Action on the liver.
1. CNS actions:
Analgesic action:
-By inhibition of PGs synthesis both centrally (subcortical on thalamus) and peripherally.
-Relieve superficial low intensity pains as headache, toothache, arthralgia, and myalgia.
-Not accompanied by euphoria, narcosis, tolerance, or addiction.
Antipyretic action:
a) In fever: IL1, IL6, and TNF stimulate PG synthesis in the hypothalamic heat regulating
centre (HRC) leading to elevation of the set point, thus increasing heat production (by
shivering) and decreasing heat loss.
NSAIDs inhibit COX enzymes centrally leading to inhibition of PG synthesis with
consequent "re-setting" of HRC. This increases heat loss by sweating, V.D. of
cutaneous blood vessels, and mobilization of fluids from tissues to blood.
b) They have no effect on normal body temperature; i.e. they are not hypothermic
drugs.
c) In cases of acute salicylate toxicity, hyperthermia (hyperpyrexia) occurs due to
uncoupling of oxidative phosphorylation.
2. Anti-inflammatory (anti-rheumatic) action:
The anti-inflammatory action of NSAIDs is due to:
Inhibition of PG synthesis peripherally mainly by inhibition of COX and indirectly by
stimulation of ACTH and cortisone release which inhibit phospholipase A2.
Inhibition of hyaluronidase and fibrinolysin.
Inhibition of kallikrein enzyme and accordingly inhibition of kinin synthesis.
3. Action on Respiration and Acid-Base Balance:
19 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
The usual analgesic-an pyre c doses (< 5 g. /day) have no eect.
Large doses (> 5 g. /day; used as an -inflammatory in rheumatoid arthritis (RA) and
rheumatic fever (RF)) stimulate R.C. and increase respiratory rate leading to wash of
CO2 from blood and respiratory alkalosis occurs.
The kidney compensates by increasing excretion of NaHCO3 in urine and
compensated respiratory alkalosis occurs.
Larger doses-especially in children- cause metabolic acidosis (may be due to the
acidity of salicylates, reduction of the alkali reserve due to loss of NaHCO3 in urine,
and disturbance of carbohydrate metabolism increasing the blood levels of pyruvic
and lactic acids).
In toxic doses R.C. depression occurs.
NSAIDs induce bronchospasm and may precipitate asthmatic attacks in susceptible
patients due to inhibition of COX and shift of arachidonic acid into synthesis of
leukotrienes (sometimes referred to as aspirin-induced asthma).
Question:
How to treat inflammatory conditions as RF and RA in asthmatic patients?
4. Action on CVS:
Therapeutic doses of salicylates have no effect on CVS, but very large and toxic doses
cause V.D. both by peripheral action and centrally by inhibition of VMC, leading to
hypotension.
5. Action on Blood:
Antiplatelet = An thrombo c ac on: very small doses of aspirin (75-150 mg. /day)
selectively inhibit platelet TXA2 synthesis leading to inhibition of platelet aggregation
which prolongs bleeding time.
Anticoagulant action = dicuomarol-like action: large doses inhibit activation of
vitamin K leading to hypoprothrombinemia and bleeding. This prolongs coagulation
time and prothrombin time.
Reduction of elevated sedimentation rate and leucocytic count to normal.
Idiosyncracy: salicylates induce hemolysis of RBCs in patients with G6PD deciency
leading to hemolytic anemia.
Question:
What are the possible mechanisms of aspirin-induced bleeding?
20 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
6. Action on serum uric acid:
Usual doses (< 5 g. /day) increase serum uric acid by inhibi on of uric acid secre on
by proximal convoluted tubules (PCT); and accordingly are contraindicated in gout
and they antagonize the action of uricosurics as probenicid.
Larger doses (> 5 g. /day) cause uricosuric ac on by inhibi on of uric acid
reabsorption from PCT; however they are not preferred in treatment of chronic gout
due to many adverse effects.
7. Actions on GIT:
Nausea and vomiting due to both local irritant action and central action through
stimulation of CTZ.
Ulceration and bleeding due to inhibition of synthesis of cytoprotective PGs (PGE2
and PGI2).
N.B.
The irritant effect of salicylates can be reduced by giving them after meals, by adding
alkalis, or by giving enteric-coated tablets (sodium salicylate).
Iatrogenic ulcers caused by NSAIDs are better prevented and treated by PG analogs
as misoprostol.
8. Action on the kidney:
Inhibition of synthesis of vasodilator PGs decrease RBF leading to Na+ and water
retention and antagonize the anti-hypertensive action of diuretics, -blockers and
ACE inhibitors.
Chronic use of large doses of NSAIDs may cause renal impairment (analgesic
nephropathy).
9. Metabolic actions:
They are noticed with large and toxic doses of salicylates and include:
Uncoupling of oxidative phophorylation and hyperthermia.
Hyperglycemia due to increased release of ACTH, cortisol, and adrenaline.
Protein catabolism (-ve nitrogen balance and increased amino acids in urine) due to
ACTH and cortisone.
Increased Glutamate / GABA ratio in CNS which may lead to convulsions.
10.Endocrine actions:
Increased release of ACTH, cortisone, and adrenaline.
Displacement of bound T3 and T4 from plasma proteins Free T3 and T4 TSH by
negative feedback radioac ve iodine uptake and interference with thyroid
function tests.
21 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
11.Actions on the liver:
Glycogenolysis and hyperglycemia (due to cortisone and adrenaline).
Hydrochloretic action (increases water content of bile).
Hepatotoxicity and encephalopathy- if salicylates are administered to children
having fever due to viral infections especially influenza.
This is known as Reye's syndrome which may be fatal.
Give reason:
Aspirin is absolutely contraindicated in children suffering from fever due to viral
infections. What is the alternative analgesic-antipyretic in such cases?
Therapeutic uses:
a) Local uses:
1. Antiseptic-fungistatic-keratolytic: salicylic acid is used.
2. Counter-irritant in arthritis: methylsalicylate is used.
b) Systemic uses:
1. Analgesic in superficial low intensity pains as headache, toothache, arthralgia,
myalgia, and common cold. Salicylates are not preferred in dysmenorrhea as they
may increase bleeding.
2. Non-specific antipyretics in fever.
3. Anti-inflammatory in RF, RA, osteoarthritis (OA).
4. Prophylaxis of thrombo-embolism (by pediatric=baby aspirin).
5. Other uses:
Prophylaxis of cataract.
Reduce the incidence of cancer colon.
Symptomatic treatment of systemic mastocytosis (with anti-histaminics).
Prevention of niacin-induced flushing.
Chronic gout as uricosuric (not commonly used).
Treatment of pre-eclampsia.
N.B.
1. Aspirin in acute RF relieves: fever, arthritis, reduces elevated sedimentation rate and
leucocytic count to normal, but has no effect on chorea and S.C. nodules.
2. In heart failure complicating RF aspirin is preferred to sodium salicylate (why?).
22 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Adverse effects Contraindications
1. Hypersensitivity (allergic reactions) as skin 1. Allergy to salicylates.
rash, urticaria, angioedema.
2. Bronchospasm and precipitation of 2. Bronchial asthma.
asthmatic attacks in susceptible patients.
3. GIT disturbances: nausea, vomiting, ulcers 3. Peptic ulcers.
and bleeding (increased occult blood in
stools).
4. Bleeding. 4. Bleeding disorders as hemophilia
and purpura.
5. Hemolysis in idiosyncratic patients with 5. Idiosyncracy in G6PD deciency
G6PD deciency. (Favism).
6. Teratogenicity in early pregnancy (1st 6. Pregnancy (early and late).
trimester).
7. Increased post-partum hemorrhage,
delayed labor, and premature obliteration
of ductus arteriosus in late pregnancy.
8. Reye's syndrome: hepatocellular damage 7. Children with fever caused by viral
and encephalopathy in children with fever infections especially influenza.
due to viral infections.
9. Salicylism=chronic salicylate toxicity:
headache, nausea and vomiting, blurred
vision, vertigo and tinnitus (ringing in ears).
10. Acute salicylate toxicity (see later).
Important note:
Paracetamol is the analgesic-antipyretic of choice whenever aspirin is contraindicated in:
allergy-bronchial asthma-bleeding disorders-favism-peptic ulcer-pregnancy-children.
23 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Acute salicylate toxicity:
Manifestations:
Convulsions-Hypotension-Hemorrhage-Hyperglycemia-Hyperventilation, respiratory
alkalosis then metabolic acidosis especially in children -GIT disturbances
(nausea,vomiting and may be ulcerations and bleeding)-Hyperthermia-Dehydration-
finally R.C. depression occurs.
Treatment:
1. Gastric lavage by NaHCO3.
2. Artificial respiration in case of depression of R.C.
3. Symptomatic treatment:
NaHCO3 to correct systemic acidosis.
Cold fomentations or ethyl alcohol fomentations to treat hyperthermia (no
antipyretics needed; why?).
Anticonvulsant drugs (e.g. as diazepam IV) to control convulsions.
Vitamin K to control hypoprothrombinemia and bleeding.
IV fluids to correct hypotension and dehydration.
4. Increasing urinary excretion of salicylates by alkalinization of urine by NaHCO3, or by
potent diuretics as loop diuretics (frusemide) IV or mannitol IV infusion. This is known
as "forced diuresis".
5. Hemodialysis may be performed in severe cases.
N.B.: there is no specific antidote for aspirin but NaHCO3 may be considered as a non-
specific antidote because it decreases oral absorption, increases renal excretion, and
corrects acidosis.
Drug interactions:
a) Pharmacokinetics interaction:
Absorption: NaHCO3 in antacids decreases oral absorption of aspirin.
Distribution: salisylates displace digitoxin, warfarin, and oral hypoglycemic drugs
from plasma protein binding sites leading to serious adverse effects of these
drugs.
Excretion: NaHCO3 promotes renal excretion of salicylates whereas vitamin C and
NH4Cl reduce excretion and may increase toxicity.
b) Pharmacodynamic interactions:
Salicylates antagonize the antihypertensive action pf -blockers, thiazides, and
ACE inhibitors by decreaseing RBF leading to salt and water retention (may
increase hyperkalemia caused by ACE Inhibitors).
24 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Small doses of salicylates antagonize the uricosuric action of "uricosuric drugs" as
probenicid, sulphinpyrazone, and benzbromarone and accordingly worsen gout.
Alcohol and glucocorticoids (cortisone) increase the incidence of GIT ulcers and
bleeding caused by salicylates.
Aspirin antagonizes the anti-inflammatory action of other NSAIDs as piroxicam and
diclofenac, because aspirin causes "irreversible" COX inhibition.
Indole Derivatives
Include: Indomethacin and Sulindac (prodrug-less gastric irritation).
Pharmacokinetics:
- Well absorbed orally.
- Pass BBB-pass placental barrier (teratogenic)-highly bound to plasma proteins.
- Metabolized by the liver, partly excreted unchanged in urine and bile and undergo
entero-hepatic circulation (long acting).
Pharmacodynamics:
- Mechanism of action: inhibition of PG synthesis by reversible non-selective COX
inhibition.
- Pharmacological actions: Anti-inflammatory (mainly) Analgesic Antipyretic.
Therapeutic uses:
1. Anti-inflammatory in acute gouty arthritis -RF- pericarditis- OA-RA.
2. Patent ductus arteriosus.
Adverse effects:
1. Allergy: skin rash.
2. Bronchospasm and precipitation of asthmatic attacks.
3. Peptic ulceration.
4. Teratogenicity in early pregnancy, delayed labor and premature closure of ductus
arteriosus in late pregnancy.
5. Renal impairment.
6. Bone marrow depression (blood dyscrasias).
7. CNS disturbances: confusion, hallucinations, psychotic manifestations, seizures, and
frontal headache.
8. Corneal opacities.
Contraindications:
1-Allergy. 2-Bronchial asthma. 3-Pep c ulcer. 4-Pregnancy.
5-Psychosis. 6-Epilepsy.
25 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Pyrazolone Derivatives
Include: Phenylbutazone, Azaprpazone (Apazone), Sulphinpyrazone (uricosuric only).
Other pyrazolone derivatives as dipyrone, antipyrine, aminopyrone are not used because
they may cause severe bone marrow depression.
Pharmacokinetics:
- Well absorbed orally.
- Pass BBB- pass placental barrier (teratogenic)- highly bound to plasma proteins and
displace other drugs as oral anticogulants, oral hypoglycemics, and thyroid hormones.
- Metabolized by the liver, and metabolites are excreted in urine.
Pharmacodynamics:
- Mechanism of action: inhibit prostaglandin synthesis by reversible non-selective COX
inhibition.
- Pharmacological actions: Anti-inflammatory (mainly)- Analgesic- Antipyretic-
Uricosuric.
N.B. only salicylates and pyrazolone derivatives are uricosurics but other NSAIDs have no
uricosuric action.
Therapeutic uses:
Anti-inflammatory in acute gouty arthritis- OA- RA.
Adverse effects:
1. Allergic reactions as skin rash.
2. Bronchospasm and induction of asthmatic attacks.
3. Peptic ulcer.
4. Teratogenicity.
5. Salt and water retention leading to edema, elevation of ABP, and worsening of heart
failure. Renal impairment may occur.
6. Bone marrow depression.
Contraindications:
1. Allergy.
2. Bronchial asthma.
3. Peptic ulcer.
4. Pregnancy.
5. Hypertension and heart failure.
Drug interactions:
1. Displacement of other drugs from plasma proteins.
2. Antagonize the action of diuretics and antihypertensive drugs.
26 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Propionic Acid Derivatives:
Include: Ibuprofen, ketoprofen, naproxen, flurbiprofen, tiaprofenic acid, and fenoprofen.
Oxicams:
Include: Piroxicam and tenoxicam.
They have entero-hepatic circulation and long duration of action.
Aryl acetic acid Derivatives:
Include: Diclofenac, tolmetin, and ketorolac.
Anthranilic Acid Derivatives = Fenamates:
Include: Mefenamic acid, and flufenamic acid.
All these derivatives have the common characters of NSAIDs (page 18 and 19).
Aniline Derivatives:
Include: Paracetamol = Acetaminophen, and phenacetin (not commonly used due to its
serious adverse effects).
Source: synthetic.
Chemistry: aniline derivatives.
Pharmacokinetics:
- Absorption: well absorbed orally (paracetamol is rapidly disintegrated in the
stomach, and the more rapid the gastric emptying the better the absorption).
- Distribution: pass BBB pass placental barrier but not teratogenic- slight binding to
plasma proteins (much less liable to drug interactions than other NSAIDs as aspirin).
- Metabolism:
Phenacetin (active) paracetamol (ac ve).
About 95% of paracetamol is metabolized by the liver mainly by conjuga on with
glucuronic acid and sulphate (major pathway) and to a less extent by oxidation by
CYP450 (minor pathway) into a toxic metabolite known as NAPQI (N-Acetyl Para-
Benzo-Quinone-Imine) which is detoxified by SH donors in the liver as glutathione.
- Excretion: metabolites and unchanged paracetamol (about 5%) are excreted in urine.
27 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Pharmacodynamics:
a) Mechanism of action: inhibit prostaglandin synthesis centrally only by reversible
selective COX-3 inhibi on.
b) Pharmacological actions: Analgesic and antipyretic actions only.
1. NO (or very weak) anti-inflammatory action.
2. NO anti-platelet action and NO anticoagulant action, and accordingly NO bleeding.
3. NO uricosuric action.
4. NO peptic ulceration.
5. NO renal impairment (except in acute toxicity).
6. NO bronchospasm or precipitation of asthmatic attacks.
7. NO uterine relaxation and NO closure of ductus arteriosus.
Therapeutic uses:
1. Analgesic in superficial low intensity pains as headache, arthralgia, common cold,
toothache, myalgia.
2. Antipyretic (non-specific) in fever.
3. Paracetamol is especially indicated in patients allergic or intolerant to aspirin (i.e.
whenever aspirin is contraindicated) as in:
Bronchial asthma peptic ulcer- bleeding disorders as hemophilia pregnancy (early
and late) children with fever due to viral infections as influenza.
Adverse effects: "paracetamol is well-tolerated by most patients except in case of
allergy or acute toxicity". Adverse reactions include:
1. Allergic reactions: rash, fever, and rarely blood dyscrasias (bone marrow depression).
2. Phenace n causes methemoglobinemia, hemoly c anemia in G6PD deciency
(idiosyncracy)-cyanosis- cardiac arrest and respiratory failure in case of acute toxicity.
3. Acute paracetamol toxicity:
Cause: occurs with toxic doses (10-15 g. in adults) due to satura on of conjuga on
pathway and formation of NABQI which is not detoxified due to depletion of SH; or in
chronic alcoholism (induces enzyme responsible for oxidation of paracetamol into
toxic NABQI).
Manifestations: early symptoms: nausea, vomiting, diarrhea, and abdominal pains.
Later; there is hepatotoxicity (hepatic necrosis) causing jaundice- nephrotoxicity
(renal tubular necrosis) causing hematuria, oliguria and anuria- hypoglycemic coma.
Treatment: mainly by SH donors as N-acetylcysteine, and supportive treatment.
Contraindications: allergy to aniline derivatives.
N.B.: Benoral (benorylate) is a combination of aspirin and paracetamol.
28 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Aspirin Paracetamol
Chemistry: Salicylic acid derivative. Aniline derivative.
Pharmacokinetics: - Well absorbed orally, partially - Well absorbed orally.
absorbed from the stomach. - Passes BBB.
- Passes BBB. - Passes placental barrier.
- Passes placental barrier. - Slightly bound to plasma
- Highly bound to plasma proteins. proteins.
- 75% is metabolized mainly by - 95% is metabolized by:
conjugation with glucuronic acid conjugation with glucuronic
and glycine, 1% oxidized into acid and sulphate (major
gentisic acid. pathway), and oxidation
- 25% is excreted unchanged in into NABQI (minor
urine (excretion is enhanced by pathway).
alkalinization of urine). - 5% excreted unchanged.
Mechanism of Inhibition of PG synthesis centrally Inhibition of PG synthesis
action: and peripherally by irreversible centrally by reversible
non-selective COX inhibition. selective COX-3 inhibi on.
Pharmacological Analgesic Antipyretic Analgesic Antipyretic only.
actions: Antiinflammatory Antiplatelet
Uricosuric.
Indications: 1. Analgesic in superficial pains. 1. Analgesic in superficial
2. Antipyretic in fever. pains.
3. Anti-inflammatory in RF, RA, OA. 2. Antipyretic in fever.
4. Antiplatelet for prophylaxis of
thrombo-embolic diseases.
Adverse effects: Allergy Bronchospasm Gut upset Allergy Acute toxicity.
and ulceration Bleeding-
Teratogenicity, delayed labor, and
premature closure of DA Salicylism
Hemoly c anemia in G6PD
deficiency Reye's syndrome
Acute toxicity.
Contraindications: Allergy-bronchial asthma-peptic
ulcer-pregnancy-favism-bleeding
disorders children with viral
infections (as influenza).
29 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Treatment of Gout
Gout is a disease characterized by: hyperuricemia (serum uric acid > 6 mg. %),
precipitation of mono-sodium urate crystals in the synovium of joints causing recurrent
acute attacks of gouty arthritis which may affect any joint but more commonly occurs in
the metatarso-phalangeal joint of the big toe. Gout may lead to the formation of renal
urate stones which may cause urate (gouty) nephropathy .
Causes:
1. Primary metabolic disorder in purine metabolism leading to excessive synthesis of
uric acid.
2. Cancer: causing increased turn over of purines into uric acid.
3. Drugs that increase serum uric acid as thiazide and loop diuretics, diazoxide, cancer
chemotherapy, some anti-tuberculous drugs as pyrazinamide and ethambutol, and
clofibrate (anti-hyperlipidemic drug).
Uric acid is synthesized from purines by the action of xanthine oxidase as follows:
X.O. X.O.
Purines---------Hypoxanthines---------Xanthines---------Uric acid
(X.O.: Xanthine Oxidase).
Uric acid undergoes 3 processes in the nephrons: ltra on, reabsorp on, and tubular
secretion.
Pathogenesis of acute gouty arthritis:
1. Precipitation of mono-sodium urate crystals (insoluble) in the synovial membrane of
joints causes inflammatory reaction.
2. Migration of phagocytic cells (polymorpho-nuclear leucocytes = PMNL) towards the
inflamed joint (chemotaxis).
3. Phagocytosis of mono-sodium urate crystals by the phagocytic cells.
4. Rupture of the phagocytic cells and release of glycoprotein (the main inflammatory
mediator) and lactic acid which causes acidity of the joint thus favoring more
precipitation of mono-sodium urate crystals and a vicious circle goes on.
30 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Drug Therapy of gout:
I. Treatment of acute gouty arthritis:
Anti-inflammatory drugs:
1. Colchicine and demecolcine (drugs of choice because they are specific anti-
inflammatory in acute gouty arthritis).
2. NSAIDs as indomethacin, diclofenac, ibuprofen, piroxicam, and others. They are used
in patients who can not tolerate colchicine.
3. Glucocorticoids (cortisone) and ACTH: if NSAIDs are ineffective.
II. Treatment of chronic gout (Prophylactic treatment):
a) Uricosuric drugs:
1. Probenicid.
2. Sulphinpyrazone.
3. Benzbromarone.
4. Aspirin (> 5 g. / day): not commonly used because of serious adverse effects.
b) Uricostatic drug:
Allopurinol inhibits uric acid synthesis by inhibition of xanthine oxidase enzyme.
N.B.:
1. Colchicine is also used in prophylaxis of gout.
2. Rasburicase:
It is a recombinant urate oxidase enzyme.
It oxidizes uric acid (insoluble) into allantoin (soluble).
It is used in hyperuricemia due to cancer chemotherapy and radiotherapy.
Adverse effects: Allergy (anaphylaxis) hemolysis in G6PD deciency GIT
disturbance- expensive.
Colchicine:
Source: plant origin (colchicum).
Chemistry: alkaloid.
Pharmacokinetics:
- Absorbed orally, may be given IV.
- Passes BBB and may cause severe CNS depression in toxic doses.
- Passes placental barrier and may cause teratogenicity.
- Excreted in urine and bile.
31 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Pharmacodynamics:
- Mechanism of action: binds to microtubular protein (tubulin) of phagocytic cells
leading to inhibition of: migration, phagocytosis, rupture of phagocytic cells, release
of glycoproteins and lactic acid. This breaks the vicious circle occurring in acute gouty
arthritis.
- Pharmacological actions:
1. Specific anti-inflammatory in acute gouty arthritis.
2. Antimitotic by binding to and inhibition of the mitotic spindle.
Therapeutic uses:
1. Acute gouty arthri s (1mg. = 2 tablets at the start of therapy followed by 0.5 mg. = 1
tablet every 2 hours un l pain is relieved or diarrhea occurs).
2. Prophylac c treatment in gout (0.5 mg. 2-3 mes / week).
3. Prophylaxis against attacks of Mediterranean fever = familial paroxysmal
polyserositis.
4. To improve liver functions in liver cirrhosis (?).
5. Treatment of psoriasis.
Adverse effects:
1. GIT disturbances are the most common adverse effects: nausea, vomiting, and
diarrhea.
2. On chronic use: alopecia (reversible)-bone marrow depression-myopathy-
nephrotoxicity-hepatotoxicity.
3. In acute toxicity: hemorrhagic gastro-enteritis (bloody diarrhea)-nephrotoxicity
(hematuria and anuria)-vascular damage-CNS depression.
Uricosuric drugs:
They increase uric acid excretion in urine by inhibition of uric acid reabsorption from PCT.
They should be given in large doses because small doses inhibit uric acid secretion and will
worsen gout.
1. Probenicid:
Adverse effects: allergic reactions (rash or fever) and GIT disturbances.
Drug interactions:
a) Inhibits tubular secretion of penicillinlonger duration of action.
b) Inhibits tubular secretion of thiazides and loop diureticsantagonism of their
diuretic action (they act from the inner side of the nephron).
32 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
2. Sulphinpyrazone.
It is a pyrazolone derivative.
It has uricosuric and antiplatelet actions bou no analgesic, antipyretic, or anti-
inflammatory actions.
Drug interaction: displaces warfarin and oral hypoglycemic drugs from plasma
proteins.
3. Benzbromarone.
4. Aspirin (> 5 g. / day): not commonly used because of serious adverse eects.
Important notes:
1. Patients treated with uricosurics should drink plenty of fluids and receive NaHCO3 to
render the urine alkaline to avoid precipitation of urate crystals in the nephrons which
may lead to the formation of urate stones and may end in urate nephropathy.
2. Uricosuric drugs should be avoided in patients already excreting large amounts of uric
acid in urine and in patients with history of recurrent urate stones or urate nephropathy.
Inhibitor of uric acid synthesis (uricostatic):
Allopurinol (Zyloric):
Pharmacokinetics: absorbed orally passes BBB- metabolized into alloxanthine (active
metabolite) - excreted in urine.
Pharmacodynamics: inhibits uric acid synthesis from xanthines and hypoxanthines by
competitive inhibition of xanthine oxidase (xanthines and hypoxanthines are increased
but they are soluble).
Therapeutic uses: prophylaxis of gouty attacks in chronic gout, especially in the following
conditions:
1. Gouty (urate) nephropathy.
2. Recurrent urate stones.
3. Patients who cannot tolerate uricosurics.
4. Failure to reduce hyperuricemia by uricosurics.
Adverse effects:
1. Hypersensitivity reactions: rash, fever, bone marrow depression.
2. GIT upsets: nausea, vomiting, diarrhea.
3. CNS disturbances: headache, vertigo.
4. Precipitation of acute gouty arthritis at the start of treatment, so colchicines is added.
5. Others: peripheral neuritis, malaise.
33 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Drug interactions:
1. Decreases metabolism of warfarin and may cause bleeding (allopurinol is a HME
inhibitor).
2. Decreases metabolism of mercaptopurine (anti-cancer) - which is metabolized by
xanthine oxidase and may cause toxicity.
N.B. Reduce the dose of warfarin and mercaptopurine in patients treated with allopurinol.
Drugs causing hyperuricemia:
1. Thiazides and loop diuretics.
2. Diazoxide (antiy-hypertensive arteriodilator-thiazide like).
3. Some anti-tuberculous drugs as: pyrazinamide and ethambutol.
4. Clofibrate (anti-hyperlipidemic).
5. Anticancer drugs.
6. Uricosuric drugs in small doses.
Gouty patients should avoid eating red meat, liver, fava beans, and nuts. However;
methyxanthine beverages as coffee, tea, and cola are allowed because they are
metabolized into "methyl" uric acid which is a soluble compound.
Anti-Parkinsonian Drugs
Parkinsonism (Parkinson's disease):
It is a neuro-degenerative disorder of the basal ganglia leading to disturbance of the
voluntary motor activity characterized by: hypokinesia =bradykinesia (difficulty to start
voluntary movements), rigidity (causes kyphosis, shuffling gate, and mask face), static
tremors, postural instability, salivation, and may be accompanied by depression.
Parkinsonism is considered as imbalance between dopamine (deficient) acting on D2-
receptors, and acetylcholine (relatively increased) acting on M-receptors in basal ganglia
(nigrostriatum).
Causes:
I. Idiopathic degeneration of dopaminergic neurons in the basal ganglia (may be related
to atherosclerosis, repeated trauma, environmental pollutants, or genetic
predisposition).
II. Secondary: following encephalitis and drugs (iatrogenic Parkinsonism):
1. D2- blockers as:
a) Typical Anti-psychotics (phenothiazines as chlorpromazine, and
butyrophenones as haloperidol and droperidol).
34 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
b) Anti-emetics as metoclopramide.
These drugs induce Parkinsonism if administered for large doses for about 3
months. Iatrogenic Parkinsonism due to D2 blockers can be prevented and
treated by anticholinergic drugs.
2. Drugs that deplete dopamine in CNS as reserpine.
3. Drugs that inhibit synthesis of dopamine as -methyl dopa.
4. MPTP (Methyl Phenyl Tetrahydro Pyridine) which destroys dopaminergic neurons
(MPTP is a narcotic drug related to meperidine which is now used to induce
Parkinsonism in experimental animal models).
III. Wilson's disease.
Aim of treatment is to restore the balance between dopamine and acetylcholine by
stimulation of D2-receptors (by increasing the level of dopamine or by other D2-agonists)
and / or by blocking M-receptors by anti-muscarinic drugs.
Accordingly; anti-parkinsonian drugs are classified into:
a) Dopaminergic drugs: they stimulate D2-receptors and include:
1. L-dopa in combination with peripheral dopa decarboxylase inhibitors (PDD-I) as
Carbidopa and Benserazide.
2. Direct Dopamine (D2) Agonists, which are either:
a) Ergolines (ergot derivatives): Bromocriptine -Pergolide-Lisuride.
b) Non-ergolines: Pramipexole and Ropinirole.
3. Deprenyl = Selegiline: selective MAO-B inhibitor.
4. COMT Inhibitors as Tolcapone and Entacapone.
5. Amantadine.
b) Anti-muscarinic (anti-cholinergic drugs):
1. Natural belladonna alkaloids: atropine and hyoscine (not used due to various
adverse effects).
2. Synthetic atropine substitutes: Benztropine- Benzhexol (trihexphenidyl)-Biperiden.
3. Seda ng (1st generation) anti-histaminics having potent atropine-like action:
diphenhydramine-orphenadrine.
Important notes:
1. Anti-muscarinic drugs are more effective in treating tremors, rigidity, and salivation but
have little or no effect on bradykinesia.
2. They prevent and treat Parkinsonism caused by typical anti-psychotics (dopaminergic
drugs would be ineffective).
3. They may be added to dopaminergic drugs (add on therapy)
4. Adverse effects: tachycardia-dry mouth-constipation-urine retention-blurred vision and
glaucoma-may cause CNS disturbances as confusion and hallucination.
5. They are contraindicated in glaucoma and benign prostatic hyperplasia.
N.B.: Beta-blockers as Propranolol may be used to control Parkinsonian tremors.
35 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Dopaminergic Drugs:
1. L-Dopa:
Dopamine itself is ineffective in treatment of Parkinsonism as it can not penetrate BBB.
L-dopa is used because it is the precursor of dopamine but only 5 % of L-dopa is
converted into dopamine in CNS by the action of central dopa decarboxylase (CDD)
enzyme.
About 95 % of L-dopa is converted into dopamine by the action of peripheral dopa
decarboxylase (PDD) enzyme in GIT (90%), blood and peripheral ssues (5%) into
dopamine which in turn can not pass BBB.
That is why L-dopa should be combined with peripheral dopa decarboxylase inhibitors
(PDD-I) as carbidopa or benserazide in a "xed combina on" in a ra o of 10:1 or 4:1 as
follows:
L-dopa (100 mg. or 250 mg.) + carbidopa (10 mg. or 25 mg.) = Sinemet
L-dopa (100 mg.) + benserazide (25 mg.) = Madopar
Part of L-dopa is converted by COMT into 3-O-methyl dopa which competes with L-dopa
for active uptake into CNS (uptake of L-dopa occurs by a transporter known as L-amino
acid transporter = LAT).
That is why COMT inhibitors as tolcapone and entacapone may be given with L-dopa /
carbidopa combination.
Pharmacokinetics:
- Absorption: L-dopa is absorbed orally by active transport which is decreased by the
presence of food especially amino acids which compete with L-dopa for the active
transporter LAT.
That is why it is better administered on empty stomach.
- Distribution: L-dopa passes BBB (see before).
- Fate: L-dopa is converted into dopamine inside CNS by the action of CDD. Dopamine
is metabolized by:
1. MAO-B and COMT into an inactive metabolite known as homo-vanillic acid (HVA)
which is excreted in urine.
2. MAO-B metabolizes dopamine into another inactive metabolite known as Di-
hydroxy-phenyl-acetic acid (DOPAC) which is also excreted in urine.
DOPAC interacts with H2O2 leading to formation of toxic oxidative metabolites
which destroy dopamine storage vesicles and loss of response to L-dopa therapy
with continous use (see adverse effects).
Pharmacodynamics:
L-dopa is decarboxylated into dopamine by the action of dopa decarboxylase in CNS.
Dopamine stimulates D2-receptors in basal ganglia.
Give reason: L-dopa is considered as a "prodrug".
36 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Therapeutic use:
Treatment of Parkinsonism; it improves rigidity and bradykinesia better than tremors.
Treatment is usually started with small doses then gradually increased. Best results are
obtained in the rst 3-4 years.
Adverse effects:
a) CNS manifestations:
1. Euphoria, anxiety, agitation, insomnia, psychological disturbances as confusion,
delusions, hallucinations, and aberrant (abnormal) sexual behaviour.
This requires either reduction of the dose of L-dopa, or adding an "atypical"
antipsychotic as Clozapine.
2. Dyskinesia (abnormal involuntary movements as chorea and athetosis which is
corrected by dose reduction).
b) CVS manifestations: postural hypotension (D1 stimulation), tachycardia (direct 1
stimulation and reflexly due to hypotension), arrhythmias (extrasystoles).
Hypertension occurs with large doses or with non-selective MAO inhibitors (1
stimulation).
c) GIT manifestations: anorexia, nausea, and vomiting due to stimulation of D2-
receptors in CTZ. Tolerance may develop to this adverse effect, but if nausea and
vomiting persist, antiemetics are given; e.g. domperidone (D2 antagonist which does
not pass BBB) but not metoclopramide (why?).
Constipation and bleeding peptic ulcer may occur.
d) Eye: active mydriasis and increased IOP which may precipitate glaucoma.
e) Fluctuation in drug response:
1. On-Off phenomenon: may be due to variable levels of dopamine in CNS (rapid rise
the drug is "on", rapid fall the drug is "o").
2. Wear off phenomenon: no more response to the drug following several years of
continous treatment. This may be due to the interaction of DOPAC with H2O2
leading to formation of toxic oxygen free radicals which destroy dopamine storage
vesicles (this can be prevented by adding selective MAO-B inhibitors as deprenyl).
3. End of dose Akinesia.
Management of fluctuation of drug response:
1. Increase the frequency of L-dopa intake.
2. Use slow release (controlled release) preparations as Sinemet CR.
3. Add long acting direct dopamine agonists as bromocriptine and pergolide.
4. Drug holiday for 3-21 days.
37 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
f) Sudden withdrawal of L-dopa leads to severe rebound Parkinsonian rigidity.
Contraindications:
1. Psychosis.
2. Glaucoma (especially narrow angle).
3. Peptic ulcer.
4. CVS diseases (arrhythmias).
5. Unfavorable drug interactions (see later).
Drug interactions:
a) Favorable (desirable) drug interactions:
1. L-dopa is potentiated by ant-muscarinic drugs.
2. With PDD inhibitors as cabidopa and benserazide (PDD-I allowed the use of smaller
doses of L-dopa leading to reduction in peripheral adverse effects but increased
central adverse effects) .
3. With COMT inhibitors as tolcapone and entacapone: inhibit synthesis of 3-o-methyl
dopa which competes with L-dopa for CNS uptake.
4. With selective MAO-B inhibitor (selegiline) which increases CNS levels of dopamine
and prevents synthesis of DOPAC (see before).
b) Unfavorable (undesirable) drug interactions:
1. L-dopa / carbidopa is antagonized by vitamin B6 (pyridoxine) which stimulates
peripheral dopa decarboxylase.
2. L-dopa is antagonized by drugs inducing iatrogenic Parkinsonism as D2-antagonists
and drugs decreasing dopamine in CNS (reserpine and -methyl dopa).
3. With non-selective MAO inhibitors: severe hypertension may occur due to reduced
metabolism of noradrenaline, adrenaline, and dopamine (treated by alpha blockers
as Prazosin).
4. Non-selective MAO inhibitors should be stopped 2 weeks before giving L-dopa.
5. Foods rich in amino acids interfere with absorption of L-dopa from GIT (drug-food
interaction).
2. Bromocriptine:
Chemistry: ergoline = ergot derivative.
Pharmacokinetics:
- Absorbed orally.
- Passes BBB.
- Extensively metabolized by the liver.
38 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Pharmacodynamics:
- Mechanism of action: agonist on D2 and partial agonist on D1.
- Pharmacological actions:
1. Anti-parkinsonian.
2. Inhibits prolactin release.
3. Inhibits growth hormone and ACTH release.
Therapeutic uses:
1. Parkinsonism (alone =monotherapy, or with sinemet=add on therapy).
Advantages over L-dopa/Carbidopa:
Longer t 1/2 and less uctua on in response.
Not affected by presence of food as it does not compete with amino acid for
active transport carriers.
No synthesis of toxic oxidative metabolites.
No need for metabolizing enzymes (dopa decarboxylase).
More specific action on D2 receptors.
2. Treatment of hyperprolactinemia (hyperprolactinemia causes galactorrhea-
amenorrhea syndrome in females, and loss of libido-gynecomastia-impotence in
males).
3. Suppression of lactation (safer than estrogen).
4. Acromegaly and ACTH-dependent tumors.
Adverse effects:
1. CNS: anxiety, insomnia, and hallucinations. Dyskinesia is less marked than with L-
dopa.
2. CVS: first-dose hypotension and collapse (especially if the patient is receiving anti-
hypertensive drugs)-digital vasospasm.
3. GIT: anorexia, nausea, vomiting, dyspepsia, constipation, and sometimes bleeding
peptic ulcer.
4. Allergy: skin eruption.
5. Erythromyalgia: painful, tender, red, hot, swollen feet.
3. Pergolide-Lisuride: ergolines (ergot derivatives) act as agonists on D2 and D1
receptors.
4. Pramipexole and Ropinirole: non-ergot dopaminergic agonists.
39 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
5. Amantadine:
Anti-viral used in prophylaxis of influenza A.
Anti-parkinsonian by increasing dopamine release and inhibiting neuronal reuptake.
Adverse effects:
1. CVS: Ankle edema, hypotension, CHF.
2. CNS: Ataxia, confusion, hallucination, insomnia, irritability, and even acute toxic
psychosis.
3. GIT upset.
6. Selegiline (Deprenyl):
selective MAO-B inhibitor usually added to L-dopa/carbidopa to enhance its action and to
prvent formation of DOPAC.
7. Tolcapone and Entacapone:
They are COMT inhibitors which inhibit synthesis of 3-O-methyl dopa which competes
with L-dopa for uptake into CNS.
They are used in combination with L-dopa/carbidopa.
Tolcapone may cause serious fulminating hepatic necrosis, but entacapone is less toxic
(no hepatotoxicity).
Drugs contraindicated in Parkinsonism =Iatrogenic Parkinsonism:
1. D2-antagonists that block D2-receptors in CNS:
a) Neuroleptics (anti-psychotics): Phenothiazines (e.g.chlorpromazine) and
Butyrophenones (as haloperidol).
b) Anti-emetics as metoclopramide.
2. Reserpine: inhibits storage of dopamine causing its depletion.
3. Alpha-methyl dopa: inhibits dopa decarboxylase and accordingly inhibits synthesis of
dopamine.
4. Muscarinic agonists that can pass BBB as physostigmine and pilocarpine.
5. MPTP.
Psychotropic Drugs
Psychotropic drugs include all drugs that affect mood, psychology (behavior, thoughts, and
emotional state), and CNS activity, they include:
I. Tranquillizers (Psycholeptics):
They are further subdivided into:
a) Minor tranquillizers = Anxiolytics = Antianxiety drugs:
These drugs are used in treatment of anxiety disorders as panic disorders, phobias,
and stress disorders. Examples include Benzodiazepines (e.g. Diazepam), Zolpidem,
Buspirone.
40 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
b) Major tranquillizers = Neuroleptics = Antipsychotics:
These drugs are used in treatment of psychotic disorders as schizophrenia. They are
subdivided into:
1. Typical Antipsychotics: they act mainly by blocking D receptors (mainly D2) in the
limbic system but also block D2 receptors in other areas of CNS leading serious
adverse effects as Parkinsonism and hyperprolactinemia.
Typical antipsychotics include the following chemical derivatives:
Phenothiazines as Chlorpromazine, Thioridazine, and Trifluperazine.
Butyrophenones as Haloperidol, and Droperidol.
Thioxanthenes as Thiothixene.
2. Atypical Antipsychotics: they act by more selective block of D2 receptors in limbic
system, and/ or by blocking 5-HT2 receptorsin limbic system and accordingly they
have much less adverse effects.
Examples include: Pimozide, Sulpiride, Clozapine, Risperidone, Olanzepine.
II. Antidepressants (Psychanaleptics) and Lithium (Antimanic and mood stabilizer).
These drugs elevate mood in patients with psychic depression. They are classified
according to the mechanism of action -into:
1. Tri-cyclic Antidepressants (TCAs).
2. MAO-Inhibitors.
3. Selective Serotonin Reuptake Inhibitors (SSRIs).
4. Atypical Antidepressants.
III. Psychotomimetics = Hallucinogenics = Psychedelics:
e.g. LSD.
IV. Psychomotor stimulants = Psychostimulants:
These drugs induce euphoria, wakefulness, alertness, and antifatigue actions. Examples
are: Methylxantines (as Caffeine), Cocaine, Amphetamine and amphetamine derivatives,
Atropine (Datura).
41 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Anti-Psychotic Drugs
(Neuroleptics Major Tranquillizers)
Anti-psychotic drugs are used in treatment of psychotic disorders as schizophrenia.
Psychosis: disorder in thoughts, behavior, and emotions characterized by positive signs
as hallucinations (usually auditory) and delusions (fixed false belief commonly paranoid),
and negative signs as emotional dullness (emotional blunting), dementia, and social
withdrawal (poor socialization).
Psychosis may be due to increased activity of dopamine-stimulating D2-receptors- and /
or serotonin-s mula ng 5-HT2-receptors- in the limbic system.
Dopaminergic receptors:
- There are 5 subtypes of dopaminergic receptors.
- D1 and D5 are coupled to Gs s mula on of adenyl cyclase increase c-AMP
synthesis.
- D2,3,4 are coupled to Gi inhibi on of adenyl cyclase and reduc on of c-AMP,
increase in K+ efflux, and decrease in Ca2+ influx.
Site D2-Agonists D2-Antagonists
(Dopamine)
1-Limbic system: Euphoria-Anxiety-Psychosis. Anti-Psychotic.
2-C.T.Z.: Nausea and vomiting (except Anti-emetics except in motion
motion sickness). sickness.
3-Basal ganglia: Anti-Parkinsonism. Induce iatrogenic Parkinsonism or
extrapyramidal manifestations.
4-Hypothalamus: - Inhibit prolactin. - Hyperprolactinemia.
- Increase heat formation - Decrease heat formation and
(increase body temperature). may lower normal body
temperature (Hypothermia).
- Reduce appetite. - Increase appetite and may cause
weight gain.
42 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Classification of Anti-Psychotic Drugs:
a) Typical Antipsychotics:
They are non-selective D2-antagonists, used as anti-psychotic and anti-emetic drugs
except in motion sickness, and may lead to Parkinsonism (extrapyramidal
manifestations) and hyperprolactinemia.
1. Phenothiazines: e.g. chlorpromazine, thioridazine , and trifluperazine.
2. Butyrophenones: e.g. haloperidol, and droperidol..
3. Thioxanthenes: e.g. thiothixene, chlorprothixene, zuclopenthixol, and flupenthixol.
b) Atypical Anti-psychotics: e.g. clozapine (may cause agranulocytosis), risperidone,
sulpiride, loxapine, pimozide and molindone.
They cause less extrapyramidal manifestations.
They are more effective in refractory cases of schizophrenia.
They improve the negative signs of schizophrenia.
Pimozide and Sulpiride: block D2 selectively in the limbic system.
Clozapine: blocks D4 and 5-HT2, but it has a high incidence of agranulocytosis (1-2% of
patients).
Risperidone: blocks equally D2 and 5-HT2.
Olanzepine: blocks 5-HT2 more than D2.
Chlorpromazine
Source: synthetic.
Chemistry: phenothiazine derivative.
Pharmacokinetics:
- Absorbed orally.
- Passes BBB.
- Passes placental barrier and may cause teratogenicity.
- Metabolized by the liver and metabolites are excreted in urine.
Pharmacodynamics:
- Mechanism of action: as anti-psychotic it acts mainly by blocking D2-receptors in the
limbic system.
43 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
- Pharmacological actions:
The pharmacological actions of chlorpromazine can be expected from the following
information:
1. Blocks D2-receptors in the limbic systemAnti-psychotic action.
2. Blocks D2-receptors in CTZAnti-emetic action except in motion sickness.
3. Blocks D2-receptors in basal gangliainduce iatrogenic Parkinsonism
and other extrapyramidal manifestations.
4. Blocks D2-receptors in the hypothalamusHyperprolacinemia, Hypothermia, and
increased appetite.
5. Blocks 1-receptorspostural hypotension, reflex tachycardia, and delayed
ejaculation.
6. Blocks 5-HT2 receptors in CNSAnti-psychotic and increased appetite.
7. Blocks H1-receptors Anti-allergic action.
8. Blocks M-receptors = Atropine-like action tachycardia, dry mouth, cons pa on,
urine retention, and elevation of IOP.
9. Blocks Nn-receptors = ganglion blocking action postural hypotension and
tachycardia.
10.Blocks Nm-receptors = Skeletal muscle weakness (curare-like action).
11.Blocks Na+-channels = Membrane stabilization Quinidine-like action on the heart
and local anaesthetic action.
12.Inhibits neuronal uptake (uptake I) of noradrenaline.
(Chlorpromazine is a potent D2, 1, and 5-HT2 blocker and weak H1, M, and N-
blocker).
The pharmacological actions of chlorpromazine are classified into:
a) CNS actions:
1. Anti-psychotic action (by blocking D2-receptors in limbic system).
2. Anti-emetic action (by blocking D2-receptors in CTZ) except in motion sickness.
3. Induction of Parkinsonism and other extrapyramidal manifestations (due to block of
D2-receptors in basal ganglia).
4. Increase in prolactin release (hyperprolactinemia) (due to block of D2-receptors in
hypothalamus).
5. Hypothermia due to increased heat loss (by inhibition of the hypothalamic heat
regulating centre and V.D. of skin blood vessels) and decreased heat formation (by
inhibition of shivering).
6. Increases appetite and causes weight gain (by blocking D2-receptors in
hypothalamus).
7. May cause seizures (convulsions) in epileptic patients.
8. Potentiates CNS depressants as analgesics, sedatives (as benzodiazepines), and
alcohol.
44 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
b) CVS actions:
1. Heart: tachycardia (reflex due to hypotension, due to atropine-like action, and
ganglion blocking action) negative inotropic action (myocardial depression) due to
quinidine-like action.
2. Blood vessels: vasodilatation of both veins and arteries due to 1-blocking action,
ganglion blocking action, inhibition of VMC and direct vasodilatation.
3. Increases coronary flow.
4. BP: postural hypotension due to V.D. and myocardial depression.
c) Receptor blocking action:
1. Potent D2-blocker.
2. Potent 1-blocker.
3. Potent 5-HT2-blocker.
4. Weak M-blocker (atropine-like action).
5. Weak H1-blocker (anti-histaminic action).
6. Weak ganglion blocker.
7. Weak neuro-muscular blocker (curare-like action).
d) Endocrine actions:
1. Increases prolactin release by blocking D2-receptors in hypothalamus.
2. Decreases ACTH, FSH, and LH (may lead to amenorrhea and infertility in females).
e) Other actions:
1. Na+-channel blocker = membrane stabilization (local anaesthetic action and
quinidine-like action).
2. Inhibits neuronal uptake (uptake I) of noradrenaline (and drugs that undergo uptake I
as guanethidine).
Therapeutic uses:
1. Anti-psychotic in treatment of schizophrenia. Typical antipsychotics improve mainly
the positive signs of schizophrenia as delusions and hallucinations.
2. Anti-emetic in treatment of nausea and vomiting except in motion sickness (not
effective) and in vomiting of pregnancy (contraindicated as it may cause
teratogenicity).
3. The anti-emetic doses are lower than the doses used as anti-psychotic.
4. Treatment of intractable (severe and persistent) hiccough.
5. Pre-anaesthetic medication (to reduce anxiety and inhibit vomiting).
6. Hypothermic agent during cardio-pulmonary surgery.
7. Anti-pruritic in treatment of itching.
45 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Adverse effects Contraindications
1. Allergic reactions: dermatitis- photosensitivity- 1. Allergy and liver diseases.
blood dyscrasias-corneal and skin deposits-
cholestatic jaundice (allergic obstructive hepatitis).
2. Parkinsonism and extrapyramidal manifestations 2. Parkinsonism.
as: akathisia (restless involuntary movements)-
acute dystonia-tremors. This can be prevented by
antimuscarinic drugs.
3. Tardive dyskinesia (abnormal involuntary
movements on prolonged use of chlorpromazine,
may be due to up-regulation of D receptors.There
is no specific treatment but can be prevented by
lithium).
4. Seizures in epileptic patients. 3. Epilepsy.
5. Teratogenicity. 4. Pregnancy.
6. Hyperprolactinemia leading to galctorrhea-
amenorrhea in females, gynecomastia, impotence,
and loss of libido in males.
7. Increased appetite and weight gain.
8. Atropine-like adverse effects: tachycardia, dry 5. Glaucoma and enlarged prostate.
mouth, constipation, urine retention, and
elevation of IOP.
9. Postural hypotension. 6. Hypotension.
10. Neuroleptic Malignant Syndrome: idiosyncratic 7. Idiosyncracy.
reaction similar to malignant hyperthermia,
treated by cooling and IV dantrolene..
11. Delayed ejaculation.
46 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Drug interactions:
1. Potentiates the actions of:
- Sedatives as alcohol, benzodiazepines, and barbiturates.
- Analgesics as morphine.
- Anticholinergic drugs as atropine.
- Vasodilators and other hypotensives.
- Skeletal muscle relaxants as curare.
2. The hypotensive action of chlorpromazine is mainly due to its 1-blocking action and
accordingly is not treated by adrenaline (more hypotension will occur = adrenaline
reversal).
3. Antagonizes the anti-hypertensive action of guanethidine (chlorpromazine inhibits
neuronal uptake of guanethidine).
Other Phenothiazines:
Trifluperazine:
Similar to chlorpromazine but is a more powerful D2 antagonist and accordingly is a more
potent antipsychotic but with more extrapyramidal manifestations.
Thioridazine:
Similar to chlorpromazine but is less potent D2 antagonist.
1. Not antiemetic.
2. Rare extrapyramidal manifestations.
3. Side effects: as chlorpromazine + Cardiotoxicity + Retinopathy.
Anti-Convulsant Drugs (Anti-Epileptic)
Epilepsy: is a CNS disorder due to the presence of hyper-excitable neurons-known as
epileptic focus-leading to abnormal behavior, loss of consciousness, and / or convulsions.
Types of epilepsy:
1. Generalized tonic-clonic seizures (grand mal epilepsy).
2. Absence seizures (petit mal epilepsy).
3. Myoclonic seizures.
4. Partial seizures.
5. Status epilepticus (severe sustained seizures which may be fatal).
General principles in treatment of epilepsy:
1. Use the minimal number of anti-epileptic drugs to avoid drug interactions.
2. Treatment should be con nued for 2-3 years a er the last seizure.
3. Anti-epileptic drugs should be gradually withdrawn to avoid status epilepticus.
47 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Mechanism of action of anti-epileptic drugs:
1. Block of Na+-channels: by Phenytoin, Carbamazepine, and Valproic acid.
2. Block of voltage-gated Ca2+-channels (T-type): by Ethosuximide, and Valproic acid.
3. Blocking the receptors of excitatory transmitters as glutamate and aspartate: by
Felbamate.
4. Potentiation of the inhibitory action of GABA: by Benzodiazepines, Barbiturates, Valprioc
acid, and Vigabatrin.
1. Phenytoin (Diphenylhydantoin):
Source: synthetic.
Chemistry: hydantoin derivative.
Pharmacokinetics:
- Well absorbed orally and can be given by injection.
- Passes BBB.
- Passes placental barrier and cause teratogenicity
- Bound to plasma proteins (displaces thyroxin and tri-cyclic antidepressants = TCAs;
but is displaced by aspirin, sulphonamides, and valproic acid).
- Metabolized by the liver by hydroxylation and conjugation. Saturation of
metabolizing enzymes occurs with large doses and elimination will follow "zero
order kinetics" and t 1/2 increases (remember aspirin).
- Metabolites are excreted in urine.
Pharmacodynamics:
- Mechanism of action: Na+-channel blocker (membrane stabilization).
- Pharmacological actions:
1. Anti-epileptic action.
2. Anti-arrhythmic action (class I-B anti-arrhythmic).
3. Hepatic microsomal enzyme (HME) inducer.
Therapeutic uses:
1. Treatment of epilepsy: in grand mal epilepsy, partial seizures, and may be used in
status epilepticus. It is not effective in petit mal epilepsy and may even worsen it.
2. Treatment of ventricular arrhythmias especially with heart block as in cases of
digitalis toxicity.
3. Treatment of neuropathic pains as trigeminal neuralgia.
48 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Adverse effects:
1. Gingival (gum) hyperplasia especially in children (irreversible).
2. GIT irritation (better given with meals).
3. Hypersensitivity reactions: rash, blood dyscrasias, and cholestatic hepatitis.
4. Teratogenic (fetal hydantoin syndrome: cleft lip, cleft palate, and cardiac septal
defect).
5. Cerebello-vestibular dysfunction: vertigo-ataxia-nystagmus-diplopia.
6. Hirsutism (may be due to increased androgen release).
7. Inhibits ADH and insulin release (may cause hyperglycemia).
Drug interactions:
- Induces its own metabolism tolerance to the anti-epileptic action.
- Induces metabolism of other drugs as digitoxin, theophylline, cortisone, and oral
contraceptives.
- Displaces thyroxine and TCAs from plasma proteins but is displaced by aspirin,
sulphonamides, and valproic acid.
- Other HME inducers as barbiturates and carbamazepine increase its metabolism.
- HME inhibitors as valproic acid and cimetidine decrease its metabolism and may
lead to phenytoin toxicity.
- Increases metabolism of vitamin K leading to hypoprothrombinemia and bleeding.
- Increases metabolism of vitamin D leading to hypocalcemia and osteoporosis.
- Increases metabolism of folic acid leading to folic acid deficiency anemia
(megaloblastic anemia) and increases toxicity of methotrexate (anticancer folate
antagonist).
Contraindications:
1. Pregnancy.
2. Allergy to hydantoins.
2. Carbamazepine (Tegretol):
Source: synthetic.
Chemistry: related to tri-cyclic antidepressants (TCAs).
Pharmacokinetics:
- Absorbed orally.
- Passes BBB.
- Passes placental barrier and may cause teratogenicity.
- Bound to plasma proteins.
- Metabolized by the liver.
49 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
Pharmacodynamics:
- Mechanism of action: Na+-channel blocker.
- Pharmacological actions:
1. Antiepilectic action.
2. HME inducer.
3. Stimulates ADH release (anti-diuretic action).
Therapeutic uses:
1. Treatment of epilepsy: grand mal and partial seizures but not in petit mal epilepsy.
2. Treatment of trigeminal neuralgia.
3. Treatment of central (pituitary) diabetes insipidus.
Adverse effects:
1. GIT irritation: nausea, vomiting, and diarrhea.
2. Hypersensitivity reactions: rash, blood dyscrasias, and cholestatic hepatitis.
3. Cerebello-vestibular dysfunction: ataxia, diplopia, nystagmus, and vertigo.
4. Fluid retention and dilutional hyponatremia due to anti-diuretic action.
5. Teratogenic (similar to fetal hydantoin syndrome).
6. Drug interactions: HME induction.
Contraindications:
1. Pregnancy.
2. Allergy.
3. Valproic acid (Sodium valproate):
Source: synthetic.
Pharmacokinetics:
- Absorbed orally.
- Passes BBB.
- Passes placental barrier and causes teratogenicity (Spina bifida).
- Highly bound to plasma proteins and displaces other drugs as phenytoin.
- Metabolized by the liver.
Pharmacodynamics:
- Mechanism of action:
1. Inhibits GABA transaminase the enzyme responsible for degradation of GABA-
leading to increase in the level of GABA.
2. Blocks Na+-channels.
3. Blocks voltage-gated Ca2+-channels (T-type).
50 Dr.Ahmed Abdel Rahman www.medadteam.org
Pharmacology of The C.N.S. 2011/2012
- Pharmacological actions:
1. Anti-epileptic.
2. HME inhibitor.
Therapeutic uses:
Treatment of all types of epilepsy (broad-spectrum anti-epileptic).
Adverse effects:
1. GIT irritation.
2. Transient alopecia.
3. Teratogenicity (spina bifida).
4. Bone marrow depression (thrombocytopenia).
5. CNS: ataxia and sedation.
6. Cholestatic jaundice (and may lead to hepatotoxicity).
Drug interactions:
- HME inhibition leading to decreased metabolism of phenytoin.
- Displaces phenytoin from plasma protein binding sites and increases its plasma
level.
4. Ehtosuximide:
Pharmacokinetics:
- Absorbed orally.
- Passes BBB.
- Mainly metabolized by the liver (75%) and partly excreted unchanged in urine
(25%).
Pharmacodynamics:
- Mechanism of action: blocks voltage gated Ca2+-channels (T- type).
- Pharmacological actions: Anti-epileptic.
Therapeutic uses:
Drug of choice in absence seizures (petit mal epilepsy.
Adverse effects:
1. GIT upset.
2. Allergy.
3. Drowsiness and mood changes.
4. Blood dyscrasias.
51 Dr.Ahmed Abdel Rahman www.medadteam.org
Vous aimerez peut-être aussi
- Business English Course BookDocument250 pagesBusiness English Course BookSoodn Kang Soodn100% (5)
- Uveal TractDocument11 pagesUveal TractSoodn Kang SoodnPas encore d'évaluation
- ScleraDocument2 pagesScleraSoodn Kang SoodnPas encore d'évaluation
- ConjunctivaDocument23 pagesConjunctivaSoodn Kang SoodnPas encore d'évaluation
- Pharm DR Ahmed Abd AlrahmanDocument24 pagesPharm DR Ahmed Abd AlrahmanAmrAliTahaPas encore d'évaluation
- RetinaDocument19 pagesRetinaSoodn Kang SoodnPas encore d'évaluation
- OrbitDocument9 pagesOrbitSoodn Kang SoodnPas encore d'évaluation
- Eyelid 2011Document25 pagesEyelid 2011Soodn Kang SoodnPas encore d'évaluation
- Lacrimal SystemDocument13 pagesLacrimal SystemSoodn Kang SoodnPas encore d'évaluation
- GlaucomaDocument24 pagesGlaucomaSoodn Kang SoodnPas encore d'évaluation
- 6 Diuretics UnlockedDocument17 pages6 Diuretics UnlockedSoodn Kang SoodnPas encore d'évaluation
- University of 6th October Faculty of Medicine Surgery Exam MCQsDocument10 pagesUniversity of 6th October Faculty of Medicine Surgery Exam MCQsSoodn Kang SoodnPas encore d'évaluation
- Epidemiology of CholeraDocument26 pagesEpidemiology of CholeraSoodn Kang SoodnPas encore d'évaluation
- Pharm Cvs McqsDocument30 pagesPharm Cvs McqsSoodn Kang Soodn100% (3)
- Antidote List 2009: Beaumont Hospital, P.O. BOX 1297, Beaumont Road, Dublin 9Document27 pagesAntidote List 2009: Beaumont Hospital, P.O. BOX 1297, Beaumont Road, Dublin 9Soodn Kang SoodnPas encore d'évaluation
- Case Studies in The Management of Acs With GP Iib/Iiia InhibitorsDocument47 pagesCase Studies in The Management of Acs With GP Iib/Iiia InhibitorsSoodn Kang SoodnPas encore d'évaluation
- LokalKeringesfokozok B12 Folsav STB ANGOL 2016-2-12Document14 pagesLokalKeringesfokozok B12 Folsav STB ANGOL 2016-2-12Soodn Kang SoodnPas encore d'évaluation
- Angol Oktatás - VTVSSVTDocument5 pagesAngol Oktatás - VTVSSVTSoodn Kang SoodnPas encore d'évaluation
- AntiarritmiasSzerek 2016-2-8Document30 pagesAntiarritmiasSzerek 2016-2-8Soodn Kang SoodnPas encore d'évaluation
- Local Anaesthetics Mcqs From LouisDocument2 pagesLocal Anaesthetics Mcqs From LouisSoodn Kang SoodnPas encore d'évaluation
- NSAID GUIDEDocument34 pagesNSAID GUIDESoodn Kang SoodnPas encore d'évaluation
- Hallgatok VeglegesDocument3 pagesHallgatok VeglegesSoodn Kang SoodnPas encore d'évaluation
- DermatologyDocument21 pagesDermatologySoodn Kang SoodnPas encore d'évaluation
- CardiologyDocument10 pagesCardiologySoodn Kang SoodnPas encore d'évaluation
- 2011 - Patient PresentationDocument12 pages2011 - Patient PresentationSoodn Kang SoodnPas encore d'évaluation
- Diagnosis 3Document10 pagesDiagnosis 3Soodn Kang SoodnPas encore d'évaluation
- Autonomic Drugs Flash CardsDocument16 pagesAutonomic Drugs Flash CardsSoodn Kang SoodnPas encore d'évaluation
- ورق مذاكره Ent في 100 صفحه بسDocument100 pagesورق مذاكره Ent في 100 صفحه بسSoodn Kang SoodnPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5783)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- ROA of AnimalsDocument23 pagesROA of AnimalsMr.White sheep MusicPas encore d'évaluation
- EE Tarek Exam Hints 2019-1Document83 pagesEE Tarek Exam Hints 2019-1Ibrahim Sayed AhmedPas encore d'évaluation
- Uji ToksisitasDocument17 pagesUji ToksisitasSri WahyuningsihPas encore d'évaluation
- Daftar Prodak Harga KhususDocument2 pagesDaftar Prodak Harga KhususLutfi QamariPas encore d'évaluation
- Medication for Motion Sickness and NauseaDocument1 pageMedication for Motion Sickness and NauseaCameron JanzenPas encore d'évaluation
- Master ObatDocument67 pagesMaster Obatbelahan jiwaPas encore d'évaluation
- Multiple VaccinationDocument1 pageMultiple VaccinationDark AghanimPas encore d'évaluation
- Dexmedetomidine: (Precedex - Abbott Laboratories)Document6 pagesDexmedetomidine: (Precedex - Abbott Laboratories)battreyPas encore d'évaluation
- List of Medicines, Medical Supplies, Facilities and InfrastructureDocument4 pagesList of Medicines, Medical Supplies, Facilities and InfrastructureAnshar ArifinPas encore d'évaluation
- Pediatric DosageDocument4 pagesPediatric DosageThe GalaxyPas encore d'évaluation
- Self Medication PracticeDocument25 pagesSelf Medication PracticeDafny CzarinaPas encore d'évaluation
- 5-Fluorouracil to Zentiva drugs manufacturer listDocument54 pages5-Fluorouracil to Zentiva drugs manufacturer listksdmksdmPas encore d'évaluation
- Dr. Dewi-Geriatric PharmacologyDocument41 pagesDr. Dewi-Geriatric PharmacologyAnne Gustriwati0% (1)
- PEMENANG PENAWARAN OBAT - PT. Novell Pharmaceutical LaboratoriesDocument28 pagesPEMENANG PENAWARAN OBAT - PT. Novell Pharmaceutical LaboratoriesRikoPas encore d'évaluation
- ElixirsDocument1 pageElixirsSOFIA ALEXIS MALIÑANAPas encore d'évaluation
- AdvairDocument1 pageAdvairE50% (2)
- Bioassays Seminar on TechniquesDocument31 pagesBioassays Seminar on TechniquesnikuPas encore d'évaluation
- Tachira P Paper ADC Breast Cancer-1 PDFDocument17 pagesTachira P Paper ADC Breast Cancer-1 PDFZeddicus Zu'l ZoranderPas encore d'évaluation
- AIIMS June 2020 DR Siraj Ahmad PDFDocument4 pagesAIIMS June 2020 DR Siraj Ahmad PDFadiPas encore d'évaluation
- Formulation, Development and Evalution of An Immediate Release Tablet of MethotrexateDocument22 pagesFormulation, Development and Evalution of An Immediate Release Tablet of MethotrexateDarlianaMelloSouzaPas encore d'évaluation
- PCO Answer Key-RED PACOPDocument40 pagesPCO Answer Key-RED PACOPViviengail GalosPas encore d'évaluation
- OmeprazoleDocument3 pagesOmeprazoleapi-3797941100% (3)
- PPGF 03.4 Safe Supply of Non-Prescription Medicines Containing DomperidoneDocument4 pagesPPGF 03.4 Safe Supply of Non-Prescription Medicines Containing Domperidoneforeveremarati90Pas encore d'évaluation
- Phenytoin: Phenytoin (PHT), Sold Under The Brand Name Dilantin AmongDocument13 pagesPhenytoin: Phenytoin (PHT), Sold Under The Brand Name Dilantin AmongMunna SahaniPas encore d'évaluation
- Psychedelic Drugs in Biomedicine. Review 2017Document14 pagesPsychedelic Drugs in Biomedicine. Review 2017Luis Henrique SalesPas encore d'évaluation
- Rang Dale S Pharmacology Self Assessment Questions 7th PDFDocument62 pagesRang Dale S Pharmacology Self Assessment Questions 7th PDFJohita Paz100% (8)
- LoperamidaDocument19 pagesLoperamidaGlo RyndaPas encore d'évaluation
- Ophthalmic Drug Delivery SystemsDocument749 pagesOphthalmic Drug Delivery Systemskulbhushan singh100% (2)
- Introduction To Essential DrugsDocument46 pagesIntroduction To Essential DrugsMrym NbPas encore d'évaluation
- PharmaLite - in Pharmacy Practice (PV Publication)Document276 pagesPharmaLite - in Pharmacy Practice (PV Publication)MD SALAHUDDIN SALAHUDDINPas encore d'évaluation