Académique Documents
Professionnel Documents
Culture Documents
United States Health Care Reform Progress To Date and Next Steps
Transféré par
Josh ShaevitzTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
United States Health Care Reform Progress To Date and Next Steps
Transféré par
Josh ShaevitzDroits d'auteur :
Formats disponibles
Clinical Review & Education
Special Communication
United States Health Care Reform
Progress to Date and Next Steps
Barack Obama, JD
Editorials
IMPORTANCE The Affordable Care Act is the most important health care legislation enacted in
the United States since the creation of Medicare and Medicaid in 1965. The law implemented
comprehensive reforms designed to improve the accessibility, affordability, and quality of
health care.
OBJECTIVES To review the factors influencing the decision to pursue health reform,
summarize evidence on the effects of the law to date, recommend actions that could
improve the health care system, and identify general lessons for public policy
from the Affordable Care Act.
EVIDENCE Analysis of publicly available data, data obtained from government agencies,
and published research findings. The period examined extends from 1963 to early 2016.
FINDINGS The Affordable Care Act has made significant progress toward solving
long-standing challenges facing the US health care system related to access, affordability,
and quality of care. Since the Affordable Care Act became law, the uninsured rate has
declined by 43%, from 16.0% in 2010 to 9.1% in 2015, primarily because of the laws reforms.
Research has documented accompanying improvements in access to care (for example, an
estimated reduction in the share of nonelderly adults unable to afford care of 5.5 percentage
points), financial security (for example, an estimated reduction in debts sent to collection of
$600-$1000 per person gaining Medicaid coverage), and health (for example, an estimated
reduction in the share of nonelderly adults reporting fair or poor health of 3.4 percentage
points). The law has also begun the process of transforming health care payment systems,
with an estimated 30% of traditional Medicare payments now flowing through alternative
payment models like bundled payments or accountable care organizations. These and related
reforms have contributed to a sustained period of slow growth in per-enrollee health care
spending and improvements in health care quality. Despite this progress, major opportunities
to improve the health care system remain.
CONCLUSIONS AND RELEVANCE Policy makers should build on progress made by the
Affordable Care Act by continuing to implement the Health Insurance Marketplaces
and delivery system reform, increasing federal financial assistance for Marketplace enrollees,
introducing a public plan option in areas lacking individual market competition, and taking
actions to reduce prescription drug costs. Although partisanship and special interest
opposition remain, experience with the Affordable Care Act demonstrates that positive
change is achievable on some of the nations most complex challenges.
Author Affiliation: President of the
United States, Washington, DC.
Corresponding Author: Barack
Obama, JD, The White House,
1600 Pennsylvania Ave NW,
JAMA. doi:10.1001/jama.2016.9797 Washington, DC 20500
Published online July 11, 2016. (press@who.eop.gov).
(Reprinted) E1
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ on 07/11/2016
Clinical Review & Education Special Communication US Health Care Reform: Progress and Next Steps
H
ealth care costs affect the economy, the federal budget,
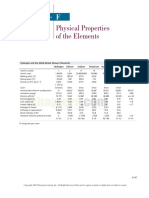
Figure 1. Percentage of Individuals in the United States Without
and virtually every American familys financial well- Health Insurance, 1963-2015
being. Health insurance enables children to excel at school,
adults to work more productively, and Americans of all ages to live Creation of Year before main ACA
Medicare and coverage provisions
longer, healthier lives. When I took office, health care costs had risen Medicaid took effect
25
rapidly for decades, and tens of millions of Americans were unin-
sured. Regardless of the political difficulties, I concluded compre-
hensive reform was necessary. 20
Uninsured Population, %
The result of that effort, the Affordable Care Act (ACA), has made
substantial progress in addressing these challenges. Americans can 15
now count on access to health coverage throughout their lives, and
the federal government has an array of tools to bring the rise of health 10
care costs under control. However, the work toward a high-quality,
affordable, accessible health care system is not over. 5
In this Special Communication, I assess the progress the ACA has
made toward improving the US health care system and discuss how 0
policy makers can build on that progress in the years ahead. I close 1960 1965 1970 1975 1980 1985 1990 1995 2000 2005 2010 2015
with reflections on what my administrations experience with the ACA Year
can teach about the potential for positive change in health policy in
Data are derived from the National Health Interview Survey and, for years prior
particular and public policy generally. to 1982, supplementary information from other survey sources and
administrative records. The methods used to construct a comparable series
spanning the entire period build on those in Cohen et al8 and Cohen9 and are
described in detail in Council of Economic Advisers 2014.10 For years 1989 and
Impetus for Health Reform later, data are annual. For prior years, data are generally but not always
biannual. ACA indicates Affordable Care Act.
In my first days in office, I confronted an array of immediate chal-
lenges associated with the Great Recession. I also had to deal with
one of the nations most intractable and long-standing problems, a
health care system that fell far short of its potential. In 2008, the rary support to sustain Medicaid coverage as well as investments in
United States devoted 16% of the economy to health care, an in- health information technology, prevention, and health research to
crease of almost one-quarter since 1998 (when 13% of the economy improve the system in the long run. In the summer of 2009, I signed
was spent on health care), yet much of that spending did not trans- the Tobacco Control Act, which has contributed to a rapid decline
late into better outcomes for patients.1-4 The health care system also in the rate of smoking among teens, from 19.5% in 2009 to 10.8%
fell short on quality of care, too often failing to keep patients safe, in 2015, with substantial declines among adults as well.7,18
waiting to treat patients when they were sick rather than focusing Beyond these initial actions, I decided to prioritize comprehen-
on keeping them healthy, and delivering fragmented, poorly coor- sive health reform not only because of the gravity of these chal-
dinated care.5,6 lenges but also because of the possibility for progress. Massachusetts
Moreover, the US system left more than 1 in 7 Americans with- had recently implemented bipartisan legislation to expand health
out health insurance coverage in 2008.7 Despite successful efforts insurance coverage to all its residents. Leaders in Congress had rec-
in the 1980s and 1990s to expand coverage for specific popula- ognized that expanding coverage, reducing the level and growth of
tions, like children, the United States had not seen a large, sus- health care costs, and improving quality was an urgent national pri-
tained reduction in the uninsured rate since Medicare and Medic- ority. At the same time, a broad array of health care organizations
aid began (Figure 18-10). The United States high uninsured rate had and professionals, business leaders, consumer groups, and others
negative consequences for uninsured Americans, who experi- agreed that the time had come to press ahead with reform.19 Those
enced greater financial insecurity, barriers to care, and odds of poor elements contributed to my decision, along with my deeply held be-
health and preventable death; for the health care system, which was lief that health care is not a privilege for a few, but a right for all. Af-
burdened with billions of dollars in uncompensated care; and for the ter a long debate with well-documented twists and turns, I signed
US economy, which suffered, for example, because workers were the ACA on March 23, 2010.
concerned about joining the ranks of the uninsured if they sought
additional education or started a business.11-16 Beyond these statis-
tics were the countless, heartbreaking stories of Americans who
Progress Under the ACA
struggled to access care because of a broken health insurance sys-
tem. These included people like Natoma Canfield, who had over- The years following the ACAs passage included intense implemen-
come cancer once but had to discontinue her coverage due to rap- tation efforts, changes in direction because of actions in Congress
idly escalating premiums and found herself facing a new cancer and the courts, and new opportunities such as the bipartisan pas-
diagnosis uninsured.17 sage of the Medicare Access and CHIP Reauthorization Act (MACRA)
In 2009, during my first month in office, I extended the Chil- in 2015. Rather than detail every development in the intervening
drens Health Insurance Program and soon thereafter signed the years, I provide an overall assessment of how the health care sys-
American Recovery and Reinvestment Act, which included tempo- tem has changed between the ACAs passage and today.
E2 JAMA Published online July 11, 2016 (Reprinted) jama.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ on 07/11/2016
US Health Care Reform: Progress and Next Steps Special Communication Clinical Review & Education
The evidence underlying this assessment was obtained from sev-
Figure 2. Decline in Adult Uninsured Rate From 2013 to 2015 vs 2013
eral sources. To assess trends in insurance coverage, this analysis re- Uninsured Rate by State
lies on publicly available government and private survey data, as well
as previously published analyses of survey and administrative data. 15
To assess trends in health care costs and quality, this analysis relies
Percentage Point Decline in Adult
on publicly available government estimates and projections of health 12
Uninsured Rate, 2013-2015
care spending; publicly available government and private survey
data; data on hospital readmission rates provided by the Centers for 9
Medicaid expansion states
Medicare & Medicaid Services; and previously published analyses
of survey, administrative, and clinical data. The dates of the data used 6
in this assessment range from 1963 to early 2016.
3
Expanding and Improving Coverage
Medicaid nonexpansion states
The ACA has succeeded in sharply increasing insurance coverage.
0
Since the ACA became law, the uninsured rate has declined by 43%, 0 5 10 15 20 25 30
from 16.0% in 2010 to 9.1% in 2015,7 with most of that decline oc- Adult Uninsured Rate in 2013, %
curring after the laws main coverage provisions took effect in 2014
Data are derived from the Gallup-Healthways Well-Being Index as reported by
(Figure 18-10). The number of uninsured individuals in the United
Witters23 and reflect uninsured rates for individuals 18 years or older. Dashed
States has declined from 49 million in 2010 to 29 million in 2015. lines reflect the result of an ordinary least squares regression relating the
This is by far the largest decline in the uninsured rate since the cre- change in the uninsured rate from 2013 to 2015 to the level of the uninsured
ation of Medicare and Medicaid 5 decades ago. Recent analyses have rate in 2013, run separately for each group of states. The 29 states in which
expanded coverage took effect before the end of 2015 were categorized as
concluded these gains are primarily because of the ACA, rather than Medicaid expansion states, and the remaining 21 states were categorized as
other factors such as the ongoing economic recovery.20,21 Adjust- Medicaid nonexpansion states.
ing for economic and demographic changes and other underlying
trends, the Department of Health and Human Services estimated
that 20 million more people had health insurance in early 2016 be- in every month since the ACA became law, and rigorous compari-
cause of the law.22 sons of Medicaid expansion and nonexpansion states show no nega-
Each of the laws major coverage provisionscomprehensive re- tive effects on employment in expansion states.28-30
forms in the health insurance market combined with financial assis- The law has also greatly improved health insurance coverage for
tance for low- and moderate-income individuals to purchase cover- people who already had it. Coverage offered on the individual mar-
age, generous federal support for states that expand their Medicaid ket or to small businesses must now include a core set of health care
programs to cover more low-income adults, and improvements in ex- services, including maternity care and treatment for mental health
isting insurance coveragehas contributed to these gains. States that and substance use disorders, services that were sometimes not cov-
decided to expand their Medicaid programs saw larger reductions in ered at all previously.31 Most private insurance plans must now cover
their uninsured rates from 2013 to 2015, especially when those states recommended preventive services without cost-sharing, an impor-
had large uninsured populations to start with (Figure 223). However, tant step in light of evidence demonstrating that many preventive
even states that have not adopted Medicaid expansion have seen sub- services were underused.5,6 This includes womens preventive ser-
stantial reductions in their uninsured rates, indicating that the ACAs vices, which has guaranteed an estimated 55.6 million women cov-
other reforms are increasing insurance coverage. The laws provision erage of services such as contraceptive coverage and screening and
allowing young adults to stay on a parents plan until age 26 years has counseling for domestic and interpersonal violence.32 In addition,
also played a contributing role, covering an estimated 2.3 million families now have far better protection against catastrophic costs
people after it took effect in late 2010.22 related to health care. Lifetime limits on coverage are now illegal and
Early evidence indicates that expanded coverage is improving annual limits typically are as well. Instead, most plans must cap en-
access to treatment, financial security, and health for the newly in- rollees annual out-of-pocket spending, a provision that has helped
sured. Following the expansion through early 2015, nonelderly adults substantially reduce the share of people with employer-provided cov-
experienced substantial improvements in the share of individuals erage lacking real protection against catastrophic costs (Figure 333).
who have a personal physician (increase of 3.5 percentage points) The law is also phasing out the Medicare Part D coverage gap. Since
and easy access to medicine (increase of 2.4 percentage points) and 2010, more than 10 million Medicare beneficiaries have saved more
substantial decreases in the share who are unable to afford care than $20 billion as a result.34
(decrease of 5.5 percentage points) and reporting fair or poor health
(decrease of 3.4 percentage points) relative to the pre-ACA trend.24 Reforming the Health Care Delivery System
Similarly, research has found that Medicaid expansion improves the Before the ACA, the health care system was dominated by fee-for-
financial security of the newly insured (for example, by reducing the service payment systems, which often penalized health care orga-
amount of debt sent to a collection agency by an estimated $600- nizations and health care professionals who find ways to deliver care
$1000 per person gaining Medicaid coverage).26,27 Greater insur- more efficiently, while failing to reward those who improve the qual-
ance coverage appears to have been achieved without negative ef- ity of care. The ACA has changed the health care payment system
fects on the labor market, despite widespread predictions that the in several important ways. The law modified rates paid to many that
law would be a job killer. Private-sector employment has increased provide Medicare services and Medicare Advantage plans to better
jama.com (Reprinted) JAMA Published online July 11, 2016 E3
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ on 07/11/2016
Clinical Review & Education Special Communication US Health Care Reform: Progress and Next Steps
Figure 3. Percentage of Workers With Employer-Based Single Coverage Figure 4. Rate of Change in Real per-Enrollee Spending by Payer
Without an Annual Limit on Out-of-pocket Spending
7
Private insurance
Affordable Care Year before out-of-pocket
6
Mean Annual Percentage Change in
Act enacted limit requirement took effect
Spending, Adjusted for Inflation
30
5
Enrolled Workers Without an Annual Limit, %
Medicare
4
25
3
20
2
1 Medicaid
15
0
10
1
2
5 2000-2005 2005-2010 2010-2014
Time Period
0
2006 2007 2008 2009 2010 2011 2012 2013 2014 2015
Data are derived from the National Health Expenditure Accounts.1 Inflation
Year
adjustments use the Gross Domestic Product Price Index reported in the
National Income and Product Accounts.40 The mean growth rate for Medicare
Data from the Kaiser Family Foundation/Health Research and Education Trust spending reported for 2005 through 2010 omits growth from 2005 to 2006 to
Employer Health Benefits Survey.33 exclude the effect of the creation of Medicare Part D.
align them with the actual costs of providing care. Research on how
past changes in Medicare payment rates have affected private pay- 2006 is omitted to avoid including the rapid growth associated with
ment rates implies that these changes in Medicare payment policy the creation of Medicare Part D).1,40 Similarly, mean real per-
are helping decrease prices in the private sector as well.35,36 The ACA enrollee growth in private insurance spending has been 1.1% per year
also included numerous policies to detect and prevent health care since 2010, compared with a mean of 6.5% from 2000 through
fraud, including increased scrutiny prior to enrollment in Medicare 2005 and 3.4% from 2005 to 2010.1,40
and Medicaid for health care entities that pose a high risk of fraud, As a result, health care spending is likely to be far lower than ex-
stronger penalties for crimes involving losses in excess of $1 mil- pected. For example, relative to the projections the Congressional
lion, and additional funding for antifraud efforts. The ACA has also Budget Office (CBO) issued just before I took office, CBO now proj-
widely deployed value-based payment systems in Medicare that ects Medicare to spend 20%, or about $160 billion, less in 2019
tie fee-for-service payments to the quality and efficiency of the care alone.41,42 The implications for families budgets of slower growth
delivered by health care organizations and health care profession- in premiums have been equally striking. Had premiums increased
als. In parallel with these efforts, my administration has worked to since 2010 at the same mean rate as the preceding decade, the mean
foster a more competitive market by increasing transparency around family premium for employer-based coverage would have been al-
the prices charged and the quality of care delivered. most $2600 higher in 2015.33 Employees receive much of those sav-
Most importantly over the long run, the ACA is moving the health ings through lower premium costs, and economists generally agree
care system toward alternative payment models that hold health that those employees will receive the remainder as higher wages in
care entities accountable for outcomes. These models include the long run.43 Furthermore, while deductibles have increased in re-
bundled payment models that make a single payment for all of the cent years, they have increased no faster than in the years preced-
services provided during a clinical episode and population-based ing 2010.44 Multiple sources also indicate that the overall share of
models like accountable care organizations (ACOs) that base pay- health care costs that enrollees in employer coverage pay out of
ment on the results health care organizations and health care pro- pocket has been close to flat since 2010 (Figure 545-48), most likely
fessionals achieve for all of their patients care. The law created the because the continued increase in deductibles has been canceled
Center for Medicare and Medicaid Innovation (CMMI) to test alter- out by a decline in co-payments.
native payment models and bring them to scale if they are success- At the same time, the United States has seen important im-
ful, as well as a permanent ACO program in Medicare. Today, an es- provements in the quality of care. The rate of hospital-acquired con-
timated 30% of traditional Medicare payments flow through ditions (such as adverse drug events, infections, and pressure ul-
alternative payment models that broaden the focus of payment be- cers) has declined by 17%, from 145 per 1000 discharges in 2010 to
yond individual services or a particular entity, up from essentially 121 per 1000 discharges in 2014.49 Using prior research on the re-
none in 2010.37 These models are also spreading rapidly in the pri- lationship between hospital-acquired conditions and mortality, the
vate sector, and their spread will likely be accelerated by the physi- Agency for Healthcare Research and Quality has estimated that this
cian payment reforms in MACRA.38,39 decline in the rate of hospital-acquired conditions has prevented a
Trends in health care costs and quality under the ACA have been cumulative 87 000 deaths over 4 years.49 The rate at which Medi-
promising (Figure 41,40). From 2010 through 2014, mean annual care patients are readmitted to the hospital within 30 days after dis-
growth in real per-enrollee Medicare spending has actually been charge has also decreased sharply, from a mean of 19.1% during 2010
negative, down from a mean of 4.7% per year from 2000 through to a mean of 17.8% during 2015 (Figure 6; written communication;
2005 and 2.4% per year from 2006 to 2010 (growth from 2005 to March 2016; Office of Enterprise Data and Analytics, Centers for
E4 JAMA Published online July 11, 2016 (Reprinted) jama.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ on 07/11/2016
US Health Care Reform: Progress and Next Steps Special Communication Clinical Review & Education
Figure 5. Out-of-pocket Spending as a Percentage of Total Health Care Figure 6. Medicare 30-Day, All-Condition Hospital Readmission Rate
Spending for Individuals Enrolled in Employer-Based Coverage
19.5
Patients Readmitted Within 30 Days, %
25
Out-of-pocket Spending as a Percentage
(12-Month Moving Average)
Medical Expenditure Panel Survey 19.0
20
of Total Spending
Health Care Cost Institute
15 18.5
Claxton et al
10
18.0
5
17.5
2008 2009 2010 2011 2012 2013 2014 2015 2016
0
2000 2002 2004 2006 2008 2010 2012 2014 Year
Year
Data were provided by the Centers for Medicare & Medicaid Services (written
Data for the series labeled Medical Expenditure Panel Survey (MEPS) were communication; March 2016). The plotted series reflects a 12-month moving
derived from MEPS Household Component and reflect the ratio of average of the hospital readmission rates reported for discharges occurring in
out-of-pocket expenditures to total expenditures for nonelderly individuals each month.
reporting full-year employer coverage. Data for the series labeled Health Care
Cost Institute (HCCI) were derived from the analysis of the HCCI claims
database reported in Herrera et al,45 HCCI 2015,46 and HCCI 201547; to capture
of unfinished business is in Medicaid. As of July 1, 2016, 19 states have
data revisions, the most recent value reported for each year was used. Data for
the series labeled Claxton et al were derived from the analyses of the Trueven yet to expand their Medicaid programs. I hope that all 50 states take
Marketscan claims database reported by Claxton et al 2016.48 this option and expand coverage for their citizens in the coming years,
as they did in the years following the creation of Medicaid and CHIP.
Medicare & Medicaid Services). The Department of Health and Hu- With respect to delivery system reform, the reorientation of the
man Services has estimated that lower hospital readmission rates US health care payment systems toward quality and accountability
resulted in 565 000 fewer total readmissions from April 2010 has made significant strides forward, but it will take continued hard
through May 2015.50,51 work to achieve my administrations goal of having at least half of
While the Great Recession and other factors played a role in re- traditional Medicare payments flowing through alternative pay-
cent trends, the Council of Economic Advisers has found evidence ment models by the end of 2018. Tools created by the ACA
that the reforms introduced by the ACA helped both slow health care including CMMI and the laws ACO programand the new tools pro-
cost growth and drive improvements in the quality of care.44,52 The vided by MACRA will play central roles in this important work. In
contribution of the ACAs reforms is likely to increase in the years parallel, I expect continued bipartisan support for identifying the root
ahead as its tools are used more fully and as the models already de- causes and cures for diseases through the Precision Medicine and
ployed under the ACA continue to mature. BRAIN initiatives and the Cancer Moonshot, which are likely to have
profound benefits for the 21st-century US health care system and
health outcomes.
Second, while the ACA has greatly improved the affordability
Building on Progress to Date
of health insurance coverage, surveys indicate that many of the re-
I am proud of the policy changes in the ACA and the progress that maining uninsured individuals want coverage but still report being
has been made toward a more affordable, high-quality, and acces- unable to afford it.53,54 Some of these individuals may be unaware
sible health care system. Despite this progress, too many Ameri- of the financial assistance available under current law, whereas oth-
cans still strain to pay for their physician visits and prescriptions, cover ers would benefit from congressional action to increase financial as-
their deductibles, or pay their monthly insurance bills; struggle to sistance to purchase coverage, which would also help middle-class
navigate a complex, sometimes bewildering system; and remain un- families who have coverage but still struggle with premiums. The
insured. More work to reform the health care system is necessary, steady-state cost of the ACAs coverage provisions is currently pro-
with some suggestions offered below. jected to be 28% below CBOs original projections, due in signifi-
First, many of the reforms introduced in recent years are still cant part to lower-than-expected Marketplace premiums, so in-
some years from reaching their maximum effect. With respect to the creased financial assistance could make coverage even more
laws coverage provisions, these early years experience demon- affordable while still keeping federal costs below initial estimates.55,56
strate that the Health Insurance Marketplace is a viable source of cov- Third, more can and should be done to enhance competition in
erage for millions of Americans and will be for decades to come. How- the Marketplaces. For most Americans in most places, the Market-
ever, both insurers and policy makers are still learning about the places are working. The ACA supports competition and has encour-
dynamics of an insurance market that includes all people regard- aged the entry of hospital-based plans, Medicaid managed care plans,
less of any preexisting conditions, and further adjustments and re- and other plans into new areas. As a result, the majority of the coun-
calibrations will likely be needed, as can be seen in some insurers try has benefited from competition in the Marketplaces, with 88%
proposed Marketplace premiums for 2017. In addition, a critical piece of enrollees living in counties with at least 3 issuers in 2016, which helps
jama.com (Reprinted) JAMA Published online July 11, 2016 E5
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ on 07/11/2016
Clinical Review & Education Special Communication US Health Care Reform: Progress and Next Steps
keep costs in these areas low.57,58 However, the remaining 12% of en- in Massachusetts in 2006 but opposed it in the ACA. They supported
rollees live in areas with only 1 or 2 issuers. Some parts of the country theemployermandateinCaliforniain2007butopposeditintheACA
have struggled with limited insurance market competition for many and then opposed the administrations decision to delay it. Moreover,
years, which is one reason that, in the original debate over health re- through inadequate funding, opposition to routine technical correc-
form, Congress considered and I supported including a Medicare- tions, excessive oversight, and relentless litigation, Republicans under-
like public plan. Public programs like Medicare often deliver care more mined ACA implementation efforts. We could have covered more
cost-effectivelybycurtailingadministrativeoverheadandsecuringbet- ground more quickly with cooperation rather than obstruction. It is not
ter prices from providers.59,60 The public plan did not make it into the obvious that this strategy has paid political dividends for Republicans,
final legislation. Now, based on experience with the ACA, I think but it has clearly come at a cost for the country, most notably for the
Congress should revisit a public plan to compete alongside private in- estimated 4 million Americans left uninsured because they live in
surers in areas of the country where competition is limited. Adding a GOP-led states that have yet to expand Medicaid.65
public plan in such areas would strengthen the Marketplace ap- The second lesson is that special interests pose a continued
proach, giving consumers more affordable options while also creat- obstacle to change. We worked successfully with some health care
ing savings for the federal government.61 organizations and groups, such as major hospital associations, to
Fourth, although the ACA included policies to help address pre- redirect excessive Medicare payments to federal subsidies for the
scription drug costs, like more substantial Medicaid rebates and the uninsured. Yet others, like the pharmaceutical industry, oppose any
creation of a pathway for approval of biosimilar drugs, those costs re- change to drug pricing, no matter how justifiable and modest,
main a concern for Americans, employers, and taxpayers alike because they believe it threatens their profits.66 We need to con-
particularly in light of the 12% increase in prescription drug spending tinue to tackle special interest dollars in politics. But we also need
that occurred in 2014.1 In addition to administrative actions like test- to reinforce the sense of mission in health care that brought us an
ing new ways to pay for drugs, legislative action is needed.62 affordable polio vaccine and widely available penicillin.
Congress should act on proposals like those included in my fiscal year The third lesson is the importance of pragmatism in both legis-
2017 budget to increase transparency around manufacturers actual lation and implementation. Simpler approaches to addressing our
production and development costs, to increase the rebates manu- health care problems exist at both ends of the political spectrum: the
facturers are required to pay for drugs prescribed to certain Medi- single-payer model vs government vouchers for all. Yet the nation typi-
care and Medicaid beneficiaries, and to give the federal government cally reaches its greatest heights when we find common ground be-
the authority to negotiate prices for certain high-priced drugs.63 tween the public and private good and adjust along the way. That was
There is another important role for Congress: it should avoid my approach with the ACA. We engaged with Congress to identify the
moving backward on health reform. While I have always been inter- combination of proven health reform ideas that could pass and have
ested in improving the lawand signed 19 bills that do just thatmy continued to adapt them since. This includes abandoning parts that
administration has spent considerable time in the last several years do not work, like the voluntary long-term care program included in
opposing more than 60 attempts to repeal parts or all of the ACA, the law. It also means shutting down and restarting a process when it
time that could have been better spent working to improve our fails. When HealthCare.gov did not work on day 1, we brought in re-
health care system and economy. In some instances, the repeal ef- inforcements, were brutally honest in assessing problems, and worked
forts have been bipartisan, including the effort to roll back the ex- relentlessly to get it operating. Both the process and the website were
cise tax on high-cost employer-provided plans. Although this pro- successful, and we created a playbook we are applying to technol-
vision can be improved, such as through the reforms I proposed in ogy projects across the government.
my budget, the tax creates strong incentives for the least-efficient While the lessons enumerated above may seem daunting, the
private-sector health plans to engage in delivery system reform ef- ACA experience nevertheless makes me optimistic about this coun-
forts, with major benefits for the economy and the budget. It should trys capacity to make meaningful progress on even the biggest pub-
be preserved.64 In addition, Congress should not advance legisla- lic policy challenges. Many moments serve as reminders that a bro-
tion that undermines the Independent Payment Advisory Board, ken status quo is not the nations destiny. I often think of a letter I
which will provide a valuable backstop if rapid cost growth returns received from Brent Brown of Wisconsin. He did not vote for me and
to Medicare. he opposed ObamaCare, but Brent changed his mind when he be-
came ill, needed care, and got it thanks to the law.67 Or take Gover-
nor John Kasichs explanation for expanding Medicaid: For those
that live in the shadows of life, those who are the least among us, I
Lessons for Future Policy Makers
will not accept the fact that the most vulnerable in our state should
While historians will draw their own conclusions about the broader be ignored. We can help them.68 Or look at the actions of count-
implications of the ACA, I have my own. These lessons learned are not less health care providers who have made our health system more
just for posterity: I have put them into practice in both health care coordinated, quality-oriented, and patient-centered. I will repeat
policy and other areas of public policy throughout my presidency. what I said 4 years ago when the Supreme Court upheld the ACA: I
The first lesson is that any change is difficult, but it is especially dif- am as confident as ever that looking back 20 years from now, the
ficultinthefaceofhyperpartisanship.Republicansreversedcourseand nation will be better off because of having the courage to pass this
rejected their own ideas once they appeared in the text of a bill that I law and persevere. As this progress with health care reform in the
supported. For example, they supported a fully funded risk-corridor United States demonstrates, faith in responsibility, belief in oppor-
programandapublicplanfallbackintheMedicaredrugbenefitin2003 tunity, and ability to unite around common values are what makes
but opposed them in the ACA. They supported the individual mandate this nation great.
E6 JAMA Published online July 11, 2016 (Reprinted) jama.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ on 07/11/2016
US Health Care Reform: Progress and Next Steps Special Communication Clinical Review & Education
ARTICLE INFORMATION Statistics. http://www.cdc.gov/nchs/health_policy 23. Witters D. Arkansas, Kentucky set pace in
Published Online: July 11, 2016. /trends_hc_1968_2011.htm. Published November 15, reducing uninsured rate. Gallup. http://www.gallup
doi:10.1001/jama.2016.9797. 2012. Accessed June 14, 2016. .com/poll/189023/arkansas-kentucky-set-pace
10. Council of Economic Advisers. -reducing-uninsured-rate.aspx. Published February
Conflict of Interest Disclosures: The author has 4, 2016. Accessed June 14, 2016.
completed and submitted the ICMJE Form for Methodological appendix: methods used
Disclosure of Potential Conflicts of Interest. to construct a consistent historical time series 24. Sommers BD, Gunja MZ, Finegold K, Musco T.
The authors public financial disclosure report for of health insurance coverage. https://www Changes in self-reported insurance coverage,
calendar year 2015 may be viewed at https://www .whitehouse.gov/sites/default/files/docs access to care, and health under the Affordable
.whitehouse.gov/sites/whitehouse.gov/files /longtermhealthinsuranceseriesmethodologyfinal Care Act. JAMA. 2015;314(4):366-374.
/documents/oge_278_cy_2015_obama_051616.pdf. .pdf. Published December 18, 2014. Accessed June 25. Shartzer A, Long SK, Anderson N. Access to
14, 2016. care and affordability have improved following
Additional Contributions: I thank Matthew Fiedler,
PhD, and Jeanne Lambrew, PhD, who assisted with 11. Baicker K, Taubman SL, Allen HL, et al; Oregon Affordable Care Act implementation; problems
planning, writing, and data analysis. I also thank Health Study Group. The Oregon experiment: remain. Health Aff (Millwood). 2016;35(1):161-168.
Kristie Canegallo, MA; Katie Hill, BA; Cody Keenan, effects of Medicaid on clinical outcomes. N Engl J 26. Dussault N, Pinkovskiy M, Zafar B.
MPP; Jesse Lee, BA; and Shailagh Murray, MS, Med. 2013;368(18):1713-1722. Is health insurance good for your financial
who assisted with editing the manuscript. All of the 12. Sommers BD, Baicker K, Epstein AM. Mortality health? Federal Reserve Bank of New York.
individuals who assisted with the preparation of the and access to care among adults after state http://libertystreeteconomics.newyorkfed.org
manuscript are employed by the Executive Office of Medicaid expansions. N Engl J Med. 2012;367(11): /2016/06/is-health-insurance-good-for-your
the President. 1025-1034. -financial-health.html. Published June 6, 2016.
13. Sommers BD, Long SK, Baicker K. Changes in Accessed June 14, 2016.
REFERENCES mortality after Massachusetts health care reform: 27. Hu L, Kaestner R, Mazumder B, Miller S,
1. Centers for Medicare & Medicaid Services. a quasi-experimental study. Ann Intern Med. 2014; Wong A. The effect of the Patient Protection
National Health Expenditure Data: NHE tables. 160(9):585-593. and Affordable Care Act Medicaid expansions
https://www.cms.gov/Research-Statistics-Data 14. Hadley J, Holahan J, Coughlin T, Miller D. on financial well-being [NBER working paper
-and-Systems/Statistics-Trends-and-Reports Covering the uninsured in 2008: current costs, No. 22170]. National Bureau of Economic Research.
/NationalHealthExpendData sources of payment, and incremental costs. Health http://www.nber.org/papers/w22170. Published
/NationalHealthAccountsHistorical.html. Published Aff (Millwood). 2008;27(5):w399-w415. April 2016. Accessed June 14, 2016.
December 3, 2015. Accessed June 14, 2016. 28. Bureau of Labor Statistics. Employment, hours,
15. Fairlie RW, Kapur K, Gates S. Is employer-based
2. Anderson GF, Frogner BK. Health spending in health insurance a barrier to entrepreneurship? and earnings from the Current Employment
OECD countries: obtaining value per dollar. Health J Health Econ. 2011;30(1):146-162. Statistics survey (national): Series ID
Aff (Millwood). 2008;27(6):1718-1727. CES0500000001. http://data.bls.gov/timeseries
16. Dillender M. Do more health insurance options /CES0500000001. Accessed June 14, 2016.
3. Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, lead to higher wages? evidence from states
Lucas FL, Pinder EL. The implications of regional extending dependent coverage. J Health Econ. 29. Kaestner R, Garrett B, Gangopadhyaya A,
variations in Medicare spending: part 1: the content, 2014;36:84-97. Fleming C. Effects of the ACA Medicaid expansions
quality, and accessibility of care. Ann Intern Med. on health insurance coverage and labor supply
2003;138(4):273-287. 17. Lee J. Im here because of Natoma. The White [NBER working paper No. 21836]. National Bureau
House. https://www.whitehouse.gov/blog/2010/03 of Economic Research. http://www.nber.org/papers
4. Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, /15/im-here-because-natoma-0. Published March
Lucas FL, Pinder EL. The implications of regional /w21836. Published December 2015. Accessed
15, 2010. Accessed June 20, 2016. June 14, 2016.
variations in Medicare spending: part 2: health
outcomes and satisfaction with care. Ann Intern Med. 18. Centers for Disease Control and Prevention. 30. Pinkovskiy M. The Affordable Care Act and the
2003;138(4):288-298. Trends in the prevalence of tobacco use: National labor market: a first look. Federal Reserve Bank of
YRBS: 19912015. http://www.cdc.gov New York Staff Reports No. 746. https://www
5. McGlynn EA, Asch SM, Adams J, et al. /healthyyouth/data/yrbs/pdf/trends/2015_us
The quality of health care delivered to adults .newyorkfed.org/medialibrary/media/research/staff
_tobacco_trend_yrbs.pdf. Updated June 9, 2016. _reports/sr746.pdf. Published October 2015.
in the United States. N Engl J Med. 2003;348(26): Accessed June 14, 2016.
2635-2645. Accessed June 14, 2016.
19. Oberlander J. Long time coming: why health 31. Office of the Assistant Secretary for Planning
6. Commonwealth Fund. Why not the best? reform finally passed. Health Aff (Millwood). 2010;
Results from the National Scorecard on US Health and Evaluation, US Department of Health and
29(6):1112-1116. Human Services. Essential health benefits:
System Performance, 2008. http://www
.commonwealthfund.org/publications/fund 20. Courtemanche C, Marton J, Ukert B, Yelowtize individual market coverage. https://aspe.hhs.gov
-reports/2008/jul/why-not-the-best--results-from A, Zapata D. Impacts of the Affordable Care Act /basic-report/essential-health-benefits-individual
-the-national-scorecard-on-u-s--health-system on health insurance coverage in Medicaid -market-coverage. Published December 16, 2011.
-performance--2008. Published July 1, 2008. expansion and non-expansion states [NBER Accessed June 20, 2016.
Accessed June 14, 2016. working paper No. 22182]. National Bureau 32. Simmons A, Taylor J, Finegold K, Yabroff R,
of Economic Research. http://www.nber.org Gee E, Chappel E. The Affordable Care Act:
7. Cohen RA, Martinez ME, Zammitti EP. Early /papers/w22182. Published April 2016. Accessed
release of selected estimates based on data from promoting better health for women. Office of the
June 14, 2016. Assistant Secretary for Planning and Evaluation,
the National Health Interview Survey, 2015.
National Center for Health Statistics. http://www 21. Blumberg LJ, Garrett B, Holahan J. Estimating US Department of Health and Human Services.
.cdc.gov/nchs/nhis/releases/released201605.htm. the counterfactual: how many uninsured adults https://aspe.hhs.gov/pdf-report/affordable-care
Published May 24, 2016. Accessed June 14, 2016. would there be today without the ACA? Inquiry. -act-promoting-better-health-women. Published
2016;53(3):1-13. June 14, 2016. Accessed June 18, 2016.
8. Cohen RA, Makuc DM, Bernstein AB, Bilheimer
LT, Powell-Griner E. Health insurance coverage 22. Uberoi N, Finegold K, Gee E. Health insurance 33. Claxton G, Rae M, Long M, et al. Employer
trends, 1959-2007: estimates from the National coverage and the Affordable Care Act, 2010-2016. health benefits: 2015 annual survey. The Henry J.
Health Interview Survey. National Center for Health Office of the Assistant Secretary for Planning and Kaiser Family Foundation. http://files.kff.org
Statistics. http://www.cdc.gov/nchs/data/nhsr Evaluation, US Department of Health and Human /attachment/report-2015-employer-health
/nhsr017.pdf. Published July 1, 2009. Accessed Services. https://aspe.hhs.gov/sites/default/files -benefits-survey. Published September 22, 2015.
June 14, 2016. /pdf/187551/ACA2010-2016.pdf. Published March 3, Accessed June 14, 2016.
2016. Accessed June 14, 2016. 34. Centers for Medicare & Medicaid Services.
9. Cohen RA. Trends in health care coverage and
insurance for 1968-2011. National Center for Health More than 10 million people with Medicare have
jama.com (Reprinted) JAMA Published online July 11, 2016 E7
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ on 07/11/2016
Clinical Review & Education Special Communication US Health Care Reform: Progress and Next Steps
saved over $20 billion on prescription drugs since .healthcostinstitute.org/issue-brief-out-pocket -marketplaces-2014-2015-impact-premiums.
2010 [news release]. https://www.cms.gov -spending-trends-2013. Published October 2014. Published August 30, 2015. Accessed June 14,
/Newsroom/MediaReleaseDatabase/Press-releases Accessed June 14, 2016. 2016.
/2016-Press-releases-items/2016-02-08.html. 47. Health Care Cost Institute. 2014 Health care 58. Avery K, Gardner M, Gee E, Marchetti-Bowick
Published February 8, 2016. Accessed June 14, cost and utilization report. http://www E, McDowell A, Sen A. Health plan choice and
2016. .healthcostinstitute.org/2014-health-care-cost premiums in the 2016 Health Insurance
35. White C. Contrary to cost-shift theory, lower -and-utilization-report. Published October 2015. Marketplace. Office of the Assistant Secretary for
Medicare hospital payment rates for inpatient care Accessed June 14, 2016. Planning and Evaluation, US Department of Health
lead to lower private payment rates. Health Aff 48. Claxton C, Levitt L, Long M. Payments and Human Services. https://aspe.hhs.gov/pdf
(Millwood). 2013;32(5):935-943. for cost sharing increasing rapidly over time. -report/health-plan-choice-and-premiums-2016
36. Clemens J, Gottlieb JD. In the shadow of a Peterson-Kaiser Health System Tracker. http://www -health-insurance-marketplace. Published October
giant: Medicares influence on private payment .healthsystemtracker.org/insight/payments-for 30, 2015. Accessed June 14, 2016.
systems. http://www.joshuagottlieb.ca -cost-sharing-increasing-rapidly-over-time/. 59. Congressional Budget Office. Key issues
/ShadowOfAGiant.pdf. Accessed June 29, 2016. Published April 12, 2016. Accessed June 14, 2016. in analyzing major health insurance proposals.
37. US Department of Health and Human Services. 49. Agency for Healthcare Research and Quality. https://www.cbo.gov/publication/41746. Published
HHS reaches goal of tying 30 percent of Medicare Saving lives and saving money: hospital-acquired December 18, 2008. Accessed June 14, 2016.
payments to quality ahead of schedule [news conditions update. http://www.ahrq.gov 60. Wallace J, Song Z. Traditional Medicare versus
release]. http://www.hhs.gov/about/news/2016/03 /professionals/quality-patient-safety/pfp private insurance: how spending, volume, and price
/03/hhs-reaches-goal-tying-30-percent-medicare /interimhacrate2014.html. Updated December change at age sixty-five. Health Aff (Millwood).
-payments-quality-ahead-schedule.html. Published 2015. Accessed June 14, 2016. 2016;35(5):864-872.
March 3, 2016. Accessed June 14, 2016. 50. Zuckerman R. Reducing avoidable hospital 61. Congressional Budget Office. Options for
38. Muhlestein D. Growth and dispersion of readmissions to create a better, safer health care reducing the deficit: 2014 to 2023. https://www
accountable care organizations in 2015. Health system. US Department of Health and Human .cbo.gov/content/options-reducing-deficit-2014
Affairs Blog. http://healthaffairs.org/blog/2015/03 Services. http://www.hhs.gov/blog/2016/02/24 -2023. Published November 13, 2013. Accessed
/31/growth-and-dispersion-of-accountable-care /reducing-avoidable-hospital-readmissions.html. June 14, 2016.
-organizations-in-2015-2/. Published March 3, 2016. Published February 24, 2016. Accessed June 14, 62. Centers for Medicare & Medicaid Services. CMS
Accessed June 14, 2016. 2016. proposes to test new Medicare Part B prescription
39. Board of Trustees of the Federal Hospital 51. Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, drug models to improve quality of care and deliver
Insurance and Federal Supplementary Medical Epstein AM. Readmissions, observation, and the better value for Medicare beneficiaries [news
Insurance Trust Funds. 2015 Annual Report of the Hospital Readmissions Reduction Program. N Engl J release]. https://www.cms.gov/Newsroom
Board of Trustees of the Federal Hospital Insurance Med. 2016;374(16):1543-1551. /MediaReleaseDatabase/Fact-sheets/2016-Fact
and Federal Supplementary Medical Insurance Trust 52. Council of Economic Advisers. 2014 Economic -sheets-items/2016-03-08.html. Published March
Funds. Washington, DC: Centers for Medicare & Report of the President. Washington, DC: Council of 8, 2016. Accessed June 14, 2016.
Medicaid Services; 2015. Economic Advisers; 2014. 63. Office of Management and Budget. Budget of
40. Bureau of Economic Analysis. Table 1.1.4. Price 53. Shartzer A, Kenney GM, Long SK, Odu Y. the United States Government: Fiscal Year 2017.
indexes for gross domestic product. http://www A look at remaining uninsured adults as of March Washington, DC: Office of Management and Budget;
.bea.gov/iTable/index_nipa.cfm. Accessed June 14, 2015. Urban Institute. http://hrms.urban.org/briefs 2016.
2016. /A-Look-at-Remaining-Uninsured-Adults-as-of 64. Furman J, Fiedler M. The Cadillac tax: a crucial
41. Congressional Budget Office. The budget -March-2015.html. Published August 18, 2016. tool for delivery-system reform. N Engl J Med. 2016;
and economic outlook: fiscal years 2009 to 2019. Accessed June 14, 2016. 374(11):1008-1009.
https://www.cbo.gov/publication/41753. Published 54. Undem P. Understanding the uninsured now. 65. Buettgens M, Holahan J, Recht H. Medicaid
January 7, 2009. Accessed June 14, 2016. Robert Wood Johnson Foundation. http://www.rwjf expansion, health coverage, and spending:
42. Congressional Budget Office. Updated budget .org/en/library/research/2015/06/understanding an update for the 21 states that have not expanded
projections: 2016 to 2026. https://www.cbo.gov -the-uninsured-now.html. Published June 2015. eligibility. http://kff.org/medicaid/issue-brief
/publication/51384. Published March 24, 2016. Accessed June 14, 2016. /medicaid-expansion-health-coverage-and
Accessed June 14, 2016. 55. Congressional Budget Office. HR 4872, -spending-an-update-for-the-21-states-that-have
43. Congressional Budget Office. Private Health Reconciliation Act of 2010 (Final Health Care -not-expanded-eligibility/. Published April 29, 2015.
Insurance Premiums and Federal Policy. Washington, Legislation). https://www.cbo.gov/publication Accessed June 14, 2016.
DC: Congressional Budget Office; 2016. /21351. Published March 20, 2010. Accessed 66. Karlin-Smith S, Norman B. Pharma unleashes
44. Furman J. Next steps for health care reform. June 14, 2016. on Part B demo. Politico. http://www.politico.com
White House. https://www.whitehouse.gov/sites 56. Congressional Budget Office. Federal subsidies /tipsheets/prescription-pulse/2016/05/pharma
/default/files/page/files/20151007_next_steps for health insurance coverage for people under -unleashes-on-part-b-demo-214193. Published
_health_care_reform.pdf. Published October 7, 2015. age 65: 2016 to 2026. https://www.cbo.gov May 9, 2016. Accessed June 29, 2016.
Accessed June 14, 2016. /publication/51385. Published March 24, 2016. 67. Garunay M. Brents letter to the President:
45. Herrera CN, Gaynor M, Newman D, Town RJ, Accessed June 14, 2016. You saved my life. The White House. https://www
Parente ST. Trends underlying employer-sponsored 57. Sheingold S, Nguyen N, Chappel A. .whitehouse.gov/blog/2016/03/03/brents-letter
health insurance growth for Americans younger Competition and choice in the Health Insurance -president-you-saved-my-life. Published March 3,
than age sixty-five. Health Aff (Millwood). 2013;32 Marketplaces 2014-2015: impact on premiums. 2016. Accessed June 14, 2016.
(10):1715-1722. Office of the Assistant Secretary for Planning and 68. Kasich JR. 2013 State of the State Address.
46. Health Care Cost Institute. Out-of-pocket Evaluation, US Department of Health and Human Lima: Ohio State Legislature; 2013.
spending trends (2013). http://www Services. https://aspe.hhs.gov/basic-report
/competition-and-choice-health-insurance
E8 JAMA Published online July 11, 2016 (Reprinted) jama.com
Copyright 2016 American Medical Association. All rights reserved.
Downloaded From: http://jama.jamanetwork.com/ on 07/11/2016
Vous aimerez peut-être aussi
- Healthy Competition: What's Holding Back Health Care and How to Free ItD'EverandHealthy Competition: What's Holding Back Health Care and How to Free ItPas encore d'évaluation
- Healthcare Reform in AmericaDocument6 pagesHealthcare Reform in AmericaIjahss JournalPas encore d'évaluation
- United States Health Care Reform Progress To Date and Next StepsDocument9 pagesUnited States Health Care Reform Progress To Date and Next StepsEva MaglinteCanonPas encore d'évaluation
- Running Head: Perspective of The U.S. Healthcare System 1Document7 pagesRunning Head: Perspective of The U.S. Healthcare System 1api-481271344Pas encore d'évaluation
- Healthcare Reform1Document10 pagesHealthcare Reform1api-449184986Pas encore d'évaluation
- Week 6 - Final Policy PaperDocument7 pagesWeek 6 - Final Policy Paperapi-458308352Pas encore d'évaluation
- Healthy, Wealthy, and Wise: 5 Steps to a Better Health Care System, Second EditionD'EverandHealthy, Wealthy, and Wise: 5 Steps to a Better Health Care System, Second EditionÉvaluation : 5 sur 5 étoiles5/5 (1)
- Running Head: Affordable HealthDocument9 pagesRunning Head: Affordable Healthapi-406368312Pas encore d'évaluation
- Responding to Healthcare Reform: A Strategy Guide for Healthcare LeadersD'EverandResponding to Healthcare Reform: A Strategy Guide for Healthcare LeadersPas encore d'évaluation
- Artifact 3 Us Healthcare SystemDocument4 pagesArtifact 3 Us Healthcare Systemapi-481366015Pas encore d'évaluation
- Running Head: The Future of U.S. Healthcare System 1Document9 pagesRunning Head: The Future of U.S. Healthcare System 1Chemiati KhisaPas encore d'évaluation
- 3480 Social Welfare Policies Portfolio AssignmentDocument19 pages3480 Social Welfare Policies Portfolio Assignmentapi-628734736Pas encore d'évaluation
- Reforming America's Health Care System: The Flawed Vision of ObamaCareD'EverandReforming America's Health Care System: The Flawed Vision of ObamaCareÉvaluation : 5 sur 5 étoiles5/5 (2)
- Revitalizing the American Healthcare System: A Comprehensive Guide to Rebuilding, Reforming, and Reinventing Healthcare in the United States: Transforming the Future of Healthcare in America: A Practical and Inclusive ApproachD'EverandRevitalizing the American Healthcare System: A Comprehensive Guide to Rebuilding, Reforming, and Reinventing Healthcare in the United States: Transforming the Future of Healthcare in America: A Practical and Inclusive ApproachPas encore d'évaluation
- Contemporary Issues in the U.S. Healthcare DebateD'EverandContemporary Issues in the U.S. Healthcare DebatePas encore d'évaluation
- TennCare, One State's Experiment with Medicaid ExpansionD'EverandTennCare, One State's Experiment with Medicaid ExpansionPas encore d'évaluation
- TennCare, One State's Experiment with Medicaid ExpansionD'EverandTennCare, One State's Experiment with Medicaid ExpansionPas encore d'évaluation
- Heading Towards A Single Government Payer SystemDocument4 pagesHeading Towards A Single Government Payer SystemNeelkumar SoniPas encore d'évaluation
- Code Red: An Economist Explains How to Revive the Healthcare System without Destroying ItD'EverandCode Red: An Economist Explains How to Revive the Healthcare System without Destroying ItPas encore d'évaluation
- Economics 6th Edition Hubbard Solutions Manual DownloadDocument20 pagesEconomics 6th Edition Hubbard Solutions Manual DownloadHarriet Mikels100% (20)
- Comparative Analysis of American Healthcare & Canadian HealthcareDocument5 pagesComparative Analysis of American Healthcare & Canadian HealthcareVishal VijPas encore d'évaluation
- Impact of ACA On US Health Care EcosystemDocument7 pagesImpact of ACA On US Health Care EcosystemUmme FarwahPas encore d'évaluation
- Solution Manual For American Public Policy An Introduction 11th EditionDocument19 pagesSolution Manual For American Public Policy An Introduction 11th EditionScottWyattognje100% (42)
- Impact of ACA On US Health Care Ecosystem RevisedDocument8 pagesImpact of ACA On US Health Care Ecosystem RevisedUmme FarwahPas encore d'évaluation
- Analysis of Health Care System Initiatives in MA and SF, CA (Function, Cost, Outcome)Document7 pagesAnalysis of Health Care System Initiatives in MA and SF, CA (Function, Cost, Outcome)Wonder LostPas encore d'évaluation
- Attachment 1Document7 pagesAttachment 1Anna AkhayanPas encore d'évaluation
- QUESTION # 1: Analyze Why Is It Important For Health Care Managers and Policy-Makers To Understand The Intricacies of The Health Care Delivery SystemDocument5 pagesQUESTION # 1: Analyze Why Is It Important For Health Care Managers and Policy-Makers To Understand The Intricacies of The Health Care Delivery SystemLenie ManayamPas encore d'évaluation
- Hca 451 Economic Analysis PaperDocument13 pagesHca 451 Economic Analysis Paperapi-535414037Pas encore d'évaluation
- Restoring Quality Health Care: A Six-Point Plan for Comprehensive Reform at Lower CostD'EverandRestoring Quality Health Care: A Six-Point Plan for Comprehensive Reform at Lower CostPas encore d'évaluation
- US Equity and Equality in HealthDocument60 pagesUS Equity and Equality in Healthnia wardhaniPas encore d'évaluation
- Macroeconomics 6th Edition Hubbard Solutions Manual DownloadDocument20 pagesMacroeconomics 6th Edition Hubbard Solutions Manual DownloadDarrell Davis100% (21)
- Controversy in U.S Healthcare System PolicyDocument5 pagesControversy in U.S Healthcare System Policydenis edembaPas encore d'évaluation
- Futurescan 2022–2027: Health Care Trends and ImplicationsD'EverandFuturescan 2022–2027: Health Care Trends and ImplicationsÉvaluation : 5 sur 5 étoiles5/5 (1)
- Universal Healthcare Final - Shawn GuevaraDocument7 pagesUniversal Healthcare Final - Shawn Guevaraapi-711489277Pas encore d'évaluation
- Patient Protection and Affordable Care Act - Gary Parker 3Document7 pagesPatient Protection and Affordable Care Act - Gary Parker 3api-469041523Pas encore d'évaluation
- A New Era in U.S. Health Care: Critical Next Steps Under the Affordable Care ActD'EverandA New Era in U.S. Health Care: Critical Next Steps Under the Affordable Care ActÉvaluation : 4 sur 5 étoiles4/5 (2)
- The Impactofthe Affordable Care Acton North Carolinas Uninsured PopulationDocument6 pagesThe Impactofthe Affordable Care Acton North Carolinas Uninsured PopulationLori A. DixonPas encore d'évaluation
- How To Write A Research Paper On Health Care ReformDocument7 pagesHow To Write A Research Paper On Health Care Reformlyn0l1gamop2Pas encore d'évaluation
- Crisis of Abundance: Rethinking How We Pay for Health CareD'EverandCrisis of Abundance: Rethinking How We Pay for Health CareÉvaluation : 3.5 sur 5 étoiles3.5/5 (2)
- Signature Assignment - SOCI 1301Document6 pagesSignature Assignment - SOCI 1301Jassmin ArandaPas encore d'évaluation
- American Healthcare Reform: Fixing the Real ProblemsD'EverandAmerican Healthcare Reform: Fixing the Real ProblemsPas encore d'évaluation
- The Medical Rights University of Maryland University CollegeDocument12 pagesThe Medical Rights University of Maryland University Collegepy007Pas encore d'évaluation
- 2023__DualDiplomaUnitedStatesGovernmentHon_A_2.04AAmendingtheConstitutionDocument8 pages2023__DualDiplomaUnitedStatesGovernmentHon_A_2.04AAmendingtheConstitutionBerta Boyer RosichPas encore d'évaluation
- Expansion of Medicaid Coverage Critical Analysis Paper - Sletta MataDocument11 pagesExpansion of Medicaid Coverage Critical Analysis Paper - Sletta Mataapi-497063972Pas encore d'évaluation
- Walker Style DraftDocument11 pagesWalker Style Draftapi-437845987Pas encore d'évaluation
- Healthcare White PaperDocument13 pagesHealthcare White PaperJacobPersily100% (1)
- Recovery: A Guide to Reforming the U.S. Health SectorD'EverandRecovery: A Guide to Reforming the U.S. Health SectorPas encore d'évaluation
- Caring for Our Communities: A Blueprint for Better Outcomes in Population HealthD'EverandCaring for Our Communities: A Blueprint for Better Outcomes in Population HealthPas encore d'évaluation
- Why Obamacare Is Wrong for America: How the New Health Care Law Drives Up Costs, Puts Government in Charge of Your Decisions, and Threatens Your Constitutional RightsD'EverandWhy Obamacare Is Wrong for America: How the New Health Care Law Drives Up Costs, Puts Government in Charge of Your Decisions, and Threatens Your Constitutional RightsPas encore d'évaluation
- Microsoft Word - Statement On Health Care ReformDocument4 pagesMicrosoft Word - Statement On Health Care ReformCommittee For a Responsible Federal BudgetPas encore d'évaluation
- Niles Chp1 2021Document22 pagesNiles Chp1 2021Trent HardestyPas encore d'évaluation
- One Sentence Health Care Reforms: 200 Alternatives and Steps Beyond the Affordable Care ActD'EverandOne Sentence Health Care Reforms: 200 Alternatives and Steps Beyond the Affordable Care ActPas encore d'évaluation
- Milwaukee Journal Sentinel - Medical Community Seeing That Better Health Hinges On Social Services 16pDocument16 pagesMilwaukee Journal Sentinel - Medical Community Seeing That Better Health Hinges On Social Services 16pJoão Pedro RamosPas encore d'évaluation
- Longman, Phillip - Vista Total Health - 20101005Document19 pagesLongman, Phillip - Vista Total Health - 20101005Sam SunshinePas encore d'évaluation
- Current and Future Devt. in HealthcareDocument12 pagesCurrent and Future Devt. in HealthcareJohn Philip MacatangayPas encore d'évaluation
- Aspen CP PosterDocument1 pageAspen CP PosterJosh ShaevitzPas encore d'évaluation
- Electromagnetism: Chapter - 2Document31 pagesElectromagnetism: Chapter - 2Izzah HzmhPas encore d'évaluation
- Sarita Shaevitz Orch Y 122 41-51702/NY4: Issued To Section ROW Seat Order NumberDocument4 pagesSarita Shaevitz Orch Y 122 41-51702/NY4: Issued To Section ROW Seat Order NumberJosh ShaevitzPas encore d'évaluation
- Predicting C. elegans Behavior from Whole-Brain Neural ActivityDocument32 pagesPredicting C. elegans Behavior from Whole-Brain Neural ActivityJosh ShaevitzPas encore d'évaluation
- Tiger Tribune 2.13.2020Document22 pagesTiger Tribune 2.13.2020Josh ShaevitzPas encore d'évaluation
- Electron ConfigurationDocument28 pagesElectron ConfigurationphillipPas encore d'évaluation
- Gray-Arranging BarbershopDocument2 pagesGray-Arranging BarbershopJosh Shaevitz50% (2)
- 03.03 LB NewsletterDocument5 pages03.03 LB NewsletterJosh ShaevitzPas encore d'évaluation
- Owner's Manual: Automatic Standby GeneratorDocument36 pagesOwner's Manual: Automatic Standby GeneratorrichPas encore d'évaluation
- QCB Flyer - 2015Document1 pageQCB Flyer - 2015Josh ShaevitzPas encore d'évaluation
- PRTM PL 88334Document7 pagesPRTM PL 88334Josh ShaevitzPas encore d'évaluation
- What Is LifeDocument32 pagesWhat Is LifeTrnyrtby Rbytryt100% (1)
- Oxtoby App ADocument8 pagesOxtoby App AJosh ShaevitzPas encore d'évaluation
- HydrogenOrbitals AuthorDocument51 pagesHydrogenOrbitals AuthorJosh ShaevitzPas encore d'évaluation
- Jimaging 03 00007 PDFDocument26 pagesJimaging 03 00007 PDFJosh ShaevitzPas encore d'évaluation
- PHS Electives 2019 - 2020 Visual & Performing Arts Practical Arts (21st C Life & Careers)Document2 pagesPHS Electives 2019 - 2020 Visual & Performing Arts Practical Arts (21st C Life & Careers)Josh ShaevitzPas encore d'évaluation
- Practical Guide to Optical Trapping and Its Applications in BiologyDocument39 pagesPractical Guide to Optical Trapping and Its Applications in BiologyJosh ShaevitzPas encore d'évaluation
- Oxtoby App F PDFDocument10 pagesOxtoby App F PDFJosh ShaevitzPas encore d'évaluation
- Lyanpunov Exponents Pikovsky PDFDocument939 pagesLyanpunov Exponents Pikovsky PDFJosh ShaevitzPas encore d'évaluation
- PhilNelson TIRF Tunnelling PDFDocument13 pagesPhilNelson TIRF Tunnelling PDFJosh ShaevitzPas encore d'évaluation
- JW WelcomeDocument2 pagesJW WelcomeJosh ShaevitzPas encore d'évaluation
- PhilNelson TIRF Tunnelling PDFDocument13 pagesPhilNelson TIRF Tunnelling PDFJosh ShaevitzPas encore d'évaluation
- PFC Summer School Schedule 180610Document1 pagePFC Summer School Schedule 180610Josh ShaevitzPas encore d'évaluation
- Hanna H. Gray Fellows Program - Trainee FormDocument2 pagesHanna H. Gray Fellows Program - Trainee FormJosh ShaevitzPas encore d'évaluation
- Read MeDocument2 pagesRead MeJosh ShaevitzPas encore d'évaluation
- PlainDocument1 pagePlainJosh ShaevitzPas encore d'évaluation
- My PortsDocument22 pagesMy PortsJosh ShaevitzPas encore d'évaluation
- Release TexliveDocument1 pageRelease TexliveWindu Nur MohamadPas encore d'évaluation
- Drag of The Cytosol As A Transport Mechanism in Neurons: Biophysical Journal June 2014 2710-2719Document10 pagesDrag of The Cytosol As A Transport Mechanism in Neurons: Biophysical Journal June 2014 2710-2719Josh ShaevitzPas encore d'évaluation
- Manual Murray 20Document28 pagesManual Murray 20freebanker777741Pas encore d'évaluation
- Refrigeration and Air Conditioning Technology 8th Edition Tomczyk Silberstein Whitman Johnson Solution ManualDocument5 pagesRefrigeration and Air Conditioning Technology 8th Edition Tomczyk Silberstein Whitman Johnson Solution Manualrachel100% (24)
- JP - Health and Wholeness Through The Holy CommunionDocument62 pagesJP - Health and Wholeness Through The Holy Communionjevontan90% (10)
- Thalassemia WikiDocument12 pagesThalassemia Wikiholy_miraclePas encore d'évaluation
- Environmental Pollution and DegradationDocument2 pagesEnvironmental Pollution and DegradationCharLene MaRiePas encore d'évaluation
- Transpo Printable Lecture4Document10 pagesTranspo Printable Lecture4Jabin Sta. TeresaPas encore d'évaluation
- Save and share GZCL training spreadsheets onlineDocument263 pagesSave and share GZCL training spreadsheets onlinejohn wick100% (1)
- Installation TubeeeDocument7 pagesInstallation TubeeeDini NovitrianingsihPas encore d'évaluation
- Introduction To Iron Metallurgy PDFDocument90 pagesIntroduction To Iron Metallurgy PDFDrTrinath TalapaneniPas encore d'évaluation
- Q A With Jaquelyn BurrerDocument3 pagesQ A With Jaquelyn Burrerapi-480718823Pas encore d'évaluation
- Ethics and Disasters: Patricia Reynolds Director, Bishopric Medical Library Sarasota Memorial Hospital Sarasota, FLDocument61 pagesEthics and Disasters: Patricia Reynolds Director, Bishopric Medical Library Sarasota Memorial Hospital Sarasota, FLChandra Prakash JainPas encore d'évaluation
- KPI and Supplier Performance Scorecard ToolDocument7 pagesKPI and Supplier Performance Scorecard ToolJayant Kumar JhaPas encore d'évaluation
- Funda PharmaDocument9 pagesFunda PharmaShiangPas encore d'évaluation
- Q 400 SYSTEM BestDocument9 pagesQ 400 SYSTEM BestTeddy EshtePas encore d'évaluation
- 'S Outfits and Emergency Escape Breathing Devices (Eebd)Document11 pages'S Outfits and Emergency Escape Breathing Devices (Eebd)Thurdsuk NoinijPas encore d'évaluation
- Electric Vehicle BatteryDocument15 pagesElectric Vehicle BatteryTotal Acess100% (1)
- Physical Therpay Protocols For Conditions of Neck RegionDocument74 pagesPhysical Therpay Protocols For Conditions of Neck Regionjrpsaavedra4599Pas encore d'évaluation
- AC7101.1 Rev G 2Document37 pagesAC7101.1 Rev G 2Namelezz ShadowwPas encore d'évaluation
- Objectives and Aspects of School Health ServicesDocument4 pagesObjectives and Aspects of School Health ServicesRaed AlhnaityPas encore d'évaluation
- Fermenting For Health - Pip MagazineDocument2 pagesFermenting For Health - Pip MagazinePip MagazinePas encore d'évaluation
- GP Series Portable Generator: Owner's ManualDocument48 pagesGP Series Portable Generator: Owner's ManualWilliam Medina CondorPas encore d'évaluation
- Amnesia With Focus On Post Traumatic AmnesiaDocument27 pagesAmnesia With Focus On Post Traumatic AmnesiaWilliam ClemmonsPas encore d'évaluation
- A Text Book On Nursing Management AccordDocument790 pagesA Text Book On Nursing Management AccordMohammed AfzalPas encore d'évaluation
- P1007 PPPS For Raw Milk 1AR SD3 Cheese Risk AssessmentDocument304 pagesP1007 PPPS For Raw Milk 1AR SD3 Cheese Risk AssessmentNicholasPas encore d'évaluation
- Review of Literature Review of LiteratureDocument31 pagesReview of Literature Review of LiteratureeswariPas encore d'évaluation
- Cholinergic DrugsDocument29 pagesCholinergic DrugsKiranPas encore d'évaluation
- Acute Atelectasis Prevention & TreatmentDocument9 pagesAcute Atelectasis Prevention & TreatmentmetabolismeproteinPas encore d'évaluation
- Employment Law Lubs 3915Document4 pagesEmployment Law Lubs 3915ogunsatoPas encore d'évaluation
- Form16 (2021-2022)Document2 pagesForm16 (2021-2022)Anushka PoddarPas encore d'évaluation
- Proceedings of BUU Conference 2012Document693 pagesProceedings of BUU Conference 2012Preecha SakarungPas encore d'évaluation