Académique Documents
Professionnel Documents
Culture Documents
Jurnal Pake 6 PDF
Transféré par
jayantiTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Jurnal Pake 6 PDF
Transféré par
jayantiDroits d'auteur :
Formats disponibles
The n e w e ng l a n d j o u r na l of m e dic i n e
original article
Effect of a Multifactorial Intervention
on Mortality in Type 2 Diabetes
Peter Gde, M.D., D.M.Sc., Henrik Lund-Andersen, M.D., D.M.Sc.,
Hans-Henrik Parving, M.D., D.M.Sc., and Oluf Pedersen, M.D., D.M.Sc.
A bs t r ac t
Background
From the Steno Diabetes Center, Copen- Intensified multifactorial intervention with tight glucose regulation and the use
hagen (P.G., H.L.-A., O.P.); Department of of reninangiotensin system blockers, aspirin, and lipid-lowering agents has been
Ophthalmology, Glostrup University Hos-
pital, Glostrup (H.L.-A.); Department of shown to reduce the risk of nonfatal cardiovascular disease among patients with
Medical Endocrinology, Rigshospitalet type 2 diabetes mellitus and microalbuminuria. We evaluated whether this approach
Copenhagen University Hospital, Copen- would have an effect on the rates of death from any cause and from cardiovascular
hagen (H.-H.P.); and Faculty of Health
Sciences, University of Aarhus, Aarhus causes.
(H.-H.P., O.P.) all in Denmark. Address
reprint requests to Dr. Pedersen at the Methods
Steno Diabetes Center, 2820 Gentofte, Co-
penhagen, Denmark, or at oluf@steno.dk. In the Steno-2 Study, we randomly assigned 160 patients with type 2 diabetes and
persistent microalbuminuria to receive either intensive therapy or conventional ther-
N Engl J Med 2008;358:580-91. apy; the mean treatment period was 7.8 years. Patients were subsequently followed
Copyright 2008 Massachusetts Medical Society.
observationally for a mean of 5.5 years, until December 31, 2006. The primary end
point at 13.3 years of follow-up was the time to death from any cause.
Results
Twenty-four patients in the intensive-therapy group died, as compared with 40 in
the conventional-therapy group (hazard ratio, 0.54; 95% confidence interval [CI],
0.32 to 0.89; P=0.02). Intensive therapy was associated with a lower risk of death
from cardiovascular causes (hazard ratio, 0.43; 95% CI, 0.19 to 0.94; P=0.04) and
of cardiovascular events (hazard ratio, 0.41; 95% CI, 0.25 to 0.67; P<0.001). One pa-
tient in the intensive-therapy group had progression to end-stage renal disease, as
compared with six patients in the conventional-therapy group (P=0.04). Fewer pa-
tients in the intensive-therapy group required retinal photocoagulation (relative risk,
0.45; 95% CI, 0.23 to 0.86; P=0.02). Few major side effects were reported.
Conclusions
In at-risk patients with type 2 diabetes, intensive intervention with multiple drug com-
binations and behavior modification had sustained beneficial effects with respect
to vascular complications and on rates of death from any cause and from cardiovas-
cular causes. (ClinicalTrials.gov number, NCT00320008.)
580 n engl j med 358;6 www.nejm.org february 7, 2008
The New England Journal of Medicine
Downloaded from nejm.org on November 28, 2015. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
Effect of Multither apy on Mortality in Type 2 Diabetes
T
ype 2 diabetes mellitus is associat- than 150 mg per deciliter (1.7 mmol per liter),
ed with a high rate of complications related a systolic blood pressure of less than 130 mm Hg,
to cardiovascular disease and diabetic ne- and a diastolic blood pressure of less than 80
phropathy, retinopathy, and neuropathy.1-3 The rate mm Hg. Patients were treated with blockers of
of death among patients with type 2 diabetes is the reninangiotensin system because of their
approximately twice as high as that among per- microalbuminuria, regardless of blood pressure,
sons without the disorder.2,3 However, trials of and received low-dose aspirin as primary preven-
interventions for single risk factors have shown tion.10,12 The numbers of patients who underwent
efficacy in reducing the development and progres- randomization, were assigned to receive treatment,
sion of complications.4-9 Furthermore, the risk of and completed the study and follow-up are shown
vascular complications was reduced by about half in Figure 1.
in the Steno-2 Study, our previous prospective, ran-
domized, open-label, blinded trial, during an av- Study Population
erage of 7.8 years of intensified multitarget inter- Of the 160 patients who were enrolled in the
vention aimed at concomitant risk factors.10 The Steno-2 Study, 27 died and 3 (including 1 patient
study encompassed treatment goals similar to in the intensive-therapy group) withdrew before
those recommended in the current guidelines of the end-of-trial examinations in 2001. All 130 re-
the American Diabetes Association.11 maining patients provided written informed con-
Although the number of deaths was lower in sent to continue participation in the observation-
the intensive-therapy group in the Steno-2 Study, al follow-up study after the intervention study
the relatively small number of patients who reached ended. The protocol for the follow-up study was
that end point precluded a determination of in accordance with the provisions of the Declara-
whether this approach affected mortality. There- tion of Helsinki and was approved by the ethics
fore, this follow-up to the Steno-2 Study was de- committee of Copenhagen County, Denmark.
signed to address the question of mortality, as well When the Steno-2 Study was completed, the
as whether the risk reductions already achieved structured treatment of patients in the intensive-
for both macrovascular and microvascular diseases therapy group stopped. However, all participating
were maintained during follow-up in a community patients in both study groups were informed in
setting. In the follow-up study, patients were ob- detail about the benefits of intensified multifac-
served for a mean of 5.5 years after the initial torial treatment, and the diabetes specialists to
trial had ended. whom the patients were referred were educated
about the new national recommendations for in-
Me thods tensified multitarget treatment on the basis of the
results of the Steno-2 Study. This education took
Study Design place both at regional and at national levels.14,15
Detailed information about the Steno-2 Study has This report includes follow-up data obtained from
been reported previously.10,12 Briefly, in 1993, a to- September 1, 2006, to December 31, 2006. At fol-
tal of 160 white Danish patients with type 2 diabe- low-up examination, 84% of patients in the inten-
tes (defined according to the criteria of the World sive-therapy group and 87% of those in the con-
Health Organization) and persistent microalbu- ventional-therapy group were still being treated
minuria were randomly assigned to receive either at diabetes clinics.
conventional multifactorial treatment, consistent
with the guidelines of the Danish Medical Asso- Procedures, Measurements, and End Points
ciation,13 or intensified, target-driven therapy in- End-point examinations were performed for both
volving a combination of medications and focused macrovascular and microvascular complications,
behavior modification. The intensive-therapy group and data regarding biochemical and clinical sta-
had defined targets consistent with the latest tus were obtained in both study groups. The mea-
guidelines of the American Diabetes Association. surements were obtained by a single laboratory
These targets included a glycated hemoglobin level technician who was not aware of the original study-
of less than 6.5%, a fasting serum total cholesterol group assignments.
level of less than 175 mg per deciliter (4.5 mmol The primary end point in the follow-up trial
per liter), a fasting serum triglyceride level of less was the time to death from any cause. It is man-
n engl j med 358;6 www.nejm.org february 7, 2008 581
The New England Journal of Medicine
Downloaded from nejm.org on November 28, 2015. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
315 Patients underwent screening
146 Were excluded
37 Declined to enroll
97 Had normoalbuminuria
7 Had macroalbuminuria
5 Had other exclusion
criteria
169 Had microalbuminuria
9 Were excluded because
they had a stimulated
serum C-peptide level
of <600 pmol/liter
160 Underwent stratification according to urinary
albumin excretion and then randomization
80 Were assigned to receive 80 Were assigned to receive
intensive therapy conventional therapy
12 Died 15 Died
7 Had cardiovascular disease 7 Had cardiovascular disease
2 Had cancer 5 Had cancer
3 Had other conditions 3 Had other conditions
1 Withdrew consent 2 Withdrew consent
67 Completed interventional study 63 Completed interventional study
12 Died 25 Died
2 Had cardiovascular disease 12 Had cardiovascular disease
10 Had other conditions 13 Had other conditions
55 Completed follow-up study 38 Completed follow-up study
Figure 1. Enrollment and Outcomes.
Three patients withdrew during follow-up because they moved to other regions: one patient in the intensive-therapy
AUTHOR: Pedersen (Gaede) RETAKE 1st
group withdrew after 3.2 years, andICM
two patients in the conventional-therapy group2nd
withdrew after 0.4 and 4.7 years.
FIGURE: 1 of 4
No other patients were lost to follow-up.
REG F
3rd
CASE Revised
EMail Line 4-C SIZE
ARTIST: ts H/T H/T
Enon
datory by law for a physician to complete a death 33p9
vascular disease events
Combo that included death from
certificate for any death occurring in Denmark; cardiovascular
AUTHOR, PLEASE NOTE: causes,
Figure has been redrawn and type has been reset.
nonfatal stroke, nonfatal
the data are coded and retained in the computer- myocardial
Please check carefully. infarction, coronary-artery bypass
ized Danish Death Registry.16 grafting, percutaneous coronary intervention or
JOB: 35806 ISSUE: 02-07-08
The secondary end points were death from revascularization for peripheral atherosclerotic ar-
cardiovascular causes and a composite of cardio- terial disease, and amputation because of ische
582 n engl j med 358;6 www.nejm.org february 7, 2008
The New England Journal of Medicine
Downloaded from nejm.org on November 28, 2015. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
Effect of Multither apy on Mortality in Type 2 Diabetes
mia.17 An independent committee whose mem- from the Danish Death Registry to the Steno Dia-
bers were unaware of study-group assignments betes Center confirmed that this milestone was
from the intervention portion of the Steno-2 Study reached in June 2006.
adjudicated the specified end points. All end points were analyzed according to the
The tertiary end points were incident diabetic intention-to-treat principle. For the primary and
nephropathy or the development or progression of secondary end points, event curves for the time to
diabetic retinopathy or neuropathy.12 Diabetic ne- the first event were based on KaplanMeier analy-
phropathy was defined as a urinary albumin ex- sis, and treatments were compared by means of
cretion rate of more than 300 mg per 24 hours in the log-rank test. The hazard ratio for the com-
two of three consecutive sterile urine specimens parison of intensive with conventional therapy and
measured at baseline; after 1.9, 3.8, and 7.8 years; 95% confidence intervals were estimated with the
and at the end of the follow-up period. use of a proportional-hazards model. We deter-
Diabetic retinopathy was graded according to mined whether the hazard ratio at the end of the
the six-level grading scale of the European Com- formal intervention subsequently changed. If so,
munity-funded Concerted Action Programme into the time since randomization was used as the
the Epidemiology and Prevention of Diabetes time scale in an adjusted model.19 Data regarding
(EURODIAB) by two independent eye specialists tertiary end points were censored according to
who were unaware of the patients study-group prespecified intervals and analyzed with the use
assignments (see the table in the Supplementary of a proportional-hazards model, with adjustment
Appendix, available with the full text of this ar- for age, duration of diabetes, sex, and microvas-
ticle at www.nejm.org).18 Progression of retinopa- cular status at baseline; these results are expressed
thy was defined as an increase of at least one level as relative risks. Changes in measured variables
in the EURODIAB grading scale in either eye, as within groups were compared by means of analy-
reported previously.12 The need for laser treatment sis of covariance, with baseline values as covari-
of either proliferative retinopathy or macular ede- ates. The MannWhitney test was used for any
ma was evaluated by ophthalmologists at the eye instances of non-Gaussian distribution. A chi-
clinic of the Steno Diabetes Center, who were un- square test was performed to compare categori-
aware of study-group assignments. Blindness was cal variables. All reported P values are two-sided.
defined according to the criteria of the World
Health Organization as a maximally corrected vi- R e sult s
sual acuity of less than 6/60 in either eye (less than
20/200 on the Snellen visual-acuity scale). Patients
Peripheral neuropathy was measured with a Behavioral, clinical, and biochemical characteris-
biothesiometer. The diagnosis of autonomic neu- tics of the patients at baseline, at the end of the
ropathy was based on a measurement of the RR trial (at 7.8 years), and at the end of the follow-up
interval on an electrocardiogram obtained during period (at 13.3 years) are shown in Table 1. The two
paced breathing and on an orthostatic-hypoten- study groups were similar at baseline but differed
sion test, with progression defined as reported significantly at the end of the intervention period,
previously.12 indicating that intensive therapy was superior to
conventional therapy in controlling the level of
Statistical Analysis glycated hemoglobin; fasting serum levels of to-
The protocol for the follow-up trial specified that tal cholesterol, low-density lipoprotein cholesterol,
no analyses of death from any cause would be per- and triglycerides; systolic and diastolic blood pres-
formed until at least 60 patients had died, as veri- sures; and rate of urinary albumin excretion (Ta-
fied by online death registration, and until at least ble 1). At the end of the follow-up period, the dif-
half the patients in either the intensive-therapy ferences in risk factors between the groups had
group or the conventional-therapy group had died. narrowed, primarily because of intensified treat-
It was estimated that this plan for analyzing death ment among patients in the original convention-
from any cause would provide a statistical power al-therapy group (Fig. 1A). In contrast, risk factors
of 0.75 and a type I error rate of 0.05 in detecting in the intensive-therapy group remained the same
a reduction in the relative risk of death of 40% in as they had been during the original trial, ex-
the intensive-therapy group. Continuous reporting cept for systolic blood pressure, which increased
n engl j med 358;6 www.nejm.org february 7, 2008 583
The New England Journal of Medicine
Downloaded from nejm.org on November 28, 2015. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
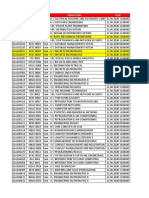
Table 1. Clinical, Demographic, Biochemical, and Other Characteristics of the Patients.*
At End of Intervention
Characteristic or Variable At Baseline Study At End of Follow-up
Intensive Conventional Intensive Conventional Intensive Conventional
Therapy Therapy Therapy Therapy Therapy Therapy
(N=80) (N=80) (N=67) (N=63) (N=55) (N=38)
Clinical and demographic
Age (yr) 54.97.2 55.27.2 62.17.2 63.16.8 66.07.0 66.16.8
Duration of follow-up (yr) NA NA 7.80.4 7.80.3 13.30.4 13.30.4
Body-mass index
Men 29.33.6 30.35.3 30.04.3 30.85.6 31.14.6 30.25.7
Women 31.14.5 28.93.8 33.86.8 30.04.4 34.77.0 33.44.3
Waist circumference (cm)
Men 10510 10714 10810 11214 11211 11017
Women 10014 10113 10814 10711 11213.7 11510.5
Blood pressure (mm Hg)
Systolic 14611 14919 13113 14618 14014 14618
Diastolic 8510 8611 7311 7810 748 737
Current smoker (%) 40 35 31 27 22 18
Daily dietary intake
Median (kcal) 2257 2137 2213 2111 2148 1944
Range (kcal) 13903764 13506062 13143563 13463277 12853686 14262587
Composition of intake (%)
Protein 15.42.5 15.62.0 17.02.5 16.92.3 17.21.8 18.11.7
Carbohydrates 37.26.3 38.66.1 46.46.5 43.76.7 45.85.2 43.95.0
Alcohol 6.39.2 4.06.6 5.97.5 4.47.0 3.85.7 3.65.7
Fat 41.16.4 41.86.5 30.65.1 35.07.0 32.64.7 34.35.3
Saturated fatty acids 17.53.4 17.44.0 10.63.1 12.73.7 12.13.4 12.83.3
Exercise duration (min/wk)
Median 120 105 144 90 120 60
Range 0725 0900 0930 0630 01050 0645
Biochemical
Fasting plasma glucose (mg/dl) 18256 18954 12945 17871 16055 17061
Glycated hemoglobin (%) 8.41.6 8.81.7 7.91.2 9.01.8 7.71.2 8.01.4
Fasting serum C peptide (pmol/
liter)
Median 846 863 676 751 704 630
Range 2941655 3001686 1172524 593650 803030 1833495
Stimulated serum C peptide
(pmol/liter)
Median 1438 1514 1140 1090 1310 912
Range 6803315 6443170 1413930 845418 2173560 2914270
Fasting serum cholesterol (mg/dl)
Total 21041 23350 15934 21650 14734 15532
Low-density lipoprotein 13336 13737 8330 12636 7129 7728
High-density lipoprotein 409 3911 4716 4512 5115 4715
584 n engl j med 358;6 www.nejm.org february 7, 2008
The New England Journal of Medicine
Downloaded from nejm.org on November 28, 2015. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
Effect of Multither apy on Mortality in Type 2 Diabetes
Table 1. (Continued.)
At End of Intervention
Characteristic or Variable At Baseline Study At End of Follow-up
Intensive Conventional Intensive Conventional Intensive Conventional
Therapy Therapy Therapy Therapy Therapy Therapy
(N=80) (N=80) (N=67) (N=63) (N=55) (N=38)
Fasting serum triglycerides (mg/dl)
Median 159 205 115 159 99 148
Range 48624 561393 35514 691931 291148 35318
Urinary albumin excretion
(mg/24 hr)
Median 78 69 46 126 69 75
Range 32265 32286 45593 34778 52838 75363
Urinary sodium excretion
(mmol per 24 hr)
Median 185 211 170 198 169 201
Range 25513 46577 32525 53436 23524 68344
Serum creatinine (mol/liter) 7817 7616 10232 11185 10053 10545
Drug therapy
No glucose-lowering drugs (%) 35 26 1 6 4 5
Metformin (%) 13 19 50 34 66 37
Sulfonylurea (%) 53 56 50 47 40 16
Glitazone (%) 0 0 0 0 0 3
Any oral hypoglycemic agent (%) 59 61 74 61 84 47
Insulin (%) 6 14 57 54 73 82
Insulin plus an oral hypoglycemic 0 1 32 21 83 42
agent (%)
Insulin dose (IU per day)
Median 42 30 62 64 60 68
Range 1052 14142 12260 12360 16220 30154
ACE inhibitor or ARB (%) 20 19 97 70 91 87
Both ACE inhibitor and ARB (%) 0 0 28 0 18 5
Diuretic (%) 21 28 58 60 82 84
Calcium antagonist (%) 14 6 36 29 42 42
Beta-blocker (%) 10 1 19 16 15 32
Other antihypertensive drug (%) 1 1 4 6 5 8
Any antihypertensive drug (%) 41 41 99 83 93 100
Statin (%) 0 3 85 22 84 82
Fibrate (%) 1 1 1 5 2 0
Aspirin (%) 14 13 87 56 85 76
* Plusminus values are means SD. The body-mass index is the weight in kilograms divided by the square of the height
in meters. Stimulated serum C peptide was measured 6 minutes after intravenous injection of 1 mg of glucagon in the
fasting state. To convert the values for glucose to millimoles per liter, multiply by 0.05551. To convert the values for
cholesterol to millimoles per liter, multiply by 0.02586. To convert the values for triglycerides to millimoles per liter,
multiply by 0.01129. To convert the values for creatinine to milligrams per deciliter, divide by 88.4. ACE denotes angio-
tensin-converting enzyme, ARB angiotensin-receptor blocker, and NA not applicable.
P<0.01 by analysis of covariance or the MannWhitney test (when appropriate) for the comparison of changes between
study groups.
P<0.05 by analysis of covariance or the MannWhitney test (when appropriate) for the comparison of changes between
study groups.
n engl j med 358;6 www.nejm.org february 7, 2008 585
The New England Journal of Medicine
Downloaded from nejm.org on November 28, 2015. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
(P=0.001) (Fig. 2A). Time curves for risk factors
Figure 2 (facing page). Changes in Selected Risk
showed a similar pattern for the 93 patients who Factors during the Interventional Study and Follow-up
were followed during the entire 13.3-year period Period.
(data not shown). No significant differences were Panel A shows mean (SE) values for selected risk fac-
observed between the two groups with respect to tors during the interventional part of the study for all
habits related to exercise and smoking, and only patients (solid lines) and during the follow-up period
(dashed lines). In the conventional-therapy group, mean
minor (although significant) changes were seen
values were obtained at baseline, at 3.8 years, at
in the intake of carbohydrates and fat. There were 7.8 years, and at 13.3 years. At these intervals, the total
also no significant differences in body weight or numbers of patients in both study groups were 160, 149,
waist circumference (Table 1). 130, and 93, respectively. Panel B shows the percentage
During the entire 13.3 years of follow-up, 24 of patients in each group in whom the treatment goals
for the intensive-therapy group were reached at the end
patients (30%) in the intensive-therapy group died,
of the study. Only one patient (in the intensive-therapy
as compared with 40 patients (50%) in the con- group) reached all five treatment goals at the end of fol-
ventional-therapy group, which corresponded to low-up. To convert the values for cholesterol to milli-
an absolute risk reduction of 20% (P=0.02 by the moles per liter, multiply by 0.02586. To convert the val-
log-rank test) (Fig. 3A). The hazard ratio for death ues for triglycerides to millimoles per liter, multiply by
0.01129. LDL denotes low-density lipoprotein.
in the intensive-therapy group, as compared with
the conventional-therapy group, was 0.54 (95%
confidence interval [CI], 0.32 to 0.89; P=0.02). in the conventional-therapy group (Table 2 and
There was no evidence of a change in the hazard Fig. 3C). The mean number of major cardiovas-
ratio after the formal intervention was stopped cular events was 0.6 in the intensive-therapy group
(P=0.27). Deaths from cancer were as expected on and 2.0 in the conventional-therapy group. The
the basis of data from the Danish Cancer Regis- average number of recurrent events among pa-
try and did not differ significantly between the tients with cardiovascular events was 2.0 in the
two study groups (two deaths in the intensive- intensive-therapy group and 3.3 in the conven-
therapy group and five in the conventional-therapy tional-therapy group.
group). During the entire observation period, diabetic
Nine patients in the intensive-therapy group nephropathy developed in 20 patients in the inten-
died from cardiovascular causes, as compared with sive-therapy group, as compared with 37 patients
19 in the conventional-therapy group (P=0.03 by in the conventional-therapy group (relative risk,
the log-rank test) (Table 2). The hazard ratio for 0.44; 95% CI, 0.25 to 0.77; P=0.004) (Fig. 4). One
death from cardiovascular causes in the intensive- patient in the intensive-therapy group had progres-
therapy group was 0.43 (95% CI, 0.19 to 0.94; sion to end-stage renal disease requiring dialysis,
P=0.04). The hazard ratio for death from cardio- as compared with six patients in the conventional-
vascular disease tended to decrease in the inten- therapy group (P=0.04).
sive-therapy group after the end of the original Progression of diabetic retinopathy occurred
trial, but the difference between the groups did in 41 patients in the intensive-therapy group and
not reach significance (P=0.06). However, because in 54 patients in the conventional-therapy group
of the borderline significance, we also analyzed (relative risk, 0.57; 95% CI, 0.37 to 0.88; P=0.01).
the data according to an adjusted model that in- Laser treatment for proliferative retinopathy or
cluded time since randomization as the time scale. macular edema was administered to 14 patients
The derived results (hazard ratio, 0.43; 95% CI, in the intensive-therapy group and 27 patients in
0.19 to 0.95; P=0.04) were similar to those de- the conventional-therapy group (relative risk,
rived from the unadjusted model. 0.45; 95% CI, 0.23 to 0.86; P=0.02); blindness in
A total of 209 cardiovascular events occurred at least one eye was diagnosed in 2 patients in the
during the 13.3 years of observation (Table 2 and intensive-therapy group and in 7 patients in the
Fig. 3B). In the intensive-therapy group, the abso- conventional-therapy group (relative risk, 0.51;
lute risk reduction was 29%, with a hazard ratio 95% CI, 0.17 to 1.53; P=0.23).
of 0.41 (95% CI, 0.25 to 0.67; P<0.001). There was Autonomic neuropathy progressed in 39 pa-
no evidence of a change in the hazard ratio after tients in the intensive-therapy group and in 52
the formal intervention study ended (P=0.20). patients in the conventional-therapy group (rel-
There were 51 events in 25 patients in the inten- ative risk, 0.53; 95% CI, 0.34 to 0.81; P=0.004),
sive-therapy group and 158 events in 48 patients and peripheral neuropathy progressed in 44 and
586 n engl j med 358;6 www.nejm.org february 7, 2008
The New England Journal of Medicine
Downloaded from nejm.org on November 28, 2015. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
Effect of Multither apy on Mortality in Type 2 Diabetes
A
Glycated Hemoglobin (%) 11 350
10
Total Cholesterol (mg/dl)
Conventional therapy 300
9 Conventional therapy
250
8
200
7 Intensive therapy
150 Intensive therapy
6
5 100
4 50
0 0
0 1 2 3 4 5 6 7 8 9 10 11 12 13 0 1 2 3 4 5 6 7 8 9 10 11 12 13
Systolic Blood Pressure (mm Hg)
170 175
160 Conventional therapy
LDL Cholesterol (mg/dl)
150
Conventional therapy
150
125
140
100 Intensive therapy
130
Intensive therapy
75
120
110 50
100 25
0 0
0 1 2 3 4 5 6 7 8 9 10 11 12 13 0 1 2 3 4 5 6 7 8 9 10 11 12 13
Diastolic Blood Pressure (mm Hg)
95 350
90 300 Conventional therapy
Triglycerides (mg/dl)
85 Conventional therapy
250
80
200
75
Intensive therapy 150
70
65 100 Intensive therapy
60 50
0 0
0 1 2 3 4 5 6 7 8 9 10 11 12 13 0 1 2 3 4 5 6 7 8 9 10 11 12 13
Years of Follow-up Years of Follow-up
B
Intensive therapy Conventional therapy
100
90 P=0.14
P=0.35 P=0.005
80
70
Patients (%)
60
50
40
30 P=0.27
20 P=0.31
10
0
Glycated Cholesterol Triglycerides Systolic Blood Diastolic Blood
Hemoglobin <175 mg/dl <150 mg/dl Pressure Pressure
<6.5% <130 mm Hg <80 mm Hg
46 patients in the two groups, ICM
respectively
AUTHOR: was reported
Pedersen (Gaede) in 80%
RETAKE 1st of patients in the intensive-
(relative risk, 0.97; 95% CI, 0.62 to
REG F 1.51; P=0.89).
FIGURE: 2 of 4 therapy group and in
2nd70% of patients in the con-
3rd
During the 13.3 years of observation,
CASE at least ventional-therapy Revised group (P=0.15). There was no
one minor episode of symptomatic EMail hypoglycemia Line 4-C
statistical difference
SIZE in major hypoglycemia epi-
ARTIST: ts H/T H/T
Enon
Combo 33p9
n engl j med 358;6 www.nejm.org
AUTHOR, february 7, 2008
PLEASE NOTE:
587
Figure has been redrawn and type has been reset.
The New
PleaseEngland Journal of Medicine
check carefully.
Downloaded from nejm.org on November 28, 2015. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical ISSUE:
JOB: 35806 Society.02-07-08
All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
A Figure 3. KaplanMeier Estimates of the Risk of Death
Cumulative Incidence of Death (%)
80 from Any Cause and from Cardiovascular Causes and
the Number of Cardiovascular Events, According to
70
Treatment Group.
60 Panel A shows the cumulative incidence of the risk of
50 death from any cause (the studys primary end point)
Conventional therapy during the 13.3-year study period. Panel B shows the
40
P=0.02 cumulative incidence of a secondary composite end
30 point of cardiovascular events, including death from
20 cardiovascular causes, nonfatal stroke, nonfatal myo-
Intensive therapy
10
cardial infarction, coronary-artery bypass grafting
(CABG), percutaneous coronary intervention (PCI), re-
0 vascularization for peripheral atherosclerotic artery dis-
0 1 2 3 4 5 6 7 8 9 10 11 12 13
ease, and amputation; Panel C shows the number of
Years of Follow-up events for each component of the composite end
No. at Risk point. In Panels A and B, the I bars represent standard
Intensive therapy 80 78 75 72 65 62 57 39 errors.
Conventional 80 80 77 69 63 51 43 30
therapy
intensive-therapy group and one in the conven-
B tional-therapy group reported having muscle pain
80 after statin treatment; however, no elevation of the
serum creatine kinase level was seen. Five patients
Cumulative Incidence of Any
70
Cardiovascular Event (%)
Conventional therapy
60 in the intensive-therapy group and four patients
50 in the conventional-therapy group reported having
40
a cough during treatment with angiotensin-con-
P<0.001 vertingenzyme inhibitors. The cough disappeared
30
Intensive therapy in all patients after a change to an angiotensin II
20
antagonist. The average number of physician-
10
prescribed drugs for type 2 diabetes or its com-
0 plications in the intensive-therapy group at the
0 1 2 3 4 5 6 7 8 9 10 11 12 13
end of the follow-up period was 5.5, as com-
Years of Follow-up
pared with 5.7 in the conventional-therapy group
No. at Risk
Intensive therapy 80 72 65 61 56 50 47 31
(P=0.64).
Conventional 80 70 60 46 38 29 25 14
therapy
Dis cus sion
C
40 Intensive therapy Conventional therapy After a mean of 13.3 years (7.8 years of multifac-
35
torial intervention and an additional 5.5 years of
No. of Cardiovascular Events
follow-up), there was an absolute risk reduction
30
for death from any cause of 20% among patients
25 with type 2 diabetes and microalbuminuria who
20 received intensive therapy, as compared with those
15 who received conventional therapy. The absolute
10 risk of death from cardiovascular causes was re-
duced by 13% among those receiving intensive
5
therapy. During the entire follow-up period, the
0
Death Stroke Myocardial CABG PCI Revascu- Amputa- rate of death among patients in the conventional-
from Infarction larization tion therapy group was 50%, a finding that underscores
Cardio-
vascular
the poor prognosis for such patients in the absence
Causes of intensive treatment.20
In comparison with the results of trials involv-
sodes (13%
AUTHOR: in the
Pedersen intensive-therapy
(Gaede) RETAKE 1stgroup and ing treatment of single risk factors in patients with
ICM
REG F
17% in
FIGURE:the
3 ofconventional-therapy
4 group,
2nd P=0.52). type 2 diabetes, the achieved risk reductions in
3rd
CASE A bleeding gastric ulcer developed
Revised in one patient our trial were considerable. However, in secondary
EMail in the intensive-therapy
Line group.
4-C TwoSIZEpatients in the interventions, individual therapy with aspirin, anti-
ARTIST: ts H/T H/T
Enon 22p3
Combo
588 n engl j med 358;6 www.nejm.org february 7, 2008
AUTHOR, PLEASE NOTE:
Figure has been redrawn and type has beenThe
reset.
New England Journal of Medicine
Please check carefully.
Downloaded from nejm.org on November 28, 2015. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
JOB: 35806 ISSUE: 02-07-08
Effect of Multither apy on Mortality in Type 2 Diabetes
Table 2. Numbers of Deaths from Any Cause, Deaths from Cardiovascular Causes, and Cardiovascular Events
at 13.3 Years.*
Variable Intensive Therapy Conventional Therapy
No. of No. of
No. of No. of First No. of No. of First
Patients Events Events Patients Events Events
Death from any cause 24 24 40 40
Death from cardiovascular causes 9 9 3 19 19 3
Myocardial infarction 8 9 7 21 35 11
Stroke 6 6 4 18 30 15
Coronary-artery bypass grafting 8 8 5 13 13 7
Percutaneous coronary intervention 1 1 0 3 11 3
Revascularization 6 8 4 10 17 4
Amputation 6 10 2 14 33 5
All cardiovascular events 25 51 48 158
* Patients could have more than one event. First events refer to the type of event for which data for a patient were cen-
sored from the proportional-hazards model after an event. Thus, the total number of first events is equal to the number
of patients having a cardiovascular event during follow-up.
hypertensive agents, and lipid-lowering drugs each apy were compared during a 6.5-year period. After
reduced the relative risk of cardiovascular events an average follow-up of 17 years, the original in-
by about 25%, and the effects appeared to be ad- tensive-therapy treatment was associated with an
ditive.21,22 Therefore, the reductions in risk absolute risk reduction of 2.8% for a composite
a 59% reduction in the relative risk and a 29% re- cardiovascular end point. In the DCCT follow-up
duction in the absolute risk in the composite of trial, glucose regulation deteriorated in the origi-
cardiovascular events fit with projections from tri- nal intensive-therapy group and improved in the
als involving single risk factors.21 control group, resulting in a convergence of the
Our study was not designed to identify which glycemic levels in the two groups.
elements of intensive diabetes therapy contributed In our follow-up trial, the risk factors in the two
most to the reduction in cardiovascular risk. How- study groups tended to converge (Fig. 2). Only the
ever, using a risk calculator based on epidemio- control of systolic blood pressure deteriorated in
logic and interventional data from patients with the intensive-therapy group, whereas glucose lev-
type 2 diabetes in the United Kingdom Prospec- els, lipid levels, diastolic blood pressure, and the
tive Diabetes Study,23 we concluded that the use rate of urinary albumin excretion improved in the
of statins and antihypertensive drugs might have conventional-therapy group, leaving the two study
had the largest effect in reducing cardiovascular groups with similar levels of risk factors after
risk during the 7.8 years of intervention, with hy- 13.3 years. The design of our study did not allow
poglycemic agents and aspirin the next most im- us to estimate the exact time at which risk factors
portant interventions.24 improved in the conventional-therapy group. How-
Even though the significant differences in the ever, since all patients were offered intensive treat-
levels of risk factors for cardiovascular disease be- ment at the end of the trial, the improvement
tween the study groups at the end of our interven- probably took place early during the follow-up pe-
tional study had disappeared by the end of the riod. The effect of blood-pressure reduction on
follow-up period (Table 1 and Fig. 2), the Kaplan cardiovascular end points usually occurs within
Meier curves for the time to the first cardiovascular months,26,27 whereas the effect of lipid lowering
event continued to diverge (Fig. 3B). A similar out- is evident after 1 to 2 years.8,28,29 The effect of
come was reported in the Diabetes Control and glucose lowering on diabetes-related end points
Complications Trial (DCCT),25 involving patients occurs even later.4 Thus, an effect of early inter-
with type 1 diabetes, in which the effects of inten- vention, as compared with late intervention, may
sive insulin therapy and conventional insulin ther- be a likely explanation for the continuing diver-
n engl j med 358;6 www.nejm.org february 7, 2008 589
The New England Journal of Medicine
Downloaded from nejm.org on November 28, 2015. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Intensive therapy Conventional therapy
A Nephropathy B Retinopathy
60 60
50 50
40 40
No. of Patients
No. of Patients
30 30
20 20
10 10
0 0
At 4 Yr At 8 Yr Post-Trial At 13 Yr At 4 Yr At 8 Yr Post-Trial At 13 Yr
C Autonomic Neuropathy D Peripheral Neuropathy
60 60
50 50
40 40
No. of Patients
No. of Patients
30 30
20 20
10 10
0 0
At 4 Yr At 8 Yr Post-Trial At 13 Yr At 4 Yr At 8 Yr Post-Trial At 13 Yr
Figure 4. Patients with Development or Progression of Diabetic Nephropathy, Retinopathy, Autonomic Neuropathy, and Peripheral
Neuropathy.
The bars labeled Post-Trial refer to the number of patients in whom the condition progressed during the period from the end of the
original intervention trial to the end-point examination after an average of 13.3 years of study and follow-up.
ICM
AUTHOR: Pedersen (Gaede) RETAKE 1st
gence in cardiovascular REGend points,4 ofrather
F FIGURE: 4 than a reported during 2nd
regular interviews with pa-
3rd
simple time-to-effect CASE
relationship. tients. 10,12
Revised In this respect, it is noteworthy that
Line 4-C
The drugs used in EMail
our study differed
ARTIST: ts between except SIZE
for atorvastatin, generic drugs with well-
H/T H/T
the study groups. For instance, a larger propor-
Enon
Combo known36p6 long-term side effects were prescribed.
tion of patients in the intensive-therapy
AUTHOR, group
PLEASEtook
NOTE:Whether newer and more expensive diabetes treat-
Figure has been redrawn and type has been reset.
metformin or sulfonylurea, despite the similar ments would have additional beneficial long-term
Please check carefully.
levels of glycemia in the two groups. Therefore, effects or risks remains to be determined.
differences in drugsJOB:
or their
35806 combinations might Recent
ISSUE: surveys have shown very slow prog-
02-07-08
have contributed to the long-term outcome. ress in achieving treatment goals and in the use
Reductions in the progression of microvascular of recommended drugs for the prevention of dia-
complications occurred after a mean of 3.8 years betic vascular complications.31,32 Therefore, since
of intensified intervention,12 changes that were intensive, multifactorial care of patients with
maintained at 13.3 years. Indeed, during continu- type 2 diabetes leads to reduced rates of death
ous follow-up, this reduction translated into a and cardiovascular disorders, the early and metic-
significant absolute risk reduction of 6.3% in the ulous implementation of current treatment guide-
need for dialysis, a condition that in many parts lines remains a major challenge.
of the world is tantamount to death.30 Supported by the Danish Health Research Council.
Dr. Parving reports receiving consulting and lecture fees
We did not monitor adverse effects continu- from Merck, Novartis, Bristol-Myers Squibb, Pfizer, and Sanofi
ously. However, few serious adverse effects were and grants from Merck, Novartis, and Bristol-Myers Squibb
590 n engl j med 358;6 www.nejm.org february 7, 2008
The New England Journal of Medicine
Downloaded from nejm.org on November 28, 2015. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
Effect of Multither apy on Mortality in Type 2 Diabetes
and having an equity interest in Novo Nordisk and Merck; and stein, A. Hoppe, S. Kohlwes, G. Lademann, J. Lohse, C. Lysn,
Dr. Pedersen, having an equity interest in Novo Nordisk. No G. Mortensen, S. Mnsson, B.B. Nielsen, J. Obel, J. Poulsen, and
other potential conflict of interest relevant to this article was K. Riemer; B. Carstensen and A. Vlund for their statistical sup-
reported. port; M. Frandsen, B.V. Hansen, B.R. Jensen, T.R. Juhl, L. Pie-
We thank the patients who participated in the study and their trascek, and U. Schmidt for their bioanalytical assistance; and J.
families; Pernille Vedel, a coinvestigator in the early phase of the Faber and P. Hildebrandt for their thorough examinations while
study; study assistants L. Askjr, M. Beck, J. Bengtsen, I. Hol- serving on the end-point committee.
References
1. Fabre J, Balant LP, Dayer PG, Fox HM, 11. American Diabetes Association. Stan- 23. Stevens RJ, Kothari V, Adler AI, Strat-
Vernet AT. The kidney in maturity onset dards of medical care in diabetes 2007. ton IM. The UKPDS risk engine: a model
diabetes mellitus: a clinical study of 510 Diabetes Care 2007;30:Suppl 1:S4-S41. for the risk of coronary heart disease in
patients. Kidney Int 1982;21:730-8. 12. Gde P, Vedel P, Parving HH, Peder type II diabetes (UKPDS 56). Clin Sci (Lond)
2. Wingard DL, Barrett-Connor EL. sen O. Intensified multifactorial interven- 2001;101:671-9. [Erratum, Clin Sci (Lond)
Heart disease and diabetes. In: Harris MI, tion in patients with type 2 diabetes mel- 2002;102:679.]
Cowie CC, Stern MP, Boyko EJ, Rieber GE, litus and microalbuminuria: the Steno 24. Gde P, Pedersen O. Intensive inte-
Bennett PH, eds. Diabetes in America. type 2 randomised study. Lancet 1999; grated therapy of type 2 diabetes: implica-
2nd ed. Bethesda, MD: National Institute 353:617-22. tions for long-term prognosis. Diabetes
of Diabetes and Digestive and Kidney Dis- 13. Beck-Nielsen H, Damsgaard EM, 2004;53:Suppl 3:S39-S47.
eases, 1995:429-48. (NIH publication no. Faber O, et al. Ikke-insulinkrvende dia- 25. The Diabetes Control and Complica-
95-1468.) betes mellitus. Copenhagen: Dansk Sel- tions Trial/Epidemiology of Diabetes Inter-
3. Gu K, Cowie CC, Harris MI. Diabetes skab for Intern Medicin, 1988. ventions and Complications (DCCT/EDIC)
and decline in heart disease mortality in 14. Beck-Nielsen H, Henriksen JE, Her- Study Research Group. Intensive diabetes
US adults. JAMA 1999;281:1291-7. mansen K, et al. Type 2-diabetes og det treatment and cardiovascular disease in
4. UK Prospective Diabetes Study metaboliske syndrom: Diagnostik og be- patients with type 1 diabetes. N Engl J
(UKPDS) Group. Intensive blood-glucose handling: Klaringsrapport. Ugeskr Laeger Med 2005;353:2643-53.
control with sulphonylureas or insulin com- 2000;162:Suppl:S1-S36. 26. Collins R, Peto R, MacMahon S, et al.
pared with conventional treatment and risk 15. Type 2 diabetes. Medicinsk teknologi- Blood pressure, stroke, and coronary
of complications in patients with type 2 dia- vurdering af screening, diagnostik og heart disease. 2. Short-term reductions in
betes (UKPDS 33). Lancet 1998;352:837-53. behandling. In: Medicinsk Teknologivur- blood pressure: overview of randomised
[Erratum, Lancet 1999;354:602.] dering. Vol. 5. No. 1. Copenhagen: Sund- drug trials in their epidemiological con-
5. Idem. Effect of intensive blood-glucose hedsstyrelsen, Center for Evaluering og text. Lancet 1990;335:827-38.
control with metformin on complications Medicinsk Teknologivurdering, 2003. (Ac- 27. Weber MA, Julius S, Kjeldsen SE, et al.
in overweight patients with type 2 diabe- cessed January 14, 2008, at http://www. Blood pressure dependent and indepen-
tes (UKPDS 34). Lancet 1998;352:854-65. sst.dk/publ/publ2003/type_2_diabetes.pdf.) dent effects of antihypertensive treatment
[Erratum, Lancet 1998;352:1558.] 16. Juel K, Helweg-Larsen K. The Danish on clinical events in the VALUE trial. Lan-
6. Idem. Tight blood pressure control registers of causes of death. Dan Med Bull cet 2004;363:2049-51.
and risk of macrovascular and microvas- 1999;46:354-7. 28. LIPID Study Group (Long-term Inter-
cular complications in type 2 diabetes: 17. Gde PH. Intensified multifactorial vention with Pravastatin in Ischaemic Dis-
UKPDS 38. BMJ 1998;317:703-13. [Erratum, intervention in patients with type 2 diabe- ease). Long-term effectiveness and safety
BMJ 1999;318:29.] tes and microalbuminuria: rationale and of pravastatin in 9014 patients with coro-
7. Colhoun HM, Betteridge DJ, Dur- effect on late-diabetic complications. Dan nary heart disease and average cholesterol
rington PN, et al. Primary prevention of Med Bull 2006;53:258-84. concentrations: the LIPID trial follow-up.
cardiovascular disease with atorvastatin in 18. Aldington SJ, Kohner EM, Meuer S, Lancet 2002;359:1379-87. [Erratum, Lancet
type 2 diabetes in the Collaborative Atorv- Klein R, Sjlie AK. Methodology for reti- 2002;360:1430.]
astatin Diabetes Study (CARDS): multicen- nal photography and assessment of dia- 29. Ford I, Murray H, Packard CJ, Shep-
tre randomised placebo-controlled trial. betic retinopathy: the EURODIAB IDDM herd J, MacFarlane PW, Cobbe SM. Long-
Lancet 2004;364:685-96. Complications Study. Diabetologia 1995; term follow-up of the West of Scotland
8. Collins R, Armitage J, Parish S, Sleigh 38:437-44. Coronary Prevention Study. N Engl J Med
P, Peto R, Heart Protection Study Collab- 19. Carstensen B. Regression models for 2007;357:1477-86.
orative Group. MRC/BHF Heart Protection interval censored survival data: applica- 30. Thomas MC, Cooper ME, Shahinfar S,
Study of cholesterol-lowering with simv- tion to HIV infection in Danish homo- Brenner BM. Dialysis delayed is death pre-
astatin in 5963 people with diabetes: a ran- sexual men. Stat Med 1996;15:2177-89. vented: a clinical perspective on the
domised placebo-controlled trial. Lancet 20. Gall MA, Borch-Johnsen K, Hougaard RENAAL study. Kidney Int 2003;63:1577-9.
2003;361:2005-16. P, Nielsen FS, Parving HH. Albuminuria 31. Saydah SH, Fradkin J, Cowie CC. Poor
9. Keech A, Simes RJ, Barter P, et al. Ef- and poor glycemic control predict mortal- control of risk factors for vascular disease
fects of long-term fenofibrate therapy on ity in NIDDM. Diabetes 1995;44:1303-9. among adults with previously diagnosed
cardiovascular events in 9795 people with 21. Yusuf S. Two decades of progress in diabetes. JAMA 2004;291:335-42.
type 2 diabetes mellitus (the FIELD study): preventing vascular disease. Lancet 2002; 32. Brown LC, Johnson JA, Majumdar SR,
randomised controlled trial. Lancet 2005; 360:2-3. Tsuyuki RT, McAlister FA. Evidence of sub-
366:1849-61. [Erratum, Lancet 2006;368: 22. Stratton IM, Cull CA, Adler AI, Mat- optimal management of cardiovascular
1420.] thews DR, Neil HAW, Holman RR. Addi- risk in patients with type 2 diabetes mel-
10. Gde P, Vedel P, Larsen N, Jensen tive effects of glycaemia and blood pres- litus and symptomatic atherosclerosis.
GVH, Parving H-H, Pedersen O. Multifac- sure exposure on risk of complications in CMAJ 2004;171:1189-92.
torial intervention and cardiovascular dis- type 2 diabetes: a prospective observation- Copyright 2008 Massachusetts Medical Society.
ease in patients with type 2 diabetes. al study (UKPDS 75). Diabetologia 2006;
N Engl J Med 2003;348:383-93. 49:1761-9.
n engl j med 358;6 www.nejm.org february 7, 2008 591
The New England Journal of Medicine
Downloaded from nejm.org on November 28, 2015. For personal use only. No other uses without permission.
Copyright 2008 Massachusetts Medical Society. All rights reserved.
Vous aimerez peut-être aussi
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Mensuration Practice SheetDocument1 pageMensuration Practice SheetSonia SabuPas encore d'évaluation
- Pump Shotgun: Instruction ManualDocument5 pagesPump Shotgun: Instruction ManualJustinPas encore d'évaluation
- Staff Code Subject Code Subject Data FromDocument36 pagesStaff Code Subject Code Subject Data FromPooja PathakPas encore d'évaluation
- Soal Test All GrammarDocument2 pagesSoal Test All GrammarAnonymous D7lnJMJYPas encore d'évaluation
- 9 Quw 9 CjuDocument188 pages9 Quw 9 CjuJavier MorenoPas encore d'évaluation
- DLP MonsoonDocument2 pagesDLP MonsoonjennifertariaoPas encore d'évaluation
- 1C09-08 Design For Seismic and Climate ChangesDocument31 pages1C09-08 Design For Seismic and Climate ChangesSanketWadgaonkarPas encore d'évaluation
- 9 Daftar Pustaka VaricelaDocument2 pages9 Daftar Pustaka VaricelaAfrina FaziraPas encore d'évaluation
- Pigging Training Course Mod 7 Rev 1Document26 pagesPigging Training Course Mod 7 Rev 1Suparerk Sirivedin100% (1)
- Money, Interest, and Inflation: Answers To CheckpointsDocument16 pagesMoney, Interest, and Inflation: Answers To Checkpointsb96309Pas encore d'évaluation
- 34 Plaza Newsletter 101317 FINALDocument4 pages34 Plaza Newsletter 101317 FINALJosef SzendePas encore d'évaluation
- Tas 5731Document60 pagesTas 5731charly36Pas encore d'évaluation
- Bar Tending TerminologyDocument3 pagesBar Tending TerminologySiska WangPas encore d'évaluation
- RA - Ducting WorksDocument6 pagesRA - Ducting WorksResearcherPas encore d'évaluation
- Grand Vitara 2005Document35 pagesGrand Vitara 2005PattyaaPas encore d'évaluation
- ENEE 222 Signals and Systems: Spring 2021 - Problem Set 7 - Due 4/13/2021Document2 pagesENEE 222 Signals and Systems: Spring 2021 - Problem Set 7 - Due 4/13/2021Tiana JohnsonPas encore d'évaluation
- MalachiteDocument2 pagesMalachiteAkhil KumarPas encore d'évaluation
- Electro-Mechanical SectorDocument22 pagesElectro-Mechanical SectorKen LeePas encore d'évaluation
- 16950Document16 pages16950uddinnadeemPas encore d'évaluation
- MHT-CET 2021 Question Paper: 25 September 2021Document3 pagesMHT-CET 2021 Question Paper: 25 September 2021Sank DamPas encore d'évaluation
- 7 Stages of NafsDocument7 pages7 Stages of NafsLilyPas encore d'évaluation
- Oertel - Extracts From The Jāiminīya-Brāhma A and Upanishad-Brāhma A, Parallel To Passages of TheDocument20 pagesOertel - Extracts From The Jāiminīya-Brāhma A and Upanishad-Brāhma A, Parallel To Passages of Thespongebob2812Pas encore d'évaluation
- Quarter 4 - Week 1Document44 pagesQuarter 4 - Week 1Sol Taha MinoPas encore d'évaluation
- Transportation ProblemDocument4 pagesTransportation ProblemPrejit RadhakrishnaPas encore d'évaluation
- Material Safety Data Sheet: KOMATSU Supercoolant AF-NAC (50/50 Pre-Diluted)Document5 pagesMaterial Safety Data Sheet: KOMATSU Supercoolant AF-NAC (50/50 Pre-Diluted)Thais Roberta CamposPas encore d'évaluation
- ANG Coupe Coco Mangue PassionDocument1 pageANG Coupe Coco Mangue PassionRicardo Rovira ChalerPas encore d'évaluation
- Neoliberalism and Altered State Developmentalism in The Twenty First Century Extractive Regime of IndonesiaDocument26 pagesNeoliberalism and Altered State Developmentalism in The Twenty First Century Extractive Regime of IndonesiaErwin SuryanaPas encore d'évaluation
- TRL Explanations - 1Document4 pagesTRL Explanations - 1Ana DulcePas encore d'évaluation
- Backlash SDPDocument11 pagesBacklash SDPPatrick Cyr GagnéPas encore d'évaluation
- Chapter 4: Palm Oil and Oleochemical Industries.: Presented By: Lovelyna Eva Nur Aniqah Siti MaryamDocument15 pagesChapter 4: Palm Oil and Oleochemical Industries.: Presented By: Lovelyna Eva Nur Aniqah Siti MaryamdaabgchiPas encore d'évaluation