Académique Documents
Professionnel Documents
Culture Documents
Blake Et Al 2006
Transféré par
satmayaniCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Blake Et Al 2006
Transféré par
satmayaniDroits d'auteur :
Formats disponibles
Facilitators and Barriers to
10 National Quality Forum Safe Practices
Sarah C. Blake, MA
Susan Kohler, RN, MPH
Kimberly Rask, MD, PhD
Anne Davis, BSN, MPA
Dorothy Vi Naylor, RN, MN
The objective of this study was to identify facilita- In November 1999, the Institute of Medicine
tors and barriers to the implementation of 10 released its landmark report titled To Err Is Human:
National Quality Forum (NQF) medication processes Building a Safer Health System.1 The report claimed
and the culture of safety practices in Georgia hospi- that more than 1 million people in the United States
tals. In-depth interviews with hospital administra-
suffer from preventable medical injuries each year
tors were conducted to identify facilitators and
barriers to the implementation of programs that sup-
and as many as 98 000 people die annually in hospi-
port the NQF safe practices. Hospitals identified sig- tals because of medical errors. Although evidence-
nificant as well as other key factors that resulted in based methods are available to prevent adverse
the adoption and/or nonadoption of medication and events, there is concern that the current lack of stan-
culture of safety practices. Informants also identified dardization among hospitals implementing such safe
strategies used to overcome barriers that were expe- practices has the potential to both diffuse and dilute
rienced. Facilitators to both practices include admin- efforts to improve patient safety.
istrative leadership support and education and To address this issue, the National Quality
training. The resistance to change was the most sig- Forum (NQF) published an evidence-based consen-
nificant barrier identified in both the safe medica- sus report listing 30 safe practices for better health
tion process interviews and the culture of safety
care that should be universally adopted. However,
interviews. Implementing safety practices can be a
difficult process, replete with organizational, finan-
while there is public pressure for hospitals to fully
cial, and professional barriers. Strategies identified comply, there is no evidence-based method of priori-
by our informants to overcome these barriers may tizing these practices. Many of the practices are
assist other hospitals currently facing this challenge. defined very broadly, for example, create a health-
(Am J Med Qual 2006;21:323-334) care culture of safety. Questions also remain as to
the utility and ease of implementing some practices
Keywords: safety management; quality of health care;
quality assurance; organizational culture; medical errors
and identifying the best strategies for implementa-
tion. As the NQF consensus report notes,
AUTHORS NOTE: This project was supported by contract
For any given healthcare provider, the choice of prac-
290-00-0011 from the Agency for Healthcare Research and Quality.
tices that will have top priority will depend on the
Ms Blake, Ms Kohler, and Dr Rask are at the Emory Center on individual providers circumstances, including which
Health Outcomes and Quality, Rollins School of Public Health, practices already have been implemented, availabil-
Atlanta, Georgia. Ms Davis and Ms Naylor are at the Georgia ity of resources, environmental constraints, and other
Hospital Association, Marietta. The authors have no affiliation with
individual factors.2
or financial interest in any product mentioned in this article. The
authors research was not supported by any commercial or corpo-
rate entity. Corresponding author: Sarah C. Blake, Rollins School of The purpose of this study was to identify facilita-
Public Health, Emory University, 1518 Clifton Road NE #672, tors and barriers to the implementation of programs
Atlanta, GA 30322 (e-mail: scblake@sph.emory.edu). that support 10 NQF patient safety practices. Nine
American Journal of Medical Quality, Vol. 21, No. 5, Sep/Oct 2006 practices focus directly on medication processes, while
DOI: 10.1177/1062860606291781 1 practice focuses on hospital safety culture. In-depth
Copyright 2006 by the American College of Medical Quality interviews were conducted with top performance
323
Downloaded from ajm.sagepub.com at UNIV OF VIRGINIA on September 6, 2015
324 Blake et al AMERICAN JOURNAL OF MEDICAL QUALITY
improvement managers from a statewide sample of culture programs. When the 2 lists were compared,
hospitals in Georgia that have and have not imple- 13 hospitals were identified as top performers for
mented clinical programs supporting the safe prac- medication process but bottom performers for COS
tices. In this article, we present key findings from this or the converse and so were eliminated from consid-
qualitative study. eration. Six hospitals were ineligible for reasons
such as being a nonacute care facility. The final
METHODS
sample resulted in 81 unique hospitals.
Design Data Collection
We conducted semistructured interviews of 2 Between April and May 2005, letters seeking
hospital groups: adopters and nonadopters of safe hospital participation in a telephone interview were
medication practices. distributed to the 81 eligible hospitals. A second mail-
ing to nonresponders was sent in early July 2005.
Participants Because researchers were blinded to the hospitals
identification, recruitment efforts were conducted by
The Georgia Hospital Association (GHA) recruited the GHA. Hospitals that wished to participate were
hospital participants from their Partnership for instructed to contact Emory University researchers
Health and Accountability (PHA) membership. PHA directly. Contact information was provided in the
is a voluntary patient safety initiative designed to introductory letter. A total of 19 hospitals agreed to
promote the health and welfare of Georgians by participate, and 18 interviews were completed. Each
improving care, reducing risk, preventing medical interview was conducted by telephone and lasted
errors, and identifying strategies needed to create a between 30 and 45 minutes. The completed inter-
culture of safety (COS). All 147 acute care hospitals views represented a participation rate of 22.2%
in the state of Georgia participate in the program. (18/81).
PHA includes a broad cross section of hospital types,
with 55% having fewer than 100 beds, 25% having Survey Instrument
100 to 299 beds, and 20% having 300 or more beds.
Hospitals are evenly divided between urban (54%) Two survey instruments were developed for this
and rural (46%) locations. project: a safe medication use questionnaire and a
COS questionnaire. The questionnaires were used
Hospital Selection to solicit feedback on key facilitators and barriers
to implementing safe practices.
Hospitals in PHA participate in statewide sur-
veys on safe medication use practices and strategies Medication Process Questionnaire
for safe culture leadership. Responses to these sur-
vey questions were used to rank all Georgia hospi- Nine of the NQF patient safety practice initia-
tals from high to low adopters. The hospital ranking tives specifically targeted medication practices
was specifically designed to capture a range of both (Table 1). Informants initially were asked to quan-
top and low adopters. Hospitals were ranked after tify the extent to which their hospital adopted each
sorting blinded hospital IDs in descending order by of the safety practices. Next, informants were
total number of fully implemented safety practices asked to select both their most successful and most
and in ascending order by total number of nonim- challenging initiative for an in-depth discussion
plemented practices. Hospitals with the highest about factors that resulted in the adoption and/or
ranking were those with the greatest number of nonadoption of these practices. Informants were
fully implemented safety practice interventions and asked to identify the most significant facilitators
the least number of nonimplemented safety prac- and barriers as well as strategies used to overcome
tices. From this list, 25 high and 25 low adopters of barriers. Finally, informants were asked how they
medication-related NQF safe practices were identi- prioritized the adoption of these safety practices
fied. A similar strategy was used to rank and ran- and their experience piggybacking initiatives
domly select 25 high and 25 low adopters of safety onto other patient safety practices.
Downloaded from ajm.sagepub.com at UNIV OF VIRGINIA on September 6, 2015
AMERICAN JOURNAL OF MEDICAL QUALITY 10 National Quality Forum Safe Practices 325
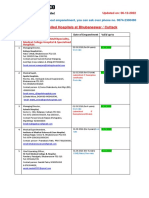
Table 1
List of National Quality Forum (NQF) Medication Process Practices
NQF Number Variable Name Description of Safe Practice
1 Culture of safety Create a health care culture of safety
5 Consultant pharmacists Pharmacists should actively participate in the
medication use process including, at a minimum, being available
for consultation with prescribers and reviewing medication orders
6 Verbal orders Verbal orders should be recorded whenever
possible and immediately read back to the prescriber
7 Abbreviations Use of standardized abbreviations and dosage designations
9 Information transfer Ensure that care information, especially changes in orders and new
diagnostic information, is transmitted to all providers
12 CPOE adoption Implement a CPOE
27 Clean work spaces Keep work spaces where medications are prepared clean, orderly,
well lit, and free of clutter, distraction, and noise
28 Labeling and storage Standardize the methods for labeling,
packaging, and storing medications
29 High-alert medications Identify all high-alert drugs
30 Unit dosing Dispense medications in unit dose or, when
appropriate, unit-of-use form whenever possible
CPOE = computerized prescriber order entry.
COS Questionnaire norms about and frequency of error reporting, non-
punitive response to error, and teamwork (T. L. Scott,
One NQF COS program initiative was targeted for L. Schuessler, E. Friedman, V. Naylor, S. Walzcak,
this study. Eleven COS dimensions were identified unpublished data, 2006).
within this initiative (Table 2). These dimensions
were identified in a safety culture assessment tool Analysis
developed by Westat for the Agency for Healthcare
Research and Quality.3 Interviews were audiotaped and transcribed.
The interviews began with assessing the interview- Interviewers also kept notes from each interview
ees job responsibilities, knowledge of and interaction that were used in combination with the transcrip-
within the hospital unit, and understanding of the tions to produce an interview summary that cap-
term culture of safety. Interviewees also were asked tured participants key points about their hospitals
to report on what resources they used to understand patient safety initiatives. Content from both the
or interpret COS. Informants were then asked to medication process interviews and the COS inter-
report which of the 11 COS dimensions were adopted views was analyzed according to the interview ques-
and/or implemented by their hospital. Next, inform- tions and organized into frameworks of categories
ants were asked to describe 2 of these initiatives that and subcategories determined by the responses. Key
were of greatest importance to their hospital. themes were then placed into summary matrixes to
Informants were then asked to discuss facilitators facilitate analysis. Both interviewers reviewed all
and barriers to the adoption of each implemented summaries and matrices and found consensus with
COS initiative, as well as to identify the most signif- the key themes that were identified, therefore
icant facilitator to adoption and strategies used to ensuring 100% interrater reliability.
overcome barriers. Finally, informants were asked
additional questions about each of the 2 COS initia- RESULTS
tives they discussed. These additional questions were
adapted from the Westat Hospital Survey on Patient Hospital Characteristics
Safety. This survey is an employee survey that meas-
ures aspects of organizational culture that affect A total of 8 medication process interviews and 10
patient safety, such as overall perceptions of safety, COS interviews were conducted with representatives
Downloaded from ajm.sagepub.com at UNIV OF VIRGINIA on September 6, 2015
326 Blake et al AMERICAN JOURNAL OF MEDICAL QUALITY
Table 2
List of National Quality Forum (NQF) Culture of Safety (COS) Dimensions
COS Dimension Description of COS Dimension
Nonpunitive response to error The hospital implements a nonpunitive policy to address patient adverse events involving medical staff
or blame-free environment and hospital employees
Frequency of reporting A user-friendly and confidential error-reporting system is available for all error levels
Staffing The hospital maintains safe staffing through cross-training, adequate staffing ratios, appropriate skill mix,
and limited work hours
Supervisor/manager Hospital supervisors/managers say a good word when they see a job done according to established
expectations and actions patient safety procedures; supervisors/managers seriously consider staff suggestions for improving
promoting safety patient safety; whenever pressure builds up, a supervisor/manager wants staff to work faster, even if
it means taking shortcuts
Organizational learning, The hospital is actively doing something to promote patient safety; mistakes have led to positive
continuous improvement changes within the hospital; hospital evaluates the effectiveness of new changes made to improve
patient safety
Teamwork within hospital units People support one another within and among hospital units; people trust each other and treat one
another with respect; there is teamwork when a lot of work needs to be done
Communication openness Staff freely speak up if they see something that may negatively affect patient care; staff feel free to
question the decisions or actions of those with more authority; staff are afraid to ask questions when
something does not seem right
Feedback and communication Managers and staff talk openly about patient safety problems that exist
about error
Hospital management support Hospital management provides a work climate that promotes patient safety; the actions of hospital
for patient safety management show that patient safety is a top priority; hospital management seems interested in
patient safety only after an adverse event happens
Teamwork across hospital There is good cooperation among hospital units that need to work together; hospital units work well
units together to provide the best care for patients; hospital units do not coordinate well with each other;
it is often unpleasant to work with staff from other hospital units
Hospital handoffs and Transferring patients between and among hospital units goes very smoothly
transitions (hospital-wide)
of the 18 participating hospitals. Eight hospitals directors of quality, 1 was a quality improvement
(44.4%) were top performers, and 12 (66.7%) were manager, and 1 was director of patient safety. Given
located in urban areas (Table 3). In contrast, among their job positions, the interviewed persons gener-
all Georgia hospitals, 50 (34.0%), are top performers, ally had good knowledge of their hospitals imple-
and 80 (54.4%) are located in urban areas. With mentation efforts. The number of participating
respect to bed size, 6 (33.3%) participating hospitals hospitals that reported having fully implemented
had fewer than 100 beds, 5 (27.8%) had 100 to 300 the targeted safe practices is shown in Table 4. Full
beds, and 7 (38.9%) had more than 300 beds. When implementation was defined as adoption in greater
compared to all Georgia hospitals, the study sample than 90% of the organization. Five of the safe prac-
had a smaller proportion of hospitals with fewer than tices were reported as being fully implemented by at
100 beds (33.3% vs 55.1%) and a larger proportion of least three fourths of the hospitals including identi-
hospitals with more than 300 beds (38.9% vs 19.7%). fication of high-alert medication (7/8), use of unit
Of the 8 top-performing hospitals that participated in doses when appropriate (6/8), minimizing verbal
this research, 4 were in urban areas of the state and orders (6/8), ensuring information transfer (6/8), and
2 had more than 300 beds. Of the 10 bottom- standardizing labeling and storage (6/8). Providing
performing hospitals, 8 were in urban areas of the clean workspaces and minimizing abbreviations
state and 5 had more than 300 beds. were reported as being fully implemented by 5 of the
8 hospitals, while availability of consultant pharma-
Adoption of 9 NQF Safe Medication Practices cists was described as being fully implemented by
4 of the study hospitals. None of the participating
Among the 8 medication practice participants, 4 hospitals had fully adopted computerized prescriber
were performance improvement coordinators, 2 were order entry.
Downloaded from ajm.sagepub.com at UNIV OF VIRGINIA on September 6, 2015
AMERICAN JOURNAL OF MEDICAL QUALITY 10 National Quality Forum Safe Practices 327
Table 3 Table 4
Hospital Characteristics Number of Hospitals Fully Implementing 9
National Quality Forum (NQF) Medication Safety
Georgia
Sample Hospitals Practices, Sorted by Percentage Adoption
(n = 18) (n = 147) NQF Number Title Full Implementation
Characteristic n % n % 29 Identification of 7/8 (87.5%)
Location* high-alert medication
Urban 12 66.7 80 54.4 6 Minimize verbal orders 6/8 (75.0%)
Rural 6 33.3 67 45.6 30 Use of unit dosing 6/8 (75.0%)
Bed size group* 28 Standardize labeling
<100 6 33.3 81 55.1 and storage 6/8 (75.0%)
100-300 5 27.8 37 25.2 9 Ensure information transfer 6/8 (75.0%)
>300 7 38.9 29 19.7 7 Minimize abbreviations 5/8 (62.5%)
Performance level 27 Provide clean workspaces 5/8 (62.5%)
Top performer 8 44.4 50 34.0 5 Availability of consultant 4/8 (50.0%)
Mid performer 0 0.0 53 36.1 pharmacists
Bottom performer 10 55.6 44 29.9 12 Computerized prescriber 0 (0.0%)
order entry adoption
*Not significant at P = .05.
Significant at P = .05.
Facilitators to Adoption: Most Successful Practice theme in almost all interviews. Random chart
audit with feedback to staff and/or physicians
Participants were asked to identify a highly suc- helped reinforce the patient safety message.
cessful safety initiative for an in-depth discussion Feedback consisted of individual profiles of past
of implementation facilitators and barriers. Most practice compared to peers coupled with face-to-
of the interviewees (6/8) chose to discuss their hos- face meetings and/or letters from administra-
pitals safety program for minimizing abbrevia- tion. Most hospitals shared results from the
tions. Frequently named facilitators, barriers, and chart audits with their performance improve-
strategies employed to overcome these barriers are ment committee and/or department chiefs.
described below beginning with those facilitators According to one interviewee, The use of any
identified as most significant. dangerous abbreviation is considered a rule vio-
lation which is against hospital policy. Another
Most Significant Facilitators to Adoption informant noted, Anytime youre monitoring
something, compliance is better . . . everyone is
Administrative leadership: The commitment of willing to change . . . its just a habit and habits
hospital executives, physician leaders, and are hard to break.
department heads was among the most fre- Education: Most hospitals initially relied on for-
quently mentioned facilitator contributing to mal or informal education efforts to raise aware-
the adoption of the unapproved abbreviation ness, confront resistance, and discuss goals
list. Four of the 6 interviewees believed leader- and/or expectations. However, according to one
ships ability to communicate and commit to respondent, education has its limits: From my
this initiative was an essential first step toward experience, simply talking to medical staff
establishing and promoting a COS. As one about their rates of abuse is only effective for
interviewee stated, We have a leadership team about 2 weeks . . . after the meetings youll start
that embraces the National Patient Safety to see the old habits beginning to creep back in.
goals and their importance . . . it is an expecta- Another participant noted, Its not just the edu-
tion at our hospital . . . an important part of our cation getting them past the bad habits, you
culture. have to keep going back and back and repeating
Audit and feedback: The importance of regular and then they get into a rhythm . . . they need
monitoring to reinforce compliance was a recurring constant reinforcement.
Downloaded from ajm.sagepub.com at UNIV OF VIRGINIA on September 6, 2015
328 Blake et al AMERICAN JOURNAL OF MEDICAL QUALITY
Champions: Several hospitals designated a predominant theme in our interviews. As one
champion leader to drive the initiative. One interviewee stated, Abbreviations was a tough
hospitals champion was a pharmacist who sell . . . we have physicians who had practiced
conducted ongoing discussions with clinical here for 25 to 30 years . . . who have used
staff on all units to raise awareness about the abbreviations so much and now they have
banned abbreviations and to emphasize the to change. Another interviewee lamented,
importance of preventing medical errors and Changing habits is very difficult . . . this one
improving patient safety. was not a bad habit that was picked up, it was
actually taught. You spend years learning the
Other Key Facilitators to Adoption abbreviations and then all of the sudden some-
one comes by and tells you not to use them
Physician and staff buy in: Most of the interview- anymore.
ees considered the involvement of physicians Strategies used to change behavior: Motivating
and staff in the development of the dangerous change through education, reinforcement, pos-
abbreviation list to be critical for success. itive incentives, and full leadership support
Several hospitals established multidisciplinary were strategies employed by most of the par-
work groups to ensure that a broad spectrum of ticipating hospitals. For example, a highly suc-
physicians and staff members were involved in cessful initiative implemented by 1 hospital
the process of creating and approving the list. included a multipronged program of education,
Surveys were conducted to solicit staff feedback positive incentives, and feedback. As described
and suggestions for changes. by the interviewee,
External pressure: Most interviewees reported
Our hospital had a drive called the Write it Right
that the compliance with Joint Commission on campaign where we made stickers, posters . . . and
Acreditation of Healthcare Organizations placed reminders on charts. We also had some
(JCAHO) recommendations was a source of rather inventive T-shirts . . . we gave big loser
motivation in adopting their unapproved abbre- T-shirts to our worst offenders and gift certificates
viation list. Several interviewees mentioned the to staff who improved the most. . . . When the cam-
fear of being out of compliance, while another paign was over we went back through orders and
noted that the tips and guidelines available from counted up to see how everybody was doing . . . and
the JCAHO were beneficial in convincing physi- we met with the doctors face-to-face [the ones that
cians of the importance of this initiative. Giving needed the most improvement] and talked to
them. . . . It turned out that our Medical Director
examples of sentinel events from the Joint
[who supported the initiative] was our biggest
Commissions website was very helpful . . . exam-
offender . . . but he was also the one who improved
ples of bad outcomes and deaths . . . [physicians] the most so he received a nice prize. . . . Now Id say
paid attention to those. were probably 99% compliant.
Reminders: Many hospitals reinforced their
education campaign by placing posters in clini- Less frequently mentioned barriers included
cal areas, break rooms, dining rooms, and on time constraints, use of contract staff, physi-
bulletin boards. One hospital placed laminated cians not directly employed by the hospital, and
copies of the unapproved list on every chart, the ongoing need to educate new residents and
while another reported removing unapproved nursing graduates. As one interviewee stated,
abbreviations from all standard forms. Since medical and nursing schools are not teach-
Facilitators named by no more than 1 interviewee ing the prohibitive abbreviations . . . it makes our
included using a multipronged approach, having job harder.
a sustained initiative, keeping communication
open and free flowing, and establishing the impor- Barriers to Adoption: Most Challenging Practice
tance of patient safety.
Interviewees were also asked to identify their most
Barriers to Adoption and Strategies challenging program for a detailed discussion about
to Overcome Barriers barriers to adoption. Challenging was defined as a
program with numerous setbacks, obstacles, and/or
Resistance to change: The challenge of chang- difficulties resulting in unanticipated delays or fail-
ing physician and staff behavior was the most ure to meet program goals. The most frequently cited
Downloaded from ajm.sagepub.com at UNIV OF VIRGINIA on September 6, 2015
AMERICAN JOURNAL OF MEDICAL QUALITY 10 National Quality Forum Safe Practices 329
practice (3/8) was ensuring transfer of relevant along the continuum of care. As one respondent
patient information. None of the remaining initia- stated, It just seems like there are so many
tives was considered challenging by more than 1 hos- facets to information transfer . . . its a very
pital participant; therefore, only information transfer complex problem. Another hospital interviewee
is included in this discussion. noted, The biggest problem we find as we inves-
Information transfer includes implementation of tigate [medication-related] events is theres a
a process for obtaining and documenting a complete communication deficit somewhere.
list of the patients medications upon admission, dis- Strategies to overcome barriers: Education and
charge, and transfer to another setting, provider, or training were commonly used strategies to
level of care within or outside the organization.4 Of increase awareness of this problem, to empha-
the 3 hospitals that chose to discuss this initiative, size the need for improved communication, and
1 had a fully operational program, while the remain- to stress the importance of medication recon-
ing hospitals were in the early stages of design and ciliation to ensure patient safety.
implementation. Barriers to adoption and strategies
to overcome these barriers are described below. Prioritization and Piggybacking of Initiatives
Barriers to Adoption and Strategies Hospitals participants reported prioritizing initia-
to Overcome Barriers tives based on several factors, including (1) JCAHO
mandates, (2) internal gaps in performance, (3) scale
Physician and staff resistance: Convincing clin- of the initiative, (4) financial constraints, (5) number
ical staff to adopt this initiative has been a of resources involved, and (6) risk to patient safety.
major impediment for the 3 hospitals. One With respect to piggybacking initiatives, 3 of the 8
interviewee underscored this barrier when she hospitals reported having initiatives running con-
noted, currently, but results were mixed. One interviewee
Its the expectation . . . that we have to reconcile was neutral as to the benefits of this approach,
medication across settings or with a previous 1 considered it burdensome, and the third believed
provider [whatever retail pharmacy the patient it was beneficial because common resources were
uses] . . . and you know how chaotic it is in the used in both initiatives. Some of these initiatives
ER . . . they dont have time to do sit down and call just dovetail together . . . once youre monitoring one
the pharmacy and reconcile patient medica- you might as well monitor others.
tions . . . but thats the expectation . . . so just get-
ting employees past the mindset . . . they just flat Adoption of a COS
cannot do it, cannot fit it into their workday, no
way, shape, form, or fashion, thats a hurdle in
A total of 11 hospitals responded to our initial
itself . . . you know, how logistically do you do it?
request for an interview. One interviewee, however,
Strategies to overcome barriers: Education, was not able to find the time to participate; thus,
training, and coaching were commonly used 10 hospital interviews were conducted. One of the
techniques to confront resistance. In addition, 10 interviews was conducted with 2 participants,
1 hospital is in the midst of developing better a director of quality and a performance improve-
communication tools such as summary reports, ment coordinator. Among the remaining partici-
rounding tools, and patient safety tools to facili- pants, 2 were directors of quality, 2 were directors
tate the medication reconciliation process. of quality management, 2 were directors of clinical
The same hospital recently implemented an quality/performance improvement, 1 was a direc-
electronic medical record system that made tor of nursing, 1 was a director of patient safety,
this change a lot easier . . . the IS department and 1 was a director of performance improvement.
and the pharmacists developed an admissions With an average of 5 years in their positions at the
report that would capture the patients current hospitals, the interviewees had in-depth knowl-
list of medications . . . so all the physician had to edge of their hospitals COS activities.
do is place a check in the box to indicate if the
medication was to be continued. Interaction/Knowledge of the Hospital Unit
Complexity of the problem: Medication recon-
ciliation can be a difficult process to implement The informants reported low-to-moderate interac-
because it affects numerous transition points tion and/or knowledge of the individual hospital
Downloaded from ajm.sagepub.com at UNIV OF VIRGINIA on September 6, 2015
330 Blake et al AMERICAN JOURNAL OF MEDICAL QUALITY
units. Some of the interviewees spend time with most important initiatives for the hospitals future.
nurses and clinical staff on the unit level when Frequency of reporting, communication openness,
implementing or overseeing a new patient safety ini- hospital management support for patient safety,
tiative, and troubleshooting on the hospital unit also and hospital handoffs and transitions each were
occasionally takes place. However, regular and ongo- discussed by 2 of the participants as the most sig-
ing unit-level interaction does not generally occur. nificant COS dimension adopted by their hospitals.
Definition of COS Facilitators to Adoption
Definitions of COS ranged from very broad con- After identifying the 2 most important COS
cepts of hospital safety to more specific ideas of dimensions adopted by their hospitals, the partici-
having a blame-free environment that promotes pants were asked to identify the factors that con-
patient safety and satisfaction. COS was reported tributed to the adoption of each COS dimension.
as a way of functioning, an awareness of staff, They were then asked to identify the most signifi-
an essence, or a sense that safety comes first. cant facilitator that resulted in adoption of the COS
Two of the informants indicated that having a just dimension. These facilitators are described below.
culture is important for their hospital. Several
interviewees explained that COS means letting Senior leadership: The support of senior hospi-
their hospital staff know that safety is a number tal leaders was the most significant facilitator to
one priority. It also means keeping staff account- the adoption of a COS. Informants reported that
able for their errors even though the system sets having senior leadership and corporate support
up people for failure. The informants reported enabled the hospital to adopt a blame-free envi-
that they relied heavily on written materials to ronment and to establish an environment in
form the basis of their understanding of COS. which communication is open and staff mem-
These materials include journal articles and publi- bers feel comfortable expressing their feelings
cations from organizations such as the JCAHO, the and concerns. As one interviewee stated, If
Institute for Healthcare Improvement, GHA, and theyre [senior leadership] willing to be open,
the Georgia Department of Human Resources. then the rest of us can be, but if youve got lead-
ership that wants errors swept under the carpet
Most Important COS Dimension Adopted because they are afraid its going to make them
look bad, youll never get it. The leadership and
Participants were asked to identify which of the support of the hospital CEO was mentioned by
11 COS dimensions were adopted by their hospital 6 interviewees as being an especially important
and to discuss which 2 were the most important or facilitator for patient safety.
significant to the hospital. The most important COS Open and clear communication: Having an envi-
dimension adopted by the hospitals was nonpuni- ronment within the hospital that promotes open
tive response to error, or a blame-free environment. and clear communication across hospital staff
Six of the 10 participants listed this dimension as was reported as an important facilitator for the
most important or significant to their hospitals adoption of a COS. An open and transparent
COS. Informants suggested that the most effective channel of communication allows staff to feel
way to ensure a blame-free environment is to edu- comfortable about reporting errors, it provides
cate staff about the need for reporting and to assure education and training to staff about patient
staff that it can be done without retribution. safety initiatives, and it promotes teamwork
The next most important COS dimension was within and among hospital units. One respon-
teamwork within hospital units, with 4 informants dent stated that openness has particularly
reporting this to be one of the most important COS helped allay some staff fears about reporting
dimensions adopted by their hospitals. Leadership errors: By being open, weve shown staff that
support and education about the need for this ini- theres no hidden agenda . . . being open is the
tiative are key to this dimensions success. One of first thing they need to see. One hospital
the 4 hospitals that discussed teamwork within reported being able to successfully implement a
hospital units at great length has not yet adopted COS because of its new administrations commu-
this COS dimension but believes it is one of the nication system. We have a new administration
Downloaded from ajm.sagepub.com at UNIV OF VIRGINIA on September 6, 2015
AMERICAN JOURNAL OF MEDICAL QUALITY 10 National Quality Forum Safe Practices 331
that promotes a very openness in communica- communication and specifically patient safety,
tion, and is very quick to recognize systems prob- having the data to support the need for patient
lems and not people problems, so to speak. safety improvement and the value of new ini-
Education and training: Participants explained tiatives, having an awards-based system that
that the education and training of staff and man- encourages the reporting of errors, and having
agement has been critically important for the staff and/or peer pressure that encourages a COS.
adoption of a COS within their hospitals. Most
education and training initiatives have focused Barriers to Adoption and
on reporting errors and assuring staff that there Strategies to Overcome Barriers
is a blame-free environment. As one informant
stated, We really educated the staff on why we Participants were asked to identify the barriers
needed to know when the errors occurred. Not they or their hospital had to overcome during the
that we wanted to get the person, but to look at course of adopting a COS. Then, they were asked to
problems that could be contributing to the report what strategies were implemented to over-
errors, and that way it would help us to help come these barriers and which, if any, barriers they
them to make things better. Participants also were unable to overcome. These barriers are
reported that the education and training must described below.
come from and be promoted by senior adminis-
tration. One hospitals senior management regu- Barriers to Adoption
larly shares error reports with all its staff
members in an effort to educate them about the Resistance to change: Informants explained that
problems occurring at the hospital. The inform- staff resistance to change is the most significant
ant feels that this is an important educational barrier to the adoption of a COS. Staff members,
experience for the staff and that it actually pro- particularly older staff, are more likely to resist
motes error reporting within the hospital. change because they have learned how to do
JCAHO and external pressure: Accreditation by things the old way. One participant described
the JCAHO and pressure by external sources this barrier as the idea that Im ok, but every-
serve as important facilitators for the adoption body else needs to change. Informants reported
of a COS. External sources usually included that the resistance to change causes conflicts
hospitals corporations, which tend to hold among staff members, thus affecting teamwork
hospitals accountable for patient safety. One within and even among hospital units. Inform-
informant stated that because the JCAHO ants find that resistance to change is an espe-
stresses patient safety in its accreditation cially challenging barrier for the hospitals
standards, the JCAHO served as a driving force efforts to create a blame-free environment. The
behind the hospitals COS activities. The informants, who are often in charge of oversee-
informant further explained, If you have no ing their hospitals error-reporting policies, have
accreditation [JCAHO] then you dont get reim- found this barrier to be very frustrating because
bursed and you dont stay open. A second par- many clinicians, particularly nurses, often state,
ticipant who stated that adopting a COS was Well, this is the way weve always done it, or
important for the hospital because it is the they are concerned and ask, Whats going to
right thing to do, listed the need for accredita- happen to me? Another informant is more posi-
tion as a close second. A third interviewee tive about overcoming this barrier: I think it
believes that the hospital is able to achieve a just takes time to get employees and probably
COS because JCAHO provides patient safety physicians more than anybody used to the idea
goals and sets clear deadlines for achieving that we can talk about it [error reporting] with-
these goals. It has especially helped the hospi- out it being a problem.
tals efforts to improve teamwork with the units. Fear and mistrust: Related to resistance to
Other facilitators: Participants listed several change is fear and mistrust. Informants reported
other facilitators for the adoption of a COS. that there is mistrust among staff, particularly
These facilitators include having a collaborative the more experienced staff members who have
team that supports patient safety goals, recogni- worked for years in hospitals that had a puni-
tion by all staff that there is a need to improve tive response to patient error reporting. Another
Downloaded from ajm.sagepub.com at UNIV OF VIRGINIA on September 6, 2015
332 Blake et al AMERICAN JOURNAL OF MEDICAL QUALITY
participant indicated that fear is a barrier to the necessary and possible. Another hospital has
hospitals establishment of an open communica- started to overcome this barrier with the help of
tion system. This barrier includes being afraid a nurse who comes to training sessions to share
of professional embarrassment, being afraid of with staff her particular experience with the
being wrong, being afraid of retaliation, being nonpunitive error-reporting system. By having
afraid of being alienated. A third participant her explain her experience, staff members are
indicated that there is a fear among staff of liti- assured that they will not be penalized for
gation related to patient errors. I think that is a reporting errors and will learn how important it
part of our culture, when people feel very pro- is for improving patient safety. A third hospital
tective and somewhat defensive because they encourages its managers to regularly stress the
are concerned about sitting on a witness stand, blame-free environment policies at their
or being sued, or having some risk. So, I think monthly staff meetings. Another informant has
our culture over time will shift, as we are more learned that changing behavior is almost impos-
and more supportive of safety culture. But it is sible to achieve, but the informant finds hope in
my guess that thats pretty well ingrained for the new blood, the newer and younger staff
people in health care. members whom the hospital can properly train
Poor communication: Poor communication and educate about its blame-free environment.
among staff has hampered hospitals efforts to Strategies to improve communication: As with
implement a COS. One informant stated that changing behavior, hospitals are educating their
poor communication exists because of the staff to improve communication. Training and
nature of hospitals as silos. The informant educational efforts focus on teamwork within
further explained that hospitals by nature are and across hospital units, among managers and
organized into different departments that are other hospital leaders, and on the need for and
isolated and tend not to communicate with one value of error reporting. One participant feels
another. Another hospital finds poor communi- that educating managers is critical to improving
cation to be a barrier to error reporting. The communication. We want to make sure its a
lack of communication exists at the clinical 2-way communication, and I think keeping them
level and the more administrative/senior level. [managers] up-to-date and informed, letting
Knowledge is power, and we werent really them know where we need the help and what
taking the information to the department resources we need is helpful. Another informant
directors and the staff-level people like we suggested that communication could be
should, or the governing board for that matter. improved if senior leaders, particularly hospital
Medical staff tend to be left out in discussions CEOs, would better promote the need for a COS.
about errors as well, which one hospital has
acknowledged and tried to correct. Poor com-
DISCUSSION
munication has also been a problem for
another hospital that has experienced high Using a qualitative approach, we identified major
turnover in both management and clinical facilitators and barriers to the implementation of
staff. These staffing changes affect almost all of programs that support NQF safe practices around
the COS dimensions. medication processes and a COS. Hospitals that
participated in the interviews identified significant
Strategies to Overcome Barriers as well as other key factors that resulted in the
adoption and/or nonadoption of 2 self-selected prac-
Strategies to change behavior: Constant educa- tices. Informants also identified strategies used to
tion and reassurance of staff that they will not overcome barriers that were experienced.
be penalized for reporting their errors has been Common among both patient safety interviews
the most popular strategy employed by the par- was the value of administrative leadership and
ticipant hospitals. One hospital conducts one- support. Patient safety initiatives were easiest to
on-one sessions with physicians to personally adopt because of the strong commitment of senior
explain to them why blame-free reporting is hospital leaders such as hospital executives, physician
Downloaded from ajm.sagepub.com at UNIV OF VIRGINIA on September 6, 2015
AMERICAN JOURNAL OF MEDICAL QUALITY 10 National Quality Forum Safe Practices 333
leaders, and department managers. Several partici- doing well in implementing these practices. The
pants reported that the adoption of patient safety extent to which this biased our conclusions is
initiatives was most successful with the help of a unknown. Each hospitals performance ranking
champion such as a CEO or pharmacist. These cham- was based on voluntarily provided self-assessment.
pions were largely responsible for driving 1 or more Interviewees were asked to quantify the extent to
patient safety initiatives. which their hospitals adopted each of the 10 safety
The participants also revealed that education practices. The hospital-reported ratings have not
and training have helped raise awareness about been independently verified for accuracy.
patient safety. These educational efforts included An additional limitation to this study was the
formal and informal approaches to patient safety, self-selection of patient safety practices. Hospital
and they have targeted medical staff and adminis- participants in both the medication process and COS
trators as well. Participants also suggested that for interviews were allowed to self-select the patient
these educational efforts to really be effective, they safety practices with which their hospital had the
must be constant, always reinforcing the message most success. In the medication process interviews,
of patient safety. informants also identified the patient safety practice
Resistance to change was the most significant bar- with which their hospital had the least success.
rier identified in the safe medication process inter- There are limitations to this approach because there
views and the COS interviews. Most of the study were no data to support these hospitals best or
participants explained that physicians as well as worst practices, nor were there any specific guide-
nurses, especially those who have been in practice for lines to define success. Thus, participants selections
many years, have the most difficult time adapting to of these patient safety practices might be biased to
new patient safety policies and procedures. These reflect areas in which the hospitals have more suc-
clinicians struggle with these policies and proce- cess or are doing better than in actual practice.
dures, including the adoption of standard abbrevia- Despite these limitations, this research study
tions and the acceptance of the hospitals blame-free has many strengths. First, it is the only known
environment, because they are used to doing things qualitative study to examine NQF patient safety
the old way. The informants reported that educa- initiatives adopted by Georgia hospitals. The
tion and positive reinforcement are strategies their researchers have gathered invaluable information
hospitals have used to change behavior. For the most about the facilitators and barriers to 2 important
part, these strategies have been successful. NQF patient safety programs: medication process
Many participants in this study sought advice practices and COS initiatives. Second, the involve-
and/or suggestions for implementing their hospitals ment of the hospitals quality assurance and/or
programs from key organizations such as the patient safety directors strengthens the validity of
JCAHO, PHA, and the Institute for Safe Medication the data because most of these informants oversee
Practices. Strategies for achieving safe medication and monitor their hospitals patient safety practices.
goals of minimizing abbreviations, minimizing ver- In addition, the research findings are timely and
bal orders, and COS are available on their respective provide current patient safety practices adopted by
Web sites. In addition, the JCAHO has made compli- Georgia hospitals.
ance with 4 NQF safe medication processes manda- In conclusion, implementing safety practices can
tory for accreditation. be a difficult process, replete with organizational,
There were some limitations to this study. First, financial, and professional barriers. Strategies
we attempted to include an equal proportion of top- identified by our informants to overcome these bar-
and lower-performing hospitals in the 2 interview riers may assist other hospitals currently facing
groups. Although we achieved this goal for hospi- this challenge. These strategies include educating
tals participating in the medication process inter- staff about safety practices and providing positive
views, the COS sample consisted of a relatively reinforcement by hospital administrators. Although
high percentage of bottom-performing hospitals full implementation of patient safety practices is
(60% vs 40% top performers). Because recruitment an ongoing process, hospital participants were gen-
efforts were coordinated by PHA, we were unable erally pleased with their progress and anxious to
to actively solicit additional hospitals that were keep moving forward.
Downloaded from ajm.sagepub.com at UNIV OF VIRGINIA on September 6, 2015
334 Blake et al AMERICAN JOURNAL OF MEDICAL QUALITY
REFERENCES 3. Nieva VF, Sorra J. Safety Culture Assessment: a tool for
improving patient safety in healthcare organizations. Qual
1. Kohn LT, Corrigan JM, Donaldson MS, eds. To Err Is Human: Saf Health Care. 2003;12(Suppl. 2):ii17-ii23.
Building a Safer Health System: A Report From the Committee 4. Joint Commission on Accreditation of Healthcare Organiza-
on Quality of Healthcare in America. Washington, DC: National tions. 2005 hospitals national patient safety goals. Available
Academy Press; 1999. at: http://www.jcaho.org/accredited+orgainizations/patient+
2. National Quality Forum. Safe Practices for Better Healthcare: A safety+/05+npsg/05_npsg_hap.htm.
Consensus Report (NQF Publication No. NQFCR-05-03).
Washington, DC: National Quality Forum; 2003.
Downloaded from ajm.sagepub.com at UNIV OF VIRGINIA on September 6, 2015
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Antisepsis, Disinfection PDFDocument379 pagesAntisepsis, Disinfection PDFsatmayaniPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Bahasa CinaDocument13 pagesBahasa CinasatmayaniPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Effect of Stress Management Training Through PRECEDE-PROCEED Model On Occupational Stress Among Nurses and Midwives at Iran Hospital, IranshahrDocument5 pagesThe Effect of Stress Management Training Through PRECEDE-PROCEED Model On Occupational Stress Among Nurses and Midwives at Iran Hospital, IranshahrsatmayaniPas encore d'évaluation
- "Q" Umentation in Nursing: Recording For Quality Client CareDocument6 pages"Q" Umentation in Nursing: Recording For Quality Client CaresatmayaniPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- An Assessment of Psychological Need in Emergency Medical Staff in The Northern Health and Social Care Trust AreaDocument7 pagesAn Assessment of Psychological Need in Emergency Medical Staff in The Northern Health and Social Care Trust AreasatmayaniPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Petunjuk Buat PenulisDocument11 pagesPetunjuk Buat PenulissatmayaniPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Reliability and Validity of The Turkish Version of The Job Performance Scale InstrumentDocument9 pagesReliability and Validity of The Turkish Version of The Job Performance Scale InstrumentsatmayaniPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Archives of Pathology & Laboratory Medicine Nov 1997 121, 11 Proquest Nursing JournalsDocument6 pagesArchives of Pathology & Laboratory Medicine Nov 1997 121, 11 Proquest Nursing JournalssatmayaniPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Contoh Jurnal Asian Nursing ResearchDocument7 pagesContoh Jurnal Asian Nursing ResearchsatmayaniPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- De Mortel 2012Document10 pagesDe Mortel 2012satmayaniPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Job Stressors and Social Support Behaviors: Comparing Intensive Care Units To Wards in JordanDocument14 pagesJob Stressors and Social Support Behaviors: Comparing Intensive Care Units To Wards in JordansatmayaniPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Archives of Pathology & Laboratory Medicine Nov 1997 121, 11 Proquest Nursing JournalsDocument6 pagesArchives of Pathology & Laboratory Medicine Nov 1997 121, 11 Proquest Nursing Journalssatmayani100% (1)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Role of The Sign-Off Mentor in The Community Setting: Karen CooperDocument6 pagesThe Role of The Sign-Off Mentor in The Community Setting: Karen CoopersatmayaniPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Stress &healthDocument18 pagesStress &healthsatmayaniPas encore d'évaluation
- Introduction To FluidizationDocument9 pagesIntroduction To FluidizationEriCisacPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Bulletin PDFDocument2 pagesBulletin PDFEric LitkePas encore d'évaluation
- Instruction Manual 115cx ENGLISHDocument72 pagesInstruction Manual 115cx ENGLISHRomanPiscraftMosqueteerPas encore d'évaluation
- Nyamango Site Meeting 9 ReportDocument18 pagesNyamango Site Meeting 9 ReportMbayo David GodfreyPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Helipal Tbs Powercube ManualDocument29 pagesHelipal Tbs Powercube Manualoualid zouggarPas encore d'évaluation
- Heart Rate Variability Threshold As An Alternative.25Document6 pagesHeart Rate Variability Threshold As An Alternative.25Wasly SilvaPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- San Mateo Daily Journal 01-28-19 EditionDocument28 pagesSan Mateo Daily Journal 01-28-19 EditionSan Mateo Daily JournalPas encore d'évaluation
- Mahatma Gandhi University: Priyadarshini Hills, Kottayam-686560Document136 pagesMahatma Gandhi University: Priyadarshini Hills, Kottayam-686560Rashmee DwivediPas encore d'évaluation
- Autodesk Nastran In-CAD PDFDocument43 pagesAutodesk Nastran In-CAD PDFFernando0% (1)
- Angelo (Patrick) Complaint PDFDocument2 pagesAngelo (Patrick) Complaint PDFPatLohmannPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Nikasil e AlusilDocument5 pagesNikasil e AlusilIo AncoraioPas encore d'évaluation
- 2011-11-09 Diana and AtenaDocument8 pages2011-11-09 Diana and AtenareluPas encore d'évaluation
- Simon Fraser University: Consent and Release FormDocument1 pageSimon Fraser University: Consent and Release FormpublicsqPas encore d'évaluation
- Learning TheoryDocument7 pagesLearning Theoryapi-568999633Pas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- R15 Understanding Business CyclesDocument33 pagesR15 Understanding Business CyclesUmar FarooqPas encore d'évaluation
- Empanelled Hospitals List Updated - 06-12-2022 - 1670482933145Document19 pagesEmpanelled Hospitals List Updated - 06-12-2022 - 1670482933145mechmaster4uPas encore d'évaluation
- Abc Uae Oil and GasDocument41 pagesAbc Uae Oil and GasajayPas encore d'évaluation
- Community Resource MobilizationDocument17 pagesCommunity Resource Mobilizationerikka june forosueloPas encore d'évaluation
- Agm 1602W-818Document23 pagesAgm 1602W-818Daniel BauerPas encore d'évaluation
- SahanaDocument1 pageSahanamurthyarun1993Pas encore d'évaluation
- Case Study On Goodearth Financial Services LTDDocument15 pagesCase Study On Goodearth Financial Services LTDEkta Luciferisious Sharma0% (1)
- Corporate Restructuring Short NotesDocument31 pagesCorporate Restructuring Short NotesSatwik Jain57% (7)
- Pautas Anatómicas para La Inserción de Minitornillos: Sitios PalatinosDocument11 pagesPautas Anatómicas para La Inserción de Minitornillos: Sitios PalatinosValery V JaureguiPas encore d'évaluation
- ArrowrootDocument8 pagesArrowrootSevi CameroPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Assignment RoadDocument14 pagesAssignment RoadEsya ImanPas encore d'évaluation
- Chapter 1 4Document76 pagesChapter 1 4Sean Suing100% (1)
- HPCL CSR Social Audit ReportDocument56 pagesHPCL CSR Social Audit Reportllr_ka_happaPas encore d'évaluation
- Epistemology and OntologyDocument6 pagesEpistemology and OntologyPriyankaPas encore d'évaluation
- Course DescriptionDocument54 pagesCourse DescriptionMesafint lisanuPas encore d'évaluation
- B0187 B0187M-16Document9 pagesB0187 B0187M-16Bryan Mesala Rhodas GarciaPas encore d'évaluation
- Guidelines for Initiating Events and Independent Protection Layers in Layer of Protection AnalysisD'EverandGuidelines for Initiating Events and Independent Protection Layers in Layer of Protection AnalysisÉvaluation : 5 sur 5 étoiles5/5 (1)