Académique Documents
Professionnel Documents
Culture Documents
Beta Adrenergic Agonists
Transféré par
Phạm Thành LýDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Beta Adrenergic Agonists
Transféré par
Phạm Thành LýDroits d'auteur :
Formats disponibles
Beta Adrenergic Agonists*
Harold S. Nelson, COL, MC, USA
Betaprincipal
adrenergic agonists and theophylline are the
bronchodilators employed in the treat-
nucleotide-sensitive regulator protein occurs. This
combination then activates the third component, ade-
ment of bronchial asthma. During the last decade, the nylate cyclase, which converts ATP to cyclic
clinical usefulness of theophylline has been enhanced
EPHEDRINE:
by the availability of serum theophylline determina-
tions and sustained release fOrmulations. Beta adre-
nergic bronchodilators were initially somewhat
eclipsed in the United States by these improvements
in theophylline therapy. Now, however, with the CATECHOLAMINE$:
introduction of selective and long lasting adrenergic
agents, appreciation of their role in the treatment of
bronchial asthma is increasing. Selection of the appro-
priate adrenergic bronchodilators is more complex
~. ~2
than the use of theophylline because of the greater [Pt'IIEPH~ I NE CH3 H
variety of available agents and routes of administra-
.-CH3
tion, because of the special problems related to proper ISOPIIIOTERNOL CH
'CH3
H
techniques of aerosol therapy, and because of the
development of beta adrenergic tolerance or subsen- ... CH3
I S0E THARIN CH Cz "!I
sitivity. 'C".,3
Recognition of receptors with differing sensitivity to
the naturally-occurring catecholamines began with
Alquist in 1948. He identified alpha receptors which
mediate predominantly excitatory responses and beta
receptors which mediate primarily inhibitory re-
sponses. Lands in 1967 further separated the beta NON-cATEOtOL ADRENERGIC IRONCHODI.AlORS:
RESORCINOLS :
receptors on the basis of their relative responsiveness
OH OM
to epinephrine and norepinephrine into beta~> modu-
lating excitatory responses of the heart and adipose oC~-CHz-NH-RI
tissue, and bet"at mediating the inhibitory responses OH
which include not only relaxation of bronchial, vascu- METAPROTERENOL
lar and uterine smooth muscle, but also inhibition of
secretory activity of a variety of cells including his- ,cH3
TERBUTALINE C 'CHJ
tamine release from mast cells, antibody production CH3
by lymphocytes and enzyme release by polymorpho- ,cH 3
nuclear leukocytes. FENOTEROL
CH'CHz O o H
The response to beta adrenergic stimulation is
mediated by three distinct structural units in the cell
membrane. First is a receptor with specificity of either OTHER :
the beta, or bet"at type. Upon occupation of this
receptor by an agonist, interaction with a quanine
ALBUTEROL
HlNCONH
O
OH /CH3
From the Allergy-Immunology Service, Fitzsimons Army Medical 1
Center, Aurora, Colorado. CA~BUTEROL OH CH- CHz - NH- C~H3
The opinions or assertions contained herein are the private views of CH3
the author and are not to be construed as official or as reflecting the
views of the Department of the Army or the Department' of FIGURE 1. The structural relationships of the adrenergic bron-
Defense. chodilators.
CHEST I 82 I 1 I July, 1882 I Supplement 338
3'5'adenosine monophosphate (cAMP) which in tum there remains a role fur this fixed combination medica-
modulates most of the beta adrenergic responses . tion in the treatment of patients who require only a
Epinephrine was first used as a bronchodilator in mild bronchodilator.
1910, followed in 1924 by the introduction of Isoproterenol is a potent but nonselective and short-
ephedrine into Western medicine. In 1941, with the acting bronchodilator. Cardiac stimulation is usually
introduction of isoproterenol, a drug free of alpha- not a problem with one or two metered doses, but
adrenergic stimulating properties, began the system- becomes evident if the dose is increased. Iso-
atic development of adrenergic bronchodilators with proterenol is clearly unsuited fur maintenance bron-
selective and long lasting effects (Fig 1). Changes in chodilator therapy or prophylactic use prior to exercise
the isoproterenol structure involved one of two ap- because of its brief duration of peak effect. The rapid
proaches. First was modification in the catechol nu- onset of bronchodilator action does provide prompt
cleus which consists of a phenolic ring with hydroxyl relief of symptoms in most patients. However, in view
groups in the 3 and 4 position. By either changing the of the proven superiority of the newer beta adrenergic
position of the hydroxyl groups to the third and fifth agonists, there would appear to be little justification,
carbons or by substituting another chemical group fur other than habit, for the continued use of iso-
the hydroxyl on the third carbon, the compound is no proterenol.
longer a catecholamine and, therefOre, no longer Isoetharine was the first widely employed drug
susceptible to degradation by the enzyme catechol-0- which clearly had increased affinity for the betas
methyl-transferase (COMT). Increased selectivity fur adrenoceptors. Although it has slightly longer dura-
the betas receptor can be achieved by increasing the tion of action due to resistance to MAO, its pattern of
size of the side chain adjacent to the nitrogen atom. bronchodilation closely resembles that of iso-
Increasing the bulk in this position also makes the drug proterenol, and its use would also appear limited to
resistant to degradation by monoamine-oxidase rapid relief of acute attacks of bronchoconstriction.
(MAO) and further prolongs its action. When repeated dosing is required, its decreased
cardiac stimulation is an advantage.
SPECIFIC BETA ADRENERGIC
By virtue of a shift of the hydroxyl groups to the third
BRONCHODILATORS
and fifth carbons on the benzene ring, metaproterenol
Epinephrine is still the drug of choice fur treatment is not susceptible to inactivation by COMT and can,
of acute anaphylaxis where a combination of alpha and therefOre, be administered orally. The bulk of the side
beta adrenergic properties are desirable. It is still chain is unchanged from that of isoproterenol and, as
employed in the treatment of severe asthma, and might be expected, metaproterenol does not differ
several recent studies have confirmed the efficacy of significantly from isoproterenol in its relative cardiac
injections of 0.25 mg (0.01 mglkg in small children) and bronchial potency. 1 Furthermore, since meta-
repeated at 15 to 20 minute intervals in the treatment proterenol is still susceptible to MAO, its duration of
of patients with acute bronchoconstriction. The princi- action is somewhat shorter than the selective betas
pal alternative to epinephrine in the United States is adrenergic agonists whether administered orally or by
terbutaline. inhalation. u Because of this shorter duration of action,
Even befure the development of the newer adre- metaproterenol is not as well suited fur either mainte-
nergic drugs, ephedrine was seldom employed alone. nance bronchodilator therapy or fur prevention of
It has demonstrable but relatively weak bronchodilat- exercise-induced bronchoconstriction unless the activ-
ing properties, its use is frequently associated with ity will be completed within two hours .
side effects, and as a single agent it probably has little Terbutaline, albuterol, fenoterol and carbuterol are
place in the modem bronchodilator armamentarium. selective betas adrenergic bronchodilators and to date
The combination of ephedrine and aminophylline there is little evidence that any one is more selective
enjoyed many years of popularity, and it has been fur bet~ receptors than the others . All these drugs are
repeatedly demonstrated that the combination pro- effective orally and by inhalation. All are long-acting
duces greater bronchodilation than either component by any route of administration. All are largely free of
alone. Furthermore, the two components comple- direct cardiac stimulation in doses employed clinically;
ment each other since initially ephedrine contributes however, all share the same dose-limiting side ef-
more to the bronchodilator effect, then, as subsen- fects-tremor and tachycardia. Both of these side
sitivity develops to ephedrine, theophylline blood effects are directly related to betas receptor stimula-
levels rise and the aminophylline becomes the princi- tion. Stimulation of betas receptors in skeletal muscle
pal contributor to the overall bronchodilator action. In causes tremor and betas stimulation of the smooth
both acute and chronic comparisons, the combination muscle in blood vessels supplying skeletal muscles
tablets have been roughly equivalent to the oral results in decreased peripheral resistance, leading to
selective betas agonists and it has been suggested that reflex tachycardia and increased cardiac output.
34S Advances In Asn11ment and Therapy of Asthma
80 TERBUTAUNE
o--o Subcutaneous
-Oral
.-- - ... Aerosol
80
0.25 mg
FIGURE 2. Changes in fOrced expiratory
volume in one second (FEV J fOllowing
three different routes of administration of
80 120 180 240 300 terbutaline. (Dulfano MJ, Glass P. Ann
1111E IN MINUTES Allergy 1976; 37:357, by permission)
recommended for terbutaline may not fully exploit its
Routes of Administration betas selectivity.
Figure 2 compares the onset and duration of bron- The advantage of administration of beta adrenergic
chodilation and the relative doses required when the bronchodilators by inhalation is evident in Figure 2.
same drug, terbutaline, is administered by mouth, by The onset is rapid, the bronchodilation produced is
injections, and by inhalation. 4 prolonged, and the therapeutic ratio of bronchodila-
The catecholamines, epinephrine, isoproterenol tion to side effects is greatly increased over the other
and isoetharine, are too rapidly degraded by CO MT to routes of administration.
be effective by mouth. Even noncatecholamine adre- By inhalation, the catecholamines isoproterenol and
nergic bronchodilators undergo significant conjuga- isoetharine, produce maximal bronchodilation by five
tion and inactivation in the gut wall and liver, so the to 15 minutes, following which the effect progressively
oral dose is quite large. When specific betas agonists, declines and is usually undetectable between one and
such as albuterol or terbutaline, are given by mouth, two hours following administration. The non-
the peak effect is usually achieved in two to four hours, catecholamine beta adrenergic agonists are only
and bronchodilation persists for four to six hours. In a slightly less rapid in onset, with 75 percent of max-
study by Wilson et al5 in which the bronchodilator imum effect attained by five minutes, peak bron-
response to terbutaline was monitored during a year of chodilation is attained between 30 and 90 minutes, and
therapy, the mean response to a 5 mg oral dose was an there is little loss of effect until after four hours.
increase in FEV1 of 23 percent, while 25 mg of An unresolved question is the proper aerosol dose
ephedrine, in the same study, produced a mean for the selective betas adrenergic agonists. When these
increase in FEV1 of only 12 percent. drugs are given orally, the occurrence of side effects
While on theoretical grounds terbutaline should be generally limits the dose to one producing consider-
superior to epinephrine for parenteral use, compara- ably less than maximal bronchodilation. This con-
tive studies employing conventional doses have not straint does not exist when these agents are inhaled,
clearly shown an advantage in the incidence of side since side effects are rarely experienced with normally
effects or in the magnitude or duration ofbronchodila- recommended doses. Some investigators have re-
tion. The report by Pang and colleagues6 suggests that ported that maximal bronchodilator effect is achieved
terbutaline may be employed in considerably larger with doses of the selective betas agonists which are
doses than would be considered with epinephrine. even less than those ordinarily employed. It is likely
They administered up to 0.04 mglkg at ten to IS- that these reports can be credited to a failure to
minute intervals in children with status asthmaticus. appreciate that bronchodilation is related to the log of
One ten-year-old patient received a total of 10.2 mg the dose (Fig 3), and if the dose is plotted arith-
over a period of three and three-quarter hours. Nine of metically, there will be an apparent asymptote. Three
the ten children, all refractory to aminophylline and observations may be made from Figure 3, which shows
conventional doses of epinephrine, responded to .this the dose response to aerosolized terbutaline delivered
regimen. This study suggests that the dosage schedule by metered dose inhaler, IPPB, and compressor pow-
CHEST I 82 I 1 I July, 1982 I Supplement 35S
encountered most commonly, but not exclusively in
the young and old. Another reason for caution in
relying solely on aerosol therapy is the potential for
abuse of this form of treatment especially by teen-
agers.
Another consideration in reliance on aerosol admin-
istration for bronchodilator therapy is the uncertainty
of the penetration of aerosols into the peripheral
. - ISOPIDTllliiCIL .I 1
airways. There is no doubt that in stable asthmatic
patients, properly inhaled beta-adrenergic agonists
II - Tl.UTAUil .IH a _.TliiUTAUil Ua 1Y CW II
- Tl.UTAL .HD a - TliiUTAUil 1.5& IY . , .
can penetrate small airways, since they have been
demonstrated to decrease frequency dependence of
.I .2 .3 .I .7 1.1 U U U Ul.U .D compliance. Also in a study in patients with acute
CIIIIIIUTM liSE U severe asthma aerosolized albuterol administered by
FrcURB 3. Comparison rX changes In FEV1 with repeated doses rX tight-fitting mask relieved paradoxic pulse more effec..
iloproterenol 0.1 mg. terbutaline O.li5 mg. and terbutaline 0.25 mg tively than did intravenous albuterol, while causing far
via pressurized canister aerosol, and terbutaline 1.5 mg aerosolized
via COMPand IPPB. (Weber Rw, Petty WE, Nelson HS. JAllergy
less cardiac stimulation. 9 On the other hand, it would
Clin lmmuno) 1979; 63:116, by permission.) not be surprising if inhaled medication failed to
penetrate uniformly the distal airways in this disease
ered nebulizer. First, there is no advantage to IPPB which is characterized by mucus plugging and uneven
over the pressure nebulizer; second, six to eight times distribution of inspired air even in relatively
as large a stated dose must be employed with either asymptomatic patients. There are studies which lend
nebulizer compared to the freon-propelled inhaler for support to this concern. They show that for the same
the same degree ofbronchodilation (and, therefore, for degree ofdilation of large airways, parenterally-admin-
the same amount of deposition in the lungs); and istered drug produced greater dilation of small airways
finally, the bronchodilator response continued up to than did the same drug by inhalation. 10
the maximum doses which were tested. 7 These curves Because of evidence suggesting more effect on
were generated by administering doses at 20-minute peripheral airways with oral medication, Thiringer
intervals and constructing a cumulative dose response and Svedmyr11 have suggested that a proper approach
curve. The same results have been obtained in a large to the chronic use of adrenergic bronchodilators in
group of patients given individual doses of albuterol of patients requiring continuous therapy would be to
increasing size on separate days. In that study there employ oral therapy with aminophylline, a beta ago-
was a linear bronchodilator response to the maximum nist, or both in doses which do not cause troublesome
dose of eight inhalations from a metered dose inhaler side effects and, if significant symptoms persist, to
or 15 mg by IPPB. Side effects were not encountered employ the inhaled beta adrenergic agonists on a
with the metered dose inhale~; but were seen with regular basis.
increasing frequency at the higher doses by IPPB.
Despite obvious advantages in the ratio of bron- Subsensitivity
chodilation to side effects with administration of beta Subsensitivity or tolerance is a diminished respon-
agonists by inhalation, there are other factors which siveness which develops in many physiologic systems
should be considered before embracing aerosols as the when receptors are repeatedly exposed to increased
exclusive route of administration. When the drug is levels of their agonist either natural or administered.
given by mouth or injected, only the most unusual With chronic administration, subsensitivity develops
circumstances will prevent the drug from reaching the to the beta adrenergic agonists and results in a reduced
adrenergic receptors in the lung. By inhalation, how- bronchodilator response. This occurs over a period of
ever, especially with the freon-propelled device, care- one to two weeks and requires a similar period of time
ful coordination between actuation and breathing, to reverse after the beta adrenergic drug has been
slow inhalation, and breathholding are required for discontinued. In vitro studies of tissue from patients in
optimal or even predictable results. A number of whom adrenergic subsensitivity has developed show
recent surveys have documented the frequency of markedly decreased numbers of available beta-adre-
patient error in using these devices. In one survey of nergic receptors and a similarly diminished generation
30 regular users of metered-dose inhalers, 14 made ofcAMP from ATP on stimulation of adenylate cyclase.
major errors, most commonly inhaling completely Since adrenergic subsensitivity is caused by de-
prior to actuating the device, and second most com- creased receptor density, it is not specific for any
monly actuating the device and holding the breath particular beta adrenergic agonist. Failure to com-
without inhaling. 8 Difficulty with use of inhalers is pletely exclude all adrenergic medication, oral and
Adloencee In A11111ment Mel Therapy ol Alllvna
inhaled, for two weeks prior to initiating drug studies marked in eight hours. Holgate et al14 induced adre-
has resulted in failure to detect the development of nergic subsensitivity in normal individuals with aero-
subsensitivity during many drug trials. solized albuterol (Table 1). Six hours following in-
What is the magnitude of the loss of the adrenergic travenous administration of 200 mg hydrocortisone,
bronchodilator response, and does it significantly their response to inhaled albuterol was restored to the
reduce the clinical effectiveness of these medications? original level. From the study by Weber et al11 (Thble 1)
Thble 1 summarizes some of the studies in which the it appears that low-dose alternate day and inhaled
development of adrenergic subsensitivity has been steroids, such as are ordinarily employed in the
reported. It is evident that adrenergic subsensitivity chronic treatment of patients with bronchial asthma,
occurs with both oral and aerosol therapy. In these are not sufficient to prevent the development of
studies, the peak FEY1 response declined by 14 to 58 adrenergic subsensitivity.
percent, and the duration during which the FEY1 Since patients with status asthmaticus have many
remained more than 15 percent above the baseline was reasons for poor response to beta adrenergic bron-
reduced even more, usually about 50 percent for long- chodilators, including mucosal edema and mucus
1\Cting bronchodilators. Once subsensitivity develops plugging, they would not be expected to respond as
to a particular dose, usually after one or two weeks, dramatically to corticosteroids as did the patients of
there is no further loss of bronchodilator effect with Ellul-Micallef and Holgate. Nevertheless, there is
continuing observation for up to 12 months. In most often a history of recent overuse of adrenergic bron-
patients, the beta agonists continue to be effective chodilators, particularly by aerosol, in patients seen in
bronchodilators even after subsensitivity has devel- emergency rooms, so an element of induced adre-
oped. Perhaps the importance of recognizing the nergic subsensitivity may exist as well. Awareness that
phenomenon of subsensitivity is to serve as a note of corticosteriods can restore adrenergic responsiveness
caution in assessing the findings ofsingle-dose studies, in as little as one hour provides an additional reason for
particularly if there is no information on preceding their prompt use in moderate doses in patients with
adrenergic therapy. Since the duration ofbronchodila- exacerbations of asthma not responding to normal
tion is reduced more than the peak, one should not adrenergic therapy.
expect patients to obtain the same prolonged bron- TnE RoLE oF BETA ADRENERGIC BRONCHODILATORS
chodilator effect during chronic administration that is IN THE TREATMENT OF AsTHMA
often reported in the literature. Inhaled beta adrenergic bronchodilators are the
Corticosteroids have been reported to restore beta treatment of choice for prompt relief of acute episodes
adrenergic responsiveness. Ellul-Micallef and Fench13 of wheezing and dyspnea no matter what has been the
identified ten stable asthmatic patients who failed to stimulus.
respond to inhaled isoproterenol. Following intra- Although exercise-induced bronchoconstriction can
venous infusion of 40 mg prednisolone, eight of the ten be prevented by therapy with cromolyn, theophylline
became responsive to isoproterenol. There was some or oral beta adrenergic agonists, it is most conve-
effect evident after one hour and it was even more niently and effectively prevented with the least num-
18ble 1-~ cf S~ willa Long-term Admlniltration cf &14-~ BronclaotUliJtora
8-Adren Route Change in Peak Change in Duration c:A
Author Washout Admin Drug Duration Bronchodilator Response Bronchodilator Response
Nelson 11 yes oral albuterol 1 week FEV 1 ~20% >6 hr to5 hr
12 weeks FEVI~~
Jenne 13 inhaled oral terbutaline 2 weeks FEVIH4%
allowed
Holgate1 yes aerosol albuterol 4 weeks SGawi54%
Plummer14 inhaled oral fenoterol 3 months but not signif
FEV 1 ~31% tFEV1>15% 5 hr to 3\11 hr
allowed oral ephedrine tFEV1>15% 2 hr to \II hr
Chervinsky11 aerosol metaproterenol 2 months SignlftFEV1 4 hr .. 2 hr
isoproterenol SigniftFEV1 3 hr .. 5 min
1hwtlein17 aerosol terbutaline 6weeks FEVIUiO%
Brandon11 aerosol fenoterol 3 months tFEV1 15% 4 hr .. 2 hr
aerosol isoproterenol tFEV1 15% 1 hr .. 20 min
Miller yes oral fenoterol 6weeks Reduced FEV1 signi~at 2+3 hr
terbutaline FEV1 signi~at 2,3+4 hr
Bransoomb10 yes aerosol fenoterol 3 months FEV 1 ~31% FEV1above baseline 6 hr .. 3 hr
Van ArsdeJII yes oral fenotero! 3 months significant reduction
We be..- yes aerosol terbutaline 3 months FEV 1 ~37% FEV1>15% 4 hr .. 2 hr
-infOrmation not given
CHEST I 82 I 1 I July, 1882 I Supplement 378
her of side effects by inhalation of a long-acting 7 Weber RW, Petty WE, Nelson HS. Aerosolized terbutaline in
adrenergic bronchodilator shortly before beginning asthmatics: comparison of dosage strength, schedule, and
method of administration. J Allergy Clin Immunol1979; 63:116
exercise.
8 Shim C, Williams Jr MH. The adequacy of inhalation of aerosol
The relative role of beta adrenergic agonists and &om canister nebulizers. Am J Med 1980; 69:891
theophylline for chronic bronchodilator therapy is not 9 Bloomfield P, Carmichael J, Etrie GR, Jewell NP, Crompton GK.
established. A recent study by Rachelefsky and co- Comparision of salbutamol given intravenously and by intermit-
authors.. on the use of oral albuterol in children clearly tent positive pressure breathing in life threatening asthma. Br
Med J 1979; 1:848
demonstrated that symptom scores, pulmonary func-
10 whkin DP, 'Iievor E, Chopra SK, 'Illplin GV. Sites of airway
tion, and need for additional medication can all be dilation in asthma fOllowing inhaled versus subcutaneous tel'-
significantly improved by oral adrenergic therapy butaline: comparison of physiologic tests with radionuclide lung
alone in tolerated doses. Smith and colleagues111 com- images. Am J Med 1980; 68:14
pared inhaled terbutaline four times daily with max- 11 Thiringer G, Svedmyr N. Comparison of infused and inhaled
terbutaline in patients with asthma. Scand J Respir Dis 1977;
imum therapeutic doses of theophylline in a group of 57:17
adult asthmatic patients. Pulmonary function tests 12 Nelson HS, Raine Jr D, Doner HC, Posey WC. Subsensitivity to
performed regularly at home were not significantly the bronchodilator action of albuterol produced by chronic
different while on either of the drugs alone, but were administration. Am Rev Respir Dis 1977; 166:871
significantly better when both drugs were taken to- 13 Jenne JW, Chick Tw, Strickland RD, Wall FJ. Subsensitivity of
beta responses during therapy with along-acting beta-2 prepara-
gether. It is evident that beta adrenergic bronchodila- tion. J Allergy Clin Immunol 1977; 59:383
tors are possible alternatives as well as additions to 14 Holgate S1: Baldwin CJ, 'Illttersfield AE. B-adrenergic agonists
long-term theophylline therapy. Further studies will resistance in normal human airways. Lancet 1977; 2:375
be necessary to determine which are the most effective 15 Plummer AL. Drug tolerance to beta-2 adrenergic agents. Chest
drug regimens for patients requiring continuous treat- 1978; 73(suppl):994
16 Chervinsky P, Bolinkoff S. Comparison of metaproterenol and
ment.
isoproterenol aerosols: spirometric evaluation after two months'
The role of beta-adrenergic bronchodilators in the therapy. Ann Allergy 1969; 27:611
emergency treatment of acute, severe episodes of 17 'Uautlein J, Allegra J, Gillin M. Aerosolized terbutaline suHate-
bronchial asthma has been clarified by several recent an evaluation of efficacy and side effects in patients with
studies. The response to repeated doses of injected reversible airway disease. J Clin Pharmacol1977; 17:76
epinephrine or inhaled short-acting beta agonists has 18 Brandon ML. Long-term study comparing fenoterol and iso-
proterenol inhalation in asthmatic patients. Ann Allergy 1978;
been compared to conventional loading doses of 40:86
aminophylline followed by continuous infusion. The 19 Miller WC, Rice DL. A comparison of oral terbutaline and
studies are in agreement that the response to adre- fenoterol in asthma. Ann Allergy 1980; 44:15
nergic bronchodilators by either route was equal and 20 Branscomb BU. Efficacy and side effects offenoterol compared
either was superior to aminophylline.111.rr The addition with isoproterenol administered by metered dose inhalers in
asthma. Chest 1978; 73(suppl):1002
of aminophylline to the adrenergic agonists provided a 21 Van Arsdel Jr PP, Schaffiin RM, Rosenblatt J, Sprenkle AC,
modest but usually significant additional bronchodila- Altman LC. Evaluation of oral fenoterol in chronic asthmatic
tor effect. rr- These studies suggest that the impor- patients. Chest 1978; 73(suppl):997
tance of aminophylline in the emergency room treat- 22 Weber Rw, Smith JA, Nelson HS. Aerosolized terbutaline in
ment of asthma may have been overemphasized in asthmatics: development of subsensitivity with chronic adminis-
tration. (submitted fur publication)
recent years, leading to underutilization of what has 23 Ellul-MicallefR, Fench FF. Effect of intravenous prednisolone in
now been proven to be the more important component asthmatics with diminished adrenergic responsiveness. Lancet
of the treatment, the adrenergic bronchodilators. 1975; 2:1269
REFERENCES 24 Rachelefsky GS, Katz RM, Siegel SC. Albuterol syrup in the
1 McEvoy JDS, Vall-Spinosa A, Paterson JW. Assessment of treatment of the young asthmatic child. Ann Allergy 1981; 47:143
orciprenaline and isoproterenol infusions in asthmatic patients. 25 Smith JA, Weber Rw, Nelson HS. Double-blind comparison of
Am Rev Respir Dis 1973; 108:490 optimal dose theophylline and aerosolized terbutaline in the
2 Formgren H. A clinical comparison of the effect of oral tel'- treatment of bronchial asthma. Chest 1980; 78:816
butaline and orciprenaline. Scand J Respir Dis 1970; 51:195 26 Rossing TH, Fanta CH, Goldstein DH, Snapper JR, McFadden
3 Formgren H. Clinical comparison of inhaled terbutaline and Jr ER. Emergency therapy of asthma: comparison of the acute
orciprenaline in asthmatic patients. Scand J Respir Dis 1970; effects of parenteral and inhaled sympathomimetics and infused
51:203 aminophylline. Am Rev Respir Dis 1980; 122:365
4 Dulfimo MJ, Glass P. The bronchodi1ator effects of terbutaline: 27 Appel D, Shim CS, Williams Jr MH. Comparative effect of
route of administration and patterns of response. Ann Allergy epinephrine and aminophylline in the treatment ofacute asthma.
1976; 37:357 Am Rev Respir Dis 1978; 177(part 2):91
5 Wilson AF, Novey HS, Cloninger P, Davis J, White D. Cardio- 28 Rossing TH, Fanta CH, McFadden Jr ER. A controlled trial of
pulmonary effects of long-term bronchodilator administration. the use of single versus combined drug therapy in the treatment
J Allergy Clin Immunol 1976; 58:204 of acute episodes of asthma. Am Rev Respir Dis 1981; 123:190
6 Pang LM, Rodriguez-Martinez F, Davis WJ, Mellins RB. Tel'- 29 Josephson GW, MacKenzie EJ, Uetman PS, Gibson G. Emel'-
butaline in the treatment of status asthmaticus. Chest 1977; gency treatment of asthma: a comparison of two treatment
72:469 regimens. JAMA 1979; 242:639
388
Vous aimerez peut-être aussi
- Comparative Endocrinology V1D'EverandComparative Endocrinology V1U. S. Von EulerPas encore d'évaluation
- Extracted Pages From Basic - and - Clinical - Pharmacology - Fourteen - 2Document8 pagesExtracted Pages From Basic - and - Clinical - Pharmacology - Fourteen - 2ed trsgf rgsfPas encore d'évaluation
- Extracted Pages From Basic - and - Clinical - Pharmacology - Fourteen - 2Document11 pagesExtracted Pages From Basic - and - Clinical - Pharmacology - Fourteen - 2ed trsgf rgsfPas encore d'évaluation
- Antihistamines: Student Learning GoalsDocument45 pagesAntihistamines: Student Learning GoalsDaniel WangPas encore d'évaluation
- 7.016 Recitation 3 - Fall 2018: (Note: The Recitation Summary Should NOT Be Regarded As The Substitute For Lectures)Document6 pages7.016 Recitation 3 - Fall 2018: (Note: The Recitation Summary Should NOT Be Regarded As The Substitute For Lectures)Manish SarkarPas encore d'évaluation
- Interaction of Nerve Agent Antidotes With Cholinergic SystemsDocument12 pagesInteraction of Nerve Agent Antidotes With Cholinergic Systemsefrahmaa watiPas encore d'évaluation
- Immunomodulators: Arthur Kavanaugh and David H BroideDocument14 pagesImmunomodulators: Arthur Kavanaugh and David H Broidesabin shaikPas encore d'évaluation
- PHARM4515 8 (Antihistamines)Document45 pagesPHARM4515 8 (Antihistamines)Street Pasutri RolferPas encore d'évaluation
- JCE 1986 TLC NitrophenolDocument3 pagesJCE 1986 TLC NitrophenolIsabella KlausPas encore d'évaluation
- Chapter 7 - Drugs Acting On The Respiratory System-Ok1Document66 pagesChapter 7 - Drugs Acting On The Respiratory System-Ok1biqilaadengPas encore d'évaluation
- Classical Vs Reverse Pharmacology in Drug DiscoveryDocument4 pagesClassical Vs Reverse Pharmacology in Drug DiscoveryGourisankar Roul100% (1)
- Asthma 2Document14 pagesAsthma 2Salman KhanPas encore d'évaluation
- Melovinone, An Open Chain Analogue of Melochinone FromDocument2 pagesMelovinone, An Open Chain Analogue of Melochinone FromwindahPas encore d'évaluation
- FF - MC LECTURE PPT 7Document46 pagesFF - MC LECTURE PPT 7Nur Kamilah IdzanPas encore d'évaluation
- Tugas Michelle 2Document7 pagesTugas Michelle 2andre nicholasPas encore d'évaluation
- Hist AntihisDocument20 pagesHist AntihisSusanti AsmiPas encore d'évaluation
- AntidepressantDocument49 pagesAntidepressantjjjiii394Pas encore d'évaluation
- Adenosine 5 Monophosphate Increases Levels of Leukotriene - 2004 - RespiratoryDocument5 pagesAdenosine 5 Monophosphate Increases Levels of Leukotriene - 2004 - RespiratoryIon CorbuPas encore d'évaluation
- Sahoo 2020Document31 pagesSahoo 2020quanleminh1203Pas encore d'évaluation
- Chapter - IDocument22 pagesChapter - IVINOTH RAJPas encore d'évaluation
- Autonomic ReceptorsDocument7 pagesAutonomic ReceptorsMia MusPas encore d'évaluation
- Darvesh 2008Document13 pagesDarvesh 2008Desye MelesePas encore d'évaluation
- 8 KoahDocument33 pages8 KoahLyrics LinePas encore d'évaluation
- 1950 - Edsall Et Al. - Light Scattering in Solutions of Serum Albumin Effects of Charge and IonicDocument16 pages1950 - Edsall Et Al. - Light Scattering in Solutions of Serum Albumin Effects of Charge and IonicNayara CarvalhoPas encore d'évaluation
- Ic50 Piperin PDFDocument7 pagesIc50 Piperin PDFDesi PermatasariPas encore d'évaluation
- Intro To Pharmacology Study GuideDocument93 pagesIntro To Pharmacology Study GuideMichelle Morgan LongstrethPas encore d'évaluation
- Salbutamol: 3-Adrenoceptive: A New, Selective Receptor StimulantDocument11 pagesSalbutamol: 3-Adrenoceptive: A New, Selective Receptor StimulantPablo Maldonado MuñozPas encore d'évaluation
- Bioorganic & Medicinal Chemistry Letters: A A B C A D e B ADocument30 pagesBioorganic & Medicinal Chemistry Letters: A A B C A D e B ABi LouPas encore d'évaluation
- Clinical Pharmacology of Bronchodilator MedicationsDocument22 pagesClinical Pharmacology of Bronchodilator MedicationsGal ChrisPas encore d'évaluation
- Butyrylcholinesterase: Degradation of AcetylcholineDocument6 pagesButyrylcholinesterase: Degradation of AcetylcholineLee-Ya AchmadPas encore d'évaluation
- Parasympathomimetics and ParasympatholyticsDocument16 pagesParasympathomimetics and ParasympatholyticsSalona Roy100% (4)
- Bioorganic & Medicinal ChemistryDocument7 pagesBioorganic & Medicinal ChemistryRodrigo Sebastian Arancibia GonzalezPas encore d'évaluation
- Organophosphate and Carbamate Poisoning: Review of The Current Literature and Summary of Clinical and Laboratory Experience in Southern IsraelDocument4 pagesOrganophosphate and Carbamate Poisoning: Review of The Current Literature and Summary of Clinical and Laboratory Experience in Southern IsraelIstigfarani InPas encore d'évaluation
- Drug Design: Drug Structure & Pharmacological ActivityDocument55 pagesDrug Design: Drug Structure & Pharmacological ActivityMominul IslamPas encore d'évaluation
- Antiulcer Proton Pump Inhibitor: Dr. Mai Ramadan Pharm Chem 4Document42 pagesAntiulcer Proton Pump Inhibitor: Dr. Mai Ramadan Pharm Chem 4Ahmed FouadPas encore d'évaluation
- ANFETAMINASDocument10 pagesANFETAMINASIza ÁlvarezPas encore d'évaluation
- Pha051 Las#7 RationaleDocument26 pagesPha051 Las#7 RationaleMonique EamiguelPas encore d'évaluation
- Catholic University of Health and ALLIED Email: Vc@bugando - Ac.tz Call Us: +255 (0) 28 250 0881 SCIENCEDocument2 pagesCatholic University of Health and ALLIED Email: Vc@bugando - Ac.tz Call Us: +255 (0) 28 250 0881 SCIENCEambrocePas encore d'évaluation
- SpectrumDocument1 pageSpectrumYash ShindePas encore d'évaluation
- Kinetics and Mechanism of N-Boc Cleavage: Evidence of A Second-Order Dependence Upon Acid ConcentrationDocument9 pagesKinetics and Mechanism of N-Boc Cleavage: Evidence of A Second-Order Dependence Upon Acid ConcentrationDiogo DiasPas encore d'évaluation
- Allergy - October 1980 - NornDocument9 pagesAllergy - October 1980 - NornGloria Stefani TeniwutPas encore d'évaluation
- Tolperisone A Typical Representative of A Class of Centrally CNS Neur...Document13 pagesTolperisone A Typical Representative of A Class of Centrally CNS Neur...Daniel RuizPas encore d'évaluation
- Adrenergic AgentsDocument7 pagesAdrenergic AgentsMuhamed ArsalanPas encore d'évaluation
- Etoricoxib - Martindale 39thDocument2 pagesEtoricoxib - Martindale 39thCachimbo PrintPas encore d'évaluation
- Cholinergics Part-IIIDocument35 pagesCholinergics Part-IIIYaman Adnan QabajaPas encore d'évaluation
- Siddharth PPT CholinergicDocument34 pagesSiddharth PPT CholinergicSiddharth Shekhar SinghPas encore d'évaluation
- Drug Action Therapeutic UsesDocument4 pagesDrug Action Therapeutic Usesstanley ogwotuPas encore d'évaluation
- Jurnal 1Document6 pagesJurnal 1KurniasaryRerungAlloPas encore d'évaluation
- Preview Farmako Katzung 3Document35 pagesPreview Farmako Katzung 3gunubgpePas encore d'évaluation
- Pharmacology of The Respiratory SystemDocument39 pagesPharmacology of The Respiratory Systemaleah morenoPas encore d'évaluation
- Aromatic CompoundsDocument16 pagesAromatic CompoundsJotillnaimPas encore d'évaluation
- Central Nervous System StimulantsDocument10 pagesCentral Nervous System StimulantsCristian F ApontePas encore d'évaluation
- Sussman 1992acetylcholinesterase Structure and Use As A Model For SPECIFIC CATIO PROTEIN INTERACTIONDocument9 pagesSussman 1992acetylcholinesterase Structure and Use As A Model For SPECIFIC CATIO PROTEIN INTERACTIONKirianova GodoyPas encore d'évaluation
- Sintesis Total de TienamicinaDocument6 pagesSintesis Total de Tienamicinajesdux09Pas encore d'évaluation
- Journal of Medicinal Chemistry, 1979, Vol. 22, No. 10Document2 pagesJournal of Medicinal Chemistry, 1979, Vol. 22, No. 10Slapdragonx100% (1)
- Yapp 2011Document7 pagesYapp 2011dana40018256Pas encore d'évaluation
- Bremer 2017Document11 pagesBremer 2017Walid Ebid ElgammalPas encore d'évaluation
- VMUF 5 Autonomic Nervous System DrugsDocument21 pagesVMUF 5 Autonomic Nervous System DrugsSharlene MacaraegPas encore d'évaluation
- 6 Gen Anasthetics 03-08-2023Document20 pages6 Gen Anasthetics 03-08-2023ashwin kPas encore d'évaluation
- Subject: Pharmacology Topic: ANS 2 Lecturer: Maria Luisa D. Delacruz, M.D. Date of Lecture:August 3, 2011 Transcriptionist: Anonymous Pages: 16Document16 pagesSubject: Pharmacology Topic: ANS 2 Lecturer: Maria Luisa D. Delacruz, M.D. Date of Lecture:August 3, 2011 Transcriptionist: Anonymous Pages: 16dtimtimanPas encore d'évaluation
- Adipic Acid SynthesisDocument2 pagesAdipic Acid SynthesisPhạm Thành Lý100% (1)
- 1 - Introduction To Medicinal ChemistryDocument19 pages1 - Introduction To Medicinal ChemistryPhạm Thành LýPas encore d'évaluation
- Hydrolysis Lab 2006Document7 pagesHydrolysis Lab 2006Phạm Thành LýPas encore d'évaluation
- Brief Summary Spring 2015 UpdatedDocument2 pagesBrief Summary Spring 2015 UpdatedPhạm Thành LýPas encore d'évaluation
- This Week Sample Test QUESTION 1. Determine A, B, C Structure in Following Reaction SequencesDocument3 pagesThis Week Sample Test QUESTION 1. Determine A, B, C Structure in Following Reaction SequencesPhạm Thành LýPas encore d'évaluation
- HC Number Bin: Column1Document2 pagesHC Number Bin: Column1Phạm Thành LýPas encore d'évaluation
- I. 1. 5 2. No AnswersDocument2 pagesI. 1. 5 2. No AnswersPhạm Thành LýPas encore d'évaluation
- Evolutionary Analyses of The Human Genome: AnalysisDocument3 pagesEvolutionary Analyses of The Human Genome: AnalysisPhạm Thành LýPas encore d'évaluation
- 10 09 2014 Work ScheduleDocument10 pages10 09 2014 Work SchedulePhạm Thành LýPas encore d'évaluation
- Perspecti VES: Sheets, Ribbons and Tubules - How Organelles Get Their ShapeDocument13 pagesPerspecti VES: Sheets, Ribbons and Tubules - How Organelles Get Their ShapePhạm Thành LýPas encore d'évaluation
- Clinic: Klinikos Is Sloping or Reclining and Latin Is ClinicusDocument3 pagesClinic: Klinikos Is Sloping or Reclining and Latin Is Clinicusfl004Pas encore d'évaluation
- Parts of The Body and Health ProblemDocument13 pagesParts of The Body and Health ProblemSonia Tri AgustinaPas encore d'évaluation
- 1.halliwck Child Principios - Halliwick - en - Nino PDFDocument7 pages1.halliwck Child Principios - Halliwick - en - Nino PDFmuhammad yaminPas encore d'évaluation
- PolygraDocument15 pagesPolygraAbdul Aziz Akil RiasPas encore d'évaluation
- Biopotential Amplifiers 2Document52 pagesBiopotential Amplifiers 2Jesus Peña100% (1)
- Critical Care Medicine An Algorithmic Approach 2023Document335 pagesCritical Care Medicine An Algorithmic Approach 2023Ahmed AbusalabPas encore d'évaluation
- Title: Artificial Intelligence in Healthcare An Integrated Approach To Healthcare DeliveryDocument13 pagesTitle: Artificial Intelligence in Healthcare An Integrated Approach To Healthcare DeliveryofhsaosdafsdfPas encore d'évaluation
- Invuity Investor Presentation - Q3 2017Document22 pagesInvuity Investor Presentation - Q3 2017medtechyPas encore d'évaluation
- 5z23. ED Crowding Overview and Toolkit (Dec 2015)Document33 pages5z23. ED Crowding Overview and Toolkit (Dec 2015)Peter 'Pierre' RobsonPas encore d'évaluation
- Gestational Trophoblastic Neoplasia: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Document45 pagesGestational Trophoblastic Neoplasia: NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines)Roshni SethiaPas encore d'évaluation
- Mhn-Issues, Trends, Magnitude, Contemporary Practice HealthDocument15 pagesMhn-Issues, Trends, Magnitude, Contemporary Practice HealthAna MikaPas encore d'évaluation
- Laporan Divisi Nefrologi 3 Maret 2020Document18 pagesLaporan Divisi Nefrologi 3 Maret 2020annisanangPas encore d'évaluation
- CE Strengths Based Nursing.24Document9 pagesCE Strengths Based Nursing.24THOHAROHPas encore d'évaluation
- Guru AppointmentDocument2 pagesGuru AppointmentKirankumar MutnaliPas encore d'évaluation
- Unite - October 2013Document40 pagesUnite - October 2013Bruce SeamanPas encore d'évaluation
- 2016 - Lancet StrokeDocument14 pages2016 - Lancet StrokeWikler Bernal TorresPas encore d'évaluation
- Read and Choose The Correct Answer From The Box Below.: Boys GirlsDocument1 pageRead and Choose The Correct Answer From The Box Below.: Boys GirlsjekjekPas encore d'évaluation
- Wmh-Cidi Papi Interview: Screening Section (SC)Document9 pagesWmh-Cidi Papi Interview: Screening Section (SC)Monia AzevedoPas encore d'évaluation
- Disease Impact 2Document31 pagesDisease Impact 2Seed Rock ZooPas encore d'évaluation
- Consequences of Traumatic Stress - Diac SabinaDocument6 pagesConsequences of Traumatic Stress - Diac SabinaSabina DiacPas encore d'évaluation
- Pediatric Unfolding Case StudyDocument4 pagesPediatric Unfolding Case StudyJessica100% (1)
- Recovery Road (Excerpt)Document13 pagesRecovery Road (Excerpt)I Read YA100% (1)
- AIDS in The Workplace LawDocument30 pagesAIDS in The Workplace LawPacific SpectrumPas encore d'évaluation
- Methanol Poisoning OverviewDocument5 pagesMethanol Poisoning OverviewDya AndryanPas encore d'évaluation
- 1999 CQfirstphaseallotments PDFDocument73 pages1999 CQfirstphaseallotments PDFISMAIL KHANPas encore d'évaluation
- Acute and Chronic CholecystitisDocument10 pagesAcute and Chronic Cholecystitisissam_1994Pas encore d'évaluation
- Medical Laboratory Technology Journal: Potensi Antifungi Tangkai Daun Jarak Pagar Terhadap PERTUMBUHAN Candida AlbicansDocument5 pagesMedical Laboratory Technology Journal: Potensi Antifungi Tangkai Daun Jarak Pagar Terhadap PERTUMBUHAN Candida Albicanskhoko holicPas encore d'évaluation
- Draf Resume Askep PpniDocument4 pagesDraf Resume Askep PpniAbu QisronPas encore d'évaluation
- Acticide Bac 50 M MSDS PDFDocument10 pagesActicide Bac 50 M MSDS PDFmePas encore d'évaluation
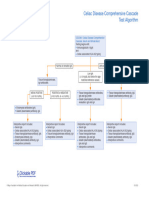
- Celiac Disease Comprehensive Cascade Test AlgorithmDocument1 pageCeliac Disease Comprehensive Cascade Test Algorithmayub7walkerPas encore d'évaluation