Académique Documents
Professionnel Documents
Culture Documents
Sheet - Respiratory Examination
Transféré par
bakesamiCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Sheet - Respiratory Examination
Transféré par
bakesamiDroits d'auteur :
Formats disponibles
2010
1- Obstructive air way disease.
2- pneumonia.
3- Plural effusion.
4- Interstitial lung disease.
Stand on the Right side of bed.
Introduce yourself.
Permission taken.
Good position for PT:-1) - ANT45 or flat.
2) - Post set patient on his bed.
Good exposure: - all chest is exposed.
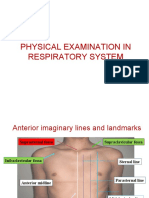
5s [Symmetry, Swelling, Scar, Superficial dilated veins, Skin discoloration].
Deformities.
Chest expansion.
R.R
Asymmetry:-bulge or retraction.
To know its bulge or retraction ask patient to breath from his mouth
The part that moves with respiration its normal & other site is the abnormal.
1)-pneumothorax 1)-collapse
2)-p.effusion 2)-fibrosis
3)-Lung mass (tumor)
Scar:-plural tap (thoracocentesis)seen in axilla .
Surgical scar may:- 1 localized Emphysema.
2 - localized Bronchiectasis.
3 hydrated cyst.
4 - Tumor rare.
Superficial veins:- occur in [svc] obstruction in lung as in (pancast tumor)
Dr. Saif Darif 1|Page
2010
Deformity: - 1- pigeon chest [pectus carinatum].
2-funnal chest [pectus excavatum].
3-barrel chest A/P diameter.
4-kyphosis, scoliosis, kyphoscoliosis.
N.B.:- any chest deformity can lead to respiratory failure type 2 .
Ask pt. to breathing normally
a) - look for accessory muscles useTracheal tugDescend of trachea with inspirationCOPD.
b)- look to nose for acting ala-nasi (flaring ).
c) - Hear for wheeze.
Comment:-bilateral equal symmetrical chest expansion all over zones no scar no dilated veins no
deformities.
Chest expiation [anterior, posterior].
Tactile vocal fremitus.
Trachea.
Apex beat.
Chest expansion: - at 3 level from front & back.
A)-From front: - 1) - supra mammary.
2) - Mammary line.
3) - Costal cartilage.
B)-From back: - 1) - shoulders.
2) - Scapula.
3) - Below scapula angle.
N.B:-Confirm by tape measure normal chest expansion (3-5cm) if <2cm means restricted .
Tactile vocal fremitus:-palpate transmitted sounds through chest wall by ask pt. to say 44.
Trachea:-set pt. firstmeasure distance between trachea & both sternocleidomastoid Ms.
normally shift slight to right side.
Apex beat:-deviated or not &palpated or not .
Note:-Trachea & apex beat useful in case of shift mediastinum.
Tracheafor upper mediastinum.
Apex beat for lower mediastinum.
Dr. Saif Darif 2|Page
2010
Anteriorly:-
1- Direct on the clavicle for apical segment lesion.
2- On the 2nd to 4th intercostal space mid-clavicular line.
3- On the 6th intercostal space anterior axillary line.
4- Lateral a) - Rt axillafor middle lobe of Rt lung.
b) - Lt Axilla for lingual in Lt Lung.
Posteriorly:-
1- Apexon supra clavicular fossa.
2- On the 3th to 9th between & infra-scapular.
1- Resonant normal.
2- Hyper-resonance emphysema, pneumothorax.
3- Dullness collapse, consolidation.
4- Stony dullness same above tibiamassive effusion.
Note:-
Only direct percussion from anterior above clavicle.
Only 2 sites percuss by 3 fingers in same time [apex from back] [axilla lateral].
When you examine anteriorly or posteriorlyin both you have to examine laterally.
Upper lobe mainly examine from front.
Middle lobe mainly examine from laterally.
Lower lobe mainly examine from back.
1- Air entry: - Good or audible, reduced, absent, no.
2- Type of breathing :-
Vesicular breathing inspiration > expirationnormally
Broncho-vesicular breathing as vesicular but expiration as in obstructive air way diseases.
Bronchial breathing inspiration = expiration with gap as in consolidation (pneumonia )
Note: - Bronchial breathing occurs only with consolidation (pneumonia).
3- Added sound:-
a. Crepitation = crackles = rales
Dr. Saif Darif 3|Page
2010
1-ILD (fibrosing alveolitis) 1-bronchiectasis.
2-pulmonary edema 2-chronic bronchitis.
3-early stage of pneumonia. 3-late pneumonia.
N.B occurs due to re-openition in distal of N.B due to air bubbling through secretion in large air
occluded alveoli or section in distal airway. way.
b.Rhonchi or wheezemainly in expiration.
Rhonchi definition: it's a musical sound due to airway obstruction and heard mainly during expiration
and its 2 types:
Monophonic: its low pitched indicates local obstruction to major airway and so unilateral.
Polyphonic: variable high pitched heard bilaterally indicated either asthma or COPD.
1- Asthma.
2- Ch. Bronchitis.
3- emphysema.
4- Bronchiectasis.
5- Pneumonia.
6- H.F with pulmonary edema
c. Vocal resonance: - As tactile vocal fremitus but hear audible vibration by ask pt. to say 44.
Whispered pecteriloquywhispered 44heard load in area with consolidation.
Ego-phony: - E heard A in area of consolidation.
Unilateral Bilateral
1)-pneumothorax Upper lobe 1-asthma.
2)-plural effusion Lower lobe 2-COPD.
3)-collapse any lobe 3-brondhiectasis.
4)-lobar pneumonia any lobe 4-broncho-pneumonia.
5-ILD.
Dr. Saif Darif 4|Page
2010
Increase Decrease
Pneumonia dull Collapse dull
Pneumothoraxhyper Resonant
Plural effusion stony dull
Away To same side
Plural effusion collapse
pneumothorax
usually unilateral lesion can be differentiated without auscultation but bilateral lesion should be
auscultating to differentiate.
1) - air entry.
2) - vesicular breathing with prolonged expiration.
3) - Rhonchi ( Crepitationin chronic bronchitis, bronchiectasis)
Rhonchi only Rhonchi +crepitation Crepitation only
asthma Chronic bronchitis ILD
COPD bronchiectasis pneumonia
bronchiectasis pneumonia
Note:-
1- The only finding in ILD is crepitation.
2- All plural disease of all chest examination.
3- Increase of TVF & VR only in pneumonia, Collapse (in present of open air way).
4- Stony dullness occurs only in massive plural effusion.
Dr. Saif Darif 5|Page
2010
[ill, underweight, distress, confusion].
1 jaundice lung CA metastasis, RVF (cardiac cirrhosis)
2 Anemia chronic illness.
3 - Plethoric face polycythemia (non-metastatic sign of lung CA).
4 - Act ala-nasi COPD & distress.
5 - Central cyanosispulmonary edema.
6 Ptosis Horner syndromeapical Tung tumor.
7 Halitosis bronchiectasis.
1- L.N metastasis, cervical, scalene.
2-JVPRVFdue to core pulmonale
3-accessory Ms. Use obstructive airway.
1- Clubbing : - most Common bronchiectasis.
2- Cyanosis.
3- Flapping tremor CO2 retention due to COPD.
Nicotine stain .
1- bilateral leg edemadue to RVF.
2-unilatDVTsever dyspnea.
What are the causes of dullness at a lung base?
1- Pleural effusion.
2- Pleural thickeningmesothelioma
3- Consolidation and collapse of the lung.
4- Raised hemi-diaphragmphrenic nerve palsy.
How would you differentiate between the above?
1- Pleural effusion: stony dull note; trachea may be deviated to the opposite side in large effusions.
2- Pleural thickening: trachea not deviated; breath sounds will be heard.
3- Consolidation: vocal resonance increased; bronchial breath sounds and associated crackles.
4- Collapse: trachea deviated to the affected side; absent breath sounds.
Dr. Saif Darif 6|Page
2010
Mention a few causes for an exudate and a transudate.
Causes for an exudate: Causes of a transudate:
1- Bronchogenic carcinoma (presence of effusion is an ominous 1- Nephrotic syndrome.
sign). 2- Cardiac failure.
2- Secondaries in the pleura (lung, breast, ovary and pancreas). 3- Liver cell failure.
3- -pneumotic effusion
4- Pulmonary infarction.
5- Tuberculosis.
6- Rheumatoid arthritis.
7- SLE.
8- Lymphoma (in young individuals).
9- Mesothelioma.
Mention a few conditions in which the pleural fluid pH and glucose levels are Iow
with a raised LDH concentration.
Empyema, malignancy, tuberculosis, rheumatoid arthritis, systemic lupus erythematosus and oesophageal
rupture Hypothyroidism.
In which conditions is the pleural fluid bloody?
Haemorrhagic fluid is seen in malignancy, pulmonary embolus, tuberculosis and trauma to the chest.
What are the earliest radiological signs of pleural fluid?
The earliest radiological signs are blunting of the costophrenic angle on the anterior-posterior view or loss
of clear definition of the diaphragm posteriorly on the lateral view.
How would you confirm your suspicions when in doubt of a small effusion ?
Either by a lateral decubitus view (which shows a layering of the fluid along the dependent chest wall
unless the fluid is loculated) or by ultrasonography.
What are the other uses of ultrasonography in the diagnosis of pleural effusion ?
Ultrasonography is also useful for loculated effusions, for guided thoracocentesis, closed pleural biopsy or
insertion of a chest drain, and to differentiate pleural fluid from pleural thickening.
What are the complications of thoracocentesis?
Pneumothorax, haemothorax, intravascular collapse and unilateral pulmonary oedema (the latter after
withdrawal of large quantities of fluid).
Dr. Saif Darif 7|Page
2010
What do you know about Meigs' syndrome?
Meigs' syndrome:- comprises pleural effusion (usually right-sided and a transudate) associated with ovarian
tumours (usually benign ovarian fibroma)
Mention a few trigger factors known to aggravate asthma.
1- Infection.
2- Emotion.
3- Exercise.
4- Drugs, e.g. beta-blockers.
5- External allergens.
6-cold weather .
What do you understand by the term 'asthma'?
Asthma is an inflammatory disorder characterized by hyper-responsiveness of the airway to various stimuli,
resulting in widespread narrowing of the airway,The changes are reversible.
What are the features of acute severe asthma?
1- Inability to complete a sentence in one breath.
2- Respiration rate greater than 25 per minute.
3- Pulse rate greater than 110 beats per minute.
4- Peak expiratory flow rate less than 50% of predicted .
What are the life-threatening indicators in acute asthma?
1- Peak expiratory flow rate less than 33% of predicted or best.
2- Exhaustion, confusion, coma.
3- Silent chest, cyanosis or feeble respiratory effort.
4- Bradycardia or hypotension.
Note. Arterial blood gases should be measured if anyof these features are present or if oxygen saturation
is less than 92%.
What are the indicators of a very severe, life-threatening attack?
1- increased carbon dioxide tension >45mmgh
2- Severe hypoxia of less than 8 kPa (60 mmHg).
3- Low pH.
Dr. Saif Darif 8|Page
2010
What are the indications for mechanical ventilation with intermittent positive
pressure ventilation ?
1- Worsening hypoxia (Pao2 <8 kPa) despite 60% inspired oxygen.
2- Hypercapnia (Pace2 >6 kPa).
3- Drowsiness.
4- Unconsciousness.
What do you understand by the term 'chronic bronchitis'?
Chronic bronchitis is cough with mucoid expectoration for at least 3 months in a year for 2 successive years.
What is the definition of emphysema?
Emphysema is the abnormal permanent enlargement of the airway distal to the terminal respiratory
bronchioles with destruction of their walls.
How would you differentiate emphysema from chronic bronchitis?
Pink puffer Blue bloater
Cyanosis Absent Prominent
Dyspnoea ++ +
Hyperinflation ++ +
Cor pulmonale - Common
Respiratory drive High Low
What do you understand by the term 'bronchiectasis'?
It is a chronic necrotizing infection of the bronchi and bronchioles leading to abnormal, permanent dilatation
of the airways.
What are the complications of bronchiectasis?
1- Pneumonia, pleurisy, pleural effusion, pneumothorax.
2- Sinusitis.
3- Haemoptysis.
4- Brain abscess.
5- Amyloidosis.
What are the major respiratory pathogens in bronchiectasis?
Staphylococcus aureus, Haemophilus infiuenzae, Pseudomonas aeruginosa.
Dr. Saif Darif 9|Page
2010
What are the common sites for localized disease?
Left lower lobe and lingula.
What are the causes of a poorly resolving or recurrent pneumonia ?
1- Carcinoma of the lung.
2- Aspiration of a foreign body.
3- Inappropriate antibiotic.
4- Sequestration (rare; suspect if left lower lobe is involved).
What are the complications of pneumonia?
1- Septicaemia.
2- Lung abscess.
3- Empyema.
4- Adult respiratory distress syndrome.
5- Multiorgan failure, renal failure.
6- Haemolytic syndrome.
7- Death.
What are the causes of lung collapse?
1- Bronchogenic carcinoma.
2- Mucus plugs (asthma, allergic bronchopulmonary aspergillosis; BMJ1982; 285: 552).
3- Extrinsic compression from hilar adenopathy (e.g. primary TB).
4- Tuberculosis (Brock's syndrome).
5- Other intrabronchial tumours including bronchial adenoma.
What is Brock's syndrome?
It is collapse due to compression of the right middle lobe bronchus by an enlarged lymph node.
When finishing the chest examination of bronchiectasis cases the examiner will ask
you "Do you like to examine any other thing in this patient?
answer yes I like to examine the hands for clubbing.
In case of Bronchiectasis the examiner will tell you that after 20 years of this
patient's disease the patient is started to develop renal failure and the examiner will
ask what do think the cause
answer will be its renal failure due to Secondary Amyloidosis .
Dr. Saif Darif 10 | P a g e
Vous aimerez peut-être aussi
- Book Index The Art of Heavy TransportDocument6 pagesBook Index The Art of Heavy TransportHermon Pakpahan50% (2)
- Orthopedics MCQs With AnswersDocument32 pagesOrthopedics MCQs With AnswerslanghalilafaPas encore d'évaluation
- Orthopedics MCQs With AnswersDocument32 pagesOrthopedics MCQs With AnswerslanghalilafaPas encore d'évaluation
- Usp Description and SolubilityDocument1 pageUsp Description and SolubilityvafaashkPas encore d'évaluation
- SOPDocument16 pagesSOPjerome marquezPas encore d'évaluation
- Physical Examination TemplateDocument9 pagesPhysical Examination Templatedhuha_minozPas encore d'évaluation
- Topographicanatomy Head TiskDocument61 pagesTopographicanatomy Head TiskRodicaPetrovaPas encore d'évaluation
- I. History Taking A. Chief Complaint B. History of Present IllnessDocument4 pagesI. History Taking A. Chief Complaint B. History of Present IllnessKen MordenoPas encore d'évaluation
- Lung Cancer ManagementDocument126 pagesLung Cancer ManagementdjonesthoracicPas encore d'évaluation
- Lymph Node Levels of NeckDocument4 pagesLymph Node Levels of NeckSaleh SaqerPas encore d'évaluation
- Anatomy of Neck MusclesDocument43 pagesAnatomy of Neck MusclesMahnoor malikPas encore d'évaluation
- History Taking and Examination For SurgeryDocument68 pagesHistory Taking and Examination For Surgerytayiba.m1995Pas encore d'évaluation
- Differential Diagnosis in ENTDocument10 pagesDifferential Diagnosis in ENTPushkar Raaj PatidarPas encore d'évaluation
- Bocca Functional Neck DissectionDocument4 pagesBocca Functional Neck DissectionNoma OlomuPas encore d'évaluation
- A Mini-Atlas of Ear-Drum Pathology PDFDocument7 pagesA Mini-Atlas of Ear-Drum Pathology PDFalexandra_i_nitaPas encore d'évaluation
- Atlas of Paranasal Sinus SurgeryDocument81 pagesAtlas of Paranasal Sinus SurgeryNemer Al-KhtoumPas encore d'évaluation
- Right Modified Neck Dissection (MND) : Case Study ONDocument71 pagesRight Modified Neck Dissection (MND) : Case Study ONAUSTIN SABUPas encore d'évaluation
- CT PNSDocument22 pagesCT PNSHany85Pas encore d'évaluation
- Acute Otitis MediaDocument18 pagesAcute Otitis MediaaliramzanPas encore d'évaluation
- MT2010 Avo10x172 8997244400Document550 pagesMT2010 Avo10x172 8997244400nursultanPas encore d'évaluation
- Chest ExaminationDocument14 pagesChest Examinationsajad abasewPas encore d'évaluation
- Examination of The Respiratory SystemDocument35 pagesExamination of The Respiratory SystemRashhmi Karthodi100% (1)
- Respiratory SystemDocument38 pagesRespiratory Systemjsreyes.402Pas encore d'évaluation
- Rev Widya Physical Examination of Respiratory SystemDocument72 pagesRev Widya Physical Examination of Respiratory SystemYuliaPas encore d'évaluation
- Nursing Care PlanDocument20 pagesNursing Care PlanmelliaiPas encore d'évaluation
- Physical Examination in Respiratory SystemDocument58 pagesPhysical Examination in Respiratory SystemMarian0% (1)
- Respiratory ExaminationDocument9 pagesRespiratory Examinationربيع ضياء ربيعPas encore d'évaluation
- Pulmonology Short CasesDocument10 pagesPulmonology Short CasesRZ Ng100% (1)
- Pemeriksaan Fisik ParuDocument7 pagesPemeriksaan Fisik ParuLila WatiningrumPas encore d'évaluation
- Respi PACES - V2Document6 pagesRespi PACES - V2Rebecca Teng Siew YanPas encore d'évaluation
- Chest 2012-2013 Dr. Sameh LabibDocument83 pagesChest 2012-2013 Dr. Sameh LabibMahmoud AbouelsoudPas encore d'évaluation
- Almaghrabi Resp ExaminationDocument33 pagesAlmaghrabi Resp ExaminationSagit Nauman81Pas encore d'évaluation
- Pediatric RadiologyDocument2 pagesPediatric RadiologyAnonymous HH3c17osPas encore d'évaluation
- Responses To Altered Respiratory FunctionDocument19 pagesResponses To Altered Respiratory FunctionKoleen KirstenPas encore d'évaluation
- Airway Anatomy &assessmentDocument44 pagesAirway Anatomy &assessmentAya AlefeshatPas encore d'évaluation
- Respiratory System SummaryDocument6 pagesRespiratory System SummaryKiara GovenderPas encore d'évaluation
- 11-The PharynxDocument73 pages11-The PharynxM.IBRAHIM ALHAMECHPas encore d'évaluation
- Resp Exam A: Wicep: Clubbing:: Emphysema Lung Cancer Cystic Fibrosis (From Pathology)Document8 pagesResp Exam A: Wicep: Clubbing:: Emphysema Lung Cancer Cystic Fibrosis (From Pathology)amsirakPas encore d'évaluation
- Respiratory ExaminationDocument20 pagesRespiratory ExaminationAmirul SyafizPas encore d'évaluation
- Lecture# 2 PR-Restrictive Lung Diseases PlanDocument28 pagesLecture# 2 PR-Restrictive Lung Diseases PlanHafsa AzizPas encore d'évaluation
- 4 Lung AuscultationDocument3 pages4 Lung AuscultationCristina TofanPas encore d'évaluation
- PneumoniaDocument2 pagesPneumoniama7moud farsPas encore d'évaluation
- Examination of The Chest and LungsDocument5 pagesExamination of The Chest and Lungsteena12aPas encore d'évaluation
- 3 Physical AssessmentDocument19 pages3 Physical AssessmentFarmisa MannanPas encore d'évaluation
- CLINICAL BronchiectasisDocument3 pagesCLINICAL BronchiectasisSyximsh FPPas encore d'évaluation
- Lesson 6 - THORAX AND LUNGSDocument2 pagesLesson 6 - THORAX AND LUNGSKuldip GillPas encore d'évaluation
- Pemeriksaan ThoraxDocument27 pagesPemeriksaan ThoraxYaasinta ArlaesPas encore d'évaluation
- C-7 Resperatory System (Tu)Document81 pagesC-7 Resperatory System (Tu)Harsh PatelPas encore d'évaluation
- Respiratory ExaminationDocument8 pagesRespiratory ExaminationKelly ReyesPas encore d'évaluation
- RS Examination PSC2021Document3 pagesRS Examination PSC2021علي 707Pas encore d'évaluation
- Suara ParuDocument31 pagesSuara ParuSuyanto nduduPas encore d'évaluation
- 4-Larynx. Cong&trauma of LarynxDocument26 pages4-Larynx. Cong&trauma of LarynxislamPas encore d'évaluation
- IPPADocument4 pagesIPPAIsaac KipchumbaPas encore d'évaluation
- Final Death Note - Compre NotesDocument1 550 pagesFinal Death Note - Compre NotesSteph TabasaPas encore d'évaluation
- MVS Pulmonary AuscultationDocument8 pagesMVS Pulmonary Auscultationvashini9151Pas encore d'évaluation
- 3 en AusculationDocument22 pages3 en AusculationsajidmuPas encore d'évaluation
- Pemeriksaan Fisik Sistem Pernapasan: Equipment NeededDocument78 pagesPemeriksaan Fisik Sistem Pernapasan: Equipment Neededsri karinaPas encore d'évaluation
- RespirationDocument16 pagesRespirationkamalPas encore d'évaluation
- MCN KweenDocument4 pagesMCN KweenAngelo SiguePas encore d'évaluation
- Physical Examinations Respiratory System: InspectionDocument5 pagesPhysical Examinations Respiratory System: InspectionAzizan HannyPas encore d'évaluation
- STUDY GUIDE 2 OXYGENATION Operaña EllayzaDocument5 pagesSTUDY GUIDE 2 OXYGENATION Operaña EllayzaOPERAñA ELLAYZA RB DECANOPas encore d'évaluation
- Radiology - Imaging of The ThoraxDocument69 pagesRadiology - Imaging of The ThoraxOrlando Daniel SitompulPas encore d'évaluation
- Medical Surgical Nursing Lecture 234 Pages Pg. 333 566Document189 pagesMedical Surgical Nursing Lecture 234 Pages Pg. 333 566Crystal Ann TadiamonPas encore d'évaluation
- Pemeriksaan ThoraxDocument27 pagesPemeriksaan ThoraxSubchanPrasetyoPas encore d'évaluation
- Respiratory System ExaminationDocument46 pagesRespiratory System ExaminationÑäd ÉèmPas encore d'évaluation
- Answer 2Document21 pagesAnswer 2bakesami100% (1)
- Gyn Obs 6th Year Exam From GazaDocument3 pagesGyn Obs 6th Year Exam From GazabakesamiPas encore d'évaluation
- CommunityDocument7 pagesCommunitybakesamiPas encore d'évaluation
- Chief Complain and History of Present IllnessDocument2 pagesChief Complain and History of Present IllnessIshaq DerbashiPas encore d'évaluation
- VurDocument6 pagesVurbakesamiPas encore d'évaluation
- FactSet London OfficeDocument1 pageFactSet London OfficeDaniyar KaliyevPas encore d'évaluation
- Entero SequencesDocument12 pagesEntero SequencesKelvin SueyzyPas encore d'évaluation
- The History of AstrologyDocument36 pagesThe History of AstrologyDharani Dharendra DasPas encore d'évaluation
- SMC VM Eu PDFDocument66 pagesSMC VM Eu PDFjoguvPas encore d'évaluation
- Keyword 4: Keyword: Strength of The Mixture of AsphaltDocument2 pagesKeyword 4: Keyword: Strength of The Mixture of AsphaltJohn Michael GeneralPas encore d'évaluation
- ContempoDocument4 pagesContempoPrincess Jonette YumulPas encore d'évaluation
- Coding DecodingDocument21 pagesCoding DecodingAditya VermaPas encore d'évaluation
- Critical Analysis of W.H Auden Poems The PDFDocument8 pagesCritical Analysis of W.H Auden Poems The PDFMöĤämmĔd äĹ-ŚäÁdï100% (1)
- Human Wildlife Conflict Resolution PDFDocument9 pagesHuman Wildlife Conflict Resolution PDFdemiPas encore d'évaluation
- Principles Involved in Baking 1Document97 pagesPrinciples Involved in Baking 1Milky BoyPas encore d'évaluation
- IBM BladeCenter S RedBookDocument36 pagesIBM BladeCenter S RedBookGuillermo García GándaraPas encore d'évaluation
- Youth Camp Registration Form-2022Document1 pageYouth Camp Registration Form-2022FlerkPas encore d'évaluation
- Course Code:TEX3021 Course Title: Wet Processing Technology-IIDocument20 pagesCourse Code:TEX3021 Course Title: Wet Processing Technology-IINakib Ibna BasharPas encore d'évaluation
- Automatic Train OperationDocument6 pagesAutomatic Train OperationAnupam KhandelwalPas encore d'évaluation
- 1 s2.0 S1110016815000563 Main PDFDocument13 pages1 s2.0 S1110016815000563 Main PDFvale1299Pas encore d'évaluation
- GB GW01 14 04 02Document2 pagesGB GW01 14 04 02Muhammad LukmanPas encore d'évaluation
- Beastlikebalsam - Muscle BuildingDocument10 pagesBeastlikebalsam - Muscle BuildingBalsam LaaroussiPas encore d'évaluation
- Region 1 - Concreting Works Materials Prices - PHILCON PRICESDocument9 pagesRegion 1 - Concreting Works Materials Prices - PHILCON PRICESMark Gregory RimandoPas encore d'évaluation
- Integration ConceptDocument34 pagesIntegration ConceptJANELLA ALVAREZPas encore d'évaluation
- Asme Code Sec Ix Ma Appe 2004Document3 pagesAsme Code Sec Ix Ma Appe 2004Guillermo CamachoPas encore d'évaluation
- Statics: Vector Mechanics For EngineersDocument39 pagesStatics: Vector Mechanics For EngineersVijay KumarPas encore d'évaluation
- Compiled LecsDocument24 pagesCompiled LecsNur SetsuPas encore d'évaluation
- Physics Unit 11 NotesDocument26 pagesPhysics Unit 11 Notesp.salise352Pas encore d'évaluation
- Prevailing Torque Locknut Technical SpecificationsDocument3 pagesPrevailing Torque Locknut Technical SpecificationsLiu YangtzePas encore d'évaluation
- PANASONIC - WebCam-TQZJ402 - TY-CC20W PDFDocument188 pagesPANASONIC - WebCam-TQZJ402 - TY-CC20W PDF123anthonyPas encore d'évaluation
- Blue Modern Company Profile PresentationDocument15 pagesBlue Modern Company Profile PresentationjanePas encore d'évaluation
- Clinical Biomechanics: Leigh W. Marshall, Stuart M. McgillDocument4 pagesClinical Biomechanics: Leigh W. Marshall, Stuart M. McgillMichael JunPas encore d'évaluation